Abstract
Alzheimer’s disease (AD) is the most common neurodegenerative disease in the world. The “amyloid hypothesis” is one of the predominant hypotheses for the pathogenesis of AD. Besides, tau protein accumulation, calcium homeostasis disruption, and glial cell activation are also remarkable features in AD. Recently, there are some reports showing that TRPC channels may function in AD development, especially TRPC6. In this chapter, we will discuss the evidence for the involvement of TRPC channels in Alzheimer’s disease and the potential of therapeutics for AD based on TRPC channels.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
7.1 Introduction
Alzheimer’s disease (AD) is one of the most common neurodegenerative diseases leading to dementia in the aged, affecting 48 million people worldwide in 2015. The prevalence is estimated that 1 in 85 persons would be living with AD by 2050, according to a report by Johns Hopkins University [12]. Clinically, AD is characterized with memory decline, cognitive impairment, emotion swings, language breakdown, and bodily function lost at the final stage [76]. Synaptic dysfunction is suggested to be responsible for the clinical manifestations, and synapse loss is found to be best correlated with the dementia degree [88]. Pathologically, AD is characterized with metabolism decline in the parietal lobe of the cerebral cortex, brain atrophy, senile plaques, and neurofibrillary tangles in autopsied AD brain sections [34]. The presence of senile plaques and neurofibrillary tangles is required for the definitive diagnosis of Alzheimer’s disease [23]. Senile plaques are mainly composed of β-amyloid (Aβ) peptides, and neurofibrillary tangles are mainly composed of hyperphosphorylated tau protein. Due to the toxicity of Aβ peptides or tau protein to AD cell and animal models, Aβ or tau is proposed to be the causative agents for the pathogenesis of the disease, giving rise to “amyloid cascade hypothesis” and “tau hypothesis” [61].
The amyloid hypothesis suggests that due to genetic or environmental factors, the balance between Aβ production and clearance is disrupted, and Aβ is overaccumulated. Aβ would then aggregate into oligomers, which could attack synapses and neurons, leading to the injury of neurites and malfunction of synapses. Aβ would also interrupt the ion homeostasis of neurons, which would generate oxidative stress. Moreover, Aβ would disrupt the balance of kinase and phosphatase, leading to the hyperphosphorylation of tau protein and the formation of neurofibrillary tangles. Finally, Aβ would induce synapse loss and neuronal death, neural circuits’ destruction, and dementia [31]. The amyloid hypothesis is accepted in the field and supported by multiple lines of evidence. First, it has been found that in early-onset Alzheimer’s patients, who are usually familial inherited, several hundreds of mutations are located within amyloid precursor protein (APP) [5] or presenilin genes [18]. APP encodes the substrates of β-amyloid, and presenilins encode the catalytic subunit of the key enzyme in APP processing. Most of the mutations results in more Aβ production or enhancement of the ratio of Aβ42/Aβ40, leading to more Aβ aggregation [92]. Second, almost half of the late-onset Alzheimer’s patients, who are usually sporadic, carry the E4 allele of the ApoE gene [24]. ApoE encodes a protein related with Aβ production and clearance, and ApoE4 has a compromised function in Aβ production and clearance [39]. Third, Aβ is found to be toxic when applying to cultured cells [95] or animal models [35], and inhibition of Aβ generation or enhancement of its clearance is reported to improve the AD-like pathology [46, 65]. Most recently and importantly, treatment of mild to moderate Alzheimer’s patients with Aβ antibody led to a delay of the disease progression [20, 79].
Aβ is a peptide composed of 39–43 amino acids, with Aβ40 and Aβ42 as the two major forms. Aβ is generated from sequential cleavage of APP by enzymes named secretase. There are two types of APP cleavage, the “amyloidosis” pathway and “nonamyloidosis” pathway [26]. In the “amyloidosis” pathway, APP is first cleaved by β-secretase (β-site of APP-cleaving enzyme, BACE1), shedding the N terminal of APP (sAPPβ) and leaving the C terminal fragment (β-CTF, C99) on the membrane, where the β-CTF is intramembrane cleaved by γ-secretase (mainly composed of presenilin, Pen2, Aph1, and nicastrin), releasing the 39–43aa Aβ peptides and the APP intracellular domain (AICD). In the “nonamyloidosis” pathway, APP is first cleaved by α-secretases (carried out by ADAM10, 17, and 9) after the 16th aa of Aβ peptide, shedding sAPPα and leaving α-CTF (C83), and then α-CTF is cleaved by γ-secretase, leaving p3 and AICD. As α cleavage precludes Aβ formation and sAPPα is neurotrophic, the nonamyloidosis pathway is proposed to be protective for the disease [26]. The Aβ monomer is mainly secreted into extracellular space and then aggregates to oligomers and fibrils finally under certain conditions [75]. The Aβ fibril is the main component of senile plaques, and the oligomer is the most toxic form of Aβ [17]. Applying Aβ oligomers to primary cultured neurons [44] and mouse models [47, 77] is able to induce AD-like pathologies.
The physiological function of Aβ peptides is basically unclear. A low level of Aβ could promote neuronal survival, enhance synaptic plasticity [69], and stimulate neurotransmitter release in hippocampal neurons [1]. The mechanism underlying the neurotoxicity of Aβ has been widely investigated [81]. It could activate caspase through ER stress [63], death receptors [37], or JNK pathway [89], to induce neuronal apoptosis. Aβ could also bind to α7 nicotinic acetylcholine receptors (α7 nAChRs) [53], regulate synaptic NMDA receptor trafficking [82], induce synaptic protein degradation [41], and lead to the dysfunction of synapses. Moreover, Aβ could bind to the receptors on the astrocytes and microglia, leading to the activation of the glial cells and the release of cytokines and other inflammatory factors, which would induce the death of neurons [58, 94]. There is accumulating evidence suggesting that Aβ can disrupt the cellular Ca2+ homeostasis to induce synapse and neuronal loss. Thus, stabilizing cellular Ca2+ homeostasis might be the potential preventative and therapeutic strategies. Aβ might form a calcium channel on the membrane [40] or potentiate calcium influx through L-type calcium channels [90], and the cytosolic calcium elevation could activate calcium-dependent protease-calpain, which could cleave p35 to p25 and induce apoptosis [45].
7.2 Genetic Evidence for the Involvement of TRPC Channels in Alzheimer’s Disease
Besides APP, presenilin1, presenilin2, and ApoE, several single nucleotide polymorphisms (SNPs) at genes implicated in immune system (CR1, CD33, EPHA1), cholesterol/lipid metabolism (clusterin, ABCA7), and vesicle trafficking (PICAM, BIN1, CD2AP) have been discovered by genome-wide association studies (GWAS) to be associated with late-onset Alzheimer’s disease (LOAD) [7, 74]. These findings provide new implications for the understanding and therapy of the disease. The first genetic evidence linking TRPC channel to AD came from a study involving two extended pedigrees, each with 15–16 siblings, and among them 5–6 siblings are affected with LOAD [70, 71]. After genotypic analysis of the microarray data of the AD samples vs. the controls, six SNPs on chromosome 20q11.22 are found to be significant after Bonferroni correction, and all six SNPs are located in the gene of TRPC4AP (TRPC4-associated protein). In addition, a set of ten SNPs, including the above six SNPs, are analyzed, and haplotype analysis reveals that nine out of the ten affected siblings have a specific haplotype, and the genotype is homozygous, while genotypes for the control samples are generally heterozygous or opposite homozygous.
Extending the work to include 199 unrelated patients and 85 unaffected spouses to determine the prevalence of the TRPC4AP haplotypes, it is found that 36% of the patients have the haplotype, while only 26% of the spouse controls have the haplotype [70, 71]. It is also found that those patients with the haplotype might have more behavioral changes as well as psychiatric problems. Thus, the TRPC4AP haplotype is associated with late-onset Alzheimer’s disease, although the results are waiting to be replicated.
TRPC4AP is also named TNF-R1 ubiquitous scaffolding and signaling protein (TRUSS) and is originally identified in a yeast two-hybrid screen as a TNF-R1-associated protein. TRPC4AP is previously found to be a component of TNF-R1 signaling complexes involved in NF-κB pathway [83]. As indicated by its name, TRPC4AP also interacts with TRPC4 as well as TRPC1 and 5. In the context of reduced endoplasmic reticulum Ca2+ storage induced by enhanced G protein-coupled m1 muscarinic acetylcholine receptor (m1AchR) signaling, TRPC4AP, TRPC4, and TNF-R1 all elevate ER Ca2+ loading. Although the physiological or pathological significance of this ER Ca2+ loading elevation is unclear, it may indicate the malfunction of TRPC4 or its associated protein could lead to the development of Alzheimer’s disease.
In the analysis of the association of SNPs with AD in publicly available GWAS data set consisting of three cohorts using data mining methods [11], 199 SNPs mostly associated with genes in calcium signaling, cell adhesion, endocytosis, immune response, and synaptic function are identified. In the model building with prior biological knowledge, 19 SNPs within six genes are identified, and four SNPs in TRPC1 are relevant in AD. However, there is no direct functional evidence linking TRPC1 and AD. Previous studies have found that TRPC1 might be involved in store-operated calcium entry (SOCE) [66], which might be dysfunctional in AD [84]. However, the functional significance of these SNPs to TRPC1 is still unclear.
7.3 TRPC Channels and Calcium Signal in Alzheimer’s Disease
Cleavages of APP by α-/β-/γ-secretases and Aβ generation have been found to be regulated by various cellular signals, including calcium signal. The effects of elevated cytosolic calcium concentration on Aβ production are controversial, depending on the concentrations of drugs and different cell lines [9, 13]. PS1 can modulate capacitative calcium entry (CCE), and FAD-linked PS1 mutation inhibits CCE and promotes Aβ formation [96]. PS1 also interacts with IP3R and SERCA directly, while FAD-linked PS1 mutation enhances IP3R/SERCA activity and Aβ formation [14, 28]. Besides, a new calcium channel CALHM can enhance α-secretase cleavage of APP and suppress Aβ generation [21]. Recently, synaptic NMDA receptor activation elevates α-secretase activity and inhibits Aβ formation [33, 56]. In addition, ionomycin-induced calcium entry activates γ-secretase cleavage of E-cadherin [55]. All these works suggest that calcium signals contribute to APP cleavage and Aβ production.
The first work linking the TRPC channels with APP processing comes from a study on SH-SY5Y neuroblastoma cells, which express abundant M3 muscarinic acetylcholine receptors (mAchR). When stimulated by carbachol or oxoM, mAchR would activate the PLC-IP3 signal to induce the calcium release from the internal store, followed by CCE [72]. In the study, stimulation of SH-SY5Y cells with M3 mAchR agonist oxoM enhances sAPPα production, which is dependent on extracellular calcium influx, but not dependent on calcium mobilization from intracellular stores. Treatment of the cells with a nonselective inhibitor (Cd2+), an L-type channel inhibitor (nifedipine), an N-type channel inhibitor (conotoxin) (CgTx), an Na+/K+-ATPase inhibitor (ouabain), or the Na+/Ca2+ exchanger inhibitor (benzamil) did not affect oxoM-induced calcium entry pattern and sAPPα release. However, treatment with CCE inhibitor Gd3+ or SKF96365 dramatically reduces the Ca2+ entry or sAPPα release induced by oxoM [42]. The involvement of TRPC channels in the CCE and sAPPα release in SH-SY5Y cells is thus proposed. Moreover, TRPC1 is expressed in SH-SY5Y neuroblastoma cells assayed by RT-PCR analysis [10]. It remains unclear whether specific TRPC channels are involved in the CCE and sAPPα release in SH-SY5Y cells.
7.4 TRPC Channels and Glial Activation in Alzheimer’s Disease
Besides senile plaques, neuronal neurofibrillary tangles, and neuronal loss, gliosis is also common in AD brains, suggesting that glial activation contributes to the pathogenesis of AD [60, 62]. Glia are nonneuronal cells of the nervous systems, and their main function is to provide physical support and nutrients to neurons, insulate one neuron from another, and clear pathogens or dead neurons [3, 87]. Glia are more than “glue” in the nervous system, and the interaction between glia and neurons is essential for normal brain function [8, 25]. For instance, astrocytes could clear neurotransmitters within the synaptic cleft and prevent possible excitotoxicity caused by accumulation of neurotransmitters such as glutamate [73, 85, 86]. Astrocytes are also crucial for brain development [16], synaptic plasticity [2, 64], and synaptogenesis [15, 80]. Many diseases such as Alzheimer’s disease [57], Parkinson’s disease [32], and ALS [67] are accompanied with glial activation.
The Aβ plaques are usually surrounded by activated astrocytes, suggesting the important contribution of astrocytes in AD brains. On one hand, astrocytes could digest Aβ. The cultured adult mouse astrocytes migrate to the plaques in response to monocyte chemoattractant protein-1 (MCP-1), a chemokine present in AD lesions. Then, the astrocytes uptake and degrade Aβ42 [93]. Compared with wild-type astrocytes, astrocytes from the apolipoprotein E (ApoE)-knockout mice are deficient in internalizing and degrading Aβ. These results suggest that ApoE is essential for the astrocyte-mediated degradation of Aβ [43].
On the other hand, Aβ could activate astrocytes and induce their inflammatory responses. In transgenic mice expressing the Swedish double mutation of human amyloid precursor protein 695, interleukin (IL)-1β-positive astrocytes are around Aβ deposits before the age of 13 months. Transforming growth factor (TGF)-β1, TGF-β3, and IL-10- and IL-6-positive astrocytes are detectable in 13-month or older transgenic mouse brain [4]. Moreover, astrocytes release soluble inflammatory factors under Aβ stimulation and exacerbate Aβ-induced caspase3 activation and neuronal death. Once the activated astrocytes are treated with anti-inflammatory agent minocycline, the astrocytic inflammatory responses and the Aβ-induced caspase3 activation, caspase3-cleaved tau, and neuronal death are also reduced [27]. Taken together, these results suggest that inhibition of inflammatory activation of astrocytes might be beneficial for AD treatment.
As the calcium signaling through TRPC channels is necessary for astrocyte activation induced by diverse factors such as lipopolysaccharide (LPS), IL-17, and thrombin, it is possible that TRPC channels might also be involved in the Aβ-induced astrocyte activation. Indeed, Aβ42 treatment could enhance DHPG-induced Ca2+ signals and store-operated Ca2+ entry (SOCE) in cultured astrocytes. At the same time, Aβ42 treatment upregulates the expression of TRPC1 and TRPC5. Moreover, SOCE is also upregulated in untreated astrocytes from the AD mice compared with astrocytes from wild-type mice. Consistently, in APP KO astrocytes, SOCE activated by ER Ca2+ store depletion with CPA is greatly reduced, and the protein levels of TRPC1 and Orai1 are downregulated. Moreover, knockdown of APP in cultured wild-type astrocytes reduces ATP- and CPA-induced ER Ca2+ release, extracellular Ca2+ influx, and TRPC1 expression level [52].
Several members of TRPC family, including TRPC1, TRPC4, TRPC5, and TRPC6, are expressed in astrocytes [6, 30, 68], and their expression levels are increased with age [54]. Several studies have shown that TPRC channels play important roles in glial activation. When stimulated by exogenous LPS, cultured astrocytes could be activated and proliferate, upregulate glial fibrillary acidic protein, and secrete IL-6 and IL-1β. Simultaneously, LPS induces [Ca2+]i increase in astrocytes. SKF-96365, the TRPC channel blocker, inhibits the LPS-induced [Ca2+]i increase and astrocyte activation [51]. These results support the potential involvement of TRPC channels in LPS-induced astrocyte activation. Similarly, TRPC channels also play important roles in IL-17-induced astrocyte activation. IL-17 activates MAPK, PI3K/Akt, and NF-kB, leading to upregulation of MIP-1a in astrocytes, while SKF96365 inhibits IL-17-induced astrocyte activation and upregulation of MIP-1a [97].
Another study shows that TRPC3 is essential for thrombin-induced astrocyte activation. Thrombin, a major blood-derived serine protease, could leak into the brain parenchyma upon blood-brain barrier disruption and induce brain injury and astrogliosis. Thrombin treatment induces morphological changes, upregulation of S100B, and proliferation in cultured cortical astrocytes. Meanwhile, thrombin induces upregulation of TRPC3 at the protein level and increased Ca2+ influx after thapsigargin treatment. The TRPC3 upregulation is mediated through protease-activated receptor 1 (PAR-1), extracellular signal-regulated protein kinase, c-Jun NH2-terminal kinase, and NF-kB signaling. Finally, the thrombin-induced astrocyte activation could be inhibited by specific knockdown of TRPC3 using RNA interference and a selective TRPC3 inhibitor, pyrazole-3. These results suggest that calcium signaling through TRPC3 is necessary for thrombin-induced astrocyte activation [78].
7.5 TRPC6 in Alzheimer’s Disease
TRPC6 in the neurons could promote neuronal survival [38], synaptogenesis [98], and learning and memory [98]. Under the condition of brain ischemia, neuronal TRPC6 is degraded, and prevention of TRPC6 degradation is beneficial for neuronal survival [22]. Moreover, genetic disruption of TRPC6 in the autism patient leads to abnormal neuronal development, morphology, and function [29]. As neuronal survival, learning, and memory are compromised in AD, TRPC6 might play a role in AD development.
The pharmacological evidence to suggest the potential role of TRPC6 in AD comes from the studies using hyperforin as a TRPC6 channel agonist. Hyperforin, a phytochemical produced by the plant Hypericum perforatum, is one of the three main active constituents of St. John’s wort and the primary active constituent responsible for the antidepressant properties of its extracts. Some studies have identified TRPC6 as a specific target of hyperforin. The hyperforin-induced cation entry is highly specific and related to TRPC6 and could be inhibited by a dominant negative mutant of TRPC6. Hyperforin elevates the intracellular Ca2+ concentration by activating TRPC6 channels without activating the TRPC3 and TRPC4. Furthermore, the stimulative effect of hyperforin on neuronal axonal sprouting is TRPC6 dependent [49]. Further study shows that hyperforin modulates dendritic spine morphology in CA1 and CA3 pyramidal neurons of hippocampal slice cultures through the activation of TRPC6 channels. Hyperforin evokes intracellular Ca2+ transients which are sensitive to the TRPC channel blocker La3+, thus mimicking the effects of the BDNF on hippocampal pyramidal neurons [50]. These findings suggest that hyperforin is a selective agonist for TRPC6 channels.
Several studies have showed that hyperforin could reduce Aβ levels and improve behavioral performance in AD models. In rats injected with amyloid fibrils in the hippocampus, hyperforin could reduce amyloid deposit formation and therefore decrease the Aβ-induced neurotoxicity, reactive oxidative species, and behavioral impairments [19]. Moreover, a hyperforin derivative IDN5706 – tetrahydrohyperforin – also prevents the cognitive deficit and synaptic impairment in double transgenic APPswe/PSEN1ΔE9 mice in a dose-dependent manner. Tetrahydrohyperforin decreases the proteolytic processing of APP, total fibrillar and oligomeric forms of Aβ, tau hyperphosphorylation, and astrogliosis [36]. Further studies show that the target of tetrahydrohyperforin appears to be TRPC6 [59]. In this study, mouse hippocampal slices are incubated with tetrahydrohyperforin, the TRPC3/6/7 activator OAG, SKF96365, and Aβ oligomers. Tetrahydrohyperforin and OAG have a similar stimulating effect on fEPSPs, which is inhibited by SKF96365. Aβ oligomers induce fEPSP reduction which could be rescued by tetrahydrohyperforin. In wild-type mice, tetrahydrohyperforin improves the spatial memory, an effect that is neutralized by coadministration of SKF96365. There is a strong pharmacophore similarity of tetrahydrohyperforin and other reported TRPC6 agonists (IDN5522, OAG, and Hyp9). These findings indicate that hyperforin and its derivatives might be effective for AD treatment and highlight the potential protective roles of TRPC6 in AD.
The association of TRPC6 with AD is further implicated by an in vitro study [48]. The effects of two familial Alzheimer’s disease-linked presenilin2 mutants (N141I and M239V) and a loss-of-function presenilin2 mutant (D263A) on the TRPC6 channel activity are assessed. The co-expression of presenilin2 or its FAD mutants and TRPC6 in HEK293T cells abolishes agonist-induced TRPC6 activation without affecting agonist-induced Ca2+ entry. The inhibitory effect of presenilin2 and its FAD mutants could not be attributed to Aβ increase in the medium because Aβ treatment alone does not affect the TRPC6 channel activity. In contrast, the co-expression of a loss-of-function PS2 mutant and TRPC6 in HEK293T cells enhances agonist-induced Ca2+ entry. These results suggest that the wild-type or familial Alzheimer’s disease-linked presenilin2 mutants influence TRPC6 channel activity in HEK293T cells and the normal function of TRPC6 might be compromised in AD.
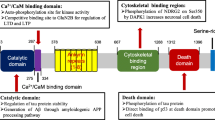
The direct evidence that TRPC6 is protective against AD comes from a work showing that TRPC6 modulates Aβ production [91]. The γ-secretase is a potential therapeutic target for AD, but its potent inhibitors would affect the normal function of γ-secretase which cleaves many substrates and lead to different side effects. The TRPC6 inhibits Aβ production by specifically interacting with APP and C99 to block the cleavage of C99 by the γ-secretase. The inhibitory effects are specific to APP, but not to Notch or other substrates tested. The substrate specificity is conferred by the specific interaction of TRPC6 with APP (C99), but not with other substrates. Once TRPC6 binds to C99, the interaction between C99 and presenilin1 (PS1) is reduced. The TRPC6 domain responsible for the inhibitory effects is identified, and a fusion peptide derived from the second transmembrane domain of TRPC6 could also reduce Aβ levels without effects on Notch cleavage. Moreover, crossing APP/PS1 mice with TRPC6 transgenic mice leads to a marked reduction in both plaque load and Aβ levels and improvement in structural and behavioral impairment. The TRPC6-derived peptide also reduces Aβ levels in APP/PS1 mice.
7.6 Conclusion and Perspectives
Most studies show indirect evidence linking the TRPC channels and Alzheimer’s disease. However, direct evidence shows that TRPC6 is protective against AD. Reducing Aβ production by enhancing TRPC6 is specifically valuable under the circumstances that all the γ-secretase inhibitors failed in the clinical trials, largely due to the severe side effects. Inhibiting APP and presenilin interaction by TRPC6 may represent a novel and viable strategy to target Alzheimer’s disease. The potential of TRPC6-based therapies such as hyperforin and TRPC6-derived peptide deserves further evaluation.
References
Abramov E, Dolev I, Fogel H, Ciccotosto GD, Ruff E, Slutsky I (2009) Amyloid-beta as a positive endogenous regulator of release probability at hippocampal synapses. Nat Neurosci 12(12):1567–1576. doi:10.1038/nn.2433
Allen NJ, Barres BA (2005) Signaling between glia and neurons: focus on synaptic plasticity. Curr Opin Neurobiol 15 (5):542–548. doi:S0959-4388(05)00125-X [pii]10.1016/j.conb.2005.08.006
Allen NJ, Barres BA (2009) Neuroscience: glia – more than just brain glue. Nature 457 (7230):675–677. doi:457675a [pii]10.1038/457675a
Apelt J, Schliebs R (2001) Beta-amyloid-induced glial expression of both pro- and anti-inflammatory cytokines in cerebral cortex of aged transgenic Tg2576 mice with Alzheimer plaque pathology. Brain Res 894(1):21–30
Benilova I, Karran E, De Strooper B (2012) The toxic Abeta oligomer and Alzheimer’s disease: an emperor in need of clothes. Nat Neurosci 15(3):349–357. doi:10.1038/nn.3028
Beskina O, Miller A, Mazzocco-Spezzia A, Pulina MV, Golovina VA (2007) Mechanisms of interleukin-1beta-induced Ca2+ signals in mouse cortical astrocytes: roles of store- and receptor-operated Ca2+ entry. Am J Phys Cell Phys 293 (3):C1103–C1111. doi:00249.2007 [pii]10.1152/ajpcell.00249.2007
Bettens K, Sleegers K, Van Broeckhoven C (2013) Genetic insights in Alzheimer’s disease. Lancet Neurol 12(1):92–104. doi:10.1016/S1474-4422(12)70259-4
Bezzi P, Volterra A (2001) A neuron-glia signalling network in the active brain. Curr Opin Neurobiol 11(3):387–394
Bojarski L, Herms J, Kuznicki J (2008) Calcium dysregulation in Alzheimer’s disease. Neurochem Int 52(4–5):621–633. doi:10.1016/j.neuint.2007.10.002
Bollimuntha S, Singh BB, Shavali S, Sharma SK, Ebadi M (2005) TRPC1-mediated inhibition of 1-methyl-4-phenylpyridinium ion neurotoxicity in human SH-SY5Y neuroblastoma cells. J Biol Chem 280(3):2132–2140. doi:10.1074/jbc.M407384200
Briones N, Dinu V (2012) Data mining of high density genomic variant data for prediction of Alzheimer’s disease risk. BMC Med Genet 13:7. doi:10.1186/1471-2350-13-7
Brookmeyer R, Johnson E, Ziegler-Graham K, Arrighi HM (2007) Forecasting the global burden of Alzheimer’s disease. Alzheimers Dement J Alzheimers Assoc 3(3):186–191. doi:10.1016/j.jalz.2007.04.381
Brzyska M, Elbaum D (2003) Dysregulation of calcium in Alzheimer’s disease. Acta Neurobiol Exp 63(3):171–183
Cheung KH, Shineman D, Muller M, Cardenas C, Mei L, Yang J, Tomita T, Iwatsubo T, Lee VM, Foskett JK (2008) Mechanism of Ca2+ disruption in Alzheimer’s disease by presenilin regulation of InsP3 receptor channel gating. Neuron 58 (6):871–883. doi:S0896-6273(08)00367-X [pii]10.1016/j.neuron.2008.04.015
Christopherson KS, Ullian EM, Stokes CC, Mullowney CE, Hell JW, Agah A, Lawler J, Mosher DF, Bornstein P, Barres BA (2005) Thrombospondins are astrocyte-secreted proteins that promote CNS synaptogenesis. Cell 120 (3):421–433. doi:S0092-8674(04)01245-0 [pii]10.1016/j.cell.2004.12.020
Clarke LE, Barres BA (2013) Emerging roles of astrocytes in neural circuit development. Nat Rev Neurosci 14 (5):311–321. doi:nrn3484 [pii]10.1038/nrn3484
Dahlgren KN, Manelli AM, Stine WB, Jr., Baker LK, Krafft GA, LaDu MJ (2002) Oligomeric and fibrillar species of amyloid-beta peptides differentially affect neuronal viability. J Biol Chem 277 (35):32046–32053. doi:10.1074/jbc.M201750200M201750200 [pii]
Dillen K, Annaert W (2006) A two decade contribution of molecular cell biology to the centennial of Alzheimer’s disease: are we progressing toward therapy? Int Rev Cytol 254:215–300. doi:10.1016/S0074-7696(06)54005-7
Dinamarca MC, Cerpa W, Garrido J, Hancke JL, Inestrosa NC (2006) Hyperforin prevents beta-amyloid neurotoxicity and spatial memory impairments by disaggregation of Alzheimer’s amyloid-beta-deposits. Mol Psychiatry 11 (11):1032–1048. doi:4001866 [pii]10.1038/sj.mp.4001866
Doody RS, Thomas RG, Farlow M, Iwatsubo T, Vellas B, Joffe S, Kieburtz K, Raman R, Sun X, Aisen PS, Siemers E, Liu-Seifert H, Mohs R (2014) Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s disease. N Engl J Med 370(4):311–321. doi:10.1056/NEJMoa1312889
Dreses-Werringloer U, Lambert JC, Vingtdeux V, Zhao H, Vais H, Siebert A, Jain A, Koppel J, Rovelet-Lecrux A, Hannequin D, Pasquier F, Galimberti D, Scarpini E, Mann D, Lendon C, Campion D, Amouyel P, Davies P, Foskett JK, Campagne F, Marambaud P (2008) A polymorphism in CALHM1 influences Ca2+ homeostasis, Abeta levels, and Alzheimer’s disease risk. Cell 133 (7):1149–1161. doi:S0092-8674(08)00751-4 [pii]10.1016/j.cell.2008.05.048
Du W, Huang J, Yao H, Zhou K, Duan B, Wang Y (2010) Inhibition of TRPC6 degradation suppresses ischemic brain damage in rats. J Clin Invest 120 (10):3480–3492. doi:43165 [pii]10.1172/JCI43165
Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P, Cummings J, Delacourte A, Galasko D, Gauthier S, Jicha G, Meguro K, O'Brien J, Pasquier F, Robert P, Rossor M, Salloway S, Stern Y, Visser PJ, Scheltens P (2007) Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS-ADRDA criteria. Lancet Neurol 6(8):734–746. doi:10.1016/S1474-4422(07)70178-3
Farrer LA, Cupples LA, Haines JL, Hyman B, Kukull WA, Mayeux R, Myers RH, Pericak-Vance MA, Risch N, van Duijn CM (1997) Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA 278(16):1349–1356
Fields RD, Stevens-Graham B (2002) New insights into neuron-glia communication. Science 298 (5593):556–562. doi:10.1126/science.298.5593.556298/5593/556 [pii]
Gandy S (2005) The role of cerebral amyloid beta accumulation in common forms of Alzheimer disease. J Clin Invest 115(5):1121–1129. doi:10.1172/JCI25100
Garwood CJ, Pooler AM, Atherton J, Hanger DP, Noble W (2011) Astrocytes are important mediators of Abeta-induced neurotoxicity and tau phosphorylation in primary culture. Cell Death Dis 2:e167. doi:cddis201150 [pii]10.1038/cddis.2011.50
Green KN, Demuro A, Akbari Y, Hitt BD, Smith IF, Parker I, LaFerla FM (2008) SERCA pump activity is physiologically regulated by presenilin and regulates amyloid beta production. J Cell Biol 181 (7):1107–1116. doi:10.1083/jcb.200706171jcb.200706171 [pii]
Griesi-Oliveira K, Acab A, Gupta AR, Sunaga DY, Chailangkarn T, Nicol X, Nunez Y, Walker MF, Murdoch JD, Sanders SJ, Fernandez TV, Ji W, Lifton RP, Vadasz E, Dietrich A, Pradhan D, Song H, Ming GL, Gu X, Haddad G, Marchetto MC, Spitzer N, Passos-Bueno MR, State MW, Muotri AR (2015) Modeling non-syndromic autism and the impact of TRPC6 disruption in human neurons. Mol Psychiatry 20 (11):1350–1365. doi:mp2014141 [pii]10.1038/mp.2014.141
Grimaldi M, Maratos M, Verma A (2003) Transient receptor potential channel activation causes a novel form of [Ca 2+]I oscillations and is not involved in capacitative Ca 2+ entry in glial cells. J Neurosci 23 (11):4737–4745. doi:23/11/4737 [pii]
Hardy J, Selkoe DJ (2002) The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 297(5580):353–356. doi:10.1126/science.1072994
Hirsch EC, Breidert T, Rousselet E, Hunot S, Hartmann A, Michel PP (2003) The role of glial reaction and inflammation in Parkinson’s disease. Ann N Y Acad Sci 991:214–228
Hoey SE, Williams RJ, Perkinton MS (2009) Synaptic NMDA receptor activation stimulates alpha-secretase amyloid precursor protein processing and inhibits amyloid-beta production. J Neurosci 29(14):4442–4460. doi:10.1523/JNEUROSCI.6017-08.2009
Holtzman DM, Morris JC, Goate AM (2011) Alzheimer’s disease: the challenge of the second century. Sci Transl Med 3(77):77sr71. doi:10.1126/scitranslmed.3002369
Hsia AY, Masliah E, McConlogue L, Yu GQ, Tatsuno G, Hu K, Kholodenko D, Malenka RC, Nicoll RA, Mucke L (1999) Plaque-independent disruption of neural circuits in Alzheimer’s disease mouse models. Proc Natl Acad Sci U S A 96(6):3228–3233
Inestrosa NC, Tapia-Rojas C, Griffith TN, Carvajal FJ, Benito MJ, Rivera-Dictter A, Alvarez AR, Serrano FG, Hancke JL, Burgos PV, Parodi J, Varela-Nallar L (2011) Tetrahydrohyperforin prevents cognitive deficit, Abeta deposition, tau phosphorylation and synaptotoxicity in the APPswe/PSEN1DeltaE9 model of Alzheimer’s disease: a possible effect on APP processing. Transl Psychiatry 1:e20. doi:tp201119 [pii]10.1038/tp.2011.19
Ivins KJ, Ivins JK, Sharp JP, Cotman CW (1999) Multiple pathways of apoptosis in PC12 cells. CrmA inhibits apoptosis induced by beta-amyloid. J Biol Chem 274(4):2107–2112
Jia Y, Zhou J, Tai Y, Wang Y (2007) TRPC channels promote cerebellar granule neuron survival. Nat Neurosci 10 (5):559–567. doi:nn1870 [pii]10.1038/nn1870
Jiang Q, Lee CY, Mandrekar S, Wilkinson B, Cramer P, Zelcer N, Mann K, Lamb B, Willson TM, Collins JL, Richardson JC, Smith JD, Comery TA, Riddell D, Holtzman DM, Tontonoz P, Landreth GE (2008) ApoE promotes the proteolytic degradation of Abeta. Neuron 58 (5):681–693. doi:S0896-6273(08)00328-0 [pii]10.1016/j.neuron.2008.04.010
Kawahara M, Kuroda Y (2000) Molecular mechanism of neurodegeneration induced by Alzheimer’s beta-amyloid protein: channel formation and disruption of calcium homeostasis. Brain Res Bull 53(4):389–397
Kelly BL, Ferreira A (2006) beta-Amyloid-induced dynamin 1 degradation is mediated by N-methyl-D-aspartate receptors in hippocampal neurons. J Biol Chem 281 (38):28079–28089. doi:M605081200 [pii]10.1074/jbc.M605081200
Kim JH, Choi S, Jung JE, Roh EJ, Kim HJ (2006) Capacitative Ca2+ entry is involved in regulating soluble amyloid precursor protein (sAPPalpha) release mediated by muscarinic acetylcholine receptor activation in neuroblastoma SH-SY5Y cells. J Neurochem 97(1):245–254. doi:10.1111/j.1471-4159.2006.03734.x
Koistinaho M, Lin S, Wu X, Esterman M, Koger D, Hanson J, Higgs R, Liu F, Malkani S, Bales KR, Paul SM (2004) Apolipoprotein E promotes astrocyte colocalization and degradation of deposited amyloid-beta peptides. Nat Med 10 (7):719–726. doi:10.1038/nm105nm1058 [pii]
Lacor PN, Buniel MC, Furlow PW, Clemente AS, Velasco PT, Wood M, Viola KL, Klein WL (2007) Abeta oligomer-induced aberrations in synapse composition, shape, and density provide a molecular basis for loss of connectivity in Alzheimer’s disease. J Neurosci 27 (4):796–807. doi:27/4/796 [pii]10.1523/JNEUROSCI.3501-06.2007
Lee MS, Kwon YT, Li M, Peng J, Friedlander RM, Tsai LH (2000) Neurotoxicity induces cleavage of p35 to p25 by calpain. Nature 405(6784):360–364. doi:10.1038/35012636
Leissring MA, Farris W, Chang AY, Walsh DM, Wu X, Sun X, Frosch MP, Selkoe DJ (2003) Enhanced proteolysis of beta-amyloid in APP transgenic mice prevents plaque formation, secondary pathology, and premature death. Neuron 40(6):1087–1093
Lesne S, Koh MT, Kotilinek L, Kayed R, Glabe CG, Yang A, Gallagher M, Ashe KH (2006) A specific amyloid-beta protein assembly in the brain impairs memory. Nature 440 (7082):352–357. doi:nature04533 [pii]10.1038/nature04533
Lessard CB, Lussier MP, Cayouette S, Bourque G, Boulay G (2005) The overexpression of presenilin2 and Alzheimer’s-disease-linked presenilin2 variants influences TRPC6-enhanced Ca2+ entry into HEK293 cells. Cell Signal 17 (4):437–445. doi:S0898-6568(04)00180-9 [pii]10.1016/j.cellsig.2004.09.005
Leuner K, Kazanski V, Muller M, Essin K, Henke B, Gollasch M, Harteneck C, Muller WE (2007) Hyperforin – a key constituent of St. John’s wort specifically activates TRPC6 channels. FASEB J 21 (14):4101–4111. doi:fj.07-8110com [pii]10.1096/fj.07-8110com
Leuner K, Li W, Amaral MD, Rudolph S, Calfa G, Schuwald AM, Harteneck C, Inoue T, Pozzo-Miller L (2013) Hyperforin modulates dendritic spine morphology in hippocampal pyramidal neurons by activating Ca(2+) -permeable TRPC6 channels. Hippocampus 23(1):40–52. doi:10.1002/hipo.22052
Li JH, Zhao ST, Wu CY, Cao X, Peng MR, Li SJ, Liu XA, Gao TM (2013) Store-operated Ca2+ channels blockers inhibit lipopolysaccharide induced astrocyte activation. Neurochem Res 38(10):2216–2226. doi:10.1007/s11064-013-1130-0
Linde CI, Baryshnikov SG, Mazzocco-Spezzia A, Golovina VA (2011) Dysregulation of Ca2+ signaling in astrocytes from mice lacking amyloid precursor protein. Am J Phys Cell Phys 300(6):C1502–C1512. doi:10.1152/ajpcell.00379.2010
Liu Q, Kawai H, Berg DK (2001) beta -Amyloid peptide blocks the response of alpha 7-containing nicotinic receptors on hippocampal neurons. Proc Natl Acad Sci U S A 98(8):4734–4739. doi:10.1073/pnas.081553598
Malarkey EB, Ni Y, Parpura V (2008) Ca2+ entry through TRPC1 channels contributes to intracellular Ca2+ dynamics and consequent glutamate release from rat astrocytes. Glia 56(8):821–835. doi:10.1002/glia.20656
Marambaud P, Shioi J, Serban G, Georgakopoulos A, Sarner S, Nagy V, Baki L, Wen P, Efthimiopoulos S, Shao Z, Wisniewski T, Robakis NK (2002) A presenilin-1/gamma-secretase cleavage releases the E-cadherin intracellular domain and regulates disassembly of adherens junctions. EMBO J 21(8):1948–1956. doi:10.1093/emboj/21.8.1948
Marcello E, Gardoni F, Mauceri D, Romorini S, Jeromin A, Epis R, Borroni B, Cattabeni F, Sala C, Padovani A, Di Luca M (2007) Synapse-associated protein-97 mediates alpha-secretase ADAM10 trafficking and promotes its activity. J Neurosci 27(7):1682–1691. doi:10.1523/JNEUROSCI.3439-06.2007
Meda L, Baron P, Scarlato G (2001) Glial activation in Alzheimer’s disease: the role of Abeta and its associated proteins. Neurobiol Aging 22 (6):885–893. doi:S0197458001003074 [pii]
Meda L, Cassatella MA, Szendrei GI, Otvos L Jr, Baron P, Villalba M, Ferrari D, Rossi F (1995) Activation of microglial cells by beta-amyloid protein and interferon-gamma. Nature 374(6523):647–650. doi:10.1038/374647a0
Montecinos-Oliva C, Schuller A, Parodi J, Melo F, Inestrosa NC (2014) Effects of tetrahydrohyperforin in mouse hippocampal slices: neuroprotection, long-term potentiation and TRPC channels. Curr Med Chem 21 (30):3494–3506. doi:CMC-EPUB-61425 [pii]
Mrak RE, Griffin WS (1996) Role of activated glia and of glial cytokines in Alzheimer’s disease: a review. EOS 16(3–4):80–84
Mudher A, Lovestone S (2002) Alzheimer’s disease-do tauists and baptists finally shake hands? Trends Neurosci 25(1):22–26
Nagele RG, Wegiel J, Venkataraman V, Imaki H, Wang KC (2004) Contribution of glial cells to the development of amyloid plaques in Alzheimer’s disease. Neurobiol Aging 25 (5):663–674. doi:10.1016/j.neurobiolaging.2004.01.007S0197458004001034 [pii]
Nakagawa T, Zhu H, Morishima N, Li E, Xu J, Yankner BA, Yuan J (2000) Caspase-12 mediates endoplasmic-reticulum-specific apoptosis and cytotoxicity by amyloid-beta. Nature 403(6765):98–103. doi:10.1038/47513
Navarrete M, Perea G, Fernandez de Sevilla D, Gomez-Gonzalo M, Nunez A, Martin ED, Araque A (2012) Astrocytes mediate in vivo cholinergic-induced synaptic plasticity. PLoS Biol 10 (2):e1001259. doi:10.1371/journal.pbio.1001259PBIOLOGY-D-11-02406 [pii]
Ohno M, Cole SL, Yasvoina M, Zhao J, Citron M, Berry R, Disterhoft JF, Vassar R (2007) BACE1 gene deletion prevents neuron loss and memory deficits in 5XFAD APP/PS1 transgenic mice. Neurobiol Dis 26(1):134–145. doi:10.1016/j.nbd.2006.12.008
Parekh AB, Putney JW Jr (2005) Store-operated calcium channels. Physiol Rev 85(2):757–810. doi:10.1152/physrev.00057.2003
Philips T, Robberecht W (2011) Neuroinflammation in amyotrophic lateral sclerosis: role of glial activation in motor neuron disease. Lancet Neurol 10 (3):253–263. doi:S1474-4422(11)70015-1 [pii]10.1016/S1474-4422(11)70015-1
Pizzo P, Burgo A, Pozzan T, Fasolato C (2001) Role of capacitative calcium entry on glutamate-induced calcium influx in type-I rat cortical astrocytes. J Neurochem 79(1):98–109
Plant LD, Boyle JP, Smith IF, Peers C, Pearson HA (2003) The production of amyloid beta peptide is a critical requirement for the viability of central neurons. J Neurosci 23(13):5531–5535
Poduslo SE, Huang R, Huang J (2009) The frequency of the TRPC4AP haplotype in Alzheimer’s patients. Neurosci Lett 450(3):344–346. doi:10.1016/j.neulet.2008.11.050
Poduslo SE, Huang R, Huang J, Smith S (2009) Genome screen of late-onset Alzheimer’s extended pedigrees identifies TRPC4AP by haplotype analysis. Am J Med Genet B Neuropsychiatr Genet Off Publ Int Soc Psychiatr Genet 150B(1):50–55. doi:10.1002/ajmg.b.30767
Putney JW Jr (1997) Type 3 inositol 1,4,5-trisphosphate receptor and capacitative calcium entry. Cell Calcium 21(3):257–261
Robinson MB (1998) The family of sodium-dependent glutamate transporters: a focus on the GLT-1/EAAT2 subtype. Neurochem Int 33(6):479–491
Rosenthal SL, Kamboh MI (2014) Late-onset Alzheimer’s disease genes and the potentially implicated pathways. Curr Genet Med Rep 2:85–101. doi:10.1007/s40142-014-0034-x
Roychaudhuri R, Yang M, Hoshi MM, Teplow DB (2009) Amyloid beta-protein assembly and Alzheimer disease. J Biol Chem 284 (8):4749–4753. doi:R800036200 [pii]10.1074/jbc.R800036200
Selkoe DJ (2004) Alzheimer disease: mechanistic understanding predicts novel therapies. Ann Intern Med 140 (8):627–638. doi:140/8/627 [pii]
Shankar GM, Li S, Mehta TH, Garcia-Munoz A, Shepardson NE, Smith I, Brett FM, Farrell MA, Rowan MJ, Lemere CA, Regan CM, Walsh DM, Sabatini BL, Selkoe DJ (2008) Amyloid-beta protein dimers isolated directly from Alzheimer’s brains impair synaptic plasticity and memory. Nat Med 14 (8):837–842. doi:nm1782 [pii]10.1038/nm1782
Shirakawa H, Sakimoto S, Nakao K, Sugishita A, Konno M, Iida S, Kusano A, Hashimoto E, Nakagawa T, Kaneko S (2010) Transient receptor potential canonical 3 (TRPC3) mediates thrombin-induced astrocyte activation and upregulates its own expression in cortical astrocytes. J Neurosci 30 (39):13116–13129. doi:30/39/13116 [pii]10.1523/JNEUROSCI.1890-10.2010
Siemers ER, Sundell KL, Carlson C, Case M, Sethuraman G, Liu-Seifert H, Dowsett SA, Pontecorvo MJ, Dean RA, Demattos R (2016) Phase 3 solanezumab trials: secondary outcomes in mild Alzheimer’s disease patients. Alzheimers Dement J Alzheimers Assoc 12(2):110–120. doi:10.1016/j.jalz.2015.06.1893
Slezak M, Pfrieger FW (2003) New roles for astrocytes: regulation of CNS synaptogenesis. Trends Neurosci 26 (10):531–535. doi:S0166-2236(03)00258-3 [pii]10.1016/j.tins.2003.08.005
Small DH, Mok SS, Bornstein JC (2001) Alzheimer’s disease and Abeta toxicity: from top to bottom. Nat Rev Neurosci 2 (8):595–598. doi:10.1038/3508607235086072 [pii]
Snyder EM, Nong Y, Almeida CG, Paul S, Moran T, Choi EY, Nairn AC, Salter MW, Lombroso PJ, Gouras GK, Greengard P (2005) Regulation of NMDA receptor trafficking by amyloid-beta. Nat Neurosci 8 (8):1051–1058. doi:nn1503 [pii]10.1038/nn1503
Soond SM, Terry JL, Colbert JD, Riches DW (2003) TRUSS, a novel tumor necrosis factor receptor 1 scaffolding protein that mediates activation of the transcription factor NF-kappaB. Mol Cell Biol 23(22):8334–8344
Stutzmann GE, Smith I, Caccamo A, Oddo S, Parker I, Laferla F (2007) Enhanced ryanodine-mediated calcium release in mutant PS1-expressing Alzheimer’s mouse models. Ann N Y Acad Sci 1097:265–277. doi:10.1196/annals.1379.025
Sutherland ML, Delaney TA, Noebels JL (1995) Molecular characterization of a high-affinity mouse glutamate transporter. Gene 162 (2):271–274. doi:037811199500293F [pii]
Sutherland ML, Delaney TA, Noebels JL (1996) Glutamate transporter mRNA expression in proliferative zones of the developing and adult murine CNS. J Neurosci 16(7):2191–2207
Temburni MK, Jacob MH (2001) New functions for glia in the brain. Proc Natl Acad Sci U S A 98 (7):3631–3632. doi:10.1073/pnas.08107319898/7/3631 [pii]
Terry RD, Masliah E, Salmon DP, Butters N, DeTeresa R, Hill R, Hansen LA, Katzman R (1991) Physical basis of cognitive alterations in Alzheimer’s disease: synapse loss is the major correlate of cognitive impairment. Ann Neurol 30(4):572–580. doi:10.1002/ana.410300410
Troy CM, Rabacchi SA, Xu Z, Maroney AC, Connors TJ, Shelanski ML, Greene LA (2001) beta-Amyloid-induced neuronal apoptosis requires c-Jun N-terminal kinase activation. J Neurochem 77(1):157–164
Ueda K, Shinohara S, Yagami T, Asakura K, Kawasaki K (1997) Amyloid beta protein potentiates Ca2+ influx through L-type voltage-sensitive Ca2+ channels: a possible involvement of free radicals. J Neurochem 68(1):265–271
Wang J, Lu R, Yang J, Li H, He Z, Jing N, Wang X, Wang Y (2015) TRPC6 specifically interacts with APP to inhibit its cleavage by gamma-secretase and reduce Abeta production. Nat Commun 6:8876. doi:ncomms9876 [pii]10.1038/ncomms9876
Wolfe MS (2007) When loss is gain: reduced presenilin proteolytic function leads to increased Abeta42/Abeta40. Talking point on the role of presenilin mutations in Alzheimer disease. EMBO Rep 8(2):136–140. doi:10.1038/sj.embor.7400896
Wyss-Coray T, Loike JD, Brionne TC, Lu E, Anankov R, Yan F, Silverstein SC, Husemann J (2003) Adult mouse astrocytes degrade amyloid-beta in vitro and in situ. Nat Med 9 (4):453–457. doi:10.1038/nm838nm838 [pii]
Yan SD, Chen X, Fu J, Chen M, Zhu H, Roher A, Slattery T, Zhao L, Nagashima M, Morser J, Migheli A, Nawroth P, Stern D, Schmidt AM (1996) RAGE and amyloid-beta peptide neurotoxicity in Alzheimer’s disease. Nature 382(6593):685–691. doi:10.1038/382685a0
Yankner BA, Duffy LK, Kirschner DA (1990) Neurotrophic and neurotoxic effects of amyloid beta protein: reversal by tachykinin neuropeptides. Science 250(4978):279–282
Yoo AS, Cheng I, Chung S, Grenfell TZ, Lee H, Pack-Chung E, Handler M, Shen J, Xia W, Tesco G, Saunders AJ, Ding K, Frosch MP, Tanzi RE, Kim TW (2000) Presenilin-mediated modulation of capacitative calcium entry. Neuron 27(3):561–572
Zhang Y, Huang R, Yi H, Bai Y, Chao J, Yao H (2016) IL-17 induces MIP-1alpha expression in primary mouse astrocytes via TRPC channel. Inflammopharmacology 24 (1):33–42. doi:10.1007/s10787-015-0256-x10.1007/s10787-015-0256-x [pii]
Zhou J, Du W, Zhou K, Tai Y, Yao H, Jia Y, Ding Y, Wang Y (2008) Critical role of TRPC6 channels in the formation of excitatory synapses. Nat Neurosci 11 (7):741–743. doi:nn.2127 [pii]10.1038/nn.2127
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media B.V.
About this chapter
Cite this chapter
Lu, R., He, Q., Wang, J. (2017). TRPC Channels and Alzheimer’s Disease. In: Wang, Y. (eds) Transient Receptor Potential Canonical Channels and Brain Diseases. Advances in Experimental Medicine and Biology, vol 976. Springer, Dordrecht. https://doi.org/10.1007/978-94-024-1088-4_7
Download citation
DOI: https://doi.org/10.1007/978-94-024-1088-4_7
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-024-1086-0
Online ISBN: 978-94-024-1088-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)