Abstract
It has been discovered that human amniotic membrane, have several properties which allow them to be applied in many medical fields, namely in the treatment of superficial wounds and burns. In dentistry, some surgical procedures results the exposure of bone surfaces to the oral cavity that is prone not only to infection but also to scar formation during secondary healing. The proper covering of the exposed periostium or bone surface is often needed to prevent these complications. Therefore, the use of amniotic membrane transplantation, to accelerate oral wound healing in humans, regardless of the genetic background, is promising. Regenerative endodontic procedure aims to provide a continuation of root development. In this field the use of amniotic membranes inside the root canals, after disinfection of the immature nonvital permanent teeth, is a promising method. This chapter will discuss the use of amniotic membranes in several fields of oral medicine.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Surgical procedures in the oral cavity that include vestibuloplasty for preprosthetic treatments and resection of broad mucosal lesions in the gingival and alveolar areas result in the exposure of bone surfaces to the oral cavity. These are prone not only to infection but also to scar formation during secondary healing.
A proper covering of the exposed periostium or bone surface is often needed to prevent these complications.
Mucosal and skin autografts have been used for this purpose and seem biologically ideal. However, these grafts require a separate surgical procedure and have other disadvantages, such as limited size of the donor mucosal graft and patient discomfort resulting from mismatching between the mucosa and the skin graft.
For these reasons, other biologic materials, such as bovine-derived collagen, chitin membranes, and human skin allografts, have been used to cover surgical defects, and the biocompatibility and availability of these materials have been investigated.
The human amniotic membrane, the innermost layer of the placenta, is a suitable tissue for allografts because of its low immunogenicity [1]. It also possesses anti-inflammatory, wound-protecting, and scar reducing properties [2].
Embryogenesis of the Mouth
The mouth is a cavity occupied by the tongue and teeth. It is limited in the front by the lips, behind by the jaws, above by the palate, below by the floor of the mouth and the tongue and laterally by the cheeks. At about the fourth week of gestation, the first branquial arch establishes the maxillary and mandibular process of the oral cavity. Thus the oral cavity is formed after development of the secondary palate, in the seventh and 8 weeks and is completed at the third month of gestation [3].
The mandible is formed from the Merckel’s cartilage after condensation of ectomesenchyme by endochondral and intramembranous ossification. The maxilla develops from a center of ossification of the maxillary process of the first branchial arch by intramembranous ossification [3]. Covering the bone tissue is the oral mucosa, which is divided into three categories: lining mucosa, masticatory mucosa and specialized mucosa [4]. The attached gingiva, bonded firmly to the bone, is continuous with alveolar mucosa. In the oral cavity the teeth are inside the bone with the periodontal ligament joining the tissues (Fig. 9.1). The tissues of the teeth are enamel, cementum and dentin recovering the pulp cavity (Fig. 9.2). The alveolar bone is a connective tissue with cells and extracellular matrix with 60 % mineral components, 20 % water and 20 % organic. The organic material components are 80 % hydroxiapatite and cells which are mainly osteoblasts and osteoclasts [5].
Regeneration in Periapical Surgery
Endodontic retreatment surgery is a therapeutic option in teeth with apical periodontitis and may be indicated when there is failure in primary endodontic treatment or nonsurgical endodontic retreatment. Another indication is the inability to perform nonsurgical retreatment or for excision of lesions for histological analysis [6, 7].
Currently, this surgery is performed with the aid of a surgical microscope and with the use of ultrasound for preparation of a cavity in the root apex, which is sealed with cement-based mineral trióxide (MTA) [8]. The purpose of this treatment is to prevent the microleakage of bacteria and fluids into the dental canal and the periapical tissue, so that the residual bacteria don not feed and perpetuate the injury. This technique, known as microsurgery, now has a success rate of around 90 %, with values similar to those of primary endodontic treatment [9].
These surgical procedures include several phases and concepts:
-
(a)
Need for deep anesthesia and perfect hemostasis;
-
(b)
Manipulation of the soft tissues;
-
(c)
Manipulation of hard tissue, bone and tooth root;
-
(d)
Correct surgical access;
-
(e)
Surgical access to the apical region of the tooth;
-
(f)
Periradicular curettage, resection of the root apex of the tooth;
-
(g)
Preparation of the apical root recess;
-
(h)
Filling the cavity created in the apical portion of the root;
-
(i)
Repositioning and suturing of soft tissue;
-
(j)
Post-operative care.
After incision and detachment of the mucoperiosteum, the endodontist accesses the periapical lesion, and needs to gain surgical access with rotary instruments, through the cortical bone. This, however, may sometimes already destroyed by the injury, with fenestration of root dental organ. As a consequence of the cystic lesion, there is a significant loss of bone structure, which needs local conditions to be created leading to its healing.
This wound healing in the bone and dental tissues of the periodontal ligament can be made by repair or regeneration of lost tissue.
Repair occurs when the healing process with new tissue is formed in different cells and structures of the original fabric.
Regeneration occurs with the destruction of the original tissue disease process and it is substituted by a cellular fabric with a similar composition structure and ability to react [10].
Repair or regeneration depends on the type of healing, the availability of undifferentiated mesenchymal cells (stem cells), growth factors and cell differentiation and the local environment, such as the presence of adhesion molecules, extracellular matrix proteins and not collagens [11].
Endodontic surgery is a clinical procedure of great dynamism and development and the – healing after periapical surgery, includes the regeneration of alveolar bone, periodontal ligament and cementum [11].
However, it must be supported by quality scientific research and a constant update of new techniques and materials. It is obvious that the root end that was removed cannot be restored.
The regeneration of tissues after apical surgery means: (I) regeneration of alveolar bone and peri-radicular tissues; (II) restoring periodontal ligament, to surround the surgically exposed root surface, and (III) the formation of new cementum on the sectioned root surface.
However, the nature of the periapical tissues regenerated after use in tissue regeneration of apical surgery remains unknown, although periapical radiographs reveal some evidence of the formation of new periodontal space (PDL).
The techniques for tissue regeneration are based on cell differentiation in cell proliferation and the induction of tissue formation.
These effects are obtained with the various protocols used in clinical practice such as bone substitutes, barrier membranes, growth factors, or a combination of these agents and materials.
Guided tissue regeneration (GTR) is a therapeutic procedure which has been recommended by some authors in periapical surgery in order to promote healing of bone injury [12].
GTR was introduced and used with great success in apical margin defects for periodontal regeneration. The placing of a physical barrier over the defect is to prevent bone growth and rapid proliferation of oral epithelium and gingival connective tissue to bone lesion, allowing the stem cells of the periodontal ligament and bone to colonize the blood clot and thus permit regeneration of lost tissue [13].
However, the use of these materials has some disadvantages such as high costs, the possibility of contamination and infection, as well as the difficulty of bringing together the edges of the wound and complete coverage of the membrane [14].
Some studies also report the risk of ankylosis that may occur with the use of membrane and tissue regeneration [15, 16].
There are several local conditions that may be encountered during apical surgery. These include: (I) large apical cystic lesions, (II) lesions in bone tunnel and (III) apical margin lesions.
In large cystic lesions or lesions in bone tunnel, where there is destruction of bone from cortical bone to the palate, that it can interfere with bone growth, resulting in the formation of a fibrous scar tissue.
For didactic, surgical and therapeutic aspects, periapical lesions are classified according to various authors [8, 17, 18]:
-
Type I – Lesion is limited to the apical area.
-
Type II – Lesion with cortical bone destruction lingual/palatal (with or without erosion of cortical bone), resulting in a failure of the tunnel.
-
Type III – Injury apical margin with complete exposure of the buccal surface of the root teeth.
Experimental animal studies and assessments of clinical cases are not unanimous as regards the use of membranes in periapical surgery.
Bernabe et al. [19] evaluated the healing of periapical tissues after the use of bone grafts, membrane, or combinations in guided tissue regeneration in apical surgery, carried out on dogs. Histological evaluation and histomorphometry showed that the repair process was similar in all groups.
Taschieri et al. [20] assessed the outcome of large surgery apical lesions (>10 mm), with or without guided tissue regeneration.
After 1 year of follow-up, the success rates of the test sites (75.0 %) and control sites (61.5 %) did not differ significantly.
In recent years, platelet-rich plasma (PRP) combined with graft materials has been used for the purpose of periodontal regeneration [21].
Platelet-rich plasma is rich in growth factors and target-specific polypeptides that play a role in cell proliferation and differentiation and can thus encourage wound repair.
PRP is a volume of autologous plasma that has a higher platelet concentration than baseline.
One histologic study comparing autologous platelet concentrate with a bioabsorbable membrane in periodontal defects found similar results between the two groups, suggesting that autologous platelet concentrate could be used in lieu of a membrane for periodontal GTR applications [22].
However, in endodontics, no reports have been found comparing the efficacy and equivalence of PRP with GTR membrane during the treatment of apical margin defects.
The application of PRP to apical margin defects, although the improvement registered over GTR is marginal, has emerged as an alternate route of treatment to the established practice of GTR membrane.
In conclusion and in resemblance to periodontally intrabony defects, it appears that GTR principles rather than the use of an osteoconductive biomaterial would be justified to enhance the surgical endodontic outcome compared with the traditional approach [23].
Published work suggests that human amniotic membrane, provides a source of undifferentiated cells with great potential that may be used in regenerative medicine [24].
As the cells are derived from epiblastic amniotic membrane before the phase of gastrulation, they are considered a source of stem cells [25].
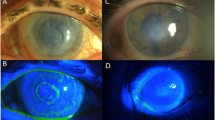
Pre-clinical and clinical studies have shown the use of amniotic membrane stem cells for repairing tissues such as the cornea [26] or spinal cord injury [27], cerebral ischemia [28] and Parkinson’s disease [29].
Despite amniotic membrane containing a large amount of undifferentiated cells that can be cryopreserved and stored as a useful potential source, fetal tissues are routinely rejected after childbirth [30–33].
A major advantage of cells isolated from the human amniotic membrane is that they are harvested after birth and can be cryogenically stored to be available in a timely manner for patient therapy after being thawed and expanded for use in tissue engineering, cell transplantation and gene therapy.
Therefore, the human amniotic membrane represents a very useful source of progenitor cells for a variety of applications.
The ability of amniotic membrane to stimulate rapid production of collagen fibres in the gingival wound has also suggested. This membrane contains transforming growth factor beta (TGF-β) and tissue inhibitors of metalloproteinase polypeptides (TIMPs), which up-regulate the production of collagen fibres by fibroblasts in wound healing [34, 35].
Amniotic membrane contains growth factors, necessary for epithelialization, and provides substrates such as laminins for rapid epithelial cell attachment which, in turn, up-regulates the expression of growth factor receptors such as epidermal growth factor (EGF) receptor on epithelial cells [35, 36].
Therefore, one may assume that these growth factors might induce rapid gingival epithelial cell migration and attachment to the wound area, thereby stimulating rapid cell proliferation and differentiation.
Therefore, the use of amniotic membrane transplantation to accelerate gingival wound healing in humans, regardless of genetic background, is promising.
Oroantral Fistula
The jaw bone is a pneumatic structure, which has inside the maxillary sinus and the paranasal sinus, bilaterally.
Because of the size of the sinus and because the proximity to the roots of some upper posterior teeth makes it easier, in some circumstances during dental extractions direct access is formed between this and the oral cavity, being termed or antral communication.
When this communication access between the oral cavity and sinus is lined with epithelial tissue, originating from the proliferation of tissues surrounding the communication, it is designated and or antral fistula [37].
The etiology of this pathology are extractions of teeth with long roots that protrude into the maxillary sinus.
A diagnosis of oroantral fistulae involves clinical and radiographic procedures. Clinical signs reported by patients are continued passing of fluid into the nose, nasal timbre, disorders in swallowing liquids and food, halitosis, runny nose, altered taste, unilateral nasal obstruction, facial pain or frontal headache (when acute maxillary sinusitis), unilateral nasal discharge and nocturnal cough due to drainage of exudate into the pharynx. The exudate swallowed may produce anorexia in the morning, as well as the patient suffering from epistaxis on the affected side and inability to blow or smoke.
One of the main complications of oroantral communications is acute or chronic maxillary sinusitis due to contamination of the maxillary sinus by the bacterial flora of the oral cavity.
Communications may be evidenced through periapical radiography where one observes the discontinuity of radiopaque line that delimits the maxillary sinus floor. Extraoral radiographs (panoramic and Incidence of Waters) are also limited with respect to small communications but may have great importance in the observation of the maxillary sinus involved, which may present a diffuse radiopacity (sinus opacification) , compared with the opposite.
The patient with acute maxillary sinusitis may have swelling and redness in the area of the sinus and malar eminence, as well as pain in the eye. Palpation of the maxilla increases pain, and teeth with roots adjacent to the sinus will often present pain or be sensitive to percussion. The treatment of oroantral communications should be done immediately, so that the opening is created, or later, in cases of failed attempts at primary closure [38].
The closure of the fistula can be made by a free tissue graft taken from the palate or via buccal flap.
The amniotic membrane possesses antibacterial, anti-tumor, anti-inflammatory properties and promotes tissue healing. It also reduces pain, inhibits scarring, and shows little or no immunogenicity. These properties enable surgeons to apply the human amniotic membrane graft on various tissue surfaces without suturing. The low cost of human amniotic membrane graft preparation and the very good clinical results in different applications, have been relevant in proposing the amnion as an alternative to other natural and synthetic wound dressings. This application may be used in the closure of the oroantral fistula.
Apexogenesis
In developing teeth, root formation starts with the epithelial cells from the cervical loop that proliferate apically and influence the differentiation of odontoblasts from undifferentiated mesenchymal cells and cementoblasts from -mesenchymal follicles [39].
This apically extending two-layered epithelial wall (merging of the inner and outer enamel epithelium) forms Hertwig’s epithelial root sheath (HERS), which is responsible for determining the shape of the root(s) and forms cementum through epithelial-mesenchymal transition [40].
It is known that dental papilla contributes to tooth formation and eventually converts to pulp tissue [39, 41, 42].
Cessation of root development caused by trauma or pulpal disease presents both an endodontic and restorative challenge. The divergent apical architecture makes complete debridement and control of obturation material nearly impossible [43]. Fragile root canal walls may be too weak to withstand the normal forces of mastication, becoming more prone to fracture [44].
Pulp regeneration can be a form of therapy for resolving teeth with open apex and thin walls resulting from trauma, decay and iatrogenic procedures, leading to necrosis of the pulp and stopping tooth development.
Several published works refer to the use of paste consisting of three antibiotics (metronidazole, ciprofloxacin and minocycline), in order to eradicate all bacteria in the pulp space. After this procedure, the channel is irrigated with a solution of sodium hypochlorite (at a concentration of 2.5–5.25 %) to remove debris and organic waste [45]. It has been reported that the apical papilla harbours multipotent cells (MSCs) that express various MSC markers and that they are capable of forming odontoblast-like cells, produce dentin in vivo, and are likely to be the cell source of primary odontoblasts for root dentin formation [46].
In order for these cells to enter the pulp space, bleeding is induced in the periapical tissues vessel, so as to enter the canal and be a source of cells to complete root teeth development.
After the formation of the clot within the pulp chamber, a bioactive cement (MTA) is placed over the clot, which will serve as a matrix for the filling of the root canal [45].
Amniotic membrane contains growth factors, necessary for epithelialization, and provides substrates such as laminins for rapid epithelial cell attachment which, up-regulates the expression of growth factor receptors such as EGF receptor on epithelial cells [35, 36].
Therefore, one may assume that these growth factors might induce rapid cell migration and attachment to the wound area, by this means stimulating rapid cell proliferation and differentiation.
So, the use of amniotic membrane transplantation in the root canal may be promising as a scaffold to be used in apexogenesis therapy, instead of the use of a biomaterial as MTA.
References
Kubo M, Sonoda Y, Muramatsu R, Usui M (2001) Immunogenicity of human amniotic membrane in experimental xenotransplantation. Invest Ophthalmol Vis Sci 42:1539–1546
Faulk WP, Stevens PJ, Burgos H et al (1980) Human amnion as an adjunct in wound healing. Lancet 315:1156–1158
Nanci A (2008) Embriology of the head, face and oral cavity. Ten cate’s oral. Histol. Dev. Struct. Funct. Elsevier Health Sciences, p 411
Roed-Petersen B, Renstrup G (1969) A topographical classification of the oral mucosa suitable for electronic data processing: its application to 560 leukoplakias. Acta Odontol Scand 27:681–695
Garant PR (2003) Oral cells and tissues. Quintessence Publishing Company, Chicago, 430
Gutmann J, Harrison J (1985) Posterior endodontic surgery: anatomical considerations and clinical techniques. Int Endod J 18:8–34
Tsesis I, Faivishevsky V, Kfir A, Rosen E (2009) Outcome of surgical endodontic treatment performed by a modern technique: a meta-analysis of literature. J Endod 35:1505–1511
Kim S, Kratchman S (2006) Modern endodontic surgery concepts and practice: a review. J Endod 32:601–623
Tsesis I, Rosen E, Schwartz-Arad D, Fuss Z (2006) Retrospective evaluation of surgical endodontic treatment: traditional versus modern technique. J Endod 32:412–416
Pecora G, De Leonardis D, Ibrahim N et al (2001) The use of calcium sulphate in the surgical treatment of a “through and through” periradicular lesion. Int Endod J 34:189–197
Lin L, Chen MY-H, Ricucci D, Rosenberg P a (2010) Guided tissue regeneration in periapical surgery. J Endod 36:618–625
Tobón S, Arismendi J, Marín M et al (2002) Comparison between a conventional technique and two bone regeneration techniques in periradicular surgery. Int Endod J 35:635–641
Dahlin C, Linde A, Gottlow J, Nyman S (1988) Healing of bone defects by guided tissue regeneration. Plast Reconstr Surg 81:672–676
Pecora G, Baek S, Rethnam S, Kim S (1997) Barrier membrane techniques in endodontic microsurgery. Dent Clin N Am 41:585–602
Karring T, Nyman S, Lindhe J, Sirirat M (1984) Potentials for root resorption during periodontal wound healing. J Clin Periodontol 11:41–52
Cury PR, Furuse C, Trierveiler M et al (2005) Root resorption and ankylosis associated with guided tissue regeneration. J Am Dent Assoc 136:337–341
von Arx T, Cochran DL (2001) Rationale for the application of the GTR principle using a barrier membrane in endodontic surgery: a proposal of classification and literature review. Int J Periodontics Restorative Dent 21:127–139
Dietrich T, Zunker P, Dietrich D, Bernimoulin J-P (2002) Apicomarginal defects in periradicular surgery: classification and diagnostic aspects. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94:233–239. doi:10.1067/moe.2002.123864
Bernabé PFE, Gomes-Filho JE, Cintra LTÂ et al (2010) Histologic evaluation of the use of membrane, bone graft and MTA in apical surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:309–314
Taschieri S, Del Fabbro M, Testori T, Weinstein R (2007) Efficacy of xenogeneic bone grafting with guided tissue regeneration in the management of bone defects after surgical endodontics. J Oral Maxillofac Surg 65:1121–1127
Plachokova AS, Nikolidakis D, Mulder J et al (2008) Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. Clin Oral Implants Res 19:539–545
Artzi Z, Wasersprung N, Weinreb M et al (2012) Effect of guided tissue regeneration on newly formed bone and cementum in periapical tissue healing after endodontic surgery: an in vivo study in the cat. J Endod 38:163–169
Nyman S, Gottlow J, Lindhe J et al (1987) New attachment formation by guided tissue regeneration. J Periodontal Res 22:252–254
Toda A, Okabe M, Yoshida T, Nikaido T (2007) The potential of amniotic membrane/amnion-derived cells for regeneration of various tissues. J Pharmacol Sci 105:215–228
Ilancheran S, Michalska A, Peh G et al (2007) Stem cells derived from human fetal membranes display multilineage differentiation potential. Biol Reprod 77:577–588
Shimmura S, Tsubota K (2002) Ocular surface reconstruction update. Curr Opin Ophthalmol 13:213–219
Sankar V, Muthusamy R (2003) Role of human amniotic epithelial cell transplantation in spinal cord injury repair research. Neuroscience 118:11–17
Sakuragawa N, Misawa H, Ohsugi K et al (1997) Evidence for active acetylcholine metabolism in human amniotic epithelial cells: applicable to intracerebral allografting for neurologic disease. Neurosci Lett 232:53–56
Kakishita K, Nakao N, Sakuragawa N, Itakura T (2003) Implantation of human amniotic epithelial cells prevents the degeneration of nigral dopamine neurons in rats with 6-hydroxydopamine lesions. Brain Res 980:48–56
Chang Y, Hwang S, Tseng C et al (2010) Isolation of mesenchymal stem cells with neurogenic potential from the mesoderm of the amniotic membrane. Cells Tissues Organs 192:93–105
Niknejad H, Peirovi H, Jorjani M et al (2008) Properties of the amniotic membrane for potential use in tissue engineering. Eur Cell Mater 15:88–99
Hennerbichler S, Reichl B, Pleiner D et al (2007) The influence of various storage conditions on cell viability in amniotic membrane. Cell Tissue Bank 8:1–8. doi:10.1007/s10561-006-9002-3
Wilshaw SS-P, Kearney JNJ, Fisher J, Ingham E (2006) Production of an acellular amniotic membrane matrix for use in tissue engineering. Tissue Eng 12:2117–2129
Hao Y, Ma DH-K, Hwang DG et al (2000) Identification of antiangiogenic and antiinflammatory proteins in human amniotic membrane. Cornea 19:348–352
Yam H-F, Pang C-P, Fan DS-P et al (2002) Growth factor changes in ex vivo expansion of human limbal epithelial cells on human amniotic membrane. Cornea 21:101
Kurpakus M, Daneshvar C, Davenport J, Kim A (1999) Human corneal epithelial cell adhesion to laminins. Curr Eye Res 19:106–114
Visscher SH, van Minnen B, Bos RR (2010) Closure of oroantral communications: a review of the literature. J Oral Maxillofac Surg 68:1384–1391
Lazow SK (1999) Surgical management of the oroantral fistula: flap procedures. Oper Tech Otolaryngol Head Neck Surg 10:148–152
D’Souza R (2002) Development of the pulpodentin complex. In: Hargreaves KM, Goodi HE (eds) Seltzer Bender’s Dent. pulp, 3rd edn. Quintessence Publishing, pp 13–40
Sonoyama W, Seo B-M, Yamaza T, Shi S (2007) Human hertwig’s epithelial root sheath cells play crucial roles in cementum formation. J Dent Res 86:594–599
Linde A, Goldberg M (1993) Dentinogenesis. Crit Rev Oral Biol Med 4:679–728
Ruch JV, Lesot H, Begue-Kirn C (1995) Odontoblast differentiation. Int J Dev Biol 39:51–68
Rafter M (2005) Apexification: a review. Dent Traumatol 21:1–8
Rabie G, Trope M, Garcia C, Tronstad L (1985) Strengthening and restoration of immature teeth with an acid-etch resin technique. Dent Traumatol 1:246–256
Banchs F, Trope M (2004) Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod 30:196–200
Ferreira MM, Botelho MF, Abrantes M et al (2014) Quantitative scintigraphic analysis of pulp revascularization in autotransplanted teeth in dogs. Arch Oral Biol 55:825–829
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Ferreira, M.M., Carrilho, E.V.P. (2015). Amniotic Membrane in Oral Medicine. In: Mamede, A., Botelho, M. (eds) Amniotic Membrane. Springer, Dordrecht. https://doi.org/10.1007/978-94-017-9975-1_9
Download citation
DOI: https://doi.org/10.1007/978-94-017-9975-1_9
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-017-9974-4
Online ISBN: 978-94-017-9975-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)