Abstract
We examined individual social capital and its relationship with well-being among community-dwelling older people in the Netherlands. This cross-sectional study included 945/1440 (66 % response rate) independently living older (≥ 70 years) adults in Rotterdam. We investigated individuals’ social capital by asking about structural (e.g., group membership) and cognitive (e.g., trust, social harmony, sense of belonging, sense of fairness) characteristics. The formation of social capital may cushion the negative effect of loss and allow for substitution when network ties become unavailable. Buffer and substitution effects may be detected that protect well-being. Looking at bivariate relationships with social capital results indicated that being born in the Netherlands, higher education, older age, and higher income were positively associated with individuals’ social capital. Multilevel regression analyses showed that older age, higher education, and higher income positively predicted social capital. Social capital in turn predicted the well-being of older adults, suggesting a direct contribution to well-being; we also found indications for buffer effects. The results of this study support the importance of social capital for the well-being of community-dwelling older people. Building social capital over one’s lifetime is likely to protect against loss of well-being if network ties become unavailable (e.g., after retirement, loss of loved ones), and may be especially important for individuals with lower educational and income levels and for older immigrants not born in the Netherlands. Neighbourhoods that foster the formation of social capital may enable people to build buffers against the negative effects of age-related loss.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Social Capital
- Marginal Return
- Social Harmony
- Neighbourhood Social Capital
- Multilevel Regression Analysis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The global population is aging (World Health Organization 2004). The percentage of the European Union (EU) population aged ≥ 65 years increased from 13.7 % in 1990 to 17.4 % in 2010, and is predicted to reach about 30 % by 2060. The proportion of the EU population aged ≥ 80 years is forecast to increase fourfold between 1990 (3.1 %) and 2060 (12.1 %) (The European Commission 2011). Within the context of a growing older population and overloaded health and welfare systems, aging in place has received much attention. Older people prefer aging in place, and it is expected to reduce health and social care costs (Gitlin 2003; Heywood et al. 2002). This concept has not been clearly defined, but consensus has been reached that it refers to the ability of older people to continue to live in their homes (Emlet and Moceri 2012), even in the context of functional decline and increased dependence (Hooyman and Kiyak 2011). Aging in place is best promoted with a holistic, comprehensive approach that maintains the well-being of community-dwelling older people (Lawler 2001); thus, the protection of their well-being becomes increasingly important. Evidence has suggested that well-being may build resilience over time (Fredrickson 2001) and enhances strategies for coping with adverse life events (Aspinwall 1998, 2001; Fredrickson and Joiner 2002), such as age-related losses (e.g., functional decline, the loss of loved ones) (Nieboer 1997). In this regard, the identification of factors that contribute to the well-being of community-dwelling older people would be helpful.
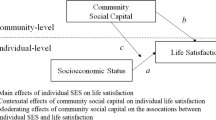
Social capital is increasingly acknowledged as an important determinant of well-being in the general population (Bjørnskov 2003, 2005; Cramm et al. 2010a, b; Wilkinson and Pickett 2006; Yip et al. 2007). It may also be an important factor in the maintenance of well-being among community-dwelling older people (Cramm et al. 2013a). Such social resources may function as buffers that individuals can access in later life to improve the odds of aging in place and to protect against the negative effects of age-related losses. People have multiple ways of realizing well-being; that is, they have buffers and they can substitute one means for another (Nieboer and Lindenberg 2002). The idea of buffers is quite simple. The realization of well-being through network ties is subject to decreasing marginal returns. If social capital is increased there comes a point where it will become less productive for well-being and therefore there will be a decrease in the marginal return of additional social capital. In other words, well-being will not be enhanced as much by increasing network size, although, neither will well-being be affected as much when network ties are lost. For example, having friends is important for realizing affection (an important means to realize well-being). But having many friends may add only a fraction of extra affection beyond the level realized by having a few friends. Since the effect of the extra friends is marginal, it creates buffers: When some of the network ties fall away, overall well-being is not much affected.
Although much research has investigated the relationship between social capital and health (Cramm and Nieboer 2011; Cramm et al. 2011a; Hyyppä and Mäki 2003; Kawachi et al. 1997; Lochner et al 2003; Rose 2000; Ziersch 2005), few studies have examined the role of social capital in well-being, especially among community-dwelling people aged 70 +. Well-being refers to an individual’s appraisal of his or her life situation as a whole, which is much broader than health (Bradburn 1969; Diener 1984; Omodei and Wearing 1990; Watson 1988). According to the Social Production Function theory (SPF-theory), besides the universal goals of physical, and social well-being (identical for all human beings), well-being entails instrumental goals stimulation, comfort, status, behavioural confirmation and affection (individual preferences for the means leading to universal goals) (Ormel et al. 1999). These are especially relevant for older people who are in the process of experiencing progressive functional decline. Investigating well-being in accordance with the SPF-theory allows much more specificity about how individuals achieve well-being (Nieboer et al. 2005).
Previous research on health and social capital suggested that social capital positively affects health through social support, encouragement of social activities, and facilitation of social bonding. These factors, in turn, may reduce feelings of stress and loneliness, while promoting self-esteem, confidence, and feelings of security (Kawachi and Berkman 2000). We expect that these findings may also apply to the well-being of older people. Thus, this study was conducted to investigate the relationship between social capital and well-being among community-dwelling older people while controlling for important background characteristics. We have previously found that neighbourhood social cohesion and social capital are important for the well-being of older adults in the community (Cramm et al. 2013), that neighbourhood security, social cohesion, and sense of belonging among community-dwelling older people are related to frailty (Cramm and Nieboer 2012) and that the neighbourhood attributes of security and solidarity are important for well-being (Cramm and Nieboer 2013). These findings underscore the importance of investigating concepts such as social cohesion, social capital and solidarity, while taking into account the neighbourhood context.
The study presented here adds to the current knowledge by investigating individuals’ social capital by asking about structural (e.g., group membership) and cognitive (e.g., trust, social harmony, sense of belonging, sense of fairness) characteristics (De Silva et al. 2006; De Silva et al 2007) and by determining the diminishing marginal returns of social capital for well-being. Social capital is assumed to have decreasing marginal value for the production of well-being. We assume that people keep producing more and more social capital until the marginal return (in terms of well-being) is equal to the marginal cost (such as the effort to meet new people and make friends). When that cost is low, people get virtually saturated with the achievement of social capital. This also means that, as a side effect, a buffer is created against great losses in well-being when certain means of production fall away (Nieboer and Lindenberg 2002), for example due to the loss of loved ones (Nieboer 1997).
2 Design and Methods
A sample of 1440 independently living older (aged ≥ 70 years) adults in four districts of Rotterdam (Lage Land/Prinsenland, Lombardijen, Oude Westen, and Vreewijk), The Netherlands , was randomly identified using the population register. The sample included some 430 eligible older adults per district and was proportionate to the 72 neighbourhoods in these districts and age (age groups: 70–74, 75–79, 80–84, ≥ 85 years).
Eligible individuals were asked by mail to complete a written or online questionnaire. Respondents were rewarded with a ticket in the monthly Dutch State Lottery. Non-respondents were first sent a reminder by mail, were then asked by telephone to participate, and were finally visited at home if they could not be reached by telephone. This strategy yielded a 66 % (n = 945) response rate. The ethics committee of the Erasmus University Medical Center of Rotterdam approved the study in June 2011. A detailed description of the study design can be found in our study protocol (Cramm et al. 2011b).
2.1 Measures
Well-being was measured with the 15-item version of the Social Production Function Instrument for the Level of Well-being (SPF-IL) (Nieboer et al. 2005). This scale measures levels of physical (comfort, stimulation) and social (behavioural confirmation, affection, status) well-being. Examples of questions are: “Do people pay attention to you?” (affection), “Do you feel useful to others?” (behavioural confirmation), “Are you known for the things you have accomplished?” (status), “In the past few months have you felt physically comfortable?” (comfort), and “Do you really enjoy your activities?” (stimulation). Responses are structured by a four-point scale ranging from never (1) to always (4), with higher mean scores indicating greater well-being. Cronbach’s alpha for the SPF-IL was 0.86, indicating good reliability. The SPF-IL has been shown to be a reliable instrument for assessing well-being in older populations (Cramm et al. 2012, 2013; Frieswijk et al. 2006; Schuurmans et al. 2005; Steverink et al. 2005).
We assessed individuals’ social capital by asking about structural (e.g., group membership) and cognitive (e.g., trust, social harmony, sense of belonging, sense of fairness) characteristics (De Silva et al. 2006, 2007). To determine the diminishing marginal returns of social capital for well-being, we also used the quadratic term after the mean of social capital is subtracted from the scores on this variable.
We asked respondents to indicate the highest educational qualification achieved using a seven-point scale ranging from 1 (primary school or less) to 7 (university degree). We dichotomized educational level as low (1: ≤ 6 years of primary school) or high (0: > 6 years of primary school).
Net monthly household income, including all types of income (e.g., social benefits, pensions, salaries) was classified using a five-point scale ranging from 1 (EUR 1000) to 5 (> EUR 3050). The total monthly household income was then divided by the number of household members. We dichotomized household members’ income as low (1: < EUR 1000) or high (0: > EUR 1000).
2.2 Analysis
We employed descriptive statistics and bivariate analyses to assess the relationships between the well-being of older adults and gender, age, marital status, ethnic background, education level, income, and social capital. We fitted a hierarchical random-effects model to account for the hierarchical structure of the study design. The structure comprised 945 older adults (level 1) nested in 72 neighbourhoods (level 2). Respondents with missing observations for any outcome were excluded, leading to the inclusion of 797 respondents in the multilevel regression analyses. The multivariate analyses included only variables that were significantly associated with well-being in bivariate analyses. Results were considered statistically significant if two-sided p values were ≤ 0.05.
3 Results
Table 9.1 displays the descriptive statistics for all independent variables and well-being. Of the 945 respondents, 57 % were women. Their average age was 77.5 (range, 70–101; standard deviation, 5.8) years. About one-third (35 %) of respondents were married and 83 % were born in the Netherlands. Looking at differences between groups and their social capital we found that more highly educated people (6.4 vs. 5.3; p < 0.001), people with higher income levels (6.5 vs. 5.6; p < 0.001), and people born in the Netherlands (6.3 vs. 5.5; p < 0.001) reported higher levels of social capital.
Table 9.2 displays associations of independent variables with the well-being of older adults. Bivariate analyses showed that being born in the Netherlands (p ≤ 0.01), low educational level (p ≤ 0.05), low income level (p ≤ 0.05), and social capital (p ≤ 0.001) were significantly related to the well-being of community-dwelling older people. No significant relationship was found between well-being and gender, age, or marital status. In addition, we found that social capital was significantly related to age (p ≤ 0.001), marital status (p ≤ 0.05), being born in the Netherlands (p ≤ 0.001), low educational level (p ≤ 0.001), and low income level (p ≤ 0.001).
Variables that were significantly related to well-being in the bivariate analyses were included in the multilevel regression model (Table 9.3). As expected, these results showed that social capital predicted the well-being of community-dwelling older people after controlling for other significant background characteristics. In addition we investigated the marginal returns of social capital by including the square of social capital in the analyses and found that social capital as well as the square of social capital predicted the well-being of community-dwelling older people pointing to the expected buffer effects. Furthermore, multilevel regression analyses showed that older age, higher education level, and higher income positively predicted social capital in this population (results not shown).
4 Discussion
The study presented in this chapter aimed to investigate the relationship between social capital and well-being among community-dwelling older people while controlling for important background characteristics. The results clearly showed that social capital (measured by structural social capital: e.g., group membership) and cognitive social capital (e.g., trust, social harmony, sense of belonging, sense of fairness) is related to older people’s well-being. Berkman and colleagues found that social capital may positively influence health, which may also promote well-being among community-dwelling older people. Building social capital over one’s lifetime is likely to protect loss of well-being if certain network ties become unavailable, for example after retirement or the loss of loved ones. Neighbourhoods in which the formation of social capital is likely may therefore enable people to build buffers that cushion the negative effects of age-related loss, which was supported by the decreasing marginal returns of social capital for the realisation of well-being. People’s ability to build buffers and to substitute has important consequences for how they deal with changes in life-circumstances. These findings underscore the importance of individuals’ social capital and formation of social capital in neighbourhoods for the well-being of community-dwelling older people, which is expected to contribute to aging in place. Public policy increasingly emphasises the importance of informal support networks to meet the needs of the aging population, such as that from family, friends, and neighbours (Fast et al. 2004; Shaw 2005). Van Dijk and colleagues (2013) reported on experiences of neighbour, volunteer, and professional support-givers in providing support to community-dwelling older people. This study indicated a naturally-occurring commitment among neighbours and that neighbours provided instrumental and emotional support to each other. In this regard, social capital in the form of neighbour support may promote higher levels of well-being and contribute to aging in place.
The research presented here also revealed that more highly educated older people, those with higher income levels, and those who were born in the Netherlands reported higher levels of social capital. Previous research has also shown that older people who are well educated and have had employment experience during their lifetime often report higher levels of social capital and social participation (Morris and Caro 1996). Attending school, being employed, and being socially active allowed these individuals to build stronger social capital during their lifetimes. Therefore, special attention is needed for people with lower educational and income levels and for older immigrants not born in the Netherlands. The results of our analyses support these findings, as we found significant associations between well-being and social capital, income level, ethnic background, and educational level.
This study has several limitations. Due to the cross-sectional design, we could not infer causality in the relationships between well-being and social capital and the diminishing returns of social capital for individuals’ well-being. Furthermore, this study was conducted in a large Dutch city; other studies are needed to confirm our study findings among community-dwelling older people in other countries and/or areas.
Strengths of this study are that we investigated the relationship between social capital and well-being among a large sample of community-dwelling older people (aged ≥ 70 years; and selecting respondents proportionate to their age) and a high response rate among such a sample of 66 %.
We can conclude that social capital is important for the well-being of community-dwelling older people. Building social capital over one’s lifetime is likely to protect against loss of well-being and may be especially important for individuals with lower educational and income levels and people not born in the Netherlands who reported lower levels of social capital. Due to mobility limitations and smaller social networks (McPherson et al. 2006; Oh and Kim 2009), older people rely even more on social capital within the neighbourhood. With the very significant increase in older people, the need for supportive neighbourhoods and formation of social capital within neighbourhoods gains further importance. Therefore, future research should focus on older peoples’ specific needs for ageing in place and the role of social capital in supporting their needs over time. Policies aimed at improving formation of neighbourhood social capital (or avoiding loss of social capital) are likely to result in higher levels of well-being among older people as they age. While neighbourhood conditions that block buffer-formation make it harder for people to cope with changing circumstances, people’s ability to build buffers on the other hand helps them deal with changes in their life circumstances.
References
Aspinwall, L. G. (1998). Rethinking the role of positive affect in self-regulation. Motivation and Emotion, 22, 1–32.
Aspinwall, L. G. (2001). Dealing with adversity: Self-regulation, coping, adaptation, and health. In A. Tesser & N. Schwarz (Eds.), The Blackwell handbook of social psychology (Vol 1, pp. 591–614). Malden: Blackwell.
Bjørnskov, C. (2003). The happy few: Cross-country evidence on social capital and life satisfaction. Kyklos, 56, 3–16. doi:10.1111/1467-6435.00207
Bjørnskov, C. (2005). The multiple facets of social capital. European Journal of Political Economy, 22, 22–40.
Bradburn, N. M. (1969). The structure of psychological well-being. Chicago: Aldine.
Cramm, J. M., & Nieboer, A. P. (2011). Socioeconomic health indicators among residents of an economically and health-deprived South African township. International Journal for Equity in Health, 10, 51.
Cramm, J. M., & Nieboer, A. P. (2012). Relationships between frailty, neighbourhood security, social cohesion and sense of belonging among community-dwelling older people. Geriatrics & Gerontology International. doi:10.1111/j.1447-0594.2012.00967.x.
Cramm, J. M., & Nieboer, A. P. (2013). Neighborhood attributes security and solidarity promote the well-being of community-dwelling older people. Accepted in Geriatrics and Gerontology International.
Cramm, J. M., Møller, V., & Nieboer, A. P. (2010a). Improving subjective well-being of the poor in the Eastern Cape. Journal of Health Psychology, 15, 1012–1019. doi:10.1177/1359105310367833.
Cramm, J. M., Møller, V., & Nieboer, A. P. (2010b). Individual-and neighbourhood-level indicators of subjective well-being in a small and poor Eastern Cape township: The effect of health, social capital, marital status, and income. Social Indicators Research. doi:10.1007/s11205-011-9790-0.
Cramm, J. M., Koolman, X., Møller, V., & Nieboer, A. P. (2011a). Socioeconomic status and self-reported tuberculosis: A multilevel analysis in a low-income township in the Eastern Cape, South Africa. African Journal of Public Health. doi:10.4081/jphia.2011.e34.
Cramm, J. M., van Dijk, H., Lötters, F., van Exel, F., & Nieboer, A. P. (2011b). Evaluating an integrated neighbourhood approach to improve well-being of frail elderly in a Dutch community: A study protocol. BMC Research Notes, 4, 532. doi:10.1186/1756-0500-4-532.
Cramm, J. M., Hartgerink J. M., de Vreede, P. L., Bakker, T. J., Steyerberg, E. W., Mackenbach, J. P., & Nieboer, A. P. (2012). The role of self-management abilities in the achievement and maintenance of well-being, prevention of depression and successful ageing. European Journal of Ageing, 9, 353–360.
Cramm, J. M., van Dijk, H. M., & Nieboer, A. P. (2013a). The importance of neighborhood social cohesion and social capital for the well-being of older adults in the community. Gerontologist, 53, 142–152.
Cramm, J. M., Hartgerink, J. M., Bakker, T. J., Steyerberg, E. W., Mackenbach, J. P., & Nieboer, A. P. (2013b). Understanding older patients’ self-management abilities: Functional loss, self-management, and well-being. Quality of Life Research, 22(1), 85–92.
De Silva, M. J., Harpham, T., Tuan, T., Bartolini, R., Penny, M. E., & Huttly, S. R. (2006). Psychometric and cognitive validation of a social capital measurement tool in Peru and Vietnam. Social Science & Medicine, 62, 941–953. doi:10.1016/j.socscimed.2005.06.050.
De Silva, M. J., Huttly, S. R., Harpham, T., & Kenward, M. G. (2007). Social capital and mental health: A comparative analysis of four low income countries. Social Science & Medicine, 64, 5–20. doi:10.1016/j.socscimed.2006.08.044.
Diener, E. (1984). Subjective well-being. Psychological Bulletin, 95, 542–575.
Emlet, C. A., & Moceri, J. T. (2012). The importance of social connectedness in building age-friendly communities. Journal of Aging Research. doi:10.1155/2012/173247.
The European Commission. (2011). Third demography report. http://europa.eu/rapid/pressReleasesAction.do?reference=MEMO/11/209. Accessed Sept 2011.
Fast, J., Keating, N., Otfinowski, P., & Derksen, L. (2004). Characteristics of family/friend care networks of frail seniors. Canadian Journal on Aging, 23(1), 5–19.
Fredrickson, B. L. (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56, 218–226.
Fredrickson, B. L., & Joiner, T. (2002). Positive emotions trigger upward spirals toward emotional well-being. Psychological Science, 13, 172–175.
Frieswijk, N., Steverink, N., Buunk, B. P., & Slaets, J. P. J. (2006). The effectiveness of a bibliotherapy in increasing the self-management ability of slightly to moderately frail older people. Patient Education and Counseling, 61, 219–227.
Gitlin, L. (2003). Conducting research on home environments: Lessons learned and new directions. Gerontologist, 43, 628–637.
Heywood, F., Oldman, C., & Means, R. (2002). Housing and home in later life. Buckingham: Open University Press.
Hooyman, N. R., & Kiyak, H. A. (2011). Social gerontology: A multidisciplinary perspective. Boston: Allyn and Bacon.
Hyyppä, M. T., & Mäki, J. (2003). Social participation and health in a community rich in stock of social capital. Health Education Research, 18, 770–779.
Kawachi, I. & Berkman, L. F. (2000). Neighbourhoods and Health. New York: Oxford University Press.
Kawachi, I., Kennedy, B. P., Lochner, K., & Prothrow-Stith, D. (1997). Social capital, income inequality, and mortality. American Journal of Public Health, 87, 1491–1498.
Lawler, K. (2001). Aging in place: Coordinating housing and health care provision for America’s growing elderly population. Cambridge: Harvard University.
Lochner, K., Kawachi, I., Brennan, R. T., & Buka, S. L. (2003). Social capital and neighborhood mortality rates in Chicago. Social Science & Medicine, 56, 1797–1805.
McPherson, M., Smith-Loving, L., & Brashears, M. E. (2006). Social isolation in America: Changes in core discussion networks over two decades. American Sociological Review, 71, 353–375.
Morris, R., & Caro, F. (1996). Productive retirement: Stimulating greater volunteer efforts to meet national needs. The Journal of Volunteer Administration, 14, 5–13.
Nieboer, A. P. (1997). Life-events and well-being. Dissertation, University of Groningen. Amsterdam: Thela Thesis.
Nieboer, A., Lindenberg, S. (2002). Substitution, buffers and subjective well-being: A hierarchical approach. In E. Gullone & R.A. Cummins (Eds.), The universality of subjective well-being indicators (pp. 175–189). Dordrecht: Kluwer Academic Publishers.
Nieboer, A., Lindenberg, S., Boomsma, A., & van Bruggen, A. C. (2005). Dimensions of well-being and their measurement: The SPF-IL scale. Social Indicators Research, 73, 313–353.
Oh, J-H., & Kim, S. (2009). Aging, neighbourhood attachment, and fear of crime: Testing reciprocal effects. Journal of Community Psychology, 37, 21–40.
Omodei, M. M., & Wearing, A. J. (1990). Need satisfaction and involvement in personal projects: Toward an integrative model of subjective well-being. Journal of Personality and Social Psychology, 59, 762–769.
Ormel, J., Lindenberg, S., Steverink, N., & Verbrugge, L. M. (1999). Subjective well-being and social production functions. Social Indicators Research, 46, 61–90.
Rose, R. (2000). How much does social capital add to individual health? A survey study of Russians. Social Science & Medicine, 51, 1421–1435.
Schuurmans, H., Steverink, N., Frieswijk, N., Buunk, B. P., Slaets, J. P. J., & Lindenberg, S. (2005). How to measure self-management abilities in older people by self-report? The development of the SMAS-30. Quality of Life Research, 14, 2215–2228.
Shaw, B. A. (2005). Anticipated support from neighbours and physical functioning during later life. Research on Aging, 27(5), 503–525.
Steverink, N., Lindenberg, S., & Slaets, J. P. J. (2005). How to understand and improve older people’s self-management of wellbeing. European Journal of Ageing, 2, 235–244.
van Dijk, H. M., Cramm, J. M., & Nieboer, A. P. (2013). The experiences of neighbour, volunteer and professional support-givers in supporting community dwelling older people. Health & Social Care in the Community, 21, 150–158.
Watson, D. (1988). The vicissitudes of mood measurement: Effects of varying descriptors, time frames, and response formats on measures of positive and negative affect. Journal of Personality and Social Psychology, 55, 128–141.
Wilkinson, R. G., & Pickett, K. E. (2006). Income inequality and population health: A review and explanation of the evidence. Social Science & Medicine, 62, 1768–1784.
World Health Organization. (2004). The global strategy on diet, physical activity and health. Geneva: World Health Organization.
Yip, W., Sybramanian, S. V., Mitchell, A. D., Lee, D. T. S., Wang, J., & Kawachi, I. (2007). Does social capital enhance health and well-being? Evidence from rural China. Social Science & Medicine, 64, 35–49.
Ziersch, A. M. (2005). Health implications of access to social capital: Findings from an Australian study. Social Science & Medicine, 61, 2119–2131.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Cramm, J., Nieboer, A. (2015). Building Social Capital May Protect against Loss of Well-Being among Older People. In: Nyqvist, F., Forsman, A. (eds) Social Capital as a Health Resource in Later Life: The Relevance of Context. International Perspectives on Aging, vol 11. Springer, Dordrecht. https://doi.org/10.1007/978-94-017-9615-6_9
Download citation
DOI: https://doi.org/10.1007/978-94-017-9615-6_9
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-017-9614-9
Online ISBN: 978-94-017-9615-6
eBook Packages: Humanities, Social Sciences and LawSocial Sciences (R0)