Abstract
Tissue non-specific alkaline phosphatase (TNAP) is present on neuronal membranes and induces neuronal toxicity via tau dephosphorylation; a mechanism which could play a role in the neuronal loss seen in Alzheimer’s disease (AD). TNAP increases in the plasma following brain injury and cerebrovascular disease. In this chapter we summarise our previous work which looked at changes in TNAP activity in the brain and plasma of AD individuals and discuss whether these changes may be reflective of neuronal loss. Our data demonstrate that TNAP activity is significantly increased in the brain in both the sporadic and familial forms of AD and that TNAP activity is significantly increased in the plasma in AD patients. In addition, we describe a significant inverse correlation between plasma TNAP activity and cognitive function in AD. Using these data we propose a model for TNAP-induced neurodegeneration in AD resulting from tau dephosphorylation following secretion of tau from neuronal cells.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Alzheimer’s disease (AD is the most common form of dementia and the impact of this neurodegenerative disease is increasing as the population ages (Burns and Iliffe 2009). AD symptoms progress from mild memory problems (mild cognitive impairment ; MCI) through to severe cognitive deficits. Studies of ageing and cognition suggest that impairment in multiple cognitive domains may be observed several years before a clinical diagnosis of AD is made (Matthews et al. 2007). It has been suggested that the observed cognitive dysfunction is not qualitatively different from that seen in normal ageing, proposing the idea that there is a continuum from normal ageing to preclinical dementia (Brayne 2007). AD is characterised by the formation of extracellular amyloid plaques and intracellular neurofibrillary tangles . Amyloid plaques are composed of amyloid-β peptide formed from the sequential cleavage of the amyloid precursor protein (APP) by the β-site APP cleaving enzyme-1 (BACE1) and the ϒ–secretase complex. Neurofibrillary tangles are composed of hyperphosphorylated and aggregated tau (Iqbal et al. 2005) and initially appear in the entorhinal cortex and hippocampus, before the expansion of tau pathology into other neighbouring areas (Braak and Braak 1991).
The spread of tau pathology in the Alzheimer’s brain was characterised by Braak and Braak in 1991 and their method of scoring tau pathology is still used for pathological analysis (Braak and Braak 1991). This characteristic spread of tau pathology has led to the idea of tau’propagation’ or ‘infectivity’, and it has been shown that extracellular tau aggregates can enter cells to induce misfolding of intracellular tau (Frost et al. 2009). Different methods have been used to demonstrate tau propagation: the injection of brain extract from mice expressing a mutated form of human tau demonstrated that tau pathology could spread from the injection site to neighbouring regions (Clavaguera et al. 2009); and the expression of a human tau transgene in specific neurons showed the spread of tau from these neurons to neighbouring, non-expressing neurons, inducing degeneration (de Calignon et al. 2012). The propagation of tau pathology is thought to involve a trans-synaptic mechanism, spreading along anatomically connected networks (Liu et al. 2012) and although the mechanism of tau secretion and tau uptake are still to be confirmed, one study has suggested that tau fibril uptake occurs via heparin sulphate proteoglycans (Holmes et al. 2013). Tau pathology is accompanied by neuronal loss, following which, tau can be found in the extracellular space either in a monomeric or an aggregated form where it is assembled into extracellular ghost tangles (Cras et al. 1995).
While the pathology of AD has been extensively studied, the underlying causes of the disease remain elusive. Less than 5 % of AD cases are inherited (Mullan et al. 1992), caused by mutations in the genes encoding APP or the presenilins in the ϒ-secretase complex. The remaining 95 % of cases are termed sporadic AD usually occurring after age 65 (hence often referred to as late-onset AD). The causes of sporadic AD are less clear; although sporadic AD is not caused by dominant mutations like familial AD (Pimplikar 2009), there may be a genetic component to some cases of sporadic AD as indicated in recent years by genome-wide association studies (GWAS). These studies use large cohorts to detect single nucleotide polymorphisms (SNPs) that are related to sporadic AD. A large number of genes have been identified by the various GWAS but nine have consistently been identified in all studies (CLU (clusterin), BIN1 (bridging integrator 1), PICALM (phosphatidylinositol clathrin associated lymphoid myeloid), CD2AP (CD2 associated protein), EPHA1 (ephrin receptor A1), CR1 (complement receptor 1), ABCA7 (ATP binding cassette transporter 7), CD33 (Myeloid cell surface antigen CD33), and the MS4A (Membrane-spanning 4-domains subfamily A) gene cluster )(Harold et al. 2009; Bertram and Tanzi 2010; Seshadri et al. 2010; Carrasquillo et al. 2011; Hollingworth et al. 2011; Hu et al. 2011; Wijsman et al. 2011); it is estimated that these genes may account for up to 50 % of sporadic AD cases (Morgan 2011) although how the proteins that these genes encode are involved in the initiation and/or progression of AD is still unclear.
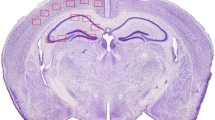
Tissue non-specific alkaline phosphatase (TNAP) is widely expressed in the brain including in the occipital-, frontal- and temporal lobe areas of the cerebral cortex (Negyessy et al. 2011) (see also Chaps. 5 and 6) and also in the hippocampus (Diez-Zaera et al. 2011; Street et al. 2013) where tau pathology initially appears. The high TNAP expression in specific brain areas suggests links to the thalamo-cortical connections (Fonta et al. 2004; Negyessy et al. 2011) which have been shown to be affected in AD (Zhou et al. 2013). TNAP has been shown to have a role in both brain development and brain function (see Chaps. 4, 14 and 18), but does it also have a role in neurodegenerative disease? Our studies, published in 2011 (Kellett et al. 2011; Vardy et al. 2012) and reviewed here, examine the changes in TNAP activity that occur as a result of AD.
2 Changes in CSF and Plasma TNAP Associated with CNS Injury; Could Changes in Plasma TNAP Reflect Neuronal Loss in the Brain?
Changes in cerebrospinal fluid (CSF) (Lampl et al. 1990) and plasma alkaline phosphatase activity (Yamashita et al. 1989; Meythaler et al. 1998) occur as a result of central nervous system injury, including non-traumatic brain injury (Meythaler et al. 1998). The changes in TNAP in brain-damaged patients was shown to increase as secondary brain damage developed and plasma TNAP concentration was shown to correlate with the functional outcome (Yamashita et al. 1989). These previous studies suggested that changes in plasma TNAP as a result of brain injury were an indirect consequence due to liver function changes; but is this an incorrect assumption based on the misconception that TNAP primarily reflects liver function? Could the increase in TNAP in the plasma and CSF as a result of brain injury, traumatic or non-traumatic, be reflective of neuronal loss? The correlation of plasma TNAP with functional outcome would suggest that it might. Previous to our studies on TNAP in AD, elevated alkaline phosphatase activity had been reported in patients with neurodegenerative disease. A study contrasting AD with vascular dementia (VD) indicated that alkaline phosphatase activity was significantly increased in VD compared to AD but did not, unfortunately, study these groups in relation to age-matched controls or correlate alkaline phosphatase activity with cognitive function (Cacabelos et al. 2004).
3 TNAP Activity Is Increased in the Brain and in the Plasma in Alzheimer’s Disease
Our studies investigated the changes in TNAP activity associated with AD in both post-mortem brain samples and in plasma samples from AD patients. In both post-mortem brain samples and in plasma we identified the isoform of alkaline phosphatase being measured as TNAP by using the TNAP-specific inhibitor, levamisole .
Our study (Vardy et al. 2012) demonstrated a significant increase in TNAP activity in post-mortem brain samples from the hippocampus of sporadic AD patients (Fig. 17.1a). TNAP has been shown to be present in the hippocampus (Diez-Zaera et al. 2011; Street et al. 2013) and the increase in TNAP activity in the AD patients compared to non-demented controls suggests a role for TNAP in the progression of AD. In addition to analysing TNAP activity in samples from sporadic AD patients, we also examined post-mortem hippocampal brain samples from familial AD patients. As in sporadic AD, TNAP activity was significantly increased in the hippocampus of familial AD patients compared to age-matched controls (Fig. 17.1b). As the major risk factor for sporadic AD is age we also investigated changes in TNAP activity in samples from an ageing cohort; the results showed that TNAP activity does not correlate with age (r = 0.063, p = 0.853). The increase in TNAP in both sporadic and familial AD demonstrate that the changes seen are likely to be a consequence of AD-associated changes in the brain rather than a primary mechanism of disease. Our data supported previous work showing that TNAP activity is increased in temporal lobe brain samples in AD (Diaz-Hernandez et al. 2010), demonstrating that TNAP activity is also increased in the hippocampus, both in the sporadic and familial forms of the disease.
TNAP activity is increased in the hippocampus in AD. TNAP activity in hippocampal brain samples from a sporadic AD compared to age-matched controls and b from familial AD compared to age-matched controls. Data shown as grouped scatter plot with bar representing the mean. Sporadic AD: n = 5 per group; Familial AD: n = 6 per group. *p < 0.05. (Vardy et al. 2012)
In addition to measuring TNAP activity in the brain we also designed 2 independent studies (Kellett et al. 2011; Vardy et al. 2012) with separate cohorts to investigate whether TNAP activity was also altered in the plasma in AD patients. For both of these studies the two main aims were to examine plasma TNAP and to correlate this with cognitive function. Our Leeds cohort consisted of 110 ‘probable’ AD patients, in accordance with international diagnostic criteria (National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer’s Disease and Related Disorders Association work group) (McKhann et al. 1984) and 110 age- and gender-matched control subjects without evidence of cognitive impairment assessed using the Mini-Mental State Examination (MMSE) (Folstein et al. 1975). Our OPTIMA (Oxford Project To Investigate Memory and Aging) cohort consisted of 121 ‘probable’ (McKhann et al. 1984) or pathologically confirmed AD patients, 89 mild-cognitively impaired (MCI) patients and 180 cognitively-screened non-demented controls assessed using the Cambridge Examination for Mental Disorders (CAMCOG) (Roth et al. 1986). In both of these cohorts we demonstrated that TNAP activity is significantly increased in the plasma of AD patients compared to controls and that these changes are not a result of other underlying conditions, such as liver, bone or inflammatory diseases (Fig. 17.2a, b). In addition, the inclusion of MCI patients in the study (Kellett et al. 2011) identified that this change in TNAP is evident in the early phase of cognitive impairment with raised TNAP levels in MCI patients compared to controls but at an intermediate level to the increase observed in the AD group (Fig. 17.2b). Plasma TNAP therefore appears to be related to clinical diagnosis and, we therefore predicted, could be related to cognitive function. Using the results from cognitive examinations in both cohorts we were able to correlate TNAP activity in plasma with cognitive function in all subjects, including controls. Interestingly, the results showed that TNAP activity significantly inversely correlated with cognitive function in AD patients from our Leeds cohort (rs = –0.211, p = 0.027) and significantly inversely correlated with cognitive function in all groups in our OPTIMA cohort (AD (z = –3.61, p = 0.0003); MCI (z = –2.49, p = 0.013); Control (z = –2.21, p = 0.027)) suggesting that changes in plasma TNAP activity may reflect changes in cognition in any individual. Our final analysis looked at follow-up over 5 years in our OPTIMA cohort. The results of this analysis determined that TNAP activity remained significantly inversely correlated to cognition over all assessments during the 5 year follow-up in AD patients. The analysis showed that the rate of decline is not dependent on TNAP but that changes in TNAP reflect changes in cognitive function in any given individual.
TNAP activity in plasma is significantly increased in AD. a In our Leeds cohort TNAP activity was significantly increased in AD compared to age-matched controls (mean ± SEM: 17.88 ± 0.603 and 15.97 ± 0.596 nmol/min/ml, respectively, p = 0.018); data represented in an error bar graph showing adjusted mean ± SEM, n = 110 per group (Vardy et al. 2012). b In our OPTIMA cohort, TNAP activity was significantly increase in AD compared to control (median (lower quartile, upper quartile): 165.5 (139.5, 195.8) and 149.5 (130.0, 178.0), respectively, p = 0.005). TNAP activity in MCI patients was at a level in between the control and AD groups (164.0 (129.0, 196.0)) but was not significantly different from either the control or AD group. Data represented in a box and whisker plot showing data from initial patient assessment, control n = 180, MCI n = 89, AD n = 121 (Kellett et al. 2011)
4 TNAP as a Marker of AD?
While TNAP activity is increased in the plasma and correlates with cognitive function in all groups (control, MCI and AD), our observations in post-mortem brain samples indicate that changes in TNAP are not correlated with age and are therefore not a result of the normal ageing process. These changes in the brain are a consequence of the disease process, reflective, therefore, of AD-associated changes. However, the correlation of plasma TNAP activity with cognitive function in all groups would suggest that changes in the plasma may also be reflective of a process occurring in all subjects irrespective of diagnosis. What is unclear is whether the increase in plasma TNAP activity is reflective of increased brain TNAP or whether there is a related systemic change in TNAP activity. While there is an increase in plasma TNAP activity in AD the mean values in the AD and control cohorts remained in the clinically ‘normal’ range (10-140 IU/l); in contrast, in traumatic brain injury, plasma alkaline phosphatase activity has been shown to increase above 200 IU/l (Yamashita et al. 1989). From these data it could therefore be concluded that TNAP could reflect brain injury and perhaps neuronal loss, with acute increases following traumatic brain injury and long-term low-level changes in AD. Unfortunately, however, as plasma TNAP activity remains within the ‘normal’ range it could not be used as a predictive or diagnostic biomarker for AD. There is, however, scope to further investigate TNAP as a marker for AD progression and/or effectiveness of therapeutic intervention within an individual patient, or perhaps, to further investigate plasma TNAP measurement in combination with other plasma proteins that have been shown to correlate with cognitive function for a combined AD marker.
5 TNAP and Tau in AD
TNAP has been shown to have a specific role in the neurotoxic events causing AD as a result of its action on hyperphosphorylated tau (See Chap. 18). TNAP can dephosphorylate the extracellular hyperphosphorylated tau that surrounds the neurons (Fig. 17.3). This dephosphorylated tau is an agonist for M1 and M3 muscarinic receptors and its action causes a sustained calcium influx into the cell which is neurotoxic and ultimately results in neuronal loss (Gomez-Ramos et al. 2008; Diaz-Hernandez et al. 2010). This mechanism linking TNAP activity to tau dephosphorylation and the resulting neuronal loss provides evidence of a direct role for TNAP in the progression of AD. The neurotoxic effects resulting from tau dephosphorylated by TNAP suggests that TNAP activity in the brain may therefore be reflective of neuronal loss. Interestingly, it was also noted that activation of muscarinic receptors by dephosphorylated tau increases TNAP expression (Diaz-Hernandez et al. 2010) (Fig. 17.3). This suggests a positive feedback loop to drive tau dephosphorylation by increased TNAP expression, possibly driven by the increased formation of hyperphosphorylated tau seen in AD. This increase in tau dephosphorylation, however, promotes neurotoxicity via its action on muscarinic receptors. Together, the evidence from our work (Kellett et al. 2011) and others (Diaz-Hernandez et al. 2010) that TNAP activity is increased in the brain regions affected in AD supports a role for TNAP in AD, suggesting that with AD progression, brain TNAP activity increases alongside tau levels, causing an increase in neuronal loss and a decline in cognitive function.
The role of TNAP in AD. Schematic diagram to show how toxicity may be mediated via TNAP in AD through tau dephosphorylation. Aβ binds to a receptor on the cell surface and initiates a signalling cascade resulting in tau hyperphosphorylation . The hyperphosphorylated tau can itself cause toxicity resulting in its release into the extracellular space following neuronal death. Alternatively, the hyperphosphorylated tau can be secreted from the donor cell via an, as yet, unknown mechanism. Following secretion, the tau can be taken up into neighbouring neurons, potentially via heparin sulphate proteoglycans (HSPG) resulting in tau infectivity in the recipient cell. Alternatively, the secreted hyperphosphorylated tau can be dephosphorylated by TNAP and the resulting dephosphorylated tau can act on M1 and M3 muscarinic receptors causing calcium influx and neuronal toxicity . The activation of the M1 and M3 muscarinic receptors also induces increased expression of TNAP thereby exacerbating its effects on extracellular hyperphosphorylated tau
6 Conclusions
In conclusion, our work has demonstrated an increase in brain and plasma TNAP activity in AD and has shown that this change in TNAP activity inversely correlates with cognitive function. A direct link between TNAP activity and tau provides a mechanism for increased neurotoxicity and neuronal loss in the AD brain which would correspond to the resulting decline in cognition seen in AD and inversely correlated to TNAP activity. Taken together these results suggest that changes in TNAP activity may reflect neuronal loss in AD.
References
Bertram L, Tanzi RE (2010) Alzheimer disease: new light on an old CLU. Nat Rev Neurol 6(1):11–13
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82(4):239–259
Brayne C (2007) The elephant in the room—healthy brains in later life, epidemiology and public health. Nat Rev Neurosci 8(3):233–239
Burns A, Iliffe S (2009) Alzheimer’s disease. BMJ 338:b158
Cacabelos R, Fernandez-Novoa L, Corzo L, Amado L, Pichel V, Lombardi V, Kubota Y (2004) Phenotypic profiles and functional genomics in Alzheimer’s disease and in dementia with a vascular component. Neurol Res 26(5):459–480
Carrasquillo MM, Belbin O, Hunter TA, Ma L, Bisceglio GD, Zou F, Crook JE, Pankratz VS, Sando SB, Aasly JO, Barcikowska M, Wszolek ZK, Dickson DW, Graff-Radford NR, Petersen RC, Morgan K, Younkin SG (2011) Replication of BIN1 association with Alzheimer’s disease and evaluation of genetic interactions. JAD 24(4):751–758
Clavaguera F, Bolmont T, Crowther RA, Abramowski D, Frank S, Probst A, Fraser G, Stalder AK, Beibel M, Staufenbiel M, Jucker M, Goedert M, Tolnay M (2009) Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol 11(7):909–913
Cras P, Smith MA, Richey PL, Siedlak SL, Mulvihill P, Perry G (1995) Extracellular neurofibrillary tangles reflect neuronal loss and provide further evidence of extensive protein cross-linking in Alzheimer disease. Acta Neuropathol 89(4):291–295
de Calignon A, Polydoro M, Suarez-Calvet M, William C, Adamowicz DH, Kopeikina KJ, Pitstick R, Sahara N, Ashe KH, Carlson GA, Spires-Jones TL, Hyman BT (2012) Propagation of tau pathology in a model of early Alzheimer’s disease. Neuron 73(4):685–697
Diaz-Hernandez M, Gomez-Ramos A, Rubio A, Gomez-Villafuertes R, Naranjo JR, Miras-Portugal MT, Avila J (2010) Tissue-nonspecific alkaline phosphatase promotes the neurotoxicity effect of extracellular tau. J Biol Chem 285(42):32539–32548
Diez-Zaera M, Diaz-Hernandez JI, Hernandez-Alvarez E, Zimmermann H, Diaz-Hernandez M, Miras-Portugal MT (2011) Tissue-nonspecific alkaline phosphatase promotes axonal growth of hippocampal neurons. Mol Biol Cell 22(7):1014–1024
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state. a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Fonta C, Negyessy L, Renaud L, Barone P (2004) Areal and subcellular localization of the ubiquitous alkaline phosphatase in the primate cerebral cortex: evidence for a role in neurotransmission. Cereb Cortex 14(6):595–609
Frost B, Jacks RL, Diamond MI (2009) Propagation of tau misfolding from the outside to the inside of a cell. J Biol Chem 284(19):12845–12852
Gomez-Ramos A, Diaz-Hernandez M, Rubio A, Miras-Portugal MT, Avila J (2008) Extracellular tau promotes intracellular calcium increase through M1 and M3 muscarinic receptors in neuronal cells. Mol Cell Neurosci 37(4):673–681
Harold D, Abraham R, Hollingworth P, Sims R, Gerrish A, Hamshere ML, Pahwa JS, Moskvina V, Dowzell K, Williams A, Jones N, Thomas C, Stretton A, Morgan AR, Lovestone S, Powell J, Proitsi P, Lupton MK, Brayne C, Rubinsztein DC, Gill M, Lawlor B, Lynch A, Morgan K, Brown KS, Passmore PA, Craig D, McGuinness B, Todd S, Holmes C, Mann D, Smith AD, Love S, Kehoe PG, Hardy J, Mead S, Fox N, Rossor M, Collinge J, Maier W, Jessen F, Schurmann B, van den Bussche H, Heuser I, Kornhuber J, Wiltfang J, Dichgans M, Frolich L, Hampel H, Hull M, Rujescu D, Goate AM, Kauwe JS, Cruchaga C, Nowotny P, Morris JC, Mayo K, Sleegers K, Bettens K, Engelborghs S, De Deyn PP, Van Broeckhoven C, Livingston G, Bass NJ, Gurling H, McQuillin A, Gwilliam R, Deloukas P, Al-Chalabi A, Shaw CE, Tsolaki M, Singleton AB, Guerreiro R, Muhleisen TW, Nothen MM, Moebus S, Jockel KH, Klopp N, Wichmann HE, Carrasquillo MM, Pankratz VS, Younkin SG, Holmans PA, O’Donovan M, Owen MJ, Williams J (2009) Genome-wide association study identifies variants at CLU and PICALM associated with Alzheimer’s disease. Nat Genet 41(10):1088–1093
Hollingworth P, Harold D, Sims R, Gerrish A, Lambert JC, Carrasquillo MM, Abraham R, Hamshere ML, Pahwa JS, Moskvina V, Dowzell K, Jones N, Stretton A, Thomas C, Richards A, Ivanov D, Widdowson C, Chapman J, Lovestone S, Powell J, Proitsi P, Lupton MK, Brayne C, Rubinsztein DC, Gill M, Lawlor B, Lynch A, Brown KS, Passmore PA, Craig D, McGuinness B, Todd S, Holmes C, Mann D, Smith AD, Beaumont H, Warden D, Wilcock G, Love S, Kehoe PG, Hooper NM, Vardy ER, Hardy J, Mead S, Fox NC, Rossor M, Collinge J, Maier W, Jessen F, Ruther E, Schurmann B, Heun R, Kolsch H, van den Bussche H, Heuser I, Kornhuber J, Wiltfang J, Dichgans M, Frolich L, Hampel H, Gallacher J, Hull M, Rujescu D, Giegling I, Goate AM, Kauwe JS, Cruchaga C, Nowotny P, Morris JC, Mayo K, Sleegers K, Bettens K, Engelborghs S, De Deyn PP, Van Broeckhoven C, Livingston G, Bass NJ, Gurling H, McQuillin A, Gwilliam R, Deloukas P, Al-Chalabi A, Shaw CE, Tsolaki M, Singleton AB, Guerreiro R, Muhleisen TW, Nothen MM, Moebus S, Jockel KH, Klopp N, Wichmann HE, Pankratz VS, Sando SB, Aasly JO, Barcikowska M, Wszolek ZK, Dickson DW, Graff-Radford NR, Petersen RC, van Duijn CM, Breteler MM, Ikram MA, DeStefano AL, Fitzpatrick AL, Lopez O, Launer LJ, Seshadri S, Berr C, Campion D, Epelbaum J, Dartigues JF, Tzourio C, Alperovitch A, Lathrop M, Feulner TM, Friedrich P, Riehle C, Krawczak M, Schreiber S, Mayhaus M, Nicolhaus S, Wagenpfeil S, Steinberg S, Stefansson H, Stefansson K, Snaedal J, Bjornsson S, Jonsson PV, Chouraki V, Genier-Boley B, Hiltunen M, Soininen H, Combarros O, Zelenika D, Delepine M, Bullido MJ, Pasquier F, Mateo I, Frank-Garcia A, Porcellini E, Hanon O, Coto E, Alvarez V, Bosco P, Siciliano G, Mancuso M, Panza F, Solfrizzi V, Nacmias B, Sorbi S, Bossu P, Piccardi P, Arosio B, Annoni G, Seripa D, Pilotto A, Scarpini E, Galimberti D, Brice A, Hannequin D, Licastro F, Jones L, Holmans PA, Jonsson T, Riemenschneider M, Morgan K, Younkin SG, Owen MJ, O’Donovan M, Amouyel P, Williams J (2011) Common variants at ABCA7, MS4A6A/MS4A4E, EPHA1, CD33 and CD2AP are associated with Alzheimer’s disease. Nat Genet 43(5):429–435
Holmes BB, Devos SL, Kfoury N, Li M, Jacks R, Yanamandra K, Ouidja MO, Brodsky FM, Marasa J, Bagchi DP, Kotzbauer PT, Miller TM, Papy-Garcia D, Diamond MI (2013) Heparan sulfate proteoglycans mediate internalization and propagation of specific proteopathic seeds. PNAS 110(33):E3138–E3147
Hu X, Pickering EH, Hall SK, Naik S, Liu YC, Soares H, Katz E, Paciga SA, Liu W, Aisen PS, Bales KR, Samad TA,John SL (2011) Genome-wide association study identifies multiple novel loci associated with disease progression in subjects with mild cognitive impairment. Transl Psychiatry 1:e54
Iqbal K, Alonso Adel C, Chen S, Chohan MO, El-Akkad E, Gong CX, Khatoon S, Li B, Liu F, Rahman A, Tanimukai H, Grundke-Iqbal I (2005) Tau pathology in Alzheimer disease and other tauopathies. Biochim Biophys Acta 1739(2–3):198–210
Kellett KA, Williams J, Vardy ER, Smith AD, Hooper NM (2011) Plasma alkaline phosphatase is elevated in Alzheimer’s disease and inversely correlates with cognitive function. Int J Mol Epidemiol Genet 2(2):114–121
Lampl Y, Paniri Y, Eshel Y, Sarova-Pinchas I (1990) Alkaline phosphatase level in CSF in various brain tumors and pulmonary carcinomatous meningitis. J Neurooncol 9(1):35–40
Liu L, Drouet V, Wu JW, Witter MP, Small SA, Clelland C, Duff K (2012) Trans-synaptic spread of tau pathology in vivo. PLoS ONE 7(2):e31302
Matthews FE, McKeith I, Bond J, Brayne C (2007) Reaching the population with dementia drugs: what are the challenges? Int J Geriatr Psychiatry 22(7):627–631
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology 34(7):939–944
Meythaler JM, Hazlewood J, DeVivo MJ, Rosner M (1998) Elevated liver enzymes after nontraumatic intracranial hemorrhages. Arch Phys Med Rehabil 79(7):766–771
Morgan K (2011) The three new pathways leading to Alzheimer’s disease. Neuropathol Appl Neurobiol 37(4):353–357
Mullan M, Crawford F, Axelman K, Houlden H, Lilius L, Winblad B, Lannfelt L (1992) A pathogenic mutation for probable Alzheimer’s disease in the APP gene at the N-terminus of beta-amyloid. Nat Genet 1(5):345–347
Negyessy L, Xiao J, Kantor O, Kovacs GG, Palkovits M, Doczi TP, Renaud L, Baksa G, Glasz T, Ashaber M, Barone P, Fonta C (2011) Layer-specific activity of tissue non-specific alkaline phosphatase in the human neocortex. Neuroscience 172:406–418
Pimplikar SW (2009) Reassessing the amyloid cascade hypothesis of Alzheimer’s disease. Int J Biochem Cell Biol 41(6):1261–1268
Roth M, Tym E, Mountjoy CQ, Huppert FA, Hendrie H, Verma S, Goddard R (1986) CAMDEX. A standardised instrument for the diagnosis of mental disorder in the elderly with special reference to the early detection of dementia. British J Psych 149:698–709
Seshadri S, Fitzpatrick AL, Ikram MA, DeStefano AL, Gudnason V, Boada M, Bis JC, Smith AV, Carassquillo MM, Lambert JC, Harold D, Schrijvers EM, Ramirez-Lorca R, Debette S, Longstreth WT Jr, Janssens AC, Pankratz VS, Dartigues JF, Hollingworth P, Aspelund T, Hernandez I, Beiser A, Kuller LH, Koudstaal PJ, Dickson DW, Tzourio C, Abraham R, Antunez C, Du Y, Rotter JI, Aulchenko YS, Harris TB, Petersen RC, Berr C, Owen MJ, Lopez-Arrieta J, Varadarajan BN, Becker JT, Rivadeneira F, Nalls MA, Graff-Radford NR, Campion D, Auerbach S, Rice K, Hofman A, Jonsson PV, Schmidt H, Lathrop M, Mosley TH, Au R, Psaty BM, Uitterlinden AG, Farrer LA, Lumley T, Ruiz A, Williams J, Amouyel P, Younkin SG, Wolf PA, Launer LJ, Lopez OL, van Duijn CM, Breteler MM (2010) Genome-wide analysis of genetic loci associated with Alzheimer disease. JAMA 303(18):1832–1840
Street SE, Kramer NJ, Walsh PL, Taylor-Blake B, Yadav MC, King IF, Vihko P, Wightman RM, Millan JL, Zylka MJ (2013) Tissue-Nonspecific alkaline phosphatase acts redundantly with PAP and NT5E to generate adenosine in the dorsal spinal cord. J Neurosci 33(27):11314–11322
Vardy ER, Kellett KA, Cocklin SL, Hooper NM (2012) Alkaline phosphatase is increased in both brain and plasma in Alzheimer’s disease. Neurodegener Dis 9(1):31–37
Wijsman EM, Pankratz ND, Choi Y, Rothstein JH, Faber KM, Cheng R, Lee JH, Bird TD, Bennett DA, Diaz-Arrastia R, Goate AM, Farlow M, Ghetti B, Sweet RA, Foroud TM, Mayeux R (2011) Genome-wide association of familial late-onset Alzheimer’s disease replicates BIN1 and CLU and nominates CUGBP2 in interaction with APOE. PLoS Genet 7(2):e1001308
Yamashita M, Sasaki M, Mii K, Tsuzuki M, Takakura K, Yoshinoya S, Ohkubo A (1989) Measurement of serum alkaline phosphatase isozyme I in brain-damaged patients. Neurol Med Chir (Tokyo) 29(11):995–998
Zhou B, Liu Y, Zhang Z, An N, Yao H, Wang P, Wang L, Zhang X, Jiang T (2013) Impaired functional connectivity of the thalamus in alzheimer’s disease and mild cognitive impairment: a resting-state FMRI study. Curr Alzheimer Res 10(7):754–766
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Kellett, K.A.B., Hooper, N.M. (2015). The Role of Tissue Non-specific Alkaline Phosphatase (TNAP) in Neurodegenerative Diseases: Alzheimer’s Disease in the Focus. In: Fonta, C., Négyessy, L. (eds) Neuronal Tissue-Nonspecific Alkaline Phosphatase (TNAP). Subcellular Biochemistry, vol 76. Springer, Dordrecht. https://doi.org/10.1007/978-94-017-7197-9_17
Download citation
DOI: https://doi.org/10.1007/978-94-017-7197-9_17
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-017-7196-2
Online ISBN: 978-94-017-7197-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)