Abstract
Preoperative anxiety is an unpleasant state resulting from the anticipation of a threatening situation. It contributes to acute preoperative stress. Up to 40 % of patients experience anxiety before surgery that is associated with adverse intraoperative course and postoperative outcomes. Assessment of preoperative anxiety is challenging and mainly based on lengthy questionnaires or plasma biomarkers that cannot be used for bedside decision-making. There is a potential role for noninvasive, real-time, and point-of-care biomarkers such as salivary amylase (SA) to identify anxious patients and to target preoperative pharmacologic or non-pharmacologic interventions in these patients. SA is the principal saliva protein and is mainly secreted by the parotid glands. The autonomic nervous system plays a major role in SA secretion. An association between changes in SA during exposure to a stressful stimulus and changes in blood norepinephrine or heart rate variability indices strongly suggests that SA is an accurate marker of sympathetic nervous system activity. There is also an association between changes in SA during exposure to a stressful stimulus and changes in anxiety state. Saliva can be collected by many methods. SA activity (SAA) is measured by its enzymatic activity and depends on the collection method, which needs to be standardized. Point-of-care SAA measurement is now possible with a handheld format automated analyzer. SAA increases quickly after exposure to a stressful stimulus (i.e., less than 5 min) and returns rapidly to baseline (i.e., less than 15 min) during soothing conditions (“on–off” marker). The high amplitude of SAA variation between basal and stress conditions makes SAA a highly sensitive and dynamic marker of the acute stress response, including preoperative anxiety. However, several non-stress-related factors (time of day, smoking, food, alcohol or caffeine intake, physical exercise, drugs, and comorbidities) can influence basal and stress-induced SAA. Saliva flow rate, age, and sex have little influence on SAA. Its great within- and between-individual variations imply that SAA should be measured for each patient both before and during the stressful event. A twofold increase in SAA after exposure to a stressful stimulus can be considered biologically relevant. Several human studies demonstrate an increase in SAA after exposure to acute stressful stimuli, including arrival at the operating theater. The literature is still scarce about the association between preoperative SAA and intraoperative course or postoperative outcome. It remains a stimulating area of research.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Key Facts on Salivary Amylase
-
Salivary amylase (SA) is the principal protein in saliva.
-
SA is mainly secreted by the parotid glands under the control of the autonomic nervous system.
-
During acute exposure to stressful stimuli, there is an association between changes in SA activity and changes in other stress markers (blood norepinephrine, heart rate variability indices) or changes in anxiety state.
-
A twofold increase in SA activity can be considered biologically relevant.
-
Several human studies demonstrate an increase in SA activity after exposure to acute stressful stimuli including clinical situations.
-
The role of SA in clinical practice remains to be determined.
Definition of Words and Terms
Stress
A state in which homeostasis is actually threatened or perceived to be so, by emotional or physical stressors.
Anxiety
An unpleasant state resulting from the anticipation of a threatening situation, i.e., the fear of what is going to happen. Preoperative anxiety contributes to preoperative stress.
Reference Change Value
The minimal difference expressed in percentage between two consecutive measurements in the same subject to consider that the difference between the two measurements is biologically significant. It takes into account the variability related to the preparation of the sample required to measure the marker, the technique of measurement, and the patient.
Index of Individuality
The ratio of the within-subject biological variation to the between-subject variation. A low index (<0.6) indicates that a patient should be assessed with respect to his or her individual level and not with respect to a population-derived reference.
Enzymatic Activity
The capacity of an enzyme to catalyze 1 μmol of substrate per minute. It is generally expressed in units per milliliter (U/mL).
Introduction
Perioperative medicine encompasses care of the patient preparing for, undergoing, and recovering from surgery or other nonsurgical interventional procedures. There is increased awareness of the high prevalence of anxiety during the preoperative period (Moerman et al. 1996; Wattier et al. 2011). Apart from compromising patients’ psychological well-being, an increasing body of evidence is available describing the adverse consequences of preoperative anxiety on patients’ intraoperative course and postoperative outcome. It may translate into significant medical problems and costs owing to the high number of surgical/interventional procedures performed annually, i.e., more than 240 million worldwide (Weiser et al. 2008). Preoperative anxiety could therefore be viewed as a public health issue.
Although anesthesiologists have always intuitively known that preoperative anxiety is a problem, structured diagnosis and management of preoperative anxiety is a relatively new field of preoperative medicine. Careful assessment of preoperative anxiety should become a routine part of preoperative evaluation in order to identify anxious patients and propose preoperative pharmacologic or non-pharmacologic interventions. However, anxiety assessment in clinical practice is challenging and time-consuming. In this context, there is a potential role for noninvasive, real-time, and point-of-care markers of anxiety (Biomarkers Definitions Working Group 2001). Several studies have focused on salivary amylase (SA) as a stress biomarker easy to collect and to measure. A growing literature originating from behavioral sciences demonstrates that exposure to a stressful or anxiogenic stimulus is associated with an increase in SA activity (SAA) (Nater and Rohleder 2009; Rohleder and Nater 2009). Evidence from medical science is still scarce but is a promising area of research.
In this chapter dedicated to SA as a marker of anxiety, we will successively introduce (i) the definition of stress and anxiety, consequences of preoperative anxiety for patients’ intraoperative course, and postoperative outcome and the assessment of patients’ preoperative anxiety; (ii) preanalytical and analytical considerations regarding SA; (iii) results of human medical studies investigating SA; (iv) and potential applications.
Preoperative Stress and Anxiety
Definition and Prevalence
Living organisms maintain a complex dynamic equilibrium called homeostasis. Homeostasis is constantly challenged by internal or external potentially adverse situations, termed stressors. Stressors comprise a long list of potentially adverse forces, which can be emotional or physical. Stress is defined as a state in which homeostasis is actually threatened or perceived to be so (McEwen 1998; Chrousos 2009). Homeostasis is reestablished by a complex repertoire of behavioral and physiological adaptive responses of the organism. The process of maintaining homeostasis by active means has been called allostasis (i.e., achieving stability through change) (McEwen 1998).
Goldstein therefore defined stress as “a condition where expectations, whether genetically programmed, established by prior learning, or deduced from circumstances do not match the current or anticipated perceptions of the internal or external environment, and this discrepancy between what is observed/sensed and what is expected/programmed elicits patterned, compensatory responses” (Goldstein 1995). Globally, it implies (i) the recognition of a difference between what is expected and what is measured, (ii) the integration of such information, (iii) the activation of several biological pathways, (iv) an immediate physiological and behavioral response, and (v) a long-term physiological and behavioral response.
The immediate response to acute stressors is relatively stereotypic. It is an innate response that has evolved to coordinate homeostasis and protect the organism (Chrousos 2009). The principal peripheral effectors are glucocorticoids, especially cortisol, and the catecholamines norepinephrine and epinephrine. Cortisol is regulated by the hypothalamic–pituitary–adrenal axis. Catecholamines are regulated by the systemic and adrenomedullary sympathetic nervous systems (the autonomic nervous system).
Although the terms anxiety and stress are used nearly interchangeably in the medical literature, the term anxiety is much more restrictive. Preoperative anxiety can be defined as an unpleasant state resulting from the anticipation of threatening situations, demands, or dangers, i.e., the fear of what is going to happen. Such a definition excludes anxiety as a chronic mental disorder.
A wide range, from 10 % to 80 %, of preoperative anxiety prevalence has been reported. It reflects the differences in the definitions, tools, and thresholds used to diagnose anxiety (Moerman et al. 1996). A recent study defining anxiety with the Spielberger State-Trait Inventory (see below) in a general preoperative population reported a prevalence of anxiety of up to 40 % (Wattier et al. 2011). Anxiety is triggered when planning surgery and reaches a maximum at the time of admission to hospital or arrival in the operating room (Johnston 1980).
In this text, we will focus on preoperative anxiety rather than stress since it is easier to measure.
Clinical Consequences of Preoperative Anxiety and Stress
There are a large number of clinical studies suggesting or demonstrating an association between preoperative anxiety and adverse intraoperative course or short- and long-term postoperative outcomes. In many of the studies, preoperative anxiety was assessed with psychometric tests such as the Spielberger State-Trait Inventory or a visual analog scale for self-evaluation (see below) (Spielberger et al. 1983; Kindler et al. 2000). The consequences supported by evidence are (i) increased requirement for hypnotic drugs to induce general anesthesia (Gras et al. 2010; Kil et al. 2012), (ii) increased incidence and severity of arterial hypotension after spinal anesthesia (Orbach-Zinger et al. 2012), (iii) increase in acute and chronic postoperative pain associated with decreased satisfaction with pain-relieving techniques (Jamison et al. 1993; Theunissen et al. 2012; Lunn et al. 2013; Masselin-Dubois et al. 2013), (iv) increased rates of surgical site infections (Levandovski et al. 2008), (v) increased rates of hospital readmission (Tully et al. 2008), and (vi) increased rates of postoperative behavioral changes in children (Kain et al. 1999).
Several consequences of preoperative anxiety are suggested but not yet unequivocally demonstrated. They include (i) occurrence of arterial hypotension during induction of general anesthesia (Fujiwara et al. 2007); (ii) decreased quality of recovery after general anesthesia (Liu et al. 1994; Kain et al. 2000, 2001); (iii) postoperative cognitive dysfunction in adults; (iv) increased cardiovascular morbidity, especially after cardiac surgery (Tully et al. 2008, 2011; Tully and Szekely 2013); and (v) impaired wound healing (Broadbent et al. 2003).
Taken together, these results strongly suggest that preoperative anxiety is associated with a significant risk of worsened intraoperative course and postoperative outcome and further underline the need for careful and systematic preoperative assessment and management of preoperative anxiety.
Measurement of Preoperative Anxiety and Stress in the Clinical Setting
There are several tools that can be used to identify patients with preoperative anxiety: (i) psychometric tests such as the Spielberger State-Trait Inventory or the Amsterdam Preoperative Anxiety and Information Scale (Spielberger et al. 1983; Moerman et al. 1996), (ii) visual analog scale for self-evaluation (also called the anxiety thermometer) (Kindler et al. 2000), (iii) physical signs (heart rate, arterial blood pressure) that can be used to derive more complex estimators of anxiety by using devices that measure the balance between the sympathetic and parasympathetic nervous system activation (Piccirillo et al. 1997; Miu et al. 2009), and (iv) biomarkers such as cortisol or catecholamines in plasma or cortisol and amylase in saliva (Nater and Rohleder 2009). Statistical correlations among the measurements of anxiety yielded by these different tools are modest. This can be explained by the complexity of the biological systems that contribute to anxiety and the possible discrepancy between self-perceived anxiety and objectively measured parameters.
The ideal marker of preoperative anxiety, from a clinical and practical point of view, should be noninvasive, easily measured, reproducible, and dynamic (rapid temporal changes) and provide real-time results that allow rapid decision-making. Markers that cannot provide real-time results (e.g., the measurement of heart rate variability or plasma catecholamine concentrations) are interesting from a research point of view, but are not useful for clinical decision-making in the operating theater. Physical signs (heart rate, arterial blood pressure) provide real-time results but can be confounded by other physiological/pathophysiological situations (e.g., heart rate can be increased because of hypovolemia or its increase attenuated as a result of chronic treatment with drugs that slow the heart rate, such as beta-blockers). Self-evaluation is not reliable as many patients estimate that they are not stressed on a visual analog scale, despite exhibiting clear, objective signs of anxiety. Moreover, self-evaluation may be too time-consuming for routine clinical practice and clinical decision-making and may not be applicable to patients with language or comprehension problems.
SA is an attractive biomarker. Its validation as a biomarker of preoperative anxiety is, however, in its infancy.
Salivary Amylase
During the past decades, SA has been investigated in numerous behavioral studies as a potential noninvasive and sensitive biomarker of acute stress-induced activity of the sympathetic nervous system (Nater and Rohleder 2009). SAA has been positively associated with plasma norepinephrine concentration, a well-established indicator of the activation of the sympathetic nervous system (Fig. 1). It has also been associated with other markers of sympathetic nervous system activity such as those derived from heart rate variability analysis (Chatterton et al. 1996; Nater et al. 2006; Thoma et al. 2012). Moreover, changes in SAA during an acute stressful exposure have been positively associated with anxiety changes, measured with the Spielberger State-Trait Inventory (Noto et al. 2005).
An association was observed between changes in SAA and changes in blood norepinephrine concentration during a psychosocial stress (the Trier Social Stress Test or TSST) in 66 healthy subjects (40 women). The TSST consists of a 5-min anticipation period, followed by a 5-min free speech in a hypothetical job interview, and another 5 min of mental arithmetic, all in front of an audience and a video camera (Data are from Thoma et al. with permission from the Publishers (Thoma et al. 2012))
In this section, we will successively introduce (i) physiological considerations about saliva and SA, (ii) saliva collection methods, (iii) SA measurement assays, and (iv) factors that influence SAA.
Saliva and Amylase Physiology (de Almeida Pdel et al. 2008)
Saliva Secretion
Saliva is a clear fluid composed of approximately 98 % water and 2 % electrolytes (i.e., sodium, potassium, chloride, calcium, bicarbonate, phosphate) and proteins such as enzymes (alpha amylase), hormones, growth factors, antimicrobial agents, and immunoglobulins. It also contains some glucose and nitrogenous products, such as urea and ammonia. Saliva has several physiological functions including protection of the oral cavity, host defense, and digestion (de Almeida Pdel et al. 2008).
The salivary glands are innervated and stimulated by both parasympathetic and sympathetic branches of the autonomic nervous system. Even in basal conditions, the secretion of saliva is dependent of autonomic nervous system stimulation. Three major salivary glands are described: the parotid glands, the submandibular glands, and the sublingual glands, distributed by pairs on each side of the oral cavity. They are associated with a multitude of minor salivary glands located in lingual, palatal, and labial tissues. Salivary gland production by a healthy subject ranges from 1 to 1.5 l/day. Saliva can be divided into specific saliva, which is produced by a specific gland, and whole saliva, which is a mixture of the saliva originating from all salivary glands (Humphrey and Williamson 2001).
The contribution of each major salivary gland to protein and fluid production is different. The parotid glands produce and secrete 80 % of amylase, and the submandibular and sublingual glands produce and secrete essentially mucins. There is also a difference in the contribution of each salivary gland depending on the state of stimulation. About 65 % of unstimulated saliva originates from the submandibular gland, 25 % from the parotid gland, 4 % from the sublingual gland, and 8 % from other salivary glands (Schenkels et al. 1995). Under stimulated conditions, the saliva from the parotid glands increases to 50 % of total saliva (Humphrey and Williamson 2001). These notions are of major importance for saliva collection, especially regarding the exact location of saliva sampling in the oral cavity and the possible stimulation of the salivary flow by the technique used for collection.
At rest, there is a small and continuous salivary flow that moisturizes and lubricates the oral tissues. Stimulated saliva is produced by mechanical, gustatory, olfactory, or pharmacologic stimuli and contributes 80–90 % of daily salivary production. The normal stimulated salivary flow ranges from 1 to 3 mL/min in adults, and the normal unstimulated salivary flow ranges from 0.25 to 0.35 mL/min. However, according to the wide biological variation of salivary flow, it must be monitored individually in order to determine individual ranges. Several factors, such as hydration, smoking, circadian cycle, medications, food, or alcohol, influence salivary flow and salivary composition and therefore SAA. They must be taken into account in study protocols to avoid misinterpretation (de Almeida Pdel et al. 2008).
Salivary α-Amylase
Human α-amylase is a 46–60 kDa protein officially classified as family 13 of the glycosyl hydrolases. It exists in two forms, produced mainly in the pancreas and in the salivary glands. α-Amylase is also present in every mucosal fluid (e.g., in tears, semen, sweat, and bronchial mucus). Salivary α-amylase is the product of the AMY1 gene and pancreatic α-amylase the product of the AMY2 gene (Schenkels et al. 1995). These two forms are very similar with 97 % amino acid homology. There is a wide variation in the number of copies of AMY1 genes, and this is directly proportional to the salivary α-amylase content in saliva (Santos et al. 2012).
SA is one of the principal proteins in saliva, accounting for 10–20 % of the total protein content. Unlike free salivary cortisol, SA does not diffuse from blood to saliva. It is locally produced by the highly differentiated acinar cells of the salivary glands, mainly by the parotid glands, and stored in granules. The sympathetic nervous system plays a key role in the SA secretion that occurs after activation of alpha- and beta-adrenergic receptors (Nater and Rohleder 2009).
There is a strong diurnal profile of SA as described by Nater et al. (2007), characterized by a pronounced decrease within 60 min after awakening followed by a steady increase in SAA during the course of the day with peak values at around 4:00–5:00 pm (Fig. 2). The maximal increase in SAA during the day does not exceed 75 %.
Diurnal course of SAA and salivary cortisol concentrations in 76 healthy subjects (44 women). A pronounced decrease within 60 min after awakening is observed followed by a steady increase in SAA during the course of the day. The maximal increase in SAA does not exceed 75 %. The change in cortisol concentration follows an inverse pattern (Data are from Nater et al. with permission from the publishers (Nater et al. 2007))
The main function of SA is the enzymatic digestion of starch and carbohydrates (glycogens, dextrins). SA catalyzes the hydrolysis of α (1,4) glycosidic linkages between glucose residues of polysaccharides. It also contributes to the mucosal immunity of the oral cavity by inhibiting adherence and growth of bacteria (Granger et al. 2007).
Saliva Collection
Saliva sampling is a noninvasive, easy-to-perform collection method and a stress-free alternative to blood collection. It also enables collection of samples in specific populations (e.g., newborns, children, elderly) and in circumstances when blood or urine sampling is not possible or feasible (Kaufman and Lamster 2002).
Collection Methods
Numerous collection methods have been described during the past decades in the literature, and different saliva collection devices are currently available (Rohleder and Nater 2009). In this section, we will focus on methods that can be used in clinical research or clinical practice. It has to be pointed out that SAA varies greatly depending on the collection methods. These methods allow the collection of (i) whole saliva or saliva from a specific gland (ii) and of unstimulated or stimulated saliva. Moreover, samples can be obtained on absorbent material (cotton roll) or by passive drooling or spitting in tubes.
The most commonly used technique on absorbent material for SAA measurement is the Salivette® (SARSTEDT AG & Co, Nümbrecht, Germany) (Fig. 3). It allows repeated collection of saliva and the measurement of other salivary components such as cortisol, allowing a multimarker approach. It consists of a cotton roll placed in the mouth for 1–5 min. When time of collection is over, the cotton roll is placed in a plastic container, and saliva is extracted by centrifugation. It is advisable to standardize saliva collection on absorbent materials within the same study to avoid bias. The participants will be allowed (or not) to chew the cotton roll to stimulate salivary flow and will be instructed on the location of the cotton roll in their mouth during the experiment to collect either saliva from specific glands or whole saliva. This saliva collection device presents some advantages. Firstly, saliva collection is easy to learn and to perform, even by untrained persons. Secondly, it is also perceived as a “clean” technique compared with drooling or spitting techniques. Thirdly, the cotton roll acts as a filter and retains the mucous components and other contaminants present in saliva. The fluid obtained after centrifugation is therefore directly available for analysis. Fourthly, independence between SAA and salivary flow rate under stress conditions has been demonstrated with this device (Rohleder et al. 2006). However, other saliva collection devices have been developed which are more appropriate for newborns such as hydrocellulose microsponges or eye spears (Sorbettes®).
The best method used to collect unstimulated saliva is the passive drooling technique described by Navazesh (1993). The sequence is simple: participants are instructed to fill their mouth with saliva for 2–5 min and then collect accumulated saliva in a tube by drooling it through a funnel, by spitting it or by aspirating it. With this technique, whole saliva is collected and represents the production of all glands, which is the major advantage of this technique. Nevertheless, this collection method needs to be done under supervision with motivated participants, and saliva collected by this technique contains mucous components and contaminants that do not allow immediate analysis.
After collection, preservatives such as sodium azide should be excluded as they interfere with the determination of SAA (DeCaro 2008). Saliva samples can be stored at room temperature or at 4 °C for up to 3 weeks without significant alteration of SAA (DeCaro 2008). Freezing at −20 °C or lower temperatures is recommended for long-term storage. Cycles of freezing and thawing do not affect SAA. It is also recommended to submit saliva samples to at least one freeze and thaw cycle, even if time between collection and analysis is short, to break down mucous components that can interfere with analysis (Shirtcliff et al. 2001).
Salivary Amylase Measurement
Measurement Assays
Pancreatic α-amylase activity in human serum or plasma is routinely determined by enzymatic measurement assays in biochemistry laboratories. Thus, numerous methods are available for the measurement of pancreatic α-amylase activity in plasma and urine. They can be applied easily to the determination of SAA, because of the high homology between the two enzymes. These measurements of enzyme kinetics can be performed directly on integrated biochemistry analyzers, as recommended by the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC). In the typical assay protocol, saliva is diluted 1:200 (vol:vol) in saline prior to the measurement of the activity. Alpha-amylase is measured by a colorimetric assay using a specific chromogenic substrate. Yamaguchi et al. have described a handheld format automated analyzer, the Cocoro meter®, adapted to point-of-care testing. It measures SAA in a saliva-loaded strip of absorbent paper (Yamaguchi et al. 2004, 2006). Enzyme-linked immunosorbent assay (ELISA) and radioimmunoassay (RIA) are obsolete, not cost-effective, and time-consuming techniques. They are of use in specifically determining the concentration of the protein and not its activity.
Units of Measurements
SAA is generally reported as units per mL (U/mL). Another way to report SAA results is to measure amylase output, which is the expression of SAA (U/mL) relative to saliva flow rate (mL/min). In this case, amylase output is reported in U/min. Saliva flow rate is determined by collecting saliva over a fixed period of time (2–5 min), and then, considering that the density of saliva is 1.0 g/mL, the volume is determined gravimetrically.
SAA Variability
SAA values are influenced by many factors. We detail below the major factors that account for SAA variability. Other factors are described in Table 1.
Timing of saliva collection should be carefully determined and controlled to avoid confusion between the natural increase occurring after awakening and a potential SA stress-related response (Beltzer et al. 2010). The SA diurnal pattern is not influenced by non-stress-related factors such as body mass index, level of physical activity, smoking, drinking, food consumption, or sleep disturbances. Age has a slight impact with reduced increase during the day in older people (Nater et al. 2007). Out et al. showed that the diurnal profile of SA is as stable over time as that of salivary cortisol (Out et al. 2011, 2013).
SAA can be influenced by the type of saliva collected. Failing to collect saliva samples always in the same location can potentially increase SAA measurement error (Harmon et al. 2008). Moreover, considering that saliva from parotid and submandibular glands has higher levels of SAA than saliva from the other glands, the SA diurnal pattern may be more pronounced if saliva is collected from these locations and falsely increase values (Beltzer et al. 2010).
According to Bosch et al., the use of Salivette® introduces measurement error for numerous salivary analytes, including SA (Bosch et al. 2011). The cotton roll has an absorbent capacity that decreases when more fluid is taken up and can reach saturation. Therefore, this limited volume of saliva absorbed can influence SA values. Moreover, further limitations are the lack of standardization of the duration of saliva collection and the stimulus determining flow rate, when using this type of device.
The influence of saliva flow rate on SAA depends on the absence or presence of a stress-induced stimulus. Using the passive drooling collection method in resting conditions, several authors have demonstrated the strong positive association between SAA (IU/L) and SA output (IU/min) (Bosch et al. 2011; Arhakis et al. 2013). On the contrary, under stress conditions and saliva collection with Salivette®, Rohleder et al. reported that that SAA is independent of saliva flow rate (Rohleder et al. 2006).
Acute physical exercise increases SAA in both adults and children (Obayashi 2013).
Recommendations for Saliva Collection
According to the numerous factors of variability, it is important before saliva collection to instruct participants:
-
To avoid eating and drinking at least 1 h before collection
-
To avoid smoking, chewing gum, and drinking coffee at least 1 h before collection
-
To rinse their mouth with deionized water
-
To rest for 5 min before beginning the collection
-
To avoid stimulation of salivary flow and protein secretion by gustatory stimuli
For Salivette®, participants should be instructed:
-
Where to place the cotton roll in their mouth
-
To keep the cotton roll in their mouth for an exact period of time (generally 2 min)
-
To chew the cotton roll or not (Soeda et al. 2012)
Salivary Amylase in the Clinical Setting
As discussed earlier, the association between stress-induced changes in SAA and changes in plasma norepinephrine concentration, heart rate variability indices, or anxiety suggests that SAA could be useful in assessing anxiety or stress in the clinical setting (Chatterton et al. 1996; Noto et al. 2005; Nater et al. 2006; Thoma et al. 2012). However, some aspects of the interpretation of SAA results must be considered before analyzing the results of human clinical studies.
Interpretation of SAA Results: Reference Change Value and Index of Individuality
SAA values are highly variable. In order to properly interpret a variation between basal SAA and SAA during acute stressful exposure, several statistical calculations must be performed, such as the reference change value (RCV) (Omar et al. 2008). The RCV is defined as the necessary variation expressed in percentage between two sequential measurements to consider the difference between the two (or more) measurements as biologically relevant. RCV is calculated as follows: \( \mathrm{R}\mathrm{C}\mathrm{V}=\sqrt{\mathrm{n}}\times \mathrm{z}\times \sqrt{\left({\mathrm{CVp}}^2+{\mathrm{CVa}}^2+{\mathrm{CVi}}^2\right)} \). The RCV takes into account the variability related to (i) the preparation of the sample required to measure the marker (preanalytical variability or CVp), (ii) the technique of measurement (analytical variability or CVa), and (iii) the patient (intra-individual variability or CVi). Analytical variation (CVa) is evaluated by the inter-assay coefficient of variation of the technique used to measure SAA. Intra-individual variation (CVi) is evaluated by the coefficient of intra-individual variation in a control population of healthy people. The Z-score depends on the probability selected for the statistical significance (Z = 1.96 for p < 0.05), and n corresponds to the number of measurements. The RCV for SAA has been estimated at +/− 76 %. Therefore, an increase or decrease in SAA of at least 1.76-fold can be considered biologically relevant (Guglielminotti et al. 2012).
The index of individuality (IOI) has been introduced to take into account both within-subject biological variation and between-subject variation (Frankenstein et al. 2009). IOI is calculated as follows: \( \mathrm{I}\mathrm{O}\mathrm{I} = \sqrt{\left({\mathrm{CVa}}^2+{\mathrm{CVi}}^2\right)}/\mathrm{C}\mathrm{V}\mathrm{g} \) where CVg is the interindividual variability. An IOI <0.6 is considered to reflect strong individuality, which in turn indicates that a patient should be assessed with respect to his or her individual level. In contrast, a high IOI indicates that the patient should be assessed with respect to a population-derived reference interval. SAA has an index of individuality of 0.58, indicating that it displays a high individuality (Guglielminotti et al. 2012). This implies that stress-induced increase in SAA of an individual patient should be assessed with respect to the patient’s basal SAA.
Human Clinical Studies
The analytical properties of SAA described previously indicate that SAA varies considerably between individuals (Guglielminotti et al. 2012). The patient should therefore be assessed with respect to his or her individual SAA level rather than to a population-derived reference interval or threshold. In other words, SAA should preferably be used to assess the temporal changes in anxiety in a patient with repeated measurements rather than to identify an anxious patient with a single measurement and an arbitrary cutoff value.
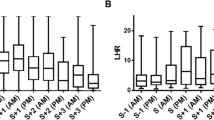
Several human studies have described the temporal changes associated with exposure to stressful stimuli. They all demonstrate that SAA increases quickly after an individual is submitted to a stressful stimulus. This increase has been observed with a wide range of stimuli such as skydiving, mental arithmetic tests, stressful video viewing, or psychosocial stress (Fig. 4) (Chatterton et al. 1996, 1997; Takai et al. 2004; Noto et al. 2005; Nater et al. 2006; Rohleder et al. 2006). SAA increase starts as early as the third minute after beginning to watch a stressful video or 5 min after a mental arithmetic task. SAA increases by 100–200 % in these situations. This increase is higher than the 75 % increase associated with the diurnal course of SAA. SAA returns to baseline after cessation of the stressful stimulus in less than 15 min. In comparison, the concentration of salivary cortisol peaks only 20 min after stress exposure. One of the important points of these results is that SAA is a very rapidly changing marker that may be usable in monitoring rapid anxiety changes during both stressful and soothing conditions (“on–off” marker).
Salivary amylase activity (SAA) and salivary cortisol concentration in response to a psychosocial stress. SAA and salivary cortisol concentration in response to the Trier Social Stress Test (TSST) and control conditions in 26 healthy men. SAA increases (and decreases) faster during (and after) stress exposure than cortisol concentration. Moreover, point-of-care measurement of SAA is possible with a handheld analyzer (Data are from Rohleder et al. with permission from the publishers (Rohleder et al. 2006))
However, temporal changes in SAA activity have been very little described during the preoperative period. Guglielminotti et al. reported a significant increase in SAA when a patient undergoing planned surgery was exposed to the stressful environment of the operating theater (Fig. 5) (Guglielminotti et al. 2012). A study by Arai et al. demonstrated a significant decrease in SAA during surgery under regional anesthesia in patients benefiting from a relaxing technique such as listening to music (Arai et al. 2008). Similarly, Shirasaki et al. demonstrated a significant decrease in SAA after pain relief with epidural analgesia (Shirasaki et al. 2007).
Salivary amylase activity (SAA) in response to a clinical stress. (a) Individual variations of SAA between two saliva collections performed 3 h apart in 18 volunteers. Intra-individual variability was 27 % and interindividual variability was 47 % leading to a reference change value of ±76 % (i.e., 1.76-fold increase or decrease) and to an index of individuality of 0.58. (b) Individual variations in 15 pregnant patients between the surgical ward and the operating theater. A 220 % median increase was observed with an increase in SAA >76 % (i.e., > the RCV) in 13 patients (Data are from Guglielminotti et al. with permission from the publishers (Guglielminotti et al. 2012))
The literature is poorer still on the relationship between preoperative SAA and intraoperative course or postoperative outcome. To the best of our knowledge, only Orbach-Zinger et al. have studied the association between a single measurement of SAA in the operating theater and an intraoperative course, i.e., arterial hypotension after spinal anesthesia (Orbach-Zinger et al. 2012). They demonstrated an association between anxiety assessed with a visual analog scale and hypotension and a weaker association between SAA and hypotension. This weak association may be explained by the use of a single measurement of SAA and not of a temporal change in SAA. An ongoing study aims to determine if salivary cortisol concentration and quantitative SAA measured upon admission to hospital and in the operating theater are associated with increased requirement for vasoactive drugs to maintain blood pressure after spinal anesthesia (ClinicalTrials.gov Identifier NCT01862055).
Potential Applications to Prognosis, Other Diseases, or Conditions
As we mentioned earlier, anxiety is triggered when planning surgery and reaches a peak at the time of admission to hospital or arrival in the operating theater (Johnston 1980). The preoperative identification of anxious patients based on SAA and its association with adverse intraoperative course and postoperative outcomes should therefore rely on repeated measurements, from the time of preanesthetic consultation to admission to the hospital or to the operating theater. This type of study has not been conducted yet. Moreover, a more comprehensive and evidence-supported description of the effects of preoperative anxiety on patient’s intraoperative course and postoperative outcome is warranted. The identification of highly anxious patients during the preoperative period should help target interventions to these patients. The unselected choices of end points in clinical trials and the preoperative administration of pharmacologic intervention such as benzodiazepines to unselected patients probably explain why the pharmacologic modulation of acute preoperative stress has, up to now, failed to improve outcome (Kain et al. 2000, 2001).
Although repeated measurements are preferable to a single measurement, one recent study suggests that a single SAA measurement could be an independent predictor of malignant ventricular arrhythmias after myocardial infarction (Shen et al. 2011). However, the small number of events observed (9) means that caution should be exercised in drawing conclusions. The second study by the same team also suggests that SAA could be an accurate diagnostic test for acute myocardial infarction in patients with acute chest pain (Shen et al. 2012). Once again, the small number of events (85 myocardial infarctions) calls for caution and underlines the need for larger-scale studies.
Another possible application of SA is the diagnosis of aspiration pneumonia. Aspiration refers to the deposition of oropharyngeal material containing SA or gastric material into the trachea and lower respiratory tract. A retrospective study by Weiss et al. suggests that the measurement of SAA in bronchoalveolar lavage may be a screening tool to identify patients with suspected aspiration (Weiss et al. 2013).
Summary Points
-
Preoperative anxiety is an unpleasant state resulting from the anticipation of a threatening situation. It contributes to acute preoperative stress.
-
Up to 40 % of patients experience anxiety before surgery. It is associated with adverse intraoperative course and postoperative outcomes.
-
Assessment of preoperative anxiety is challenging and mainly based on lengthy questionnaires or biomarkers that cannot be used for bedside decision-making.
-
There is a potential role for noninvasive, real-time, and point-of-care biomarkers such as salivary amylase (SA) to identify anxious patients and to target pharmacologic or non-pharmacologic interventions to these patients.
-
SA is the principal protein of saliva and is mainly secreted by the parotid glands. The autonomic nervous system plays a major role in the secretion of SA.
-
SA is measured using its enzymatic activity (SAA). A specific point-of-care analyzer of SAA has been described.
-
There is an association between changes in SAA and changes in blood norepinephrine, heart rate variability indices, and anxiety during exposure to stressful stimuli.
-
Saliva can be collected by different methods. SAA varies depending on the collection method, which needs to be standardized.
-
SAA increases quickly (i.e., less than 5 min) after exposure to an acute stressor and returns rapidly (i.e., less than 15 min) to baseline during soothing conditions (“on–off” marker). The high amplitude of the variation of SAA between basal and stress conditions makes SAA a highly sensitive marker of acute stress exposure.
-
Several factors (time of day, smoking, food, alcohol or caffeine intake, intense physical exercise, drugs, and comorbidities) influence SAA. However, saliva flow rate, age, and sex have little influence on SAA during exposure to a stressful stimulus.
-
Its very high within- and interindividual variations imply that SAA should be measured for each patient before and during exposure to a stressful stimulus. A twofold increase in SAA during exposure to a stressful stimulus can be considered biologically relevant.
-
Several human studies demonstrate an increase in SAA after exposure to acute stressful stimuli including arrival at the operating theater.
-
The literature is still scarce on the association between preoperative SAA and intraoperative course or postoperative outcome. It remains a stimulating area of research.
Abbreviations
- IOI:
-
Index of Individuality
- RCV:
-
Reference Change Value
- SA:
-
Salivary Amylase
- SAA:
-
Salivary Amylase Activity
References
Arai YC, Sakakibara S, et al. Intra-operative natural sound decreases salivary amylase activity of patients undergoing inguinal hernia repair under epidural anesthesia. Acta Anaesthesiol Scand. 2008;52(7):987–90.
Arhakis A, Karagiannis V, et al. Salivary alpha-amylase activity and salivary flow rate in young adults. Open Dent J. 2013;7:7–15.
Beltzer EK, Fortunato CK, et al. Salivary flow and alpha-amylase: collection technique, duration, and oral fluid type. Physiol Behav. 2010;101(2):289–96.
Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69(3):89–95.
Bosch JA, Veerman EC, et al. Alpha-amylase as a reliable and convenient measure of sympathetic activity: don’t start salivating just yet! Psychoneuroendocrinology. 2011;36(4):449–53.
Broadbent E, Petrie KJ, et al. Psychological stress impairs early wound repair following surgery. Psychosom Med. 2003;65(5):865–9.
Chatterton Jr RT, Vogelsong KM, et al. Salivary alpha-amylase as a measure of endogenous adrenergic activity. Clin Physiol. 1996;16(4):433–48.
Chatterton Jr RT, Vogelsong KM, et al. Hormonal responses to psychological stress in men preparing for skydiving. J Clin Endocrinol Metab. 1997;82(8):2503–9.
Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5(7):374–81.
de Almeida Pdel V, Gregio AM, et al. Saliva composition and functions: a comprehensive review. J Contemp Dent Pract. 2008;9(3):72–80.
DeCaro JA. Methodological considerations in the use of salivary alpha-amylase as a stress marker in field research. Am J Hum Biol. 2008;20(5):617–9.
Frankenstein L, Remppis A, et al. Variability of N-terminal probrain natriuretic peptide in stable chronic heart failure and its relation to changes in clinical variables. Clin Chem. 2009;55(5):923–9.
Fujiwara Y, Ito H, et al. Preoperative ultra short-term entropy predicts arterial blood pressure fluctuation during the induction of anesthesia. Anesth Analg. 2007;104(4):853–6.
Goldstein DS. Stress, catecholamines, and cardiovascular disease. New York: Oxford University Press; 1995.
Granger DA, Kivlighan KT, et al. Salivary alpha-amylase in biobehavioral research: recent developments and applications. Ann N Y Acad Sci. 2007;1098:122–44.
Gras S, Servin F, et al. The effect of preoperative heart rate and anxiety on the propofol dose required for loss of consciousness. Anesth Analg. 2010;110(1):89–93.
Guglielminotti J, Dehoux M, et al. Assessment of salivary amylase as a stress biomarker in pregnant patients. Int J Obstet Anesth. 2012;21(1):35–9.
Harmon AG, Towe-Goodman NR, et al. Differences in saliva collection location and disparities in baseline and diurnal rhythms of alpha-amylase: a preliminary note of caution. Horm Behav. 2008;54(5):592–6.
Humphrey SP, Williamson RT. A review of saliva: normal composition, flow, and function. J Prosthet Dent. 2001;85(2):162–9.
Jamison RN, Taft K, et al. Psychosocial and pharmacologic predictors of satisfaction with intravenous patient-controlled analgesia. Anesth Analg. 1993;77(1):121–5.
Johnston M. Anxiety in surgical patients. Psychol Med. 1980;10(1):145–52.
Kain ZN, Wang SM, et al. Distress during the induction of anesthesia and postoperative behavioral outcomes. Anesth Analg. 1999;88(5):1042–7.
Kain ZN, Sevarino F, et al. Attenuation of the preoperative stress response with midazolam: effects on postoperative outcomes. Anesthesiology. 2000;93(1):141–7.
Kain ZN, Sevarino FB, et al. Preoperative anxiolysis and postoperative recovery in women undergoing abdominal hysterectomy. Anesthesiology. 2001;94(3):415–22.
Kaufman E, Lamster IB. The diagnostic applications of saliva–a review. Crit Rev Oral Biol Med. 2002;13(2):197–212.
Kil HK, Kim WO, et al. Preoperative anxiety and pain sensitivity are independent predictors of propofol and sevoflurane requirements in general anaesthesia. Br J Anaesth. 2012;108(1):119–25.
Kindler CH, Harms C, et al. The visual analog scale allows effective measurement of preoperative anxiety and detection of patients’ anesthetic concerns. Anesth Analg. 2000;90(3):706–12.
Levandovski R, Ferreira MB, et al. Impact of preoperative anxiolytic on surgical site infection in patients undergoing abdominal hysterectomy. Am J Infect Control. 2008;36(10):718–26.
Liu R, Barry JE, et al. Effects of background stress and anxiety on postoperative recovery. Anaesthesia. 1994;49(5):382–6.
Lunn TH, Gaarn-Larsen L, et al. Prediction of postoperative pain by preoperative pain response to heat stimulation in total knee arthroplasty. Pain. 2013;154(9):1878–85.
Masselin-Dubois A, Attal N, et al. Are psychological predictors of chronic postsurgical pain dependent on the surgical model? A comparison of total knee arthroplasty and breast surgery for cancer. J Pain. 2013;14(8):854–64.
McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–9.
Miu AC, Heilman RM, et al. Reduced heart rate variability and vagal tone in anxiety: trait versus state, and the effects of autogenic training. Auton Neurosci Basic Clin. 2009;145(1–2):99–103.
Moerman N, van Dam FS, et al. The Amsterdam Preoperative Anxiety and Information Scale (APAIS). Anesth Analg. 1996;82(3):445–51.
Nater UM, Rohleder N. Salivary alpha-amylase as a non-invasive biomarker for the sympathetic nervous system: current state of research. Psychoneuroendocrinology. 2009;34(4):486–96.
Nater UM, La Marca R, et al. Stress-induced changes in human salivary alpha-amylase activity: associations with adrenergic activity. Psychoneuroendocrinology. 2006;31(1):49–58.
Nater UM, Rohleder N, et al. Determinants of the diurnal course of salivary alpha-amylase. Psychoneuroendocrinology. 2007;32(4):392–401.
Navazesh M. Methods for collecting saliva. Ann N Y Acad Sci. 1993;694:72–7.
Noto Y, Sato T, et al. The relationship between salivary biomarkers and state-trait anxiety inventory score under mental arithmetic stress: a pilot study. Anesth Analg. 2005;101(6):1873–6.
Obayashi K. Salivary mental stress proteins. Clin Chim Acta Int J Clin Chem. 2013;425:196–201.
Omar F, van der Watt GF, et al. Reference change values: how useful are they? J Clin Pathol. 2008;61(4):426–7.
Orbach-Zinger S, Ginosar Y, et al. Influence of preoperative anxiety on hypotension after spinal anaesthesia in women undergoing Caesarean delivery. Br J Anaesth. 2012;109(6):943–9.
Out D, Bakermans-Kranenburg MJ, et al. State and trait variance in salivary alpha-amylase: a behavioral genetic study. Biol Psychol. 2011;88(1):147–54.
Out D, Granger DA, et al. Disentangling sources of individual differences in diurnal salivary alpha-amylase: reliability, stability and sensitivity to context. Psychoneuroendocrinology. 2013;38(3):367–75.
Piccirillo G, Elvira S, et al. Abnormal passive head-up tilt test in subjects with symptoms of anxiety power spectral analysis study of heart rate and blood pressure. Int J Cardiol. 1997;60(2):121–31.
Rohleder N, Nater UM. Determinants of salivary alpha-amylase in humans and methodological considerations. Psychoneuroendocrinology. 2009;34(4):469–85.
Rohleder N, Wolf JM, et al. The psychosocial stress-induced increase in salivary alpha-amylase is independent of saliva flow rate. Psychophysiology. 2006;43(6):645–52.
Santos JL, Saus E, et al. Copy number polymorphism of the salivary amylase gene: implications in human nutrition research. J Nutrigenet Nutrigenomics. 2012;5(3):117–31.
Schenkels LC, Veerman EC, et al. Biochemical composition of human saliva in relation to other mucosal fluids. Crit Rev Oral Biol Med. 1995;6(2):161–75.
Shen YS, Chan CM, et al. Initial salivary alpha-amylase activity predicts malignant ventricular arrhythmias and short-term prognosis after ST-segment elevation myocardial infarction. Emerg Med J. 2011;28(12):1041–5.
Shen YS, Chen WL, et al. Diagnostic performance of initial salivary alpha-amylase activity for acute myocardial infarction in patients with acute chest pain. J Emerg Med. 2012;43(4):553–60.
Shirasaki S, Fujii H, et al. Correlation between salivary alpha-amylase activity and pain scale in patients with chronic pain. Reg Anesth Pain Med. 2007;32(2):120–3.
Shirtcliff EA, Granger DA, et al. Use of salivary biomarkers in biobehavioral research: cotton-based sample collection methods can interfere with salivary immunoassay results. Psychoneuroendocrinology. 2001;26(2):165–73.
Soeda R, Tasaka A, et al. Influence of chewing force on salivary stress markers as indicator of mental stress. J Oral Rehabil. 2012;39(4):261–9.
Spielberger CD, Gorsuch RL, et al. Manual for the State-Trait Anxiety Inventory (STAI) Form Y. Palo Alto: Consulting Psychologists Press; 1983.
Takai N, Yamaguchi M, et al. Effect of psychological stress on the salivary cortisol and amylase levels in healthy young adults. Arch Oral Biol. 2004;49(12):963–8.
Theunissen M, Peters ML, et al. Preoperative anxiety and catastrophizing: a systematic review and meta-analysis of the association with chronic postsurgical pain. Clin J Pain. 2012;28(9):819–41.
Thoma MV, Kirschbaum C, et al. Acute stress responses in salivary alpha-amylase predict increases of plasma norepinephrine. Biol Psychol. 2012;91(3):342–8.
Tully PJ, Szekely A. Anxiety and depression as predictors of cardiovascular outcomes after cardiac surgery. Am J Cardiol. 2013;111(7):1079.
Tully PJ, Baker RA, et al. The role of depression and anxiety symptoms in hospital readmissions after cardiac surgery. J Behav Med. 2008;31(4):281–90.
Tully PJ, Bennetts JS, et al. Anxiety, depression, and stress as risk factors for atrial fibrillation after cardiac surgery. Heart Lung. 2011;40(1):4–11.
Wattier JM, Barreau O, et al. Measure of preoperative anxiety and need for information with six issues. Ann Fr Anesth Reanim. 2011;30(7–8):533–7.
Weiser TG, Regenbogen SE, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372(9633):139–44.
Weiss CH, Moazed F, et al. Bronchoalveolar lavage amylase is associated with risk factors for aspiration and predicts bacterial pneumonia. Crit Care Med. 2013;41(3):765–73.
Yamaguchi M, Kanemori T, et al. Performance evaluation of salivary amylase activity monitor. Biosens Bioelectron. 2004;20(3):491–7.
Yamaguchi M, Deguchi M, et al. Hand-held monitor of sympathetic nervous system using salivary amylase activity and its validation by driver fatigue assessment. Biosens Bioelectron. 2006;21(7):1007–14.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media Dordrecht
About this entry
Cite this entry
Robert-Mercier, T., Dehoux, M., Longrois, D., Guglielminotti, J. (2015). Salivary Amylase as a Preoperative Marker of Anxiety in Perioperative Medicine. In: Preedy, V., Patel, V. (eds) General Methods in Biomarker Research and their Applications. Biomarkers in Disease: Methods, Discoveries and Applications. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-7696-8_31
Download citation
DOI: https://doi.org/10.1007/978-94-007-7696-8_31
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-7695-1
Online ISBN: 978-94-007-7696-8
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences