Abstract
Cirrhotic patients may present body asymmetry and presence of ascites and edema, and the assessment of nutritional status is limited and fails when using the methods of anthropometric assessment. In addition, scores currently used, Model for End-Stage Liver Disease (MELD) and Child–Turcotte–Pugh, have limitations as to predict the prognosis of these patients. In this sense, as a complementary evaluation for liver disease, the analysis of the phase angle (PA) by bioelectrical impedance analysis (BIA) could be a new biological method to be used.
The BIA is a noninvasive method for evaluation of body composition, easy to perform, and fast, reproducible, and economical and can be performed in outpatient or inpatient. It tells us the nutritional status of patients by estimating the amount of lean body mass, fat mass, body water, and cell mass. The method also allows the assessment of patient’s prognosis through the PA, which has been applied in patients with various diseases, including chronic liver disease. The phase angle varies according to the population and, in our environment, if we adopt the value of 5.4° as the cutoff point; values above represent a good prognosis and below this a poor prognosis.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
Key Facts of Child
-
The Child score was originally proposed to evaluate the risk of cirrhotic patient subjected to portacaval anastomosis or esophageal transection.
-
This prognostic model was developed by Child and Turcotte in 1964, but in the 1970s Pugh made a change in the score, replacing the variable “nutritional status” with “prothrombin time,” thus creating the score we know today by Child or Child–Turcotte–Pugh score.
-
The Child score is currently used to determine the prognosis, the response to treatment, and the need for liver transplantation.
-
The Child–Pugh score includes three continuous variables (prothrombin time, bilirubin, and albumin) and two quantitative (ascites and hepatic encephalopathy). They are awarded points 1–3 according to the classification of each of the variables. The score is the sum of these points, ranging from 5 to 15, and the higher the score, the worse the prognosis.
In general, patients with a score of 5 and 6 are classified as A, between 7 and 9 as B, and 10–15 as C.
-
Regarding the MELD score, the Child score has the disadvantage of relying on subjective clinical severity variables (ascites and encephalopathy), which can hamper the classification of the patient.
Definitions of Words and Terms
- Bioimpedance electrical:
-
It is the device which indirectly measures the body composition of individuals by passing an electric current, which measures fat-free mass, fat mass, body cell mass, total body water, intracellular water, and extracellular water. In addition, the bioelectrical impedance provides the phase angle.
- Phase angle:
-
It evaluates the integrity, functionality, and cell membrane permeability. It is calculated by the resistance and reactance and provides information about the patient’s prognosis.
- Resistance:
-
It is the opposition offered by the body to the passage of electric current and inversely related to water and electrolytes contained in body tissues.
- Reactance:
-
It is the capacitance (viability) of the properties of the cell membrane and may vary as a result of their integrity, function, and composition.
- Multi-body model compartmentalization:
-
It is an indirect method of assessing body composition, based on the quantification of fat mass, fat-free mass, minerals, water, tissue, blood, cell, and bone mass. Obtaining these data will depend on the model to be used.
- Body asymmetry:
-
It is the absence of proportionality of the body parts in a sagittal plane, such as the human body. It can be caused by fluid retention (ascites, edema) often present in patients with liver disease.
- Prognostic marker:
-
It is an indicator of the evolution of the patient’s disease. It may be composed of complications from the disease.
- Child–Turcotte–Pugh:
-
It is a staging system and clinical classification of cirrhotic patients. It is considered the value of serum bilirubin, serum albumin, and prothrombin time; the presence of ascites; and the development of hepatic encephalopathy.
- MELD score:
-
It is a system currently used to allocate patients enlisted for liver transplant, which uses three laboratory parameters, and they are serum bilirubin, creatinine, and international normalized ratio (INR).
- Protein calorie malnutrition:
-
It is the consequence of insufficient intake of energy and protein. In liver disease patients, their presence is related to complications of the disease (fluid retention, hepatic encephalopathy) and symptoms (dysgeusia, lack of appetite, early satiety, abnormal bowel movements, nausea and/or vomiting).
Introduction
Patients with liver disease have a poor prognosis by the natural course of the disease and clinical complications arising from it along time (Parise et al. 2010).
Current methods for assessment and clinical staging of chronic liver disease are complex, objective, and/or subjective, such as the MELD score (the Model for End-Stage Liver Disease) and Child–Turcotte–Pugh, with reasonable reliability (Durand and Valla 2005; Huo et al. 2005). However, these methods do not contemplate or quantify important variables such as ascites, jaundice, encephalopathy, and disease severity (Botta et al. 2003). At the same time, patients should be evaluated sequentially, at different times, with clinical and/or laboratory tests, in order to establish the dynamic staging and prognosis. Thus, these methods are not fast, accurate, or instantaneous procedures, to respond faithfully to the actual state of the patient.
Chronic liver disease patients show numerous pathophysiological changes that compromise various organs and systems, as well as metabolic disorders, dysgeusia, severe depletion of skeletal muscles, and changes in hydration status (Fernandes et al. 2012). A constant feature, in variable order, is the nutritional deficits of macro- and micronutrients, varying levels during the evolution of time, and disease staging, considering that these patients are malnourished per se, by the catabolic disease condition, and also have to follow a restrictive diet which further compromises the malnutrition framework (Müller et al. 1999; Matos et al. 2002).
Nutritional assessment of chronic liver disease by objective (anthropometry, body composition assessment, biochemical parameters, and evaluation of food consumption) and subjective (physical examination and the overall subjective assessment) methods is all partial, incomplete, discrepant, and not comparable, so it ends up being classified as unsuitable for the chronic liver disease patient (Fernandes et al. 2012; Ritter and Gazzola 2006; Gottschall et al. 2004; Donaghy 2002). There is not a standardized method considered gold standard for nutritional evaluation of chronic liver disease until now (Fernandes et al. 2012). Several nutritional assessment methods are often used together so that we can get an idea of the nutritional status of the patient resulting in clinical management and allowing directly intervention and improved nutritional status.
Among the methods used to assess the individual’s nutritional status, the assessment by bioelectrical impedance analysis (BIA) was shown to be an accurate method to determine the components of body composition and proportions (fat mass, lean mass, body water, basal metabolic rate) and to establish the nutritional status of patients that exhibit no change in body symmetry. This compartmentalized evaluation of the body through the BIA (fat mass and fat-free mass) can provide, quantitatively, the actual nutritional status of the patient assessed.
On the other hand, chronic liver disease patients may show a change in body composition that affects the evaluation by BIA (Fig. 1), because as we will see later in more details, BIA assumes that the human body is a cylinder and that the cross-sectional areas represent the tissues of the organs analyzed by the passage of an electric current. Therefore, if the patient is overhydrated, the body lean mass is overestimated by modifying the result of the body evaluation (Kyle et al. 2004; Bera 2014). This is the greatest limitation of this method in chronic liver disease.
In the 1980s, it was found that BIA could assess the cellularity of living beings, through an observation of parameters obtained during the examination, placed in a special formula, and this does not depend on the body asymmetry observed in cirrhotic patients with edema and ascites. The result of this observation, calculated numerically, was called phase angle (PA) (Baumgartner et al. 1988).
Bioelectrical Impedance Analysis (BIA)
Bioelectrical impedance analysis is a noninvasive, inexpensive, and portable method that has been used mainly for body composition analysis (Barbosa-Silva et al. 2005). BIA is a safe technique and hazard-free that measures fat-free mass, fat mass, body cell mass, total body water, intracellular water, and extracellular water with an excellent consistency for repeated measurements (Bera 2014).
Different methods seek to evaluate body composition (Fig. 2). The classic model of two components of the body composition (2-C) divides the body into two parts, one of which consists of body fat and all the remaining tissues are collected and termed as fat-free mass (FFM).
Multi-body model compartmentalization. The figure above describes the basic two-compartment model that evaluates the fat mass and lean mass body composition. Atomic compartment model evaluates the body by dividing it into four compartments: compartment of minerals, compartment of carbon, compartment of hydrogen, and compartment of oxygen. The molecular model, in turn, evaluates the body according to the mineral content, protein, lipid, and water. The mobile model evaluates the contents of fat, extracellular fluid, extracellular solids, and cell mass. The functional model measures, in turn, the content of skeletal muscle, blood, bones, fat, and others. EF extracellular fluid, ES extracellular solids (Adapted from Ellis 2000)
Another model, the three components of the body composition (3-C), not only identifies the fat-free mass but also divides into two parts, liquid content (water) and remaining solids (predominantly proteins and minerals) (Cezar 2000).
More detailed than the previous models, the 4-component model, the cellular model, subdivides the fat-free mass into three basic or physiological compartments: body cell mass (BCM), water or extracellular fluid (ECF), and extracellular solids (ECS). So the fat-free mass (FFM) is defined as BCM + ECF + ECS and total fat mass as FFM – body weight (mass) (Cezar 2000).
Through the BIA method, it is possible to assess the body composition of all the proposed models. The BIA is an evaluation through which there is a passage of painless electric current through the organism, with low amplitude and low and high frequencies, applied by means of cables that are connected to electrodes or to conductive surfaces, which are placed in contact with the skin (Lukaski et al. 1985). The patient remains in dorsal decubitus position, with legs and hands placed parallel on the body. One electrode is placed on the dorsal hand, at the middle-finger level, and one in the wrist joint, both on the right side. Another pair of electrodes is placed on the dorsal foot, at the middle-toe level, and in the ankle joint, also on the right side (Fig. 3).
Bioelectrical impedance analysis in cirrhotic patient. Cirrhotic patient being evaluated in outpatient care through bioelectrical impedance method. As we can see, the electrodes are placed on the hand and foot. The passage of an electric current through the organism can estimate the body composition and phase angle (Source: author, Fernandes S.)
The electric current passes through the body at a differential rate depending on body composition (Fig. 4) (Dehghan and Merchant 2008). The compartment known as fat-free mass consists of all that is not body fat and involves the following components: bone mineral content (≈7%), extracellular water (≈29%), intracellular water (≈44%), and visceral protein. Total body water (TBW) is a compartment which can be divided into extracellular water (ECW) and intracellular water (ICW). In turn, body cell mass (BCM) is the protein-rich compartment that is affected in catabolic states, and the loss of BCM is associated with unsatisfactory clinical results. Finally, the fat mass (FM) consists of total body fat, and it is obtained by subtracting fat-free mass (FFM) from total body weight (Mialich et al. 2014).
Division of body compartments assessed by bioelectrical impedance. Among body compartments that can be evaluated using the bioelectrical impedance method is a fat-free mass, which is based on quantification of visceral protein, intracellular water, extracellular water, and bone mass, whereas fat mass corresponds to the subtraction of the fat-free mass of total body weight. The intracellular and extracellular water compartments provide the data of total body water and intracellular water, while the protein associated with visceral refers to the data of body cell mass (Source: Kyle et al. 2004)
Considering the different composition of the body’s compartments, the flow of electric current occurs differently in the muscle tissue compared to the fat, bone, and skin, and by this principle, it becomes possible to evaluate the resistance (R) and reactance (Xc) from the passage of electrical current. The muscle tissue contains a large amount of water and electrolyte and exhibits high conductivity and low electrical current strength. On the other hand, the fat, skin, and bones have low conductivity and high strength by containing small amount of fluid and electrolytes. Therefore, it identifies the resistance (R) and reactance (Xc), and it is possible to calculate the impedance (Z) and the phase angle (φ) (Lukaski et al. 1985). The phase angle between direct measurements that are provided by evaluating BIA shows itself as a prognostic indicator and mortality rates in several diseases, and its application in liver diseases is discussed later in this chapter.
Obtaining specific body compartment information depends on the type of electrical bioimpedance device used. Analysis of bioimpedance information obtained at 50 KHz electric current is known as single-frequency bioimpedance analysis (SF-BIA), which is the most used. In this case, the electrodes are placed on the hand and foot. SF-BIA allows estimating fat-free mass and total body water, but cannot determine differences in intracellular water (Kyle et al. 2004). Since it has a single frequency, this instrument may mask the interpretation of the data in tests in which the subject has altered body composition in some compartment. Thus, its use is not recommended in a situation of altered hydration (Mialich et al. 2014). Despite its limitations, the SF-BIA provides the phase angle (PA), which is related to the prognosis of cirrhotic patients (Fernandes et al. 2013).
Analysis of bioimpedance that is obtained at more than two frequencies is known as multiple-frequency bioimpedance analysis (MF-BIA) (Khalil et al. 2014). This method has more resources for assessment such as the determination of intracellular water since it involves currents with frequencies ranging from 5 to 100 kHz. Another resource of this instrument is its use as a marker of cell integrity, mentioned as a prognostic factor (Mialich et al. 2014).
Prior to completion of the bioelectrical impedance, the patient’s preparation is important for the obtained result to be reliable. Among factors that can influence body composition stands out the consumption of drinks and food. Although food or fluid intake before BIA measurement affects total body water and extracellular water, a general agreement on the ideal amount of time between food and fluid intake and BIA measurements has yet to be consolidated. For this reason undertaking an overnight fasting is recommended as a routine standardization technique before impedance measurements (Dehghan and Merchant 2008).
The practice of exercise before taking a test may also influence body composition analysis. Although exercise of mild intensity may not affect BIA measurements, moderate and intensive exercise before measurements may change the measured impedance by different mechanisms (Garby et al. 1990). Therefore, in order to minimize the risk of error in the assessment by BIA, moderate to intense physical exercise between 2 and 3 h prior to testing is not recommended.
Furthermore, it is noted that the body asymmetry should be considered for evaluation of patients by bioelectrical impedance. It is understood by physical asymmetry in the absence of proportionality of the body parts in a sagittal plane, such as the human body. Thus, patients with ascites and edema, morbidly obese patients, pregnant women, and amputees will present change of body fluids. It should be noted that even if the patient is asymmetrical, there is no change in phase angle in these cases, which will be addressed ahead.
Phase Angle
The use of the BIA has shown efficiency in the measurement of body compartments in various clinical situations such as malnutrition, trauma, pre- and postoperative, compensated liver disease , renal dialysis, and cancer (Kyle et al. 2004).
Changes in body shape may influence the results of the examination. In these situations, the use of BIA may be more advisable to obtain better results. Recalling that BIA is based on the body symmetry theory, where the level of hydration and percentage body fat are constant, when faced with different situations, such as age, ethnicity, body shape, or various clinical conditions, this method does not have “universal equations,” used in all situations, requiring another reference point as a parameter (Barbosa-Silva and Barros 2005a; Barbosa-Silva et al. 2003).
Given these differences, the clinically established bioelectrical impedance parameter is the phase angle (PA). The phase angle is calculated by the formula that considers the resistance (R) and reactance (Xc) (Fig. 5).
Phase angle. PA = arctangent (Xc/ R ) x 180. Formula and geometric distribution of the formation of PA and its relationship with resistance, reactance, impedance, and frequency of the applied current (Source: Kyle et al. 2004)
The PA gained popularity in recent years, because it shows to be highly predictive of clinical outcome in a variety of diseases. Recent studies report that the PA values correlate well with clinical outcome parameters of the studied disease (Kyle et al. 2004). There are numerous diseases evaluated by PA, such as cancer, HIV, lung disease, heart disease, and others.
The phase angle is a fast method, is applicable in the clinic, and reflects the vitality and cell integrity, where higher values indicate cellular activity preserved (Máttar 1996; Norman et al. 2012). In healthy subjects, the PA can vary between 6° and 7° (Bosy-Wesrphal et al. 2006). Different cutoff values are used based on reference values for age and gender. Standardized PA (SPA) values exist for the Swiss, German, American, and Brazilian populations. The SPA can be used to compare results among different populations and to correlate an SPA with a particular disease, as reported by Barbosa-Silva et al. (2008), in the Brazilian population. The results of this study allow us to use the SPA values as parameters for other several diseases.
Phase Angle and Chronic Liver Disease
It is noted that the preserved function of the cells is closely linked to the nutritional status of cirrhotic individual, and it became an independent marker of mortality.
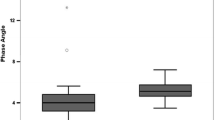
Selberg and Selberg (2002), in a prospective study of 305 patients with cirrhosis, correlated the PA with muscle mass, muscle strength, and survival rates. They observed that patients with a PA equal or lower than 5.4° showed lower survival rates than those with PA values above 6.6°. Variables such as total body potassium, anthropometric measurements, and BIA were evaluated separately; however, only the PA proved to be an isolated predictor of survival.
In a retrospective study, Pirlich et al. (2000) analyzed 41 cirrhotic patients (20 with ascites and 21 without) through BIA, considered as the reference method. The study shows that the PA is a tool able to detect body cellular mass and identify its decrease in cirrhotic patients. The PA offers reliable PCM estimates even when used in patients with large amount of ascites, proving to be superior to commonly used techniques, showing that the PA becomes an important prognostic marker.
A cohort that assessed 66 cirrhotic patients stratified by their clinical condition through the Child–Pugh score, followed up for a 17-month period, established PA for this population in 5.18°. Patients with values below this angle were considered to have poor prognosis and shorter survival rates. It is worth highlighting that as the patient’s clinical situation worsened, the PA decreased, showing a prognostic value (Peres et al. 2012).
Corroborating with these findings, we assessed the nutritional status of 129 cirrhotic patients through different methods and demonstrated that the only method able to correlate malnutrition with the liver disease’s staging, evaluated through the Child–Turcotte–Pugh classification, is PA. We set the PA cutoff point as 5.4°, same as Selberg and Selberg (2002), in which patients with values below this discriminatory level showed a worse prognosis. We should point out the discrepancies between the results of different evaluation methods (anthropometry, hand grip strength (HGS), and BIA), used to diagnose PCM, once the diagnosis for malnutrition may vary from 5.4% to 69.3% in the same population, depending on the assessment method employed (Fernandes et al. 2012). PA analysis demonstrated sensitivity and specificity when compared to BIA and HGS, with values of 68.9–70.0% and 49.2–56%, respectively (Fernandes et al. 2012).
Later, another study performed in our center evaluated 195 cirrhotic patients, reinforcing the idea that the PA is a good prognostic marker when compared to other methods, as it is the only one correlated with the real clinical condition of the patient (Fernandes et al. 2013).
Recently, Ruiz Margain et al. (2015) assessed 249 compensated cirrhotic patients in a prospective cohort study with a 48-month follow-up period. The PA cutoff point for malnutrition was lower or equal to 4.9°, the cutoff based in a pilot study. This study also concluded that PA is a good prognostic marker, associating PCM with mortality rate.
A cohort study conducted in our center evaluated 32 cirrhotic patients enlisted for liver transplant (Aydos et al. 2016). The patients were evaluated on the moment before the transplant and 1, 6, and 12 months after surgery. The assessment of nutritional status was performed applying diagnostic procedures in sequence: anthropometry, non-dominant hand grip strength, abductor pollicis muscle (APMT), and PA. Methods that better demonstrated the real prevalence of malnourished patients before transplantation were PA (25%), arm muscle circumference (AMC) (21.9%), and arm circumference (AC) (18.8%). The percentage of malnourished patients was significantly higher after 1 month of transplantation when compared to the percentage in 6 months and 1 year after transplantation. Among these methods, the one that followed the disease’s staging was PA, because as the patient improved, PA accompanied this increase. It was suggested that the PA could be widely used with this population since the results are consistent, reliable, and reproducible.
Wagner et al. (2011) evaluated nutritional methods that informed the nutritional status of 71 posttransplantation patients. Patients were divided into three groups according to the time since their transplantation: 5 years, between 5 and 10 years, and over 10 years. They used the PA cutoff point as below 5° in order to diagnose malnutrition. The PCM diagnosis was made in 81.2%, 31.6%, and 31.7% in each group, respectively (p = 0.008). In this study, PA showed a higher prevalence of malnutrition among the population of patients in the first years after liver transplantation.
Recently, Ruiz-Margáin et al. (2016) analyzed the clinical and nutritional status of 79 consecutive cirrhotic patients, prospectively, on intensive care unit. Sequentially, clinical, laboratory, and nutritional assessments (with BIA phase angle and measure of arm muscle circumference) were made to determine its evolution and prognosis . Evaluations were daily until discharge or death. All patients who died were malnourished. The PA decreased in patients with major complications, in the most severe ones, and in those who died. The decrease in PA in the first 24 h was associated with higher mortality. The PA has been shown as an early biomarker for prognosis that would make it useful as part of an initial full real-time assessment of these patients.
Analyzing patients with chronic hepatitis by the hepatitis C virus (HCV) with advanced fibrosis, PA/BIA was shown to be a predictor of the development of fibrosis, since for each degree of reduction of PA, there is a fourfold increase in the risk of fibrosis (de Souza et al. 2016). In patients with chronic C virus hepatitis in antiviral treatment, the reduction of PA/BIA joined to the increase of the adverse effects of this therapy (Kahraman et al. 2010).
The BIA is feasible in any living being and the PA calculation as well. Therefore, we use it in our research group, BIA and PA in rats with cirrhosis induced by carbon tetrachloride (CCl4), and observed that the values of PA decreased with the worsening of animals for disease progression (Fig. 6). Under that circumstance the cell membranes are compromised by lipoperoxidation and were confirmed by TBARS technique. In similar experiments using the model of cirrhosis diethylnitrosamine (DEN), we obtained the same results with reduced PA and its recovery, with improvement of animals by the use of antioxidants such as melatonin (Bona et al. 2012). In secondary biliary cirrhosis produced in rats by ligation of common bile duct, melatonin improved morphological and nutritional parameters, and the phase angle of the bioelectrical impedance has increased along with these improvements (Marroni et al. 2016).
The electrical conductivity in biological tissues is virtually ionic, meaning that the electrical charges were transferred to the ionization salts. Thus, the organic conductivity is directly proportional to the volume of body fluid.
Additionally, muscle strength and phase angle correlate, which is suggestive of a lower phase angle being associated with decreasing functioning status.
Several markers have been associated with sarcopenia in the elderly, including bioelectrical indexes. Phase angle (PA) is an impedance parameter and has been suggested as an indicator of cellular death. Thus, the relationship between PA, muscle mass, and strength was investigated in 207 elderly participants (mean age 76.2 ± 6.7years) admitted for multidimensional geriatric evaluation. Muscle strength by grip strength using a handheld dynamometer and muscle mass were measured by bioimpedentiometer. PA was calculated directly with its arctangent (resistance/reactance × 180°/π). Linear relationship among muscular mass and strength and with clinical and biochemical parameters, including PA at uni- and multivariate analyses, was performed. Linear regression analysis demonstrated that lower level of PA is associated with reduction in grip strength (y = 3.16 + 0.08x; r = 0.49; p < 0.001) and even more with muscle mass (y = 3.04 + 0.25x; r = 0.60; p < 0001). Multivariate analysis confirms these relationships (grip strength β = 0.245, p = 0.031; muscular mass β = 0.623, p < 0.01). Thus, PA is inversely related to muscle mass and strength in elderly subjects, and it may be considered a good bioelectrical marker to identify elderly patients at risk of sarcopenia (Basile et al. 2014).
Phase angle is an objective bedside nutritional marker reflecting the integrity of cellular membranes and tissue homeostasis, translating into nutritional status and suitable for daily assessment in cirrhotic patients ; thus, it could be a useful tool in the hospitalized population.
The PA has become an important prognostic marker in various clinical conditions in which integrity of cell membrane is compromised and there is a change in the balance of fluids (Kahraman et al. 2010). Studies suggest that PA is an important tool to evaluate the clinical outcome or disease progression . (Llames et al. 2013).
Potential Application of the Method for Other Diseases’ Prognosis and Conditions
The phase angle has been studied for application as a prognostic indicator in several other clinical conditions, such as cancer, acquired human immunodeficiency virus (HIV), and chronic obstructive pulmonary disease (COPD); surgical patients; and kidney dialysis patients.
Gupta et al. (2004a) showed that PA is a powerful predictor of survival when compared to traditional parameters of nutritional assessment , such as albumin, prealbumin, and transferrin in patients with advanced pancreatic cancer. This study identified a cutoff for PA 5.0°. In a similar study conducted in patients with advanced lung cancer, there was a lower survival rate in patients with PA ≤ 4.5° (Toso et al. 2000). The same trend was observed in the use of PA as a predictor of mortality of patients with colorectal cancer, and patients presenting PA > 5,57° had an average survival rate five times higher than those with PA below this cut point (40.4 months vs. 8.4 months) (Gupta et al. 2004b).
Regarding HIV-infected patients on highly active antiretroviral therapy (HAART), Schwenk et al. (2000) noted that PA has a strong ability to predict survival and clinical outcome, regardless of the level of immunodeficiency and viremia.
When evaluating a population composed of 225 presurgical individuals, Barbosa-Silva and Barros (2005b) found that weight loss greater than 10%, the subjective global assessment, nutritional risk assessment, extracellular mass/body cell mass, and PA were prognostic factors significantly associated with postoperative complications in the crude analysis. However, after adjusting for sex, age, marital status, tumor, and preoperative infections, only the PA remained as a prognostic factor.
Regarding heart disease, PA also appears to be a good predictor of survival (Doesch et al. 2010; G. Brenta et al. 2011) and a marker of severity of congestive heart failure (CHF) (Castillo et al. 2007). Doesch et al. (2010) investigated the association between PA and the epicardial adipose tissue (EAT) quantified by cardiac magnetic resonance (CMR) in 41 patients with CHF and 16 controls. CHF patients showed a decrease of PA (vs. 5.5° 6.4°, P < 0.02) when compared to controls. Linear regression analysis showed a significant correlation TAE index with PA, and the ROC curve showed good predictive performance PA and TAE regarding cardiac death (Doesch et al. 2010). Brenta et al. (2011), considering the plasma levels of triiodothyronine (T3) as a predictor of mortality in patients with CHF, studied its association with PA. In this study the authors found that the lowest tertile of T3 was associated with more advanced CHF and the lower PA values. Castillo et al. (2007), evaluating 243 patients with CHF, noted that PA was positively correlated with functional capacity, that is, the worse the functional capacity, the lower was the PA.
Conclusion
Although there are few studies about the PA as a prognostic factor in liver diseases, the articles published to date indicate that PA is an important predictor of mortality and disease progression in liver cirrhosis and hepatitis C virus.
The PA determined by the BIA in the evaluation of chronic liver disease patients shows itself as easy, inexpensive, reproducible, and reliably free of complications, which ultimately become an important element in determining the prognosis of the disease and can be used sequentially and repetitively to follow-up.
However, the PA obtained from the BIA is a value related to a given normal population which has not been universally characterized; therefore, studies should be carried out for new population cutoff determination of each population.
Summary Points
-
Bioelectrical impedance analysis (BIA) is an important method of assessing body composition of healthy individuals.
-
The BIA is a simple test, easy, economical, feasible in the hospital or clinic, and reproducible with reliability.
-
In order to assess the body composition, the bioelectrical impedance to be held in rest conditions, without the individual, has practiced moderate or intense physical activity between 2 and 3 h previous to the test and without ingested food or liquids 12 h before the test.
-
Phase angle (PA)/BIA is a biological marker of prognosis in patients with cirrhosis or hepatitis C virus.
-
The PA of the bioelectrical impedance is a biological marker of prognosis and progression of various diseases.
-
Population studies should be done to determine the value of the PA of BIA in these populations, which will serve as parameters for prognostic assessment of diseases.
-
The PA, in our experience, has a cutoff value of 5.4° to chronic liver disease.
Abbreviations
- AC:
-
Arm circumference
- AMC:
-
Arm muscle circumference
- APMT:
-
Abductor pollicis muscle
- BCM:
-
Body cell mass
- BIA:
-
Bioelectrical impedance analysis
- CCl4:
-
Carbon tetrachloride
- CHF:
-
Congestive heart failure
- CMR:
-
Cardiac magnetic resonance
- COPD:
-
Chronic obstructive pulmonary disease
- DEN:
-
Diethylnitrosamine
- EAT:
-
Epicardial adipose tissue
- ECW:
-
Extracellular water
- EF:
-
Extracellular fluid
- ES:
-
Extracellular solids
- FFM:
-
Fat-free mass
- FM:
-
Fat mass
- HAART:
-
Highly active antiretroviral therapy
- HCV:
-
Hepatitis C virus
- HGS:
-
Hand grip strength
- HIV:
-
Human immunodeficiency virus
- ICW:
-
Intracellular water
- MELD:
-
Model for End-Stage Liver Disease
- MF-BIA:
-
Multiple-frequency bioimpedance analysis
- PA:
-
Phase angle
- PCM:
-
Protein caloric malnutrition
- R:
-
Resistance
- SF-BIA:
-
Single-frequency bioimpedance analysis
- SPA:
-
Standardized phase angle
- TBARS:
-
Thiobarbituric acid reactive substances
- TBW:
-
Total body water
- Xc:
-
Reactance
- Z:
-
Impedance
References
Aydos MED, Fernandes SA, Nunes FF, et al. One-year follow-up of the nutritional status of patients undergoing liver transplantation. Nutr Hosp. 2016;33:8–13.
Barbosa-Silva MC, Barros AJ. Bioelectrical impedance analysis in clinical practice: a new perspective on its use beyond body composition equations. Curr Opin Clin Nutr Metab Care. 2005a;8(3):311–7.
Barbosa-Silva MC, Barros AJ. Bioelectric impedance and individual characteristics as prognostic factors for post-operative complications. Clin Nutr. 2005b;24:830–8.
Barbosa-Silva MC, Barros AJ, Post CL, et al. Can bioelectrical impedance analysis identify malnutrition in preoperative nutrition assessment? Nutrition. 2003;19(5):422–6.
Barbosa-Silva MC, Barros AJ, Wang J, et al. Bioelectrical impedance analysis: population reference values for phase angle by age and sex. Am J Clin Nutr. 2005;82(1):49–52.
Barbosa-Silva MC, Barros AJ, Larsson E. Phase angle reference values for Brazilian population. Int J Body Compos Res 2008;6: 67–68.
Basile C, Della-Morte D, Cacciatore F, et al. Phase angle as bioelectrical marker to identify elderly patients at risk of sarcopenia. Exp Gerontol. 2014;58:43–6.
Baumgartner RN, Chumlea WC, Roche AF. Bioelectrical impedance phase angle and body composition. Am J Clin Nutr. 1988;48:16–23.
Bera TK. Bioelectrical impedance methods for noninvasive health monitoring: a review. J Med Eng. 2014;2014:381251.
Bona S, Moreira ACJ, Oliveira MS, et al. Caracterização do modelo experimental de carcinoma hepatocelular por Indução Química em Ratos. Rev HCPA. 2012;32(Suppl):151.
Bosy-Westphal A, Danielzik S, Dörhöfer RP, et al. Phase angle from bioelectrical impedance analysis: population reference values by age, sex, and body mass index. JPEN J Parenter Enteral Nutr. 2006;30(4):309–16.
Botta F, Giannini E, Romagnoli P, et al. MELD scoring system is useful for predicting prognosis in patients with liver cirrhosis and is correlated with residual liver function: a European study. Gut. 2003;52(1):134–9.
Brenta G, Thierer J, Sutton M, et al. Low plasma triiodothyronine levels in heart failure are associated with a reduced anabolic state and membrane damage. Eur J Endocrinol. 2011;164(6):937–42.
Castillo LM, Colín ER, Orea AT, et al. Bioelectrical impedance and strength measurements in patients with heart failure: comparison with functional class. Nutrition. 2007;23(5):412–8.
Cezar C. Alguns aspectos básicos para uma proposta de taxionomia no estudo da composição corporal, com pressupostos em cineantropometria. Rev Bras Med Esporte. 2000;6(5):188–93.
de Souza DM, Santos LA, Gondo FF, et al. Phase angle is associated with advanced fibrosis in patients chronically infected with hepatitis C virus. Life Sci. 2016;154:30–33. pii: S0024–3205(16)30112–6.
Dehghan M, Merchant AT. Is bioelectrical impedance accurate for use in large epidemiological studies? Nutr J. 2008;7:26.
Doesch C, Suselbeck T, Leweling H, et al. Bioimpedance analysis parameters and epicardial adipose tissue assessed by cardiac magnetic resonance imaging in patients with heart failure. Obesity (Silver Spring). 2010;18(12):2326–32.
Donaghy A. Advances in liver disease: alcoholic hepatitis, non-cirrhotic portal fibrosis and complications of cirrhosis. J Gastroenterol Hepatol. 2002;17:462–6.
Durand F, Valla D. Assessment of the prognosis of cirrhosis: Child–Pugh versus MELD. J Hepatol. 2005;42:100–7.
Ellis KJ. Human body composition: in vivo methods. Physiol Rev. 2000;80(2):649–80.
Fernandes SA, Bassani L, Nunes FF, et al. Nutritional assessment in patients with cirrhosis. Arq Gastroenterol. 2012;49(1):19–27.
Fernandes SA, Gonzalez MC, Bassani L, et al. Is the phase angle, a prognostic indicator for nutritional status in cirrhotic patients? J Antivir Antiretrovir. 2013;S3:004.
Garby L, Lammert O, Nielsen E. Negligible effects of previous moderate physical activity and changes in environmental temperature on whole body electrical impedance. Eur J Clin Nutr. 1990;44(7):545–6.
Gottschall CBA, Álvares-da-Silva MR, Camargo ACR, et al. Avaliação nutricional de pacientes com cirrose pelo vírus da hepatite C: a aplicação da calorimetria indireta. Arq Gastroenterol. 2004;41:220–4.
Gupta D, Lis CG, Dahlk SL, et al. Bioelectrical impedance phase angle as a prognostic indicator in advanced pancreatic cancer. Br J Nutr. 2004a;92(6):957–62.
Gupta D, Lammersfeld CA, Burrows JL, et al. Bioelectrical impedance phase angle in clinical practice: implications for prognosis in advanced colorectal cancer. Am J Clin Nutr. 2004b;80(6):1634–8.
Huo TI, Wu JC, Lin HC, et al. Evaluation of the increase in model for end-stage liver disease (DeltaMELD) score over time as a prognostic predictor in patients with advanced cirrhosis: risk factor analysis and comparison with initial MELD and Child-Turcotte-Pugh score. J Hepatol. 2005;42:826–32.
Kahraman A, Hilsenbeck J, Nyga M, et al. Bioelectrical impedance analysis in clinical practice: implications for hepatitis C therapy BIA and hepatitis C. Virol J. 2010;7:191.
Khalil SF, Mohktar MS, Ibrahim F. The theory and fundamentals of bioimpedance analysis in clinical status monitoring and diagnosis of diseases. Sens (Basel). 2014;14(6):10895–928.
Kyle UG, Bosaeus I, De Lorenzo AD, et al. Composition of the ESPEN working group. Bioelectrical impedance analysis – part I: review of principles and methods. Clin Nutr. 2004;23(5):1226–43.
Llames L, Baldomero V, Iglesias ML, et al. Values of the phase angle by bioelectrical impedance; nutritional status and prognostic value. Nutr Hosp. 2013;28(2):286–95.
Lukaski HC, Johnson PE, Bolonchuk WW, et al. Assessment of fat-free mass using bioelectrical impedance measurements of the human body. Am J Clin Nutr. 1985;41(4):810–7.
Marroni NP, Colares JR, Schemitt EG, et al. Melatonin mitigates the Nutritional and Morphological changes of rat tongue with secondary biliary cirrhosis induced by ligation of the common bile duct. In: The International Liver Congress, 2016, Barcelona. Journal of Hepathology. 2016;64:S317–S318.
Matos C, Porayko MK, Francisco-Ziller N, et al. Nutrition and chronic liver disease. J Clin Gastroenterol. 2002;35:391–7.
Máttar JA. Application of total body bioimpedance to the critically ill patient. Brazilian Group for Bioimpedance Study. New Horiz. 1996;4(4):493–503.
Mialich MS, Sicchieri JMF, Jordao Jr AA. Analysis of body composition: a critical review of the use of bioelectrical impedance analysis. Int J Clin Nutr. 2014;2(1):1–10.
Müller MJ, Böttcher J, Selberg O, et al. Hypermetabolism in clinically stable patients with cirrhosis. Am J Clin Nutr. 1999;69:1194–201.
Norman K, Stobäus N, Pirlich M, et al. Bioelectrical phase angle and impedance vector analysis – clinical relevance and applicability of impedance parameters. Clin Nutr. 2012;31(6):854–61.
Parise ER, de Oliveira AC, de Carvalho L. Cirrose Hepática. In: Mattos AA, Dantas-Corrêa EB, editors. Tratado de hepatologia. 1st ed. Rio de Janeiro: Rubio; 2010. p. 429–37.
Peres WA, Lento DF, Baluz K, et al. Phase angle as a nutritional evaluation tool in all stages of chronic liver disease. Nutr Hosp. 2012;27(6):2072–8.
Pirlich M, Schütz T, Spachos T, et al. Bioelectrical impedance analysis is a useful bedside technique to assess malnutrition in cirrhotic patients with and without ascites. Hepatology. 2000;32:1208–15.
Ritter L, Gazzola J. Avaliação nutricional no paciente cirrótico: uma abordagem objetiva, subjetiva ou multicompartimental? Arq Gastroenterol. 2006;43:66–70.
Ruiz-Margáin A, Macías-Rodríguez RU, Duarte-Rojo A, et al. Malnutrition assessed through phase angle and its relation to prognosis in patients with compensated liver cirrhosis: a prospective cohort study. Dig Liver Dis. 2015;47:309–14.
Ruiz-Margáin A, Macías-Rodríguez RU, Chi-Cervera L, et al. Phase angle as an early nutritional marker of short-term outcome in hospitalized patients with cirrhosis. In: The International Liver Congress, 2016, Barcelona. Journal of Hepathology. 2016;64:S253.
Schwenk A, Beisenherz A, Römer K, et al. Phase angle from bioelectrical impedance analysis remains an independent predictive marker in HIV-infected patients in the era of highly active antiretroviral treatment. Am J Clin Nutr. 2000;72(2):496–501.
Selberg O, Selberg D. Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis. Eur J Appl Physiol. 2002;86(6):509–16.
Toso S, Piccoli A, Gusella M, et al. Altered tissue electric properties in lung cancer patients as detected by bioelectric impedance vector analysis. Nutrition. 2000;16(2):120–4.
Wagner D, Adunka C, Kniepeiss D, et al. Serum albumin, subjective global assessment, body mass index and the bioimpedance analysis in the assessment of malnutrition in patients up to 15 years after liver transplantation. Clin Transplant. 2011;25:E396–400.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media Dordrecht
About this entry
Cite this entry
Marroni, C.A., Miranda, D., Boemeke, L., Fernandes, S.A. (2017). Phase Angle Bioelectrical Impedance Analysis (BIA) as a Biomarker Tool for Liver Disease. In: Patel, V., Preedy, V. (eds) Biomarkers in Liver Disease. Biomarkers in Disease: Methods, Discoveries and Applications. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-7675-3_43
Download citation
DOI: https://doi.org/10.1007/978-94-007-7675-3_43
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-7674-6
Online ISBN: 978-94-007-7675-3
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences