Abstract
Glioblastomas (GBMs) are the most aggressive primary brain tumors and are heterogeneous at the cellular level. Current therapeutic means are limited to a largely palliative role, with modest improvement in clinical response. The cellular and molecular heterogeneity of GBMs indicates that individual mechanisms are likely to exert different levels of influences on patient treatment response. Glioma-propagating cells (GPCs) which are purportedly enriched in tumor-initiating and sustaining potential are important because they mirror primary tumors at the phenotypic and molecular level. Moreover, they display long-term self-renewal capability, possibly accounting for the frequently observed tumor recurrence and re-growth. Hence, elucidation of GPC targets that confer therapeutic resistance is essential for effective treatment outcome. Here, we highlight several key intrinsic mechanisms that contribute to the perpetuation of GPCs, including the multi-drug resistant phenotype, DNA damage repair as well as key self-renewal signaling cascades. Another integral factor is the paracrine cues from the perivascular/hypoxic milieu. Targeting these multifaceted pathways might therefore sensitize GPCs to chemotherapeutic agents and lead to long-lasting therapies. In addition, we discuss how transcriptome analysis of GPCs derived from histologically similar yet molecularly distinct primary tumors can stratify patient subtypes, each bearing their own unique genetic and clinical profile. These findings highlight the clinical contribution of GPCs to disease progression and survival outcome. Identification of patient subtypes may account for the heterogeneity in treatment response and thus accelerate the development of personalized therapy that can induce sustained clinical outcome. The road ahead will likely be filled with obstacles but these emerging therapeutic paradigms promise new opportunities to patient cohorts lacking in effective treatment options.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Gliomas represent the most prevalent of primary adult malignant brain tumors, with GBM exhibiting the worst prognosis and mean survival period of 15 months post-diagnosis. The highly recurrent, infiltrative and heterogeneous nature of the disease has prompted much research into the origin of gliomas to develop more effective therapeutic targeting. Recent transgenic mouse models utilizing lineage-tracing methodologies have implicated neural stem cells and oligodendrocyte precursor cells as the tumor-initiating cells. These cells display long-term self-renewal and are able to differentiate into all neural lineages, thus recapitulating the eventual tumor phenotype. Although transgenic models allow us to study a limited number of mutations in the tumor-initiating process; moreover such models contain an intact host immune response that more accurately reflects the microenvironmental niche; they often do not reform the phenotypic and molecular heterogeneity of patient tumors. Consequently, complementary approaches encompassing patient tumor-derived GPCs are needed. Such GPCs have been shown to mirror the phenotype and molecular fingerprint of their primary tumors. Furthermore, recent evidence demonstrates that their transcriptomic pathway networks contribute to GBM disease progression and patient survival outcome. These findings emphasize the importance of GPCs as clinically relevant in vitro culture systems. Although their use precludes the identification of the true cell-of-origin; moreover no definitive marker can be ascribed to tumor-initiating capability, nevertheless, their stem-like properties are important to understand and target for an effective and long-lasting cure.
Our previous work highlighted the molecular heterogeneity of GPCs derived from histologically similar primary tumors. These findings may account for the frequently observed patient heterogeneity to treatment response. In addition, we showed that pathway predictions based on GPC transcriptomic data matched actual cellular response to small molecules targeting various oncologic pathways. This is an important conceptual advance as traditional drug screening with commercially available cell lines often utilizes short-term viability readouts as endpoints, thus compounds that target slowly-dividing, stem-like cells may inadvertently be de-prioritized. The understanding that gliomas are heterogeneous, and that an often minor, slow-growing cellular subset is responsible for tumor-propagation thus presents a paradigm in therapeutic design. Recent reports have illustrated that multiple, closely-related driver genes are amplified and activated in intermingled, clonal populations of tumor cells, further reinforcing the functionally heterogeneous nature of the disease. In addition, GPCs display enhanced resistance to common chemotherapeutic agents and radiotherapy, and has been shown to rely on surrounding vascular networks to maintain its own survival (Bao et al. 2006b). Such observations highlight that GPCs are not likely to standalone in the tumorigenic process, and that a composite of cell-autonomous and paracrine signaling is vital to consider in effective targeting.
In this review, we will focus on several primary resistance mechanisms of GPCs, including the multi-drug resistance family of proteins, DNA damage repair pathways, and self-renewal mechanisms typified in normal stem cells, as well as the influence of the microenvironmental niche. Additionally, with the advent of public efforts in glioma molecular and clinical profiling, such as The Cancer Genome Atlas and REMBRANDT, we discuss how bioinformatics analyses can play a role in identifying patient cohorts amenable to pathway inhibition predicted by their GPC content. Our review summarizes the cellular and molecular heterogeneity of gliomas, and further highlights the limitations of relying on solely morphology-based histological methods in patient diagnosis, consequently impacting on treatment decision.
Role of the Multi-Drug Resistance Family
One of the most important mechanisms that a cancer cell can resist chemotherapeutic agents is the expression of multiple drug resistance transporters to actively efflux a broad range of anti-cancer drugs so as to maintain an intracellular drug concentration below a threshold that is detrimental to the cell. Multiple drug transporters belong to the ATP Binding Cassette (ABC) transporter superfamily of proteins. The functions of the ABC transporters include the efflux of various endogenous organic molecules (e.g. bile acids, cholesterol, glutathione, and peptides) across the cell membrane and in some instances, expelling inorganic drugs that cause toxicity to the cells. Like normal stem cells, tumor stem-like cells have been shown to express high levels of ABC transporters. Three of the ABC transporters that have been commonly implicated in the development of treatment resistance in cancers include: ABCB1 (also known as P-glycoprotein or MDR1), ABCC2 and ABCG2 (also known as Breast Cancer Resistance Protein). ABCB1 is the first member of the ABC family to be discovered and has been shown to be overexpressed in more than 50% of all drug-resistant tumors. ABCB1 transporter is a broad spectrum multidrug efflux pump that consists of 12 transmembrane domains and two ATP-binding domains. It acts as an ATP-dependent transporter to remove cytotoxic drugs and many other structurally unrelated hydrophobic compounds from the lipid bilayer. It has been demonstrated that ABCB1 expression is higher in the fraction of cancer stem-like cells derived from spheroid cultures of the glioma cell line U87MG, compared to its non-stem-like counterparts (Nakai et al. 2009). In addition, these cancer stem-like cells possess greater drug resistance against a panel of commonly used anti-cancer drugs such as doxorubicin (Dox), etoposide (VP-16), carboplatin, and BCNU, compared to the non-stem-like fraction. The ability of stem-like cells to efflux drugs using the ABC transporters is an important property that allows for the isolation and analysis of stem-like populations. This property enables investigators to isolate stem-like cells termed the “side population” (SP) that excludes the fluorescent dye, Hoechst 33342, by fluorescence-activated cell sorting. SP cells display enhanced expression of both ABCB1 and ABCG2. Although the molecular basis of SP cells in conferring the stemness property remains unclear, the SP phenotype has been largely attributed to the compensatory activity of the ABCG2 transporter as bone marrow cells derived from ABCB1-knockout mice retain normal numbers of SP cells. Studies from our laboratory have shown that SP cells possess progenitor cell-like characteristics and tumor-initiating potential in an immune-compromised mouse model. More importantly, the number of SP cells increase with Temozolomide (TMZ) treatment and this corresponds to elevated progenitor-like cells with increased expression of several ABC transporters (Chua et al. 2008). Furthermore, Bleau et al. (2009) showed that the PTEN/PI3K/AKT signaling axis, a central regulatory network in GBM growth, regulates that SP phenotype and the activity of ABCG2 transporters. Importantly, they showed that TMZ treatment increases the proportion of SP in glioma cells, especially in cells with loss of PTEN.
Role of DNA Damage Repair Pathways
Radiotherapy is essential in the treatment regime of glioma patients; yet, in combination with adjuvant chemotherapy, tumor recurrence and re-growth is frequent. Such resistance can be attributed to DNA-repair proficiency, a multitude of deregulated molecular pathways, and more recently, to the particular biologic behaviour of GPCs. Indeed, resistance to TMZ has been ascribed to enhanced expression and activity of O6-methylguanine-DNA-methyltransferase (MGMT), an enzyme that mediates repair of double-strand DNA (dsDNA) breaks, often induced by chemotherapeutic agents such as TMZ, VP-16 and carboplatin. Epigenetically silenced MGMT in particular patients has allowed significant prolongation of survival following therapy. Interestingly, the gene expression profiles of 80 glioblastoma patients has been studied for associations with resistance to therapy. An expression signature dominated by HOX genes (and comprising CD133), evocative of a self-renewal signature recently described for leukemia, emerged as a predictor for poor survival in patients treated with concomitant chemoradiotherapy. More importantly, the HOX signature was an independent prognostic factor in multivariate analysis, adjusted for the MGMT status. These findings highlight that treatment resistance is due to a combination of not only the MGMT status, but also specific stem cell-related pathways.
Several investigators have shown that GPCs display enhanced resistance to several chemotherapeutic agents and express elevated MGMT mRNA expression compared to non-stem cells (Liu et al. 2006). Moreover, recent work by Rich and colleagues elucidated the mechanism governing radioresistance of CD133+GPCs (Bao et al. 2006a). They showed that CD133+GPCs were more efficient at repairing dsDNA breaks through activated checkpoint responses including ataxia telangiectasia (ATM) mutated and the checkpoint kinases, Chk1 and Chk2. Moreover, the checkpoint activation in CD133+ cells was biologically important as pharmacologic targeting of checkpoint function reversed the cancer stem cell radioresistance, suggesting that Chk1/2 inhibitors may warrant additional clinical development, particularly in combination with cytotoxic therapies. Together, the findings support that the development or maintenance of a cancer stem cell may select for an activated checkpoint implicating a form of convergent evolution toward a cellular behavior rather than a single molecular target. Indeed, follow-up studies by this group demonstrated that L1CAM, a neural cell adhesion molecule, marks CD133+GPCs, and is responsible for mediating the DNA damage checkpoint response via the NBS1-ATM axis (Cheng et al. 2011).
Other stem cell-related pathways that may underlie cancer stem cell radioresistance include Wnt/β-catenin, Notch, sonic hedgehog, Pten, EGFR and Bmi-1. Wnts and β-catenin have clearly defined roles in normal stem cell development and cancer, but their role in cancer stem cell biology is less clear. Recent studies have suggested that Wnt and β-catenin signaling may contribute to radioresistance of mammary cancer stem cells. In addition, elevated Notch activity in response to radiation in breast cancer mammospheres is known. Hedgehog and Gli signaling can also be inhibited to attenuate cancer stem cell renewal and tumor growth (Bar et al. 2007). Loss of PTEN function alters Chk1 localization and function to initiate genetic instability and confers radiation resistance in glioblastoma cell lines. EGF is a primary growth cytokine used to maintain GPCs in vitro and marks a dose-dependent tumorigenic capacity of the cells in orthotopic mouse models. EGFR mediates radioresistance in glioma models that can be disrupted by EGFR tyrosine kinase inhibitors. Collectively, inhibitors of stem cell pathways may sensitize GPCs to the effects of ionizing radiation, providing a broad therapeutic paradigm.
Role of Self-Renewal Signaling Pathways
Key signaling cascades that are crucial for normal neural stem cells, such as Notch, Hedgehog, Wnt, and the PI3K-Akt axis, have been a focus of increasing interest in cancer therapy as these pathways may underlie GBM therapeutic response and manipulation of these pathways may preferentially deplete GPCs. Even though GBMs share many of these alterations, each individual patient tumor has its unique genetic profile, making it a challenge to develop effective therapeutic interventions. Thus, the Achilles heel of GBMs may not be a single major genetic alteration, but rather a secondary acquired imbalance in the aberrant regulatory signaling networks.
Notch Pathway
The four Notch proteins (Notch 1–4) mediate cellular communication via interaction with their cognate ligands, including Jagged-1, -2, and Delta-like -1, -3, and -4. Activation of the Notch signaling cascade involves proteolytic cleavage by γ-secretase and is critical for the maintenance of stem and progenitor cells in promoting self-renewal and repressing differentiation. Aberrant Notch signaling has been implicated in the pathogenesis of multiple tumors including gliomas, and the overexpression of Notch and its ligands, Delta-like-1 and Jagged-1, is commonly associated with glioma survival and proliferation. The role of Notch signaling in GBMs has been widely characterized and it has been shown that downregulation of NOTCH1, Delta-like-1, or Jagged-1 leads to glioma cell apoptosis and translates into a prolonged survival in a mouse orthotopic brain tumor model. Fan et al. (2010) demonstrated that specific Notch targeting of patient-derived GPCs by γ-secretase inhibitor (GSI) attenuated neurosphere-forming ability with marked decrease in the expression of stemness-related markers, increased sensitivity to chemotherapeutic agents in vitro and blocked tumor propagation in vivo, suggesting a potential dependence on Notch signaling in GPCs. Activation of Notch by upstream oncogenic stimuli and microenvironmental cues is essential for the maintenance of GPCs and the facilitation of tumor propagation, suggesting a role of Notch at the centre of key regulatory GPC signaling networks. Another study has shown that overexpression of NOTCH1 in glioma cells leads to an increase in proliferation and formation of nestin-positive, neurosphere-forming stem cells (Hu et al. 2011). Previous reports have demonstrated that exposure to radiation modulated the activation of Notch signaling in the CD44+/CD24-/low breast cancer stem cells. In addition, Notch signaling has been implicated in the radioresistance phenotype of GPCs where knockdown of NOTCH1 or NOTCH2 effected radiosensitivity of GPCs but not that of differentiated glioma cells (Wang et al. 2010a), suggesting that inhibition of Notch signaling may not only deplete GPC frequency and engraftment potential but also reduce the radioresistance of GPCs. Furthermore, inhibition of the Notch cascade in irradiated GPCs brought about increased apoptotic marker caspase 3/7 and positive labeling of apoptotic marker Annexin V. Thus, these data suggest that, in the case of gliomas, Notch may be a possible target in stem-like glioma cells as GPCs express Notch family genes and tumor-derived neurospheres have elevated Notch activity and might be involved in evading apoptosis and promoting proliferation. Thus, targeting of Notch and its components underlying the radioresistance of GPCs promises to confer sustained benefit for glioma therapeutics.
Additional studies have shown that γ-secretase inhibition of Notch signaling upregulated the Wnt and Hedgehog pathways, both essential for normal neural development. The Notch target Hes1 binds Gli1 directly, blocking its transcriptional level. Concomitant inhibition of Notch and Hedgehog dramatically decreased proliferation of neurospheres and primary human GBM cells, suggesting this regulatory mechanism may contribute to resistance. These findings demonstrate that Notch-targeted therapeutics can lead to alterations in other developmental signaling cascades that promote tumor survival, and suggest that combinatorial treatment with Hedgehog pathway inhibitors may be able to increase the efficacy of γ-secretase inhibition in cancer patients.
Hedgehog-Gli pathway
The Sonic Hedgehog signaling is one of key regulatory pathways critical for the maintenance of several types of adult stem cells, including neural stem cells (Clement et al. 2007). The Hedgehog signaling cascade is commonly known to be expressed by tumor-associated endothelial cells and astrocytes in platelet-derived growth factor (PDGF)-driven mouse models of GBM. The main components of this signaling pathway are the ligands (secreted Hedgehog proteins), the Patched receptor (Ptch, a 12-pass transmembrane protein), the intracellular transducing molecules Smoothened (Smo – a second transmembrane protein) and Gliotactin (Gli, zinc-finger transcription factors). Ligand-binding of Hedgehog to Ptch represses Smo inhibition, allowing the activation of the canonical Hedgehog pathway through Gli-dependent transcription of multiple targets, including N-myc, cyclin D, Ptch, Gli1, and Gli2.
Several studies have implicated the ligand-dependent activation of Hedgehog signaling in tumorigenesis for various cancers. These studies ascribe a cell-autonomous role for Hedgehog signaling and propose that even in the absence of mutations in the Hedgehog cascade, tumor cells still produced and responded to the Hedgehog ligand in an autocrine manner. However, more controversial studies on pancreatic cancer have implicated a role for paracrine Hedgehog signaling in tumor stromal cells in the maintenance of the cancer stem cell microenvironment. Hedgehog-overexpressing tumor cells induce a response in surrounding stromal cells whilst epithelial tumor cells are refractory to Hedgehog pathway modulation. The expression of Hedgehog ligands by tumor cells was not associated with their expression of target genes but rather, was in concordance with the canonical pathway activity by infiltrating tumor stromal cells. Notably, analysis of human tumor xenografts revealed that levels of Hedgehog ligand mRNA expression in tumor cells corresponded with elevated Gli1 and Ptch1 mRNA levels in the stroma but not the tumor compartment, indicating that the Hedgehog ligands activate Hedgehog signaling in the adjacent stroma microenvironment and not the tumor epithelium. Specific inhibition of Hedgehog signaling in the stroma with either an antagonist of Hedgehog or a neutralizing anti-Hedgehog antibody or genetic ablation of Smo resulted in xenograft tumor inhibition, further substantiating the role of Hedgehog-activated stroma in tumor propagation. It has also been demonstrated that a constitutively activated stromal Hedgehog signal is adequate to accelerate tumor growth even in the absence of a Hedgehog ligand. In addition, chimeric xenografts coinjected with a human prostate cancer cell line that did not respond to Hedgehog ligand and a Hedgehog-overexpressing cell line were composed of a mixed population with equal cell numbers and similar tumor proliferation rate, suggesting that paracine Hedgehog signaling exerts a non-cell autonomous effect on tumor growth. The authors then identified a transcriptional gene signature of Hedgehog signaling that is reminiscent of the fetal mesenchyme, faithfully recapitulating human prostate tumors with a reactive stroma phenotype. Thus, insights into the mechanisms driving the Hedgehog pathway will be critical since patients bearing mutation-driven Hedgehog tumors, as in the case of basal cell carcinomas and medulloblastoma, are more likely to display a more favourable clinical response to Hedgehog inhibitors whilst tumors regulated by the paracrine mode remain resistant. Hence, elucidation of Hedgehog inhibition via either the stromal microenvironment or the tumor epithelia will allow for the development of more effective targeted Hedgehog antagonists for a broad range of cancers.
Hedgehog signaling is highly deregulated in a small subpopulation of human medulloblastoma and Gli1, a key Hedgehog target, was highly expressed in primary GBMs and CD133+GBMs (Bar et al. 2007). Conventional sources of Hedgehog ligands include CD133+GPCs and tumor-induced vasculature in GBMs (Clement et al. 2007). Several groups have investigated the role of Hedgehog-Gli signaling in GPCs and found that this signaling pathway regulates GPC function, self-renewal and tumorigenesis (Clement et al. 2007; Ehtesham et al. 2007). Forced differentiation of GBM neurospheres reduced both stemness and Hedgehog activity expression. However, not all GBMs have activated Shh signaling as determined by Gli expression (Bar et al. 2007), indicating the presence of molecular subgroups of brain tumors in which targeting of Shh would be ineffective. Treatment of GPCs with the Hedgehog inhibitor cyclopamine or Gli knockdown drastically depleted the GPCs by suppressing self-renewal ability and proliferation while increasing apoptotic cell death in vitro and inhibiting tumor propagation in vivo. Importantly, cyclopamine inhibition of Hedgehog-Gli signaling enhances the efficacy of TMZ to abolish GPC proliferation and improve the effect of radiation on GPCs. Taken together, these studies indicate that the Hedgehog-Gli module is critical for GPC maintenance and targeting this pathway with specific pharmacologic inhibitors may attenuate GPC self-renewal and offer improved therapy efficiency against gliomas.
Gli1 acts at the distal end of the Hedgehog pathway, where it regulates transcription in response to activation or inhibition of the pathway. Moreover, Gli activity correlates with tumor grade in a genetically engineered mouse model. As such, further investigation must be performed to explore its role in GPC growth, maintenance and GBM recurrence. Cui et al. (2010) investigated the role of Gli1 in primary and recurrent gliomas and its ability to confer chemosensitivity or chemoresistance of glioma cells. Overexpression of Gli1 associated with GPC chemoresistance, resulting in glioma perpetuation. Conversely downregulation of Gli1 enhanced the susceptibility of GPCs to the synergistic effects of cyclopamine and chemotherapeutic agents, promoting apoptotic cell death, thus suggesting that Gli1 is a key mediator of chemoresistance in GBMs with aberrant Hedgehog signaling. Moreover, the constitutive Hedgehog pathway activity contributes to the resistance of glioma cells to chemotherapeutic agents by promoting self-renewal and tumor regrowth following therapy in an autocrine and/or paracrine manner (Bar et al. 2007). In contrast, abolishment of Hedgehog pathway activity abrogates tumor growth and restricts tumor recurrence, by downregulation of the expressions of MDR1, MRP1, LRP, MGMT, BCL2 and Survivin, which play important roles in glioma chemoresistance and repopulation, thus providing a mechanism to explain the recurrence of some gliomas.
Mouse models of medulloblastoma CSCs localized in the perivascular vicinity express Nestin and are protected from radiation, owing to the ability to activate the PI3K/Akt pathway and undergo a transient, p53-dependent cell cycle arrest. This suggests that GPCs’ therapeutic response cannot be considered in isolation from the tumor microenvironment with its potential dependence on the perivascular compartment. It is therefore imperative to understand the interactions between self-renewal pathways and signals known to be altered in cancer in the context of specific microenvironments found in the perivascular niche. Hence, the Hedgehog-Gli signaling network could provide important therapeutic implications as synergistic inhibition of the Hedgehog pathway and Gli activity in some gliomas may be a potential target for the alleviation of therapeutic resistance and enhanced the chemotherapeutic response in glioma patients.
EGFR/PI3K/AKT Axis
The presence of autocrine and paracrine growth factor loops are common in malignant gliomas and these pathways regulate numerous pro-tumorigenic cellular functions including cellular proliferation, apoptotic resistance, invasion and angiogenesis. Epidermal growth factor (EGF), routinely used in culturing EGF-responsive neural precursors, is a key growth factor used in the maintenance of GPCs. GBMs frequently display EGFR amplification, with expression of the constitutively active variant EGFRvIII, mediated through PI3K-Akt and Ras/mitogen-activated protein kinase (MAPK) downstream signaling in GBMs and is associated with enhanced tumorigenic potential and more aggressive phenotypes, such as invasiveness and therapeutic resistance. Shinojima et al. evaluated 87 primary GBM patients and found EGFR amplification to be an independent, unfavorable predictor for overall survival. In this cohort, EGFRvIII overexpression in the presence of EGFR amplification is the strongest indicator of a poor survival prognosis.
Intratumoral heterogeneity plays a major role in contributing to GBM resistance to EGFR targeted therapy due either to pre-existing resistant clones within the tumor or the interaction of non-resistant clones with the tumor cells or the tumor niche. Mazzoleni et al. (2010) showed that despite both the molecularly and functionally distinct EGFRpos and EGFRneg GPCs being able to form tumors that phenocopy the original tumor sample, only EGFRpos GPCs had elevated tumorigenic proliferation and highly invasive characteristic. Conversely, the EGFRneg GPCs formed tumors sporadically and required enforced EGFR gene transfer to form tumors. Hence, the presence of distinct subpopulations within the same tumor might contribute to GBM resistance and EGFR targeted therapies since EGFRneg GPCs are insusceptible to treatment and will survive to reform the tumor mass. Inda et al. demonstrated that EGFRvIII cells secrete IL-6 and LIF, which in turn promote the growth and proliferation of wild-type EGFR cells that form the tumor bulk. This small subset of EGFRvIII cells, driven in a paracrine manner to recruit wild type EGFR cells into accelerated proliferation, enhances the tumorigenic potential of the bulk tumor and actively maintains a heterogeneous expression of both the wild type and the mutant form (Inda et al. 2010). Mice orthotopic tumors overexpressing EGFRvIII are refractory to radiation therapy, with sustained repopulation and nondescript effect on overall survival. The efficacy of EGFR kinase inhibitors have been disappointing so far as silencing of EGFRvIII compels GBM cells to undergo selective pressure in vivo to employ alternative compensatory pathways such as upreglating receptor tyrosine kinases (PDGFR, IGF1-R and c-Met) to maintain aggressiveness. These findings suggest that tumor cells are adept at bypassing single EGFR targeted therapies, reforming the tumor after an initial period of stasis, and inhibition of EGFR alone will not be adequate for translation into a beneficial clinical response in GBM patients. An effective therapeutic strategy should take into account the role of residual EGFRneg GPCs or that of the secreted factors in the tumor niche, and the development of a tailored combinatorial therapy targeted at both the aggressive EGFRpos GPCs and the less malignant EGFRneg GPCs or the microenvironment will be imperative to improve the clinical response of GBM patients.
One of the main molecular changes accompanying progression of gliomas to high grade, with simultaneous elevated stem cell expression and resistance to chemotherapy, is the loss of Phosphatase and tensin homolog (PTEN) and consequent elevation of Akt pathways activity. Deficiency in PTEN modulates CHK1 localization, initiating genetic instability and thereby conferring chemoradioresistance in GBMs. A number of intracellular signaling cascades are activated upon EGFR stimulation, but the PI3K-Akt module has been predominantly linked to GPC biology and contribution to the resistant phenotype (Eyler et al. 2008). Various studies have shown that hyperactivation of the PI3K/Akt and Ras/MAPK signaling pathways in cancer cells promotes tumorigenesis, increases tumor cell survival, proliferation, invasion and is significantly associated with radiotherapy resistance, either through the modulation of cell survival signaling or, by direct regulation of the DNA repair machinery. In human gliomas, there is evidence at genomic, mRNA and protein levels showing that aberrant Akt signaling prognosticates poorer survival. Indeed, chemoresistance in hepatocarcinoma stem cells may be conferred by activation of Akt, and Akt signaling promotes survival of stem-like tumor cells in the perivascular niche of mouse medulloblastoma models. It has been recently demonstrated that GPCs are more dependent on Akt signaling than their matched non-stem counterparts (Eyler et al. 2008). It has been observed that GBMs expressed significantly higher levels of phospho-PI3K and phospho-p70s6k, but not of phospho-Akt, compared to their non-GBM counterparts, implying that GBMs display dependency on these pathways possibly for their survival, proliferation and therapeutic resistance. In addition, inverse correlation between phospho-PI3K, phospho-Akt, and phospho-p70s6k levels with cleaved caspase 3 implicates the likely mechanisms employed by the members of the PI3K family in the inhibition of apoptosis and promotion of radioresistance in GBMs. Functional inhibition of Akt with the pharmacologic inhibitors preferentially disrupts GPC neurosphere formation, reduces motility and invasion, induces apoptosis in vitro, and significantly prevents intracranial tumor formation of GPCs (Eyler et al. 2008; Bleau et al. 2009). Although in vitro targeting of the EGFR-PI3K-Akt signaling cascade may have specific effects on GPC self-renewal and tumorigenic progression, clinical trials of EGFR inhibitors, such as Imatinib, have not resulted in significant survival, suggesting that EGFR inhibition solely is an insufficient therapeutic paradigm, prompting greater focus on PI3K inhibitors.
EGFR/EGFRvIII’s cross-interaction with the oncogenic transcription factor STAT3 and receptor tyrosine kinases (c-Met and PDGFR) mediates GPC resistance to anti-EGFR therapy. JAK-STAT3 pathway is constitutively activated in the majority of GBMs and the dynamic interactions between STAT3 and EGFR underlie resistance of GBM cells to Iressa. Combinatorial inhibition of JAK and EGFR/EGFRvIII abolishes STAT3 activation and synergistically suppresses the GPC proliferation. JSI-124 acts as a highly selective inhibitor of the JAK/STAT3 signaling pathway and has been shown to sensitize malignant glioma and medulloblastoma cells to TMZ, 1,3-bis(2-chloroethyl)-1-nitrosourea, and cisplatin.
Taken together, these findings discussed here suggest that EGFR signaling, either directly through the interaction with the DNA repair machinery or indirectly through the activation of key oncogenic PI3K/Akt and JAK/STAT signaling pathways, modulates sensitivity to radiation. Therefore, elucidation of the dynamic interactive EGFR networks will enable us to identify mechanisms that circumvent therapeutic resistance in GPCs and improve the modest efficacy of current EGFR-targeted therapy in GBM patients. Given the central role of the EGFR signaling pathway in conferring the aggressive phenotype in tumors, treatment resistance, and poor prognosis, considerable effort has been invested in the development of imaging strategies to non-invasively ascertain EGFR status and therapeutic response to EGFR targeting agents. Such approaches would enable more accurate stratification of the patients who are likely to benefit from EGFR targeting therapeutics and for monitoring treatment efficacy.
Wnt Signaling
The primary role of the Wnt/β-catenin pathway in embryogenesis and normal stem cell development such as the regulation of stem cell proliferation and self-renewal, has been well established. Wnts are a family of 19 secreted glycoproteins that regulate embryonic patterning and initiate a series of signaling cascade throughout development of the nervous system. Secreted regulator proteins of the Wnt family bind to specific Frizzled (Fzd) receptor complexes on the surface of target cells to initiate Wnt signaling cascades that can be broadly classified into canonical or non-canonical, determined by the composition of the Wnt/Fzd complex. The canonical pathway, which regulates the ability of the β-catenin protein to promote the activation of downstream genes, is better characterized and is therefore more relevant in the development of Wnt therapeutic interventions.
Wnt signaling has been implicated in the control over various types of stem cells and may act as a niche factor to maintain stem cells in a self-renewing state. The Wnt signaling pathway has been shown to be the predominant driving force of stem cells of the colonic crypt, hematopoietic and central nervous system. In particular, tumor-propagating cells of the colon, breast and hematopoietic system have been shown to promote tumorigenesis through major contributions from aberrant Wnt signaling. Mutations in Wnt pathway genes such as adenomatous polyposis coli (APC) and CTNNB1, are commonly present in a majority of hepatocellular carcinoma, thyroid cancer, and ovarian cancer. The fact that Wnt signaling is also dysregulated in multiple solid cancers suggests that it may also play a crucial role in the maintenance of GPCs. It has been demonstrated that Wnt2, an activator of the canonical pathway, was significantly overexpressed in gliomas and their expression levels correlated positively with malignancy. Similarly, higher grade gliomas were observed to express elevated CTNNB1 expression, which subsequently correlated to a poorer prognostic impact in GBM patients. In addition, the expression of other Wnt regulators, including Dvl2, Dvl3, FRAT-1, Pygo-2, Tcf4, and Lef-1 and of specific Wnt target genes, Cyclin D1 and c-myc, also increases with glioma grades. Of note, knockdown of Dvl2 abrogated both the self-renewal ability and proliferation of gliomas and stimulated the differentiation of patient GBM samples. Tumor propagation in immune-compromised mice was repressed upon Dvl2 depletion. In addition to regulation of the expression of Wnt members, antagonists of the Wnt pathway are often repressed in GBMs and their expression is mostly inversely correlated with glioma grades. Frequent aberrant promoter hypermethylation of these Wnt antagonists, such as the Wnt inhibitory factor (WIF), secreted-Frizzled-related protein (sFRP) and the LRP antagonist Dickkopf (Dkk) is significantly associated with GBMs. Furthermore, a novel proto-oncogene PLAGL2, which is overexpressed in GBMs and induces GPCs proliferation and tumorigenic potential, has been identified. PLAGL2 stimulates the expression of Wnt-6, Fz-9, and Fz-2, inhibits differentiation, and increases proliferation of neural progenitors. PLAGL2 amplification also associates with elevated levels of CTNNB1 in GBMs, suggesting a possible role of PLAGL2 in GPCs via the regulation of Wnt signaling. It has been shown that hypermethylation of paternally expressed gene 3 (PEG3) promoter in glioma mitigates expression of PEG3 and correlates with high-grade gliomas. Upon PEG3 promoter hypermethylation, β-catenin accumulates, resulting in GPCs proliferation. A recent study by Zhang et al. (2011) showed that the interaction between the transcription factor Forkhead box M1 (FoxM1) and β-catenin promotes β-catenin nuclear localization, controls transcriptional activation of Wnt target genes expression and maintains GPC self-renewal. Together, these findings validate the role of Wnt and activated β-catenin signaling in mediating GPCs self-renewal.
The Wnt/β-catenin pathway has been imputed in conferring radioresistance in mammary progenitor cells and breast cancer cell lines expressing common cancer stem cell markers. Woodward et al. demonstrated that radiotherapy results in enrichment for the stem- and progenitor-cell– containing population in a murine mammary epithelial cell culture, and particularly augments the stem-cell antigen (Sca)–positive compartment of the side population cells. Consistent with this, tumor-initiating cells from a p53-null mouse mammary tumor had upregulation of active β-catenin and were able to undergo DNA damage repair more efficiently compared to the non-TICs. It is known that Wnt1 ectopic expression activates the DNA damage response in epithelial mammary cells. WJ2, a cancer stem-cell cell line derived from GBM, displayed higher expression of stemness markers with concomitant Wnt1 expression. Overexpression of MDR1, a downstream target of Wnt-1/Fz-1 signaling, confers chemoresistance in neuroblastoma cells, implicating a similar chemoresistance mechanism in gliomas. Taken together, these findings suggest a possible role for Wnt signaling in the chemoradioresistance mechanisms developed by GPCs. Elucidation of the specific genetic lesions in the Wnt signaling cascade in GBMs will allow for the design of specific therapeutic tools to decrease tumor recurrence and improve patient survival.
Role of the Tumor Microenvironment
The diffuse nature of gliomas, its anatomic complexities and the cellular heterogeneity of GBM contributes to the poor response to currently available treatment regimens as chemotherapeutics are unable to reach tumor sites. Regional variations in the tumor microvasculature resulting in the heterogeneous nature of GPCs, as well as the diversity of the cancer cell subpopulation that results from the progressive stochastic selection of genetically resistant subclones, confers GPCs their therapeutic resistance property. Intimate interaction between the tumor microenvironment and the GPCs thus presents a potential avenue for therapeutic targeting of the microenvironment components as well as the GPCs.
In the adult brain, normal neural stem cells (NSCs) were observed to be concentrated around vasculature, known to have low oxygen availability and distinct extracellular matrix (ECM) profiles, for convenient access to signaling molecules, nutrition and migration. The subversion of this normal vascular microenvironment modulates GPC function and similar to NSCs, these specialized GPC niches tightly regulate oxygen and nutrition to maintain GPC phenotype, thereby facilitating its invasive and tumor proliferating properties. This disorganized florid neovasculature is a hallmark of GBMs and has a protective role in shielding GPCs from therapeutic insults, enabling them to reform a tumor mass following initial clinical response (Gilbertson and Rich 2007). The degree of vascularization is significantly correlated with glioma malignancy, tumor aggressiveness and clinical prognostication. Calabrese et al. (2007) identified a fraction of CD133+/Nestin+ cells enriched in areas of increased microvessel density, suggesting that tumor vasculature generates a specialized niche microenvironment in which the formation and maintenance of GPCs proceeds. In addition, co-implantation of tumor cells with endothelial cells led to rapid tumor propagation, implicating the influence of the vascular niche on tumor initiation. GPCs are enriched in functional aberrant niches, predominantly the perivascular niche, which provides microenvironmental cues for the maintenance of GPCs. Abrogation of this niche via anti-angiogenic drugs effected impaired GPC self-renewal and depleted tumor growth, further validating the importance of the perivascular niche in the regulation of tumorigenesis.
Bidirectional interplay between the supportive tumor vascular niche and GPCs was validated by Bao et al.when they demonstrated that GPCs released vascular endothelial growth factor (VEGF), modulating endothelial cell migration and subsequently, facilitating tumor growth by stimulating tumor vasculature, influencing angiogenesis and vasculogenesis through increased expression of VEGF and stromal cell-derived factor-1 (SDF-1) respectively (Bao et al. 2006b; Folkins et al. 2009). Tumor angiogenesis is an essential hallmark of GBMs, whereby vascular proliferation is a WHO histopathology indicator of GBMs, and is frequently associated with resistance to radiation. Tumor vasculogenesis, which involves the recruitment of endothelial precursors to induce the formation of new capillaries, represents a possible treatment approach to prevent tumor recurrence. Kioi et al. employed a murine intracranial GBM xenograft model and demonstrated that following radiation-induced damage, increased vasculogenesis was observed to reinitiate tumor proliferation. This cascade was triggered by upregulation of hypoxia in the tumor, leading to increased levels of SDF-1. The chemokine receptor, CXCR4, is then activated by SDF-1 to promote angiogenesis and VEGF production in gliomas. GPCs express high levels of SDF-1 and given their inherent radioresistance phenotype, it is imperative that the role of GPCs in post-irradiation vasculogenesis be further elucidated to develop more effective therapeutic strategies in order to circumvent resistance to conventional GBM therapies.
Owing to the fact that GBMs are vascular-rich tumors with high levels of VEGF production, clinical trials for the anti-VEGF antibody bevacizumab (Avastin) were conducted. However, despite its initial promise in a phase II clinical trial where GBM patients responded to the combinatorial treatment of bevacizumab and irinotecan, bevacizumab only conferred a transient respite with short term tumor burden control and patients’ tumor inevitably repopulated. It has been reported that treatment with bevacizumab had marginal effect on tumor growth, coupled with significant decrease of vascular supply, elevated infiltration by tumor cells in the brain parenchyma and a more aggressive tumor phenotype. Therefore, there is a pressing need to better elucidate this insidious mechanism of failure for targeted anti-angiogenesis treatment so as to improve the clinical outcomes for GBM patients. Recent studies have shown that GPCs could differentiate to tumor endothelium and when targeted, resulted in ablated tumor burden (Wang et al. 2009; Ricci-Vitiani et al. 2010; Soda et al. 2011). Ricci-Vitiani et al. (2010), Wang et al. (2009) and Soda et al. (2011) identified endothelial cells in GBM microvasculature that possessed genomic aberrations specific for the tumor, suggesting that GPCs are involved in vasculogenesis and that these endothelial cells are of tumor origins. These GPCs could also differentiate into endothelial-like cells both in vitro and in vivo, highlighting that the positive paracrine feedback between GPCs and the vascular niche is integral to promote tumor maintenance and growth. Furthermore, Wang et al. (2009) observed that exposure to bevacizumab or VEGF silencing inhibits the maturation of tumor endothelial progenitors into endothelium without affecting the differentiation of GPCs into endothelial progenitors, whereas γ-secretase inhibition or NOTCH1 silencing blocks the transition of GPCs into endothelial progenitors, suggesting that the failure of bevacizumab could be due to inability to block this transdifferentiation process. An in-depth understanding of this lineage plasticity could provide new insights into GPC biology and enable the development of more efficacious combination therapy.
Apart from interaction with endothelial cells, GPCs residing in the perivascular regions are in contact with ECM components, including microglia, T-lymphocytes, neural precursor cells, GFAP-expressing astrocytes and fibroblastic pericytes, that are preferentially expressed within and around blood vessels. Cell-ECM interactions have been shown to contribute to the response of tumor cells to radiation by: (1) Serving as a repository for proteins that modulate therapeutic response, (2) Operating as a substratum for the activation of prosurvival integrin-mediated signaling cascades following irradiation, and (3) Creating a more favorable niche for the proliferation of cells that survive therapy. Lathia et al. (2010) observed perivascular colocalization of integrin α6 with CD31-expressing endothelial cells in GBM patient samples, underlining the significance of the interplay between GPCs and the tumor vasculature (Lathia et al. 2010). Previous studies have implicated growth factors (Bao et al. 2006b), laminins and cell-to-cell signaling (Calabrese et al. 2007) in the regulation of GPCs, demonstrating the maintenance of GPCs by the ECM present in the perivascular niche via integrin α6. Targeting integrin α6 decreases GPC survival and tumorigenic potential. Another secreted factor produced by the tumor microenvironment is the cytokine interleukin 6 (IL6). IL6 expression is highly correlated with tumor propagation as well as poor clinical outcome in GBM (Wang et al. 2009). Knockdown of IL6 impairs GPC proliferation, demonstrating the key role of IL6 autocrine signals in GPC phenotype. Importantly, administration of anti-IL6 antibody delayed the growth of tumors initiated with GPCs. These data strongly suggest that targeting IL6 may be useful as anti-glioma therapies.
In gliomas of higher malignancy grade, the blood brain barrier (BBB) gets leaky, because tumors can actively degrade tight junctions by secreting soluble factors. However, drug uptake remains restricted as new vessels formed by GBM-released VEGFs are leaky, resulting in accumulating interstitial pressure and restricted oxygen tension. As such, this hostile microenvironment represents a serious obstacle for drug penetration. A second niche where GPCs are concentrated is the perinecrotic hypoxic microenvironment. Low oxygen levels (i.e. hypoxia) activates pro-apoptotic and pro-angiogenic pathways, and drive tumor progression by triggering a set of adaptive transcriptional response that regulates tumor angiogenesis, metabolism, migration, response to changes in redox status in the niche and tumor survival. As hypoxia promotes stem cell maintenance, the critical role of hypoxia in defining cellular sensitivity to radiation may entwine with stem cell maintenance and therapeutic resistance. The extent of hypoxia has been shown to associate with poorer patient survival, therapeutic resistances and aggressive glioma phenotype. Resistance to the chemotherapeutic TMZ has been linked to hypomethylation and overexpression of MGMT in the hypoxic regions within gliomas, suggesting that restricted oxygenation levels may be critical for the GPC response to DNA-damage inducing agents and cells that reside in hypoxic niches may be better suited to evade such treatment. The complexity of vasculature and high flux of oxygen status has been observed to correlate with radiation resistance, making it highly challenging to directly disrupt the hypoxic niche.
A more effective approach would therefore be to target the canonical hypoxia responsive pathways, mediated through the hypoxia inducible factors (HIFs), which are in turn regulated by prolyl hydroxylase (PHD) family. Restricted oxygen has also been shown to play an integral role in GPC maintenance and function, contributing to the formation of both GPC and non-stem-like neurospheres, with concomitant upregulation of stemness-related genes such as SOX2 and OCT4. Current studies have revealed that both HIF1α and HIF2α are critical for GPC function and tumor propagation. HIF1α is involved in maintaining the self-renewal ability of the GPC population as stabilization of the protein expands the GPC population in a bulk tumor, mediated by central oncogenic pathways such as PI3K/Akt, epidermal growth factor receptor (EGFR) and the Extracellular signaling Related Kinase (ERK) 1/2 pathways. Recent studies have shown that HIF-1 regulates tumor radioresponses by either sensitizing tumor cells to radiation through induction of ATP metabolism, proliferation, and p53 activation or by increased survival of endothelial cells. Regrettably, HIF1α is critical for the normal function of neural progenitor cells as well as normal endothelial cells, thus limiting its therapeutic index (Li et al. 2009). In contrast, HIF2α has recently emerged as a potential therapeutic target for GPCs, with response to a broader range of oxygen tensions compared to HIF1α, enabling the capability to adapt to a highly dynamic microenvironment. A recent study revealed that HIF2α is preferentially expressed in the GPC population without expression in normal progenitors (Li et al. 2009) and self-renewal ability of GPCs was abrogated upon HIF2α knockdown. HIF2α can also promote a more tumorigenic phenotype in non-stem glioma cells, driving the expression of genes involved in core stem cell pathways such as Oct4, c-myc and Nanog (Heddleston et al. 2009). Further substantiation data was extrapolated from the REMBRANDT database where patients with higher expression of HIF2α mRNA resulted in poorer survival. Due to a clear reliance of GPCs on HIF proteins for their survival, there is compelling evidence for HIF2α as a therapeutic target that could impair GPC responses to the hypoxic microenvironment via disruption of the niche using drugs such as the aminoglycoside digoxin. However the caveat to digoxin administration is that they indiscriminately target both HIF1α and HIF2α, thereby resulting in off-target effects in normal neural progenitors. More effective pharmacological inhibitors must thus be developed to specifically target HIF2α for more efficient clinical treatment and improved patient survival.
The contributions of extracellular tumor states may also be critical for maintaining GPC function and mediating therapeutic resistance. Acidic stress has been shown to induce plasticity in non-stem GBM cells, making them more GPC-like (Hjelmeland et al. 2011). Following exposure to physiologic tumor pH of 6.5, expression of stemness-related genes are upregulated with concurrent increase in tumorigenic potential. Elevation of pH reverts the induction of HIF2 and other GPC markers by acidic stress, suggesting that increasing intratumoral pH may be a conceivable strategy to eradicate GPCs. Subsequent to GPC targeted therapies, intrinsic cues in the GPC niche may reform a subset of GPCs to maintain tumor cell homeostasis. Hence, targeting the acidic microenvironment, through restoration of a neutral pH, followed by GPC-specific treatment may be an effective anticancer stem cell therapy.
Escape mechanisms directing adaptation and tumor progression include migration of tumor cells or intercellular communication with tumor niche, ECM secreted factors and viable circulating endothelial cells (CECs). However, adaptation forces resulting from microenvironmental influences of hypoxia, vascularity, acidic stress, starvation, exogenous growth factors, and altered responses to endogenous growth factors as well as exogenous factors including therapeutic interventions, must be evaluated. These complexities underscore the pressing need to identify the intercellular communications between resident cell types in the perivascular niche of brain tumors, the diverse cell population and signaling factors involved in maintaining the GPC phenotype within this niche so as to unravel mechanism of therapeutic resistance.
Molecular Classification
In 2006, the National Cancer Institute initiated an effort to deep profile, as one of the first cancers, glioblastoma multiforme, because of its dismal prognosis despite advanced surgical intervention and adjuvant chemotherapy and radiation treatment. This effort is predicated on the belief that histologically similar tumors can be molecularly heterogeneous, and that distinct pathways drive the biological phenotype. The first publication arising from The Cancer Genome Atlas (TCGA) effort showed that patients with GBM sustain mutations that can be grouped into three major signaling networks: Receptor tyrosine kinases (RTKs), p53 and Retinoblastoma tumor suppressor pathways. Importantly, GBM tumors are molecularly heterogeneous, further highlighting the limitations of relying solely on morphology-based histological methods to diagnose and subsequently treat patients. A follow-up study then showed that GBM tumors can be molecularly classified into four subgroups (Proneural, Classical, Mesenchymal, Neural), with each subgroup containing unique gene expression, genomic aberrations and clinical profile. A major inference from such studies is that GBM patients can now potentially be treated according to their molecular subclasses and pathway activation. Indeed, it is known through pharmacological targeting in a panel of GBM cell lines that co-deletion of CDKN2A and CDKN2C served as a strong predictor of sensitivity to a selective inhibitor of CDK4/6. This mapped to similar patterns of CDKN2A and CDKN2C mutations in TCGA patients, leading to hyperactivated CDK4/6. The Wiedemeyer study thus demonstrates that the integration of genomic, functional and pharmacologic data can be exploited to inform the development of targeted therapy directed against specific cancer pathways. Importantly, the TCGA effort emphasizes that gene expression drives GBM disease progression and patient survival outcome.
In assessing the contribution of GPCs to the primary tumor phenotype, several studies have focused on analyzing common GPC marker expression in tissue paraffin sections, often with ambiguous data. This may be reconciled by the fact that GPC properties that sustain the tumor phenotype may reside in more than just specific marker profiles. Consequently, pathway activation resembling those functioning in stem-like cells, represented by a set of genes, is more likely to correctly interrogate the clinical contribution of GPCs. Some information is available regarding BRCA1 mutation-associated breast tumors. Based on this information differentially regulated genes in subsets of epithelial cells can be derived and luminal progenitors are highly represented in BRCA1 mutation-associated basal tumors, even more than the commonly anticipated stem cell population. This suggests that luminal progenitors are more likely the cells-of-origin for BRCA1 mutation-associated breast cancers, later confirmed in a transgenic mouse model study. Such studies underscore the predictive ability of gene expression mapping of pathway activation, rather than focus on a specific marker identity. It is known that serial tumor-propagating (and not marker-defined) acute myeloid leukemia stem cells contribute to disease progression and patient survival outcome, highlighting the importance of functionally defining the cancer stem cell. Two other more relevant studies demonstrated that GPCs contribute to GBM patient survival outcome, with preferential activation of core stem cell programs (hematopoietic, neural and embryonic stem cells). The key message from such studies is that cancer stem cells perpetuate tumors not merely in terms of their cell numbers, but more accurately reflected by their pathway activation. Consequently, the primary tumor phenotype is a manifest of cancer stem cell behavior and signaling.
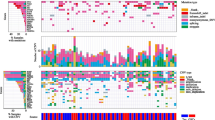
In conclusion, understanding the regulatory pathways of GPCs and the influence of their microenvironmental niche is crucial and is likely to contribute to disease progression and clinical outcome. Several primary resistance mechanisms of GPCs, such as the multi-drug resistance family of proteins (e.g. ABCB1and ABCG2), DNA damage repair pathways (e.g. CD133, L1CAM and MGMT), and self-renewal mechanisms (e.g. Notch, Hedgehog-Gli, Wnt/β-catenin and EGFR/PI3K/AKT axis) typified in normal stem cells, as well as the microenvironmental niche (including VEGF/SDF-1, Integrin α6, IL-6 and HIF2) have demonstrated to play critical roles in the development of radio- and chemoresistance in GPCs (Fig. 7.1 and Table 7.1). The cancer stem cell theory presents a paradigm in therapeutic design towards a long-lasting and effective cure.
Mechanisms implicated in the chemoresistance and radioresistance of glioma propagating cells (GPCs). GPCs are regulated at multiple levels by a complex network of pathways. Self-renewal signals are mainly contributed by Notch, Hedgehog, Wnt and EGF pathways. Mechanisms that mediate radio- and chemo-resistance in GPCs include ABC family of drug transporters and DNA repair pathways. Multiple environmental cues e.g. hypoxia, ECM, VEGF exert additional support to the maintenance of GPCs and provide resistance to conventional therapeutics
References
Bao S, Wu Q, McLendon RE, Hao Y, Shi Q, Hjelmeland AB, Dewhirst MW, Bigner DD, Rich JN (2006a) Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature 444:756–760
Bao S, Wu Q, Sathornsumetee S, Hao Y, Li Z, Hjelmeland AB, Shi Q, McLendon RE, Bigner DD, Rich JN (2006b) Stem cell-like glioma cells promote tumor angiogenesis through vascular endothelial growth factor. Cancer Res 66:7843–7848
Bar EE, Chaudhry A, Lin A, Fan X, Schreck K, Matsui W, Piccirillo S, Vescovi AL, DiMeco F, Olivi A, Eberhart CG (2007) Cyclopamine-mediated hedgehog pathway inhibition depletes stem-like cancer cells in glioblastoma. Stem Cells 25:2524–2533
Bleau AM, Hambardzumyan D, Ozawa T, Fomchenko EI, Huse JT, Brennan CW, Holland EC (2009) PTEN/PI3K/Akt pathway regulates the side population phenotype and ABCG2 activity in glioma tumor stem-like cells. Cell Stem Cell 4:226–235
Calabrese C, Poppleton H, Kocak M, Hogg TL, Fuller C, Hamner B, Oh EY, Gaber MW, Finklestein D, Allen M, Frank A, Bayazitov IT, Zakharenko SS, Gajjar A, Davidoff A, Gilbertson RJ (2007) A perivascular niche for brain tumor stem cells. Cancer Cell 11:69–82
Cheng L, Wu Q, Huang Z, Guryanova OA, Huang Q, Shou W, Rich JN, Bao S (2011) L1CAM regulates DNA damage checkpoint response of glioblastoma stem cells through NBS1. EMBO J 30:800–813
Chua C, Zaiden N, Chong KH, See SJ, Wong MC, Ang BT, Tang C (2008) Characterization of a side population of astrocytoma cells in response to temozolomide. J Neurosurg 109:856–866
Clement V, Sanchez P, de Tribolet N, Radovanovic I, Ruiz i Altaba A (2007) HEDGEHOG-GLI1 signaling regulates human glioma growth, cancer stem cell self-renewal, and tumorigenicity. Curr Biol 17:165–172
Cui D, Xu Q, Wang K, Che X (2010) Gli1 is a potential target for alleviating multidrug resistance of gliomas. J Neurol Sci 288:156–166
Ehtesham M, Sarangi A, Valadez JG, Chanthaphaychith S, Becher MW, Abel TW, Thompson RC, Cooper MK (2007) Ligand-dependent activation of the hedgehog pathway in glioma progenitor cells. Oncogene 26:5752–5761
Eyler CE, Foo WC, LaFiura KM, McLendon RE, Hjelmeland AB, Rich JN (2008) Brain cancer stem cells display preferential sensitivity to Akt inhibition. Stem Cells 26:3027–3036
Fan X, Khaki L, Zhu TS, Soules ME, Talsma CE, Gul N, Koh C, Zhang J, Li YM, Maciaczyk J, Nikkhah G, Dimeco F, Piccirillo S, Vescovi AL, Eberhart CG (2010) NOTCH pathway blockade depletes CD133-positive glioblastoma cells and inhibits growth of tumor neurospheres and xenografts. Stem Cells 28:5–16
Folkins C, Shaked Y, Man S, Tang T, Lee CR, Zhu Z, Hoffman RM, Kerbel RS (2009) Glioma tumor stem-like cells promote tumor angiogenesis and vasculogenesis via vascular endothelial growth factor and stromal-derived factor 1. Cancer Res 69:7243–7251
Gilbertson RJ, Rich JN (2007) Making a tumour’s bed: glioblastoma stem cells and the vascular niche. Nat Rev Cancer 7:733–736
Heddleston JM, Li Z, McLendon RE, Hjelmeland AB, Rich JN (2009) The hypoxic microenvironment maintains glioblastoma stem cells and promotes reprogramming towards a cancer stem cell phenotype. Cell Cycle 8:3274–3284
Hjelmeland AB, Wu Q, Heddleston JM, Choudhary GS, MacSwords J, Lathia JD, McLendon R, Lindner D, Sloan A, Rich JN (2011) Acidic stress promotes a glioma stem cell phenotype. Cell Death Differ 18:829–840
Hu YY, Zheng MH, Cheng G, Li L, Liang L, Gao F, Wei YN, Fu LA, Han H (2011) Notch signaling contributes to the maintenance of both normal neural stem cells and patient-derived glioma stem cells. BMC Cancer 11:82
Inda MM, Bonavia R, Mukasa A, Narita Y, Sah DW, Vandenberg S, Brennan C, Johns TG, Bachoo R, Hadwiger P, Tan P, Depinho RA, Cavenee W, Furnari F (2010) Tumor heterogeneity is an active process maintained by a mutant EGFR-induced cytokine circuit in glioblastoma. Genes Dev 24:1731–1745
Lathia JD, Gallagher J, Heddleston JM, Wang J, Eyler CE, Macswords J, Wu Q, Vasanji A, McLendon RE, Hjelmeland AB, Rich JN (2010) Integrin alpha 6 regulates glioblastoma stem cells. Cell Stem Cell 6:421–432
Li Z, Bao S, Wu Q, Wang H, Eyler C, Sathornsumetee S, Shi Q, Cao Y, Lathia J, McLendon RE, Hjelmeland AB, Rich JN (2009) Hypoxia-inducible factors regulate tumorigenic capacity of glioma stem cells. Cancer Cell 15:501–513
Liu G, Yuan X, Zeng Z, Tunici P, Ng H, Abdulkadir IR, Lu L, Irvin D, Black KL, Yu JS (2006) Analysis of gene expression and chemoresistance of CD133+ cancer stem cells in glioblastoma. Mol Cancer 5:67
Mazzoleni S, Politi LS, Pala M, Cominelli M, Franzin A, Sergi Sergi L, Falini A, De Palma M, Bulfone A, Poliani PL, Galli R (2010) Epidermal growth factor receptor expression identifies functionally and molecularly distinct tumor-initiating cells in human glioblastoma multiforme and is required for gliomagenesis. Cancer Res 70:7500–7513
Nakai E, Park K, Yawata T, Chihara T, Kumazawa A, Nakabayashi H, Shimizu K (2009) Enhanced MDR1 expression and chemoresistance of cancer stem cells derived from glioblastoma. Cancer Invest 27:901–908
Ricci-Vitiani L, Pallini R, Biffoni M, Todaro M, Invernici G, Cenci T, Maira G, Parati EA, Stassi G, Larocca LM, De Maria R (2010) Tumour vascularization via endothelial differentiation of glioblastoma stem-like cells. Nature 468:824–828
Soda Y, Marumoto T, Friedmann-Morvinski D, Soda M, Liu F, Michiue H, Pastorino S, Yang M, Hoffman RM, Kesari S, Verma IM (2011) Transdifferentiation of glioblastoma cells into vascular endothelial cells. Proc Natl Acad Sci USA 108:4274–4280
Wang H, Lathia JD, Wu Q, Wang J, Li Z, Heddleston JM, Eyler CE, Elderbroom J, Gallagher J, Schuschu J, MacSwords J, Cao Y, McLendon RE, Wang XF, Hjelmeland AB, Rich JN (2009) Targeting interleukin 6 signaling suppresses glioma stem cell survival and tumor growth. Stem Cells 27:2393–2404
Wang J, Wakeman TP, Lathia JD, Hjelmeland AB, Wang XF, White RR, Rich JN, Sullenger BA (2010a) Notch promotes radioresistance of glioma stem cells. Stem Cells 28:17–28
Wang R, Chadalavada K, Wilshire J, Kowalik U, Hovinga KE, Geber A, Fligelman B, Leversha M, Brennan C, Tabar V (2010b) Glioblastoma stem-like cells give rise to tumour endothelium. Nature 468:829–833
Zhang N, Wei P, Gong A, Chiu WT, Lee HT, Colman H, Huang H, Xue J, Liu M, Wang Y, Sawaya R, Xie K, Yung WK, Medema RH, He X, Huang S (2011) FoxM1 promotes beta-catenin nuclear localization and controls Wnt target-gene expression and glioma tumorigenesis. Cancer Cell 20:427–442
Acknowledgements
The authors would like to acknowledge grant support to C. Tang (BMRC: 09/1/33/19/611) and Singapore Institute for Clinical Sciences (A*STAR) core funding to B.T. Ang.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Koh, L.W.H., Toh, T.B., Tang, C., Ang, B.T. (2014). Glioma Propagating Cells Show Enhanced Chemoresistance and Radioresistance (an Update). In: Hayat, M. (eds) Stem Cells and Cancer Stem Cells, Volume 11. Stem Cells and Cancer Stem Cells, vol 11. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-7329-5_7
Download citation
DOI: https://doi.org/10.1007/978-94-007-7329-5_7
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-7328-8
Online ISBN: 978-94-007-7329-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)