Abstract
Hospital-acquired infections (HAIs) pose a worldwide problem. They primarily concern intensive care, hematology-oncology, and surgical units. Coagulase-positive and coagulase-negative Staphylococci, especially their subgroups possessing the ability to develop resistance to methicillin, and Enterococci have a particular role in the etiology of HAIs. The aim of this study was to determine the therapeutic minimal inhibitory concentration (MIC) values for vancomycin and teicoplanin, two of the most commonly administered antibiotics in the treatment of infections caused by Staphylococci resistant to methicillin, and infections caused by Enterococci. The material analyzed included 200 bacterial strains collected from patients treated in the Intensive Care Unit, the Musculoskeletal Infections Unit, and Surgical Clinics of the Military Institute of Medicine in Warsaw, Poland. The study was conducted in accord with the European Committee for Antimicrobial Susceptibility Testing (EUCAST) criteria by means of the Etest® gradient strips. We demonstrate a full susceptibility of Staphylococci MSSA (methicillin susceptible Staphylococcus aureus), Staphylococci MRSA (methicillin resistant Staphylococcus aureus), and Enterococci to both antibiotics. Coagulase-negative Staphylococci had a higher sensitivity to vancomycin. Teicoplanin had a lower MIC than vancomycin against the analyzed strains of Enterococci. As regards the coagulase-negative Staphylococci, vancomycin had a lower MIC than teicoplanin. In conclusion, the study confirmed current recommendations on the use of vancomycin and teicoplanin in the treatment of infections caused by gram-positive bacteria, emphasizing the need for the determination of MIC values.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Hospital-acquired infections (HAIs) pose a worldwide problem. They primarily concern intensive care, hematology-oncology, and surgical units. The risk of nosocomial infections depends on the host characteristics, the number of interventions, invasive procedure, asepsis of techniques, the duration of stay in the hospital and inappropriate use of antimicrobials. Most often the endogenous flora of the patient, which may be altered because of hospitalization, is responsible for nosocomial infections (Jones 2010; Wisplinghof et al. 2004). Both coagulase-positive and coagulase-negative Staphylococci, especially their subgroups possessing the ability to develop resistance to methicillin, have a particular role in the etiology of HAIs (Piette and Verschragen 2009). Staphylococci spp. is commensal on human body surfaces and colonizes intravenous devices, which become a focus of infection in hospitalized individuals. Staphylococci spp. is responsible for nosocomial pneumonia, surgical site infections, bloodstream infections, and urinary tract infections (Jain and Agarwal 2009). Vancomycin remains the antibiotic of choice to treat methicillin-resistant Staphylococcus aureus (MRSA) infections (Pitz et al. 2011). However, due to a dramatic rise in MRSA infections and widespread use of vancomycin, which is known to have marginal tissue penetration and slow bacterial activity, MRSA strains with reduced susceptibility to vancomycin are emerging (Pitz et al. 2011). Several studies have already reported elevated minimal inhibitory concentration (MIC) for vancomycin in MRSA isolates, with MICs at the upper end of the susceptibility range (Lodise et al. 2008; Rybak et al. 2008; Hussain et al. 2002). There are increasing numbers of report indicating the emergence of vancomycin resistant Staphylococcus aureus (VRSA). Associated with this issue is the presence of heterogeneous vancomycin-intermediate Staphylococcus aureus (hVISA). These microorganisms are described as being susceptible to vancomycin, but contain a subpopulation that possesses a thicker cell wall and expresses resistance to vancomycin. Infections caused by hVISA are a growing concern in hospitals, resulting in prolonged bacteremia, endocarditis, and osteomyelitis and leading to vancomycin treatment failure (Cui et al. 2006, 2003).
Another group of Gram-positive pathogens that became a cause of HAIs in the 1990s are Enterococci spp. (Jones 2010; Wisplinghof et al. 2004). Enterococci spp. are intestinal commensals of humans and other animals, in addition to being isolated from environmental sources. During the past decades, enhanced prevalence of enterococcal infections emerged, such as bacteremia and urinary tract infections, along with multi-antimicrobial resistance, particularly vancomycin resistant enterococci (VRE) (Courvalin 2006; Cetinkaya et al. 2000). Among this group of bacteria, especially Enterococcus faecium has a mechanism for developing resistance to vancomycin. Six different glycopeptide-resistant phenotypes (VanA to VanE and VanG) have been described in enterococci, while VanA and VanB are of greatest clinical relevance. Strains resistant to vancomycin and teicoplanin have been assigned to Van A phenotype, while those susceptible to teicoplanin but resistant to vancomycin are considered as the VanB phenotype (Thierfelder et al. 2012; Courvalin 2006; Cetinkaya et al. 2000).
Therapeutic success in the treatment of infections depends not only on determining the susceptibility of given bacteria to antibiotics (determined on the basis of the upper cut-off level for MIC), but also on identifying absolute MIC value in a wide range of concentrations (Hryniewicz 2000). The aim of the present study was to determine the therapeutic MIC values for vancomycin and teicoplanin, two of the most commonly administered antibiotics in the treatment of infections caused by Staphylococci spp. and infections caused by Enterococci.
2 Methods
The study was approved by the Ethics Committee of the Military Institute of Medicine in Warsaw, Poland. The biological material analyzed was collected from patients treated in the Clinical Intensive Care Unit, the Musculoskeletal Infections Unit, and Surgical Clinics of the Military Institute of Medicine in Warsaw in the period April-July 2011. The source of the samples analyzed included cultures from blood (14 samples), bronchial tree (14 samples), peritoneal cavity (7 samples), wounds (123 samples), abscesses (20 samples), and ulcerations (22 samples). Two hundred strains of Gram-positive bacteria were subject to analysis, including 50 Enterococci strains (39 strains of Enterococcus faecalis cultured from blood – 1, peritoneal cavity – 4, wounds – 29, abscess – 1, ulcerations – 4; 11 strains of E. faecium cultured from peritoneal cavity – 3, wounds – 7, abscess – 1); 89 strains of Staphylococcal aureus MSSA (methicillin-susceptible S. aureus, cultured from blood – 7, bronchial tree – 8, wounds – 47, abscess – 13, ulcerations – 14); 24 strains of S. aureus MRSA (methicillin-resistant S. aureus, cultured from blood – 3, bronchial tree – 6, wounds – 12, abscess – 1, ulcerations – 2); and 37 strains of coagulase-negative Staphylococci, (cultured from blood – 3, wounds – 28, abscess – 4, ulcerations – 2; including 14 strains of MSCNS, methicillin-susceptible coagulase negative Staphylococcus and 23 strains of MRCNS, methicillin-resistant coagulase negative Staphylococcus).
The species of isolated bacterial strains were identified using the VITEK 2 system (bioMérieux, France) by means of GN cards, following the guidelines issued by the manufacturer. The strains which were identified were next subject to manual determination of MIC value of glycopeptides by means of Etest® gradient strips which measure the concentration of a given antibiotic on the Müeller-Hinton plates (bioMérieux, France). The range of concentrations analyzed, for both vancomycin and teicoplanin, was from 0.032 to 256.0 μg/mL. The analysis was carried out in compliance with recommendations from the National Reference Center for Drug Susceptibility of Microorganisms in Poland. The results of the research were interpreted in line with the European Committee on Antimicrobial Susceptibility Testing (EUCAST) criteria, which have been legally binding in Poland since 1 April 2011. Reference strains Staphylococcus aureus ATCC29213 and Enterococcus faecalis ATCC 29212 were used to control test strips. MIC limiting values used to classify a strain as either susceptible or resistant according to EUCAST guidelines are presented in Table 19.1. A commercial packet of Statsoft Statistica 9 was used to perform all calculations.
3 Results
Data regarding the exact number and type of particular bacterial strains, and their susceptibility or resistance to the glycopeptides studied are presented in Table 19.2. Table 19.3 illustrates the distribution of vancomycin and teicoplanin MIC values against different bacterial strains.
Data presented in Table 19.2 confirm high efficacy of both vancomycin and teicoplanin against Enterococci spp. and Staphylococci spp. However, as regards coagulase-negative Staphylococci, teicoplanin has not been effective towards 16.2 % of the bacterial strains analyzed.
According to the values presented in Table 19.4, teicoplanin exhibits lower MIC 50 and MIC 90 values in case of Enterococci. No such difference was noted as regards MRSA. MIC 50 of teicoplanin in regard to S. aureus MSSA was slightly lower. Large differences were observed for E. faecium, for which MIC 50 and MIC 90 values of teicoplanin were lower and thus more favorable. With regard to the coagulase-negative Staphylococci, vancomycin exhibited much lower MIC 50 and MIC 90 values than teicoplanin.
4 Discussion
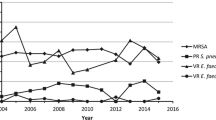
Our data indicate good susceptibility of Enterococci spp. and Staphylococci spp. to vancomycin, as none of isolated strains were resistant to it, which is consistent with the results obtained in other studies (Nimmo et al. 2011). Enterococci spp., MSSA and MRSA, were also fully susceptible to teicoplanin, while 16.2 % of coagulase-negative Staphylococci were resistant to it. The proportion of the coagulase-negative staphylococci resistant to teicoplanin in our study seems high when compared with that observed in other studies. Ma et al. (2011) found the increasing trend in the prevalence of strains of coagulase-negative Staphylococci non-susceptible to teicoplanin (from 4.5 to 6.7 %).
Our present results relating to coagulase-negative Staphylococci need to be discussed separately. The bacteria demonstrate exceptional ability to adhere to synthetic materials. Therefore, these materials are the main source of infection spread through central venous catheters and the like, inserted into the patient’s body. Such cases were reported in the Musculoskeletal Infections Unit, in which the cultures to be analyzed were collected from patients with artificial joints or those with fractures that had been stabilized using bonding materials. Out of the 37 strains of coagulase-negative Staphylococci, 23 developed resistance to methicillin. As mentioned above, 16.2 % of all studied coagulase-negative Staphylococci exhibited resistance to teicoplanin, which is a common phenomenon as regards this type of infections (Piette and Verschragen 2009). Our data presented in Table 19.4, where MIC 50 and MIC 90 values are lower for vancomycin than for teicoplanin, confirm the above statement. Data regarding susceptibility of MSSA to vancomycin and teicoplanin are of little clinical significance as administration of semi-synthetic penicillin or first-generation cephalosporins is a much better therapeutic choice (Piette and Verschragen 2009). According to our results, vancomycin is still a good antibiotic choice for patients suspected of infections with Enterococci spp. and Staphylococci spp.
In general, there is a wider range of possibilities for treating Gram-positive than Gram-negative bacterial infections. Currently, apart from the classic antibiotics, discussed in the present article, used to treat Gram-positive infections, new substances such as linezolid or tigecycline have been more commonly used. In addition, a number of new betalactam antibiotics, exhibiting high activity against MRSA, are under phase 2 and phase 3 clinical trials (Hryniewicz 2000). However, according to one of the published analyses, the effects of treating MRSA pneumonia with linezolid were no better than those produced by administration of vancomycin or teicoplanin (Kalil et al. 2010).
MRSA exhibiting reduced vancomycin susceptibility have recently been reported in many countries (Cui et al. 2003, 2006). In such a case, an increase in the dose of the antibiotic, even up to 4 g/24 h, may be required to achieve vancomycin concentration in the serum of 20–30 μg/mL (Smuszkiewicz et al. 2007). This situation was not observed while conducting the present study. The majority of the MRSA strains obtained from the patients proved to be susceptible to vancomycin and teicoplanin at equal values of MIC 50 and MIC 90. In response to increasing presence of vancomycin MICs and MRSA isolates, the Infectious Diseases Society of America, the American of Society of Health-Systems Pharmacists, and the Society of Infectious Diseases Pharmacists developed weight-based dosing recommendations for vancomycin based on pharmacokinetic and pharmacodynamic data (15–20 mg/kg i.v., every 12 h), but a recent multicenter study has not confirmed a reduced mortality rate associated with the empiric use of weight-based, guideline-recommended vancomycin dosing (Hall et al. 2012).
It has been previously discussed that nosocomial enterococcal infections pose a considerable health problem, especially if the source of infection is located in the lower part of the digestive tract. Enterococci accounted for 25 % of the isolates discussed in this article (including 39 strains of E. faecalis and 11 strains of E. faecium). According to the values presented in Table 19.2, teicoplanin is a better therapeutic choice in the treatment of enterococcal infections than vancomycin. The distribution of MIC values indicates that, regarding Enterococci (including E. faecium), the teicoplanin MIC 50 and MIC 90 values are much lower, and hence more favorable, compared with vancomycin. Teicoplanin is preferred in the treatment of enterococcal infections as it reduces the risk of a therapeutic failure, which may arise due to the emergence of VanB- and VanE-genotype resistance. Administration of vancomycin in such cases could facilitate the development of vancomycin-resistant of Enterococci. Teicoplanin penetrates into tissue more easily than vancomycin whose serum concentration in lungs amounts to 30 %. While studying the levels of teicoplanin in pulmonary alveoli mucus, it has been determined that the optimum therapeutic dose of intravenous teicoplanin is 12 mg/kg twice on the first day, followed by 12 mg/kg daily later on (Mimoz et al. 2006). In patients suffering from severe sepsis or a septic shock, who are given large volume of infusion fluids or receive catecholamines, penetration of a drug is reduced due to vessel shrinkage. As a result, the concentration of a drug in tissue is below the therapeutic level, although MIC values in the serum are satisfactory (Joukhadar 2001).
The present study confirmed current recommendations on the use of vancomycin and teicoplanin in the treatment of infections caused by Gram-positive bacteria, emphasizing the need for the determination of MIC values.
5 Conclusions
On the basis of MIC 50 and MIC 90 values the following conclusions can be drawn: (1) teicoplanin exhibits higher clinical efficacy in the treatment of infections caused by Enterococci; (2) efficacy of vancomycin and teicoplanin to S. aureus MSSA and MRSA is comparable; (3) vancomycin exhibits more favorable MIC values than teicoplanin in regard to the coagulase-negative Staphylococci.
References
Cetinkaya, Y., Falk, P., & Mayhall, C. (2000). Vancomycin-resistant enterococci. Clinical Microbiology Reviews, 19, 816–822.
Courvalin, P. (2006). Vancomycin resistance in gram-positive cocci. Clinical Infectious Diseases, 42, S25–S34.
Cui, L., Ma, K., Sato, M., Okuma, K., Tenover, F. C., Mamizuka, E. M., Gemmell, C. G., Kim, M. N., Ploy, M. C., El-Solh, N., Ferraz, V., & Hiramatsu, K. (2003). Cell wall thickening is a common feature of vancomycin resistance in Staphylococcus aureus. Journal of Clinical Microbiology, 41, 5–14.
Cui, L., Iwamoto, J., Neoh, H., Mruyama, T., Horikawa, Y., & Hiramatsu, K. (2006). Novel mechanisms of antibiotic resistance originating in vancomycin-intermediate Staphylococcus aureus. Antimicrobial Agents Chemotherapy, 50, 428–438.
Hall, R., Giuliano, C., Haase, K., Hazelwood, K., Frei, C., Forcade, N., Brouse, S., Bell, T., Bedimo, R., & Alvarez, C. (2012). Empiric guide-line-recommended weight-based vancomycin dosing and mortality in methicillin-resistant Staphylococcus aureus bacteraemia: A retrospective cohort study. BMC Infectious Diseases, 12, 104–124.
Hryniewicz, W. (Ed.). (2000). Contemporary views on resistance of bacteria to antibiotics. Infections in intensive care – the place and role of antibiotics (pp. 1–15). Wroclaw: Urban & Partner (in Polish).
Hussain, F., Boyle-Vavra, P., Shete, B., & Daum, R. (2002). Evidence for continuum of decreased vancomycin susceptibility in unselected Staphylococcus aureus clinical isolates. Journal of Infectious Diseases, 186, 661–667.
Jain, A., & Agarwal, A. (2009). Biofilm production, a marker of pathogenic potential of colonizing and commensal staphylococci. Journal of Microbiological Methods, 76, 88–92.
Jones, R. N. (2010). Microbial etiologies of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia. Clinical Infectious Diseases, 51(Suppl 1), S81–S87.
Joukhadar, C. (2001). Impaired target site penetration of b-lactams may account for therapeutic failure in patients with septic shock. Critical Care Medicine, 31, 2102–2109.
Kalil, A. C., Murthy, M. H., Hermsen, E. D., Neto, F. K., Sun, J., & Rupp, M. E. (2010). Linezolid versus vancomycin or teicoplanin for nosocomial pneumonia: A systematic review and meta-analysis. Critical Care Medicine, 38, 1802–1808.
Lodise, T., Grawes, A., Evans, A., Graffunder, E., Helmecke, M., Lomaestro, B., & Stellrecht, K. (2008). Relationship between vancomycin MIC and failure among patients with methicillin-resistant Staphylococcus aureus bacteremia treated with vancomycin. Antimicrobial Agents and Chemotherapy, 52, 3315–3320.
Ma, X., Wang, E., Liu, Y., & Luo, E. (2011). Antibiotic susceptibility of coagulase-negative staphylococci (CoNS): Emergence of teicoplanin-non-susceptible CoNS strains with inducible resistance to vancomycin. Journal of Medical Microbiology, 60, 1661–1668.
Mimoz, O., Rolland, D., Adoun, M., Marchand, S., Breilh, D., Brumpt, I., Debaene, B., & Couet, W. (2006). Steady-state trough serum and epithelial lining fluid concentrations of teicoplanin 12 mg/kg per day in patients with ventilator-associated pneumonia. Intensive Care Medicine, 32, 775–779.
Nimmo, G., Pearson, J., Collignon, P., Christiansen, K., Coombs, G., Bell, J., & McLaws, M. (2011). Australian group on antimicrobial resistance. Communicable Diseases Intelligence, 35(3), 237–243.
Piette, A., & Verschragen, G. (2009). Role of coagulase-negative staphylococci in human disease. Veterinary Microbiology, 134, 45–54.
Pitz, A., Yu, E., Hermsen, E., Rupp, M., Fey, P., & Olsen, M. (2011). Vancomycin susceptibility and prevalence of heterogeneous vancomycin-intermediate Staphylococcus aureus in clinical methicillin-resistant S. aureus isolates. Journal of Clinical Microbiology, 49(1), 269–274.
Rybak, M., Leonard, S., Rosii, C., Cheung, C., Sader, H., & Jones, R. (2008). Characterization of vancomycin-hetero resistant Staphylococcus aureus from the metropolitan area of Detroit, Michigan, over a 22-year period (1986 to 2007). Journal of Clinical Microbiology, 46, 2950–2954.
Smuszkiewicz, P., Szalek, E., Tomczak, H., Trojanowska, I., & Błaszyk, M. (2007). Pharmacokinetic and pharmacodynamic use of antibiotics in patients treated for sepsis. Anaesthesiology Intensive Therapy, 3, 166–174 (in Polish).
Thierfelder, C., Keller, P., Kocher, C., Gaudenz, R., Hombach, M., Bloemberg, G., & Ruef, C. (2012). Vancomycin-resistant Enterococcus. A multi-strain outbreak of eight weeks duration at a Swiss tertiary care hospital. Swiss Medical Weekly, 5, 1–6.
Wisplinghof, H., Bischoff, T., Tallent, S., Seifert, H., Wenzel, R., & Edmond, M. (2004). Nosocomial bloodstream infections in US hospitals: Analysis of 24,179 cases from a prospective national wide surveillance study. Clinical Infectious Diseases, 39, 309–317.
Acknowledgments
We thank Dr. Dariusz Tomaszewski from the Clinic of Anesthesiology and Intensive Care of the Military Institute of Medicine in Warsaw, for stylistic editing of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Guzek, A., Korzeniewski, K., Nitsch-Osuch, A., Rybicki, Z., Prokop, E. (2013). In Vitro Susceptibility of Staphylococci and Enterococci to Vancomycin and Teicoplanin. In: Pokorski, M. (eds) Neurobiology of Respiration. Advances in Experimental Medicine and Biology, vol 788. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-6627-3_19
Download citation
DOI: https://doi.org/10.1007/978-94-007-6627-3_19
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-6626-6
Online ISBN: 978-94-007-6627-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)