Abstract
MDM2 is a major negative regulator of p53 and in some tumors that present a wild type p53 gene deregulated expression of MDM2 could contribute to tumor development. In particular, in neuroblastoma, an extracranial pediatric tumor with unfrequent genetic inactivation of p53, deregulation of MDM2 could significantly decrease the activity of p53, resulting in failure of p53-regulated functions such as cell cycle arrest, apoptosis and senescence. A single nucleotide polymorphism (SNP309,T>G change; rs 2279744) in the MDM2 promoter increases the affinity for the transcription factor SP1, enhancing MDM2 expression and attenuating the activity of the p53 pathway. In this chapter, we review the role of MDM2 and its SNP309 on neuroblastoma development and progression and discuss future pharmacological approaches based on the presence of this polymorphism.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Neuroblastoma, a tumor arising from neuroectodermal precursor cells of the neural crest, represents the most common extracranial solid tumor in children, accounting for 8–10% of all childhood cancers but for 15% of all deaths due to pediatric malignancies (Maris et al. 2007). The clinical hallmark of neuroblastoma is its heterogeneity: age at diagnosis (Breslow and McCann 1971), clinical stage (based on International Neuroblastoma Staging System; Brodeur et al. 1993), and tumor histology (Shimada et al. 1999) are the most important factors for predicting the course of the disease and modulate the treatment accordingly. Age at diagnosis >1 year, advanced stage (3 and 4) and unfavorable histology are predictive of adverse outcome, but the response to treatment in patients with neuroblastoma is quite variable, probably reflecting differences in biological characteristics of tumor cells. Several biological markers related to outcome have been identified and they have further improved risk stratification. MYCN oncogene amplification, hemizygous deletions of chromosomal region 1p36, and unbalanced gain of 17q regions are the most common genomic aberrations in neuroblastoma (Maris and Matthay 1999). MYCN oncogene is amplified in 20% of cases and represents the most powerful marker of poor outcome (Komuro et al. 1993). In contrast with other malignancies, only 2–3% of neuroblastomas harbor mutations of the p53 gene (Imamura et al. 1993). p53 is a tumor suppressor gene activated by cellular stresses such as DNA damage, hypoxia, cold and heat shock that, primarily through its transcription activation function, is involved in many biological processes such as cell cycle arrest, apoptosis, and cellular senescence (Sharpless and DePinho 2002). Alteration of such processes has important implications for clinical behavior and response to treatment. p53 also activates the transcription of the MDM2 gene that encodes the major negative regulator of p53, thereby generating a negative feedback loop that leads to inhibition of p53 activity and proteasome-dependent protein degradation (Piette et al. 1997). Different studies in neuroblastoma cell lines and primary tumors have shown that the p53/MDM2 pathway is genetically intact, but that the function of p53 may be attenuated by aberrant expression/activity of MDM2 (Maris and Matthay 1999; Rodriguez-Lopez et al. 2001). In this regard, MDM2 expression can be enhanced by increased MYCN levels in tumors with MYCN amplification (Slack et al. 2005b), whereas in tumors with the 1p36 deletion expression of an activator of ARF (alternate reading frame) (which interacts with MDM2) is reduced (Bagchi et al. 2007), possibly enhancing MDM2 functional levels. A single nucleotide polymorphism (SNP309) in the first intron of MDM2 causes an increase in the affinity for SP1, a transcription factor able to increase MDM2 mRNA and protein level and, consequently, an attenuation of the p53-regulated pathways that increase the risk for tumorigenesis (Bond et al. 2004). Because mutations of the p53 gene are rarely found in neuroblastoma (Imamura et al. 1993), it is an intriguing possibility that a more aggressive neuroblastoma might develop in individuals harboring MDM2 SNP309 variants that promote functional inactivation of p53.
Murine Double Minute Gene 2
MDM2 (murine double minute gene 2), also known as HDM2 in humans, is one of the most important negative regulator of tumor suppressor p53. MDM2 was first described as one of the genes amplified in double minute chromosomes present in the spontaneously transformed Balb/c3T3 murine cell line 3T3DM (Cahilly-Snyder et al. 1987). MDM2 encodes a 90-kDa protein that comprises several distinct, highly conserved regions. The N-terminal domain harbors the main p53 binding interface. Two other notable regions of MDM2 are the central domain (amino acids ∼200–300), often referred to as the acidic domain (AD), and the C-terminal RING (really interesting new gene) domain (amino acids 438–478). The latter functions as an E3 ligase responsible for p53 ubiquitylation. Like other RING domain proteins, the MDM2 RING has intrinsic E3 ubiquitin ligase activity, in that it can promote the transfer of ubiquitin molecules from an E2 conjugating enzyme directly to lysine residues of target substrates (Deshaies and Joazeiro 2009). MDM2 functions as a homodimer or forms heterodimers with MDMX (also known as MDM4 and HDMX) through their RING fingers and both types of dimers are active as E3s (Lipkowitz and Weissman 2011). When wild-type p53 is activated by various stimuli such as DNA damage, MDM2 binds to p53 (that is in form of tetramer) at the N-terminus to inhibit the transcriptional activation of p53 and directs the export of p53 away from its site of action in the nucleus to the cytoplasm, thanks to a central nuclear export signal and promote the degradation of p53 via ubiquitin-proteasome pathway generating a negative feedback loop.
Up to 50% of malignancies retain wild-type p53 and in most of these there is increased MDM2 activity towards p53 as a consequence of amplification of MDM2, increased MDM2 expression due to promoter hyperactivity, gene polymorphisms, alterations in ARF activity or other mechanisms (Lipkowitz and Weissman 2011). Amplification and overexpression of MDM2 is found in about 10% of all human tumors (Ganguli and Wasylyk 2003). In gliomas, for example, MDM2 amplification identifies a subset of high-risk patients that do not have p53 mutations (Slack et al. 2005a). In many soft tissue sarcomas, MDM2 amplification and overexpression correlates with poor prognosis (Slack et al. 2005a). Studies of acute lymphoblastic leukemia and non-Hodgkin’s lymphoma also demonstrate that MDM2 overexpression is associated with poor survival and aggressive disease (Slack et al. 2005a). Thus, deregulation of MDM2 gene expression likely contributes to the pathogenesis of a wide range of human tumors.
Murine Double Minute Gene 2 in Neuroblastoma
Different studies in neuroblastoma cell lines and primary tumors have shown that p53 is generally functional, accumulates in the nucleus in response to DNA damage and is efficiently degraded by MDM2 (Tweddle et al. 2001). Some reports strongly suggest that p53 function may be compromised as a consequence of aberrant MDM2 expression. The activity of MDM2 is critical in neuroblastoma, as the MDM2 ubiquitin ligase activity seems to be rate-limiting for p53 degradation (Isaacs et al. 2001). Consistent with the notion that MDM2 levels regulate p53 activity, a study examining etoposide-induced p53 activity in neuroblastoma cells suggested an important role for elevated MDM2 expression levels in the regulation of p53 translocation (Rodriguez-Lopez et al. 2001). Indeed, in SH-EP cells, which express high levels of MDM2, p53 accumulates in the cytoplasm upon exposure to etoposide. However, antisense oligodeoxynucleotide inhibition of MDM2 restored p53 nuclear localization and apoptotic activation, suggesting that increased MDM2 expression levels can play a role in the inappropriate modulation of p53 function (Rodriguez-Lopez et al. 2001). Additionally, elevated MDM2 expression and the accompanying loss of p53 function are associated with multidrug resistance in some neuroblastoma cell lines (Keshelava et al. 2001). Together, these data demonstrate that the MDM2/p53 pathway is intact in neuroblastoma and suggest that deficiencies in p53 functions may be a consequence of aberrant MDM2 expression. In neuroblastomas with MYCN amplification, increased expression/activity of MDM2 as an effector of MYCN (Slack et al. 2005a) could significantly decrease the activity of p53, resulting in failure to undergo appropriate cell cycle arrest and apoptosis. Recent studies (see below) show that MDM2 can be involved in neuroblastoma development if harbors single nucleotide polymorphism variants (such as SNP309) that increase its expression and promote functional inactivation of p53.
Single Nucleotide Polymorphisms in Genes Relevant for Neuroblastoma
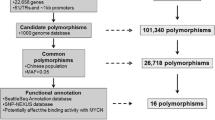
In recent years, there has been an increasing interest in identifying and assessing the frequency of gene variants (polymorphisms) as a tool to predict inter-individual cancer risk and response to cancer therapies (Dong et al. 2008). A polymorphism is defined as a DNA sequence change that occurs in a significant proportion (more than 1%) of a large population (Olivier et al. 2002). The most common type of genetic variation is a single nucleotide polymorphism (SNP). The p53 and MDM2 genes both present several SNPs that appear to modify their expression/activity. p53 is a tumor suppressor gene which is activated by cellular and genomic stresses such as DNA damage, oncogene mutation, hypoxia, cold and heat shock and is involved in many biological processes such as cell cycle arrest, apoptosis, and cellular senescence (Sharpless and DePinho 2002). The effects of p53 are, mostly, transcription-dependent as it binds DNA in a sequence-specific manner to enhance the transcription of a number of genes, including p21WAF1, MDM2 and BAX. WAF1 inhibits G1 cyclin-dependent kinases, blocking cell cycle progression from G1 into S phase. In tumor cells, the selective pressure to delete or inactivate p53 is very high. This primarily occurs through amplification/overexpression of its inhibitors like MDM2, MDM4 (MDM2 family member) and loss or inactivation of upstream activators such as p14ARF (p19ARF in mice) and p16INK4a (Toledo and Wahl 2006). Different combinations of these events diminish or abolish wild type p53 levels and activity leading to defective apoptosis, uncontrolled proliferation, and cellular transformation. For the p53 gene, a SNP has been identified within exon 4 at codon 72 causing an Arg>Pro substitution (Matlashewski et al. 1987). The p53-72R isoform appears to be more potent than the p53-72P isoform in inducing apoptosis, and among the proposed mechanisms that may be responsible for such an effect are increased mitochondrial localization and reduced affinity of the p53-72R isoform for the p53 inhibitor iASPP (Dumont et al. 2003; Bergamaschi et al. 2006).
Different studies in neuroblastoma cell lines and primary tumors have shown that the p53/MDM2 pathway is genetically intact, but that the function of p53 may be attenuated by aberrant expression/activity of MDM2 (Rodriguez-Lopez et al. 2001). In this regard, MDM2 expression can be enhanced by increased MYCN levels in tumors with MYCN amplification (Slack et al. 2005b), whereas in tumors with the 1p36 deletion expression of an activator of ARF (alternate reading frame) (which interacts with MDM2) is reduced (Bagchi et al. 2007), possibly enhancing MDM2 functional levels. In the first intron of MDM2, there is one of the two gene promoter enhancers (the other one is in the first exon; Bond et al. 2005). In humans, the first intron consists of a 524-nucleotide segment that includes two different single nucleotide polymorphisms (SNP; Bond et al. 2005). One of these, the SNP309 (a T>G change at nucleotide 309; rs 2279744), causes a fourfold increase in the affinity of the promoter for the transcription factor SP1, resulting in higher levels of MDM2 mRNA and protein, attenuation of the p53-regulated pathways, and increased risk for tumorigenesis (Bond et al. 2004).
Single Nucleotide Polymorphism 309 Incidence in Neuroblastoma and Disease Progression
The influence of MDM2 SNP309 in neuroblastoma incidence and disease progression is a recent object of investigation. Until now, only few reports have investigated the relationship of MDM2 SNP309 to neuroblastoma (Cattelani et al. 2008; Perfumo et al. 2008, 2009) and all are based on Italian cohorts of patients.
A first study performed by Cattelani et al. (2008) in a cohort of 239 primary and untreated neuroblastoma patients assessed whether the frequency of the SNP309 in neuroblastoma patients was associated with variables predictive of poor outcome such age at diagnosis >1 year, adrenal primary site, advanced clinical stage (3 and 4), MYCN amplification, and chromosome 1p status (deletion or imbalance). They found a significant association (P =0.016; two-sided Fisher’s Exact Test) between heterozygous (T/G) and homozygous (G/G) variant genotypes at SNP309 and advanced clinical stage. Cumulative Kaplan Meier 5-year overall survival in neuroblastoma patients with the T/G and G/G variants of SNP309 was shorter than in those with the predominant T/T variant (P = 0.046; log-rank test), suggesting that, in its homozygous (G/G) or heterozygous (T/G) form, the SNP309 might be a novel indicator of poor outcome in neuroblastoma.
A successive study performed by Perfumo et al. (2009) in a larger cohort of neuroblastoma patients (n = 437) confirmed that the presence of the G/G or T/G SNP309 correlates with poor survival in particular in stage 4 disease.
The impact of the MDM2 SNP309 genotypes on overall survival, event free survival and survival after relapse was evaluated by the Cox regression model, while survival curves were obtained by the Kaplan–Meier method. Analyses were performed both on the whole cohort and after stratifying by stage at diagnosis, grouping patients with a localized disease (i.e., stage 1–3). Finally, a stratified analysis by patients’ clinical and biological characteristics was also carried out, and differences in survival probabilities by MDM2 SNP309 status were assessed by the log-rank test.
The results show that in stage 4 patients, the TG/GG polymorphism was correlated with a poorer outcome in particular among children with MYCN amplification. This effect was more evident for overall survival and survival after relapse than for event free survival, suggesting that the G allele is mainly associated with the progression of the disease instead of an increased risk of relapse.
All these studies strongly suggest that MDM2 SNP309 may be an independent prognostic factor for neuroblastoma, whose impact is restricted to survival of stage-4 patients and is particularly evident in those with MYCN amplified tumors.
These results indicate that the MDM2 SNP309 G allele is associated with significantly worse survival even in the presence of MYCN amplification. This observation suggests that targeting the MDM2/p53 circuit could represent an effective strategy for the treatment of such patients. In fact, the MDM2 SNP309 G allele, which is predicted to achieve higher expression of MDM2, as observed in various cell line models (Bond et al. 2004), could attenuate the p53 response pathway possibly contributing to resistance to genotoxic chemotherapy in p53 wild-type neuroblastoma cells. Hence, targeting MDM2 expression levels or the MDM2/p53 proteins interaction to obtain p53 stabilization could make neuroblastoma cells more sensitive to genotoxic drugs.
Conclusions
The biological characteristics of neuroblastoma suggest that targeting the molecular interaction of MDM2 and p53 may be an effective therapeutic strategy. As noted, the majority of neuroblastomas are p53 wild type and therefore dependent on MDM2 regulation of p53 to prevent apoptotic cell death. In several other tumor models, inhibition of MDM2 leads to increased p53 activity and triggers an apoptotic stress response (Vassilev et al. 2004; Zhang et al. 2004). In neuroblastoma cell lines, it has been recently demonstrated that down-regulation of MYCN leads to decreased MDM2 expression, p53 stabilization and subsequent rapid cell death. Since MYCN also sensitizes cells to apoptotic stress, neuroblastoma should be particularly sensitive to targeted disruption of the MDM2/p53 interaction in vivo. The MDM2 SNP309 G allele is associated with significantly worse survival even in the presence of MYCN amplification. This observation suggests that also in this case targeting the MDM2/p53 circuit could represent an effective strategy for the treatment of such patients. In fact, the MDM2 SNP309 G allele, which is predicted to achieve higher expression of MDM2, as observed in various cell line models (Bond et al. 2004), could attenuate the p53 response pathway possibly contributing to the resistance to genotoxic chemotherapy in p53 wild-type neuroblastoma cells.
MDM2 as a drug target is the topic of extensive reviews and is an active area of research. Notably, treatment of p53 wild-type neuroblastoma cells with the small molecule MDM2 antagonist nutlin-3 resulted in activation of the p53 pathway leading to cell cycle arrest and apoptosis (Van Maerken et al. 2006).
Hence, targeting MDM2 expression levels or the MDM2/p53 proteins interaction to obtain p53 stabilization could make neuroblastoma cells more sensitive to genotoxic drugs. The unique developmental biology of neuroblastoma suggests that targeting MDM2 could be an effective therapy, especially in the context of MYCN-driven tumors or in presence of MDM2 SNP309 polymorphism. The future evaluation of such approaches will advance our understanding of neuroblastoma pathogenesis and hopefully lead to important clinical advances for this highly fatal pediatric malignancy.
References
Bagchi A, Papazoglu C, Wu Y, Capurso D, Brodt M, Francis D, Bredel M, Vogel H, Mills AA (2007) CHD5 is a tumor suppressor at human 1p36. Cell 120:459–475
Bergamaschi D, Samuels Y, Sullivan A, Zvelebil M, Breyssens H, Bisso A, Del Sal G, Syed N, Smith P, Gasco M, Crook T, Lu X (2006) iASPP preferentially binds p53 proline-rich region and modulates apoptotic function of codon 72-polymorphic p53. Nat Genet 38:1133–1141
Bond GL, Hu W, Bond EE, Robins H, Lutzker SG, Arva NC, Bargonetti J, Bartel F, Taubert H, Wuerl P, Onel K, Yip L, Hwang SJ, Strong LC, Lozano G, Levine AJ (2004) A single nucleotide polymorphism in the MDM2 promoter attenuates the p53 tumor suppressor pathway and accelerates tumor formation in humans. Cell 119:591–602
Bond GL, Hu W, Levine A (2005) A single nucleotide polymorphism in the MDM2 gene: from a molecular and cellular explanation to clinical effect. Cancer Res 65:5481–5484
Breslow N, McCann B (1971) Statistical estimation of prognosis for children with neuroblastoma. Cancer Res 31:2098–2103
Brodeur GM, Pritchard J, Berthold F, Carlsen NL, Castel V, Castelberry RP, De Bernardi B, Evans AE, Favrot M, Hedborg F (1993) Revisions of the international criteria for neuroblastoma diagnosis, staging and response to treatment. J Clin Oncol 11:1466–1477
Cahilly-Snyder L, Yang-Feng T, Francke U, George DL (1987) Molecular analysis and chromosomal mapping of amplified genes isolated from a transformed mouse 3 T3 cell line. Somat Cell Mol Genet 13(3):235–244
Cattelani S, Defferrari R, Marsilio S, Bussolari R, Candini O, Corradini F, Ferrari-Amorotti G, Guerzoni C, Pecorari L, Menin C, Bertorelle R, Altavista P, McDowell HP, Boldrini R, Dominici C, Tonini GP, Raschellà G, Calabretta B (2008) Impact of a single nucleotide polymorphism in the MDM2 gene on neuroblastoma development and aggressiveness: results of a pilot study on 239 patients. Clin Cancer Res 14:3248–3253
Deshaies RJ, Joazeiro CAP (2009) RING domain E3 ubiquitin ligases. Annu Rev Biochem 78:399–434
Dong LM, Potter JD, White E, Ulrich CM, Cardon LR, Peters U (2008) Genetic susceptibility to cancer: the role of polymorphisms in candidate genes. JAMA 299:2423–2436
Dumont P, Leu JI, Della Pietra AC 3rd, George DL, Murphy M (2003) The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat Genet 33:357–365
Ganguli G, Wasylyk B (2003) p53-independent functions of MDM2. Mol Cancer Res 1:1027–1035
Imamura J, Bartram CR, Berthold F, Harms D, Nakamura H, Koeffler HP (1993) Mutation of the p53 gene in neuroblastoma and its relationship with N-myc amplification. Cancer Res 53:4053–4058
Isaacs JS, Saito S, Neckers LM (2001) Requirement for HDM2 activity in the rapid degradation of p53 in neuroblastoma. J Biol Chem 276:18497–18506
Keshelava N, Zuo JJ, Chen P, Waidyaratne SN, Luna MC, Gomer CJ, Triche TJ, Reynolds CP (2001) Loss of p53 function confers high-level multidrug resistance in neuroblastoma cell lines. Cancer Res 61:6185–6193
Komuro H, Hayashi Y, Kawamura M, Hayashi K, Kaneko Y, Kamoshita S, Hanada R, Yamamoto K, Hongo T, Yamada M (1993) Mutations of the p53 gene are involved in Ewing’s sarcomas but not in neuroblastomas. Cancer Res 53:5284–5288
Lipkowitz S, Weissman AM (2011) RINGs of good and evil: RING finger ubiquitin ligases at the crossroads of tumour suppression and oncogenesis. Nat Rev 11(9):629–643
Maris JM, Matthay KK (1999) Molecular biology of neuroblastoma. J Clin Oncol 17:2264–2279
Maris JM, Hogarty MD, Bagatell R, Cohn SL (2007) Neuroblastoma. Lancet 369:2106–2120
Matlashewski GJ, Tuck S, Pim D, Lamb P, Schneider J, Crawford LV (1987) Primary structure polymorphism at amino acid residue 72 of human p53. Mol Cell Biol 7:961–963
Olivier M, Eeles R, Hollstein M, Khan MA, Harris CC, Hainaut P (2002) The IARC TP53 database: new online mutation analysis and recommendations to users. Hum Mutat 19:607–614
Perfumo C, Parodi S, Mazzocco K, Defferrari R, Inga A, Haupt R, Fronza G, Tonini GP (2008) Impact of MDM2SNP309 genotype on progression and survival of stage 4 neuroblastoma. Eur J Cancer 44:2634–2639
Perfumo C, Parodi S, Mazzocco K, Defferrari R, Inga A, Scarrà GB, Ghiorzo P, Haupt R, Tonini GP, Fronza G (2009) MDM2 SNP309 genotype influences survival of metastatic but not of localized neuroblastoma. Pediatr Blood Cancer 53(4):576–583
Piette J, Neel A, Marechal V (1997) Mdm2: keeping p53 under control. Oncogene 15:1001–1010
Rodriguez-Lopez AM, Xenaki D, Eden TO, Hickman JA, Chresta CM (2001) MDM2 mediated nuclear exclusion of p53 attenuates etoposide-induced apoptosis in neuroblastoma cells. Mol Pharmacol 59:135–143
Sharpless NE, DePinho RA (2002) p53: good cop/bad cop. Cell 110:9–12
Shimada H, Ambros IM, Dehner LP, Hata J, Joshi VV, Roald B, Stram DO, Gerbing RB, Lukens JN, Matthay KK, Castleberry RP (1999) The international neuroblastoma pathology classification (the Shimada system). Cancer 86:364–372
Slack A, Chen Z, Tonelli R, Pule M, Hunt L, Pession A, Shohet JM (2005a) The p53 regulatory gene MDM2 is a direct transcriptional target of MYCN in neuroblastoma. Proc Natl Acad Sci U S A 102:731–736
Slack A, Lozano G, Shohet JM (2005b) MDM2 as MYCN transcriptional target: implications for neuroblastoma pathogenesis. Cancer Lett 228(1–2):21–27
Toledo F, Wahl GM (2006) Regulating the p53 pathway: in vitro hypotheses, in vivo veritas. Nat Rev Cancer 6:909–1023
Tweddle DA, Malcolm AJ, Cole M, Pearson AD, Lunec J (2001) p53 cellular localization and function in neuroblastoma: evidence for defective G(1) arrest despite WAF1 induction in MYCN-amplified cells. Am J Pathol 158:2067–2077
Van Maerken T, Speleman F, Vermeulen J, Lambertz I, De Clercq S, De Smet E, Yigit N, Coppens V, Philippé J, De Paepe A, Marine JC, Vandesompele J (2006) Small-molecule MDM2 antagonists as a new therapy concept for neuroblastoma. Cancer Res 66:9646–9655
Vassilev LT, Vu BT, Graves B, Carvajal D, Podlaski F, Filipovic Z, Kong N, Kammlott U, Lukacs C, Klein C, Fotouhi N, Liu EA (2004) In vivo activation of the p53 pathway by small-molecule antagonists of MDM2. Science 303:844–848
Zhang Z, Wang H, Prasad G, Li M, Yu D, Bonner JA, Agrawal S, Zhang R (2004) Radiosensitization by antisense anti-MDM2 mixed-backbone oligonucleotide in in vitro and in vivo human cancer models. Clin Cancer Res 10:1263–1273
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Cattelani, S., Ferrari-Amorotti, G., Soliera, A.R., Manzotti, G., Raschellà, G., Calabretta, B. (2013). Neuroblastoma: Role of MDM2 and SNP309 as Markers. In: Hayat, M. (eds) Pediatric Cancer, Volume 4. Pediatric Cancer, vol 4. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-6591-7_3
Download citation
DOI: https://doi.org/10.1007/978-94-007-6591-7_3
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-6590-0
Online ISBN: 978-94-007-6591-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)