Abstract
In our research in a South African community, we examined HIV-related stigma among women who were HIV infected (n = 609) and a community sample of unknown status (n = 1,077) using qualitative and quantitative methods. Our research showed that an HIV diagnosis was often associated with death, immoral behaviour, punishment and lack of adherence to cultural traditions. HIV-infected women perceived the community to be highly stigmatising, and they internalised aspects of the stigma in their own self-evaluation. The degree to which they perceived community members to be stigmatising was directly linked to their own internalised stigma. This perception had a negative influence on their psychological well-being, including increased depression and decreased self-esteem and disclosure of their HIV status. Despite their fear of disclosure, women did not report high levels of enacted stigma. Internalised stigma and the stigma attributed to others both declined slightly over the last several years, largely due to increases in HIV/AIDS knowledge. In contrast, although community members did not reveal high levels of personal stigma, they regarded others in their community to be highly stigmatising. Factors contributing to community stigma were age, gender, level of education, HIV knowledge and personal experience of knowing someone with HIV. Typical stigmatising reactions were mostly observed in subtle behaviour, though acts of overt discrimination were also reported. These data highlight the importance of different perspectives on HIV-related stigma. Results are interpreted in the context of developments around HIV/AIDS policy in South Africa which allow us to make suggestions to address HIV stigma in this community.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Background and Politics of HIV in South Africa
Since HIV/AIDS first appeared in the 1980s, it has been associated with fear, stigmatization and discrimination (Parker and Aggleton 2003; see also chapters in Part I in this volume). Several studies have reported the pervasive and detrimental effects of HIV-related stigma on the lives of people living with HIV. Furthermore, stigma contributes to the expansion of the epidemic in several ways (Parker and Aggleton 2003; Campbell et al. 2005). Stigma and its accompanying secrecy affects decisions about HIV testing, disclosure and treatment and is therefore an obstacle to reducing the spread of infection (Bond et al. 2002; Parker et al. 2002; Mbonu et al. 2009). A comprehensive understanding of stigma is therefore necessary in managing the epidemic.
HIV infection has reached epidemic proportions in South Africa and has serious consequences for individuals as well as the country’s health resources and economy. South Africa boasts the greatest prevalence of HIV/AIDS in the world – with estimates hovering around 11 % for the country as a whole and 17.8 % for adults aged 15–49 years. Approximately 5.6 million people in South Africa are living with HIV, and women account for an estimated 58 % of all HIV infections (Shisana et al. 2009; UNAIDS 2010). In fact, almost one in three women aged 25–29 are living with HIV in some provinces such as KwaZulu-Natal and Mpumalanga (Department of Health South Africa 2009; Shisana et al. 2009). These alarming statistics, however, are only part of the story. For a more complete understanding of the South African context, we must recognise both the sociocultural situation of the country and the political action and inaction taken in response to the pandemic. In fact, many have suggested the disproportionate size of the epidemic is partly attributable to the government’s response to HIV/AIDS (Butler 2005; Chigwedere et al. 2008; see also Chaps. 1 and 8 in this volume).
Although HIV/AIDS was introduced in South Africa later than in other African countries due to the relative political and economic isolation during the 1980s (Grimond 2001), there was a lack of early response to the epidemic from the South African government. This contributed to community apathy and denial and allowed for the development of many misconceptions. Sociopolitical issues were perceived as far more important than the developing HIV/AIDS epidemic. This view was largely due to the political turmoil resulting from the country’s long history of apartheid and attempts to end the regime. During the late 1980s and early 1990s, all communication was seen as political and part of an ongoing ‘racial war’. Misconceptions regarding HIV emerged, including the notions that HIV was a war strategy invented by the apartheid government or a disease to stop black population growth. After the 1994 democratic election, radical changes took place at almost all levels of the society, again keeping people involved in sociopolitical issues and hampering serious dedication to combating the spread of HIV/AIDS. Sherriffs wrote (1997: 11) “[m]uch of the response to AIDS has been too much talk and too little action. We knew about AIDS so long but we didn’t do enough…We have lost half a generation of time to do something significant.”
Despite the general acknowledgement that HIV/AIDS was crippling South Africa during the late 1990s into the twenty-first century, President Thabo Mbeki (in office 1999–2008) strongly criticised the conventional wisdom around HIV. He refused to believe that HIV was a virus which could be treated with antiretroviral medications (ARVs). During the inaugural session of the 13th International AIDS Conference in 2000, Mbeki publicly denounced the idea that the “world’s biggest killer and the greatest cause of ill health and suffering across the globe” could be attributable to a “single virus.” He believed it was the result of “extreme poverty.” The solution he suggested, therefore, was the alleviation of poverty instead of investment in expensive Western medicines (Horton 2000). The South African government therefore rejected free drugs and grants to support treatment of HIV up until the end of 2003. After serious internal and international pressure on the government, ARVs became available in the public health sector for treatment of those with low CD4 counts (first <200 and later <300) in selected health facilities in April 2004. This political context and governmental response to HIV resulted in poor understanding of the epidemic, denial of the magnitude of the epidemic, the inhibition of prevention strategies and HIV-related stigma and discrimination.
In Western countries, the fear and hostility directed towards people with HIV/AIDS is often derived from negative attitudes towards homosexuality and drug use (Herek et al. 2002). In Africa, however, the virus is spread primarily through heterosexual contact and from mother to child (Department of Health 2009). Women in South Africa are particularly vulnerable because of gender inequality. Many women depend on male partners for survival (Abdool Karim 1998; Warwick et al. 1998; Strebel et al. 2006; Kasese-Hara et al. 2008). As a result, men are often “excused” for engaging in high-risk sexual behavior, such as having multiple sex partners, while women are often wrongly perceived as the main transmitters of the disease (Warwick et al. 1998; Strebel et al. 2006; Amuyunzu-Nyamongo et al. 2007; Campbell et al. 2007). Consequently, the stigma associated with HIV in South Africa is largely embedded in beliefs about contamination, sexuality, morality and religion (Mbonu et al. 2009). Women living with HIV are often considered promiscuous, dirty, irresponsible (Bond et al. 2002) and bewitched (Aggleton and Chase 2001; Bond et al. 2002). It is through this political and sociocultural context that the unique HIV-related stigma in South African communities should be examined.
2 Definition of Stigma
Stigma is a multidimensional concept primarily focused on deviance or departure from an accepted standard or convention. The term stigma originates from the Greek language and refers to a tattoo mark branded on the skin of an individual as a result of some incriminating action, identifying the person as someone to be avoided (Crawford 1996). In the social sciences, stigma can be described as a deviation from an ideal or expectation, contributing to a powerful, discrediting social label that reduces the way individuals see themselves and are viewed by others (Goffman 1963; see also Chaps. 1, 2 and 17 in this volume). The attribute is not inherently deviant, but the deviance is derived from culturally embedded meanings in the context of a particular historic period and culture. Deacon and colleagues (2005) integrate several definitions of stigma and describe it as a social process that results in differentiating those with the disease in negative social terms. The function of stigma was originally to secure social structures, safety and solidarity by casting out offenders or reaffirming societal values (Gilmore and Somerville 1994).
Stigma in an African context is built on a series of shared beliefs that HIV is associated with immoral behavior, religious punishment and lack of adherence to cultural norms. These beliefs result in blame for contracting the disease and perceiving those with HIV as socially dead (Aggleton and Chase 2001; Nyblade et al. 2003; Deacon et al. 2005; Niehaus 2006). Two essential core elements of HIV-related stigma in Africa are the fear of transmission derived from a lack of knowledge about HIV and judgment created by asserting morality and assigning blame (Ogden and Nyblade 2005; Nyblade and MacQuarrie 2006).
Various perspectives can influence ways the HIV-related stigma is perceived and experienced. These perspectives include those of the infected (a subjective experience defined as internalized stigma), the noninfected (an outsider perspective defined as personal stigma of community members) and the general perception of stigma levels in the community (stigma attributed to others). Levels of enacted stigma refer to actual experiences of stigma and discrimination (Gilmore and Somerville 1994; Deacon et al. 2005).
Theoretically, these various perspectives on stigma are interrelated. For instance, the development of stigmatizing attitudes within a community is often expressed through discriminatory actions towards people with HIV. An individual’s perspective can then be influenced by the extent to which stigmatizing attitudes are attributed to others in the community. For people living with HIV, direct or indirect experiences or even their anticipation of stigmatization can contribute to their sense of being stigmatized. Stigmatized persons often accept some of the negative social judgments and discredit themselves (internalized stigma). Internalized stigma is rooted in a survival mechanism aimed at protecting the individual from enacted stigma through reluctance to disclose (Mbonu et al. 2009). This can be psychologically damaging for the infected person, since high levels of internalized stigma is often associated with lower levels of self-esteem, more symptoms of depression (Berger et al. 2001; Freeman et al. 2007; Brandt 2009) and less disclosure of HIV status (Kalichman et al. 2003; Sethosa and Petlzer 2005; Makin et al. 2008; see also Chap. 5 in this volume). Stigmatized people respond to community stigma by either conforming to it or resisting it. This response can affect the impact of stigma in a community, irrespective of the actual level of enacted stigma or discrimination (Deacon et al. 2005). High levels of internalized stigma then reduce incentives to challenge stigmatization, thereby perpetuating this perception and propagating negative consequences for both the individual and public health programs.
To gain a greater understanding of the complexity of HIV-related stigma in a South African community, we conducted a series of scientific studies involving HIV-infected women and community members from the same community. These studies were part of the Serithi project, a longitudinal study which examined disease progression in women diagnosed with HIV during pregnancy. Our first task was to develop parallel stigma scales for measuring distinct aspects of the HIV-related stigma in both sample groups. These results are presented elsewhere (Visser et al. 2008). Using these scales, we then sought to (1) understand the experience of stigma and characteristics associated with levels of stigma in two sample groups, (2) examine how these facets of HIV-related stigma may have changed over time and (3) compare the different perspectives of stigma in the two sample groups to understand the level of stigma in communities.
3 The Study
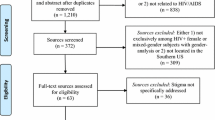
The Serithi project assessed the experiences of HIV-related stigma in two samples: HIV-infected women and community members of unknown status. Both samples were recruited from a community that is part of Tshwane in South Africa.
3.1 HIV-Infected Women
3.1.1 Participants and Study Design
Women diagnosed with HIV during pregnancy were recruited from four antenatal clinics in two urban townships in Tshwane (Atteridgeville and Mamelodi). The study enrolment period occurred over 3 years, from June 2003 to July 2006 (N = 609). Participants were interviewed during pregnancy shortly after diagnosis (mean gestational age 28 weeks) and when they brought their babies to the clinic for their 3- and 9-month check-ups. Interviews were conducted by trained research assistants in the subject’s preferred language, Sepedi, Setswana or Isizulu.
3.1.2 Measurement
3.1.2.1 Stigma
Two stigma scales (Visser et al. 2008) were used to assess (1) the level of internalised stigma, which is the extent in which a person accepts being stigmatized, and (2) stigma attributed to others in the community. The scales consist of 12 items each, assessing moral judgment and social distancing which are core elements of HIV-related stigma in Africa (Ogden and Nyblade 2005; Nyblade and MacQuarrie 2006). Scale scores ranged from 1 (low stigma) to 12 (high stigma). The internal consistency of the scales was 0.70 for internalised stigma and 0.77 for attributed stigma. An open-ended question was also included to explore the women’s first reaction when they became aware of their HIV status.
3.1.2.2 Socio-demographic Characteristics
Women reported their age, marital status and education level. Women also reported whether they had a regular income and whether they had ever been a victim of physical or sexual violence. Last, socio-economic status was derived from a series of three questions about the presence of amenities in the home (i.e. material their house was made of, electricity and water source). These items were sumed for a socioeconomic status score ranging from 0 to 3, with higher scores indicating higher status.
3.1.2.3 Epidemic-Related Characteristics
Four variables that were considered likely to change as the epidemic spread were included. First, knowledge about HIV was assessed using a series of 15 questions to determine a participant’s understanding of HIV transmission and clinical presentation (WHO 1990). Total scores represented the number of questions answered correctly and thus could range from 0 to 15. Second, participants reported whether or not they knew someone else with HIV. Third, women reported whether or not she had disclosed her HIV status to her partner, family or friends. And forth, enacted stigma was assessed using 9 items regarded as potential discriminatory behavior that women may experience because of stigmatization in the community.
3.1.2.4 Psychological Characteristics
Psychological characteristics included self-esteem, depression, social support and coping. Established measures were adapted for the South African context. Self-esteem was assessed using the Rosenberg self-esteem scale (RSE) (1965) which measures the extent to which one values and feels content with oneself on a four-point scale (10 items, α = 0.75). Depression was measured with the Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff 1977), which asks respondents to indicate the frequency with which depressive symptoms were experienced during the previous week. The somatic items which could have been related to either pregnancy or HIV status, identified by Kalichman and colleagues (2000), were removed (15 items, α = 0.88). The Multidimensional Social Support Inventory (MSSI) of Bauman and Weiss (1995) was adapted to assess the individual’s perceived practical, emotional and affirmational social support integrated into a positive support scale (9 items, α = 0.87). The Brief COPE scale (Carver 1997) was used to assess various coping strategies. An exploratory factor analysis identified two factors: positive coping (13 items, α = 0.75) and avoidant coping (8 items, α = 0.54).
3.1.3 Analysis
Descriptive statistics were first generated to describe the characteristics of our sample at baseline. Our analytic approaches then followed according to our aims. To describe the stigma experienced by the HIV-infected women, we used both a qualitative and quantitative approach. Content analysis (Stemler 2002) was used to explore the responses to an open-ended question about the women’s initial reactions to discovering that they were infected with HIV. Next, basic means and frequencies were generated to describe levels of internalized and attributed stigma, epidemic-related characteristics and psychological health reported at baseline. We then tested the unadjusted associations between these variables and levels of both internalized and attributed stigma using analyses of variance (ANOVAs) and Pearson correlations (r) for categorical and continuous variables, respectively. Variables that were significant (p < 0.2) in the unadjusted analyses with internalized and attributed stigma were entered into corresponding linear regression models. Backward elimination was used to determine covariates that were independently associated with internalized and attributed stigma (removal p > 0.1).
To explore the way HIV-related stigma changed over time (objective 2), we used two different approaches, examining changes on both the individual and population levels. First, we compared women’s scores at baseline, 3 and 9 months postpartum to determine the experiences of women up to 1 year after diagnosis. We used a within-subject analysis to examine these changes and thus demonstrate how women’s experience of stigma changes from shortly after diagnosis to having known their status over approximately 1 year.
We then examined how stigma may change over time among populations of newly diagnosed pregnant women. We used baseline data collected between June 2003 and July 2006. Time was used as a continuous measure, obtained by calculating the difference (in months) between the date of the first baseline interview (June 10, 2003; time = 0) and the date of the index participant’s interview. Larger values therefore indicated later/more recent interview dates. We tested the unadjusted associations between each variable and time to determine which factors may have changed over time. ANOVAs and Pearson correlations (r) were used for categorical and continuous measures, respectively. Those that were marginally significant (p < 0.2) were considered potential confounders and were entered into multiple linear regression models. We then modelled changes over time for both internalized and attributed stigma while controlling for potential socio-demographic and HIV epidemic-related confounders.
3.2 Community Sample
3.2.1 Participants and Study Design
Our community sample (n = 1,077) was recruited in 2004 from the same communities in Tshwane (Atteridgeville and Mamelodi). These townships are part of a historically disadvantaged area and are home to a mainly black, low to middle socio-economic class urban population. The townships are comprised of both informal dwellings (temporary housing) and permanent formal housing and are representative of a large portion of the urban population in South Africa. A proportional sample was obtained using a stratification technique to approximate the age and gender distribution of the population in each community based on 2001 census data. Participants were recruited from clinics, shopping centres, community centres, taxi waiting areas and the areas around street vendors. These sites were purposely selected because they represented public access sites within the community. A systematic sampling method was used (Struwig and Stead 2001) in which interviewers approached every third passer-by and requested an interview. Consenting adults aged older than 18 years were eligible to participate in the survey (Visser et al. 2009).
The study was repeated in 2005 1 year after the initial community survey with a sample of 500 respondents in one of the townships (Atteridgeville). The same scales were used to determine changes in stigma, HIV knowledge and knowing people with HIV over time (Forsyth et al. 2008). A similar sampling technique was used, by recruiting a proportional sample according to community gender and age ratios (based on 2001 census data). Four public sites were chosen for data collection, selected because of their accessibility and potential to facilitate the recruitment of participants. Permission to use the sites was attained from the ward coordinator. Participants were eligible if they were South African, over 18 years of age and resided in the area. In both samples, university students conducted the interviews with consenting participants in their chosen language.
3.2.2 Measurement
3.2.2.1 Stigma
Two stigma scales (Visser et al. 2008) were used to assess (1) personal perceptions and reactions towards people living with HIV/AIDS (personal stigma) and (2) stigma attributed to most people in their community. These scales were similar to those used with the infected women, though the wording was slightly different to reflect the specific perspective. In a factor analysis of both scales, two factors were identified: a moral component (blame and judgment) and interpersonal component (social distancing). The Cronbach alpha coefficient was 0.76 for the personal stigma scale and 0.88 for the attributed stigma scale.
3.2.2.2 Socio-demographic Characteristics
These included age, gender, marital status, level of education, employment status and length of stay in the community.
3.2.2.3 Epidemic-Related Variables
Four variables related to the experience of the epidemic were included. First, knowledge of HIV was assessed using the same 15 questions used with HIV-positive women. All correct answers were counted into a scale score ranging from 0 to 15. Second, respondents reported whether they knew someone else with HIV. Third, respondents reported whether they had been tested for HIV. And fourth, responses to an open-ended question was used to determine experienced or witnessed acts of discrimination towards persons living with HIV/AIDS in their community, here referred to as enacted stigma.
3.2.2.4 Cultural Beliefs
Respondents were asked whether they believed traditional healers could cure HIV and whether they believed people with HIV are bewitched. In an open-ended question, respondents were asked how members of their community viewed HIV/AIDS from a cultural or spiritual viewpoint.
3.2.3 Analysis
Descriptive statistics were used to describe the characteristics of the sample. Our analytic approaches then followed according to our aims.
To describe the stigma experienced by community members, we again used a qualitative and quantitative approach. Content analyses (Stemler 2002) were performed to categorize and code responses to the two open-ended questions. Two independent researchers interpreted the data and whenever there were discrepancies, developed consensus after discussion (Visser et al. 2009). Exploratory analyses were performed to assess the relationships between independent variables and the two stigma scales, personal and attributed community stigma using analyses of variance (ANOVAs) and correlations. Variables that were significantly related (p < 0.05) in the unadjusted analyses with internalized and attributed community stigma were entered into backward stepwise linear regression models to determine factors that were independently associated with personal and attributed community stigma (p < 0.05).
Stigma over time in the community was investigated by comparing data of the 2004 and 2005 community samples using independent t-tests (objective 2). Stigma scores for the community and HIV-positive samples were thereafter compared to illustrate similarities and differences in perceptions of HIV-related stigma (objective 3). We specifically examined the differences between the internalized stigma felt by HIV-positive women, the level of stigma they attribute to others and the personal stigma expressed by members of their community and the stigma they attribute to others in their community using t-tests.
4 Results
A description will be given of the experience of stigma (objective 1) and the experience of stigma over time (objective 2) separately for both sample groups. Stigma scores in the two sample groups will then be compared (objective 3).
4.1 HIV-Infected Women
4.1.1 Sample Characteristics
The socio-demographic characteristics of the HIV-infected women are shown in Table 12.1. The average age of the women was 26.6 (SD = 5.16) years. The majority (82.9 %) were not married, but 89 % had partners. Almost 90 % had secondary school education or higher. Only 25 % of the women had a regular income. Eleven per cent had been victims of physical violence, and 4 % had been victims of sexual violence. The median time from diagnosis to the first interview was 4 weeks.
4.1.2 Objective 1: Description of Stigma Among HIV-Infected Women
4.1.2.1 Women’s Experiences of HIV and Stigma
Women’s reaction when they first received the diagnosis were the following: 25 % feared death; 24 % reacted with sadness and helplessness; 23 % accepted passively; 19 % reacted with shock, denial and confusion, while 7 % were angry with their partners; and 2 % blamed themselves (Mdlalose 2006).
Many women experienced aspects of internalized stigma. Half (49 %) of the women indicated that they felt ashamed of their status, 33 % blamed themselves and 27 % saw HIV as punishment (moral judgment scale). In terms of social distancing, 63 % of women felt uncomfortable interacting with others, 49 % would understand if others do not want to be friends with them, and 56 % expect employers not to hire them because of their HIV status. Comparing women’s internalized stigma scores (mean 4.5) with the stigma they attribute to others (mean 9.6) suggests that they perceived people in their community to be highly stigmatizing. Internalized and attributed stigma were significantly correlated (r = 0.334, p < 0.01); higher levels of internalized stigma were generally associated with higher levels of attributed stigma.
On average, women responded to 10 of the 15 questions about HIV knowledge correctly. Slightly more than 40 % knew someone else with HIV, about half of which were family members. At baseline, which for most of the women was approximately 4 weeks after diagnosis, 59 % of the women had disclosed their status to one person. Seventy-four per cent of these women had disclosed their status to their partners, and 26 % had disclosed their status to someone else, mostly family members.
Of the women who disclosed their status at baseline, 25 % had experienced some kind of enacted stigma as a result of their HIV status. The percentage of women who experienced discriminatory behavior is given in Table 12.2. Enacted stigma ranged from loss of friendships and rejection to verbal and physically abuse and being threatened with death. Enacted stigma was mostly subtle in nature, though 13 % experienced verbal abuse, 4 % were threatened with death and 9 % lost their partners.
4.1.2.2 Factors Associated with Stigma Scores
To determine which factors were independently associated with levels of internalized and attributed stigma at baseline, we first assessed the unadjusted associations between the independent and dependent variables. In bivariate analyses, age, education, having been a victim of physical violence, HIV knowledge, knowing someone with HIV and having disclosed her status were all associated with internalized stigma (p < 0.2). Furthermore, all psychological variables – including self-esteem, depression, social support, active coping and negative coping – were also associated with internalized stigma (p < 0.2). We entered these independent variables simultaneously into a linear regression model and used backward elimination to derive our final model (Table 12.3). Age and level of depression were positively associated with levels of internalized stigma, while having disclosed her status and higher education were both negatively associated with internalized stigma. Self-esteem and social support were also inversely related to internalized stigma.
In our unadjusted analysis, attributed stigma was associated with age, marital status, employment, having a regular income, having been a victim of sexual violence, HIV knowledge and all psychological variables (p < 0.2). Our final linear regression model, however, suggests only six remaining characteristics that were independently associated with levels of attributed stigma. Older age, having been a victim of sexual violence and having more HIV knowledge, was statistically associated with greater attributed stigma. As with internalised stigma, self-esteem was negatively associated with attributed stigma, and depression was positively associated with attributed stigma, after controlling for all other related characteristics.
4.1.3 Objective 2: HIV-Related Stigma Over Time Among HIV-Infected Women
Because the data in this study was collected over a 3-year period, this allowed us to observe possible changes in the perception and experience of stigma over time.
4.1.3.1 Changes in the Experience of Stigma During the First Year After Diagnosis Among HIV-Infected Women
Longitudinal data for each participant was used to compare the experience of stigma from being recently diagnosed at baseline to living with HIV for almost 1 year. Stigma scores at enrolment, at 3 and 9 months, are compared in Fig. 12.1.
Women’s experience of internalized stigma was the highest at enrolment shortly after diagnosis and progressively decreased at the follow-up interviews (F = 33.7; p < 0.000). There was a significant effect of positive coping on internalized stigma over time – when positive coping was high, the women experienced less internalized stigma and vice versa. In contrast, their attribution of stigmatizing attitudes to others in the community was much higher than their internalized stigma at enrolment (p < 0.000) and remained at this high level over time.
4.1.3.2 Changes in the Experience of Stigma Among Newly Diagnosed Pregnant Women Over Time
The women’s stigma scores at baseline were compared over time to determine changes in internalized stigma and attributed stigma over 3 years of enrolment. After controlling for changes in the socio-demographic characteristics of the sample population seen over time (socio-economic status, past experience with sexual violence and marital status), there was evidence of a significant decrease in internalized stigma women experienced over 3 years (p = 0.034) (Fig. 12.2).
This decline, however, became nonsignificant after controlling for changes in epidemic-related characteristics (p = 0.212; HIV knowledge and knowing someone with HIV). These models suggest that decrease in internalized stigma can be partly attributed to an increase in knowledge about HIV over time and more women knowing someone else with HIV. Internalized stigma was significantly higher among those of lower socio-economic status and those who were less knowledgeable about HIV.
Conversely, attributed stigma decreased significantly only when changes in the epidemic where taken into account (Fig. 12.3). Those with increased knowledge of HIV attributed more stigmatizing attitudes to others in the community. Furthermore, women who reported having experienced sexual violence attributed higher levels of stigma to others in their community.
4.2 Community Members
4.2.1 Sample Characteristics
The sample was representative of the proportions of people in the age and gender categories, with the majority between the ages of 26 and 50 years (Table 12.4). The majority had at least a secondary school education, yet two-thirds of the sample was unemployed. The majority of the respondents had stayed in these communities for more than 10 years (Visser et al. 2009).
4.2.2 Objective 1: Description of Stigma Among Community Members
4.2.2.1 Community Members’ Experience of HIV and Stigma
In an open-ended question, respondents indicated how members of their community perceived HIV. Themes identified through content analysis indicate that members of these communities often associated HIV with death (31.4 %), immoral behavior (that they did something wrong) (27.6 %) or punishment from God or something evil happening (19.1 %). A small percentage of respondents (13.5 %) indicated a traditional cultural perspective on HIV by relating HIV to bewitchment or the lack of adherence to cultural traditions, while 8.1 % indicated that people in their community denied the existence of HIV.
In the second open-ended question, respondents were asked to describe incidents of discrimination that they had either witnessed or experienced in their community (enacted stigma). Seventy-eight per cent (78 %) of the respondents reported such incidents. Subtle discrimination, such as gossip (38.1 %), not treating people living with HIV/AIDS (PLWA) with respect (20.7 %) and keeping a distance (18.2 %) from PLWA, was the most common form of stigmatization, whereas overt discrimination, such as attempts to humiliate (11.0 %) or physically harm (2.3 %) and not taking care of infected people (1.2 %), was less commonly reported.
The level of HIV knowledge was relatively high in this sample (M = 11.8, SD 2.6, range 0–15). More than 90 % of the respondents knew the major transmission routes and that the virus could not be transmitted through casual contact. Most respondents knew someone with HIV (72.9 %), whether a family member, close friend or an acquaintance. Almost one-third reported that they had been tested for HIV. A small percentage of the respondents believed that people with HIV are bewitched (5.7 %) and that traditional healers could cure HIV/AIDS (15.7 %). There was a low but significant correlation (r = 0.14, p < 0.00) between the beliefs that traditional healers could cure HIV/AIDS and that people with HIV are bewitched.
The proportion of participants indicating agreement with each of the items in the two stigma scales are shown in Table 12.5.
The most frequently endorsed items in the personal stigma scale were those that had to do with blame and judgment, while respondents endorsed the interpersonal distancing statements, indicating fear or discomfort, less frequently. For each of the items, respondents more often attributed more stigma to others in their community than they themselves did. Scale scores showed that personal stigma scores (X = 2.8; SD = 2.5; range 0–12) were significantly lower than attributed stigma scores (X = 7.4; SD = 3.7; range 0–12), (t = 34.26; p < 0.001). There was a weak but statistically significant correlation between personal and attributed stigma scores (r = 0.09, p < 0.005) (Visser et al. 2009).
4.2.2.2 Factors Associated with Stigma Scores
In bivariate analyses, age, gender, level of education and marital status were associated with levels of personal stigma. Additionally, HIV knowledge, knowing someone with HIV, having tested for HIV and traditional beliefs were related to personal stigma (p < 0.01). Variables with a significant relationship (p < 0.01) with personal stigma scores were entered into a backward stepwise linear regression model to determine the manifestation of stigma in the community. The analysis showed that male respondents and those who were older, less educated and held traditional cultural beliefs had higher levels of personal stigma, while those with more knowledge of HIV and knew someone with HIV had lower levels of personal stigma. The final model accounted for a fair proportion of the variance in personal stigma (R 2 = 0.23, p < 0.00).
The same was done for attributed stigma. Age, level of education, HIV knowledge and knowing someone with HIV were associated with attributed community stigma. The linear regression model examining attributed community stigma indicated a similar pattern as for personal stigma, but in the reverse direction. Respondents who were more knowledgeable about HIV or knew someone with HIV considered the community to be more stigmatizing, while older respondents considered the community to be less stigmatizing. The variables in the model, however, do not contribute substantially to the variance in attribute community stigma (R 2 = 0.07).
4.2.3 Objective 2: HIV-Related Stigma Over Time Among Community Members
To shed some light on the possible changes in HIV-related stigma in communities over time, the stigma data of 2004 was compared with data obtained 1 year later in a similar sample in one of the communities (Atteridgeville, n = 500).
Results revealed that personal stigma was significantly lower in the 2005 cohort than the 2004 cohort (Table 12.6); however, the 2005 cohort perceived the community to be more stigmatizing than the previous year. In the 2005 sample, significantly more participants (87 %) knew of someone living with HIV/AIDS, as compared with t mple (73 %), (p < 0.001). There was no difference between the levels of HIV/AIDS knowledge between the two cohorts (p = 0.64) (Forsyth et al. 2008).
4.3 Objective 3: Comparison of Stigma Scores in the Two Samples
The scores obtained on the stigma scales in the two study samples are compared in Table 12.7.

Participants in the community sample attributed much higher levels of stigma to others than they reported for themselves (mean score 7.32 vs. 2.79, t = −34.35, p < 0.001). HIV-positive women felt that people in the community were even more stigmatizing than did community members (9.83 vs. 7.32, t = −11.28, p < 0.001). The level of internalized stigma felt by the HIV-positive women was significantly higher than the level of stigma expressed by community members (4.64 vs. 2.79, t = −11.19, p < 0.001).
There was only a weak correlation between personal and attributed stigma scores in the community sample (r = 0.09, p < 0.05) although this association was stronger among the HIV-positive women (r = 0.28, p < 0.001). This suggests that women who attributed higher levels of stigma to others tended to feel more stigmatised. Analysis of the scores on the two subscales for the two sample groups showed that the scores for blame and judgment were significantly higher than the interpersonal distancing scores for all scales (p < 0.001) except for the scale measuring internalized stigma among the HIV-positive women in which the scores obtained on the two subscales were similar. For each of the scales, there was a strong association between the scores obtained on the two subscales (r > 0.4, p < 0.001 for each of the four scales).
5 Conclusion
This research shows that HIV/AIDS is perceived in negative terms by both HIV-infected women and community members three decades into the epidemic. Our samples considered HIV/AIDS to be directly associated with death, immoral behavior, punishment or failure to adhere to cultural traditions. Furthermore, results suggest that moral issues were more important in the formation of stigma in this community than fear of contamination through social interaction.
Internalized stigma among women with HIV seems to be higher than the stigma reported in community groups. Although their experience of internalized stigma decreased during the first year following their diagnosis, these women still attributed extremely high levels of stigma to others in their community, more than what other community members did. Both internalized and attributed stigma were related to decreased states of well-being for the women – self-esteem and social support were negatively related, and depression was positively related with stigma scores. Higher levels of internalized stigma were also related to lower levels of disclosure, which could negatively influence their health-seeking behavior. In this sample, 59 % of the women disclosed their status to at least one person about 4 weeks after the diagnosis. A small percentage of women reported some forms of enacted stigma – but only a few reported serious adverse effects such as death threats (4 %) and abandonment by their partners (9 %) because of their HIV status. The presence of mostly subtle forms of stigma (such as gossiping and keeping a distance) is confirmed by the responses of the members in the community sample. Only a few community members referred to incidents of humiliation, physical harm or not taking care of HIV-infected people in their community.
The different perspectives on stigma and the low levels of enacted stigma reported in the two sample groups make conclusions about the actual level of stigma present in the community difficult. It seems as if infected women may overrate the level of stigma attributed to members in their community, but this stigma may be disguised by women’s selective disclosure.
Similar to the finding from a meta-analysis of studies done in sub-Saharan Africa that stigma decreases over time (Mbonu et al. 2009), this research found that the experience of stigma decreased in both sample groups over the period of 2–3 years. On a personal level, infected women reported lower levels of internalized stigma after a year of knowing their status. This change was related to increased positive coping strategies. On a community level, women diagnosed with HIV experienced less internalized stigma if diagnosed more recently. This lower level of internalized stigma is likely related to lower levels of stigma reported by community members in the 2005 community sample.
In both sample groups, the level of stigma was related to epidemic-related factors such as HIV knowledge and knowing someone with HIV. The more involved people are with HIV, the less personal stigma they reported. Lower levels of stigma can therefore be explained by higher levels of HIV knowledge and greater awareness of HIV as the epidemic develops. On the contrary, the level of attributed stigma remained high over time in both sample groups. Whereas knowledge of HIV and personal involvement with someone who is infected was associated with lower levels of personal stigma in both groups, more involvement with HIV resulted in higher levels of attributed stigma. The perception that communities are stigmatizing is thus not changing, and this may continue to influence the behavior of both the infected and uninfected.
It needs to be recognized that the personal attitudes reported by individuals in the community may be falsely low as it is possible that they may have wanted to project themselves in the most positive light. Also, items that explore social distancing often represent hypothetical situations, and responses may not be an accurate reflection of an individual’s behavior in a similar situation where additional social dynamics play a role. The direct relationship between personal and attributed stigma indicates that the level of attributed stigma is positively associated with a person’s personal stigma and behavior. These relationships add to this work’s conceptual complexity as we cannot say that stigma is overrated in these communities.
Our results suggest opportunities for addressing the internalized stigma felt by those living with HIV and for decreasing stigmatizing attitudes within communities. While it is true that HIV-infected individuals suffer adverse societal consequences because of their disease, helping them recognize the extent to which stigma has been internalized could help them cope better with their HIV status and thus improve their overall health status. For interventions focused on decreasing stigmatizing attitudes within communities, an important first step is to make people aware of the difference between the limited extent to which people express stigmatizing attitudes and the possibility of exaggerated attribution of stigma to others in their community. An attempt to address high levels of attributed stigma (which is a generalized belief) could have an important effect both for HIV-infected individuals and changing behaviors of those in the community, such as making HIV testing more acceptable. More knowledge and close interaction with people living with HIV could decrease personal stigma in communities. To challenge attributed stigma as a shared belief, more openness in communities is needed to discuss sexuality and HIV and to openly demonstrate compassion and support for people infected with and affected by HIV.
References
Abdool Karim, Q. (1998). Women and AIDS, the imperative for a gendered prognosis and preventive policy. Agenda, 39, 15–25.
Aggleton, P., & Chase, E. (2001). Stigma, HIV/AIDS and prevention of mother-to-child transmission: A pilot study in Zambia, India, Ukraine and Burkina Faso. New York: United Nations Children’s Fund (UNICEF)/The Panos Institute.
Amuyunzu-Nyamongo, M., Okeng’o, L., Wagura, A., & Mwenzwa, E. (2007). Putting on a brave face: The experiences of women living with HIV and AIDS in informal settlements of Nairobi, Kenya. AIDS Care, 19(1), S25–S34.
Bauman, L. J., & Weiss, E. (1995). Multidimensional social support inventory: Revised. Bronx: Albert Einstein College of Medicine.
Berger, B., Ferrans, C. E., & Lashley, F. R. (2001). Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing and Health, 24(6), 518–529.
Bond, V., Chase, E., & Aggleton, P. (2002). Stigma, HIV/AIDS and prevention of mother-to-child transmission in Zambia. Evaluation and Program Planning, 25(4), 347–356.
Brandt, R. (2009). Putting mental health on the agenda for HIV+ women: A review of evidence from Sub-Saharan Africa. Women & Health, 49(2), 215–228.
Butler, A. (2005). South Africa’s HIV/AIDS policy, 1994–2004: How can it be explained? African Affairs, 104(417), 591–614.
Campbell, C., Foulis, C., Maimane, S., & Sibiya, Z. (2005). ‘I have an evil child at my house’: Stigma and HIV/AIDS management in a South African community. American Journal of Public Health, 95(5), 808–815.
Campbell, C., Nair, Y., Maimane, S., & Nicholson, J. (2007). “Dying twice”: A multi-level model of the roots of AIDS stigma in two South African communities. Journal of Health Psychology, 12(3), 403–416.
Carver, C. S. (1997). You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100.
Chigwedere, P., Seage, G. R., Gruskin, S., Lee, T.-H., & Essex, M. (2008). Estimating the lost benefits of antiretroviral drug use in South Africa. Journal of Acquired Immune Deficiency Syndrome, 49(4), 410–415.
Crawford, A. M. (1996). Stigma associated with AIDS: A meta-analysis. Journal of Applied Social Psychology, 26(5), 398–416.
Deacon, H., Stephney, I., & Prosalendis, S. (2005). Understanding HIV/AIDS stigma: A theoretical and methodological analysis. Cape Town: Human Sciences Research Council.
Department of Health. (2009). 2008 National antenatal sentinel HIV and syphilis prevalence survey, South Africa. Pretoria: Department of Health.
Forsyth, B., Vandormael, A., Kershaw, T., & Grobbelaar, J. (2008). The political context of AIDS-related stigma and knowledge in a South African township community. Journal of Social Aspects of HIV/AIDS, 5(2), 74–82.
Freeman, M., Nkomo, N., Kafoor, Z., & Kelly, K. (2007). Factors associated with prevalence of mental disorder in people living with HIV/AIDS in South Africa. AIDS Care, 19(10), 1201–1209.
Gilmore, N., & Somerville, M. A. (1994). Stigmatization, scapegoating and discrimination in sexually transmitted diseases: Overcoming ‘them’ and ‘us’. Social Sciences & Medicine, 39(9), 1339–1358.
Goffman, E. (1963). Stigma: Notes on the management of spoiled identity. Englewood Cliffs: Prentice-Hall.
Grimond, J. (2001, February 24–March 2). A survey of South Africa. Africa’s great black hope. The Economist, pp. 3–16.
Herek, G. M., Capitanio, J. P., & Widaman, K. F. (2002). HIV-related stigma and knowledge in the United States: Prevalence and trends, 1991–1999. American Journal of Public Health, 92(3), 371–377.
Horton, R. (2000). Mbeki defiant about South African HIV/AIDS strategy. Lancet, 356(July 15), 225–232.
Kalichman, S. C., Rompa, D., & Cage, M. (2000). Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. The Journal of Nervous and Mental Disease, 188(10), 662–670.
Kalichman, S. C., DiMarco, M., Austin, J., Luke, W., & DiFonzo, K. (2003). Stress, social support and HIV-status disclosure to family and friends among HIV-positive men and women. Journal of Behavioral Medicine, 26(4), 315–332.
Kasese-Hara, M., Mayeksio, T., Modipa, O., Mzobe, N., & Mango, T. (2008). Depression, mother’s concerns and life events experienced by HIV-positive, HIV-negative and mothers with unknown HIV status in Soweto. South African Journal of Psychology, 38(3), 575–588.
Makin, J. D., Forsyth, B. W. C., Visser, M. J., Sikkema, K. J., Neufeld, S., & Jeffery, B. (2008). Factors affecting disclosure in South African HIV positive pregnant women. AIDS Patient Care and STDs, 22(11), 907–916.
Mbonu, N. C., van den Borne, B., & De Vries, N. K. (2009). Stigma of people with HIV/AIDS Sub-Saharan Africa: A literature review. Journal of Tropical Medicine, 2009, 1–14. doi:10.1155/2009/145891, Article ID 145891.
Mdlalose, B. N. N. (2006). Women’s experience of being HIV positive, the stigma related to HIV and disclosure of their status. Unpublished dissertation. University of Pretoria, Pretoria.
Niehaus, I. (2006, October). Leprosy of a deadlier kind: Conceptions of AIDS, sex and death in the South African lowveld. Paper presented at the Institute for Social and Economic Research, Rhodes University, Grahamstown.
Nyblade, L., & MacQuarrie, K. (2006). Can we measure HIV/AIDS-related stigma and discrimination? Current knowledge about quantifying stigma in developing countries. Policy project. Washington, DC: International Center for Research on Women (ICRW) and United States Agency for International Development (USAID).
Nyblade, L., Pande, R., Mathur, S., MacQuarrie, K., Kidd, R., Banteyerga, H., Kidanu, A., Kilonzo, G., Mbwambo, J., & Bond, V. (2003). Disentangling HIV and AIDS stigma in Ethiopia, Tanzania and Zambia. Washington, DC: International Center for Research on Women (ICRW).
Ogden, J., & Nyblade, L. (2005). Common at its core: HIV-related stigma across contexts. Washington, DC: International Center for Research on Women (ICRW).
Parker, R., & Aggleton, P. (2003). HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Social Science & Medicine, 57, 13–24.
Parker, R., Aggleton, P., Attawell, K., Pulerwits, J., & Brown, L. (2002). HIV/AIDS-related stigma and discrimination: A conceptual framework and an agenda for action. Horizons Program. New York: The Population Council.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychology Measurement, 1(3), 385–401.
Rosenberg, M. (1965). Society and the adolescent self image. Princeton: Princeton University Press.
Sethosa, E., & Petlzer, K. (2005). Evaluation of HIV counselling and testing, self-disclosure, social support and sexual behaviour change among a rural sample of HIV reactive patients in South Africa. Curationis, 28(1), 29–41.
Sherriffs, P. (1997). A time for review – HIV in a democratic South Africa. Positive Outlook, 4(3), 10–12.
Shisana, O., Rehle, T., Simbayi, L. C., Zuma, K., Jooste, S., Pillay-van-Wyk, V., Mbelle, N., Van Zyl, J., Parker, W., Zungu, N. P., Pezi, S., & The SABSSM III Implementation Team. (2009). South African national HIV prevalence, incidence, behaviour and communication survey 2008: A turning tide among teenagers? Cape Town: HSRC Press.
Stemler, S. (2002). An overview of content analysis practical assessment. Research & Evaluation, 7(17), 124–130.
Strebel, A., Crawford, M., Shefer, T., Cloete, A., Henda, N., Kaufman, M., et al. (2006). Social constructions of gender roles, gender-based violence and HIV/AIDS in two communities of the Western Cape, South Africa. SAHARA, 3(3), 516–528.
Struwig, F. W., & Stead, G. B. (2001). Planning, designing and reporting research. Cape Town: Pearson Education.
UNAIDS. (2010). UNAIDS report on the global AIDS epidemic. Geneva: Joint United Nations Programme on HIV/AIDS.
Visser, M. J., Kershaw, T., Makin, J. D., & Forsyth, B. W. C. (2008). Development of parallel scales to measure HIV-related stigma. AIDS and Behavior, 12, 759–771.
Visser, M. J., Makin, J. D., Vandormael, A., Sikkema, K. J., & Forsyth, B. W. C. (2009). HIV/AIDS stigma in a South African community. AIDS Care, 21(2), 197–206.
Warwick, I., Bharat, S., Castro, R., Garcia, R., Leshabari, M., Singhanetra-Renard, A., & Aggleton, P. (1998). Household and community responses to AIDS in developing countries. Critical Public Health, 8(4), 291–310.
World Health Organization. (1990). Research package: Knowledge, attitudes, beliefs and practices on AIDS, Phase 1: The Questionnaire. The global programme on AIDS, Social and Behavioural Research Unit. Geneva: World Health Organization.
Acknowledgement
This study was funded by National Institute of Child Health and Human Development (NICHD) grant R24HD43558. The research referred to in this chapter was done in a joint venture between researchers at the University of Pretoria and Yale University, under the leadership of Brian Forsyth, Bridget Jeffrey and Jenny Makin. The authors would like to acknowledge the contribution of the following colleagues in various aspects of this research: Jonathan Mundell, Annelize de Villiers, (University of Pretoria), Kathleen Sikkema (Duke University) and the Serithi team of research assistants, R. Mkhondo, J. Tatane, M. Zondo, J., Ramodike, F. Nkomo, R. Kgoebane, M. Dikolometsa, P. Mabota, B. Moalosi, S. Sono and K. Lehobye.
We would like to thank the women who agreed to participate in the study, despite only recently finding out about their HIV status.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Note
The chapter integrates a large number of findings from the Serithi project and draws from several research papers based on the data of this overall project.
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Visser, M., Sipsma, H. (2013). The Experience of HIV-Related Stigma in South Africa. In: Liamputtong, P. (eds) Stigma, Discrimination and Living with HIV/AIDS. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-6324-1_12
Download citation
DOI: https://doi.org/10.1007/978-94-007-6324-1_12
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-6323-4
Online ISBN: 978-94-007-6324-1
eBook Packages: Humanities, Social Sciences and LawSocial Sciences (R0)