Abstract
For more than 10 years, pediatric AIDS has been virtually eradicated from Northern developed countries. In Africa, despite technical means and apparent political will, the percentage of pregnant women involved in preventing mother-to-child transmission (PMTCT) interventions is not increasing as fast as public health authorities would expect. There has been real progress during the last years, but these changes are still limited to Southern and East Africa. Eradication of pediatric AIDS in Africa seems a difficult objective to reach in 2015 as UNAIDS targeted it. This chapter is based on the combination of a literature review, an analysis of databases and empirical evidence collected during 15 years of PMTCT implementation, childcare research, and treatment programs in West Africa. One way to progress is to analyze why in some countries, PMTCT programs do not work properly and how in some others it works well. It seems important to analyze the process of PMTCT programs at several levels (site, regional, and national), step-by-step through literature, databases, and qualitative studies. It should be the better way to understand the successes and failures of the programs and how to “scale up” PMTCT programs, where there are gaps or obstacles and how to try to go through these obstacles. It includes analyses of the health system, of health workers expectations and limitations, of mothers’ expectations, and of relationships between mothers and the care system.
Perinatal intervention itself changes with new recommendations of the World Health Organization (WHO). Women can, however, give up or vanish at any time during the whole process. With new recommendations of WHO on breastfeeding and antiretroviral drugs, we can expect a dramatic decrease of postnatal transmission of HIV, but new problems arise, such as difficulties in getting formula milk, when HIV-infected mothers make that choice. This additional step gives many problems as women and exposed children have to be followed longer, and the final diagnosis cannot be given before the end of breastfeeding.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Until now, prevention of mother-to-child transmission of HIV (PMTCT) is the most effective intervention for combating new HIV infections. For more than 12 years, pediatric AIDS has been virtually eradicated from Northern developed countries (McKenna and Xiaohong 2007; Yéni 2010). According to the most recent UNAIDS report (2010), in developing countries the evolution of PMTCT is very different from country to country. In Africa, in the last 5 years, real progress has been observed in Southern Africa, where four countries (Botswana, Namibia, Swaziland, and South Africa) and in some countries of Eastern Africa reached the coverage of 90% of HIV-infected pregnant women with prophylaxis or treatment. In Central and West Africa, progression exists but is slower, as less than 30% of HIV-infected pregnant women have received any treatment or prophylaxis for PMTCT in 2009.
UNAIDS has called for a virtual elimination of mother-to-child transmission (MTCT) of HIV by 2015. This objective could only be realized if there is a significant increase in actions to prevent transmission to children in countries where programs are not optimal. However, pediatric AIDS has long been in Africa as they are already 2.3 million children living with HIV, which represent around 90% of HIV-infected children in the world. They are around 1.3 million children in need of antiretroviral treatment, and even if it is a dramatic improvement, coverage is still below 30% of the need. But, with antiretroviral treatments, these children have a real future as teenagers and young adults. This is another topic which will not really be addressed in this chapter, but must be underscored.
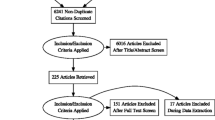
This chapter is based on the combination of a literature review, an analysis of databases, and empirical evidence collected during 15 years of PMTCT implementation, childcare research, and treatment programs in Central, East, and West Africa. In a previous paper, I discussed how to improve mothers’ access to PMTCT programs in West Africa (see Msellati 2009). This question is still important even if the PMTCT field is the subject of many publications with a very rapid updating. For example, recommendations for PMTCT were modified three times between 2006 and 2010. It is a field where things move fast in technical matters but much more slowly, as usual, for behavioral changes.
One way to progress in the scaling up of PMTCT is to analyze why in some countries, implementation has been possible and in others these programs do not work properly. It seems important to analyze the process of PMTCT programs at several levels (site, regional, and national) and step-by-step through literature, databases, and qualitative studies. It should be the better way to understand the successes and failures of the programs and how to “scale up” PMTCT programs, where there are gaps or obstacles and how to try to go through these obstacles. It includes analyses of the health system, health workers’ expectations and limitations, mothers’ expectations, and relationship between mothers and the care system.
2 PMTCT: Theoretical Understanding
As UNAIDS and WHO describe it (2003), PMTCT is based on four components and strategic approaches: (1) primary prevention of HIV infection in young women in childbearing age, (2) prevention of unwanted pregnancies in HIV-infected women, (3) prevention of mother-to-child transmission of HIV, and (4) appropriate treatment care and support for HIV-infected women and their children and families.
About the first component, as most pediatric HIV infections are acquired from the HIV-infected mothers, the most effective means of preventing pediatric infection is the prevention of HIV infection in women of childbearing age. There are many interventions in the field of education campaigns. But, as the prevalence among young women and young men in Africa shows, they work poorly as there are three to five times more 15–19-year-old HIV-infected girls than young men. Young women could be often involved in sexual relations with older men (“sugar daddies”) for many reasons (such as need of money or protection, social promotion, and sexual abuse), and these older men have a higher probability of being infected than teenager boys.
Some poverty and development experimental researches show possibilities of efficient interventions among young women at secondary schools. These interventions, as Dupas describes (2009), based on targeted information about “sugar daddies” and specific risk in relation with them, had a real efficacy in terms of sexual behavior change, measured by pregnancy incidence. Another work, also in Kenya, presented by Duflo et al. (2009), showed that offering free school uniforms to girls had an impact on school attendance and also on unwanted pregnancies (and therefore on risk of exposure to HIV and other STDs).
The second component of PMTCT is prevention of unwanted pregnancies in HIV-infected women. It has not been promoted as far as other components but adequate family planning services are an essential component of PMTCT. According to Delvaux and Nöstlinger (2007) and Curtis and colleagues (2009), the safety of contraception methods, including hormonal and intrauterine methods, is quite well established. The integration between the two health programs (reproductive health/family planning and PMTCT) should be implemented as a cost-effective strategy to reduce mother-to-child transmission of HIV, as Johnson and colleagues (2009) advocate for. In East Africa, several teams (Elul et al. 2009; Keogh et al. 2009) have shown that fertility desires are different among HIV-infected women and that preventing unwanted pregnancies among them should be addressed as a priority by family planning and PMTCT programs. This prevention component could decrease the number of HIV-exposed children by 40%.
The third component is the most addressed in the literature. PMTCT is a package of interventions such as voluntary counseling and testing for pregnant women, ARV prophylaxis for pregnant women and children, infant feeding counseling, and postnatal follow-up until diagnosis of HIV infection in exposed children. The majority of papers published in the last 5 years have highlighted failures of programs either from a quantitative point of view (Noba et al. 2001; Penda and Msellati 2010; Toro et al. 2010) or from a qualitative one (Painter et al. 2004; Levy 2009; Larsson et al. 2010) more than on technical aspects of PMTCT in itself. But some papers, particularly in recent years, show improvements and successes of these PMTCT programs and give some keys for scaling up access (Chandisarewa et al. 2007; Doherty et al. 2009; Lim et al. 2010; Muchedzi et al. 2010). With the improvement of antiretroviral drugs access, this component is highly related with the fourth component.
When we consider broad figures, from United Nations Agencies (UNAIDS 2010), worldwide, 53% (40–79%) pregnant HIV-infected women in low- and middle-income countries received antiretroviral medication to prevent the mother-to-child transmission of HIV in 2009. But this percentage recovers quite different things as the effectiveness of antiretroviral drugs in preventing mother-to-child transmission of HIV varies with the type of regimen used and the duration over which it is given. Combination regimens of antiretroviral drugs are more efficacious than monotherapies, as Leroy showed in 2005 (Leroy et al. 2005). In the countries that provided disaggregated data for their prevention of mother-to-child regimens, around 30% of HIV-infected pregnant women received single-dose nevirapine, while 54% received a combination regimen. About 15% of all HIV-infected mothers received ongoing antiretroviral therapy for their own health.
In new guidelines, WHO recommends (2009) that all pregnant women, as other adults, should receive highly active antiretroviral treatment when they are eligible for treatment with a higher threshold than previously, around 350 CD4, for their own health. Over that limit, HIV-infected pregnant women should receive a combination of antiretroviral drugs rather than nevirapine alone during pregnancy and delivery. For women living in developing countries and unable to provide a safe alternative infant feeding to breastfeeding, they should breastfeed and receive a prophylaxis during the duration of breastfeeding and a week after the end of breastfeeding.
3 Indicators of Effectiveness of PMTCT Programs
As Stringer and colleagues (2008) point out, some indicators of PMTCT effectiveness have been elaborated, to measure in fine the proportion of HIV-infected mothers/exposed infants that receive the intervention and the proportion of HIV-infected children at 15 months of life among all HIV-exposed children. HIV-free survival at 15 months or 2 years of age among children of HIV-infected pregnant women should be the best indicator for the success of PMTCT programs. But this indicator is seldom available as most health structures are not used to following mothers and children for a long period of time. Thus, the attrition is very important and the proportion of HIV-exposed or HIV-infected children still followed at 15 months of age is very low.
4 Antenatal Care Offer and Coverage
Coverage for PMTCT is in strong relation with coverage of antenatal care, and as Druce and Nolan (2007) argue, there have been a lot of mis-opportunities to link the two activities. When there is a low attendance to antenatal care, there is definitely a low coverage of counseling and testing for HIV among pregnant women (see also Chap. 19 in this volume). Some countries have quite an excellent coverage of antenatal care, and as a consequence, it is easier to implement a PMTCT program. Others have a good geographical coverage of PMTCT but the antenatal care is not good, and therefore, the performances of PMTCT program are poor. This is what Penda and Msellati have showed in their recent study in Cameroon (2010).
5 HIV Counseling and Testing in Pregnant Women
For Rwanda, Lim and colleagues (2010) reported that there can be improvements in PMTCT as far as there is a comprehensive learning from the field and meetings where improvements are identified, discussed, and experimented. Step-by-step, with an active biweekly supervision, it was possible to improve PMTCT care in 17 health centers. In 15 health centers, 95% of HIV-infected pregnant women received PMTCT services. Even antenatal care attendance improved as well as the proportion of women delivering in participating health centers (56–72%). Coverage of cotrimoxazole prophylaxis was 98% in exposed children.
One study described by Labhard and colleagues (2009) show that in rural Cameroon, PMTCT programs have to be adapted in rural areas, especially in settings where they are only nurses to lead the clinics. Training and providing equipment are major components. Authors also underscore the need to avoid any shortage of tests and drugs.
In Zimbabwe, Shetty and colleagues (2008) pointed out that it was possible to develop a PMTCT program in urban areas with peer counselors. In Malawi, Levy (2009) examined women’s decisions about HIV testing and PMTCT. Women accept HIV testing for expected benefits on their own health and their infant’s health (see also Chap. 4 in this volume). But they are often disappointed because of health system weakness, absence of good referral for their own health, and absence of integration of care. According to Painter and colleagues (2004) in Côte d’Ivoire, and Anand and colleagues (2009) in Kenya, site factors as health workers’ attitudes could be more important than women factors in acceptance of HIV test.
In 2007, WHO provided guidelines for provider-initiated HIV testing and counseling (PITC) which is also called “opt-out” approach of HIV testing (WHO 2007). Until that time, in antenatal care units, health workers had to propose explicitly the HIV test and to ask the women if they wanted to be tested or not. With these guidelines, after a pretest counseling on HIV, women are not asked any more if they want the HIV test, they have to explicitly refuse it. In terms of acceptance of the test, it makes a dramatic difference and a real increase. Certainly, from a public health point of view, it is good as it improves rates of HIV acceptance. Chandisarewa and colleagues (2007) reported improvement in acceptance and return for results. But attrition of the number of women is still important even in this study. HIV testing is only the entry point for a long process through pregnancy, delivery, and infancy that makes PMTCT work. What if women did not understand they had an HIV test? And what happens if this test was positive? How would they manage such “bad news” during pregnancy?
As Kakimoto pointed out (2008), we need a cautious evaluation of consequences of HIV testing at a large scale. Similarly, in some places in Africa, results of HIV testing are immediately given back to the women at the end of the antenatal session. It is not always easy for pregnant women to learn in such a rapid process they are HIV-infected, as a vast majority of them are surprised by this result, as Painter and colleagues (2007) showed in Abidjan. This method, while it improves the proportion of pregnant women learning about their HIV status, could have a limited impact if the stress produced by this news overwhelms the capacities of HIV-infected women to manage the PMTCT process.
In Mulago Hospital, in Uganda, Namukwaya and colleagues (2011) reported a dramatic difference between highly active antiretroviral therapy (HAART) and other regimens on rate of HIV infection in children, from 1.7% with HAART to over 30% in mothers who did not take any drug. The paper also shows the same cascade in this population where acceptance of HIV test among pregnant women is 99.7% and return for treatment or prophylaxis in HIV-infected women is 96.5%. They are around 60% that deliver in the same sites, and only 30% of children were early tested. We can always improve HIV testing (by new techniques or improvement in counseling), but we will still not understand why women do not come back for delivery and postnatal follow-up.
6 PMTCT Intervention and Access to Care for HIV-Infected Pregnant Women
From 1999 and the results of a randomized trial reported by Guay and colleagues (1999), the use of nevirapine for PMTCT has been recommended for a decade. The intervention is easy to implement and allows around 50% of reduction of HIV transmission from mother to child with a very low cost. However, quick emergence of resistance to nevirapine, which was also one of the most used drugs for treatment, hampered this intervention, as Arrivé and colleagues (2007) described it. As resistance occurs, it is necessary to use other drugs than nevirapine, both in mothers, as Lockman and colleagues (2010) have proved, and infected children who were exposed to nevirapine during pregnancy, as Palumbo and colleagues (2010) have proved. However, it remains as a possible intervention when nothing else is possible in remote rural places. But, as Stringer and colleagues (2010) showed in different African countries, even for such a simple intervention, in a large population of exposed children, they were only 51% who have actually a good coverage of nevirapine.
Since the last decade, there are PMTCT programs that include access to care for women and families. Some initiatives, as FSTI (Fonds de Solidarité Thérapeutique Internationale) or MTCT-Plus, have implemented HIV/AIDS care and treatment to families identified through PMTCT programs (Noba et al. 2001; Abrams et al. 2007). As reported by Toro (2010), these programs improve dramatically the proportion of retention of women in PMTCT and the mortality of HIV-infected women. Muchedzi and colleagues (2010) studied obstacles and challenges that pregnant women have to overcome to access HAART. And Stinson and colleagues (2010) noticed in South Africa that even when HAART and PMTCT programs are present, services fail to initiate a high proportion of eligible pregnant women on HAART.
7 PMTCT and Men
For at least one decade, there is an advocacy for the involvement of male partners of pregnant women in PMTCT. But, in most of the African countries, this involvement remains marginal and less than 10% of partners come for HIV testing through these PMTCT programs. We have to admit that antenatal care units are seldom men friendly and that it is certainly something that has to be improved. Aluisio and colleagues (2011) showed in Nairobi that a much higher attendance of men than usual (31%) is associated with a reduction in HIV infection and mortality in HIV-exposed children. Katz and colleagues (2009) in Kenya also presented ways to involve men and to increase HIV testing among them. In Côte d’Ivoire, in a prospective qualitative study, Tijou and colleagues (2009) described decision-making process about PMTCT and breastfeeding among couples. PMTCT actions should be an interaction between three actors (health workers, women, and their partners). In Uganda, Larsson and colleagues (2010) identified, through a qualitative study among fathers of HIV-exposed infants, many reasons that men argue for not having a test. They worry about relations in the couple after testing and prefer to have the opportunity to test themselves on their own, without “control” of their partner. In Uganda, as in other places, a misbelief has never been really addressed. When a woman is tested for HIV and share this result with her partner, quite often the partner consider that his HIV status is the same as the status of his partner. Therefore, it is useless to do the test! This should be specifically addressed in information campaigns.
8 Breastfeeding Under HAART and New Recommendations
Following the results of several clinical trials, WHO changed recommendations on breastfeeding HIV-exposed children (Kilewo et al. 2009; The Kesho Bora Study Group 2011). Clinical trials showed that HAART given to the mother until 6 months of breastfeeding was safe and prevented most of postnatal HIV infections. Curiously, in its recommendations, WHO extrapolated, without data, the protection duration of HAART until 1 year of age and proposed exclusive breastfeeding until 6 months and then mixed feeding. This recommendation of HAART during breastfeeding, either in mothers or in children, will certainly decrease dramatically postnatal transmission of HIV. But firstly, we do not know if it is feasible and if women are able to understand and follow all changes of feeding recommendations. Secondly, it is even more difficult for women who choose infant feeding alternatives to express their choices and to obtain infant formula. That reinforces health inequalities in a field where health authorities tried to reach equity. Thirdly, if a mother breastfeeds her HIV-exposed child until 1 year, it will be useless to test the infant before 1 year (as exposed), and the HIV-infected children will not be diagnosed in time and remain untreated. Even with HAART during breastfeeding, there will still be failures, and some children will be HIV-infected. These children will probably be resistant to several antiretroviral drugs such as nevirapine used in prophylaxis regimen in exposed children during breastfeeding. These rare HIV-infected children will be “scapegoats” of PMTCT programs.
9 Infant Testing and Large Access Testing in Children
Greater efforts are needed to scale up early testing of HIV-exposed infants, reduce the rate of loss to follow up among them, and further integrate HIV care with services for child health. As a clinical trial conducted by Violari and colleagues (2008) has shown, it is important to treat all HIV-infected children as soon as the diagnosis is carried out. And this diagnosis should be done as early as possible from 6 weeks of age. Unfortunately, until 12–15 months of life, we cannot use antibodies as a diagnosis tool, just as a first sorting tool to identify HIV-exposed children. Then, we need to use much more sophisticated techniques, such as real-time polymerase chain reaction tests, which are often available only in capital cities in Africa. For several years now, new techniques were developed as dried blood spots (DBS) for HIV (as it is used for decades for metabolic diseases in West countries in neonates). These DBS can be easily collected and transported from remote places to reference laboratories as it allows 1 month to 6 weeks to use them. It is only if this is developed everywhere in PMTCT sites in Africa that we can expect to have a real scale-up of early testing in exposed children and treatment in HIV-infected children. We can also expect to lower attrition in mothers if programs are able to give the diagnosis of exposed children early in life. In high prevalence settings, as emphasized by Rollins et al. (2009) and Kellerman and Essajee (2010), universal testing of children should be promoted, including immunization programs. Health workers should systematically propose the HIV test to ill children services, children in tuberculosis departments, malnourished children services, and also siblings of HIV-exposed children.
10 Conclusion
In conclusion, we can say that there has been a huge work on PMTCT during the last decade. The drug regimens for treatment and prophylaxis are effective, and there are regular improvements. There have also been improvements in programs and scaling up in Southern and East Africa. The effectiveness of PMTCT is not always good, and the eradication of mother-to-child transmission of HIV, as an objective, will be difficult to achieve by 2015. But we learn and progress day by day. There has been a very interesting and enlightening experience in South Africa that Doherty and colleagues (2009) developed. After a situation assessment, they improved training and supervision on a day-to-day basis in a district hospital. Improvements in coverage were really important in CD4 testing as well as in nevirapine intake and early diagnosis. This quality improvement intervention as a process and a way to identify, analyze, and resolve bottlenecks in PMTCT should be used everywhere when PMTCT indicators are not good. It is probably one of the best ways to try to achieve an eradication of mother-to-child transmission of HIV in Africa.
References
Abrams EJ, Myer L, Rosenfield A, El Sadr WM (2007) Prevention of mother to child transmission services as a gateway to family based human immunodeficiency virus care and treatment in resource limited settings: rationale and international experiences. Am J Obstet Gynecol 197:S101–S106
Aluisio A, Richardson BA, Bosire R, John-Stewart G, Mbori-Ngacha D, Farquhar C (2011) Male antenatal attendance and HIV testing are associated with decreased infant HIV infection and increased HIV-free survival. J Acquir Immune Defic Syndr 56:76–82
Anand A, Shiraishi RW, Sheikh AA, Marum LH, Bolu O, Mutsotso W et al (2009) Site factors may be more important than participant factors in explaining HIV test acceptance in the prevention of mother-to-child HIV transmission programme in Kenya, 2005. Trop Med Int Health 14:1215–1219
Arrivé E, Newell ML, Ekouevi DK, Chaix ML, Thiebaut R, Masquelier B et al (2007) Prevalence of resistance to nevirapine in mothers and children after single-dose exposure to prevent vertical transmission of HIV-1: a meta-analysis. Int J Epidemiol 36:1009–1021
Chandisarewa W, Stranix-Chibanda L, Chirapa E, Miller A, Simoyi M, Mahomva A et al (2007) Routine offer of antenatal HIV testing (“opt-out” approach) to prevent mother-to-child transmission of HIV in urban Zimbabwe. Bull World Health Organ 85:843–850
Curtis KM, Nanda K, Kapp N (2009) Safety of hormonal and intrauterine methods of contraception for women with HIV/AIDS: a systematic review. AIDS 23(suppl 1):S55–S67
Delvaux T, Nöstlinger C (2007) Reproductive choice for women and men living with HIV: contraception, abortion and fertility. Reprod Health Matters 15(suppl 29):46–66
Doherty T, Chopra M, Nsibande D, Mngoma D (2009) Improving the coverage of the PMTCT programme through a participatory quality improvement intervention in South Africa. BMC Public Health 9:406. doi:10.1186/1471-2458-9-406
Druce N, Nolan A (2007) Seizing the big missed opportunity: linking HIV and maternity care services in Sub-Saharan Africa. Reprod Health Matters 15:190–201
Duflo E, Dupas P, Kremer M (2009) Education and fertility: experimental evidence from Kenya. Massachusetts Institute of Technology. Working Paper
Dupas P (2009) Do teenagers respond to HIV risk information? Evidence from a field experiment in Kenya. PWP-CCPR-2009-066. California Center for Population Research: Online Working Paper Series
Elul B, Delvaux T, Munyana E, Lahuerta M, Horowitz D, Ndagije F et al (2009) Pregnancy desires, and contraceptive knowledge and use among prevention of mother-to-child transmission clients in Rwanda. AIDS 23(suppl 1):S19–S26
Guay LA, Musoke P, Fleming T, Bagenda D, Allen M, Nakabilto C et al (1999) Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother to child transmission of HIV-1 in Kampala, Uganda: HIVNET 012 randomised trial. Lancet 354:795–802
Johnson KB, Akwara P, Rutstein SO, Bernstein S (2009) Fertility preferences and the need for contraception among women living with HIV: the basis for a joint action agenda. AIDS 23(suppl 1):S7–S17
Kakimoto K (2008) Response to opt-out approach to prevent mother-to-child transmission of HIV. Bull World Health Organ 86:D
Katz DA, Kiarie JN, John-Stewart GC, Richardson BA, John FN, Farquhar C (2009) Male perspectives on incorporating men into antenatal HIV counseling and testing. PLoS ONE 4:e7602. doi:10.1371/journal.pone.0007602
Kellerman S, Essajee S (2010) HIV testing for children in resource-limited settings: what are we waiting for? PLoS Med 7. doi:10.1371/journal.pmed.1000285
Keogh SC, Urassa M, Kumogola Y, Mngara J, Zaba B (2009) Reproductive behaviour and HIV status of antenatal clients in northern Tanzania: opportunities for family planning and preventing mother-to-child transmission integration. AIDS 23(suppl 1):S27–S35
Kilewo C, Karlsson K, Ngarina M, Massawe A, Lyamuya E, Swai A et al (2009) Prevention of mother-to-child transmission of HIV-1 through breastfeeding by treating mothers with triple antiretroviral therapy in Dar es Salaam, Tanzania: The Mitra Plus study. J Acquir Immune Defic Syndr 52:406–416
Labhardt ND, Manga E, Ndam M, Balo JR, Bischoff A, Stoll B (2009) Early assessment of the implementation of a national programme for the prevention of mother-to-child transmission of HIV in Cameroon and the effects of staff training: a survey in 70 rural health care facilities. Trop Med Int Health 14:288–293
Larsson EC, Thorson A, Nsabagasani X, Namusoko S, Popenoe R, Ekström AM (2010) Mistrust in marriage – reasons why men do not accept couple HIV testing during antenatal care: a qualitative study in Eastern Uganda. BMC Public Health 10:769. http://www.biomedcentral.com/1471-2458/10/769
Leroy V, Sakarovitch C, Cortina-Borja M, McIntyre J, Coovadia H, Dabis D et al (2005) Is there a difference in the efficacy of peripartum antiretroviral regimens in reducing mother-to-child transmission of HIV in Africa? AIDS 19:1865–1875
Levy JM (2009) Women’s expectations of treatment and care after an antenatal HIV diagnosis in Lilongwe, Malawi. Reprod Health Matters 17:152–161
Lim Y, Kim JY, Rich M, Stulac S, Niyonzima JB, Smith Fawzi MC et al (2010) Improving prevention of mother-to-child transmission of HIV care and related services in Eastern Rwanda. PLoS Med 7. doi:10.1371/journal.pmed.1000302
Lockman S, Hughes MD, McIntyre J, Zheng Y, Chipato T, Conradie F et al (2010) Antiretroviral therapies in women after single-dose Nevirapine exposure. N Engl J Med 363:1499–1509
McKenna MT, Xiaohong H (2007) Recent trends in the incidence and morbidity that are associated with perinatal human immunodeficiency virus infection in the United States. Am J Obstet Gynecol 197:S10–S16
Msellati P (2009) Improving mothers’ access to PMTCT programs in West Africa: a public health perspective. Soc Sci Med 69:807–812
Muchedzi A, Chandisarewa W, Keatinge J, Stranix-Chibanda L, Woelk G, Mbizvo E et al (2010) Factors associated with access to HIV care and treatment in a prevention of mother to child transmission programme in urban Zimbabwe. J Int AIDS Soc 13:38. doi:10.1186/1758-2652-13-38
Namukwaya Z, Mudiope P, Kekitiinwa A, Musoke P, Matovu J, Kayma S et al (2011) The impact of maternal highly active antiretroviral therapy and short-course combination antiretrovirals for prevention of mother-to-child transmission on early infant infection rates at the Mulago national referral hospital in Kampala, Uganda, January 2007 to May 2009. J Acquir Immune Defic Syndr 56:69–75
Noba V, Sidibe K, Kaba K, Malkin JE (2001)Voluntary screening and prevention of mother-to-child transmission of HIV among pregnant women in Côte d’Ivoire: a public health program of the International Therapeutic Solidarity Fund. Paper presented at the 8th American conference on retrovirus and opportunistic infections, Chicago, USA, 4–8 February
Painter TM, Diaby KL, Matia DM, Lin LS, Sibailly TS, Kouassi MK et al (2004) Women’s reasons for not participating in follow up visits before starting short course antiretroviral prophylaxis for prevention of mother to child transmission of HIV: qualitative interview study. BMJ 329:543–548
Painter TM, Diaby KL, Matia DM, Lin LS, Sibailly TS, Kouassi MK et al (2007) Faithfulness to partners: a means to prevent HIV infection, a source of HIV infection risks, or both? A qualitative study of women’s experiences in Abidjan, Côte d’Ivoire. Afr J AIDS Res 6:25–31
Palumbo P, Lindsey JC, Hughes MD, Cotton MF, Bobat R, Meyers T et al (2010) Antiretroviral treatment for children with peripartum nevirapine exposure. N Engl J Med 363:1510–1520
Penda I, Msellati P (2010) Bottle neck of HIV PMTCT programmes in Cameroon. Analysis of 2008 data from “littoral” region. Paper presented at the XVIII International AIDS conference, Vienna, Austria, 18–23 July 2010. Abstract CDE1196
Rollins N, Mzolo S, Moodley T, Esterhuizen T, van Rooyen H (2009) Universal HIV testing of infants at immunization clinics: an acceptable and feasible approach for early infant diagnosis in high HIV prevalence settings. AIDS 23:1851–1857
Shetty KA, Marangwanda C, Stranix-Chibanda L, Chandisarewa W, Chirapa E, Mahomva A et al (2008) The feasibility of preventing mother-to-child transmission of HIVusing peer counselors in Zimbabwe. AIDS Res Ther 2008(5):17
Stinson K, Boulle A, Coetzee D, Abrams EJ, Myer L (2010) Initiation of highly active antiretroviral therapy among pregnant women in Cape Town, South Africa. Trop Med Int Health 15:825–832
Stringer EM, Chi BH, Chintu N, Creek TL, Ekouevi DK, Coetze D et al (2008) Monitoring effectiveness of programmes to prevent mother-to-child HIV transmission in lower-income countries. Bull World Health Organ 86:57–62
Stringer EM, Ekouevi DK, Coetzee D, Tih PM, Creek TL, Stinson K et al (2010) Coverage of nevirapine-based services to prevent mother-to-child HIV transmission in 4 African countries. J Am Med Assoc 304:293–302
The Kesho Bora Study Group (2011) Triple antiretroviral compared with zidovudine and single-dose nevirapine prophylaxis during pregnancy and breastfeeding for prevention of mother-to-child transmission of HIV-1 (Kesho Bora study): a randomised controlled trial. Lancet Infect Dis 11:171–180
Tijou Traore A, Querre M, Brou H, Leroy V, Desclaux A, Desgrées-du-Loû A (2009) Couples, PMTCT programs and infant feeding decision-making in Ivory Coast. Soc Sci Med 69:830–837
Toro PL, Katyal M, Carter RJ, Myer L, El Sadr WM, Nash D et al (2010) Initiation of antiretroviral therapy among pregnant women in resource-limited countries: CD4+ cell count response and program retention. AIDS 24:515–524
UNAIDS (2010) Global report: UNAIDS report on the global AIDS epidemic 2010. Geneva, Joint United Nations Programme on HIV/AIDS. UNAIDS/10.11E | JC1958E, Geneva
Violari A, Cotton MF, Gibb DM, Babiker AG, Steyn J, Madhi SA et al (2008) Early antiretroviral therapy and mortality among HIV-infected infants. N Engl J Med 359:2233–2244
World Health Organization (2003) Strategic approaches to the prevention of HIV infection in infants. Report of a WHO meeting, Morges, Switzerland, 20–22 March 2002. World Health Organization, Geneva. http://www.who.int/hiv/mtct/StrategicApproaches.pdf. Accessed 23 May 2011
World Health Organization (2007) Guidance on provider-initiated HIV testing and counselling in health facilities. World Health Organization, Geneva. http://whqlibdoc.who.int/publications/2007/9789241595568_eng.pdf. Accessed 23 May 2011
World Health Organization (2009) HIV and infant feeding. Revised Principles and Recommendations. Rapid Advice. World Health Organization, Geneva
Yéni P (2010) Prise en charge médicale des personnes infectées par le VIH. Rapport 2010. Recommandations du groupe d’experts. Direction Générale de la Santé. Agence Nationale de Recherches sur le SIDA et les hépatites virales, Paris
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Msellati, P. (2013). Improving Access to Mother-to-Child Transmission (PMTCT) Programs in Africa: An Ongoing Process. In: Liamputtong, P. (eds) Women, Motherhood and Living with HIV/AIDS. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-5887-2_11
Download citation
DOI: https://doi.org/10.1007/978-94-007-5887-2_11
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-5886-5
Online ISBN: 978-94-007-5887-2
eBook Packages: Humanities, Social Sciences and LawSocial Sciences (R0)