Abstract
Mindfulness meditation as an intervention to promote stress reduction has become increasingly studied and implemented over the last decade and consistently shows promising beneficial effects on psychological well-being. The development of mindfulness is integrated in several structured training programs and therapies such as mindfulness-based stress reduction, mindfulness-based cognitive therapy, as well as programs integrating mindfulness training specifically developed for cancer patients. These programs and therapies have shown promising results in improving different psychological outcomes. In particular, mindfulness-based stress reduction programs have shown a strong potential for changing peoples’ experiences of stress-related complaints and increasing well-being. A meta-analysis of results from randomized controlled studies of mindfulness training among cancer patients presented in this chapter gives support for the positive effect of such interventions. Results show moderate intervention effect sizes for increased positive affective outcomes, such as quality of life and frequency of positive experiences; increases in physical health outcomes and measures of mindfulness; and reduction of negative affective outcomes such as depression, anxiety, and perceived stress.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
8.1 Introduction
Mindfulness is a concept refers to a state of conscious awareness of present mental states and processes as they are here-and-now and the skills related to conscious awareness involving an observing, accepting attitude to one’s own experiences (Bishop et al. 2004). Training of mindfulness skills originates from Eastern meditation traditions, but during the past decades mindfulness has increasingly been used and integrated into Western forms of stress management interventions and different types of psychotherapy.
The two main components of mindfulness – a self-regulation of awareness towards present mental states and a non-evaluative openness and acceptance towards moment-to-moment experiences – can be trained by practicing various forms of meditation or through mental exercises (Kabat-Zinn 1990). The development of mindfulness is integrated in several structured training programs and therapies such as mindfulness-based stress reduction (MBSR) (Kabat-Zinn 1990), mindfulness-based cognitive therapy (MBCT) (Segal et al. 2002), dialectical behavior therapy (Linehan 1993), as well as acceptance and commitment therapy (Hayes 2005). These programs and therapies have shown promising results in improving different psychological outcomes. In particular, mindfulness based stress reduction programs have shown a strong potential for changing peoples’ experiences of stress-related complaints and increasing well-being (Baer et al. 2006; Bishop 2002; Bishop et al. 2004; Carlson et al. 2001; Grossman et al. 2004; Ott et al. 2006; Shapiro et al. 2006; Smith et al. 2005; Speca et al. 2000).
Among patients with cancer and cancer survivors several different interventions and therapies have been used to reduce stress and symptoms related to the diagnosis and treatment of their disease. In particular, the MBSR meditation program developed by Jon Kabat-Zinn (1990) and his colleagues at the Stress Reduction and Relaxation Clinic, Massachusetts Medical Center, and different adaptations of this program have been used. It has been shown to have potential to decrease stress and depression in cancer populations. It has shown positive effects on quality of life (QoL) and decreased stress symptoms in patients with varying cancer diagnoses. Studies have also shown promising results of MBSR programs on sleep disturbances among cancer patients.
In this chapter, a summary of current findings regarding mindfulness-based interventions for cancer patients are presented along with a description of the current knowledge regarding potential mechanisms and a suggested theoretical framework.
8.2 Mindfulness-based Programs for Cancer Patients
8.2.1 MBSR Program
The MBSR program is the most widely used mindfulness program. The program was developed by Kabat-Zinn and his colleagues (1990) at the Stress Reduction and Relaxation Clinic, Massachusetts Medical Center, USA. It was originally developed for patients with chronic pain, but has been applied for patients with a wide variety of medical diagnoses. It is a group-based program with up to 30 participants, and it involves 8–10 weekly sessions and consists of experiential and group exercises. During the program, the theoretical foundations of mindfulness regarding relaxation, meditation, and the body-mind connection are described. A variety of meditation, relaxation and yoga exercises are practiced during group sessions and at home. Participants are encouraged to practice meditation six days a week at home using an instruction tape during the 8-week period. Training involves body scan meditation, sitting and walking meditation and yoga exercises. The group process is focused on solving problems and challenges regarding successful meditation practice and the everyday application of mindfulness, and learning from each other’s experiences. An example of a suggested week-to-week schedule of a MBSR program is presented in Table 8.1.
8.2.2 MBCT
MBCT was developed by Segal et al. (2002) at the University of Oxford and is largely based on the MBSR-program. It is also an 8-week group-based intervention, and follows a manual combining mindfulness training with elements of cognitive therapy. MBCT was originally developed as an approach to prevent depression relapse, but has since been applied to a larger variety of mental complaints such as bipolar disorder, suicidal behavior, and social phobia (Keng et al. 2011), as well as for cancer patients (Foley et al. 2010). Similarly to cognitive behavioral therapy, MBCT puts its focus on helping participants to view thoughts as mental events rather than as facts and to recognize maladaptive automatic thoughts that maintain depressive symptoms (Segal et al. 2002). The difference from traditional cognitive behavioral therapy lies primarily in the emphasis put in MBCT on changing participants’ awareness of and relationship to thoughts and emotion, rather than trying to change the content of thoughts and encouraging the development of alternative thoughts. The theoretical assumption is that mindfulness meditation facilitates loosening the association between dysfunctional thoughts and negative emotions.
8.2.3 Variations of Mindfulness-based Interventions
There are a number of alternative mindfulness-based intervention programs that have been developed with influence from MBSR and MBCT programs. Some of these have also been applied among cancer patients. A program independently developed but similar to the MBSR specifically developed for use among cancer patients, mindfulness-based cancer recovery has been developed at the University of Calgary, Canada (Carlson et al. 2010). This program closely resembles the MBSR program but is specifically adjusted for patients with a cancer experience (Speca et al. 2000). Another variant of a mindfulness-based intervention used for cancer patients is mindfulness-based art therapy (MBAT). This program integrates mindfulness meditation training with art therapy within an 8-week supportive group therapy (Monti et al. 2006). The program includes opportunities for both verbal and non-verbal communication and is intended to increase emotion regulation capacity.
8.3 Effects of Mindfulness Interventions in Cancer Patients – A Meta-analysis
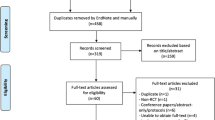
During the last decade, a fair amount of studies have been published that give support for positive effects of mindfulness-based interventions among cancer patients (Smith et al. 2005; Ledesma and Kumano 2009). The large majority of these studies are observational studies without a control group or lacking randomizations to control condition. Despite the methodological limitations of the studies of the effects of mindfulness interventions, there is substantial support for positive effect on indicators of well-being and physical health. To give additional strength to our knowledge about these effects, a meta-analysis of published randomized studies of mindfulness-based interventions for cancer patients was created. Searches in PubMed and PsychInfo databases with keywords “mindfulness” and “cancer” were screened for randomized controlled studies. Five studies were identified that reported adequate results from randomized controlled studies and had quantitative measures of either psychological or health outcomes. The studies reported a number of different outcomes, and for this meta-analysis, outcomes were categorized into four categories: positive affect, i.e. QoL (Monti et al. 2006; Lengacher et al. 2009; Foley et al. 2010); frequency of positive states of mind (Bränström et al. 2010); negative affect, i.e. depression (Lengacher et al. 2009; Bränström et al. 2010; Foley et al. 2010), anxiety (Lengacher et al. 2009; Bränström et al. 2010; Foley et al. 2010), perceived stress (Speca et al. 2000; Lengacher et al. 2009; Bränström et al. 2010; Foley et al. 2010), distress (Monti et al. 2006), negative mood (Speca et al. 2000), and post-traumatic stress symptoms (Bränström et al. 2010); and physical health, i.e. self-reported physical health (Speca et al. 2000; Monti et al. 2006; Lengacher et al. 2009).
The meta-analysis comprised a total of 453 individuals with a mix of different cancer diagnoses, a mean age of 54 years, and in all studies the large majority of participants were women (between 77 and 99%). All but one study (Lengacher et al. 2009) used a waiting-list control group, the control group in this study received care as usual. Details of the studies included in the analysis are presented in Table 8.2. The effect sizes were calculated based on means and standard deviation in intervention and control groups at baseline and post intervention follow-up. Fixed effects models were used to calculate effect sizes and we interpret these as small, medium, or large according to Cohen’s criteria (Cohen 1988), e.g. effect size of d = 0.20 as small, d = 0.50 as medium, and d = 0.80 as large. For studies with several measures within one outcome category, an average effect was calculated within this category. Results are presented in Table 8.3.
The study by Bränström et al. (2010) reports on findings among 71 patients with varying cancer diagnoses and examined an 8-week MBSR group training program. The study showed positive post-intervention effect on perceived stress [effect size (ES) = 0.63], post-traumatic avoidance symptoms (ES = 0.41), and positive states of mind (ES = 0.50). Further, the study showed that those who participated in the intervention reported a significant increase in mindfulness when compared to controls. The increase in mindfulness mediated the effects of the intervention on perceived stress, and post-traumatic avoidance symptoms. This mediation supports the assumption that mindfulness can be increased through exercises and that this increase in mindfulness can lead to positive psychological effects. The intervention study also indicated that the stress reduction intervention influenced the HPA axis functioning. Awakening cortisol was measured and among those with initial low levels of cortisol there was a post-intervention increase in cortisol, and among those with initial high levels there was a post-intervention decreased level of cortisol indicating a “normalization” of HPA axis functioning (Bränström et al. 2012). However, longer-term follow-up of the participants did not show significant effects of the intervention as compared to controls (Bränström et al. 2011b). Suggestions for future studies include the encouragement of continued post-intervention mindfulness training and the integration of mindfulness awareness in everyday life to promote longer-term effects.
The study by Foley et al. (2010) reports on findings among 115 patients with varying cancer diagnoses and examined the effect of an 8-week MBCT program. The study showed large post intervention increases in mindfulness (ES = 0.55) and clinically meaningful reductions in depression (ES = 0.83), anxiety (ES = 0.59), and distress (ES = 0.53) among those who participated in the program as compared to the waiting-list control participants. The study gives supports for providing MBCT training among cancer patients.
The study by Lengacher et al. (2009) reports on findings among 84 patients with breast cancer and examined the effect of a 6-week MBSR program. The study showed beneficial post-intervention effects in the group that participated in the program as compared to controls. The program resulted in lower depression, fear of recurrence, and higher energy, physical functioning, and physical role functioning. The study showed clinically meaningful changes on psychological outcomes and provides support for providing MBSR training to breast cancer patients.
The study by Speca et al. (2000) reports on findings among 90 patients with varying cancer diagnoses and examined the effect of a 7-week mindfulness-based training program specifically developed for cancer patients. The study showed beneficial post-intervention effects in the group that participated in the program as compared to controls. The program resulted in lower overall mood disturbance, depression, anxiety, anger, confusion, symptoms of stress, cardiopulmonary and gastrointestinal symptoms, emotional irritability, and cognitive disorganization. Participants in the program further reported higher levels of vigor that control participants. The study showed clinically meaningful changes on psychological and health outcomes and provides support for providing MBSR training to cancer patients.
The study by Monti et al. (2006) reports on findings among 93 women with varied cancer diagnoses and examined the effect of an 8-week MBAT program. The study showed decreased post-intervention symptoms of distress and improved health-related QoL among those who participated in the program as compared to controls. The study showed clinically meaningful changes on psychological outcomes and provides support for providing MBAT training to women with a cancer diagnosis.
8.3.1 Effects on Positive Affect Outcomes
Controlled studies of the effect of mindfulness-based interventions in varying populations have found support for an increase in positive affect, satisfaction with life, and QoL among participants participating in several different program such as MBSR (Anderson et al. 2007; Nyklicek and Kuijpers 2008; Bränström et al. 2010), MBCT (Kuyken et al. 2008; Foley et al. 2010; Godfrin and van Heeringen 2010), and MBAT (Monti et al. 2006). The meta-analysis of randomized controlled trials (RCTs) studying the effects of mindfulness-based interventions on measures of positive affect among cancer patients presented in this chapter gave an average medium effect size 0.36 on positive affect i.e. QoL and frequency of positive states of mind. This is of particular importance as positive affect has been suggested as an important facilitator promoting persistent and successful coping with stressful circumstances (Folkman and Moskowitz 2000; Folkman 2008), and an increasing number of studies give support for this assumption (Fredrickson et al. 2003; Moskowitz 2003; Moskowitz et al. 2008). However, all studies included in the meta-analysis showing an effect on positive affect had a relatively short follow-up period and reported results shortly after program completion. Only one RCT reports longer-term effects, and this study did not find significant intervention effects on positive affect at six months follow-up after baseline (Bränström et al. 2011b).
The increase in positive affect following mindfulness stress reduction training supports the use of mindfulness stress reduction training to increase well-being among cancer patients. Future research should focus on understanding which specific elements of the mindfulness training influence particular sub-dimensions of mindfulness and psychological outcomes. Studies among patients with specific cancer diagnoses at particular times after diagnosis might clarify when and for whom mindfulness interventions are the most efficient.
8.3.2 Effects on Negative Affect Outcomes
Previous controlled studies of the effect of mindfulness-based interventions conducted among populations with varying complaints have found support for decreases in negative affect such as depression, anxiety, psychological distress, perceived stress, and post-traumatic symptoms among participants participating in several different program such as MBSR (Shapiro et al. 1998; Speca et al. 2000; Williams et al. 2001; Anderson et al. 2007; Astin 1997; Koszycki et al. 2007; Sephton et al. 2007; Nyklicek and Kuijpers 2008; Bränström et al. 2010; Grossman et al. 2010), and MBCT (Kuyken et al. 2008; Hepburn et al. 2009; Godfrin and van Heeringen 2010; Thompson et al. 2010), and MBAT (Monti et al. 2006). The meta-analysis of RCTs studying the effects of mindfulness-based interventions on measures of negative affect among cancer patients presented in this chapter gave an average medium effect size 0.54 of negative affect, i.e. depression, anxiety, post-traumatic stress symptoms, perceived stress, distress, and negative mood. All studies included in the meta-analysis showing an effect on negative affect had a relatively short follow-up period and reported results shortly after program completion. Only one RCT reports longer-term effects, and this study did not find significant intervention effects on negative affect at six months follow-up after baseline (Bränström et al. 2011b).
Although more extended follow-up studies are needed, the results give support for a reduction of negative affective states and emotional distress in cancer patients as a result of mindfulness interventions.
8.3.3 Effects on Physical Health Outcomes
Although several smaller studies have demonstrated a potentially beneficial effect of mindfulness interventions on physical health outcomes such as sleep quality, physical well-being, and immunological functioning (Carlson et al. 2003, 2004; Carlson and Garland 2005), only a few controlled studies have shown effects of mindfulness-based interventions on physical health measures such as medical symptoms (Williams et al. 2001), activation in brain regions associated with present-focused self-reference (Farb et al. 2007), and self-reported health (Speca et al. 2000; Monti et al. 2006; Lengacher et al. 2009). The meta-analysis of RCTs studying the effects of mindfulness-based interventions on measures of physical health among cancer patients presented in this chapter gave an average medium effect size 0.40 for self-reported physical health. All studies included in the meta-analysis showing an effect on physical health outcomes had a relatively short follow-up period and reported results shortly after program completion.
Although increased body awareness might potentially increase perceived and reported bodily symptoms, no negative effects of mindfulness have been reported in the studies reviewed. Quite the opposite, the results from the current meta-analysis show increases on indicators of physical health. This is a promising result that lends support for the use of such interventions among cancer patients.
8.3.4 Effects on Measures of Mindfulness
A few controlled studies have reported effects of mindfulness-based interventions on different measures of mindfulness (Anderson et al. 2007; Nyklicek and Kuijpers 2008; Bränström et al. 2010). The meta-analysis of RCTs studying the effects of mindfulness-based interventions among cancer patients presented in this chapter gave an average medium effect size 0.62 on measures of mindfulness. Most studies reported an intervention effect of mindfulness training shortly after program completion. However, one RCT reports longer-term effects of mindfulness training and showed continued elevated levels of mindfulness at six months follow-up after baseline in the intervention group (Bränström et al. 2011b).
8.4 Components of Mindfulness Meditation Interventions
In the current research literature, there are a number of suggested theoretical models describing the mechanisms through which mindfulness interventions lead to positive outcomes.
Shapiro et al. (2006) describe a model with several components that together explains, mediates, and leads to positive effects of mindfulness training. They describe mindfulness as an inherent state of consciousness that entails “consciously attending to one’s moment-to-moment experience” (Shapiro et al. 2006). Reaching this state is enabled by practicing mindfulness and they describe three axioms that they see as essential building blocks of mindfulness: intention, attention, and attitude. Intention refers to the individual reason behind the initiation and continuation of a mindfulness practice. Attention refers to the self-regulation of attention to internal and external experiences as they unfold in the present moment. Attitude refers to the feelings and thoughts we attach to the experience we encounter as we attend mindfully, with an aim to cultivate a non-evaluative, accepting and curious attitude towards these experiences. They do not see the three axioms as separate processes but rather as simultaneous, interwoven processes that together account directly or indirectly for positive change related to mindfulness practice (Shapiro et al. 2006).
A number of related but more specific processes are described by Brown et al. (2007). They put a focus on the nature of consciousness and its relevance for mindfulness interventions and propose that insight, exposure, non-attachment, enhanced mind-body functioning, and integrated functioning are fundamental processes in the effects to mindfulness practice. According to Brown et al. (2007), practice of being mindful leads to an ability to pay attention in a new way, permitting a more direct contact with phenomena such as thought, emotions, sensations, and events as they occur, with less influence by habitual thought patterns and judgments. An ability to perceive events more objectively and to respond psychologically and behaviorally in a less automatic way is cultivated.
A third model describing the mechanisms of mindfulness has been presented by Baer et al. (2006). She developed a scale to capture different components of mindfulness, the Five Facet Mindfulness Questionnaire (FFMQ) (Baer et al. 2006, 2008). The instrument was developed by use of an exploratory factor analytic study of five independently developed mindfulness questionnaires. The analysis yielded five factors that appear to represent elements of mindfulness. The five facets were observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience (Baer et al. 2006). Several studies of the validity of the FFMQ supports the possibility to assess mindfulness by means of self-report and has shown a positive relationship between mindfulness and meditation experience (Baer et al. 2008), as well as a buffering effect of mindfulness on the negative effects of stress on psychological and health outcomes (Bränström et al. 2011a).
8.5 Mechanisms of Mindfulness Interventions – A Theoretical Framework
There are several possible pathways through which mindfulness might influence psychological functioning. Being mindful may lead to a view of thoughts and feelings as being transient, allowing the individual to view cognitions as “just thoughts” and affects as “just feelings”. This perspective may lead to less automatic thought patterns and rumination and can lead to more effective affect regulation and reduced reactivity to unpleasant states. Mindfulness also involves an acceptance of being with what is as opposed to having the need to alter present unpleasant states and striving towards future, more pleasant goals. This focus on being content with the present situation without constantly striving towards future possible states might in itself generate a greater sense of well-being and happiness that is not conditional on experience. Mindfulness might also promote physical and mental health through the promotion of relaxation and reduction of experiences of heightened physiological stress reactivity. Studies trying to measure different aspects of mindfulness have found increases in mindfulness to mediate the effect of MBSR programs (Nyklicek and Kuijpers 2008; Bränström et al. 2010).
Studies have further indicated an increase in rational decision-making among practitioners of regular mindfulness meditation (Kirk et al. 2011) and greater emotional information processing (Roberts-Wolfe et al. 2012). Of particular importance for the effects of mindfulness on psychological functioning has been the concept of self-compassion. Self-compassion has been described as entailing three major components: self-kindness (being kind rather than self-critical to oneself in instances of perceived inadequacy); common humanity (to see oneself as part of a greater whole rather that as separate and isolated); and mindfulness (in this case to view cognitions as “just thoughts” and affects as “just feelings” without over-identifying with them) (Neff and Vonk 2009). Without being an explicit goal, self-compassion is implicitly integrated into mindfulness-based programs. Although the mechanism of mindfulness is not yet well understood, some studies have found self-compassion to mediate the effect of MBCT on depressive symptoms (Kuyken et al. 2008).
In a recent review of the mindfulness literature Hölzel et al. (2011) propose a comprehensive theoretical framework integrating earlier suggested models. They suggest that four main components, in combination, can describe the mechanisms behind how mindfulness works: attention regulation; body awareness; emotion regulation, including reappraisal and exposure, extinction, and reconsolidation; and change in perspective on the self. Hölzel et al. (2011) suggest that together these components interact to improve self-regulation. A fuller description of their framework is presented in their article “How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective” (Hölzel et al. 2011) but a summary of each component is provided below. An illustration of the proposed theoretical model, its components, and the relationships between these components are presented in Fig. 8.1.
8.5.1 Attention Regulation
Focused attention is a fundamental aspect of meditation and in mindfulness practice. To increase ability to develop focused attention, practitioners are instructed to continuously pay attention to a specific object or sensation. Even if the mind wanders off, the practitioner is encouraged to return their focus to the chosen object or sensation. In mindfulness meditation, a focus on breathing is an essential starting point for this type of attention training. Participants in mindfulness meditation are typically instructed to focus their attention to their breath without being distracted, the air moving in and out, and the sensation of breathing. If the mind wanders off, they are instructed to make a mental note and return to focusing on their breathing. Self-report studies as well as some studies using cognitive tests and neuroimaging techniques, support the idea that mindfulness meditation practice increases the ability to disregard distractions and direct attention to relevant stimuli, and may lead to enhanced executive attention and attention regulation (Hölzel et al. 2011).
8.5.2 Body Awareness
Body awareness relates to the ability to pay attention to sensations and changes in the body. Exercises to increase the ability to notice bodily sensations are an important ingredient in mindfulness practice. These exercises often focus on the sensation of breathing, walking, scanning the body for tensions and sensations, as well as on integrating body awareness into everyday life. Some self-report studies give support for increased body awareness as a result of participation in mindfulness training programs (Carmody et al. 2008; Bränström et al. 2010). It is hypothesized, and some studies support the idea, that a higher degree of body awareness is related to and facilitates emotion regulation, and increases empathic responses (Hölzel et al. 2011).
8.5.3 Emotion Regulation
Emotion regulation is a complex and multi-componential process in which choice of situations, perception of situation, selective interpretation and appraisal of situation, and response modification can happen automatically or controlled, conscious or non-conscious (Gross 2007). Depending on a person’s individual goals, emotion regulation can lead to strengthening, weakening, or maintenance of emotions. Increased awareness of emotional sensation and increased ability to direct attention with less distraction is thought to enhance peoples’ ability to successfully regulate emotions. Hölzel et al. (2011) suggests that mindfulness increases the ability to regulate emotions, in particular through two regulatory processes: reappraisal and extinction.
Reappraisal is a process by which a stressful stimuli or situation is interpreted cognitively in a new and less stressful or threatening way so as to change its emotional impact (Gross 2007). A stressful event is seen as neutral, unthreatening, or even beneficial instead of as harmful. Mindfulness is thought to facilitate reappraisal and the process by which an initial appraisal of a threat is reinterpreted and seen in a different light by increased meta-cognitive ability (Garland et al. 2009). Meta-cognition involves taking a mental step back from thoughts and emotions, and thus facilitates reevaluation or shifting of perspectives.
When practicing mindfulness, individuals are instructed to focus their attention to thoughts, feelings, and emotions with an accepting and curious attitude, without direct reactivity. Training involves meeting both pleasant and unpleasant emotions by turning towards them, rather that turning away (Hölzel et al. 2011). This way of exposing yourself to unpleasant emotions when in a relaxed state and in safe circumstances is hypothesized to promote extinction of threatening emotions. Both the increased relaxation associated with mindfulness meditation and the increased attention regulation skills are thought to facilitate extinction as an emotion regulatory strategy. The ability to expose oneself to internal thoughts and feelings without direct reactivity has been measured with the “non-reactivity to inner experience” – subscale in the FFMQ, and has been shown to increase substantially as a result of participation in a mindfulness training intervention (Bränström et al. 2010).
8.5.4 Change in Perspective on the Self
The fourth and last component that describes the mechanisms behind how mindfulness works according to Hölzel et al. (2011) is change in perspective on the self. This refers to a view of the self as transient rather than static. This change is enabled by increased meta-awareness generated by mindfulness training. According to this view internal awareness becomes enhanced through meditation, and this enhanced awareness leads to the ability to observe mental processes with increased clarity and the sense of self can be experienced as an event rather than a static entity (Hölzel et al. 2011). The consequences of this change in perspective on the self is a more positive view of oneself, greater self-esteem, and a more accepting attitude towards ones’ emotional reactions and thoughts. An interview study of cancer patients participating in an 8-week MBSR training program gave support for the significance of the accepting attitude promoted by the program and training, as patients mentioned these aspects of mindfulness as important in interviews after the program (Kvillemo and Bränström 2011).
8.6 Clinical Significance
Getting a cancer diagnosis is coupled with many different stressful experiences both physically and emotionally. In addition to the excessive physiological stress caused by the disease and its treatment, many patients experience psychological stress regarding worries about diagnosis and prognosis, demanding treatments and treatment decisions, and disruption of ordinary life functions and roles (McGregor and Antoni 2009). Following treatment, patients commonly report psychological complaints such as depressive symptoms, anxiety, symptoms of stress, sleep disturbance, fear of recurrence, fatigue, and decreased QoL. Although many of these complaints may resolve over time, many patients experience extended suffering. A recent US study of long-term cancer survivors reported an increased prevalence of serious psychological distress in cancer survivors even among those who had been disease free for five years or more as compared to the general population (Hoffman et al. 2009). That study also showed that long-term psychological distress was more prevalent among those with less education and much more prevalent among younger cancer patients [odds ratio (OR)≥65 years, 95% confidence interval (CI) (reference value); OR45–64 years, 95% CI = 2.7 (1.8–4.0); OR<45 years, 95% CI = 5.6 (3.3–9.5)].
The findings from the studies included in the current meta-analysis are relevant for clinical practice as they indicate reduced psychological distress and increases on indicators of physical health among patients with a mix of cancer diagnoses. Even though the overall effect sizes were moderate, a reduction of psychological stress in conjunction to a cancer diagnosis and treatment are valuable and should be recommended. Foley et al. (2010) report clinically significant reductions in depression, anxiety, distress, and increased QoL compared to a waiting list control group. Similar results with reduction in perceived stress, post-traumatic stress symptoms, and increased positive affect was reported by Bränström et al. (2010). Clinical meaningful changes with improved psychological status and QoL in MBSR participants as compared to those treated with usual care were also reported by Lengacher et al. (2009). Monti et al. (2006) reported clinically significant reductions in symptoms of distress as well as increases in QoL measures among participants in a mindfulness training program as compared to wail-list controls. Finally, Speca et al. (2000) reported reduction in depression, anxiety, anger, confusion, and overall symptoms of stress, as well as an increase in vigor, among MBSR participants as compared to controls.
8.7 Integration of Mindfulness Meditation in Cancer Care, and Future Directions
Although mindfulness-based interventions for cancer patients holds great promise for reduction of negative mental and physical consequences of a cancer diagnosis, more high quality studies of mindfulness-interventions for cancer patients with active control groups, longer follow-ups, and studies among both men and women are needed to clarify issues such as for whom, when and exactly how mindfulness interventions can be most effective. Further studies should examine questions related to the implementation of mindfulness-based interventions in health care settings such as: Which patients benefit the most from participation in mindfulness training, e.g. type of cancer, disease stage? At what stage in the cancer treatment process should programs be offered? What is the optimal length of a mindfulness-based program? Are there alternative means of program delivery than group based programs e.g. internet-based interventions?
These questions are yet to be answered before we can fully and successfully integrate mindfulness interventions into cancer care. However, the relative low risk with providing patients with this type of treatment coupled with the increasing scientific support for such interventions gives no reason to discourage dissemination and implementation of mindfulness practice in cancer care. To facilitate dissemination and increase the availability of this type of treatments, the development of manual-based easily administered individual, group, and internet-based interventions should be encouraged.
References
Anderson ND, Lau MA, Segal ZV, Bishop SR (2007) Mindfulness-based stress reduction and attentional control. Clin Psychol Psychother 14:449–463
Astin JA (1997) Stress reduction through mindfulness meditation. Effects on psychological symptomatology, sense of control, and spiritual experiences. Psychother Psychosom 66(2):97–106
Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L (2006) Using self-report assessment methods to explore facets of mindfulness. Assessment 13(1):27–45
Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S et al (2008) Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment 15(3):329–342
Bishop SR (2002) What do we really know about mindfulness-based stress reduction? Psychosom Med 64(1):71–83
Bishop SR, Lau M, Shapiro S, Carlson L, Andreson ND, Carmody J et al (2004) Mindfulness: a proposed operational definition. Clin Psychol Sci Pract 11(3):230–241
Bränström R, Kvillemo P, Brandberg Y, Moskowitz JT (2010) Self-report mindfulness as a mediator of psychological well-being in a stress reduction intervention for cancer patients – a randomized study. Ann Behav Med 39(2):151–161
Bränström R, Duncan LG, Moskowitz JT (2011a) The association between dispositional mindfulness, psychological well-being, and perceived health in a Swedish population-based sample. Br J Health Psychol 16(Pt 2):300–316
Bränström R, Kvillemo P, Moskowitz JT (2011b) A randomized study of the effects of mindfulness training on psychological well-being and symptoms of stress in patients treated for cancer at 6-month follow-up. Int J Behav Med 19(4):535–542
Bränström R, Kvillemo P, Åkerstedt T (2012) Effects of mindfulness training on levels of cortisol in cancer patients. Psychosomatics pii:S0033–3182(12)00076–X
Brown KW, Ryan RM, Creswell JD (2007) Mindfulness: theoretical foundations and evidence for its salutary effects. Psychol Inq 18(4):211–237
Carlson LE, Garland SN (2005) Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med 12(4):278–285
Carlson LE, Ursuliak Z, Goodey E, Angen M, Speca M (2001) The effects of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients: 6-month follow-up. Support Care Cancer 9(2):112–123
Carlson LE, Speca M, Patel KD, Goodey E (2003) Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med 65(4):571–581
Carlson LE, Speca M, Patel KD, Goodey E (2004) Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology 29(4):448–474
Carlson L, Speca M, Segal ZV (2010) Mindfulness-based cancer recovery. New Harbinger Publications, Inc., Oakland
Carmody J, Reed G, Kristeller J, Merriam P (2008) Mindfulness, spirituality, and health-related symptoms. J Psychosom Res 64(4):393–403
Cohen J (1988) Statistical power analysis for the behavioral sciences. L. Erlbaum Associates, Hillsdale
Farb NA, Segal ZV, Mayberg H, Bean J, McKeon D, Fatima Z et al (2007) Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Soc Cogn Affect Neurosci 2(4):313–322
Foley E, Baillie A, Huxter M, Price M, Sinclair E (2010) Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: a randomized controlled trial. J Consult Clin Psychol 78(1):72–79
Folkman S (2008) The case for positive emotions in the stress process. Anxiety Stress Coping 21(1):3–14
Folkman S, Moskowitz JT (2000) Positive affect and the other side of coping. Am Psychol 55(6):647–654
Fredrickson B, Tugade M, Waugh C, Larkin G (2003) What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J Pers Soc Psychol 84:365–376
Garland E, Gaylord S, Park J (2009) The role of mindfulness in positive reappraisal. Explore (NY) 5(1):37–44
Godfrin KA, van Heeringen C (2010) The effects of mindfulness-based cognitive therapy on recurrence of depressive episodes, mental health and quality of life: a randomized controlled study. Behav Res Ther 48(8):738–746
Gross J (2007) Handbook of emotion regulation. The Guilford Press, New York
Grossman P, Niemann L, Schmidt S, Walach H (2004) Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res 57(1):35–43
Grossman P, Kappos L, Gensicke H, D’Souza M, Mohr DC, Penner IK et al (2010) MS quality of life, depression, and fatigue improve after mindfulness training: a randomized trial. Neurology 75(13):1141–1149
Hayes SC (2005) Get out of your mind & into your life: the new acceptance & commitment therapy. New Harbinger Publications, Oakland
Hepburn SR, Crane C, Barnhofer T, Duggan DS, Fennell MJ, Williams JM (2009) Mindfulness-based cognitive therapy may reduce thought suppression in previously suicidal participants: findings from a preliminary study. Br J Clin Psychol 48(Pt 2):209–215
Hoffman KE, McCarthy EP, Recklitis CJ, Ng AK (2009) Psychological distress in long-term survivors of adult-onset cancer: results from a national survey. Arch Intern Med 169(14):1274–1281
Hölzel B, Lazar S, Gard T, Schuman-Olivier Z, Vago D, Ott U (2011) How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci 6(6):537–559
Kabat-Zinn J (1990) Full catastrophe living: using the wisdom of your body and mind to face stress, pain and illness. Delacourt, New York
Keng SL, Smoski MJ, Robins CJ (2011) Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev 31(6):1041–1056
Kirk U, Downar J, Montague PR (2011) Interoception drives increased rational decision-making in meditators playing the ultimatum game. Front Neurosci 5:49
Koszycki D, Benger M, Shlik J, Bradwejn J (2007) Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behav Res Ther 45(10):2518–2526
Kuyken W, Byford S, Taylor RS, Watkins E, Holden E, White K et al (2008) Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. J Consult Clin Psychol 76(6):966–978
Kvillemo P, Bränström R (2011) Experiences of a mindfulness-based stress-reduction intervention among patients with cancer. Cancer Nurs 34(1):24–31
Ledesma D, Kumano H (2009) Mindfulness-based stress reduction and cancer: a meta-analysis. Psychooncology 18(6):571–579
Lengacher CA, Johnson-Mallard V, Post-White J, Moscoso MS, Jacobsen PB, Klein TW et al (2009) Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology 18(12):1261–1272
Linehan MM (1993) Skills training manual for treating borderline personality disorder. The Guilford Press, New York
McGregor BA, Antoni MH (2009) Psychological intervention and health outcomes among women treated for breast cancer: a review of stress pathways and biological mediators. Brain Behav Immun 23(2):159–166
Monti DA, Peterson C, Kunkel EJ, Hauck WW, Pequignot E, Rhodes L et al (2006) A randomized, controlled trial of mindfulness-based art therapy (MBAT) for women with cancer. Psychooncology 15(5):363–373
Moskowitz JT (2003) Positive affect predicts lower risk of AIDS mortality. Psychosom Med 65(4):620–626
Moskowitz JT, Epel ES, Acree M (2008) Positive affect uniquely predicts lower risk of mortality in people with diabetes. Health Psychol 27(1 Suppl):S73–S82
Neff KD, Vonk R (2009) Self-compassion versus global self-esteem: two different ways of relating to oneself. J Pers 77(1):23–50
Nyklicek I, Kuijpers KF (2008) Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Ann Behav Med 35(3):331–340
Ott MJ, Norris RL, Bauer-Wu SM (2006) Mindfulness meditation for oncology patients: a discussion and critical review. Integr Cancer Ther 5(2):98–108
Roberts-Wolfe D, Sacchet M, Hastings E, Roth H, Britton W (2012) Mindfulness training alters emotional memory recall compared to active controls: support for an emotional information processing model of mindfulness. Front Hum Neurosci 6:15
Segal ZV, Williams JMG, Teasdale JD (2002) Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. Guilford Press, New York
Sephton SE, Salmon P, Weissbecker I, Ulmer C, Floyd A, Hoover K et al (2007) Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: results of a randomized clinical trial. Arthritis Rheum 57(1):77–85
Shapiro SL, Schwartz GE, Bonner G (1998) Effects of mindfulness-based stress reduction on medical and premedical students. J Behav Med 21(6):581–599
Shapiro SL, Carlson LE, Astin JA, Freedman B (2006) Mechanisms of mindfulness. J Clin Psychol 62(3):373–386
Smith JE, Richardson J, Hoffman C, Pilkington K (2005) Mindfulness-Based Stress Reduction as supportive therapy in cancer care: systematic review. J Adv Nurs 52(3):315–327
Speca M, Carlson LE, Goodey E, Angen M (2000) A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med 62(5):613–622
Thompson NJ, Walker ER, Obolensky N, Winning A, Barmon C, Diiorio C et al (2010) Distance delivery of mindfulness-based cognitive therapy for depression: project UPLIFT. Epilepsy Behav 19(3):247–254
Williams KA, Kolar MM, Reger BE, Pearson JC (2001) Evaluation of a Wellness-Based Mindfulness Stress Reduction intervention: a controlled trial. Am J Health Promot 15(6):422–432
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Bränström, R. (2013). Effect of Mindfulness-based Interventions in Cancer Care. In: Cho, W. (eds) Evidence-based Non-pharmacological Therapies for Palliative Cancer Care. Evidence-based Anticancer Complementary and Alternative Medicine, vol 4. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-5833-9_8
Download citation
DOI: https://doi.org/10.1007/978-94-007-5833-9_8
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-5832-2
Online ISBN: 978-94-007-5833-9
eBook Packages: MedicineMedicine (R0)