Abstract
Anticancer-related adverse events, particularly chemotherapy-induced nausea and vomiting, are significant problems for both healthcare professionals and patients. The use of alternative medicine is receiving more recognition for control of such adverse events as an adjunct therapy along with administration of anti-emetics. This chapter examines the current available research evidence on the efficacy of acupuncture and moxibustion for reducing anticancer treatment-induced nausea and vomiting as well as safety of such treatments, searching the major databases resulted in four systematic reviews and three new trials being identified and reviewed. These evidence supports the use of acupoint-stimulation for reducing chemotherapy-induced nausea and vomiting in both adult and pediatric cancer patients with very low risk of serious adverse events. Concerning different stimulation methods, acupressure on pericardium meridian demonstrate reasonably strong evidence for reducing the severity of acute nausea. Electroacupuncture on pericardium meridian can alleviate acute vomiting. In contrast, manual acupuncture and non-invasive stimulation methods fail to provide strong evidence for such effect. A meta-analysis of two small-scale studies showed significantly beneficial effects of moxibustion but further large-scale studies are needed to provide indisputable recommendations for practice. Overall, well-designed studies with a large sample size are needed for developing a solid evidence base that promotes acupuncture and moxibustion in cancer care.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
6.1 Introduction
The practice of acupuncture originated in China over 3,500 years ago. Today, acupuncture is widely used throughout the world and is one of the main pillars of traditional Chinese medicine. Acupuncture has become increasingly popular in Western world and is often referred to as medical acupuncture in that context. The general theory of acupuncture is based on the premise that there are patterns of energy flow (Qi) through the body that are essential for good health. Disruptions of this flow are believed to be responsible for disease. Acupuncture may correct imbalances of flow at identifiable points close to the skin (Ma 2009).
Acupuncture is a therapeutic technique that involves stimulation of anatomical locations on the skin by a variety of techniques. The most studied mechanism of stimulation of acupuncture points employs penetration of the skin by thin, solid, metallic needles, which are manipulated manually (manual acupuncture) or by electrical stimulation (electroacupuncture) (Ezzo et al. 2006; Urroz et al. 2012). Electrical stimulation can also be applied via electrodes on the skin surface or by a relief band, a wristwatch-like device (non-invasive electrostimulation). Pressure can be applied either by pressing on the point with the fingers or by wearing an elastic wristband with an embedded stud (acupressure) (Ezzo et al. 2006; Allais et al. 2012).
Several professional bodies have provided recommendations and guidelines for using acupuncture for several indications, including various types of pain and several kinds of nausea and vomiting (Cassileth et al. 2007; Deng et al. 2007, American Cancer Society (http://www.cancer.org/Treatment/TreatmentsandSideEffects/ComplementaryandAlternativeMedicine/ManualHealingandPhysicalTouch/acupuncture?sitearea = ETO), World Health Organization (http://apps.who.int/medicinedocs/en/d/Js4926e/6.html)). They all recognize the beneficial effects of acupuncture for controlling anticancer treatment-induced nausea and vomiting and recommend its clinical use for managing such symptoms.
The acupuncture points that have been widely used for nausea control are Neiguan (PC6) and Zusanli (ST36) (World Health Organisation 2003). PC6 is located between the tendons of palmaris longus and flexor carpi radialis at 2 body-inches proximal to the wrist crease (1 body-inch is the greatest width of a patient’s thumb at the distal phalanx). ST36 is located on the anterior lateral side of the leg, 1 body-inch from the anterior crest of the tibia (World Health Organisation 2003). PC6 is the most commonly used acupuncture point to control nausea and vomiting, and PC6 can be stimulated by various methods (Ezzo et al. 2006).
Stimulation of these areas by moxibustion—the use of a cone or cylinder of dried herbs burned on or near the skin at acupuncture points to strengthen blood, stimulate Qi and maintain general health—is most commonly practiced in conjunction with acupuncture (Manheimer et al. 2009). In traditional Chinese medicine moxibustion can be used on its own or to augment the effect of acupuncture needles.
A number of other indications have been investigated, but there is a lack of adequate evidence to recommend for or against use of these indications (Manheimer et al. 2009). In some cases, this is due to methodological challenges inherent in acupuncture trials, such as placebo control and blinding. Other challenges include the diversity of approaches, the practice of individualizing treatment for each patient, and practitioners’ differing skill levels. However, the body of trial data for acupuncture continues to grow, with innovative approaches to these methodological quandaries being developed.
Many acupuncture-related adverse events , most of them owing to improper technique have been described (Zhang et al. 2010). Adverse effects due to improper sterilization and disposing of needles can lead to infection or cross-transmission of human immunodeficiency virus , hepatitis and other infectious diseases. Mild side effects, including bleeding or bruising at needles sites, fainting, and nausea, may also occur. Complications , including bent or broken needles, typically occur due to improper technique. Serious adverse effects, however, are few, and acupuncture can generally be considered inherently safe in the hands of well-trained practitioners (Zhang et al. 2010).
This book chapter is designed to provide an evidence-based guide on using acupuncture and/or moxibustion to control anticancer therapy-induced nausea and vomiting based on a thorough systematic review of the available scientific studies. Furthermore, this chapter contains a detailed methodology and practical processes for assessing, pooling, disseminating and using the best available international evidence concerning acupuncture. In all healthcare systems, there is a growing consensus that evidence-based practice offers the most responsible course of action for improving health outcomes. All clinicians and healthcare professionals want to provide the best possible care for patients, families and communities, and our aim in this chapter is to close the gap between evidence and action, and therefore make this possible.
6.2 SR Method
To identify existing evidence, the following major databases were searched: PubMed, CINAHL, EMBASE, TRIP, Cochrane Library, CCTR (Cochrane Controlled Trials Registry) and JBI Library. Regarding the use of acupuncture, a previous Cochrane systematic review (SR) (2006) examined studies published up to 2003. Therefore, this particular search was extended to identify new trials published from 2004 to the current date (October 2011) with specific reference to the use of acupuncture. Concerning trials that used moxibustion, one SR (2010) considered studies published until 2005 and this search for new trials aimed to identify relevant studies published from 2006 to the present (March 2012). The search aimed to identify randomised controlled trials (RCT) and SRs of RCTs published in any language. This resulted in the finding that the majority of studies were published in English and a few were published in Chinese.
6.3 Result for Acupuncture
The database search identified two SRs investigating the effectiveness or adverse events of acupuncture for chemotherapy-induced nausea and vomiting (CINV) in patients with mixed cancer type (Ezzo et al. 2006) and patients with only breast cancer (Chao et al. 2009). A third SR reported on adverse events caused by acupuncture (Ladas et al. 2010). The details of the three SRs are presented in Table 6.1. The details of the primary studies from the three SRs are listed in Table 6.2.
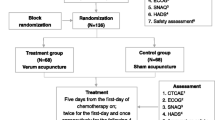
Three new trials were also identified as reporting on the effects of acupuncture (Reindl et al. 2006; Gottschling et al. 2008) or a combination of acupressure and acustimulation (Melchart et al. 2006). These include one trial on adult patients (Melchart et al. 2006) and two trials on paediatric patients (Reindl et al. 2006; Gottschling et al. 2008). The study by Reindl et al. (2006) constituted a preliminary report of Gottschling et al. (2008). As such only the latest study (Gottschling et al. 2008) was reviewed in this chapter.
6.3.1 A Cochrane SR by Ezzo et al. (2006)
Ezzo et al. (2006) examined the evidence for the effectiveness of acupuncture therapies including manual acupuncture , electroacupuncture, acupressure and non-invasive electro stimulation for controlling CINV in patients of any age group and cancer type.
The databases searched were MEDLINE, EMBASE, PsychLIT, MANTIS, Science Citation Index, CCTR (Cochrane Controlled Trials Registry), Cochrane Complementary Medicine Field Trials Register, Cochrane Pain, Palliative Care and Supportive Care Specialized Register, Cochrane Cancer Specialized Register, and conference abstracts. The SR included studies published up to 2003. The inclusion criteria were any type of cancer, any stage of cancer and any age group as long as the outcomes of interest were related to chemotherapy-induced nausea and/or vomiting. The review identified 11 RCTs of moderate to high quality. The details of the primary studies consisting of SRs are provided in Table 6.2.
The review defined acute nausea and vomiting as being events occurring within 24 h following the initiation of chemotherapy, and delayed nausea and vomiting referred to such events occurring after 24 h to 5–8 days (Ezzo et al. 2006).
All studies administered standard anti-emetics for both experimental and control groups. Most included studies used an anti-emetic regimen following the American Society of Clinical Oncology (ASCO) guidelines using 5-HT3 antagonist plus steroid prior to chemotherapy, and steroid plus either metoclopramide or a 5-HT3 antagonist for delayed nausea. The results of the review will be presented in a later section.
6.3.2 A Systematic Review by Chao et al. (2009)
A more recently published SR by Chao et al. (2009) examined the effectiveness of acupoint-stimulation for chemotherapy-induced adverse events including CINV for patients with breast cancer.
This particular review searched studies published from 1999–2008 in the English and Chinese languages. Eleven studies discussed CINV but only following three (Roscoe et al. 2005; Dibble et al. 2007; Molassiotis et al. 2007) were deemed to be of reasonably high quality, scoring three out of five using the modified Jade scale (Jadad et al. 1996). Consequently, this chapter discusses only the data from these three studies.
The SR analysed the data narratively without pooling. The detailed results of the SR are presented in a later section in this chapter.
6.3.3 New Trials
The details of the three newly identified trials are listed in Table 6.3.
6.3.4 Studies Examining Manual Acupuncture or Electroacupuncture
From the Cochrane SR, the following four studies assessed manual acupuncture and electroacupuncture. Manual acupuncture involves insertion and manual rotation of needles while electroacupuncture employs electrical stimulation via inserted needles.
Only one study used manual acupuncture and it failed to identify evidence that encouraged the use of manual acupuncture for treating CINV. Streitberger et al. (2003) examined whether manual acupuncture reduces chemotherapy-induced acute nausea and vomiting on 80 patients with various types of cancer . The acupuncture was applied at PC6 for 30 min both before the first chemotherapy session and the following day. Deqi sensation was elicited, which is a sensation that patients feel when the needle reaches the Qi level. The needle was left for 20 min without further manipulation. The control group received non-invasive placebo acupuncture at the same point. As for anti-emetics, all patients received 8 mg of 5-HT3 without steroid. The result did not show a statistically significant benefit of acupuncture compared with the control (p = 0.82) concerning the occurrence of acute nausea and vomiting.
The following three studies assessed electroacupuncture but no indisputable evidence was found to promote the use of electroacupuncture for reducing CINV. In the three studies, all patients received anti-emetics following the ASCO guideline. A study by Shen et al. (2000) used three-armed parallel group design to compare: (1) low frequency (2–10 Hz) electroacupuncture at PC6 and ST36 points for 20 min, (2) acupuncture with fake electrostimulation, and (3) no acupuncture. One hundred and four females with breast cancer participated. The intervention was provided 2 h before chemotherapy every day over a 5-day period. A statistically significant reduction in the frequency of vomiting was found in the electroacupuncture group compared with the other two groups during the study period (p < 0.001). However, no significant difference was found in the follow-up period (6–9 days) regarding the number of vomiting episodes.
Dundee et al. (1987, 1988) reported two small studies with conflicting results. However, due to the small sample size in both studies, the results should be interpreted with caution. A first study by Dundee et al. (1987) examined acupressure at PC6. Deqi was elicited. Electroacupuncture was applied (10 Hz, pulse width 0–25 ms) using a DC stimulator. Ten patients with testicular cancer participated. The session was held for 5 to 6 times over 3 days. At least 8 h interval was maintained between each session. The control group received sham acupuncture in the right elbow. The result showed significant reduction of nausea in the group with acupuncture on PC6 over the acupuncture on sham point group (p < 0.001).
Another study by Dundee et al. (1988) used the same intervention involving 20 patients with various types of cancer. The session was held for 5 min prior to the chemotherapy or soon after the initiation of chemotherapy. The control group received only anti-emetics. There was no statistically significant group difference (risk ratio (RR) 0.50; 95% CI 0.17 to 1.46).
In the next section, the data are pooled, if appropriate, to determine the effectiveness of acupuncture and/or electroacupuncture according to acuity of nausea and vomiting. No other SRs or primary studies were identified from the search addressing the effectiveness of manual acupuncture or electroacupuncture for anticancer treatment-induced nausea and vomiting for all age groups.
6.3.4.1 Effects of Acupuncture or Electroacupuncture for Nausea and Vomiting Within 24 h
Since no new SRs or new primary studies were identified, the data presented by the Cochrane SR (2006) are deemed the most up-to-date evidence.
Only one study was identified that assessed manual acupuncture. The use of manual acupuncture (Streitberger et al. 2003) did not provide statistically significant effects on acute vomiting. Similarly, use of manual acupuncture did not provide significant reduction in severity of acute nausea (standard mean difference (SMD) 0.02; 95% CI −0.42 to 0.40; p = 0.9).
The Cochrane SR pooled the data from the three studies reporting on electroacupuncture. The electroacupuncture group indicated significantly fewer episodes of acute vomiting (57%) over the control group (80%) (RR 0.76; 95% CI 0.60 to 0.97; p = 0.02). The SR also pooled the data from all four studies to determine the overall effects of acupuncture involving insertion of needles (manual acupuncture and/or electroacupuncture) for CINV.
Acute vomiting occurred in 37% of the acupuncture group and 60% in the control group. The meta-analysis revealed that acupuncture alone or electroacupuncture can significantly reduce acute vomiting (RR 0.74; 95% CI 0.57 to 0.94; p = 0.01).
From these results, the following evidence is derived to guide practice:
-
Electroacupuncture can be used to reduce chemotherapy-induced acute vomiting in conjunction with standardized anti-emetics.
-
There is no reasonable evidence to encourage the use of manual acupuncture for reducing CINV. Further high quality studies are required.
-
There is a lack of evidence supporting the use of electroacupuncture for reducing chemotherapy-induced acute nausea. More high quality studies are required.
6.3.4.2 Effects of Acupuncture or Electroacupuncture for Nausea and Vomiting after 24 h
Of the four acupuncture or electroacupuncture studies from the Cochrane SR, no studies reported on the outcomes concerning delayed nausea and vomiting that occurred 24 h or later after chemotherapy began. No new trial and no other SR was found that addressed delayed nausea and vomiting.
Judging by these results the following evidence statement can be drawn:
-
No sufficient data were available to determine the effect of manual or electroacupuncture for reducing chemotherapy-induced delayed nausea and vomiting.
6.3.5 Studies Examining Acupressure
Acupressure involves pressure on the acupuncture point by finger or devices such as a small plastic button attached to a self-administering device. The Cochrane SR reviewed three studies reporting on the effects of acupressure for improving CINV and the SR by Chao et al. (2009) also reported a further two studies. Of five primary studies from the SRs, four reported favourable results for encouraging the use of acupressure while one study found a conflicting result.
Using a three-armed controlled trial design, Roscoe et al. (2003) compared bilateral acupressure band (SeaBand ) on PC6 point, single acustimulation band (ReliefBand ) and anti-emetics only (Roscoe et al. 2005). The study involved 747 patients who are receiving initial doxorubicin or cisplatin . The bilateral bands were worn on both wrists. The single acustimulation band was worn on one wrist but the patients were allowed to wear it on their wrist or alternated between wrists as desired. These patients were also allowed to the change level of stimulation between 10 to 35 mA as desired. Both bands were given to patients prior to the chemotherapy and they were worn for 5 days. All patients received anti-emetics as recommended in the ASCO guideline. The study indicated a favourable result for the acupressure group with significantly less acute nausea compared to the other two groups (p < 0.05). For acute vomiting and delayed nausea or vomiting, no significant group differences were reported. Furthermore, acustimulation resulted in significantly less nausea and vomiting only in men (p < 0.05) compared to the control group. Women showed less but not statistically significant acute nausea in the acupressure group compared to the control group (p = 0.052).
In a small study by Dibble et al. (2000), seventeen women with breast cancer were instructed to administer self-acupressure at PC6 and ST36 points for up to 3 min in the morning before chemotherapy and anytime throughout the day if required. The control group received only anti-emetics. Anti-emetics were administered following the ASCO guideline. The study highlighted significantly fewer episodes of nausea (p < 0.01) and nausea intensity (p < 0.04) in the acupressure group during the first 10 days of the chemotherapy cycle compared to the control group.
Another study by Dibble et al. (2007) was reviewed in the SR by Chao et al. (2009). The study involved in total 160 women with breast cancer receiving chemotherapy. The duration of follow-up was 21 days and it emerged that acupressure had a statistically significant effect in reducing the amount of delayed vomiting and delayed intensity of nausea. In contrast, no significant effects were demonstrated for acute nausea or vomiting compared with the sham point group and control group.
A study by Molassiotis et al. (2007) included in the SR by Chao et al. (2009) also reported favourable results supporting the use of acupressure. Thirty-six patients with breast cancer were allocated either to the SeaBand group or control group. SeaBand was worn for 5 days following chemotherapy. The result demonstrated acupressure provided beneficial effects by inducing fewer experiences of nausea and retching, and occurrence of nausea, vomiting and retching and distress were all significantly lower in the experimental group compared to the control group. The experience of vomiting was not statistically significant. Caution should be applied to these results due to the small sample size. The authors also noted that the use of standardized anti-emetics was not possible from day 2 to day 3 due to ethical considerations.
A study by Noga et al. (2002) from the Cochrane SR (Ezzo et al. 2006) reported a conflicting outcome. The study examined whether the use of an acupressure wrist band can reduce chemotherapy-induced acute nausea and vomiting and delayed nausea and vomiting. One hundred and twenty patients with hematologic cancer were involved . SeaBand was worn at PC6 for 24 h following chemotherapy. The control group received an acupressure band at a sham point. All patients received anti-emetics following the ASCO guideline. The result did not confirm beneficial effects that had been reported in other studies. The authors reported no significant group difference in patients’ demographic data. No significant difference was found in the demographic data of patients in both groups. The authors called for further clinical trials with placebo -controlled design and investigation of the mechanism of acupressure on the human body.
6.3.5.1 Effects of Acupressure on Acute Nausea and Vomiting
The Cochrane SR conducted a meta-analysis using data from two studies (Dibble et al. 2000; Roscoe et al. 2005) that reported on the same outcome measures (mean severity of acute nausea). Other studies could not be pooled due to reported outcome measures at different time points. The pooled data showed that acupressure had a positive effect on reducing mean acute nausea severity over control within the first 24 h (SMD −0.19; 95% CI −0.37 to −0.01; p = 0.04).
Based on this result the following evidence statement can be made:
-
The use of acupressure may reduce the severity of chemotherapy-induced acute nausea.
The data from three studies were combined to determine the effects on acute vomiting. Overall, 17% of patients in the acupressure group and 20% in control group had acute vomiting. However the difference was not statistically significant (RR 0.83; 95% CI 0.60 to 1.16; p = 0.3).
Based on this analysis, the following evidence statement can be elucidated:
-
There is no strong evidence to support the use of acupressure band for reducing chemotherapy-induced acute vomiting.
6.3.5.2 Effects on Delayed Nausea and Vomiting
The following evidence statement can be drawn:
-
No indisputable evidence was found to support or to discourage the use of acupressure for reducing chemotherapy-induced delayed nausea or vomiting.
In addition, Melchart et al. (2006) reported on the combination of acupuncture and acupressure for CINV but the study failed to demonstrate a beneficial effect of such a combination. Twenty-eight cancer patients were randomly allocated to the experimental group with a combination of acupuncture and acupressure at point PC6 while the control group used a close sham point. The study was conducted over one chemotherapy cycle. The study did not find any statistically significant difference between the experimental group and the control group at the sham point for the nausea score. The authors suggested that more large-scale studies are required.
6.3.6 Studies Examining Non-invasive Electrostimulation
Non-invasive electrostimulation provides electrostimulation on the surface of the skin without insertion of acupuncture needles or application of pressure on acupuncture point(s). The Cochrane SR reviewed five studies assessing non-invasive electrostimulation for reducing chemotherapy-induced nausea and/or vomiting. The SR by Chao et al. (2009) also reported on one new study. Overviews of all six studies are presented in the following section. These studies used transcutaneous electrical nerve stimulation (TENS) with wrist band on the PC6 point. Three studies reported some beneficial effects of non-invasive acustimulation for CINV, while two studies found no significant effects on nausea or vomiting at any time point during the study period.
A double-blind, placebo-controlled parallel-subjects trial with a follow-up cross-over trial by Pearl et al. (1999) compared TENS with ReliefBand on PC6 and sham ReliefBand at the same point for managing chemotherapy-induced nausea and/or vomiting. Forty-two patients with gynaecologic cancer participated in the trial. All patients were given ReliefBand following their discharge from the hospital after chemotherapy and the band was worn for 7 days. All patients received anti-emetics as recommended in the ASCO guideline. Of these 42 patients, 32 were evaluable for the parallel-subjects component, 16 in each group. The percentage of patients with absent or minimal nausea was 59% overall, which was similar to that for both the active (56%) and placebo (62%) groups. The incidence and severity of nausea and vomiting was similar for each group. Eighteen patients completed two consecutive cycles and were evaluable for the cross-over component. The average age of the cross-over patients and their dose intensity were comparable with those of the overall study population (56.3 vs 58.6 years and 22.7 vs 22.7 mg/m2/week, respectively). Overall, the percentage of cycles with absent or minimal nausea was 47%, which was similar to that of the active (50%) and placebo (44%) cycles. However, the severity of nausea was significantly less in the active cycles during days 2–4. Patients averaged less than one episode of vomiting daily in each cycle.
The study showed that the ReliefBand is an effective adjunct to standard anti-emetic agents for controlling nausea induced by cisplatin-based chemotherapy in gynecologic oncology patients.
Roscoe et al. (2002) reported that TENS had beneficial effects for delayed nausea and vomiting as well as less rescue anti-emetic pills being required. Their study compared the effects of TENS (ReliefBand ) on the control group without any acustimulation. Forty-two patients with breast cancer , lung cancer , ovarian cancer or colorectal cancer were involved in this study. Patients in the experimental group wore the band before chemotherapy for as long as helpful. All patients received anti-emetics including ondansetron and granistron without dexamethasone. This was not consistent with the ASCO guideline. There was no statistically significant difference between the groups regarding the severity of nausea. The experimental group had less delayed nausea and vomiting compared with the control group (p < 0.06). The use of significantly less anti-emetic pills was reported in the experimental group (p < 0.05).
A study by Treish et al. (2003) also compared the effect of TENS using active ReliefBand and sham ReliefBand with 49 patients experiencing a range of cancers. The band was worn at the beginning of the chemotherapy session for 5 days. Both groups received an anti-emetics regimen that was consistent with the ASCO recommendation. The active ReliefBand group indicated significantly less overall vomiting (p = 0.05), overall retching (p = 0.05), and overall nausea severity (p = 0.01) over the five-day study period compared to the controls with sham ReliefBand. Furthermore, utilizing active ReliefBand significantly reduced delayed vomiting (p = 0.032) and acute nausea (p = 0.028) and delayed nausea (p = 0.02) periods. However, due to the small sample size, this result should be treated cautiously. The authors suggested larger and well-designed RCTs are required to build a strong evidence base.
The following three studies did not find any significant benefits of acustimulation for CINV at any time during the designated study periods.
The study by Roscoe et al. (2003) has already been addressed in the section on acupressure. The study failed to demonstrate that acustimulation had any positive effects in reducing CINV.
Another study by Roscoe et al. (2005) was reviewed by Chao et al. (2009). The study compared acustimulation wrist band (ReliefBand) with active stimulation, sham acustimulation, and no acustimulation in 96 women experiencing breast cancer. No significant difference was found in any outcomes including acute nausea, delayed nausea, vomiting, quality of life (QoL) and total amount of anti-emetic medication used.
A final study included in the Cochrane SR was conducted by McMillan et al. (1991). The study also compared TENS stimulation on PC6 and anti-emetics consisting of only 16 patients receiving chemotherapy for 5 consecutive days. The result failed to demonstrate that TENS had a significant benefit in reducing acute nausea (SMD −0.16; 95% CI −1.14 to 0.82).
6.3.6.1 Effects on Acute Nausea and Vomiting
The Cochrane SR pooled the data from five studies to determine the effect of non-invasive electrostimulation for reducing chemotherapy-induced acute nausea. The analysis showed no statistically significant effect (SMD −0.07; 95% CI −0.23 to 0.10; p = 0.43).
The data from two studies (Pearl et al. 1999; Roscoe et al. 2002) were pooled to determine the effect of non-invasive electrostimulation for reducing acute vomiting. The incident rate of acute vomiting in each group was 22% in the intervention group and 24% in the control group. No statistically significant effect was found (RR 0.90; 95% CI 0.67 to 1.19; p = 0.45) between the groups.
The later study by Roscoe et al. (2005) also reported that acustimulation for acute nausea and vomiting elicited a non-significant effect.
Based on these results, the following evidence statement can be made:
-
There is no evidence to encourage the use of non-invasive electrostimulation for reducing chemotherapy-induced acute nausea and vomiting.
6.3.6.2 Effects on Delayed Nausea and Vomiting
The meta-analysis of all four studies demonstrated no significantly positive effects of non-invasive electrostimulation for delayed nausea (SMD 0.03; 95% CI −0.14 to 0.19; p = 0.73).
The data from two studies (Pearl et al. 1999; Roscoe et al. 2002) were pooled to determine the effect of non-invasive electrostimulation for delayed vomiting. The meta-analysis showed that non-invasive electrostimulation had no positive effects over the control group (SMD 0.06; 95% CI −0.11 to 0.22; p = 0.49) in regard to reducing delayed vomiting.
From these results, the following evidence statement can be made as follows:
-
There is no evidence to encourage the use of non-invasive electrostimulation for reducing chemotherapy-induced delayed nausea and/or delayed vomiting.
6.3.7 All Acupoint-stimulation Methods
The Cochrane SR also pooled the data from all 11 studies to assess whether acupoint -stimulation regardless type of method, is effective in reducing CINV. The result showed that the incidence of acute vomiting had a statistically significant reduction (RR 0.82; 95% CI 0.69 to 0.99; p = 0.04). No significant reduction was reported in other outcomes including delayed vomiting, acute nausea and delayed nausea.
Based on this result, the following evidence statement can be established:
-
Acupoint-stimulation regardless of type of stimulation method, may reduce chemotherapy-induced acute vomiting. However, it should be noted that any beneficial effects of each method have not yet been demonstrated yet except for electroacupuncture and acupressure .
6.3.8 Acupuncture for Pediatric Patients
One newly identified study examined whether acupuncture can reduce the necessity to use rescue anti-emetics for CINV in pediatric oncology patients.
Reindl et al. (2006) presented the preliminary results of their multicenter cross-over study at five tertiary hospitals in Germany. This was completed in 2008 and published in Gottschling et al. (2008). Therefore, the data from Reindl et al. (2006) was not reviewed. Nonetheless the report demonstrated promising findings that encourage the use of acupuncture in pediatric oncology.
In a cross-over trial reported by Gottschling et al. (2008), 23 children (13.6 ± 2.9 years of age) with solid malignant tumor were randomly allocated to acupuncture treatment during either the second or third identical chemotherapy course. All patients received standard anti-emetics. The acupuncture required significantly less rescue anti-emetics compared to the control (p = 0.001). Significantly fewer occurrences of vomiting were also reported (p = 0.01). Only four out of 23 patients reported pain from receiving a needle.
Based on this result, the following evidence statement can be developed:
-
Acupuncture as a supportive anti-emetic approach may reduce the need for anti-emetic rescue medication during highly emetogenic chemotherapy in pediatric cancer patients. However, trials with a large sample size are required to develop a solid evidence base.
6.3.9 Safety of Acupoint-stimulation
One SR and one new trial reported on side effects caused by acupuncture. Overall, the studies found that acupuncture is safe to use for most patients.
Jindal et al.’s review (2008) of commonly reported adverse reactions caused by acupuncture was based on 22 clinical trials for patients of any age range and conditions. These included the following scenarios: sedation (32.05%), needle pain (26.33%), neuropathy/nervous system-related issues (15.96%), MSK/connective tissue-related issues (14.22%), puncture redness/irritation (6.94%), hematomas (1.04%), feelings of faintness/sycope (1.04%), vascular disorder (0.69%), hysterectomy (0.35%), headache (0.35%) and unscheduled overnight hospital admission (0.35%).
From nine clinical trials involving 782 pediatric patients (2–18 years of age) (Schlager et al. 1998; Shenkman et al. 1999; Radmayr et al. 2001; Somri et al. 2001; Rusy et al. 2002; Wang and Kain 2002; Alimi et al. 2003; Butkovic et al. 2005; Reindl et al. 2006), a total of 29 acupuncture/sham adverse events were reported caused by acupuncture (incidence rate 1.55 per 100 acupuncture treatments). The most common adverse reaction in pediatric patients was puncture redness. The risk of serious adverse event was 5.36/10,000 treatments in pediatrics and 0.05/10,000 treatments in the overall population. The details of nine studies are presented in Table 6.4.
A more recently published retrospective chart review (Ladas et al. 2010) concerned 32 patients (237 acupuncture sessions) undergoing treatment for cancer or stem cell transplantation. Japanese J-type Seirin needles were inserted at 0.5-cun depth, with mild manual stimulation. Of these patients, many had thrombocytopenia including severe (20%), moderate (8%) and mild (19%) thrombocytopenia. However, no bleeding side effects were reported.
From these results, the following evidence statement is developed:
-
Acupuncture can be considered a safe treatment method for both adults and pediatric patients. However, clinicians should be aware of possible adverse events so that they can provide timely interventions.
6.4 Results for Moxibustion
Lee et al. (2010a) published a SR of clinical trials examining the effectiveness of moxibustion for managing cancer. In addition, Lee et al. (2010b) recently published an umbrella review of existing SRs on various clinical conditions. Because of overlapping and duplication of findings on nausea and vomiting in anticancer treatment, only the data from the first SR (Lee et al. 2010a) is reported here. The detailed information on the SR (Lee et al. 2010a) is summarised in Table 6.5.
Further information on the included primary studies in the SR by Lee et al. (2010b) is presented in Table 6.6.
6.4.1 A Systematic Review by Lee et al. (2010)
The major databases searched included MEDLINE, EMBASE, AMED, Cochrane Library, Scopus and CINAHL for studies published up to June 2007. The review identified the following two trials.
One RCT by Chen et al. (2000) compared salt-separated moxibustion on Shenque (CV8) with control. Fifty-six patients with stages III and IV of nasopharyngeal carcinoma were involved and all underwent radiotherapy and chemotherapy according to the AD protocol. The experimental group received the moxibustion on 30 occasions from the beginning of the radiotherapy and chemotherapy sessions. The experimental group showed significantly less occurrence of side effects than the control group (p < 0.05).
The other study concerned a three-armed trial involving 36 patients with gastric cancer (Cao et al. 1997). The patients were randomly assigned to the following groups: moxibustion on CV8 three times per week, control, and drug therapies for side effects . The analysis showed that the moxibustion group received a significant benefit (p < 0.05) compared to the other groups.
6.4.1.1 Effects of Moxibustion
The data from the two trials were pooled to determine the effectiveness of moxibustion for reducing cancer treatment-induced nausea and vomiting. A moxibustion group (n = 80) experienced significantly less frequency of nausea and vomiting caused by chemotherapy (RR 0.38, 95% CI 0.22–0.65; p = 0.0005, heterogeneity: chi square 0.18, p = 0.67, I2 = 0%).
From these results, the following evidence statement is developed:
-
The use of moxibustion may be effective for reducing nausea and vomiting induced by cancer therapies. However, the methodological quality of the included two studies is not high. More RCTs with large sample sizes are required to develop a strong evidence base to justify the use of moxibustion in cancer care.
6.4.2 Safety of Moxibustion
The existing trials did not report on adverse effects caused by moxibustion. High quality clinical trials are required to determine the safety of moxibustion for cancer patients who undergo chemotherapy.
6.5 Mechanism of Acupuncture and Moxibustion on Anti-nausea and Vomiting
The mechanisms behind the beneficial anti-emetic impacts of acupuncture are well explained by Takahashi (2011), largely based on its neuromodulation effect in the gut. This paper proposes that acupuncture stimulation of somatosensory neurons activates various nuclei at the CNS, including the nucleus tractus solitarius (NTS) , the dorsal motor nucleus of vagi (DMV) , the rostral ventrolateral medulla (RVLM) , and periaqueductal gray (PAG) . Activation of the NTS, DMV and RVLM modulates the imbalance between sympathetic and parasympathetic activity. Opioid released from the PAG is involved in mediating the anti-emetic and anti-nociceptive effects of acupuncture.
Acupuncture treatment involves the insertion of thin needles into the skin and underlying muscle and the subsequent manual or electrical stimulation of the needles . Thus, acupuncture stimulates the somatic afferent nerves of the skin and muscles. Somatic sensory information from the body is carried to the cortex area of the brain. Somatic sensory fibers also project to the various nuclei at the brain stem and hypothalamus . Through the process of somato-autonomic reflex, acupuncture modulates various biomechanical responses, such as prokinetic, anti-emetic, and anti-nociceptive effects (Takahashi 2011).
The role of polymodal receptors (PMRs) has also been emphasized based on the fact that PMRs are responsive to both acupuncture and moxibustion stimuli. Thermal sensitivity is essential in moxibustion therapy, and the characteristics of acupuncture points and trigger points are similar to those of sensitized PMRs. Axon reflexes mediated by PMRs may represent the mechanism whereby acupuncture and moxibustion trigger immediate action (Lin and Chen 2008).
Experiments in healthy human subjects have shown that electrical stimulation of acupuncture points may enhance the regularity of gastric myoelectrical activity. For example electroacupuncture at PC6 reduces gastric tachyarrhymia in vection-induced motion sickness in healthy volunteers (Hu et al. 1992). Combined acupuncture at ST36 and PC6 increases the percentage of regular slow waves, resulting in the normalization of arrhythmia in healthy humans (Lin et al. 1997). However, the mechanisms of acupuncture’s anti-emetic effect were not explained in these studies.
Published data from experimental studies imply the evidence that acupuncture does have an anti-emetic effect. The level of plasma arginine vasopressin is rapidly elevated in response to diverse emetic stimuli such as motion stimuli (Kim et al. 1997) and anticancer drugs (Edwards et al. 1989; Cubeddu et al. 1990). Intravenous injection of vasopressin results in vomiting and retching in humans (Kim et al. 1997) and dogs (Carpenter et al. 1984; Chen et al. 2003). Acupuncture at ST36 and PC6 attenuates symptom scores of emesis induced by vasopressin infusion in dogs (Chen et al. 2003). Retrograde propulsive movement is closely linked to the frequency of retching and vomiting. Electroacupuncture at PC6 reduces the frequency of retrograde propulsive movement induced by vasopressin in dogs (Tatewaki et al. 2005).
Studies investigating the relationship between acupuncture and endogenous opiates (beta-endorphin, enkephalin, endomorphin and dynorphin) agreed with the contention that in normal animal models , lower frequency electroacupuncture stimulates the release of beta-endorphin , enkephalin and endomorphin , which in turn activates the mu- and delta-opioid receptors. Further higher frequency electroacupuncture stimulates dynorphin which activates the kappa-opioid receptor (Lin and Chen 2008). Opioids have dual effects—an anti-emetic effect as well as an emetic effect. It has been shown that central opioid plays a major role in mediating the anti-emetic effect (Costello and Borison 1977). The emetic effect is mediated via the chemoreceptor trigger zone (CTZ) , whereas the anti-emetic effect is mediated via the vomiting center (Costello and Borison 1977; Blancquaert et al. 1986; Foss et al. 1998). The CTZ is contained in the area postrema on the caudal margin of the fourth ventricle. Since the area postrema has no blood brain barrier, naloxone methiodide (a peripheral opioid antagonist) can antagonize the emetic effect of opioid mediated via the CTZ. In contrast, the vomiting center is located deep beneath the solitary tract of the caudal brain stem. Both the emetic and anti-emetic effects of opioid can be blocked by naloxone , because naloxone can cross the blood brain barrier (Foss et al. 1998).
Naloxone hydrochloride, but not naloxone methiodide, abolishes the anti-emetic effect of electroacupuncture at PC6 in dogs (Tatewaki et al. 2005). This suggests that the anti-emetic effect of electroacupuncture at PC6 is mediated via the central opioid pathway.
Figure 6.1 is a visual presentation of the anti-emetic mechanism of acupuncture point stimulation.
To sum up, it has been stated with reference to traditional Chinese medicine, that “acupuncture is believed to restore the balance of yin and yang”. This has been translated into Western medical terminology as meaning: “Acupuncture modulates the imbalance between parasympathetic and sympathetic activity” (Takahashi 2011). Acupuncture may be effective in patients with functional gastrointestinal (GI) disorders and in particular nausea and vomiting due to chemotherapy. This is because it has a neuromodulation effect on GI motility and the mechanism involving endogenous opiates (Takahashi 2011).
6.6 Practical Guidelines for Clinicians
The best-practical methods/procedures for various types of acupoint-stimulation have not been fully investigated using a rigorous scientific approach. More well-designed studies are required to determine factors related to the best outcomes such as best timing, length, duration and frequency for providing such interventions to reduce anticancer treatment-induced nausea and vomiting. The following guideline has been developed based on the reviewed trials and available guidelines provided by various professional bodies.
For any type of acupressure-point stimulation, patients should be fully informed about the benefits and possible harm. Clinicians should be aware of the risk of a serious adverse event such as pneumothorax and appropriate safeguards should be in place.
6.6.1 Practical Guideline for Manual or Electroacupuncture
Based on the available evidence, the following recommendations can be made for reducing CINV:
-
Patient type: Patients with breast cancer , testicular cancer or possibly other types of cancer. Cancer patients with prior history of CINV. WHO (http://apps.who.int/medicinedocs/en/d/Js4926e/6.html) also recommends the use for radiotherapy-induced nausea and vomiting. Contraindication could be the site of a tumor or metastatic limbs with lymphedema, areas with considerable anatomic distortion due to surgery . Careful consideration is required in applying to patients with thrombocytopenia , coagulatopathy or nuetropenia.
-
Acupuncture point(s): PC6 alone or with ST36.
-
Needle type: Sterile single use needles.
-
Insertion technique: From available studies, no strong scientific evidence was found regarding insertion technique. However, Deqi sensation should be elicited.
-
Length and timing of procedure: Preferably before chemotherapy (5 min to 2 h before chemotherapy) for 20 min for 5 days or longer.
-
Electrostimulation: 2 to 10 Hz.
-
Anti-emetics: The anti-emetics should be provided following the ASCO guideline.
6.6.2 Practical Guideline for Acupressure
Based on the available evidence, the following recommendations can be drawn for reducing CINV:
-
Patient type: Patients with breast cancer or patients with cancer who receive doxorubicin or cisplatin . Patients with prior history of chemotherapy induced nausea and vomiting.
-
Acupuncture point(s): PC6 or possibly with ST36.
-
Length and timing of procedure: Acupressure band or self acupressure device should be used before the commencement of chemotherapy for 3–6 min. Patients should be encouraged to use the acupressure as desired for 5 days or longer.
-
Others: The anti-emetics should be provided following the ASCO guideline.
6.6.3 Practical Guideline for Non-invasive Electrostimulation
Due to the lack of scientific evidence on the efficacy of non-invasive electrostimulation for controlling anticancer treatment-induced nausea and vomiting, clinicians’ judgement is required when introducing non-invasive electrostimulation for patients. Other types of acupuncture are recommended including electroacupuncture and acupressure based on available evidence:
-
Patient type: Patients with breast cancer, lung cancer, gynaecologic cancer, or colorectal cancer patients who had previous history of CINV. Possibly patients with other types of cancer may be also considered.
-
Acupuncture point: PC6.
-
Length and timing of procedure: TENS device such as a ReliefBand should be worn before chemotherapy or soon after chemotherapy for 5–7 days or as long as patient feels that it is helping.
-
Intensity of stimulation: Patients should be allowed to adjust the strength by turning the dial from 10–35 mA.
-
Others: The anti-emetics should be provided in accordance with the ASCO guideline.
6.6.4 Practical Guideline for Pediatric Patients
Based on the available evidence, the following recommendations can be made for clinicians:
-
Patient type: Patients aged from six to eighteen with solid malignant tumor or possibly other types of cancer.
-
Acupuncture point: PC6.
-
Length and timing of procedure: Acupuncture (or laser acupuncture if needle pain is felt) for 20 min on a first day preferably before chemotherapy starts, and every day throughout the chemotherapy course.
-
The standard anti-emetics based on the ASCO guideline should be administered.
6.6.5 Practical Guideline for Moxibustion
Again, due to the extremely limited number of high quality studies reporting on the efficacy of moxibustion and the effective practical methods for applying moxibustion, strong recommendations are not possible. Again, well-designed large scale studies are required to develop the scientific evidence base to promote the use of moxibustion for oncological care:
-
Patients: Patients who undergo anticancer treatments such as chemotherapy and/or radiotherapy for nasopharyngeal cancer, gastric cancer or possibly other types of cancer.
-
Moxibustion point: CV8.
-
Type of moxibustion treatment: Only “indirect method” was reported (indirect placement of moxibustion on some insulating material such as ginger, sale or others).
-
Timing and frequency: At the beginning of the anticancer treatment, three times or more up to around 30 times throughout the treatment.
-
Types of grass: No sufficient evidence was identified from available reports but salt-separated moxibustion was used.
6.7 Conclusion
This chapter has provided a review of currently available evidence on the efficacy and safety of acupuncture and moxibustion for reducing anticancer treatment-induced nausea and vomiting. All trials accessed acupuncture as an adjunct therapy for standardized anti-emetic drugs . Overall, evidence supports the use of acupoint-stimulation for reducing CINV in both adult and pediatric cancer patients with very low risk of serious adverse events . However, reasonably strong evidence is available only for electroacupuncture and acupressure on PC6. Electroacupuncture on PC6 can reduce acute nausea and vomiting while acupressure on PC6 is effective for reducing acute nausea. No indisputable scientific evidence was found to promote or discourage the use of manual acupuncture or non-invasive acupoint stimulation method . Some evidence supports the use of moxibustion but further studies are required to determine the levels of safety in clinical application. A lack of well-designed studies with a large sample size is a serious issue for developing a solid evidence base where acupuncture and moxibustion can be used widely.
References
Alimi, D., Rubino, C., Pichard-Léandri, E., Fermand-Brulé, S., Dubreuil-Lemaire, M. L., & Hill, C. (2003). Analgesic effect of auricular acupuncture for cancer pain: A randomized, blinded, controlled trial. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 21, 4120–4126.
Allais, G., Rolando, S., Castagnoli, G. I., Burzio, C., Airola, G., Borgogno, P., et al. (2012). Acupressure in the control of migraine-associated nausea. Neurology Science, 33, S207–210.
Blancquaert, J., Lefebvre, R. A., & Willems, J. L. (1986). Emetic and antiemetic effects of opioids in the dog. European Journal of Pharmacology, 128, 143–150.
Butkovic, D., Toljan, S., Matolic, M., Kralik, S., & Radesić, L. (2005). Comparison of laser acupuncture and metoclopramide in PONV prevention in children. Paediatric Anaesthesia, 15, 37–40.
Cao, J., Xiao, X. H., & Tang, X. Y. (1997). Elemene fluorouracil Moxibustion “Shenque” effect in the treatment of advanced gastric cancer observed. Chinese Journal of Clinical Oncology, 24, 549–550.
Carpenter, D., Briggs, D. B., & Strominger, N. (1984). Peptide-induced emesis in dogs. Behavioural Brain Research, 11, 277–281.
Cassileth, B., Deng, G. E., Gomez, J. E., Johnstone, P. A., Kumar, N., & Vickers, A. J. (2007). American College of Chest Physicians. Complementary therapies and integrative oncology in lung cancer: ACCP evidence-based clinical practice guidelines (2nd ed.). Chest, 132, 340S–354S.
Chao, L., Zhang, A. L., Liu, H. E., Cheng, M. H., Lam, H. B., & Lo, S. K. (2009). The efficacy of acupoint stimulation for the management of therapy-related adverse events in patients with breast cancer: A systematic review. Breast Cancer Research and Treatment, 118, 255–267.
Chen, K., Jiang, Y., Wen, H., Lu, X. Z., Lu, L., Wang, H. et al. (2000). Clinical study on treatment of nasopharyngeal carcinoma by radio and chemotherapy with supplementary moxibustion on Shenque point. Chinese Journal of Integrative Medicine, 20, 733–735.
Choo, S., Kong, K., Lim, W., Gao, F., Chua, K., & Leong, S. (2006). Electroacupuncture for refractory acute emesis caused by chemotherapy. The Journal of Alternative and Complementary Medicine, 12, 963–969.
Chen, J., Qian, L., Ouyang, H., & Yin, J. (2003). Gastric electrical stimulation with short pulses reduces vomiting but not dysrhythmias in dogs. Gastroenterology, 124, 401–409.
Costello, D. J., & Borison, H. L. (1977). Naloxone antagonizes narcotic self blockade of emesis in the cat. The Journal of Pharmacology and Experimental Therapeutics, 203, 222–230.
Cubeddu, L., Lindley, C. M., Wetsel, W., Carl, P. L., & Negro-Vilar, A. (1990). Role of angiotensin II and vasopressin in cisplatin-induced emesis. Life Sciences, 46, 699–705.
Deng, G., Cassileth, B. R., Cohen, L., Gubili, J., Johnstone, P. A., & Kumar, N. (2007). Society for integrative oncology executive committee. Integrative oncology practice guidelines. Journal of the Society for Integrative Oncology, 5, 65–84.
Dibble, S. L., Chapman, J., Mack, K. A., & Shih, A. S. (2000). Acupressure for nausea: Results of a pilot study. Oncology Nursing Forum, 27, 41–47.
Dibble, S. L., Luce, J., Cooper, B. A., Israel, J., Cohen, M., Nussey, B., et al. (2007) Acupressure for chemotherapy induced nausea and vomiting: A randomized clinical trial. Oncology Nursing Forum, 34, 813–820.
Dundee, J., Ghaly, R. G., Fitzpatrick, K. T., Lynch, G. A., & Abram, W. P. (1987). Acupuncture to prevent cisplatin-associated vomiting. Lancet, 1, 1083.
Dundee, J., Sourial, F. B., Ghaly, R. G., & Bell, P. F. (1988). P6 acupressure reduces morning sickness. Journal of the Royal Society of Medicine, 81, 456–457.
Edwards, C., Carmichael, J., Baylis, P. H., & Harris, A. L. (1989). Arginine vasopressin—a mediator of chemotherapy induced emesis? British Journal of Cancer, 59, 467–470.
Ezzo, J., Richardso, M. A., Vickers, A., Allen, C., Dibble, S. L., Issell, B. F., et al. (2006). Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database of Systematic Reviews (Online), 19, CD002285.
Foss, J., Yuan, C. S., Roizen, M. F., & Goldberg, L. P. (1998). Prevention of apomorphine- or cisplatin-induced emesis in the dog by a combination of methylnaltrexone and morphine. Cancer Chemotherapy and Pharmacology, 42, 287–291.
Gottschling, S., Reindl, T. K., Meyer, S., Berrang, J., Henze, G., Graeber, S., et al. (2008). Acupuncture to alleviate chemotherapy-induced nausea and vomiting in pediatric oncology—a randomized multicenter crossover pilot trial. Klinische Pädiatrie, 220, 365–370.
Gu, S., Yang, J., & Zhang, M. (2007). Contrast study for the effects of different administration route of dexamethasone on gastrointestinal reaction induced by chemotherapy. Advanced Nursing, 22, 399–400.
Ho, Y. F. (2006). Acupressure and psychological intervention for emesis due to chemotherapy on the patients with mammary cancer. Guangxi Medical Journal, 28, 738–739.
Hu, S., Stern, R. M., & Koch, K. L. (1992). Electrical acustimulation relieves vection-induced motion sickness. Gastroenterology, 102, 1854–1858.
Jadad, A., Moore, R. A., Carroll, D., Jenkinson, C., Reynolds, D. J., Gavaghan, D. J., et al. (1996). Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clinical Trials, 17,, 1–12.
Jindal, V., Ge, A., & Mansky, P. J. (2008). Safety and efficacy of acupuncture in children: A review of the evidence. Journal of Pediatric Hematology/Oncology, 30, 431–442.
Kim, M., Chey, W. D., Owyang, C., & Hasler, W. L. (1997). Role of plasma vasopressin as a mediator of nausea and gastric slow wave dysrhythmias in motion sickness. The American Journal of Physiology, 272, G853–G862.
Ladas, E., Rooney, D., Taromina, K., Ndao, D. H., & Kelly, K. M. (2010). The safety of acupuncture in children and adolescents with cancer therapy-related thrombocytopenia. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer, 18, 1487–1490.
Lee, M., Choi, T. Y., Park, J. E., Lee, S. S., & Ernst, E. (2010a) Moxibustion for cancer care: A systematic review and meta-analysis. BMC Cancer, 10, 130.
Lee, M., Kang, J. W., & Ernst, E. (2010b) Does moxibustion work? An overview of systematic reviews. BMC Research Notes, 3, 284.
Lin, J., & Chen, W. (2008). Acupuncture analgesia: A review of its mechanisms of actions. The American Journal of Chinese Medicine, 36, 635–645.
Lin, X., Liang, J., Ren, J., Mu, F., Zhang, M., & Chen, J. (1997). Electrical stimulation of acupuncture points enhances gastric myoelectrical activity in humans. American Journal of Gastroenterology, 92, 1527–1530.
Ma, L. (2009) Acupuncture as a complementary therapy in chemotherapy-induced nausea and vomiting. Proceedings of the Baylor University Medical Center, 22, 138–141.
Manheimer, E., Wieland, S., Kimbrough, E., Cheng, K., & Berman, B. M. (2009). Evidence from the cochrane collaboration for traditional chinese medicine therapies. The Journal of Alternative and Complementary Medicine, 15, 1001–1014.
McMillan, C., Dundee, J. W., & Abram, W. P. (1991). Enhancement of the antiemetic action of ondansetron by transcutaneous electrical stimulation of the P6 antiemetic point, in patients having highly emetic cytotoxic drugs. British Journal of Cancer, 64, 971–972.
Melchart, D., Ihbe-Heffinger, A., Leps, B., von Schilling, C., & Linde, K. (2006). Acupuncture and acupressure for the prevention of chemotherapy-induced nausea-a randomised cross-over pilot study. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer, 14, 878–882.
Molassiotis, A., Helin, A. M., Dabbour, R., & Hummerston, S. (2007). The effects of P6 acupressure in the prophylaxis of chemotherapy-related nausea and vomiting in breast cancer patients. Complementary Therapies in Medicine, 15, 3–12.
Ng, D. K., Chow, P., & Ming, S. (2004). A double-blind, randomized, placebo-controlled trial of acupuncture for the treatment of childhood persistent allergic rhinitis. Pediatrics, 114, 1242–1247.
Ning, C. H. (2004). Contrast observation on injection metoclopramide in different acupuncture point for the treatment of emesis after chemical treatment to mammary cancer. Guiding Journal of Traditional Chinese Medicine and Pharmacology, 10, 39–41.
Noga, S., Tolman, A., & Roman, J. (2002). Acupressure as an adjunct to pharmacologic control of nausea, vomiting and retching (N/V) during blood and marrow transplantation (BMT): A randomized, placebo-controlled, algorithm based study. Proceedings of the American Society of Clinical Oncology, 21, 361a.
Nystrom, E., Ridderstrom, G., & Leffler, A. (2008). Manual acupuncture as an adjunctive treatment of nausea in patients with cancer in palliative care–a prospective, observational pilot study. Acupuncture in Medicine, 26, 27–32.
Pearl, M., Fischer, M., McCauley, D. L., Valea, F. A., & Chalas, E. (1999). Transcutaneous electrical nerve stimulation as an adjunct for controlling chemotherapy-induced nausea and vomiting in gynecologic oncology patients. Cancer Nursing, 22, 307–311.
Radmayr, C., Schlager, A., Studen, M., & Bartsch, G. (2001). Prospective randomized trial using laser acupuncture versus desmopressin in the treatment of nocturnal enuresis. European Urology, 40, 201–205.
Reindl, T., Geilen, W., Hartmann, R., Wiebelitz, K. R., Kan, G., Wilhelm, I., et al. (2006). Acupuncture against chemotherapy-induced nausea and vomiting in pediatric oncology. Interim results of a multicenter crossover study. Support Care Cancer, 14, 172–176.
Roscoe, J., Morrow, G., & Bushunow, P. (2002). Acustimulation wristbands for the relief of chemotherapy-induced nausea. Alternative Therapies in Health and Medicine, 8, 56–63.
Roscoe, J. A., Morrow, G. R., Hickok, J. T., Bushunow, P., Pierce, H. I., Flynn, P. J., et al. (2003). The efficacy of acupressure and acustimulation wrist bands for the relief of chemotherapy-induced nausea and vomiting. Journal of Pain and Symptom Management, 26, 731–742.
Roscoe, J., Matteson, S. E., Morrow, G. R., Hickok, J. T., Bushunow, P., Griggs, J., et al. (2005). Acustimulation wrist bands are not effective for the control of chemotherapy-induced nausea in women with breast cancer. Journal of Pain and Symptom Management, 29, 376–384.
Rusy, L. M., Hoffman, G. M., & Weisman, S. J. (2002). Electroacupuncture prophylaxis of postoperative nausea and vomiting following pediatric tonsillectomy with or without adenoidectomy. Anesthesiology, 96, 300–305.
Schlager, A., Offer, T., & Baldissera, I. (1998). Laser stimulation of acupuncture point P6 reduces postoperative vomiting in children undergoing strabismus surgery. British Journal of Anaesthesia, 81, 529–532.
Shen, J., Wenger, N., Glaspy, J., Hays, R. D., Albert, P. S., Choi, C., et al. (2000). Electroacupuncture for control of myeloablative chemotherapy-induced emesis: A randomized controlled trial. JAMA: The Journal of the American Medical Association, 284, 2755–2761.
Shenkman, Z., Holzman, R. S., Kim, C., Ferrari, L. R., DiCanzio, J., Highfield, E. S., et al. (1999). Acupressure-acupuncture antiemetic prophylaxis in children undergoing tonsillectomy. Anesthesiology, 90, 1311–1316.
Somri, M., Vaida, S. J., Sabo, E., Yassain, G., Gankin, I., & Gaitini, L. A. (2001). Acupuncture versus ondansetron in the prevention of postoperative vomiting. A study of children undergoing dental surgery. Anaesthesia, 56, 972–932.
Streitberger, K., Friedrich-Rust, M., Bardenheuer, H., Unnebrink, K., Windeler, J., Goldschmidt, H., et al. (2003). Effect of acupuncture compared with placebo-acupuncture at P6 as additional antiemetic prophylaxis in high-dose chemotherapy and autologous peripheral blood stem cell transplantation: A randomized controlled single-blind trial. Clinical Cancer Research: An Official Journal of The American Association for Cancer Research, 9, 2538–2544.
Takahashi, T. (2011). Mechanism of acupuncture on neuromodulation in the gut–a review. Neuromodulation, 14, 8–12 (discussion 12).
Tatewaki, M., Strickland, C. & Fukuda, H. (2005). Effects of acupuncture on vasopressin-induced emesis in conscious dogs. American JJournal of Physiology, Regulatory, Integrative and Comparative Physiology, 288, R401–R408.
Treish, I., Shord, S., Valgus, J., Harvey, D., Nagy, J., Stegal, J., et al. (2003). Randomized double-blind study of the Reliefband as an adjunct to standard antiemetics in patients receiving moderately-high to highly emetogenic chemotherapy. Support Care Cancer, 11, 516–521.
Urroz, P., Colagiuri, B., Smith, C.A., & Cheema, B.S. (2012). Effect of acute acupuncture treatment on exercise performance and postexercise recovery: a systematic review. Journal of Alternative and Complementary Medicine, in press.
Wang, S. M., & Kain, Z. N. (2002). P6 acupoint injections are as effective as droperidol in controlling early postoperative nausea and vomiting in children. Anesthesiology, 97, 359–366.
World Health Organization. (2003). Acupuncture: Review and analysis of reports on controlled clinical trials: 87. Geneva: World Health Organization.
Xu, Y., Wang, J. L., – Du, H. Y. (2005). Contrast observation on injection metoclopramide in acupuncture point for the treatment of emesis after chemical treatment to 100 patients with cancer. Central Plains Medical Journal, 32, 58.
Zhang, J., Shang, H., Gao, X., & Ernst, E. (2010). Acupuncture-related adverse events: A systematic review of the Chinese literature. Bull World Health Organ, 88, 915C–921C.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Konno, R., Gyi, A. (2012). Use of Acupuncture and Moxibustion in the Control of Anticancer Therapy-induced Nausea and Vomiting. In: Cho, W. (eds) Acupuncture and Moxibustion as an Evidence-based Therapy for Cancer. Evidence-based Anticancer Complementary and Alternative Medicine, vol 3. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-4833-0_6
Download citation
DOI: https://doi.org/10.1007/978-94-007-4833-0_6
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-4832-3
Online ISBN: 978-94-007-4833-0
eBook Packages: MedicineMedicine (R0)