Abstract
Acupuncture and moxibustion are frequently used in palliative and supportive cancer care. Many clinical trials have been conducted, and their results have been evaluated in numerous systematic reviews (SRs). The objective of this chapter is to provide an overview of these SRs. Fourteen databases were searched from their inception through November 2011. Study selection, data extraction, and validations were performed independently by two reviewers. The quality of SRs was assessed using The Overview Quality Assessment Questionnaire. We identified 14 relevant SRs: 11 SRs relating to acupuncture, 2 SRs relating to acupressure and 1 SR related to moxibustion met our inclusion criteria. The adverse events observed among cancer patients included hot flashes, chemotherapy-induced nausea and vomiting (CINV), leucopenia, xerostomia and pain. The indications supported by reasonably good evidence were CINV and cancer pain. This chapter concluded that CINV and cancer pain are the only indications for acupuncture, acupressure or moxibustion currently supported by concrete evidence. Future studies should be of high quality with a particular emphasis on designing adequate control interventions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1.1 Introduction
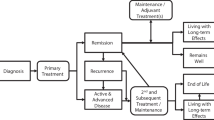
Cancer is a leading cause of death worldwide, accounting for 7.6 million deaths (approximately 13% of all deaths in 2008) (Jemal et al. 2011). The estimated 5-year survival rate for all cancers has risen to approximately 66% (American Cancer Society 2012a,b). Cancer survivors experience a wide range of symptoms during and following the completion of treatment, and some of these symptoms may persist for years or even decades. While pharmacologic treatments relieve many symptoms, they may have negative side effects (Cassileth et al. 2007; Wesa et al. 2008).
During the last two decades, the use of complementary and alternative medicine (CAM), including acupuncture, as an adjunctive therapy for cancer-related symptoms and for improving a patient’s quality of life has increased (Richardson et al. 2000). Several studies have shown rates of CAM use for cancer ranging from 34–91% in the USA (Dean-Clower et al. 2010). The usage of CAM therapies may be higher among those with more advanced cancer or significant cancer therapy-related symptoms (Bardia et al. 2007). The widespread use of CAM by cancer patients is attributed to their hope of improving survival , reducing recurrence, reducing the side effects of surgery and chemotherapy , and also treating physical and psychosocial issues. CAM is often administered to treat nausea and vomiting , fatigue , pain and other symptoms. Most cancer patients employ CAM as an adjunct rather than an alternative to conventional oncological care (Levinson et al. 2000; Beinfield and Korngold 2003).
However, the clinical effectiveness of CAM remains uncertain (Alimi et al. 2003; Vickers et al. 2004; American Society of Clinical Oncology 2006), and many experts doubt its biological plausibility.
Acupuncture and its variants are commonly used to control the symptoms of cancer patients, and some evidence suggests that it can play an important role in the support care for cancer-related conditions (Konkimalla and Efferth 2008).
The National Institutes of Health (NIH) Consensus Development Conference in 1997 stated that acupuncture is an effective treatment modality, particularly for nausea and vomiting induced by chemotherapy and for the relief of pain (NIH Consensus Statement 1998). The American Cancer Society informs patients that, “Acupuncture is simple, and often works. It has few side effects or complications , and the cost is low. For these reasons, “It can be a good choice for some problems” (American Cancer Society). The frequency of acupuncture use among cancer patients ranges between 1.2 and 31% (Filshie and Hester 2006; Gansler et al. 2008).
Numerous clinical trials of acupuncture for cancer care have emerged; however, their results are contradictory. Systematic reviews (SRs) summarizing this evidence may provide clarification. To date, several such articles have been published. Unfortunately, their conclusions are also conflicting.
Thus, this overview is aimed at summarizing and critically evaluating all SRs on acupuncture, acupressure and moxibustion as a symptomatic treatment for cancer patients. Our ultimate goal is to provide clinicians with clearer guidance as to the value of these approaches.
1.2 Methods
1.2.1 Data Sources
The following databases were searched from the date of their inception to November 27, 2011, without language restrictions: Medline, EMBASE, AMED, CINHAL, the Cochrane Library, six Korean Medical Databases (Korean Studies Information, DBPIA, Korea Institute of Science and Technology Information, Korea Education and Research Information Service, KoreaMed and Korean National Assembly Library) and the China National Knowledge Infrastructure (CNKI). In addition, our extensive departmental files were searched by hand. The keywords used in the search were (systematic review OR meta-analysis) AND (acupuncture OR acupressure OR moxa OR moxibustion) AND (cancer OR tumor OR carcinoma). Articles were included if they related to a formal SR or meta-analysis on any type of acupuncture, acupressure or moxibustion as a symptomatic treatment for any type of cancer condition. Reviews, comments and overviews without a systematic methods section were excluded.
1.2.2 Study Selection
All systematic reviews were included if they investigated patients with cancer who received acupuncture, acupressure or moxibustion. Reviews that were not systematic were excluded. There were no language restrictions. Two review authors (TYC and MSL) independently reviewed the articles according to predefined criteria, including conditions, number of primary studies, methodological quality of the primary studies, conclusion of each SR, and data related to the search. Any disagreement between review authors was resolved by discussion, and, if necessary, by the other author.
1.2.3 Data Extraction
All clinical endpoints were considered, but the main outcome measures were the effectiveness of acupuncture, moxibustion or acupressure for the treatment of symptoms in cancer patients and cancer survivors. Two independently trained review authors extracted data for each eligible trial. Disagreements were resolved by a discussion between the authors to reach a consensus. If there was no agreement, a third review author acted as the arbitrator.
1.2.4 Assessment of the Quality of SRs
The Overview Quality Assessment Questionnaire (OQAQ) was used to evaluate the methodological quality of all included SRs (Oxman and Guyatt 1991; Jadad and McQuay 1996). In the OQAQ, the score ranges from 1 to 7. A score of 3 or less was considered as indicative of major flaws, whereas a score of 5 or more suggested only minor flaws. The two authors performed these assessments independently, and discrepancies were settled by discussion.
1.3 Results
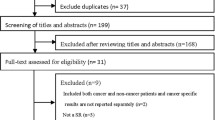
Our searches generated 101 articles, and 14 SRs met our inclusion criteria (Fig. 1.1, Table 1.1 (Klein and Griffiths 2004; Jedel 2005; Lee et al. 2005, 2008, 2009a,b, 2010; Ezzo et al. 2006; Lu et al. 2007; Chao et al. 2009; Hollis 2010; O’Sullivan and Higginson 2010; Peng et al. 2010; Paley et al. 2011). They address a range of different symptoms among cancer patients including chemotherapy-induced nausea and vomiting (CINV) (Klein and Griffiths 2004; Ezzo et al. 2006; Lee et al. 2008, 2010), chemotherapy-induced neutropenia (Lu et al. 2007), cancer pain (Lee et al. 2005; Hollis 2010; Peng et al. 2010; Paley et al. 2011), xerostomia (Jedel 2005; O’Sullivan and Higginson 2010) and hot flashes (Lee et al. 2009a,b). Four studies originated from the UK (Klein and Griffiths 2004; Lee et al. 2005; O’Sullivan and Higginson 2010; Paley et al. 2011), 3 from the US (Ezzo et al. 2006; Lu et al. 2007; Hollis 2010), 4 from Korea (Lee et al. 2008, 2009a,b, 2010), one from Taiwan (Chao et al. 2009), one from China (Peng et al. 2010) and one from Sweden (Jedel 2005). Five SRs arrived at positive conclusions (Klein and Griffiths 2004; Ezzo et al. 2006; Lee et al. 2010; Peng et al. 2010; Paley et al. 2011). Most of the SRs were of good quality, but all were based on primary studies of poor quality (Table 1.1 and 1.2).
1.3.1 Chemotherapy-Induced Nausea and Vomiting
Based on the included reviews, acupuncture (Ezzo et al. 2006), acupressure (Klein and Griffiths 2004; Lee et al. 2008) and moxibustion (Lee et al. 2010) reduce CINV.
Ezzo et al. (2006) evaluated the efficacy of acupuncture-point stimulation on acute and delayed CINV in cancer patients. Eleven studies (n = 1,247) were included in the meta-analysis. Overall, the combined effect of all interventions reduced the incidence of acute vomiting (risk ratio (RR) = 0.82; 95% confidence interval (CI) 0.69 to 0.99; p = 0.84), but not of severe acute or delayed nausea compared to controls. Needle acupuncture reduced acute vomiting (RR = 0.74; 95% CI 0.58 to 0.94; p = 0.014) but not the severity of acute nausea. Electroacupuncture reduced acute vomiting (RR = 0.77; 95% CI 0.61 to 0.97; p = 0.026), but manual acupuncture did not (delayed symptoms were not reported). Acupressure reduced the mean acute nausea-severity (standard mean difference = 0.02; 95% CI -0.42 to 0.46; p = 0.92) but not acute vomiting or delayed symptoms. Non-invasive electrostimulation generated no benefits for any outcome measure. All trials used concomitant pharmacologic anti-emetics, and all, except the electroacupuncture trials, used state-of-the-art anti-emetics. However, this review complements data on post-operative nausea and vomiting suggesting a biological effect of acupuncture-point stimulation.
Klein and Griffiths (2004) assessed the effectiveness of acupressure in the form of SeaBand for the relief of treatment-related nausea and vomiting. The use of acupressure plus standard care was compared with standard care alone. Adult patients receiving cancer chemotherapy were monitored for the frequency and severity of nausea or vomiting. This SR identified two RCTs (n = 482) that compared acupressure to no such intervention. One RCT reported significant differences over the 10-day follow-up period in favor of acupressure in terms of both the experience (p < 0.01) and the intensity of nausea (p < 0.04) but not regarding the Chemotherapy Problem Checklist related to nausea (p = 0.845). The other RCT reported no significant effects (p > 0.05) on vomiting, delayed nausea or anti-emetic use, but there was a significant (p < 0.05) benefit in the acupressure group with regard to early nausea (0.4 points on a 7-point scale). These results therefore suggest that acupressure may decrease nausea among patients undergoing chemotherapy.
Lee et al. (2008) conducted an SR evaluating the effects of acupressure combined with anti-emetics for CINV. Ten RCTs were included (n = 1,464). Four of seven acupressure band RCTs demonstrated the positive effects of acupressure, whereas three acupressure band trials yielded negative results. All studies with negative results had methodological weaknesses. One quasi-experimental and two randomized finger acupressure trials demonstrated positive effects of acupressure. The overall effect of acupressure was suggestive but not conclusive.
Lee et al. (2010) published an SR investigating the effects of moxibustion for supportive cancer care. Five RCTs (n = 301) compared the effects of moxibustion with conventional therapy. Four RCTs failed to show favorable effects on the response rate compared with chemotherapy (n = 229, RR 1.04, 95% CI 0.94 to 1.15, p = 0.43). Two RCTs assessing the occurrence of adverse effects of chemotherapy demonstrated the positive effects of moxibustion. A meta-analysis generated a favorable effect on the frequency of CINV (n = 80, RR 0.38, 95% CI 0.22 to 0.65, p = 0.0005, heterogeneity: c2 = 0.18, p = 0.67, I2 = 0%). All studies had a high risk of bias, and thus the overall result was inconclusive.
In summary, the evidence is positive for acupuncture as a treatment for CINV. For other acupuncture-related interventions, the evidence is less certain.
1.3.2 Chemotherapy-induced Neutropenia
Lu et al. (2007) conducted an SR assessing the effectiveness of acupuncture for chemotherapy-induced leukopenia. Eleven RCTs with cancer patients (n = 682) who were undergoing or had just completed chemotherapy or chemoradiotherapy were included. They were randomized to either acupuncture therapy or standard care . The median sample size of each comparison group was 45, and the median trial duration was 21 days. The frequency of the acupuncture treatment was once a day, with a median of 16 sessions in each trial. In the seven trials in which white blood cell (WBC) counts were available, acupuncture use was associated with an increase in leukocyte counts in patients during chemotherapy or chemoradiotherapy, with a weighted mean difference of 1,221 WBC/mL (95% CI 636 to 1,807; p < 0.0001). The poor quality of the primary data prevented firm conclusions about the value of acupuncture for this indication.
In summary, the evidence fails to show definitively that acupuncture is effective for this indication.
1.3.3 Cancer Pain
Lee et al. (2005) conducted an SR summarizing the evidence for acupuncture for cancer-related pain. Of the seven studies included (n = 368), one high-quality RCT of ear acupuncture reported statistically significant pain relief in comparison with placebo ear acupuncture. All the other studies were either not blinded (n = 2) or uncontrolled (n = 4). A visual analog scale (VAS) and the patient’s verbal assessment were used as primary pain-related outcome measures. The authors concluded that the notion of acupuncture as an effective analgesic adjunctive method for cancer patients is not supported by sound evidence.
Peng et al. (2010) published an SR of seven RCTs testing the effects of acupuncture on cancer pain. They compared acupuncture with placebo, Western drugs, Chinese herbal medicines, or acupuncture therapy plus drug treatments. The high-quality trial showed that auricular acupuncture therapy was significantly superior to placebo in alleviating pain. This SR therefore arrived at positive conclusions.
Hollis (2010) conducted an SR and meta-analysis of three studies investigating the effect of acupuncture treatment as a treatment modality for cancer pain. A synthesis of the current evidence revealed a lack of level I and II evidence. The majority of the evidence is level III or lower; therefore, the conclusions of this SR are not positive.
Paley et al. (2011) conducted an SR evaluating the efficacy of acupuncture for the relief of cancer-related pain in adults. Three RCTs (n = 204) were included. One high-quality study investigated the effect of auricular acupuncture compared with auricular acupuncture at placebo points with non-invasive vaccaria ear seeds attached at placebo points. There was a high risk of bias in both studies because of the low methodological quality. One study comparing acupuncture with medication concluded that both methods were effective in controlling pain, although acupuncture was the most effective. The second study compared acupuncture, point-injection and medications in participants with stomach cancer. Long-term pain relief was reported for both acupuncture and point-injection compared with medications administered during the last 10 days of treatment. Although both studies support the use of acupuncture, they should be interpreted with caution due to their methodological limitations, small sample size, poor reporting and inadequate analyses. Therefore, there is insufficient evidence to determine whether acupuncture is effective in treating cancer pain in adults.
In summary, these SRs do not arrive at uniform conclusions. The studies of better quality tend to be negative or cautious about the value of acupuncture or related interventions for reducing cancer pain. It therefore follows that the best current evidence fails to convincingly demonstrate the effectiveness of acupuncture for this indication.
1.3.4 Xerostomia
Jedel (2005) conducted an SR to assess the efficacy of acupuncture in the management of xerostomia . Three RCTs (n = 79) met the criteria for inclusion, and a criteria list was used to assess the quality of these studies, which turned out to be variable. The results of the trials were equally variable ranging from positive to negative. This SR therefore produced little evidence for the effectiveness of acupuncture in the management of xerostomia.
O’Sullivan and Higginson (2010) published an SR of three RCTs (n = 108) investigating the effectiveness and safety of acupuncture in radiation-induced xerostomia (RIX) in patients with head and neck cancer (HNC) . Two trials compared acupuncture with sham acupuncture , and one compared acupuncture with standard care . The outcome measurements included salivary flow rates (SFRs) in two trials and subjective questionnaires in three. All three trials reported significant reductions in xerostomia vs the baseline SFR (p < 0.05); one reported greater effects for stimulated SFR in the intervention group (p < 0.01). A subjective assessment reported significant differences between true acupuncture and control treatment in two trials (p < 0.02–0.05). This limited evidence therefore suggests that acupuncture might be beneficial for RIX.
In summary, these SRs generated somewhat contradictory findings. The value of acupuncture as a treatment for xerostomia is therefore not firmly established.
1.3.5 Hot Flashes
Lee et al. (2009a) conducted an SR evaluating the effectiveness of acupuncture for hot flashes in patients with breast cancer . Six studies (n = 281) were included in the meta-analysis . The RCTs compared true acupuncture with sham acupuncture , another active treatment or no treatment. Three RCTs compared the effects of manual acupuncture with those of sham acupuncture . One RCT demonstrated favorable effects of acupuncture in reducing the frequency of hot flashes, while two RCTs failed to do so. The meta-analysis showed significant effects of acupuncture compared with sham acupuncture (n = 189, weighted mean difference 3.09, 95% CI -0.04 to 6.23, p = 0.05), but marked heterogeneity was observed in this model (c2 = 8.32, p = 0.02, I2 = 76%). One RCT compared the effects of electroacupuncture with hormone replacement therapy . Hormone therapy was more effective than electroacupuncture. Another RCT compared acupuncture with venlafaxine and reported no significant differences between the groups. The authors concluded that there is inadequate evidence to suggest that acupuncture is an effective treatment for hot flashes in patients with breast cancer.
Lee et al. (2009b) tested the effects of acupuncture as a treatment for hot flashes in prostate cancer (PC) patients. Six studies (n = 132) met the inclusion criteria. One RCT compared the effects of manual acupuncture with acupuncture plus electroacupuncture. The other five studies were uncontrolled observational studies that were open to a range of biases. The authors concluded that there is no strong evidence to suggest acupuncture is an effective treatment for hot flashes in patients with PC.
In summary, these SRs fail to generate good evidence for acupuncture as treatment for cancer-related hot flashes .
1.3.6 Treating the Adverse Effects of Conventional Cancer Therapies
Chao et al. (2009) conducted an SR evaluating the evidence for acupoint stimulation in the management of therapy-related adverse events in breast cancer. This SR identified clinical trials that were designed to examine the efficacy of acupressure , acupuncture, or acupoint stimulation for the management of adverse events associated with breast cancer treatment. Twenty-six trials (18 RCTs and eight CCTs) satisfied the inclusion criteria. They assessed the application of acupoint stimulation on six disparate conditions related to anticancer therapies, including vasomotor syndrome, CINV, lymphedema, post-operation pain, aromatase inhibitor-related joint pain and leukopenia. The modalities of acupoint stimulation used included traditional acupuncture, acupressure, electroacupuncture, and the use of magnetic devices on acupuncture points. The methodological quality of the trials was assessed using a modified Jadad scale. Overall, 23 trials (88%) reported positive outcomes for at least one of the conditions examined. Three high-quality trials suggested that acupoint stimulation on Neiguan (PC6) was beneficial to CINV. In summary, apart from the evidence relating to CINV, there is little evidence to suggest that acupuncture is effective in reducing the adverse effects of oncological treatments.
In conclusion, numerous systematic reviews have recently become available, but evidence of the effectiveness of acupuncture or moxibustion for the symptomatic treatment or prevention of cancer symptoms is mixed, e.g. CINV is sometimes positively judged and sometimes not. Further limitations of our overview are the potentially poor quality of the primary data and the poor reporting of results, which were highly heterogeneous in virtually every respect. In the future, the areas that warrant further investigation include the efficacy of acupuncture or moxibustion interventions utilizing rigorous RCT designs.
1.4 Discussion
Our overview shows that several SRs on acupuncture, moxibustion or acupressure therapies have been published. Given that most of them were published recently, the scientific interest in CAM therapies seems to be growing. Many of the reviews were of poor quality, based on few and often less than rigorous clinical trials, and arrived at overall positive conclusions.
There were four reviews that focused on the treatment of CINV (Jedel 2005; Ezzo et al. 2006; Lee et al. 2008, 2010) (Table 1.3). They are all positive, but unfortunately they were based on primary studies that were mostly of poor quality.
Four systematic reviews on the treatment of cancer pain have been published (Lee et al. 2005; Hollis 2010; Peng et al. 2010; Paley et al. 2011) (Table 1.3). They were of relatively high quality and included seven mostly rigorous trials (Paley et al. 2011). Lee et al. (2005) concluded that “the evidence is negative”, while Peng et al. (2010) and Paley et al. (2011) reported that “the evidence is positive”. Hollis (2010) concluded that “the evidence is not consistent”. The evidence is thus not conclusive. More well-designed trials using rigorous methodology are required to determine the effectiveness of acupuncture interventions for managing cancer pain.
For the treatment of hot flashes, there were two published SRs (Lee et al. 2009a,b): one on breast cancer in women and one on prostate cancer in men. Both were low-quality studies that reported negative results and were mostly based on poor-quality primary studies. The evidence is thus inadequate to recommend acupuncture as an effective treatment for hot flashes in breast cancer and prostate cancer patients.
The other two SRs investigated chemotherapy-induced leucopenia (Lu et al. 2007) and xerostomia (Jedel 2005; O’Sullivan and Higginson 2010) (Table 1.3). Both were of poor quality and relied on a small number of flawed studies. Thus, the value of acupuncture is not well documented for either of these conditions.
Overall, the effectiveness of acupuncture, moxibustion and acupressure for the symptomatic treatment of cancer is currently not well documented. This is in sharp contrast to the many claims made by the proponents of these modalities.
Relatively encouraging evidence was found for the use of these tools in treating nausea and vomiting in cancer patients (Klein and Griffiths 2004; Ezzo et al. 2006; Lee et al. 2008, 2010). Unfortunately, these SRs were mostly based on poor quality primary studies . Thus, there is considerable uncertainty about the value of acupuncture, moxibustion and acupressure therapies for these indications.
Adverse events were reported in two SRs (Chao et al. 2009; Lee et al. 2009a). Chao et al. (2009) reported that the adhesive for the acu-magnet device and the electrocurrent stimulation generated a few side effects , including skin irritation and a shock sensation. Lee et al. (2009a) reported mild adverse events for acupuncture, such as distress, fatigue , a hematoma at the insertion site and a few second transient increase in vasomotor symptoms . However, there were no serious adverse events that required medical management.
Most SRs of acupuncture, moxibustion or acupressure therapies have stressed that their conclusiveness was limited by the often poor quality of the primary data. Our analysis confirms this impression. Many of the primary acupuncture, moxibustion or acupressure therapy trials originate in China (data not shown). Vickers et al. (1998) demonstrated that virtually 100% of Chinese acupuncture trials are positive. This disturbing finding casts considerable doubt on the reliability of these studies and limits the conclusions that can be drawn from many of the SRs included in this overview. Systematic reviews have been criticized for being unable to provide specific guidance. However, even if uncertainty persists, SRs have the important function of highlighting these concerns. Thus, as mentioned above, our overview highlights areas of research that require further clinical trials.
Our overview has several important limitations. Although our search strategy was thorough, it is possible that some relevant articles were missed. By evaluating systematic reviews rather than clinical trials, important details of the primary studies may have been lost. Most importantly, the poor quality of the primary data and the systematic reviews was a major weakness. Collectively, these limitations limit the conclusions that can be drawn.
Future RCTs of acupuncture-type therapies for supportive cancer care should adhere to the accepted standards of clinical trial methodology. The studies included in this review demonstrate a number of problems that have been previously noted by other reviews that examined the efficacy of acupuncture-type therapies. Furthermore, even though it is difficult to blind subjects to treatment, the use of examiner blinding and allocation concealment are important for reducing bias.
1.5 Conclusion
CINV and cancer pain are the only indications for acupuncture, acupressure or moxibustion currently supported by sound evidence. Future studies should be of high quality with a particular emphasis on designing adequate control interventions. In conclusion, numerous systematic reviews have recently become available, but evidence of the effectiveness of acupuncture or moxibustion for symptomatic treatment or for the prevention of cancer symptoms is mixed, e.g. CINV is sometimes positively judged and sometimes not. Further limitations of our overview are the potential poor quality of the primary data and the poor reporting of results, which were highly heterogeneous in virtually every respect. The areas that warrant further investigations include the efficacy of acupuncture or moxibustion interventions using a rigorous RCT design.
References
Alimi, D., Rubino, C., Pichard-Léandri, E., Fermand-Brulé, S., Dubreuil-Lemaire, M.L., Hill, C. (2003) Analgesic effect of auricular acupuncture for cancer pain: a randomized, blinded, controlled trial. Journal of Clinical Oncology, 15, 4120–4126.
American Cancer Society (2012a). Acupuncture. http://www.cancer.org/Treatment/TreatmentsandSideEffects/ComplementaryandAlternativeMedicine/ManualHealingandPhysicalTouch/acupuncture. Accessed 12 Sep 2012.
American Cancer Society (2012b). Cancer facts & fig. 2012. http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-031941.pdf. Accessed 12 Sep 2012.
American Society of Clinical Oncology, Kris, M.G., Hesketh, P.J., Somerfield, M.R., Feyer, P., Clark-Snow, R., et al (2006) American Society of Clinical Oncology guideline for antiemetics in oncology: update 2006. Journal of Clinical Oncology, 24, 2932–2947.
Bardia, A., Greeno, E., Bauer, B.A. (2007) Dietary supplement usage by patients with cancer undergoing chemotherapy: does prognosis or cancer symptoms predict usage? The Journal of Supportive Oncology, 5, 195–198.
Beinfield, H., Korngold, E. (2003) Chinese medicine and cancer care. Alternative Therapies in Health and Medicine, 9, 38–52.
Cassileth, B.R., Deng, G.E., Gomez, J.E., Johnstone, P.A., Kumar, N., Vickers, A.J. (2007) Complementary therapies and integrative oncology in lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest, 132, 340–354.
Chao, L.F., Zhang, A.L., Liu, H.E., Cheng, M.H., Lam, H.B., Lo, S.K. (2009) The efficacy of acupoint stimulation for the management of therapy-related adverse events in patients with breast cancer: a systematic review. Breast Cancer Research and Treatment, 118, 255–267.
Dean-Clower, E., Doherty-Gilman, A.M., Keshaviah, A., Baker, F., Kaw, C., Lu, W., et al (2010) Acupuncture as a palliative therapy for physical symptoms and quality of life for advanced cancer patients. Integrated Cancer Therapies, 9, 158–167.
Ezzo, J.M., Richardson, M.A., Vickers, A., Allen, C., Dibble, S.L., Issell, B.F., et al (2006) Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database of Systematic Reviews (Online), 19, CD002285.
Filshie, J., Hester, J. (2006) Guidelines for providing acupuncture treatment for cancer patients--a peer-reviewed sample policy document. Acupuncture in Medicine, 24, 172–182.
Gansler, T., Kaw, C., Crammer, C., Smith, T. (2008) A population-based study of prevalence of complementary methods use by cancer survivors: a report from the American Cancer Society’s studies of cancer survivors. Cancer, 113, 1048–1057.
Hollis, A.S. (2010) Acupuncture as a treatment modality for the management of cancer pain: the state of the science. Oncology Nursing Forum, 37, E344–348.
Jadad, A.R., McQuay, H.J. (1996) Meta-analyses to evaluate analgesic interventions: a systematic review of their methodology. Journal of Clinical Epidemiology, 49, 235–243.
Jedel, E. (2005) Acupuncture in xerostomia: a systematic review. Journal of Oral Rehabilitation, 32, 392–396.
Jemal, A., Bray, F., Center, M.M., Ferlay, J., Ward, E., Forman, D. (2011) Global Cancer Statistics. CA: A Cancer Journal for Clinicians, 61, 69–90.
Klein, J., Griffiths, P. (2004) Acupressure for nausea and vomiting in cancer patients receiving chemotherapy. British Journal of Community Nursing, 9, 383–388.
Konkimalla, V.B., Efferth, T. (2008) Evidence-based Chinese medicine for cancer therapy. Journal of Ethnopharmacology, 116, 207–210.
Lee, H., Schmidt, K., Ernst, E. (2005) Acupuncture for the relief of cancer-related pain-a systematic review. European Journal of Pain, 9, 437–444.
Lee, J., Dodd, M., Dibble, S., Abrams, D. (2008) Review of acupressure studies for chemotherapy-induced nausea and vomiting control. Journal of Pain and Symptom Management, 36, 529–544.
Lee, M.S., Choi, T.Y., Park, J.E., Lee, S.S., Ernst, E. (2010) Moxibustion for cancer care: a systematic review and meta-analysis. BMC Cancer, 10, 130–138.
Lee, M.S., Kim, K.H., Choi, S.M., Ernst, E. (2009a) Acupuncture for treating hot flashes in breast cancer patients: a systematic review. Breast Cancer Research and Treatment, 115, 497–503.
Lee, M.S., Kim, K.H., Shin, B.C., Choi, S.M., Ernst, E. (2009b) Acupuncture for treating hot flushes in men with prostate cancer: a systematic review. Supportive Care in Cancer, 17, 763–770.
Levinson, W., Gorawara-Bhat, R., Lamb, J. (2000) A study of patient clues and physician responses in primary care and surgical settings. JAMA, 284, 1021–1027.
Lu, W., Hu, D., Dean-Clower, E., Doherty-Gilman, A., Legedza, A.T., Lee, H.,et al (2007) Acupuncture for chemotherapy-induced leukopenia: exploratory meta-analysis of randomized controlled trials. Journal of the Society for Integrative Oncology, 5, 1–10.
NIH Consensus Statement. (1998) Acupuncture. JAMA, 280, 1518–1524.
O’Sullivan, E.M., Higginson, I.J. (2010) Clinical effectiveness and safety of acupuncture in the treatment of irradiation-induced xerostomia in patients with head and neck cancer: a systematic review. Acupuncture in Medicine Society, 28, 191–199.
Oxman, A.D., Guyatt, G.H. (1991) Validation of an index of the quality of review articles. Journal of Clinical Epidemiology, 44, 1271–1278.
Paley, C.A., Johnson, M.I., Tashani, O.A., Bagnall, A.M. (2011) Acupuncture for cancer pain in adults. Cochrane Database of Systematic Reviews, 19, CD007753.
Peng, H., Peng, H.D., Xu, L., Lao, L.X. (2010) Efficacy of acupuncture in treatment of cancer pain: a systematic review. Journal of Chinese Integrative Medicine, 8, 501–509.
Richardson, M.A., Sanders, T., Palmer, J.L., Greisinger, A., Singletary, S.E. (2000) Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. Journal of Clinical Oncology, 18, 2505–2514.
Vickers, A., Goyal, N., Harland, R., Rees, R. (1998) Do certain countries produce only positive results? A systematic review of controlled trials. Controlled Clinical Trials, 19, 159–166.
Vickers, A.J., Straus, D.J., Fearon, B., Cassileth, B.R. (2004) Acupuncture for postchemotherapy fatigue: a Phase II study. Journal of Clinical Oncology, 22, 1731–1735.
Wesa, K., Gubili, J., Cassileth, B. (2008) Integrative oncology: complementary therapies for cancer survivors. Hematology/Oncology Clinics of North America, 22, 343–353.
Acknowledgment
MSL and TYC were supported by the KIOM (K11111 and C12080).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Choi, TY., Lee, M.S., Ernst, E. (2012). An Overview of Acupuncture and Moxibustion for Cancer Care. In: Cho, W. (eds) Acupuncture and Moxibustion as an Evidence-based Therapy for Cancer. Evidence-based Anticancer Complementary and Alternative Medicine, vol 3. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-4833-0_1
Download citation
DOI: https://doi.org/10.1007/978-94-007-4833-0_1
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-4832-3
Online ISBN: 978-94-007-4833-0
eBook Packages: MedicineMedicine (R0)