Abstract
An intestinal transplant for vaginoplasty in a nontranssexual patient was reported for the first time in 1892. The first application of the technique in a transsexual patient was described only in 1974 that performed a one-stage vaginoplasty with the use of both cecum and sigmoid transplants. Development of this technique was possible as the sigmoid mesocolon has a long and easily mobilized mesentery that allows the selected tract to reach the perineum in a satisfactory way. The surgical procedure should be preferably performed under both general anesthesia and epidural analgesia. The epidural catheter is left in place for a better postoperative analgesia. Some authors present the possibility of a combined laparoscopic and perineal approach for rectosigmoidal vaginoplasty. A case of a robot-assisted sigmoid vaginoplasty in a woman with vaginal agenesia was also presented in the literature. Peri- and postoperative complications usually occur only in a small proportion of patients (incidence lower than 10 %). The most frequent complications are excessive mucosal discharge and malodor.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
An intestinal transplant for vaginoplasty in a nontranssexual patient was reported for the first time in 1892 by Sneguireff using the rectum 40 and in 1904 by Baldwin using the ileum 41. The first application of the technique in a transsexual patient was described only in 1974 by Markland and Hastings that performed a one-stage vaginoplasty with the use of both cecum and sigmoid transplants 42. The advantages of using a rectosigmoid transplant are its length and texture and appearance similar to a natural vagina 48, 49. In addition, it is the only method that provides a vaginal lining with natural lubrication 43, 48.
Although this technique could be used to create a neovagina in naïve transsexual patients, many authors agree that it is the best choice for transsexual patients who have previously undergone penectomy and orchidectomy and that it is also the best technique for patients with an unfavorable previous vaginoplasty.
In fact, in about 10–20% of patients who underwent sex reassignment surgery with penoscrotal flap or penile skin inversion, the one-stage operation fails, usually because of inadequate perineal dissection or flap necrosis or infection, leading to loss of vaginal depth and introital stenosis. In these cases, a corrective operation is then indicated. Although further skin grafting procedures may be considered, they are often subject to the same factors as the initial procedure. To remedy such complications, the technique of vaginal bowel reconstruction evolved [1–4].
1 Surgical Technique
The development of this technique was possible as the sigmoid mesocolon has a long and easily mobilized mesentery that allows the selected tract to reach the perineum in a satisfactory way. The sigmoid segment is isolated by division of the sigmoid mesocolon so that the most distal long sigmoid branch of the inferior mesenteric artery is preserved to function as the main segmental blood supplier. The more proximal branches are divided. The blood supply then, depending on the primary arterial arcade, runs on the mesenteric side of the bowel. The sigmoid is reverted so the previous proximal end can be brought down for the perineal-cutaneous anastomosis. In this way, considerable length can be achieved without generating unnecessary tension in the mesenteric blood supply, thus reducing chances of ischemic necrosis.
The surgical procedure should be preferably performed under both general anesthesia and epidural analgesia. The epidural catheter is left in place for a better postoperative analgesia. The preoperative preparation included full mechanical preparation of the colon and prophylactic administration of heparin. The patient is placed in an extended lithotomy position with the buttocks slightly elevated. The lithotomy position guarantees a wide access to the perineum, with excellent intra-abdominal exposure.
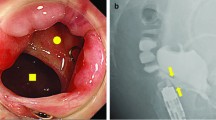
Through a Pfannenstiel incision (semicircular, slightly above the mons pubis – Fig. 18.1), the descending colon is mobilized down to, and including, the sigmoid colon. Then, a sigmoid segment was isolated with its vascular pedicle (Figs. 18.2 and 18.3). It is of paramount importance that before choosing the definitive sigmoid colon segment, surgeons should assess the length of the sigmoid and its mesentery in order to determine whether it can reach the perineum. Usually, a tension-free rectosigmoid vagina can be made up if the lowest point of the sigmoid can be pulled down to reach easily the pubic symphysis. The length of the isolated rectosigmoid segment should range from 8 to 12 cm, to avoid excessive postoperative mucus production. Rectosigmoid is harvested with its blood supply originating from sigmoidal arteries and/or superior hemorrhoidal vessels. Preferably, it should be divided distally first in order to check its mobility and determine the correct site for its proximal division. The proximal end of the isolated segment was closed in two layers using absorbable sutures. Bowel continuity was restored with a hand-sewn single-layer anastomosis with 3-0 silk sutures. The mesenteric defect is closed with the neovagina and its mesentery at the left side of the field (Figs. 18.4 and 18.5). Afterwards, an H-shaped incision is performed in the perineum, and a blunt dissection is performed between the urethra and rectum to create a space for the allocation of the neovaginal colon conduit. In salvage intervention for female transsexuals, scarred and nonfunctional vagina is completely excised to provide adequate space to position the sigmoid loop.
Then isolated sigmoid is brought down to the perineal canal without tension to create a tension-free coloperineal anastomosis. In order to prevent purse-string scarring, introital or perineal skin flaps are formed and approximated to the sigmoid vagina. In order to avoid prolapse, some authors perform a “U”-shaped incision posterior to the urethra and complete it with two lateral vascularized introital flaps. Vascularized flaps are completely mobilized to push the neo-introital opening as high as possible to prevent mucosal prolapse and to yield better aesthetic results with the anastomosis deeply hidden. Some other surgeons prefer to fix the proximal end of the neovagina to the sacral promontory.
Then the neovagina was packed with a compressive dressing for about 7 days, and a Foley catheter is placed and removed 4–5 days after surgery, in order to facilitate the fixation of the rectosigmoid graft to the surrounding tissues. Patients are instructed on how to perform self-dilation of the neovaginal introitus and irrigation of the neovagina for mucus removal, daily for 8 weeks and weekly thereafter.
The final result is showed in Figs. 18.6 and 18.7
The maintenance of hormonal therapy after surgery allows to aid the feminine aspect of external genitalia (hair and fat distribution) rectosigmoidal vaginoplasty.
As described more successfully for ileal vaginoplasty, some authors present the possibility of a combined laparoscopic and perineal approach for rectosigmoidal vaginoplasty. A three-port transperitoneal approach is used for the complete vaginal isolation and mobilization, for rectosigmoid segment isolation, and for vaginal anastomosis [10–11].
Furthermore, Kim et al. presented a case of a robot-assisted sigmoid vaginoplasty in a woman with vaginal agenesia. To date, this operation has never been performed for transsexual surgery [12].
2 Complications
The advantages of rectosigmoid vaginoplasty are summarized in Table 18.1. Although the neovaginal length is usually regarded as an advantage, it can also lead to stasis and dehydration of mucus in the deepest portion of the vagina. Further disadvantages of this technique are the need for additional abdominal surgery and occasional disappointing long-term results. Furthermore, the colonic mucosa is more vulnerable and thus more accessible to sexually transmitted diseases including human immunodeficiency virus infection.
Peri- and postoperative complications usually occur only in a small proportion of patients (incidence lower than 10 %). The most frequent complications are excessive mucosal discharge and malodor. Diversion colitis (inflammation that occurs in the bypassed colonic tissue related to diversion of the fecal stream), ulcerative colitis, peritonitis, intestinal obstruction, junctional neuroma, adenocarcinoma, introital stenosis, mucocele, and constipation have been reported to occur more rarely but are deserving of more attention by the clinicians.
Usually, patients who had partners are able to have sexual intercourse starting 6 months after surgery, and only a small percentage of patients (<5 %) used lubricants or dilators before intercourse for more than a year postoperatively. During intercourse, a high amount of M-to-F transsexual patients experienced orgasm [13–14].
References
Sneguireff WF (1904) Zwei Falle von Restitutio Vaginiae per Transplantationen. Ani Recti Zentralbl Gynakol 28:772
Baldwin JF (1904) The formation of an artificial vagina by intestinal transplantation. Ann Surg 40:398–403
Markland C, Hastings D (1974) Vaginal reconstruction using cecal and sigmoid bowel segments in transsexual patients. J Urol 111:217
Vecchietti G (1965) Neovagina nella syndrome di Rokitansky-Kuster-Hauser. Annu Ostet Gunecol 11:131–147
Creatsas G, Deligeoroglou E, Makrakis E, Kontoravdis A, Papadimitriou L (2001) Creation of a neovagina following Williams vaginoplasty and the Creatsas modification in 111 patients with Mayer-Rokitansky-Kuster-Hauser syndrome. Fertil Steril 76:1036–1040
Davies MC, Creighton SM, Woodhouse CR (2005) The pitfalls of vaginal reconstruction. BJU Int 95:1293–1298
Jarolím L, Sedý J, Schmidt M, Nanka O, Foltán R, Kawaciuk I (2009) Gender reassignment surgery in male-to-female transsexualism: a retrospective 3-month follow-up study with anatomical remarks. J Sex Med 6:1635–1644
Hensle TW, Reiley EA (1998) Vaginal replacement in children and young adults. J Urol 159:1035–1038
Djordjevic ML, Stanojevic DS, Bizic MR (2011) Rectosigmoid vaginoplasty: clinical experience and outcomes in 86 cases. J Sex Med 8(12):3487–3494
Liguori G, Trombetta C, Bucci S, Salamè L, Bortul M, Siracusano S, Belgrano E (2005) Laparoscopic mobilization of neovagina to assist secondary ileal vaginoplasty in male-to-female transsexuals. Urology 66(2):293–298
Wedler V, Meuli-Simmen C, Guggenheim M, Schneller-Gustafsson M, Künzi W (2004) Laparoscopic technique for secondary vaginoplasty in male to female transsexuals using a modified vascularized pedicled sigmoid. Gynecol Obstet Invest 57(4):181–185
Kim C, Campbell B, Ferrer F (2008) Robotic sigmoid vaginoplasty: a novel technique. Urology 72(4):847–849
Kapoor R, Sharma DK, Singh KJ, Suri A, Singh P, Chaudhary H, Dubey D, Mandhani A (2006) Sigmoid vaginoplasty: long-term results. Urology 67(6):1212–1215
Kwun Kim S, Hoon Park J, Cheol Lee K, Min Park J, Tae Kim J, Chan Kim M (2003) Long-term results in patients after rectosigmoid vaginoplasty. Plast Reconstr Surg 112(1):143–151
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Italia
About this chapter
Cite this chapter
Verze, P., Arcaniolo, D., Franco, M., La Rocca, R., Mirone, V. (2015). Surgery in Complications: Colon Vaginoplasty. In: Trombetta, C., Liguori, G., Bertolotto, M. (eds) Management of Gender Dysphoria. Springer, Milano. https://doi.org/10.1007/978-88-470-5696-1_18
Download citation
DOI: https://doi.org/10.1007/978-88-470-5696-1_18
Published:
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-5695-4
Online ISBN: 978-88-470-5696-1
eBook Packages: MedicineMedicine (R0)