Abstract
The acute and long-term consequences of alcohol use disorders are very well known. Multiple treatments for these disorders have been investigated, and some of them have received approval by regulatory agencies. Disulfiram blocks the natural degradation of alcohol. It inhibits the acetaldehyde dehydrogenase, and the accumulation of acetaldehyde in the body results in unpleasant symptoms such as rush, nausea, headache, diarrhea, vomiting, and a drop in blood pressure. Disulfiram should only be prescribed once the patient has been detoxified and is free of alcohol and without withdrawal symptoms. Naltrexone is a competitive opiate antagonist with high affinity to the μ-receptor and lower affinity to the δ- and κ-receptors and is approved to treat alcohol dependence in individuals who are not opioid dependent. Acamprosate binds to NMDA receptors and thus dampens the glutamate-mediated excitability and is approved for the treatment of alcohol dependence in people who already established a state of alcohol abstinence. Nalmefene is the most recent medication approved for use in alcohol dependence. It was approved by the European Medicines Agency in 2012 for a reduction of heavy drinking days and/or total alcohol consumption. Nalmefene is a selective opioid ligand with an equally high affinity to the μ- and κ-receptors and medium affinity to the δ-receptor. It acts as an antagonist at the μ- and δ-receptor, but different from naltrexone, it is a co-agonist at the κ-receptor. The official indication for nalmefene is to reduce alcohol consumption. The chapter will discuss these and other medications that are being investigated for the treatment of alcohol use disorders.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Ever since mankind realized that alcohol consumption can be accompanied by serious consequences and by what later was called impaired control, ways out of this dilemma were searched. Myths and magic around the world deal with remedies to solve or at least reduce this problem. Greek mythology has it that an amethyst helps to cope with alcohol intoxication. In the Middle Ages in France, draconian measures were taken to deal with public drunkenness. King Francois I ordered that “anyone who appeared in public in a state of intoxication should on the first occasion be imprisoned on bread and water, on the second chastised with birch and whip, and on the third publicly flogged. Should further relapses occur the delinquent was to have an ear cut off and suffer banishment” (Lewin 1931). Obviously this approach failed as so many following later. During the nineteenth and much of the twentieth century, alcoholism was considered a moral weakness. Cure was awaited from secluding individuals into asylums with strong elements of education and strengthening religious beliefs. First pharmacological attempts such as Dr. Shilo’s “lemon cure” seem peculiar in retrospect. He recommended the use of 231 lemons over a period of precisely 29 days. “All five subjects developed a complete indifference to alcohol, with the craving stamped out” (Edwards 2000, 2005). Obviously this attempt did not make it into widespread use either.
In the last century, the development and testing of psychotherapies was put on the agenda. Likewise, more sophisticated pharmacological ways of securing abstinence or of reducing alcohol consumption to less harmful levels began to be considered. Some advances were based on serendipity and good clinical observation and judgment. The best-known example is the observation that workers in the rubber industry reported to feel sick when they drank alcohol. It was found that disulfiram as a by-product of rubber fabrication was released into the air and that this explained the reduction in alcohol consumption in those workers who were exposed.
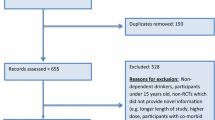
As first claims for successful treatments were made, a need for standardized ways of assessing patients’ improvements became evident. At the end of this process, randomized, controlled double blind trials seem the mandatory standard, although good clinical judgment keeps its place in finding new treatment options. In this chapter, we shall give an overview on currently available medications for the long-term treatment of alcohol dependence. We concentrate on the compounds for which sufficient evidence base is available, which are approved for alcohol dependence and which are currently being used in many parts of the world. Wherever possible we concentrate on meta-analyses without referring to all the individual studies. Should there be Cochrane reviews on specific medications, our recommendations shall rely on those. The presentation of medications roughly follows the order of their approval by national or international authorities. There are a few other medications which are not approved for alcoholism but for other medical indications and which are currently suggested for an off-label use in alcoholism. These will be mentioned on a shorter note.
2 Pharmacological Treatment Options
2.1 Disulfiram
2.1.1 Pharmacology
As mentioned above, the potential of disulfiram (tetraethylthiuram disulfide) to modify alcohol consumption was found by serendipity. After disulfiram had been identified as the substance which caused the change in drinking habits, further research revealed the mechanism of action (Martensen-Larsen 1948). Disulfiram blocks the natural degradation of alcohol. Specifically it irreversibly inhibits the acetaldehyde dehydrogenase for 2–5 days, a condition which is only terminated by de novo synthesis of the enzyme. The accumulation of acetaldehyde in the body results in unpleasant symptoms such as rush, nausea, headache, diarrhea, vomiting, and a drop in blood pressure. Similar symptoms can be seen in about 50 % of the Asian population with a genetically determined lack of an ISO-enzyme of the acetaldehyde dehydrogenase which again leads to an accumulation of acetaldehyde when alcohol is consumed.
2.1.2 Indications and Contraindications
The indication for severe alcohol dependence is clear. Disulfiram should only be prescribed once the patient has been detoxified and is free of alcohol and without withdrawal symptoms. Several contraindications need to be taken into account: cardiomyopathy, coronary heart disease, severe heart arrhythmia, esophageal varicosis, hypothyroidism, and advanced arteriosclerosis. Disulfiram should also not be prescribed when patients suffer from asthma bronchiale, decompensated liver cirrhosis, and severe hypotonia. Accumulation of acetaldehyde in the human body as mentioned above can lead to very aversive reactions including death in a number of cases where the administration of disulfiram was not sufficiently supervised. Therefore, disulfiram should only be prescribed by doctors who are well aware of its potential but also of its risks and who have ample experience with the drug. For this caveat many colleagues consider disulfiram only as a “second choice treatment”; others prescribe it quite regularly (Brewer 1993).
2.1.3 Dosage and Undesired Effects
The dosage of disulfiram has to be tapered up starting with 250 mg in the first day moving to 500 mg as of the third day of treatment for maintenance dosage. Higher doses up to 1,000–1,500 mg might be appropriate when patients take the pill every second day (Mon-Wed-Fri). The drug should be taken orally; attempts with subcutaneous implants were not really convincing in the long run (Marie 1955). Originally patients were asked to drink alcohol after having taken disulfiram. Under supervision they should thus experience the aversive effects of the drug when alcohol is consumed. Later studies indicated that this test is not mandatory. Disulfiram worked as well without it (Krampe et al. 2006). If no alcohol is consumed, the most important side effect is sedation and initial sleepiness. However, this is transient in most cases and therefore no real reason for concern.
2.1.4 Efficacy
An early meta-analysis showed the superiority of disulfiram over placebo (Agosti 1995). However, this result was questioned by a large randomized trial in the USA where no significant benefit was found (Fuller et al. 1986). While this trial was very influential in some parts of the world, it did not convince clinicians who had long worked with this drug especially after some of the earlier safety issues had been resolved (Chick 1999). In Germany, disulfiram witnessed a renaissance after a group at Göttingen University published a long-term study with extremely ill patients who had been coming into the clinic literally every day for supervised intake for more than a year (Krampe et al. 2006). So far we have only limited evidence on disulfiram from head-to-head comparisons with other anticraving medications. Some publications point to a superiority over other approved medications such as acamprosate and naltrexone (Besson et al. 1998; De Sousa 2004; Laaksonen et al. 2008). This was reflected in several meta-analyses as well (i.e., Berglund et al. 2003).
2.2 Naltrexone
Naltrexone is the second drug which was approved for the long-term treatment of alcoholism. Based on observations in monkeys (Altshuler et al. 1980), two clinical trials were undertaken in the USA which showed a benefit over placebo (Volpicelli et al. 1992; O’Malley et al. 1992) and convinced the FDA to grant a rapid approval.
2.2.1 Pharmacology
Naltrexone is a competitive opiate antagonist with high affinity to the μ-receptor and lower affinity to the δ- and κ-receptors . The consumption of alcohol increases the release of brain endorphin (Gianoulakis et al. 1996) and subsequently of dopamine which results in the positive reinforcing effects of alcohol . A specific blockade of the μ-receptors and thus of the positive reinforcement of alcohol is the most likely explanation of naltrexone’s clinical efficacy (Sinclair et al. 2002; Heilig et al. 2011). Although the plasma half-life of naltrexone and its active metabolite ß-naltrexol is only about 10–12 h, its μ-receptor occupancy shown with PET studies lasts for about 48–72 h (Lee et al. 1988). For the specific impact of a polymorphism of the μ opiate receptor gene, see below.
2.2.2 Indications and Contraindications
Naltrexone has been approved for the treatment of drug and alcohol dependence. When prescribing naltrexone, it is important to assure that there was no recent opioid consumption either as pain medication or consumed illegally.
2.2.3 Dosage and Undesired Effects
While dosages of 100 g and more have been tested, it is a broad consensus nowadays that a daily dosage of 50 mg which means one pill a day is sufficient in the treatment of alcoholism. Nausea, dizziness, headache, and insomnia are the most prevalent side effects of naltrexone. In the USA, naltrexone carries a box warning by the FDA due to its potentially aggravating effects of alcoholic liver dysfunction.
2.2.4 Efficacy
The two pivotal trials (Volpicelli et al. 1992; O’Malley et al. 1992) were followed by many more studies around the world (Mann 2004). More than half of them showed significant superiority over placebo. Those which did not were often not powered well enough, were done in difficult to treat patients (Krystal et al. 2001), or had a very high placebo response (Gastpar et al. 2002; Mann et al. 2013). Recent meta-analyses and a Cochrane analysis conclude that there is a clear benefit of naltrexone in the treatment of alcoholism (Rösner et al. 2010a, b). A genetic component in treatment response was first demonstrated in a post hoc analysis of three independent trials (Oslin et al. 2003). Patients were genotyped looking for carriers of the Asp40 allele (A/G, G/G) versus individuals carrying the Asn40 allele (A/A). The positive treatment effect was confined to patients who carried at least one G allele. This finding has been replicated several times (Anton 2008) but remains somewhat controversial due to negative studies (Gelernter et al. 2007).
2.3 Acamprosate
Acamprosate , a calcium-bis-acetylhomotaurinat, was first discovered and tested in France (Lhuintre et al. 1985; Mann 2004). The results of several clinical studies led to an approval in most European countries in the mid-1990s. The approval in the USA followed about a decade later.
2.3.1 Pharmacology
Acamprosate is the calcium salt of N-acetyl homotaurine, a small, highly flexible molecule with similarities to many amino acids, most notably glutamate, gamma-aminobutyric acid, aspartate, glycine, and taurine (Spanagel and Zieglgänsberger 1997; Spanagel and Kiefer 2008). Its mechanism of action seems to be linked to a high activity of the glutamatergic system in alcoholics. Acamprosate binds to NMDA-receptors and thus dampens the glutamate mediated excitability (Spanagel and Mann 2005). There are some reports about a binding of acamprosate to the polyamine site of the NMDA receptor as well as binding to the mGluR5 receptor (Harris et al. 2002). It could be shown that a blockade of the mGluR5-receptor reduced the self-administration of alcohol in free-choice paradigms in animal models (Spanagel and Mann 2005). Although most recent work has focused on the glutamatergic system, homotaurine is a known GABA(A) receptor agonist, and studies on neuronal networks in vivo suggest that acamprosate may have differential effects on glutamate/NMDA receptors at low concentrations, with effects on GABA(A) receptors at higher concentrations (Pierrefiche et al. 2004). Some data suggest that acamprosate dampens alcohol-induced dopamine release (Cowen et al. 2005). The same could be true in conditioned withdrawal situations. This would mean that acamprosate also acts via a blockade of the reinforcing effect of alcohol (for a more exhaustive discussion of acamprosate’s potential mechanisms of action including its neuroprotective effects , see de Witte et al. (2005) and Mann et al. (2008).
2.3.2 Indications and Contraindications
Acamprosate is approved for the treatment of alcohol dependence. It is supposed to be prescribed for the maintenance of an already established state of abstinence . Contraindications are pregnancy and lactation as well as renal insufficiency with serum creatinine levels of more than 120 μmol/l.
2.3.3 Dosage and Undesired Effects
The daily dosage of acamprosate is 1996 mg (three times two tablets). Since it takes several days until clinically meaningful brain concentrations are established, the treatment should begin as soon as possible. Acamprosate does not interact with other medications and does not influence alcohol toxicity. Its main side effects are diarrhea and other gastrointestinal symptoms as well as headache and pruritus.
2.3.4 Efficacy
There have been a large number of randomized controlled trials worldwide testing acamprosate against placebo (Kiefer and Mann 2010). The majority showed a significant benefit of acamprosate. This is corroborated by Cochrane analyses, the latest of which was published in 2012 (Rösner et al. 2010a, b). However, there were several negative studies as well such as the large COMBINE study in the USA (Anton et al. 2006) and more recently by Mann et al. (2013). Based on its potential mechanism of action described above (dampening of a hyper-glutamatergic state ) it was speculated that acamprosate could be more beneficial in severely affected patients who are more likely to suffer from an upregulated glutamate system (Spanagel and Kiefer 2008). Our own study with a head-to-head comparison of two cohorts of patients who differed in severity measures did not support this assumption (Mann et al. 2013). Another idea according to which acamprosate would be more beneficial to individuals who relapse for the negative reinforcing effect of alcohol (Verheul et al. 1999; Mann et al. 2009; Heilig et al. 2011) still awaits empirical support. The first studies aiming to associate acamprosate’s efficacy with genetic markers suggest an involvement of a single-nucleotide polymorphism located in the GATA binding protein 4 (GATA4) gene (Kiefer et al. 2011). GATA4 represents a factor regulating the transcription of ANP and showed an association with alcohol dependence in two independent genome-wide association studies on alcohol dependence (Treutlein et al. 2009; Edenberg et al. 2010).
2.4 Nalmefene
Nalmefene is the most recent medication approved for use in alcohol dependence. It was approved by the European Medicines Agency in 2012 for a reduction of heavy drinking days and/or total alcohol consumption.
2.4.1 Pharmacology
Nalmefene is a selective opioid ligand with an equally high affinity to the μ- and κ-receptors and medium affinity to the δ-receptor. It acts as an antagonist at the μ- and δ-receptors, but different from naltrexone, it is a co-agonist at the κ-receptor (Bart et al. 2005). Studies in rodents seem to show that the difference compared with naltrexone concerning the action at the κ-receptor might be of relevance lending the drug higher potency in animals with more severe dependence (Walker et al. 2011). However, this finding needs to be replicated in humans.
Nalmefene has several metabolites which have much less affinity to the μ-receptors than the parent substance. Only nalmefene 3-O-sulfate contributes to the pharmacological effect, but this metabolite is only present in low concentrations. Nalmefene has a plasma half-life of 10–12 h. Blockade of brain receptors with nalmefene lasts between 48 and 72 h.
The mechanism of action is mainly based on its antagonistic properties at the μ-receptor. This counteracts the reinforcement driven by an alcohol-triggered mesolimbic dopamine release which is facilitated by the release of ß-endorphins. In studies with animal models, an additional effect based on nalmefene’s role as a partial κ-receptor agonist (Walker et al. 2011) was observed. This is currently being investigated in humans.
2.4.2 Indications and Contraindications
The official indication for nalmefene is to reduce alcohol consumption (number of heavy drinking days, total alcohol consumption) in alcohol-dependent patients who have a high drinking level according to the World Health Organization (WHO 2000: men >60 g/day and women >40 g/day) and continue to have this level 2 weeks after the initial assessment. It is important to ensure that patients have not recently consumed opioids either as pain medication or illegally.
2.4.3 Dosage and Undesired Effects
The dosage per day is 20 mg, but nalmefene can be taken as needed. Dizziness, nausea, and insomnia are the most prevalent side effects. In the recent clinical trials, these were mild to moderate and mostly transient.
2.4.4 Efficacy
Several earlier studies indicated its efficacy in reducing consumption in alcohol-dependent patients (Mason et al. 1999; Karhuvaara et al. 2007). One study did not show a significant effect (Anton et al. 2004). Recently three large-scale phase III studies were conducted in Europe which showed efficacy over placebo in reducing heavy drinking days and total alcohol consumption; all three studies are published (Mann et al. 2013; Gual et al. 2013; van den Brink et al. 2013).
2.5 Topiramate
This medication is approved for the treatment of epilepsy. Its use in alcoholism has been tested because of indications that it reduces the reinforcing effects of alcohol and inhibits glutamatergic pathways in the corticomesolimbic system (Johnson 2005; White et al. 2004). A first positive single-site trial (Johnson et al. 2003) was followed by a larger multisite trial (Johnson et al. 2007). This latter showed a significant effect over placebo in reducing alcohol consumption. Patients did not have to be abstinent to participate which was different from many other studies referred to in this chapter (with the exception of the nalmefene trials, see above). The effect size was considerable, but undesired effects were as important as expected. Therefore, the medication had to be carefully titrated from week 0 to week 5. Undesired effects were paresthesia, headache, taste perversion, fatigue , and difficulty with concentration and memory. A smaller and more recent study did not show a significant effect (Likhitsathian et al. 2013). However, as expected the first meta-analysis comes to a positive overall effect of the drug (Arbaizar et al. 2010). In conclusion, off-label use may be worth trying but only with a titration of the dose and under very careful consideration and monitoring of these side effects (Aubin and Daeppen 2013).
2.6 Baclofen
Baclofen acts as an agonist at the B subunit of GABA receptor (GABA-B). Since GABA neurotransmission is known to be involved in the regulation of anxiety as a common symptom in patients being treated for alcohol withdrawal and alcohol dependence, baclofen was repeatedly tested in alcohol-dependent subjects (Addolorato and Leggio 2010). Recently, Brennan et al. (2013) assessed the benefit of baclofen for alcohol dependence in a review of the literature based on randomized controlled trials and case series. Although primary outcomes differed between trials, patients treated with baclofen (30 mg) experienced higher rates of abstinence from alcohol than those taking placebo in the majority of case series and two of the randomized controlled trials (Addolorato et al. 2002, 2007). Data suggest that baclofen was safe in patients with alcohol dependence, including those with moderate to severe liver cirrhosis and may provide beneficial anxiolytic effects. However, the largest available randomized controlled trial by Garbutt et al. (2010) failed to show a benefit for 30 mg baclofen in assessing the efficacy and safety in terms of weekly heavy drinking days and percentage of abstinent days or for the secondary outcomes of craving, for example, depression. Again, baclofen was well tolerated with no significant reported adverse events.
Taken together, positive effects from using baclofen for the treatment of alcohol dependence can be surmised; however, the small number of studies currently does not allow a final conclusion. Larger trials that include higher dosages of baclofen (up to 270 mg daily) are currently ongoing.
2.7 Combining Anticraving Medications
There were a number of attempts to combine anticraving medications. The most important maybe were testing acamprosate plus naltrexone versus placebo or versus each single medication. While a first combination study (Kiefer et al. 2003) showed a benefit of the combination over placebo, an Australian study (Morley et al. 2006) and the COMBINE study (Anton et al. 2006) were not able replicate this finding. However, treatment groups differed markedly, and the role of detoxification and abstinence when starting medication as well as the role of the interaction with concomitant psychotherapy remain to be determined. At least two comparisons of acamprosate and/or naltrexone with disulfiram point to a higher efficacy of disulfiram (Besson et al. 1998; Laaksonen et al. 2008), but these studies had to be done single blind with all the limitations involved here. In conclusion, to date a combination of anticraving medications in uncomplicated alcoholics (no depression, etc.) does not seem overly convincing.
2.8 Additional Psychosocial Treatment
Some kind of counseling to ensure motivation and compliance was mandatory in almost all of the trials referred to in this chapter. In most cases this additional psychosocial treatment was manualized, and staff had to be trained to deliver it (Starosta et al. 2006; Pettinati et al. 2004; Johnson et al. 2007; Brüeck and Mann 2006). It varied in intensity with no hint that more is better (see COMBINE study, Anton et al. 2006). For clinical practice this means that some kind of counseling including advice and maybe motivational elements is recommended when these medications are prescribed to alcohol-dependent patients.
References
Addolorato G, Caputo F, Capristo E et al (2002) Baclofen efficacy in reducing alcohol craving and intake: a preliminary double-blind randomized controlled study. Alcohol Alcohol 37:504–508
Addolorato G, Leggio L, Ferrulli A et al (2007) Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: a randomized, double-blind, controlled study. Lancet 370(9603):1915–1922
Addorolato G, Leggio L (2010) Safety and efficacy of baclofen in the treatment of alcohol-dependent patients. Curr Pharm Des 16(19):2113–2117
Agosti V (1995) The efficacy of treatments in reducing alcohol consumption: a meta-analysis. Int J Addict 30:1067–1077
Altshuler HL, Phillips PE, Feinhandler DA (1980) Alteration of ethanol self-administration by naltrexone. Life Sci 26:679–688
Anton RF (2008) Genetic basis for predicting response to naltrexone in the treatment of alcohol dependence. Pharmacogenomics 9(6):655–658
Anton RF, Pettinati H, Zweben A, Kranzler HR, Johnson B, Bohn MJ, McCaul ME, Anthenelli R, Salloum I, Galloway G, Garbutt J, Swift R, Gastfriend D, Kallio A, Karhuvaara S (2004) A multi-site dose ranging study of nalmefene in the treatment of alcohol dependence. J Clin Psychopharmacol 24:421–428
Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, Gastfriend DR, Hosking JD, Johnson BA, LoCastro JS, Longabaugh R, Mason BJ, Mattson ME, Miller WR, Pettinati HM, Randall CL, Swift R, Weiss RD, Williams LD, Zweben A, COMBINE Study Research Group (2006) Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA 295:2003–2017
Arbaizar B, Diersen-Sotos T, Gómez-Acebo I, Llorca J (2010) Topiramate in the treatment of alcohol dependence: a meta-analysis. Actas Esp Psiquiatr 38:8–12
Aubin HJ, Daeppen JB (2013) Emerging pharmacotherapies for alcohol dependence: a systematic review focusing on reduction in consumption. Drug Alcohol Depend. doi:pii: S0376-8716(13)00154-3. 10.1016/j.drugalcdep. Epub ahead of print
Bart G, Schluger JH, Borg L, Ho A, Bidlack JM, Kreek MJ (2005) Nalmefene induced elevation in serum prolactin in normal human volunteers: partial kappa opioid agonist activity? Neuropsychopharmacology 30:2254–2262
Berglund M, Thelander S, Salaspuro M, Franck J, Andréasson S, Ojehagen A (2003) Treatment of alcohol abuse: an evidence-based review. Alcohol Clin Exp Res 27:1645–1656
Besson J, Aeby F, Kasas A, Lehert P, Potgieter A (1998) Combined efficacy of acamprosate and disulfiram in the treatment of alcoholism: a controlled study. Alcohol Clin Exp Res 22:573–579
Brennan JL, Leung JG, Gagliardi JP, Rivelli SK, Muzyk AJ (2013) Clinical effectiveness of baclofen for the treatment of alcohol dependence: a review. Clin Pharmacol 5:99–107
Brewer C (1993) Long-term, high-dose disulfiram in the treatment of alcohol abuse. Br J Psychiatry 163:687–689
Brüeck G, Mann K (2006) Alkoholismusspezifische Psychotherapie: Manual mit Behandlungs-smodulen. (Alcoholism-specific psychotherapy: manual with treatment modules). Deutscher Ärzteverlag, Köln
Chick J (1999) Safety issues concerning the use of disulfiram in treating alcohol dependence. Drug Saf 20:427–435, Review
Cowen MS, Adams C, Kraehenbuehl T, Vengeliene V, Lawrence AJ (2005) The acute anti-craving effect of acamprosate in alcohol-preferring rats is associated with modulation of the mesolimbic dopamine system. Addict Biol 10:233–242
De Sousa A (2004) A one-year pragmatic trial of naltrexone vs disulfiram in the treatment of alcohol dependence. Alcohol Alcohol 39:528–531
Edenberg HJ, Koller DL, Xuei X, Wetherill L, McClintick JN, Almasy L, Bierut LJ, Bucholz KK, Goate A, Aliev F, Dick D, Hesselbrock V, Hinrichs A, Kramer J, Kuperman S, Nurnberger JI Jr, Rice JP, Schuckit MA, Taylor R, Todd Webb B, Tischfield JA, Porjesz B, Foroud T (2010) Genome-wide association study of alcohol dependence implicates a region on chromosome 11. Alcohol Clin Exp Res 34:840–852
Edwards G (2000) Alcohol: the world’s favorite drug. St. Martin’s Press, New York, p 118
Edwards G (2005) History of prevention of relapse. In: Spanagel R, Mann K (eds) Drugs for relapse prevention of alcoholism. Birkhäuser Verlag, Switzerland
Fuller RK, Branchey L, Brightwell DR, Derman RM, Emrick CD, Iber FL, James KE, Lacoursiere RB, Lee KK, Lowenstam I et al. (1986) Disulfiram treatment of alcoholism. A Veterans Administration Cooperative Study. JAMA 256:1449–1455
Garbutt JC, Kampov-Polevoy AB, Gallop R, Kalka-Juhl L, Flannery BA (2010) Efficacy and safety of baclofen for alcohol dependence: a randomized, double-blind, placebo-controlled trial. Alcohol Clin Exp Res 34:1–9
Gastpar M, Bonnet U, Böning J, Mann K, Schmidt LG, Soyka M, Wetterling T, Kielstein V, Labriola D, Croop R (2002) Lack of efficacy of naltrexone in the prevention of alcohol relapse: results from a German Multicenter Study. J Clin Psychopharmacol 22:592–598
Gelernter J, Gueorguieva R, Kranzler HR, Zhang H, Cramer J, Rosenheck R, Krystal JH, VA Cooperative Study #425 Study Group (2007) Opioid receptor gene (OPRM1, OPRK1, and OPRD1) variants and response to naltrexone treatment for alcohol dependence: results from the VA Cooperative Study. Alcohol Clin Exp Res 31(4):555–563
Gianoulakis C, de Waele JP, Thavundayil J (1996) Implication of the endogenous opioid system in excessive ethanol consumption. Alcohol 13:19–23
Gual A, He Y, Torup L, van den Brink W, Mann K, for the ESENSE 2 Study Group (2013) A randomised, double-blind, placebo-controlled, efficacy study of nalmefene, as-needed use, in patients with alcohol dependence. Eur Neuropsychopharmacol. doi:pii: S0924-977X(13)00075-8. 10.1016/j. Epub ahead of print
Harris BR, Prendergast MA, Gobson DA, Rogers DT, Blanchard JA, Holley RC, Fu MC, Hart SR, Pedigo NW, Littleton JM (2002) Acamprosate inhibits the binding and neurotoxic effects of trans-ACPD, suggesting a novel site of action at metabotropic glutamate receptors. Alcohol Clin Exp Res 26:1779–1793
Heilig M, Goldman D, Berrettini W, O’Brien CP (2011) Pharmacogenetic approaches to the treatment of alcohol addiction. Nat Rev Neurosci 12:670–684
Johnson BA (2005) Recent advances in the development of treatments for alcohol and cocaine dependence: focus on topiramate and other modulators of GABA or glutamate function. CNS Drugs 19:873–896, Review
Johnson BA, Ait-Daoud N, Bowden CL, DiClemente CC, Roache JD, Lawson K, Javors MA, Ma JZ (2003) Oral topiramate for treatment of alcohol dependence: a randomised controlled trial. Lancet 361:1677–1685
Johnson BA, Rosenthal N, Capece JA, Wiegand F, Mao L, Beyers K, McKay A, Ait-Daoud N, Anton RF, Ciraulo DA, Kranzler HR, Mann K, O’Malley SS, Swift RM (2007) Topiramate for treating alcohol dependence: a randomized controlled trial. JAMA 298:1641–1651
Karhuvaara S, Simojoki K, Virta A, Rosberg M, Löyttyniemi E, Nurminen T, Kallio A, Mäkelä R (2007) Targeted nalmefene with simple medical management in the treatment of heavy drinkers: a randomized double-blind placebo-controlled multicenter study. Alcohol Clin Exp Res 31:1179–1187
Kiefer F, Mann K (2010) Acamprosate: how, where, and for whom does it work? Curr Pharm Des 16(19):2098–2102
Kiefer F, Jahn H, Tarnaske T, Helwig H, Briken P, Holzbach R, Kämpf P, Stracke R, Baehr M, Naber D, Wiedemann K (2003) Comparing and combining naltrexone and acamprosate in relapse prevention of alcoholism: a double-blind, placebo-controlled study. Arch Gen Psychiatry 60:92–99
Kiefer F, Witt SH, Frank J, Richter A, Treutlein J, Lemenager T, Nöthen MM, Cichon S, Batra A, Berner M, Wodarz N, Zimmermann US, Spanagel R, Wiedemann K, Smolka MN, Heinz A, Rietschel M, Mann K (2011) Involvement of the atrial natriuretic peptide transcription factor GATA4 in alcohol dependence, relapse risk and treatment response to acamprosate. Pharmacogenomics J 11:368–374
Krampe H, Stawicki S, Wagner T, Bartels C, Aust C, Rüther E, Poser W, Ehrenreich H (2006) Follow-up of 180 alcoholic patients for up to 7 years after outpatient treatment: impact of alcohol deterrents on outcome. Alcohol Clin Exp Res 30:86–95
Krystal JH, Cramer JA, Krol WF, Kirk GF, Rosenheck RA (2001) Naltrexone in the treatment of alcohol dependence; Veterans Affairs Naltrexone Cooperative Study 425 Group. N Engl J Med 345:1734–1749
Laaksonen E, Koski-Jännes A, Salaspuro M, Ahtinen H, Alho H (2008) A randomized, multicentre, open-label, comparative trial of disulfiram, naltrexone and acamprosate in the treatment of alcohol dependence. Alcohol Alcohol 43:53–61
Lee MC, Wagner HN Jr, Tanada S, Frost JJ, Bice AN, Dannals RF (1988) Duration of occupancy of opiate receptors by naltrexone. J Nucl Med 29:1207–1211
Lewin L (1931) Phantastica: narcotic and stimulating drugs. Kegan Paul/Trench and Trubner, London
Lhuintre JP, Daoust M, Moore ND, Chretien P, Saligaut C, Tran G, Bosimare F, Hillemand B (1985) Ability of calcium bis acetyl homotaurine, a GABA agonist, to prevent relapse in weaned alcoholics. Lancet 1:1014–1016
Likhitsathian S, Uttawichai K, Booncharoen H, Wittayanookulluk A, Angkurawaranon C, Srisurapanont M (2013) Topiramate treatment for alcoholic outpatients recently receiving residential treatment programs: a 12-week, randomized, placebo-controlled trial. Drug Alcohol Depend. doi:pii: S0376-8716(13)00251-2. Epub ahead of print
Mann K (2004) Pharmacotherapy of alcohol dependence: a review of the clinical data. CNS Drugs 18:485–504
Mann K, Lehert P, Morgan MY (2004) The efficacy of acamprosate in the maintenance of abstinence in alcohol-dependent individuals: results of a meta-analysis. Alcohol Clin Exp Res 28:51–63
Mann K, Kiefer F, Spanagel R, Littleton JM (2008) Acamprosate: recent findings and future research directions. Alcohol Clin Exp Res 32:1105–1110
Mann K, Kiefer F, Smolka M, Gann H, Wellek S, Heinz A (2009) Searching for responders to acamprosate and naltrexone in alcoholism treatment: rationale and design of the PREDICT study. Alcohol Clin Exp Res 33:674–683
Mann K, Bladström A, Torup L, Gual A, van den Brink W, The ESENSE 1 Study Group (2013) Extending the treatment options for patients with alcohol dependence – a randomised controlled study of nalmefene. Biol Psychiatry 73:706–713
Marie C (1955) A propos d’un nouveau mode de traitement de l’alcoolisme chronique par implantation de disulfure de tétraéthylthiourame. (A new way of treating chronic alcoholism by implanting tetraethylthiuran disulfat) Thèse, Paris
Martensen-Larsen O (1948) Treatment of alcoholism with a sensitizing drug. Lancet 25:6539
Mason BJ, Salvato FR, Williams LD, Ritvo EC, Cutler RB (1999) A double-blind, placebo-controlled study of oral nalmefene for alcohol dependence. Arch Gen Psychiatry 56:719–724
Morley KC, Teesson M, Reid SC, Sannibale C, Thomson C, Phung N, Weltman M, Bell JR, Richardson K, Haber PS (2006) Naltrexone versus acamprosate in the treatment of alcohol dependence: a multi-centre, randomized, double-blind, placebo-controlled trial. Addiction 101:1451–1462
O’Malley SS, Jaffe AJ, Chang G, Schottenfeld RS, Meyer RE, Rounsaville B (1992) Naltrexone and coping skills therapy for alcohol dependence. A controlled study. Arch Gen Psychiatry 49:881–887
Oslin DW, Berrettini W, Kranzler HR, Pettinati H, Gelernter J, Volpicelli JR, O’Brien CP (2003) A functional polymorphism of the mu-opioid receptor gene is associated with naltrexone response in alcohol-dependent patients. Neuropsychopharmacology 28:1546–1552
Pettinati HM, Weiss RD, Miller WR, Donovan D, Ernst DB, Rounsaville BJ (2004) volume 2. Medical management treatment manual: a clinical research guide for medically trained clinicians providing pharmacotherapy as part of the treatment for alcohol dependence. DHHS publication no. (NIH) 04-5289. NIAAA, Bethesda
Pierrefiche O, Daoust M, Naassila M (2004) Biphasic effect of acamprosate on NMDA but not on GABAA receptors in spontaneous rhythmic activity from the isolated neonatal rat respiratory network. Neuropharmacology 47:35–45
Rösner S, Hackl-Herrwerth A, Leucht S, Lehert P, Vecchi S, Soyka M (2010a) Acamprosate for alcohol dependence. Cochrane Database Syst Rev 9, CD004332
Rösner S, Hackl-Herrwerth A, Leucht S, Vecchi S, Srisurapanont M, Soyka M (2010b) Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev 12:CD001867
Sinclair JD, Alho H, Shinderman M (2002) Naltrexone for alcohol dependence. N Engl J Med 346:1329–1331
Spanagel R, Kiefer F (2008) Drugs for relapse prevention of alcoholism: ten years of progress. Trends Pharmacol Sci 29(3):109–115
Spanagel R, Mann K (eds) (2005) Drugs for relapse prevention in alcoholism. Birkhäuser Verlag, Basel
Spanagel R, Zieglgänsberger W (1997) Anti-craving compounds for ethanol: new pharmacological tools to study addictive processes. Trends Pharmacol Sci 18:54–59
Starosta AN, Leeman RF, Volpicelli JR (2006) The BRENDA model: integrating psychosocial treatment and pharmacotherapy for the treatment of alcohol use disorders. J Psychiatr Pract 12:80–89
Treutlein J, Cichon S, Ridinger M, Wodarz N, Soyka M, Zill P, Maier W, Moessner R, Gaebel W, Dahmen N, Fehr C, Scherbaum N, Steffens M, Ludwig KU, Frank J, Wichmann HE, Schreiber S, Dragano N, Sommer WH, Leonardi-Essmann F, Lourdusamy A, Gebicke-Haerter P, Wienker TF, Sullivan PF, Nöthen MM, Kiefer F, Spanagel R, Mann K, Rietschel M (2009) Genome-wide association study of alcohol dependence. Arch Gen Psychiatry 66:773–784
van den Brink W, Aubin HJ, Bladström A, Torup L, Gual A, Mann K (2013) Efficacy of nalmefene as-needed in alcohol dependent patients with at least high drinking risk level: results from a subgroup analysis of two randomised controlled 6-month studies. Alcohol & Alcohol, ahead of print
Verheul R, van den Brink W, Geerlings P (1999) A three-pathway psychobiological model of craving for alcohol. Alcohol Alcohol 34:197–222
Volpicelli JR, Alterman AI, Hayashida M, O’Brien CP (1992) Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry 49:876–880
Walker BM, Zorrilla EP, Koob GF (2011) Systemic κ-opioid receptor antagonism by nor-binaltorphimine reduces dependence-induced excessive alcohol self-administration in rats. Addict Biol 16:116–119
White HS, Brown SD, Woodhead JH, Skeen GA, Wolf HH (2004) Topiramate modulates GABA-evoked currents in murine cortical neurons by a nonbenzodiazepine mechanism. Epilepsia 41(Suppl 1):S17–S20
Witte P, Bachteler D, Spanagel R (2005) Acomprasate: preclinical data. In: Spanagel and Mann (eds) Drugs for Relapse Prevention of Alcoholism. Birkhäuser Verlag, Basel, Boston, Berlin, 2005:73–84
World Health Organization (WHO) (2000) International guide for monitoring alcohol consumption and related harm. WHO/MSD/MSB/00.4. 2000 http://whqlibdoc.who.int/hq/2000/who_msd_msb_00.4.pdf
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Italia
About this entry
Cite this entry
Mann, K., Kiefer, F. (2015). Pharmacological Long-Term Treatment of Alcohol Use Disorders. In: el-Guebaly, N., Carrà, G., Galanter, M. (eds) Textbook of Addiction Treatment: International Perspectives. Springer, Milano. https://doi.org/10.1007/978-88-470-5322-9_12
Download citation
DOI: https://doi.org/10.1007/978-88-470-5322-9_12
Published:
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-5321-2
Online ISBN: 978-88-470-5322-9
eBook Packages: MedicineReference Module Medicine