Abstract
Neoplasms of the biliary tree include a wide spectrum of lesions that range from benign tumors, such as adenomas, to malignant lesions, such as adenocarcinomas. Cholangiocarcinoma is the tumor of the biliary tract that has the highest incidence and the poorest prognosis, which depends most of all on the therapeutic strategy. Accurate characterization in terms of diagnosis and staging of the neoplasms can be crucial for determining prognosis and treatment planning, and different imaging techniques can be used to achieve the best diagnostic setting of the case. Magnetic resonance cholangiopancreatography (MRCP) is one of the best imaging techniques for the depiction of the biliary tree, and it can be very helpful in cases of tumors with poor prognosis in which a life-saving therapeutic strategy depends mostly on the initial staging of the disease (e.g., in cholangiocarcinoma). For these reasons, in this chapter, cholangiocarcinoma is first comprehensively described, and following on from this there are brief descriptions of benign neoplasms of the biliary tree.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Bile Duct
- Primary Sclerosing Cholangitis
- Biliary Tree
- Intraductal Papillary Mucinous Tumor
- Biliary Stricture
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Neoplasms of the biliary tree include a wide spectrum of lesions that range from benign tumors, such as adenomas, to malignant lesions, such as adenocarcinomas. Cholangiocarcinoma is the tumor of the biliary tract that has the highest incidence and the poorest prognosis, which depends most of all on the therapeutic strategy. Accurate characterization in terms of diagnosis and staging of the neoplasms can be crucial for determining prognosis and treatment planning, and different imaging techniques can be used to achieve the best diagnostic setting of the case. Magnetic resonance cholangiopancreatography (MRCP) is one of the best imaging techniques for the depiction of the biliary tree, and it can be very helpful in cases of tumors with poor prognosis in which a life-saving therapeutic strategy depends mostly on the initial staging of the disease (e.g., in cholangiocarcinoma). For these reasons, in this chapter, cholangiocarcinoma is first comprehensively described, and following on from this there are brief descriptions of benign neoplasms of the biliary tree.
2 Cholangiocarcinoma
Cholangiocarcinoma is the most frequent malignant neoplasm of the biliary tree, and it grows from the epithelial cells of the intrahepatic and extrahepatic bile ducts [1]. In approximately 90% of cases it is an adenocarcinoma, with glandular structures growing in cellular nests separated by fibrous stroma [2, 3].
Several risk factors are described for cholangiocarcinoma; these include: primary sclerosing cholangitis, choledochal cysts, familial polyposis, congenital hepatic fibrosis, infection with Clonorchis sinensis, intrahepatic stone disease, and a history of chemical and thorium dioxide exposure. Cholangiocar ― cinoma has a poor prognosis, with an overall 5-year survival rate of 1% [4], which becomes 20% after surgery [5]. For this reason, accurate pre-operative staging, available through different imaging techniques, is mandatory for assessment of the correct therapeutic strategy.
According to the localization of the tumor, cholangiocarcinoma is classified into intrahepatic, hilar and extrahepatic. Intrahepatic cholangiocarcinoma arises from the bile ducts peripheral to the secondary bifurcation of the left or right hepatic duct; hilar cholangiocarcinoma arises from one of the hepatic ducts and can involve the bifurcation of the common bile duct; extrahepatic cholangiocarcinoma arises from any part of the extrahepatic duct [3, 6].
2.1 Intrahepatic Cholangiocarcinoma
Intrahepatic cholangiocarcinoma originates from biliary epithelium at any portion of the intrahepatic biliary system, from the segmental bile ducts to the ductal epithelium [1, 7] (Fig. 5.1). It accounts for almost 10% of all bile duct tumors. It presents local spread and may have small satellite nodules, with focal or segmental intrahepatic bile duct obstruction. As it does not cause clinical symptoms in its early stages, it usually presents as a large mass at diagnosis; when small, it is usually found incidentally during ultrasound (US) or computed tomography (CT) performed for other causes [8]. When symptomatic, clinical manifestations are non-specific, such as abdominal pain, malaise, night sweats and cachexia. Since intrahepatic cholangiocarcinoma is the most common primary malignant intrahepatic mass lesion in the absence of a history of other primary solid malignancies or cirrhosis, a differential diagnosis must be made, especially with hepatocellular carcinoma.
Peripheral cholangiocarcinoma. Axial magnetic resonance (MR) T1-weighted images during the arterial (a) and portal venous (b) phases show a nodular lesion in the fourth segment with heterogeneous and peripheral enhancement of the contrast medium in the early phase and slow accumulation during the portal venous phase (arrow). c The coronal post-contrast MR T1-weighted image shows the origin of the lesion (arrow) in the parietal thickening of a bile duct responsible for dilatation of the upstream biliary branches (arrowheads). d MR cholangiopancreatography confirms exclusive dilatation of the bile ducts in the paramedian segments of right hepatic lobe (arrowheads), and this comes to an abrupt halt at the right secondary biliary bifurcation (arrow). e Axial contrast-enhanced computed tomography section after a surgical procedure (mesohepatectomy extended to caudate lobe) shows multiple metallic clips (short arrows) and patency of the left portal branch (dashed arrow). f Post-operative cholangiography performed through two biliary drainages (open arrow) shows the normal caliber of the bile ducts for the right posterior-lateral sector (p) and the intrahepatic biliary ducts of the left lobe (s)
For intrahepatic cholangiocarcinoma, prognostic factors confirmed on multivariate analysis include tumor number and differentiation, lymph node metastases and vascular invasion [9]. While US can usually detect only focal duct dilatation, CT and magnetic resonance imaging (MRI) are comparable in the detection and correct diagnosis of the tumor. CT is the preferable technique for the assessment of vascular encasement [10]. Traditional direct cholangiography, now replaced by MRCP, is the technique of choice for evaluating the extent of biliary disease, showing stricture, segmental or lobar bile duct dilatation, and filling defects. MRCP, especially if it is included in a complete study of the upper abdomen, with axial T1-weighted and T2-weighted imaging, can allow detection, characterization and staging of the lesion, giving the clinician all the information necessary for adequate treatment planning [11]. In patients selected for major hepatic resection, portal vein embolization, via either the percutaneous transhepatic or the transileocolic route, has been proposed as a useful procedure in pre-operative treatment for patients whose liver remnants will be too small to allow resection. In this way, selective hypertrophy of the healthy portion of the liver can be achieved [12]. CT and MRI are useful tools to depict hepatic segmentation and portal venous anatomy before performing this procedure.
2.2 Hilar Cholangiocarcinoma: Klatskin Tumor
Hilar cholangiocarcinoma accounts for 25% of all cholangiocarcinomas. It arises from the right or left hepatic ducts, and can involve the bifurcation of the common hepatic duct. The middle and distal portions of the common hepatic duct are affected in about 17% and 18% of cases, respectively, while there is diffuse cancerous involvement in about 7% of cases [7]. Since this type of tumor causes localized biliary duct stricture, it is discovered early, usually when it is very small, because of the presence of jaundice or cholangitis. Typical spread occurs by local extension from the biliary tree invading the liver. Perineural invasion and periductal spread, which are frequent in hilar cholangiocarcinoma, are usually underestimated and they represent a cause of treatment failure. Surgery is the only therapeutic option, and the role of diagnostic imaging in this type of tumor is to assess tumor resectability by identifying the level of bile duct obstruction, and the presence or absence of vascular invasion, satellite nodules, intrahepatic tumor spread and lymph node involvement [13].
Criteria for unresectability include the following: evidence of bilateral extension to the segmental branches of the intrahepatic bile ducts; infiltration of the main portal vein of one lobe of the liver, combined with involvement of the hepatic artery of the other lobe; a combination of vascular involvement in one side of the liver with extensive bile duct involvement of the contralateral side; hepatic or nodal metastases [14].
Sonography is usually the initial imaging study in patients with jaundice: it is accurate in visualizing the biliary obstruction at the level of the hepatic hilus, but not equally as effective in demonstrating the obstructing lesion. Overall, sonography detects about 21–45% of these tumors. Although it is difficult to diagnose hilar cholangiocarcinoma with conventional CT because of its small size, spiral or multidetector CT allows more effective evaluation of these small lesions, and better demonstrates the status of the hepatic arterial or portal venous circulation. Although the accuracy of CT in establishing tumor resectability is about 60%, invasion of the intrahepatic bile ducts is usually underestimated in 13% of patients and overestimated in 4% [15].
MRI in combination with MRCP can enable direct visualization of hilar cholangiocarcinoma and determine resectability [14]. The morphology of bile duct stricture detectable on MRCP closely reflects the gross morphological changes occurring along the biliary ductal walls. MRCP can visualize intraluminal tumor extent and characteristics of bile duct stricture. A recent study demonstrated that accuracy of MRCP and endoscopic retrograde cholangiopancreatography (ERCP) in assessing the level and features of bile duct obstruction are similar, while accuracy of MRCP is superior in determining suprahilar tumor extension [14]. Another study comparing the accuracy of MRCP and ERCP in detecting the cause of perihilar biliary obstruction revealed superior sensitivity of MRCP in describing the cause and depicting the anatomical extent of the jaundice, especially in cases associated with tight biliary stenosis and long segmental biliary stricture [16, 17]. MRCP, in contrast to ERCP, can depict bile ducts both proximal and distal to the obstruction. Furthermore, combined use of MRCP and dynamic MRI can display the overall extent of biliary tree involvement, describing vascular and liver parenchyma invasion. Perineural spread, correlated with delayed enhancement along the bile ducts, can also be identified with MRI.
For pre-operative assessment of resectability of hilar cholangiocarcinoma, however, several types of invasive imaging, such as cholangiography and angiography, are sometimes required. Cholangiography, through a retrograde endoscopic or percutaneous transhepatic (PTC) approach, can provide the most accurate anatomical information pertaining to which segmental branches are involved, but it is an invasive technique. For this reason and because of the availability of non-invasive imaging techniques with the same diagnostic accuracy such as MRCP, ERCP and PTC are today considered to be therapeutic tools only. Furthermore, since bile duct visualization in ERCP depends on the duct opacification with injected contrast medium, duct opacification may be limited because of technical demands of duct cannulation and gravitational factors, as occurs when the contrast medium is heavier than the bile and it does not adequately fill the proximal ducts. Previous abdominal surgery, such as hepatojejunostomy or gastrojejunostomy, can be an obstacle for ERCP, but not for MRCP [18].
Differential diagnosis must be made first with other diseases that can cause hilar obstruction indistinguishable from hilar cholangiocarcinoma; these include: metastases to periportal lymph nodes, gallbladder cancer invading the hepatoduodenal ligament, lymphadenopathy due to other inflammation, and idiopathic benign focal stricture of the bile duct (Fig. 5.2).
Hilar lymphoadenomegaly. a At MR cholangiopancreatography, the common hepatic duct is occluded (long arrow) and the intrahepatic bile ducts are markedly dilated; below the common bile duct there is narrowing of the caliber in the middle third (short arrow). b Endoscopic retrograde cholangiopancreatography (ERCP) showing a guide wire that reaches the biliary confluence (dashed arrow), and opacification of extrahepatic bile ducts; the ERCP findings are comparable with those observed at MRCP. c Coronal magnetic resonance (MR) T2-weighted half-Fourier acquisition single-shot turbo-spin-echo (HASTE) section showing the etiology of the occlusion of the common hepatic duct (long arrow) and of the stenosis of the common bile duct (short arrow): a bulky solid mass, hypointense, located in the hilar region, portacaval space and along the hepatoduodenal ligament (arrowheads), surrounding and compressing the extrahepatic bile ducts. d Axial MR T1-weighted section in the venous phase showing the newly formed tissue (arrowheads) appearing as a nodal agglomeration, with inner necrotic areas (asterisks), that includes the portal vein (open arrow), coming into contact with the inferior vena cava without infiltrating it (dashed arrow) and occluding the common hepatic duct (arrow)
According to the Bismuth-Corlette classification, hilar stenosis can be classified in four groups (Fig. 5.3).
-
Type I: tumors involving the common hepatic duct proximal to the primary hepatic confluence (Fig. 5.4).
-
Type II: tumors involving the hepatic duct bifurcation and both hepatic ducts (Fig. 5.5).
-
Type IIIa: tumors involving the right secondary confluence (Fig. 5.6).
-
Type IIIb: tumors involving the left secondary confluence (Fig. 5.7).
-
Type IV: tumors involving both secondary confluences (Fig. 5.8).
Type I Klatskin tumor. Magnetic resonance (MR) imaging on coronal T2-weighted half-Fourier acquisition single-shot turbo-spin-echo (HASTE) (a) and MR cholangiopancreatography (b) showing intrahepatic bile ducts that appear moderately dilated up to the common hepatic duct where an endoluminal formation (arrow, a) is recognizable. Internal-external biliary drainage is shown by the dashed arrow. c, d The framework shown in the MR imaging is completely comparable to endoscopic retrograde cholangiopancreatography shown here, and during which sampling of endoluminal tissue is performed by biopsy forceps at the level of the common hepatic duct (short arrow, d). At 6 months after resection of the common bile duct, cholecystectomy and biliary-jejunal anastomosis, the patient develops jaundice. e During placement of two external-internal biliary drainage tubes for both sides (dashed arrows), the cholangiography examination documents the dilatation of intrahepatic bile ducts in relation to the extensive occlusion of the confluence (arrow). f Axial contrast-enhanced computed tomography section showing heterogeneously hypodense area at the confluence of the bile ducts (arrow) compatible with recurrent disease. The two external-internal biliary drainage tubes are recognizable (dashed arrows)
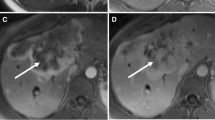
Type II Klatskin tumor. Three-dimensional MR cholangiopancreatography in thinner (a) and thicker section (b) showing the occlusion of the biliary confluence (arrow), which is responsible for the widespread dilatation of the entire biliary tree. Axial contrast-enhanced late phase magnetic resonance (c) and computed tomography (d) sections showing thickening of the walls of biliary confluence responsible for occlusion of the lumen (arrow); the newly formed tissue shows infiltrative growth and accumulation of contrast medium in late phase in both methods. e Cholangiography of the left biliary hemisystem through percutaneous access in paraxiphoid (short arrow) confirming the abrupt, tight stenosis of the confluence (long arrow); the visualization of the bile ducts for the fourth hepatic segment (arrowheads) is needed to assess that the secondary division of the left hepatic duct is not involved by the disease, in planning a right hemi-hepatectomy. f The patient undergoes placement of two internal-external biliary drainage tubes, one for the right posterior-lateral segment (p) and other for the third hepatic segment (s) to reduce jaundice, and prevent cholangitis, while waiting for a surgical procedure
Type IIIA Klatskin tumor. a, b Axial magnetic resonance T1-weighted images showing a hypointense focal liver lesion (arrows) with progressive retention of contrast agent (b). c T2-weighted image showing the neoplasm appearing mildly hyperintense. The lesion has its epicenter in the right hepatic duct, which presents thickened walls with delayed retention of contrast medium (arrowhead, b); glissonian retraction coexists (dashed arrows). d MR cholangiopancreatography in which dilatation of intrahepatic bile ducts is recognized because of stenosis of the primary biliary confluence (arrow). e Axial contrast-enhanced computed tomography (CT) section after intervention of hemi-hepatectomy, showing multiple clips (arrowheads, e, f) recognizable along the shearing of resection. f Axial contrast- enhanced CT section in the same craniocaudal position (as shown in e) 1 year later: some small hypodense hepatic lesions during the portal venous phase (short arrows) have appeared marginally to the shearing of resection, compatible with recurrent disease
Type IIIB Klatskin tumor. a Ultrasound showing a slightly hypoechoic nodule (arrow) recognizable at the biliary confluence, with consequent dilatation upstream of the intrahepatic bile ducts of both hemi-systems (arrowheads). b Contrast-enhanced ultrasound (15 min after injection) showing the lesion (arrow) with no contrast enhancement because of the intravascular nature of the contrast medium. c Post-contrast axial T1-weighted magnetic resonance image showing weak enhancement of bile duct, which appears thickened (short arrow) and in close proximity to the left portal branch (asterisk). d MR cholangiopancreatography showing diffuse dilatation of the entire biliary tree that is abruptly interrupted at the confluence (arrow)
Type IV Klatskin tumor. Axial magnetic resonance imaging (MRI) sections in early (a), venous (c) and delayed (e) contrast-enhanced phase show dilatation of the intrahepatic bile ducts of both lobes because of biliary stenosis at the primary confluence (long arrow), in which we can observe in the venous phase a nodular lesion, with slight enhancement in early phase and increased enhancement during the late phase, which causes a reduction of the left portal branch caliber (short arrow). b MR cholangiopancreatography confirms the dilatation of the intrahepatic biliary tree up to the primary confluence (arrow). Downstream, the size of the common bile duct up to the papilla is regular (arrowheads). d A coronal post-contrast T1-weighted MRI during the portal venous phase shows the newly formed solid tissue (arrow) at the biliary confluence. The palliation of jaundice and cholangitis requires the placement of three external-internal biliary drainage (cholangiography, f): one for the left hemi-system (s), one for posterolateral sectors (p) and one for paramedian sectors (a) of the right hemi-system, indicating a disease extent at second-order biliary bifurcation
2.3 Distal Extrahepatic Cholangiocarcinoma
Extrahepatic cholangiocarcinoma arises between the common bile duct and the ampulla of Vater. In 50–75% of reported cases it occurs in the upper third of the duct, including the hepatic hilum, in 10–30% it occurs in the middle third, and in 10–20% it occurs in the lower third [19].
Because of the site, the tumor usually causes biliary obstruction and jaundice and it manifests early when the mass is small (Fig. 5.9). Bile ducts proximal to the tumor are usually enlarged, while at the level of the tumor they are completely obstructed, and distal to the mass they are of normal diameter. Involvement of the periductal lymphatics, nerves and perineural tissue is frequent.
Cholangiocarcinoma of the terminal common bile duct. Axial contrast-enhanced MR sections in early (a) and late (b) phase in the same craniocaudal position show a late impregnation of endoluminal contrast medium in the prepapillary common bile duct region (arrow). c MR cholangiopancreatography shows a widespread dilatation of the entire biliary tree visible to the level of the terminal common bile duct, which is occluded (arrow). d The findings described in c are completely comparable to those of endoscopic retrograde cholangiopancreatography examination
Because of the difficulty of locating lesions in the early stages of growth, and their poor responses to therapy, extrahepatic cholangiocarcinoma is a challenging pathology in terms of diagnosis, treatment and management.
Since surgical resection of all detectable tumor is the only therapy that improves 5-year survival rate (patients with unresectable cholangiocarcinoma typically die within 6–18 months from the date of diagnosis), the role of diagnostic imaging is extremely important in terms of obtaining tumor-free surgical margins. The major determinants of resectability to consider are: extent of tumor within the biliary tree, vascular invasion, hepatic lobar atrophy and metastatic disease. Hepatic lobe hemiatrophy is usually the result of portal vein involvement or a longstanding biliary obstruction. Involvement of a segment of portal vein shorter than 2 cm can allow tumor resection with vein reconstruction. Otherwise, the presence of lymph node metastases at the N2 level, or at the celiac, periportal or superior mesenteric level, is a contraindication to surgery because it is usually associated with advanced disease [20].
Specifically in the field of diagnostic imaging, no single method that is capable of detecting and accurately localizing cholangiocarcinoma has been introduced, and comprehensive and rigorous approaches using invasive and non-invasive modalities are needed to enable an accurate pre-surgical evaluation of this disease.
Although ultrasonography is the first diagnostic imaging procedure used in cases of extrahepatic cholangiocarcinoma, it can usually detect only common indirect signs of the tumor, such as an abrupt change in ductal diameter with ductal dilatation above it. Contrast-enhanced CT can assess, with good accuracy, the level of obstruction, the vascular involvement, liver atrophy and enlarged lymph nodes, and metastases. It has been demonstrated that CT with axial and coronal images tends to underestimate the longitudinal tumor extent [21]. MRI can evaluate the resectability of biliary duct cancer with more advantages. Furthermore, with MRI it is possible to comprehensively evaluate biliary duct cancer because of the variable tissue contrasts involved. In most cases, cholangiocarcinoma shows low intensity on T2 contrast images because of its rich collagenous fiber content. T1-weighted images are informative when used with fat-saturation pulses and an extracellular contrast agent, such as a gadolinium chelate. A bile duct wall that is thickened by a cholangiocarcinoma shows strong enhancement during the equilibrium phase of MRI. This enhancement may be explained in the same manner as enhancement by an iodinated contrast medium on CT. In addition, MRCP can show the biliary duct lumen, assessing it both upstream of a tumor, where is often dilated, and downstream of the tumor in the same examination [20]. The sensitivity of MRCP in defining stenoses and the level of obstruction has been reported to be in the order of 86–100% [22]. The biliary tree is depicted on both sides of a stricture, thereby defining the stricture length, its proximal extent, and its anatomical relations with other intrahepatic bile ducts. In cases of biliary drainage positioning, MRCP may not be of diagnostic value because of biliary tree collapse; in such cases, if is not possible to defer the drainage, a slow and careful injection of a small amount of saline through the drainage tube (up to 20 ml) is advised. ERCP can provide useful information with regard to the level of obstruction, and can show clearly that an obstruction is arising from a bile duct and does not involve the pancreatic duct. Direct cholangiography sometimes fails to accurately depict the longitudinal spread of a tumor because tumor extensions are often submucosal or extramural.
Tumor resectability often depends on the extent of vascular involvement. Angiography has played a major role in documenting the vascular encasement of the portal vein and hepatic artery; however, the technique is no longer compulsory as a pre-operative examination in cholangiocarcinoma. Recent MRI and CT developments are increasingly replacing this methodology.
Endoscopic ultrasonography (EUS) can depict the mass within the bile duct and the possible disruption of the subserosal fat layer. It is a useful technique for assessing the distal extrahepatic biliary tree, the gallbladder, and even the regional lymph nodes; in fact, the accuracy of EUS is higher in distal cholangiocarcinoma and in non-stented bile ducts, while the sensitivity of EUS for detecting nodal metastasis in cholangiocarcinoma is quite low [23].
When an obstruction of the biliary tree is detected, distinguishing between a malignant and benign nature of the cause of the obstruction can provide a diagnostic clue. In addition to extrahepatic cholangiocarcinoma, malignant strictures include pancreatic head carcinoma, duodenal carcinoma, metastatic lymph nodes, metastases from hepatocellular carcinoma and gastric carcinoma. Benign strictures can be caused by portal cavernoma, iatrogenic cholangitis, post-traumatic cholangitis and Mirizzi syndrome. In a recent study comparing ERCP and MRCP in the differentiation of extrahepatic cholangiocarcinoma from benign stricture, irregular and asymmetric stricture margins were more common in cholangiocarcinoma, and smooth and symmetric stricture margins were more common in the benign stricture, while irregular margins and asymmetric narrowing were seen in both benign and malignant strictures. The frequency of appearance of the „double-duct sign” was not significantly different between cholangiocarcinomas and benign strictures. Sensitivity, specificity and accuracy for the differentiation of malignant from benign causes of biliary stricture at MRCP were 81%, 70% and 76%, respectively, and at ERCP they were 74%, 70% and 72%, respectively [24].
3 Classification of Cholangiocarcinoma According to the Liver Cancer Study Group of Japan
The Liver Cancer Study Group of Japan has proposed a classification for intrahepatic and extrahepatic cholangiocarcinoma based on gross appearance, mode of spread, and biological and clinical behavior. This morphological classification includes: mass-forming, periductal-infiltrating and intraductal-growing cholangiocarcinoma (Fig. 5.10) [25, 26].
Cholangiocarcinoma classification depending on growth pattern. Intrahepatic cholangiocarcinoma involving the medial segmental bile duct of the left lobe (a, mass-forming; b, periductal-infiltrating; c, intraductal-growing). Extrahepatic cholangiocarcinoma (d, mass-forming; e, periductal-infiltrating; f, intraductal-growing)
3.1 Mass-Forming Cholangiocarcinoma
Mass-forming cholangiocarcinoma usually grows as a homogenous, sharply circumscribed mass with well-defined undulating margins (Fig. 5.11). It is frequently characterized by desmoplastic reaction, fibrosis and central coagulative necrosis, while calcifications are rare. The mass can be single or surrounded by multiple small satellite nodules with the same appearance. It is the most common form of intrahepatic cholangiocarcinoma. Dimensions are variable, from few millimeters to larger than 15 cm, but tumors are usually large because they are rarely symptomatic at early stage [27]. It arises from the mucosa and, growing inside the lumen, usually invades the bile duct wall, which becomes narrow and obstructed. Patients with intrahepatic mass-forming cholangiocarcinoma have late symptoms because of obstructive jaundice.
Mass-forming cholangiocarcinoma. On axial T1-weighted magnetic resonance images during the arterial (a) and portal venous (b) phases, a mass-forming lesion is recognizable in the hilar region (arrow) with extension to the caudate lobe that wraps around the inferior vena cava for about 180° (arrowhead). The lesion shows early heterogeneous enhancement of the peripheral region, with delayed retention. c Concomitant expansion of the entire biliary tree upstream because of the confluence occlusion (arrow) is clearly highlighted by MR cholangiopancreatography. The patient undergoes a right portal branch embolization procedure in preparation for a right hemi-hepatectomy intervention for a hypertrophied contralateral liver lobe; final portography (d) and coronal computed tomography (CT) section during the arterial phase (e) show the acrylic glue molds of the right portal branches (dashed arrows). The distal termination of the internal-external biliary drainage (short arrow) and some calcifications of the lesion are recognizable (arrow). The axial CT section during the portal venous phase (f) following right hemi-hepatectomy shows some fluid collections (asterisks), multiple metallic clips (arrowheads) and a normal patent left portal branch (dashed arrow)
Capsular retraction, probably due to a desmoplastic reaction, is described in 21% of cases [28]. Bile ducts are diffusely dilated: moderately around the tumor and severely next to the tumor. Generally, obstruction of the portal vein is not common even though extrinsic compression by the tumor can occur. In 50–67% of cases, the cholangiocarcinoma manifests with extrahepatic spread, and often with lymph node metastasis of the celiac and left gastric areas, or direct invasion of the omentum.
At MRI, the mass appears with variable signal intensity on T2-weighted images and low signal intensity on T1-weighted images. As with CT, after contrast material administration, the mass shows gradual centripetal enhancement on the equilibrium and delayed phases. The areas with greater contrast enhancement are usually at the periphery and correspond to active growth cell areas. Otherwise, as already demonstrated in previous studies, cholangiocarcinomas with marked hypervascularity have a vascular fibrotic stroma. They have a characteristically hyperintense central core on delayed contrastenhanced T1-weighted images. The delayed enhancement pattern is mostly due to the extravascular and extracellular contrast distribution volume of the central part of the tumor and to the slow accumulation of the contrast agent in this part of the tumor by diffusion.
At MRCP, mass-forming cholangiocarcinoma usually presents with focal strictures and sometimes irregular dilatation of the bile ducts. When intrahepatic, the tumor spreads between hepatocyte plates, and expands via the hepatic sinusoidal spaces invading the bile duct walls. A larger mass is formed from the fusion of adjacent satellites together with the primary mass. When extrahepatic, the tumor grows intraluminally from the mucosa of the bile ducts, invading the serosa and therefore causing obstructive jaundice. For this reason, mass-forming cholangiocarcinoma is more often symptomatic at earlier stages of the disease [25].
Differential diagnosis must be made with hepatocellular carcinoma with cirrhotic stroma, sclerosing hepatocarcinoma, combined hepatocarcinoma-cholangiocarcinoma and metastasis from an extrahepatic tumor [29].
3.2 Periductal-Infiltrating Cholangiocarcinoma
Periductal-infiltrating cholangiocarcinoma grows along the bile duct without mass formation, and causes a concentric thickening of the wall with elongated, speculated or branch-like appearance.
Most hilar cholangiocarcinomas have this appearance, while they are rarely located inside the liver. The hepatic parenchyma and the hilum are invaded in the latter stage only, when the tumor becomes exophytic. At this stage a focal wall thickening of the bile duct, with secondary dilatation of the proximal bile ducts, is usually observed. At imaging, the ducts appear abnormally dilated or irregularly narrowed because of the periductal thickening (Fig. 5.12). When located at the periphery of the liver, a periductal-infiltrating cholangiocarcinoma is more often a mass-forming type of tumor. The adjacent hepatic artery or portal vein can be encased by a dense fibroblastic reaction. Vascular invasion is not very common, but vessels may be involved by adherence and fibrosis. On the other hand, intrahepatic and extrahepatic bile ducts are often involved.
Periductal-infiltrating cholangiocarcinoma. a The MR cholangiopancreatography image shows mild dilatation of the intrahepatic bile ducts up to the common hepatic duct, which shows a luminal stenosis (arrow). b On the coronal T1-weighted contrast-enhanced magnetic resonance image, the walls of the common hepatic duct are thickened concentrically (arrow), and this results in complete stenosis of the lumen of the bile duct. Axial computed tomography scans, before (c) and after (d) contrast medium administration, confirm the strong enhancement of the newly formed tissue (arrow)
Differential diagnosis must be made with lymphangitic metastasis from an extrahepatic tumor, which is characterized by absence of bile duct dilatation and diffuse involvement of both sides of the liver. Otherwise, confined disease in one segment or lobe, and presence of ductal dilatation, are specific features of a periductal-infiltrating cholangiocarcinoma.
When located at the hilum, the detection of the tumor mass on CT or sonography can be very difficult. The depiction of the right and left hepatic ducts without the confluence is a typical feature of hilar periductal-infiltrating cholangiocarcinoma. When extrahepatic, the cancer is formed by concentric layering of cellular stroma around the neoplastic glands; the bile duct wall is up to 1 cm thick. At MRCP or direct cholangiography, the lumen of the involved segment is string-like or sometimes not visible at all. Spread of periductal-infiltrating cholangiocarcinoma is usually along the bile duct wall, via nerve and perineural tissue of Glisson’s capsule, toward the porta hepatis.
3.3 Intraductal-Growing Cholangiocarcinoma
Intraductal-growing cholangiocarcinoma is a tumor of the bile ducts, with a better prognosis, and is usually limited to the mucosa, invading the bile duct wall in only the later stages of the disease (Fig. 5.13). Its features can be very variable: diffuse ectasia of the bile ducts without a grossly visible papillary mass or a visible extrinsic mass; intraductal polypoid mass within localized ductal dilatation; intraductal cast-like lesions within a mildly dilated duct, or a focal stricture-like lesion with mild proximal ductal dilatation. When microscopic, it can be considered to be a tumor with micropapillary growth, associated with a precursor of cholangiocarcinoma (Bi1IN, which is the first, low-grade step of a multistep carcinogenesis) [30]. The first type that has been described consists of a diffuse dilatation with multifocal superficial spreading papillary or plaque-like masses, usually isoattenuating with the liver at pre-contrast CT or MRI, and with enhancement after contrast administration, and an intact bile duct wall. If any mass is visible inside the bile duct, it can be caused by the micropapillary nature of the tumor or the limited spatial resolution of the imaging technique. The second type that has been described is a mass located inside the bile duct, with or without ductal dilatation, and which is different from a mass-like stone because there is enhancement after contrast administration, although the presence of associated hepatolithiasis can be demonstrated. The most frequent intraductal-growing cholangiocarcinomas are papillary adenocarcinomas, which are usually small, sessile or polypoid.
Intraductal cholangiocarcinoma of the common bile duct. MR cholangiopancreatography (a) and endoscopic retrograde cholangiopancreatography (b) images show a filling defect within the lumen of the bile duct (arrowheads) extending from the primary biliary confluence to the intrapancreatic segment; moderate dilatation of the biliary tree coexists. Axial computed tomography sections, before contrast administration (c) and during the portal venous phase of the dynamic study (d), at the same craniocaudal level show an endoluminal impregnation of contrast medium in the common bile duct (arrow), compatible with intraductal vegetation. e, f At endosonography, the prepapillary region of common bile duct is identifiable, within which, a little further upstream, newly formed solid tissue is recognizable (asterisk)
When multiple lesions are present, papillomatosis or papillary carcinomatosis must be suspected. Often, these types of tumor have low-grade dysplasia, are confined within the bile duct, and invade the wall in the late phases only. Dilatation of bile ducts is caused by tumor obstruction, sloughed tumor debris or an excessive amount of mucin, such as in the papillary mucinous tumor that is a common variant (Fig. 5.14). The intraductal papillary mucinous tumor of the bile duct is characterized by production of large amounts of mucin that can protrude from the duodenal papilla at endoscopy and cause dilatation of both proximal and distal bile ducts because of the possible obstruction of the papilla of Vater. The viscous nature of the mucin can impede the flow of bile, causing segmental to entire biliary tree dilatation, which sometimes appears as aneurysms or cysts. At MRCP or direct cholangiography, the tumor and the irregularity of the bile duct wall can be seen. The spread of this type of tumor is usually confined to the mucosal layer, without invasion of the submucosal layer. Sometimes the differential diagnosis between intraductal-growing cholangiocarcinoma and mass-like cholangiocarcinoma can be difficult because both can manifest as a single or multiple intraductal filling defect and bile duct dilatation. As recently demonstrated by Kim et al., MRI with MRCP can help at differential diagnosis [31]. In intraductal-growing cholangiocarcinoma, the shape is of one or multiple small and papillary lesions, the caliber of the tumorbearing segment is dilated or normal, there is dilatation of both the proximal and the distal bile ducts, there is no thickening of the bile duct adjacent to the tumor, and there is no significant enhancement after contrast administration [31]. In contrast, mass-forming cholangiocarcinoma shows wall thickening, it is a single lesion, the tumor-bearing segment is usually narrowed, the bile duct dilatation is located at the proximal bile duct only, and there is enhancement after contrast administration. The differential diagnosis is important because of the different growth patterns and the need to choose a different pre-operative work-up protocol.
4 Papillary Tumors of the Bile Ducts
Papillary tumors of the bile ducts have a good prognosis, and they are being detected with an increasing incidence as a result of the higher sensitivity of radiological imaging.
They are a distinctive entity of intraductalgrowing cholangiocarcinoma, characterized by the presence of innumerable minute, frondlike papillary projections. Papillary lesions are usually small, sessile or polypoid. The lesion can be an intraductal papillary adenocarcinoma, adenoma or dysplasia, or a coexistence of all three (Fig. 5.15).
Cholangiocarcinoma arising from intraductal papillomatosis of the common bile duct. The MR cholangiopancreatography (a) and axial T2-weighted half-Fourier acquisition single-shot turbo-spin-echo (HASTE) (b) images show diffuse dilatation of the intrahepatic bile ducts, and a common bile duct that presents multiple intraluminal defects (arrows) stacked along its course, to beyond the confluence. In the head and tail of the pancreas (a) some cystic lesions (arrowheads) compatible with small intraductal papillary mucinous neoplasms of the secondary ducts are recognizable. On pre-contrast axial computed tomography scan (c) and post-contrast scan during the portal venous phase (d), suspicion of a biliary stone is excluded by the clear enhancement of the intraluminal structures with contrast medium at the level of the confluence (arrow). e Endoscopic retrograde cholangiopancreatography confirms the presence of multiple mural nodules (arrows) along the common bile duct walls. Some metallic clips adjacent to the confluence from previous cholecystectomy (short arrow) are depicted. f The surgical specimen confirms the presence of multiple vegetations of mucosa with papillary morphology and foci of cholangiocarcinoma
The tumor itself, and its debris or the amount of mucin produced by it, can cause partial or complete biliary obstruction, which is usually the first symptom at onset of the disease.
Dilatation of the bile ducts is often associated with the tumor, and it may be lobar, segmental, generalized or cystic, depending on the location of the tumor [32]. When the tumor forms a unique cyst, it can resemble biliary cystadenoma or cystadenocarcinoma; differential diagnosis can made through the identification of the communication of the cyst with a bile duct.
Dilatation of the involved segment of the bile ducts, from mild to severe when tumor spread is wider, is usually depicted at US, CT or MRCP. At US, there is an echogenic intraductal mass that fills the bile ducts, without acoustic shadow (differential diagnosis with bile stones). As reported by Lim et al. papillary tumors can be differentiated from bile duct stones by the presence of a non-shadowing intraductal echogenic cast at US, an intraductal non-calcified soft-tissue mass with asymmetric wall thickening at CT, an intraductal mass with a papillary surface, and a serrated bile duct margin at cholangiography [33]. An intraductal mass can be seen on CT, but it can be enhanced if the tumor is fixed to the duct wall. A segmental asymmetric thickening of the bile duct wall, with enhancement, can also be depicted. At ERCP, direct cholangiography or MRCP, single or multiple nodular filling defects of variable size can be detected. Because of the inner friability of this kind of tumor, it may slough spontaneously, and float inside the bile ducts simulating bile duct stone disease.
Occasionally papillary tumors of the bile ducts can produce a large amount of mucin (intraductal papillary mucinous tumors of the bile ducts), thus hindering the flow of bile and leading to obstructive jaundice. At endoscopy, and similar to intraductal papillary tumors of the pancreas, mucin plugs from the duodenal papilla can be of diagnostic value. Because of the possible obstruction of duodenal papilla from the mucin plugs, bile ducts both proximal and distal to the tumor are usually dilated. MRCP can allow rapid visualization of a dilated bile duct, therefore depicting the small intraductal papillary tumors that are masked by mucin but, because mucin and bile have the same magnetic resonance signal intensity, magnetic resonance cannot distinguish between them. However, direct cholangiography can visualize the movable mucin as an amorphous filling defect within the bile duct, and it moves slowly because of the contrast injection pressure. For these reasons, direct cholangiography is the most accurate method for detecting intraductal mucin, although CT or MRI shows higher sensitivity for detecting the tumor mass [34].
Otherwise, when tumors are of large size they can spontaneously slough and float within the bile duct, outside the duodenal papilla, and then disappear clinically and radiologically (Laputa tumor) [32].
Sometimes, the tumors form a unique cystic mass resembling biliary cystadenoma or cystadenocarcinoma.
5 Differential Diagnosis
Since cholangiocarcinoma can show many different features with variable growth pattern, there is a large heterogeneous group of diseases, including benign and malignant entities, that can mimic it.
It is essential to differentiate these other entities from cholangiocarcinoma by using imaging features that enable the clinician to decide on the best therapeutic strategy for the patient. Recently, a study of a large surgical series demonstrated that in 24% of patients undergoing surgery for presumed cholangiocarcinoma, a benign disease was found [35]. MRCP can be a fundamental tool to characterize benign and malignant neoplasms of the biliary tree, and to differentiate them from the cholangiocarcinoma.
5.1 Benign Diseases
5.1.1 Primary Sclerosing Cholangitis
Primary sclerosing cholangitis is a chronic cholestatic disease, of idiopathic autoimmune origin, characterized by diffuse inflammation and progressive fibrosis of the intrahepatic and extrahepatic bile ducts. It usually occurs in males in the fourth or fifth decade of life, and, because of the autoimmune origin, can be associated with inflammatory bowel disease, such as ulcerative colitis [36].
The chronic inflammation of bile ducts increases the incidence of cholangiocarcinoma; indeed cholangiocarcinoma develops in 10% of patients with primary sclerosing cholangitis, with the highest incidence in the first 2 years after onset of primary sclerosing cholangitis. In the majority of cases, the cholangitis involves both small and large ducts, while the involvement of only one type of duct is rare.
MRCP has high sensitivity for imaging the smallest of ducts and it can usually detect multifocal strictures, segmental ectasias, and ductal wall thickening with irregular beading of intrahepatic and extrahepatic bile ducts. Sometimes, when primary sclerosing cholangitis manifests only as a focal short bile duct stricture, it can be difficult to distinguish it from a periductal-infiltrating type of cholangiocarcinoma [37] (Fig. 5.16).
Sclerosing cholangitis. a Using MR cholangiopancreatography, the intrahepatic biliary tree presents some segmental dilatation of the more peripheral ducts (short arrow), while the bile ducts close to the hilum tend to be of small caliber and are partially not recognizable (arrow). The caliber of the common bile duct is within normal limits, in relation to previous cholecystectomy (open arrow). b On axial contrast-enhanced T1-weighted magnetic resonance imaging, obtained during the portal venous phase, ductal wall thickening is not recognizable at the primary biliary confluence (arrow). c, d The coronal contrast-enhanced T1-weighted magnetic resonance images taken during the delayed phase (20 min after the injection of hepatospecific contrast medium) show regular passage of contrast medium in the intrahepatic and extrahepatic tree (dashed arrows)
Moreover, a cholangiocarcinoma can occur as a complication of primary sclerosing cholangitis, and it must be suspected when there is a focal mass greater than 4 mm diameter, progressive dilatation of the bile duct, thickening of bile duct wall or a dominant ductal stricture [38].
5.1.2 Adenoma
Intraductal tubular adenomas are rare biliary neoplasms composed of glands resembling pyloric glands, with minimal cytological atypia. They are usually located in the intrapancreatic part of the common bile duct. This type of tumor usually produces a small mass within the bile ducts, and is difficult to differentiate from a mass-forming cholangiocarcinoma [19, 39].
The tumor has been reported to be rare and currently is categorized as a benign counterpart of papillary adenocarcinoma.
5.1.3 Mucinous Cystic Neoplasm
Hepatic mucinous cystic neoplasms are cystforming epithelial neoplasms, usually without communication with the bile ducts, and they are composed of cuboidal to columnar, variably mucin-producing epithelium, and associated with ovarian-type subepithelial stroma (Fig. 5.17). Of the cystic neoplasms of the liver, biliary cystic adenoma and cystic adenocarcinoma are the most frequent lesions. The main differential diagnosis has to be made with intraductal papillary cholangiocarcinoma. In a recent study by Zen et al. that compared these two neoplasms, mucinous cystic neoplasms were larger and they showed multilocular cysts with septation or a cyst-in-cyst appearance, while intraductal papillary neoplasms were smaller, multicystic with a grapelike appearance, and they all presented papillary mural nodules [40]. Even more rarely, biliary cystadenoma can be extrahepatic causing obstructive jaundice and recurrent cholangitis [41].
Biliary cystadenoma. a At MR cholangiopancreatography, a cystic lesion is recognizable in the left hepatic lobe (arrow). It is mildly hyperintense, and probably due to a high protein content. The lesion is responsible for segmental dilatation of some upstream peripheral bile ducts (arrowheads). b On axial fat-suppressed T1-weighted magnetic resonance imaging (MRI), the mass (arrow) is localized in the fourth liver segment and appears hyperintense (paramagnetic effect) because of its high protein content. c The axial T2-weighted MRI confirms the cystic nature of the lesion (long arrow); an internal septum (short arrows) is responsible for the bi-lobed pattern of the lesion. d The lesion walls and the septum (short arrow) appear to show contrast enhancement on the this axial contrast-enhanced T1-weighted MRI
5.2 Malignant Diseases
5.2.1 Malignant Diseases
Intrabiliary metastases are rare, and tumors that metastasize to the bile ducts include primary cancers of the lung, breast, gallbladder, colon, testicle, prostate and pancreas, and also melanoma and lymphoma (Fig. 5.18). Of these cancers, adenocarcinoma of the colon shows a high propensity to spread along the epithelial surfaces, thus involving the biliary ducts.
Liver metastases from pancreatic ductal adenocarcinoma. On axial T1-weighted magnetic resonance image (MRI) during arterial (a) and portal venous (b) phases, an area (arrow in a, b) with slight and inhomogeneous enhancement in the early phase, and with a tendency to peripheral retention of contrast medium in the later phase, is highlighted at the biliary confluence; a dilation of the entire biliary tree is present upstream (arrowheads). c Cholangiography examination confirms the dilatation of the intrahepatic bile ducts of both lobes, with abrupt interruption at the level of primary confluence (arrow). d The patient underwent placement of two biliary stents: one for the left lobe (s) and one for the posterolateral sectors (p) of the right lobe. e At MR cholangiopancreatography, the stenosis of the biliary confluence (arrow) is visible, with normal caliber of the downstream common bile duct (arrowheads). f An axial contrast-enhanced T1-weighted MRI, obtained on a plane slightly more caudal than a and b, shows a solid hypointense neoplasm of the pancreatic tail (open arrow) with multiple hepatic repetitions (dashed arrows), one of which, in a more cranial plane, is responsible for occlusion of the biliary confluence
Liver metastases with intrabiliary duct growth may mimic all three growth patterns of cholangiocarcinoma. Since there are actually no imaging features peculiar to either one of the two diseases, diagnosis is based mainly on clinical history and histological findings.
The presence of a pathological precursor of cholangiocarcinoma, such as clonorchiasis, recurrent pyogenic cholangitis or primary sclerosing cholangitis, can suggest diagnosis of tumor of the bile ducts. Also, some bulky metastatic tumors with a central necrotic area occasionally mimic exophytic peripheral cholangiocarcinoma.
5.2.2 Hepatocellular Carcinoma
Some subtypes of hepatocellular carcinoma rich in fibrous stroma, including fibrolamellar and sclerosing heapatocellular carcinoma, can mimic cholangiocarcinoma features, showing hypervascularity and prolonged enhancement. Even hepatocellular carcinoma rarely invades and grows within bile ducts, and when it presents with intrabiliary growth it forms a burden of soft-tissue masses causing dilatation of the bile ducts. For this reason MRCP is not very useful for the differential diagnosis with cholangiocarcinoma.
A combination of hepatocellular carcinoma and cholangiocarcinoma is commonly called cholangiohepatocellular carcinoma and it contains neoplastic cells from both entities. The subtypes of cholangiohepatocellular carcinoma described so far are: double cancer or collision tumor, which is composed of two separate masses of the two different carcinomas; combined type or transitional tumor, which is formed by contiguous masses of independent elements of the two carcinomas; mixed type or fibrolamellar tumor, which is made up of two masses, with an intimate mingling of the two entities.
However, since hepatocellular carcinoma is the most common cancer growing in cirrhotic liver, when dealing with a patient with positive serological results for hepatitis B or C and high serum levels of α-fetoprotein, a diagnosis of hepatocellular carcinoma should be suggested first.
5.2.3 Biliary Tract Melanoma
Biliary tract melanoma can be a primary lesion or a metastasis from a primary location outside the liver. It usually presents as an intraluminal polypoid soft-tissue mass, thus simulating an intraductal-growing cholangiocarcinoma. At MR, the polypoid mass, because of the melanin content, presents high signal intensity on T1-weighted images and low signal intensity on T2- weighted images.
5.2.4 Lymphoma of the Bile Ducts
Lymphomatous involvement of the biliary system is a rare, usually secondary, manifestation of systemic disease. Biliary strictures caused by a soft-tissue mass are usually seen in patients who have systemic symptoms.
5.2.5 Leukemic Involvement of the Bile Ducts
It has been reported that acute myelogenous leukemia can mimic periductal-infiltrating cholangiocarcinoma with biliary strictures. Even chloroma can involve the extrahepatic biliary ducts, appearing as a soft-tissue mass in the bile ducts.
Acknowledgements The authors thank Alma Olivieri and Matteo de Iorio for their help in preparing the manuscript.
References
Blechacz B, Komuta M, Roskams T, Gores GJ (2011) Clinical diagnosis and staging of cholangiocarcinoma. Nat Rev Gastroenterol Hepatol 8:512–522
Lim JH (2003) Cholangiocarcinoma: morphologic classification according to growth pattern and imaging findings. AJR Am J Roentgenol 181:819–827
Clemett AR (1985) Carcinoma of the major bile ducts. Radiology 84:894–903
Alexander F, Rossi RL, O’Bryan M (1984) Biliary carcinoma: a review of 109 cases. Am J Surg 147:503–509
Nesbit GM, Johnson CD, James EM et al (1998) Cholangiocarcinoma: diagnosis and evaluation of resectability by CT and sonography as procedures complementary to cholangiography. AJR Am J Roentgenol 151:933–938
Edmondson HA (1958) Tumors of the liver and intrahepatic bile ducts: atlas of tumor pathology. Washington, DC: Armed Forces Institute of Pathology
Choi BI, Lee JM, Han JK (2004) Imaging of intrahepatic and hilar cholangiocarcinoma. Abdom Imaging 29:548–557
Han JK, Lee JM (2004) Intrahepatic intraductal cholangiocarcinoma. Abdom Imaging 29:558–564
Choi SB, Kim KS, Choi JY et al (2009) The prognosis and survival outcome of intrahepatic cholangiocarcinoma following surgical resection: association of lymph node metastasis and lymph node dissection with survival. Ann Surg Oncol 163048–3056
Vilgrain V (2008) Staging cholangiocarcinoma by imaging studies. HPB (Oxford) 10:106–109
Pavone P, Laghi A, Passariello R (1999) MR cholangiopancreatography in malignant biliary obstruction. Semin Ultrasound CT MR 20:317–323
Madoff DC, Hicks ME, Vauthey JN et al (2002) Transhepatic portal vein embolization: anatomy, indications, and technical considerations. Radiographics 22:1063–1076
Masselli G, Manfredi R, Vecchioli A, Gualdi G (2008) MR imaging and MR cholangiopancreatography in the preoperative evaluation of hilar cholangiocarcinoma: correlation with surgical and pathologic findings. Eur Radiol 18:2213–2221
Manfredi R, Masselli G, Maresca G et al (2003) MR imaging and MRCP of hilar cholangiocarcinoma. Abdom Imaging 28:319–325
Lee HY, Kim SH, Lee JM et al (2006) Preoperative assessment of respectability of hepatic hilar cholangiocarcinoma: combined CT and cholangiography with revised criteria. Radiology 239:113–121
Yeh TS, Jan YY, Tseng JH (2000) Malignant perihilar biliary obstruction: magnetic resonance cholangiopancreatography findings. Am J Gastroenterol 95:432–440
Stroszczynski C, Hunerbein M (2005) Malignant biliary obstruction: value of imaging findings. Abdom Imaging 30:314–323
Vogl TJ, Schwarz WO, Heller M, Herzog C (2006) Staging of Klatskin tumours (hilar cholangiocarcinomas): comparison of MR cholangiography, MR imaging, and endoscopic retrograde cholangiography. Eur Radiol 16:2317–2325
Lim JH, Lee WJ, Takehara Y, Lim HK (2004) Imaging of extrahepatic cholangiocarcinoma. Abdom Imaging 29:565–571
Takehara Y (2004) Preoperative assessment of extrahepatic cholangiocarcinoma with imaging. Abdom Imaging 29:572–580
Seo H, Lee JM, Kim IH et al (2009) Evaluation of the gross type and longitudinal extent of extrahepatic cholangiocarcinomas on contrast-enhanced multidetector row computed tomography. J Comput Assist Tomography 33:376–382
Adamek HE, Albert J, Weitz M (1998) A prospective evaluation of magnetic resonance cholangiopancreatography in patients with suspected bile duct obstruction. Gut 43:680–683
Mohamadnejad M, DeWitt JM, Sherman S et al (2011) Role of EUS for preoperative evaluation of cholangiocarcinoma: a large single-center experience. Gastrointest Endosc 73:71–78
Park MS, Kim TK, Kim KW et al (2004) Differentiation of extrahepatic bile duct cholangiocarcinoma from benign stricture: findings at MRCP versus ERCP. Radiology 233:234–240
Liver Cancer Study Group of Japan (2000) The general rules for the clinical and pathological study of primary liver cancer, 4th edn. Tokyo: Kanehara
Lim JH (2003) Cholangiocarcinoma: morphologic classification according to growth pattern and imaging findings. AJR Am J Roentgenol. 181: 819–827
Lim JH, Park CK (2004) Pathology of cholangiocarcinoma. Abdom Imaging 29:540–547
Kim TK, Choi BI, Han JK (1997) Peripheral cholangiocarcinoma of the liver: two-phase helical CT findings. Radiology 204:539–543
Lee WJ, Lim HK, Jang KM (2001) Radiologic spectrum of cholangiocarcinoma: emphasis on unusual manifestations and differential diagnosis. Radiographics 21:S97–116
Zen Y, Adsay NV, Bardadin K (2007) Biliary intraepithelial neoplasia: an international interobserver agreement study and proposal for diagnostic criteria. Mod Pathol 20:701–709
Kim JE, Lee JM, Kim SH et al (2010) Differentiation of intraductal growing-type cholangiocarcinomas from nodular-type cholangiocarcinomas at biliary MR imaging with MR cholangiography. Radiology 257:364–372
Lim JH, Chin AY, Lim HK et al (2002) Radiological spectrum of intraductal papillary tumors of the bile ducts. Korean J Radiol 3:57–63
Lim JH, Kim MH, Kim TK et al (2003) Papillary neoplasms of the bile duct that mimic biliary stone disease. Radiographics 23:447–455
Han JK, Lee JM (2004) Intrahepatic intraductal cholangiocarcinoma. Abdom Imaging 29:558–564
Clayton RA, Clarke DL, Currie6EJ et al (2003) Incidence of benign pathology in patients undergoing hepatic resection for suspected malignancy. Surgeon 1:32–38
Elsayes KM, Oliveira EP, Narra6VR et al (2006) MR and MRCP in the evaluation of primary sclerosing cholangitis: current applications and imaging findings. J Comput Assist Tomogr 30:398–404
Vitellas KM, Keogan MT, Freed KS et al (2000) Radiologic manifestations of sclerosing cholangitis with emphasis on MR cholangiopancreatography. Radiographics 20:959–975
Lee WJ, Lim HK, Jang KM et al (2001) Radiologic spectrum of cholangiocarcinoma: emphasis on unusual manifestations and differential diagnoses. Radiographics 21:S97–S116
Sato Y, Osaka H, Harada6K et al (2010) Intraductal tubular neoplasm of the common bile duct. Pathol Int 60:516–519
Zen Y, Pedica F, Patcha VR et al (2011) Mucinous cystic neoplasms of the liver: a clinicopathological study and comparison with intraductal papillary neoplasms of the bile duct. Mod Pathol 24:1079–1089
Ray S, Khamrui S, Mridha AR, Mukherjee B (2010) Extrahepatic biliary cystadenoma: an unusual cause of recurrent cholangitis. Am J Surg 199:e3–e4
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2013 Springer-Verlag Italia
About this chapter
Cite this chapter
Manfredi, R., Contro, A., Ambrosetti, M.C., Alfonsi, U., Di Paola, V., Mucelli, R.P. (2013). Neoplasms of the Biliary Tree. In: Magnetic Resonance Cholangiopancreatography (MRCP). Springer, Milano. https://doi.org/10.1007/978-88-470-2844-9_5
Download citation
DOI: https://doi.org/10.1007/978-88-470-2844-9_5
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-2843-2
Online ISBN: 978-88-470-2844-9
eBook Packages: MedicineMedicine (R0)