Abstract
There is no question that when a youngster develops bipolar disorder, it can severely affect the normal development and psychosocial functioning of the child or adolescent and significantly increase the risk for suicide, substance abuse, academic, social and legal problems. Despite the diagnostic criteria being so well delineated, there has been much debate and interest in how bipolar disorder presents in pediatric populations, how professionals assess and diagnosis bipolar disorder in children and adolescents, and how this impacts treatment. This chapter will aim to not only discuss the epidemiology, risk and genetic factors, assessment and treatment of bipolar disorder in children and adolescents but also highlight recent trends, advancements, and research to better understand pediatric bipolar disorder.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Case Example
Billy is a 15-year-old adopted male with a history of attention deficit hyperactivity disorder and learning disorder who presents with a decline in functioning in school setting. Billy has always been a good-natured, well-mannered young teenager who was kind and thoughtful. Billy struggled with his social interactions and appeared to be slightly more immature than his same age peers. When Billy entered high school, although he was ready for this new educational milestone he struggled from the start in his large high school setting. Billy’s mood appeared depressed and he was withdrawn and isolative at times. With the support of his individualized educational plan (IEP), Billy was able to do the work, but he had significant difficulty with his decision-making strategies and navigating social constructs. Billy began to follow negative behaviors of his peers. The peers with whom he was spending time had conflict with another group at school to the point that they began to be verbally aggressive and even threatened physical harm to Billy and his associates. Thus out of fear, Billy brought a knife to school for protection. A female peer noticed it in his backpack and notified school officials and Billy was subsequently placed in an alternative school setting. After a month of settling into his new school placement, more incidents began to occur. Billy began to leave home for long periods of time. He was supposed to take out the trash but would be gone for 2 h. His mother would drop him off at school but then he would wander off school grounds and be marked absent for the day. Billy even was detained shortly for shoplifting after he was “dared” by his peers to steal some speakers from a store. Other electronics would appear in his possession over time, which he would explain as either someone gave them to him or he bought them off of another person. Billy stated that he was able to purchase these electronics with his own money from the “candy business” he had recently started. Billy denied rapid thoughts, disturbed sleep, and pressured speech but during this time felt that he had unique skateboarding techniques that no one else could do. He also felt that he could teach the lessons in school better than his teachers. He felt a thrill of adrenaline when he was dared to do something and did it even though he knew it was wrong “I felt good. I felt powerful.” He also felt that if anyone tried to take his possessions he would fight them and protect himself. As mentioned previously, Billy was adopted but when family history was further explored it was discovered that his biological father with whom he has no contact has a history of bipolar disorder. One night Billy left his home for 24 h. When he finally came back home he was taken to the emergency department for assessment and was subsequently hospitalized. Billy was started on a low dose atypical antipsychotic medication and the hypomanic/manic symptoms began to remit.
2 Introduction
There has been much debate and interest on how bipolar disorder presents in pediatric populations, how professionals assess and diagnosis bipolar disorder in children and adolescents, and how this impacts treatment. There is no question that when bipolar disorder strikes, it can severely affect the normal development and psychosocial functioning of the child or adolescent and significantly increase the risk for suicide, substance abuse, academic, social, and legal problems.
The diagnostic criteria for bipolar disorder is quite clear in the Diagnostic Statistical Manual of Mental Disorders—DSM-5 (American Psychiatric Association 2013). The one critical manic episode upon which this diagnosis is paramount requires that there is a distinct period of abnormally and persistently elevated, expansive, or irritable mood lasting at least 1 week (4 days for hypomania) and be present most of the day, nearly every day. It also requires a distinct period of abnormally and persistently increased goal-directed activity or energy, lasting at least 1 week (4 days for hypomania) and be present most of the day, nearly every day. In addition, there must be the presence of at least 3 (4 if the mood is only irritable) symptoms that include grandiosity, decreased need for sleep, pressured speech, racing thoughts, distractibility, psychomotor agitation or increased goal-directed activity, and involvement in high-risk activities (American Psychiatric Association 2013). Despite the diagnostic criteria being well delineated, much interest has gone into how bipolar disorder presents in pediatric populations, as the DSM criteria do not differentiate between how these symptoms might manifest in children compared to adults. This chapter will aim to not only discuss the epidemiology, risk and genetic factors, assessment and treatment of bipolar disorder in children and adolescents but also highlight recent trends, advancements, and research to better understand pediatric bipolar disorder.
3 Epidemiology
Multiple prevalence studies have been done to try to examine rates of bipolar disorder in pediatric populations, although most of the literature examines adolescent populations and not pre-pubertal children. The prevalence of pediatric bipolar disorder is approximately 1.8 % (Van Meter et al. 2011). This finding is further supported by the fact that approximately 60 % of adults with bipolar disorder had the onset of their symptoms prior to age 20 (Birmaher 2013). Prevalence rates can be as high as 5–6 % in subsyndromal pediatric bipolar disorder. Subsyndromal bipolar disorder is characterized by a distinct period of abnormal or persistently elevated, expansive, or irritable mood plus one or more symptoms of mania; but not meeting full criteria for bipolar disorder (Lewinsohn et al. 2000). Interestingly, being categorized as having subsyndromal bipolar disorder in adolescence was more greatly associated with developing a major depressive episode in young adulthood compared to meeting criteria for bipolar disorder in young adulthood. Further, having diagnoses of bipolar disorder or subsyndromal bipolar disorder was associated with greater psychosocial impairment, poorer global functioning, and being more likely to utilize mental health care as adults. Billy appears to fall into either one of these diagnostic categories.
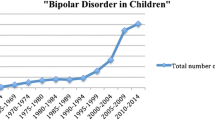
Recent studies in the United States show a trend of increasing rates of diagnosis of bipolar disorder in pediatric populations. One study showed that in outpatient office-based settings, the number of youth with a diagnosis of bipolar disorder increased 40-fold during these time periods (1994–1995 and 2002–2003 survey data), while only increasing twofold in the adult populations (Moreno et al. 2007).
To further the importance of recognizing that individuals with bipolar disorder may start to have onset of symptoms in childhood, another study looked at adults with a diagnosis of bipolar disorder and used self reports to group them into three categories: those with the symptom onset in childhood (<13 years of age), adolescent onset(13–18 years), and adult onset. Individuals that had child onset bipolar disorder were more likely to have experienced more prolonged manic episodes, non-remitting courses (<2 months without symptoms) and greater risk of having diagnosis of antisocial personality disorder in adulthood. Childhood and adolescent onset type also had higher prevalence of substance use disorders (Goldstein and Levitt 2006).
4 Risk Factors
Research has looked into what factors may predispose children to develop bipolar disorder in their lifetime. The best established early marker of bipolar disorder risk remains family history. This factor has ben widely accepted in clinical practice, despite the fact that the majority of the high-risk offspring of individuals with mood disorders do not develop bipolar disorder in particular. However, a large proportion of offspring develop other mental disorders (Paaren et al. 2014). A meta-analysis of offspring studies where at least one parent has a diagnosis of bipolar disorder showed that 52 % of their offspring had a mental disorder in childhood compared to 29 % of offspring of parents with no mental disorder diagnosis. Those offsprings of a parent with bipolar disorder were four times more likely to develop a mood disorder, including bipolar disorder (DelBello and Geller 2001). A more recent longitudinal study that looked at 129 offspring (aged 16–26-years old) that had at least one parent with a diagnosis of bipolar disorder over a 5 year period found that there was an increase in diagnosis of bipolar disorder in the offspring from 3 to 10 % over the 5 year period. Prevalence rates of any psychiatric disorder increased from 44 to 59 %, showing that a positive family history of bipolar disorder is a risk factor for developing bipolar disorder and should be taken into consideration in evaluations of children (Hillegers et al. 2005). Another study that examined potential biological risk factors for development of pediatric bipolar disorder found rates of positive family history of a bipolar disorder diagnosis in first-degree relatives to be significantly higher in children diagnosed with bipolar I disorder. It also found there to be a positive association with the presence and number of perinatal risk factors, such as in utero medication exposure prescribed for medical reasons, illegal drug use during pregnancy or birth complications, and children diagnosed with bipolar disorder; suggesting family history and perinatal risk factors as potential risk factors for bipolar disorder in children (Pavuluri et al. 2006).
From the case example, there could much debate on whether Billy’s clinical presentation was classic bipolar disorder or a subsyndromal type. The most compelling element that favors a bipolar process is Billy’s first-degree family history of bipolar disorder.
Family studies show potential genetic and environmental links to the development of pediatric bipolar disorder. Strober et al. showed increased rates of bipolar disorder and major depressive disorder in first-degree relatives of bipolar disorder patients. Interestingly, they found an even higher prevalence of bipolar disorder in first-degree relatives of pediatric bipolar disorder patients, compared to adult onset cases (29.4 % vs. 7.4 %) (Strober et al. 1988). Another study showed that relatives of bipolar disorder patients that had onset before the age of 21 years of age were twice as likely to have bipolar disorder than those patients with onset after the age of 21 (Neuman et al. 1997). Twin studies to better understand the genetic heritability of bipolar disorder has primarily been on adult onset cases, but one study looked at pediatric twins using data from the Child Behavior Checklist (CBCL) and identifying cases with potential bipolar disorder through a profile of elevated scores on attention problems, aggressive behavior, and anxious/depressed subscales. This study showed there was a shared genetic and environmental component in the children that met the profile through the CBCL suggestive of pediatric bipolar disorder, but was limited in that the children were not interviewed and assessed to meet DSM criteria for bipolar disorder (Hudziak et al. 2005).
Premorbid psychiatric problems are common in pediatric bipolar disorder. Numerous studies have demonstrated high rates of developing mania in children and adolescents who are experiencing difficulties with disruptive behavior disorders, irritability, depressive, and anxiety symptoms. Approximately 20 % of children and adolescents with major depression go on to experience manic episodes in adulthood. Factors that predict the eventual development of mania in depressed children and adolescents include: (1) a depressive episode characterized by rapid onset, psychomotor retardation, and psychotic features; (2) a family history of affective disorders, particularly bipolar disorder; and (3) a history of mania or hypomania after treatment with antidepressants (McClellan et al. 2007).
Genetic studies have been an area of interest in better understanding the etiology and potential risk for development of bipolar disorder and a number of potential genes that are implicated in bipolar disorder include COMT (catechol-O-methyltransferase), MAO (monoamine oxidase), the dopamine transporter, and BDNF (brain-derived neurotrophic factor) (Althoff et al. 2005). Genetic studies looking at juvenile bipolar cases have been more limited, but include one small study that showed a polymorphism in the BDNF gene, suggesting that there could be a shared gene in both pediatric and adult onset bipolar disorder cases (Geller et al. 2004).
There is a growing consensus that bipolar disorder can be a progressive disease process in children and adolescents. Neuroscience findings thus far underscore the importance of tracking the progression of the underlying processes from early manifestations of the disease onward. This step is considered necessary to clarify neurophysiology prior to the confounding effects of medication exposure and illness course. Several thought provoking hypotheses have been suggested such as: increase cortical volume might represent failed pruning and white matter abnormalities may exist prior to the illness onset. These alterations in neurodevelopment may lead to affective dysregulation and eventual onset of the first manic episode (Fristad and Algorta 2013).
5 Diagnostic Challenges
Early studies suggested that children with bipolar disorder tend to have presentations that have a mood disturbance characterized by irritability, rather than euphoria; and have a course that is more chronic as opposed to episodic (Wozniak et al. 1995). There has been debate about the presentation of chronic irritability and if this is a true presentation of bipolar disorder in youth versus being a separate diagnostic category altogether, or a presentation of an alternative diagnosis characterized by the non-specific symptom of irritability. This led to the idea of identifying different phenotypes of mania in children for research purposes, which included a narrow phenotype that fits the criteria and definition of discrete hypomanic or manic episodes for the duration of 7 days or more (or 4 days for hypomania); intermediate phenotypes consisting either of the episodes with hallmark symptoms of mania, but lacking the duration criteria or episodes meeting the duration criteria but not meeting enough of the hallmark or “cardinal” symptoms of bipolar disorder; and a broad phenotype consisting of a more chronic course of irritability and hyperarousal that does not meet the discrete episodic nature of the narrow phenotype. Because of the uncertainty at the time of whether the broad phenotype is truly a presentation of bipolar disorder, it was termed ‘severe mood dysregulation’ (SMD) (Leibenluft et al. 2003). Further studies, regarding SMD suggested higher prevalence rates compared to bipolar disorder (3.3 % in a sample of 9–19-year old), and also suggested an association between meeting criteria for SMD in childhood and being diagnosed with a depressive disorder when followed prospectively. Surprisingly, the study did not show an association with meeting criteria for bipolar disorder in the future (Brotman et al. 2006). Other studies include a longitudinal community-based study that examined 776 youth at three different time points (mean ages 13.8–22.1-years old) and found that chronic irritability at the first time point was associated with meeting criteria for ADHD at the second time point and major depressive disorder at the third time point. In contrast, having episodic irritability at the first time point was associated with simple phobias and mania at the second time point. The study also showed that the type of irritability (chronic versus episodic) was likely to be stable when following it through the longitudinal course (Leibenluft et al. 2006). Yet another longitudinal study looked at children who met criteria for SMD followed them over a 2-year period to determine if there was an increased risk of developing the more classic hypomanic or manic presentations of bipolar disorder when compared to children meeting criteria for bipolar disorder. The study found that only 1 out of 84 subjects identified at the start of the study with SMD went on to develop a hypomanic or manic episode during the follow up period, contrasted with a more than 50 times greater probability of developing a hypomanic or manic episode in those children that met criteria for bipolar disorder at the start of the study (Stringaris et al. 2010).
Given that much of the evidence have shown that children presenting with the more chronically irritable phenotype seem to follow a different course than children with the more narrow, classic phenotype of bipolar disorder; a new diagnostic category was created and included in the DSM-5: disruptive mood dysregulation disorder (DMDD), to capture this phenotypic presentation. This was listed under the depressive disorder category and not the bipolar disorder section in the DSM-5. Criteria for DMDD include severe recurrent temper outbursts that are out of proportion to the situation, occurring three or more times/week and our inconsistent with the child’s developmental level; presence of a persistently irritable or angry mood for most of the day nearly every day, presence for greater than 12 months without a 3 month period of absence of the above symptoms, and presence of the above symptoms in 2 out of 3 settings with the level of impairment being severe in at least one setting and at least mild-moderate in the other setting. The diagnosis should not be made for the first time before 6 years of age or after 18 years of age, and the onset be before 10 years of age. The child should not have had a distinct period of more than 1 day where the full criteria (besides duration) of hypomania or mania have been met, the behaviors do not occur exclusively in the context of a major depressive episode and are not better explained by an alternative mental disorder, or are attributable to effects of a substance or a medical condition. Given these recent changes in the diagnostic classifications, clinicians should be attentive in interviewing patient to get a good history of the time course of irritability in addition to the standard symptoms of mania. In addition, clinicians should be attentive to the overlap of some of the DMDD symptoms with ODD, but differentiating the two by the severity of the impairment, presence of severe, frequent outbursts, and presence of persistent mood disturbance in between outbursts. If the child meets both criteria for DMDD and ODD, only the diagnosis of DMDD is given (American Psychiatric Association 2013).
Another significant change in the DSM-5 criteria from DSM-IV for bipolar disorders, was that the “A” criterion now requires the combination of both the period of change in mood (euphoric, expansive, or irritable) and a change of increased goal-directed activity or energy; as opposed to these being two independent criterion. In applying the DSM-5 criterions to children and adolescents, a number of challenges arise: the symptom of irritable mood is commonly found in many other psychiatric disorders that affect children; including anxiety disorders, major depressive disorder, ADHD, developmental disorders, ODD, and PTSD. In particular, a number of symptoms such as increased rate of speech, distractibility, and increased energy can be seen in ADHD as well as bipolar disorder. A comparison study between children with ADHD versus bipolar disorder, showed that rates of irritability, hyperactivity, distractibility, and accelerated speech were similar between groups making their use for differentiating the groups challenging. Symptoms that were shown to be more specific for mania were elated mood, grandiosity, racing thoughts, hypersexuality, and decreased need for sleep that do not overlap with ADHD (Geller et al. 2002). This has led some to believe that elated mood and grandiosity should be considered “cardinal” symptoms of mania, as they appear to be more specific to bipolar disorder.
In terms of common symptoms of mania (not to be confused with the “cardinal” symptoms), (Kowatch et al. 2005) completed a meta-analysis of the phenomenology of bipolar disorder to determine what symptoms were most commonly found in children with bipolar disorder. The most common symptoms were increased energy (89 %), distractibility (84 %), pressured speech (82 %), irritability (81 %), and grandiosity (78 %). Interestingly, hypersexuality, which is one of the more specific symptoms for pediatric bipolar disorder was found to be the least commonly found symptoms (38 %) and psychosis, which does not always accompany manic episodes was found to occur at a rate of 42 % (Kowatch et al. 2005). Care must also be taken to differentiate what types of behaviors in children are developmentally appropriate versus a symptom of mania. Examples include differentiating the elation a child may feel at a party or holiday event versus elation without any clear reason to be; or the roles children may take in imaginative play such as pretending to be a superhero versus behaving in this way outside of the context of play (Geller et al. 2002). Further detailed histories must be taken to help differentiate other potential causes for what is seen as irritability, such as a major depressive episode; or what is perceived to be racing thoughts, which may actually be a manifestation of frequent ruminations and worries—as seen in a patient with an anxiety disorder.
In Billy’s clinical presentation the main diagnostic challenge is discerning which part of his clinical presentation is secondary to normal adolescence in which Billy is attempting to develop his sense of self and self-identity and be autonomous and independent with his new found freedom and expansion of social network in his school setting versus understanding these events and his decision-making strategies as secondary to a disease process and representing a stark change from his baseline level of functioning. Given the persistence of the symptoms, impairment of functioning in both the home and school setting and the stark change from being a more isolative withdrawn youth to one who is thrilled by a dare, it appears that Billy’s symptomatology is more accurately understood as part of an underlying mood disorder such as bipolar disorder or DMDD.
6 Assessment
In order to make the diagnosis of bipolar disorder, a comprehensive diagnostic assessment must be completed. This includes a parent–child interview, child interview, and interviewing the parents alone. The illness represents a marked departure from baseline functioning and it should be reflected in the level of impairment in different realms of the child’s life. Normal social/emotional development, contextual framework (i.e., family, peers, school and other psychosocial factors), and cultural implications are extremely important to integrate as symptomatology is being assessed and understood in children and adolescents. The pattern of illness, duration of symptoms, and association with psychomotor, sleep and cognitive changes are important diagnostic clues given that manic like symptoms of irritability and emotional reactivity for instance may be found in a variety of childhood disorders (McClellan et al. 2007). Collateral information should be obtained from schools, primary care physician, etc. Structured diagnostic interviews and questionnaires are available that may be helpful for diagnosing bipolar disorder in children and adolescents such as the KSADS and the WASH-U-KSADS. The Young Mania Rating Scale is commonly used to assess the severity of manic symptoms and assess treatment response. However, the YMRS is not a diagnostic instrument. To date there are no biological tests such as imaging or genetic studies that are helpful in making the diagnosis of bipolar disorder in children and adolescents (McClellan et al. 2007). The clinical interview is the gold standard and the child usually needs to be seen over a period of time as symptoms often fluctuate and are episodic.
Billy’s clinical presentation unfolded over the course of the school year in a fluctuating episodic nature. The integration of collateral information from parent and school and monitoring the symptom emergence over a period of time aided in understanding the disease process and accurate diagnosis.
7 Course of Illness
The clinical course of bipolar disorder in a child or adolescent diagnosed with this disorder can often times be an undulating and tumultuous one. Most studies have shown that at least 70–100 % of children and adolescents will recover (i.e., no significant symptoms within 2 months). However, of those who recover, up to 80 % will experience one or more recurrences in a period of 2–5 years (Birmaher et al. 2009). It has been found that these youth may suffer multiple hospitalizations, psychosis, suicide attempts and completion, substance abuse, unemployment, legal problems, and poor academic, and psychosocial functioning, which have a negative impact of multiple realms in the global level of functioning and interpersonal relationships (Martin and Volkmar 2007). In fact, the World Health Organization (WHO) reported that bipolar disorder is the fourth leading cause of disability among adolescents globally (Birmaher 2013).
The course of the illness is characterized with multiple fluctuations between syndromal and subsyndromal symptoms. Recent studies have shown that approximately 60 % of youth experience both syndromal and subsyndromal symptoms including both depressive and mixed states, which seems to be much more common in children and adolescents than adults (Martin and Volkmar 2007). Studies have shown that youth with bipolar disorder spent approximately 20 % of their follow up treatment course with full syndromal symptoms, 40 % of the time with subsyndromal symptoms and 40 % of the time euthymic (Birmaher 2013). The fluctuations in symptomatology are often rapid which contribute to the difficulty in diagnosing bipolar disorder in children.
The literature has demonstrated that early age of onset, long duration of illness, low socioeconomic status (SES), mixed or rapid cycling episodes, psychosis, subsyndromal symptoms, comorbid disorders, exposure to negative life events, and family psychopathology are associated with worse outcome (Birmaher et al. 2009; Martin and Volkmar 2007).
Furthermore, youth with subsyndromal mania (BP-NOS), especially those with a family history of bipolar disorder, are at risk to convert to BP-1 or 2 with rates of conversion of 45 %. And youth with BP-NOS have been shown to have just as much psychosocial impairment and risk for suicidality and substance abuse as the children with full syndromal bipolar type 1 (Birmaher et al. 2014).
8 Treatment
Treatment can usually be divided into phases: acute, continuation, and maintenance. A comprehensive treatment plan that is culturally sensitive, combining both medications and psychotherapeutic modalities should be considered to address both the frank symptoms and the psychosocial sequelae in children and adolescents with bipolar disorder. The goal of this comprehensive treatment plan is to improve symptoms, provide education about the illness, and promote treatment compliance in order to prevent relapse, reduce long-term morbidity, and promote normal growth and development (McClellan et al. 2007).
Psychoeducation and supportive therapy are essential during all of the phases of treatment. Given the significant psychosocial impairment and poor long-term prognosis associated with pediatric bipolar disorder, psychosocial intervention is imperative for a multimodal treatment approach (Weinstein et al. 2013). The unique symptoms of bipolar disorder in children and adolescents are associated with significant psychosocial impairment in several domains across development. Academically, youth with bipolar disorder demonstrate neurocognitive deficits and academic underperformance as well as disruptive school behaviors. Social functioning is influenced by limited peer networks, peer victimization, and poor social skills. Further, families of bipolar youth experience frequent sibling and parental conflict, lower levels of warmth, family adaptability and cohesion, and chronic stress in the context of family life. Children and adolescents with bipolar disorder also struggle internally with low self-esteem, hopelessness, and maladaptive coping skills (Weinstein et al. 2013).
Over recent years, there has been burgeoning research on evidence-based psychosocial interventions for pediatric bipolar disorder. Based on the literature, family psychoeducation plus skill building has the most empirical support and are considered first-line psychosocial interventions for pediatric bipolar disorder. These treatment modalities include multi-family psychoeducational psychotherapy (MF-PEP) and family-focused treatment for adolescents with bipolar disorder (FFT-A and FFT) (Fristad and MacPherson 2014). MF-PEP is a manualized intervention for children with depressive and bipolar spectrum disorders and their parents that combine psychoeducation with family therapy and cognitive behavioral therapy techniques. FFT-A consists of psychoeducation, communication enhancement training, and problem-solving skills training with adolescents, parents, and siblings. Child- and family-focused CBT as well as dialectical behavioral therapy with both a psychoeducation and skills building component have also demonstrated promising results, but more randomized controlled trials are needed. Interpersonal and social rhythm therapy that primarily targets medication compliance, interpersonal stress, and circadian rhythm dysregulation demonstrated preliminary positive findings in the current literature (Fristad and MacPherson 2014). It is important to note the similarities in all of the therapeutic approaches. The common active ingredients that should be included in the treatment of pediatric bipolar disorder should include: family involvement, psychoeducation about etiology, symptoms, course, medications, risk and protective factors, and effective treatment of bipolar disorders; skill building (especially communication, problem solving, CBT, and emotion regulation skills); and relapse prevention (Fristad and MacPherson 2014). Theses studies have also shown that clinicians should focus on improving parents’ knowledge of mood disorders and beliefs about treatment, and equipping them with skills to be effective advocates and coordinators of services for their child. Lastly, youth who are the most impaired, or come from negative familial environments, will benefit the most from implementation of family psychoeducation plus skill building interventions (Fristad and MacPherson 2014).
Pharmacotherapy primarily targets symptom improvement but often does not address the associated social, academic, and family difficulties that compromise quality of life and long-term outcomes. Thus, adjunctive psychosocial treatment has been indicated as a critical component of optimally effective treatment for pediatric bipolar disorder (Weinstein et al. 2013).
In the acute phase of treatment, stabilization of symptoms is the goal. Until recently, for mania or mixed states monotherapy with either a mood stabilizer such as lithium, valproate, or carbamazepine or an atypical antipsychotic was first-line treatment. Over the past few years, pharmacologic trials have increased rapidly and have led to updated treatment algorithms, placing atypical antipsychotics ahead of mood stabilizers as a first-line treatment choice (Fristad and Algorta 2013). Although atypical antipsychotics as a group are more effective in reducing manic symptoms, they are fraught with more metabolic side effects (Peruzzolo et al. 2013). Atypical antipsychotics have been shown to have a more rapid response and highly effective in reducing manic symptoms (Geller et al. 2012). If monotherapy fails and/or there is a partial response then the combination of two mood stabilizers or a mood stabilizer and an atypical antipsychotic must be considered. For children and adolescents who has mania with psychosis an atypical antipsychotic is considered first-line treatment. In bipolar youth with depression, mood stabilizers including lamotrigine and lithium in particular or atypical antipsychotics are still first-line treatment. However, often times, there is a partial response and the addition of an antidepressant such as a selective serotonin reuptake inhibitor or bupropion is needed. For youth with bipolar disorder in particular, cognitive behavioral therapy, interpersonal therapy, and dialectical behavioral therapy have been shown to be helpful in addition to psychoeducation and supportive therapy.
At times, adjunctive medications are needed to target severe agitation, insomnia, or aggression. In those circumstances, benzodiazepines such as lorazepam or clonazepam have been efficacious. In cases of severe illness, which has been treatment refractory, ECT in adolescents can be considered (Martin and Volkmar 2007). Once acute symptoms have been stabilized, the continuation and maintenance treatment phase goal is to prevent new mood episodes. Relapse can be as high as 92 % in children and adolescents who stop taking their medications. Thus, most youth require at minimum monotherapy for maintenance treatment (Martin and Volkmar 2007).
In regards to the case example, Billy responded very well to monotherapy with an atypical antipsychotic and has been maintained on the same dose without any further mood episodes.
It is clear that pharmacotherapy can be quite effective. Thus, choosing the right medication is very important. The most influential factors are efficacy, the long-term side effect profile and practicality. Lithium has been shown to be quite an effective medication for youth with bipolar disorder in both manic/mixed states and depressive states. However, from a practical point of view, given that lithium levels will need to be drawn on a regular basis, consideration must be given for the patient if he/she can sustain recurrent blood draws. In regards to atypical antipsychotics, the metabolic side effects are the most problematic and must be taken into account in the decision-making process. If the patient is already overweight and/or prediabetic these factors become even more important when contemplating treatment with these medications.
With comorbid illnesses, it is very important to treat both the bipolar disorder and the comorbid disorders; because if left untreated (i.e., ADHD), it will worsen the prognosis of bipolar disorder. It is recommended that the treatment for bipolar disorder be optimized first and then subsequently address the comorbid symptoms. Since there is overlap in the symptoms of bipolar disorder and ADHD such as impulsivity and short attention span—often when the underlying bipolar disorder is successfully treated—the patient may no longer have the symptoms of ADHD suggesting that ADHD was not a comorbid condition in that case.
9 Future Directions
Given the growing consensus that bipolar disorder is a progressive disease, obtaining real-time psychologic and self-report measures is extremely helpful to both understand the disease process but also to ascertain efficacious real-time coaching or other interventions in order to provide highly personalized and timely interventions to children and adolescents with bipolar disorder (Fristad and Algorta 2013). Technology can pave the way for this and children and adolescents have already demonstrated in the burgeoning telepsychiatry literature that they actually like using technology in the scope of treatment. Utilizing novel technological devices such as smartphones or higher definition, more sophisticated devices for daily monitoring of mood changes could permit identification of individual disease patterns, which could possibly provide new avenues to early detection of full episodes, as well as guide treatment adjustments. These technological advances have the potential to lead to the development of precise prognostic models and personalized, timely treatment, which may ultimately include the prevention of suicide and long-term disability. These new treatment strategies also have the potential to reach populations with poor access to services and reduce costs associated with the provision of care. Treatment might include modules on: compliance to pharmacological and psychosocial treatment modalities; sustaining a regular sleep pattern; identifying mood features; developing cognitive restructuring strategies; enhancing relaxation techniques; and could include real-time personalized feedback. It may also be possible via technology to improve communication strategies with family members and other supports in a child’s life (Fristad and Algorta 2013). This type of work has already been implemented with adults, and by initial accounts appear to be quite promising in youth. There has been only one feasibility study to date in pediatric samples (Fristad and Algorta 2013).
As research has examined the benefits of both pharmacological and psychosocial interventions in pediatric bipolar disorder, the importance of nutrition in the treatment of bipolar disorder in youth has recently been empirically investigated. Recent studies have examined the role of Vitamin D and mood impairment suggesting that Vitamin D deficiency may be associated with severity of mood symptoms and psychosis. Studies have also looked at the role of omega-3 fatty acids in mood stabilization (Fristad and Algorta 2013).
Further more, machine-learning approach has been utilized in emerging research to help diagnose children and adolescents with bipolar disorder. Several studies have used pattern recognition and neuroimaging to decode present and future symptom severity in behaviorally and emotionally dysregulated youth (Mwangi et al. 2014; Mourão-Miranda et al. 2016).
Lastly, although the emergence and efficacy of evidence-based psychosocial treatment interventions have been promising more work needs to be done in the development of treatment and psychosocial approaches to be utilized in the school setting and also for dually diagnosed children and adolescents with drug and alcohol use/abuse (Fristad and Algorta 2013).
10 Case Outcome
Although Billy had a fluctuating episodic course, it was eventually discerned that had bipolar disorder and was promptly started on a low dose atypical antipsychotic medicine. Billy responded well to the medication and his hypomania/manic symptoms dissipated. However, Billy continued to struggle with his decision-making strategies and navigating social constructs. With ongoing individual therapy and family therapy over time, Billy has demonstrated improvement in these areas as well and has made it through his sophomore year in high school without incident.
11 Conclusion
Bipolar disorder can be a devastating illness, which is associated with significant morbidity and sadly at times mortality due to suicide. However, it is a treatable illness and if a child or adolescent is provided the appropriate and timely pharmacotherapy and psychotherapeutic interventions symptoms can be alleviated and the patients stabilized so they can do well and enjoy a healthy emotional life. Bipolar disorder in children and adolescents provides an added level of complexity diagnostically due to a number of factors: the rapid fluctuation in mood symptoms, developmental issues that impact the clinical picture, the difficulties that youth have in articulating how they feel and the high rates of comorbid disorders. Recent research has emerged that has shed light on symptom presentation and treatment efficacy in children and adolescents with bipolar disorder. But there remains much more to learn about risk/genetic factors and a better understanding of the biological underpinnings, cognitive development and changes in the brain. Further, we do not currently fully appreciate all of the long-term effects and efficacy of the treatment modalities and their long-term impact. Several studies are underway examining the role of social/environmental factors such as: parental lifetime and current psychopathology, level of psychological support, and exposure to negative life events (abuse, poor school or neighborhoods, and ongoing family conflict). Without question, combination treatment that includes pharmacotherapy, family involvement, psychoeducation about etiology, symptoms, course, medications, risk and protective factors, skill building (especially communication, problem solving, CBT, sleep hygiene, emotion regulation skills), and relapse prevention can reduce symptoms and improve overall level of functioning. However, much more needs to be learned to improve treatment response and ultimately prevent and/or cure bipolar disorder in children and adolescents.
References
Althoff, R. R., Faraone, S. V., Rettewe, D. C., Morley, C. P., & Hudziake, J. J. (2005). Family, twin, adoption, and molecular genetic studies of juvenile bipolar disorder. Bipolar Disorders, 7(6), 598–609.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Birmaher, B. (2013). Bipolar disorder in children and adolescents. Child and Adolescent Mental Health, 18(3), 140–148.
Birmaher, B., Axelson, D., Goldstein, B., Strober, M., Gill, M., & Hunt, J. (2009). Four year longitudinal course of children and adolescents with bipolar spectrum disorder. American Journal of Psychiatry, 166(7), 795–804.
Birmaher, B., Gill, M. K., Axelson, D. A., Goldstein, B. I., Goldstein, T. R., Yu, H., et al. (2014). Longitudinal trajectories and associate baseline predictors in youths with bipolar spectrum disorders. American Journal of Psychiatry, 171(9), 990–999.
Brotman, M. A., Schmajuk, M., Rich, B. A., Dickstein, D. P., Guyer, A. E., Costello, E. J., et al. (2006). Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biological Psychiatry, 60(9), 991–997.
DelBello, M. P., & Geller, B. (2001). Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disorders, 3(6), 325–334.
Fristad, M., & Algorta, G. (2013). Future directions for research on youth with bipolar spectrum disorders. Journal of Clinical Child and Adolescent Psychology, 42(5), 734–747.
Fristad, M., & MacPherson, H. (2014). Evidence-based psychosocial treatments for child and adolescent bipolar spectrum disorders. Journal of Clinical Child and Adolescent Psychology, 43(3), 339–355.
Geller, B., Badner, J. A., Tillman, R., Christian, S. L., Bolhofner, K., & Cook, E. H., Jr. (2004). Linkage disequilibrium of the brain derived neurotrophic factor Val66Met polymorphism in children with a prepubertal and early adolescent bipolar disorder phenotype. American Journal of Psychiatry, 161(9), 1698–1700.
Geller, B., Luby, J. L., Joshi, P., Wagner, K. D., Emslie, G., Walkup, J. T., et al. (2012). A randomized controlled trial of risperidone, lithium or divalproex sodium for initial treatment of bipolar 1 disorder, manic or mixed phase, in children and adolescents. Archives of General Psychiatry, 69(5), 515–528. doi:10.1001/archgenpsychiatry.2011.1508
Geller, B., Zimerman, B., Williams, M., DelBello, M. P., Bolhofner, K., Craney, J. L., et al. (2002a). DSM-IV mania symptoms in a prepubertal and early adolescent bipolar disorder phenotype compared to attention-deficit hyperactive and normal controls. Journal of Child and Adolescent Psychopharmacology, 12(1), 11–25.
Geller, B., Zimerman, B., Williams, M., DelBello, M. P., Frazier, J., & Beringer, L. (2002b). Phenomenology of prepubertal and early adolescent bipolar disorder: Examples of elated mood, grandiose behaviors, decreased need for sleep, racing thoughts and hypersexuality. Journal of Child and Adolescent Psychopharmacology, 12(1), 3–9.
Goldstein, B. I., & Levitt, A. J. (2006). Further evidence for a developmental subtype of bipolar disorder defined by age at onset: Results from the national epidemiologic survey on alcohol and related conditions. American Journal of Psychiatry, 163(9), 1633–1636.
Hillegers, M. H., Reichart, C. G., Wals, M., Verhulst, F. C., Ormel, J., & Nolen, W. A. (2005). Five-year prospective outcome of psychopathology in the adolescent offspring of bipolar parents. Bipolar Disorders, 7(4), 344–350.
Hudziak, J. J., Althoff, R. R., Derks, E. M., Faraone, S. V., & Boomsma, D. I. (2005). Prevalence and genetic architecture of child behavior checklist-juvenile bipolar disorder. Biological Psychiatry, 58(7), 562–568.
Kowatch, R. A., Youngstrom, E. A., Danielyan, A., & Findling, R. L. (2005). Review and meta-analysis of the phenomenology and clinical characteristics of mania in children and adolescents. Bipolar Disorders, 7(6), 483–496.
Leibenluft, E., Charney, D. S., Towbin, K. E., Bhangoo, R. K., & Pine, D. S. (2003). Defining clinical phenotypes of juvenile mania. American Journal of Psychiatry, 160(3), 430–437.
Leibenluft, E., Cohen, P., Gorrindo, T., Brook, J. S., & Pine, D. S. (2006). Chronic versus episodic irritability in youth: A community-based, longitudinal study of clinical and diagnostic associations. Journal of Child and Adolescent Psychopharmacology, 16(4), 456–466.
Lewinsohn, P., Klein, D., & Seeley, J. (2000). Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disorders, 2(3Pt2), 281–293.
Martin, A, Volkmar, F. (2007). Lewis’ child and adolescent psychiatry. A comprehensive textbook (4th ed.). USA: Lippincott Williams & Wilkins.
McClellan, J., Kowatch, R., & Findling, R. (2007). Practice parameter for the assessment and treatment of children and adolescents with bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 1.
Moreno, C., Laje, G., Blanco, C., Jiang, H., Schmidt, A. B., & Olfson, M. (2007). National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Archives of General Psychiatry, 64(9), 1032–1039.
Mourão-Miranda, J., Oliveira, L., Ladouceur, C. D., Marquand, A., Brammer, M., Birmaher, B., et al. (2016). Pattern recognition and functional neuroimaging help to discriminate healthy adolescents at risk for mood disorders from low risk adolescents. Journal of Affective Disorders, 192(1), 219–225.
Mwangi, B., Spiker, D., Zunta-Soares, G. B., & Soares, J. C. (2014). Prediction of pediatric bipolar disorder using neuroanatomical signatures of the amygdala. Bipolar Disorders, 16(7), 713–721.
Neuman, R. J., Geller, B., Rice, J. P., & Todd, R. D. (1997). Increased prevalence and earlier onset of mood disorders among relatives of prepubertal versus adult probands. Journal of the American Academy of Child and Adolescent Psychiatry, 36(4), 466–473.
Paaren, A., Bohman, H., von Knorring, L., & Olsson, G. (2014). Early risk factors for adult bipolar disorder in adolescents with mood disorders: A 15 year follow up of a community sample. BMC Psychiatry, 14, 3638.
Pavuluri, M. N., Henry, D. B., Nadimpalli, S. S., O’Connor, M. M., & Sweeney, J. A. (2006). Biological risk factors in pediatric bipolar disorder. Biological Psychiatry, 60(9), 936–941.
Peruzzolo, T., Tramontina, S., Rohde, L., & Zeni, C. (2013). Pharmacotherapy of bipolar disorder in children and adolescents: An update. Revista Brasileira de Psiquiatria, 35(4), 393–405.
Stringaris, A., Baroni, A., Haimm, C., Brotman, M., Lowe, C. H., Myers, F., et al. (2010). Pediatric bipolar disorder versus severe mood dysregulation: Risk for manic episodes on follow-up. Journal of the American Academy of Child and Adolescent Psychiatry, 49(4), 397–405.
Strober, M., Morrell, W., Burroughs, J., Lampert, C., Danforth, H., & Freeman, R. (1988). A family study of bipolar I disorder in adolescence. Early onset of symptoms linked to increased familial loading and lithium resistance. Journal of Affective Disorders, 15(3), 255–268.
Van Meter, A. R., Moreira, A. L. R., & Youngstrom, E. A. (2011). Metaanalysis of epidemiologic studies of pediatric bipolar disorder. Journal of Clinical Psychiatry, 72(9), 1250–1256.
Weinstein, S., West, A., & Pavuluri, M. (2013). Psychosocial intervention for pediatric bipolar disorder (PBD): Current and future directions. Expert Review of Neurotherapeutics, 13(7), 843–850.
Wozniak, J., Biederman, J., Kiely, K., Ablon, J. S., Faraone, S. V., Mundy, E., et al. (1995). Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. Journal of the American Academy of Child and Adolescent Psychiatry, 34(7), 867–876.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer India
About this chapter
Cite this chapter
Cullins, L.M., Call, D.C., Joshi, P.T. (2016). Pediatric Bipolar Disorders: Current Understanding and Management. In: Malhotra, S., Santosh, P. (eds) Child and Adolescent Psychiatry. Springer, New Delhi. https://doi.org/10.1007/978-81-322-3619-1_1
Download citation
DOI: https://doi.org/10.1007/978-81-322-3619-1_1
Published:
Publisher Name: Springer, New Delhi
Print ISBN: 978-81-322-3617-7
Online ISBN: 978-81-322-3619-1
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)