Abstract
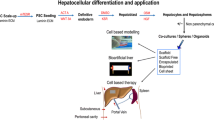
Cellular compensation from extrahepatic resources is expected to improve the prognosis of liver diseases. Currently, liver dysfunction is treated by a variety of modalities including drugs, cytokines, vascular interventions, energy devices, surgery, and liver transplantation; however, in recent years there have been few significant advancements in treatment efficacy. A next-generation therapeutic strategy for liver disease, cellular compensatory therapy (i.e., cell therapy), is now being considered for clinical practice. Liver dysfunction is attributed to a lack of sufficient functional cells. However, processes involved in recovery of liver function are not fully elucidated, which has complicated the interpretation of treatment effects at the cellular level. Our genotyping study of living donor liver transplantation revealed that a variety of graft liver tissues contained the donor genotype, indicating that extrahepatic cells had differentiated into liver component cells during liver regeneration. Multilineage-differentiating stress-enduring (Muse) cells appear to be a strong candidate for extrahepatic resources that can contribute to liver regeneration. Muse cells are defined as stage-specific embryonic antigen 3-expressing cells that contribute to tissue regeneration and have the potential to differentiate into three germ layers. The significant advantage of Muse cells over other “pluripotent cells” is that Muse cells are present in bone marrow/blood as well as a variety of connective tissues, which provides safety and ethical advantages for clinical applications. Here, we review current therapeutic topics in liver diseases and discuss the potential for cell therapy using Muse cells based on our recent studies of Muse cell administration in a mouse model of physical partial hepatectomy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Liver regeneration
- Hepatectomy
- Physical partial hepatectomy
- Partial hepatectomy
- Living donor liver transplant
- Chimerism
- Extrahepatic cells
- Mesenchymal stem cells
- Multilineage-differentiating stress-enduring cells
- SSEA-3
12.1 Introduction
The legend of Prometheus describes the liver as an organ that has the power to recover from acute loss of physiological mass. Although probable, yet not fully realistic in a practical sense, “organ regeneration” requires differentiation into the multiple cell types that comprise the organ. Liver regeneration after resection (i.e., hepatectomy) generally implies “volume gain” after reduction of liver volume in clinical practice, but how volume loss is compensated is unclear. Notably, hepatocyte hypertrophy is reported to play a central role in “volume gain” in response to liver volume loss, particularly in the acute stages of liver damage [1, 2]. We recently demonstrated that liver regeneration is a multistep process in which the size of hepatocytes increases in the acute phase, followed by cellular proliferation and subsequent differentiation [3]. These observations suggest that “organ regeneration” of the liver requires cells that can differentiate into multiple distinct cell types such as hepatocytes and cholangiocytes. Thus, therapies for liver disease would be predicted to require either fully differentiated cells that can compensate for loss of cellular function and volume or an enriched cell population with proliferative potential to differentiate into multiple cell types.
Current modalities for liver diseases are roughly divided into three major categories: (i) drugs, (ii) cytokines, and (iii) vascular/surgical interventions. Drugs and cytokines generally target the entire liver to treat diffuse types of liver disease, such as hepatitis and nonalcoholic fatty liver disease [4, 5], whereas interventions are mostly performed to treat local lesions such as neoplasms and injury [6]. Although these statuses are distinct, structure reconstruction and volume compensation of the liver are mandatory for both diffuse and local liver diseases. Some of these modalities are established as “standard therapy,” but none were based on the concept of tissue-level regeneration.
As one candidate for assisting current therapies for liver disease, cell therapy has been discussed for decades as an alternative for patients for whom no other modalities were effective. Cell therapies for liver diseases can be roughly divided into two groups that involve hepatocytes or mesenchymal stem cells (MSCs). Hepatocyte transplantation was developed for patients with metabolic disorders that have a hepatic basis and acute or chronic liver failure. However, due to difficulties in acquiring good quality “donor” hepatocytes, the number of hepatocyte transplantation cases was approximately 80 worldwide as of 2011 [7]. Although hepatocyte transplantation reportedly can be performed safely and improve disease status [8,9,10], practical constrains such as a shortage of donors, limited success of hepatocyte engraftment in a severely damaged liver, and difficulties in obtaining high-quality hepatocytes remain before this approach can be applicable in a routine fashion [11].
Because MSCs are fractions generally isolated from the bone marrow or adipose tissue and lack genetic or biochemical modifications, the risk of tumor formation following treatment with these cells is extremely low despite their ability to display multiple germ layer differentiation markers in vitro [12, 13]. Recent observations suggest that paracrine-mediated functions of MSCs attenuate acute liver failure [14]. However, which cell populations present in crude MSCs isolates make significant contributions to biological activities that encourage tissue repair is unclear [12, 15]. Based on the estimation that only a very small fraction of cells in MSCs actually contribute to liver regeneration, we found that Muse cells directly committed to the replacement of multiple liver component cells [3]. Muse cells exist in bone marrow/blood as well as a variety of connective tissues and have demonstrated a differentiating ability in various tissue types in the context of tissue repair and regeneration [16]. We examined whether “extrahepatic” Muse cells were involved in liver regeneration processes that occur after physical partial hepatectomy (PPHx). Using a mouse PPHx as a model of human living donor liver transplantation (LDLT), we demonstrated how Muse cells were integrated into the damaged liver during liver regeneration and participated in the tissue reconstruction [3].
The human LDLT procedure uses a healthy donor graft explanted with a portion of liver that is physically removed from the healthy organ, namely, hepatectomy. This unique feature of LDLT provides an opportunity to trace what types of cells are involved in liver tissue repair and regeneration. Cells in the liver, post-engraftment of liver transplantation, have been shown to possess the recipient genotype, which suggests that extrahepatic cells are indeed integrated in the graft liver [17,18,19,20,21]. Interestingly, among the cells engrafted, cholangiocytes were reported to possess multipotency as evidenced by their expression of both hepatocyte and cholangiocyte lineage markers [20].
In this chapter, we will first review current therapies for liver diseases and then discuss possibilities for cellular therapy, with a special focus on Muse cells. Based on our current findings that suggest a substantial role for Muse cells in post PPHx liver regeneration, we will discuss the biology and potential applications for cell therapy using Muse cells.
12.2 Hepatectomy
Hepatectomy involves surgical resection for localized liver disease and LDLT donors. In humans, hepatectomy has been performed to treat various liver neoplastic diseases including hepatocellular carcinoma [22] and metastatic liver tumors [23, 24], as well as for the acquisition of graft liver for LDLT [25, 26]. At 1 year post-operation, the percentage of liver growth of the remnant left liver of LDLT donors has been reported to be 146% in average, whereas the “simple” right liver graft becomes 152% of the original graft volume in average [27, 28]. However, the detailed mechanism of liver volume recovery in humans remains unclear because of the difficulties in acquiring multiple biopsy samples from the injury front. Additionally, no markers exist to trace the lineage of cells participating in regeneration. Therefore, to study liver regeneration mechanisms at a cellular level, partial hepatectomy (PHx) of rodents has been widely used. Most PHx procedures for rodents use a 2/3 PHx because, in contrast to the human liver, the rodent liver is divided into distinct four lobes [29, 30]. Also in contrast to the human liver, in rodents, a simple ligation of the lobe stem is sufficient to accurately remove the liver and leave an intended volume. In fact, ligation of the base of the left lateral lobe and the median lobes corresponds to a 2/3 volume reduction [31, 32]. However, there is no “injury” region in the remnant liver resulting from the “hepatectomy” mimicked by the ligation technique. PHx in humans is almost always concomitant with an injury caused by transection, where acute inflammatory reactions and wound-healing processes actively occur. Thus, to assess liver regeneration mechanism after an injury at the cellular level, we recently introduced the PPHx technique, which involves a transection line made in the middle of the left lobe of the rodent liver that results in approximately a 30% hepatectomy. The PPHx also retains a long transection (i.e., injured) line, such that the procedure is relatively similar to that of a hepatectomy in humans in terms of the degree of invasiveness and the recovery process from the local liver injury. This model is thus particularly useful for studying host reactions in acute local liver regeneration.
12.3 LDLT
Whether extrahepatic factors (i.e., cytokines or extrahepatic cells) are involved in human liver repair regeneration has long been controversial. Examination of the involvement of such factors has been extremely difficult to investigate directly in humans because it requires cellular labeling in patients undergoing hepatectomy. The only example from which insight can be gained into cellular involvement in graft liver is human LDLT genotyping [33]. For LDLT, a section of liver (i.e., graft) transected out from a healthy donor is transplanted into a patient from whom the entire malfunctioning liver has been removed (Fig. 12.1). Therefore, at a histological level, the graft liver has a transection line equivalent to the liver injury created by discontinuation of the hepatic parenchyma and vessels [34]. The transplanted graft liver appears to undergo three important steps in the recovery process: (a) acute inflammatory reactions, particularly in the area of injury; (b) semi-acute volume recovery via hepatocyte hypertrophy; and (c) liver vascular regeneration.
Schematic illustration of LDLT. The right lobe of the donor is removed by hepatectomy (D) and transplanted into the recipient (R) as a graft (G). During liver regeneration, including tissue repair processes in the graft, two genotypes, from donor and recipient, are present in the graft liver. D donor, R recipient, and G graft liver. (The data are reproduced from Katagiri et al. [3])
All three steps require cellular resources for local tissue repair and liver volume compensation. To clarify how the liver acquires volume through these steps, we must first evaluate hepatocytes in LDLT grafts in terms of liver volume rendering and histological examinations. Among 13 available LDLT graft liver cases treated at Iwate Medical University Hospital that were examined at three time points, 8 cases showed liver volume gains (range, 108–169% of initial graft volume), whereas the other 5 cases had reduced volume (range, 82–99%; Fig. 12.2A). However, chronologic traces of cellular density revealed that all cases had reduced hepatocyte density at early time points that recovered by late time points, indicating that hepatocytes were hypertrophic during the engraftment process (Fig. 12.2B) [35]. Although the final liver volume may be affected by various other factors in the clinical course [36,37,38,39,40], these results suggest that hepatocyte hypertrophy plays a role in liver volume gains during the acute phase and that liver volume may later be compensated by a recovery in cell number.
Changes in volume and hepatocyte number in graft liver tissue. (A) Change in the LDLT graft liver volume in recipients, relative to the initial “zero-point” graft volume, represented as 100%. A horizontal dashed line indicates 80% relative to the initial volume. (B) The number of hepatocytes counted in needle biopsy specimens at three different time points. The view area is 200 × 200 μm2. (The data are reproduced from Katagiri et al. [35])
Notably, Miyaoka et al. reported that liver volume recovery after a 30% partial hepatectomy in a murine model could be fully achieved solely through hypertrophy of the remnant liver without cell division [2]. Furthermore, their 70% partial hepatectomy model demonstrated that most of the liver volume recovery process is primarily due to hepatocyte hypertrophy and subsequent cell division. However, putative “liver progenitor cells (LPCs)” could emerge and contribute to liver regeneration in circumstances when the liver is severely injured and hepatocyte proliferation process is disrupted [41]. Although the origin of the LPCs remains to be identified, one source for LPCs could be the Canals of Hering, where hepatocytes and cholangiocytes are connected, which implies the potential for structural development into hepatocytes and cholangiocytes [42]. Our observations on LDLT show the presence of cytokeratin (CK)19+/alpha-fetoprotein (AFP)+ cells in the periportal area, suggesting that cells with bipotential play certain roles in liver regeneration [3]. We also performed genotyping using extracted DNA from laser microdissection to determine whether hepatocytes and cholangiocytes comprise donor- and/or recipient-derived cells (Fig. 12.3A–C). Genotyping analysis of human polymorphic short tandem repeat (STR) markers for hepatocytes revealed that 35.3% of LDLT patients exhibited chimeric genotypes (i.e., donor and recipient), although in most cases the allele fraction appeared to be small. Conversely, 70.6% of recipient cholangiocytes showed a chimeric genotype (Fig. 12.3D). In addition, using female-to-male LDLT samples, our fluorescence in situ hybridization (FISH) analysis also revealed the chimeric genotype (i.e., XY chromosomes in the graft liver) in hepatocytes and cholangiocytes (Fig. 12.3E–F). These results collectively suggest that hepatocyte hypertrophy plays an important role in response to hepatectomy and some fraction of extrahepatic cells may contribute to liver regeneration.
Genotyping of LDLT samples. (A) CD68 and (B) CK7 immunostaining provide the orientation for laser microdissection of the liver sinusoid and bile duct, respectively. (C) Samples before (left column) and after (right column) laser microdissection. Each laser-microdissected specimen was subjected to DNA extraction and yielded sufficient amounts of DNA for PCR analysis. (D) Three STR markers (Amelogenin, TH01, and FGA) are represented for four different histological fractions. Donor and recipient DNA were obtained from peripheral blood mononuclear cells. (E) Frequency of cells carrying a Y chromosome in cases of female donors and male recipient specimens in respective cell types (n = 3). (F) FISH images of one sex-mismatch case. From the top row, hepatocytes, cholangiocytes, and sinusoidal endothelial cells. Cell types were identified by immunohistochemistry. Green and red fluorescence represents Y and X chromosomes, respectively. D donor, R recipient, and NI not informative. H&E, hematoxylin and eosin; IHC, immunohistochemistry; and FISH, fluorescent in situ hybridization. (The data are reproduced from Katagiri et al. [3])
LDLT is often performed under complicated conditions, and the recovery process can have substantial limitations. Biopsy of postoperative LDLT is performed only when necessary, and for safety reasons, samples must be taken at site distant from the “damaged area” instead of the active regeneration front. Despite these practical limitations, chimeric genotypes are still seen in substantial fractions of the LDLT graft liver. These results suggest that extrahepatic cells capable of differentiating into liver component cells can originate from the blood flow, most likely from the recipient’s bone marrow.
12.4 Extrahepatic Resources for Liver Regeneration
One of the demands for liver disease treatment using extrahepatic cells is the support for hepatic local injury. In fact, hepatectomy in humans is one of the most invasive and advanced surgical procedures currently performed. Extrahepatic cell support of liver regeneration at the tissue level for postoperative patients has been reported on human hematopoietic stem cells (HSCs), MSCs, hepatocytes, and others; however, no practical example standards have been established [9, 11, 14, 43]. One major difficulty has been due to the fact that the pathological liver regeneration process has not been fully clarified. It is indeed difficult to see the entire process of liver regeneration after hepatectomy in humans because multiple pathological and imaging examinations are required, such as biopsy from the injury front, where the most active histological liver regeneration takes place. Yet, this area must be avoided due to the risk of bleeding. Using a time axis observation of the injury front after PPHx in a mouse, we were able to chronologically observe the events at the tissue level [3]. In the first 24–48 h after PPHx, a substantial number of neutrophils and monocytes infiltrated along the injury front. The cellular infiltration decreased by 72 h, but bile duct-like structures occasionally emerged in the injury front, particularly in the periportal area [44]. These observations established the baseline for steps that are adoptable for any type of support by extrahepatic cells for liver regeneration. Taken together with LDLT genotyping findings, we prioritized exploration of the potential of extrahepatic cells to support liver regeneration, particularly for such a liver injury.
One of the most “intuitive” extrahepatic cell applications to treat liver failure may be hepatocyte transplantation [45]. In principle, hepatocyte transplantation involves a collagenase perfusion technique that does not require special cell separation by fractionation [46, 47]. The route for hepatocyte infusion can be via the portal vein or intrasplenic or intraperitoneal areas [8]. Though limited, the life expectancy of some patients was extended by hepatocyte transplantation, and a few patients fully recovered [8]. Although most previous reports suggested the feasibility and safety of this procedure, obtaining high-quality donor cells and characterization of mechanisms associated with cellular engraftment remain uncertain [11].
The application of MSCs, also known as “mesenchymal stromal cells,” has been established and is gaining broad acceptance as an approach to achieve cell-mediated recovery from liver failure [48]. MSCs have no associated ethical issues due to their derivation from bone marrow or adipose tissue. In a clinical setting, HSC transplantation of BM transplants likely containing a small number of BM-MSCs has already been performed and demonstrated to be safe [48, 49]. Indeed, the therapeutic effect of BM-MSCs for liver diseases has been demonstrated in humans [50, 51].
As one of the extrahepatic resources for liver regeneration, Muse cells have few ethical concerns and show low tumorigenicity in comparison with induced pluripotent stem (iPS) and embryonic stem (ES) cells [16]. The natural application of Muse cell administration is to treat liver failure by supporting tissue-level development at liver damage sites. A previous study already demonstrated that Muse cells can contribute to liver regeneration in response to carbon tetrachloride-induced acute liver failure, and our more recent study showed that Muse cells are meaningful contributors to liver damage induced by a local injury in the context of liver regeneration at the tissue level [3, 16].
12.5 Differentiation of Muse Cells that Are Integrated into the Liver
Muse cells were first reported in 2010 as a distinct population of pluripotent stem cells that account for a small percentage of MSCs [16]. The functional identification of Muse cells was reported as a stress-tolerant fraction of MSCs that survived in the presence of trypsin or in the presence of limited nutrients [52]. Although Muse cells share properties with MSCs and express mesenchymal markers such as CD105, CD90, and CD29, Muse cells can be specifically characterized by the expression of the glycolipid, stage-specific embryonic antigen-3 (SSEA-3), which is a well-known marker of undifferentiated ESs and other pluripotent cells in humans. The SSEA-3+ fraction comprises ~1% of BM-MSCs in human BM aspirates and represents ~0.03% of BM-mononucleated cells [16]. Recent studies have revealed that Muse cells could be found in peripheral blood and in a wide range of connective tissues [53,54,55]. In addition, Muse cells have been reported to be a primary source of iPS cells [56, 57].
The PPHx model, in contrast to postoperative human specimens, provides opportunities to continually trace chronological changes in the liver, particularly in areas close to physical damage sites. From results of our LDLT genotyping studies, we speculated that extrahepatic cells such as Muse cells play certain roles in liver regeneration [3]. Moreover, accumulated findings implied that extrahepatic cells could contribute to recovery from various hepatic failures [45]. Thus, we combined the PPHx model and Muse cell administration so that the process of Muse cell integration could be observed in the context of liver regeneration.
We showed that intravenous infusion of GFP-labeled human Muse cells into the SICD mouse xenograft model demonstrated the integration of Muse cells in the damaged area adjacent to the transection line wherein GFP-labeled Muse cells appeared in the periportal regions adjacent to the actual injury at 1 week post-hepatectomy (Fig. 12.4). However, at that point, those cells did not appear to be immediately differentiated into any tissue components and were difficult to distinguish from cells that had simply proliferated around the injury as part of the inflammation process. At 2 weeks after infusion, some of the Muse cells began to form bile duct-like structures. Muse cells were also found in the sinusoid area. Integration of the Muse cells traced up to 4 weeks showed that the population of Muse cells that had integrated into the liver composed of cholangiocytes (17.7%), hepatocytes (74.3%), Kupffer cells (6.0%), and sinusoidal endothelial cells (2.0%). Importantly, these differentiation and functional markers were completely absent in all GFP+ non-Muse cells, namely, cells other than Muse cells in BM-MSCs as control.
(A–G) Immunohistochemical images of the liver from a GFP-labeled Muse cell-transplanted mouse. (A) GFP-labeled cells at the transection border of the liver. (B) An intact periportal area close to the transection border, where GFP-positive cells are occasionally seen. (C) GFP-positive bile ducts along the transection border. (D) GFP-positive cells in sinusoids. (E) GFP-positive cells form a duct-like structure. (F) GFP-positive hepatocytes. (G) GFP-positive sinusoidal cells. (H–J) No GFP-positive cells were seen in livers from the non-Muse cell-transplanted group. Dashed lines indicate the transection border. (The data are reproduced from Katagiri et al. [3])
We also assessed the molecular and morphological features of these integrated cells. In the early phases (i.e., 1 week) after hepatectomy and Muse cell administration, the small number of Muse cells expressed human liver progenitor markers, such as CK19, delta-like protein (DLK), OV-6 (an oval cell marker), and AFP, in the periportal area adjacent to the transection line, suggesting that Muse cells may be integrated into each functional structure of the liver through the appropriate progenitor forms (Fig. 12.5). A chronological tracing of the integrated Muse cells revealed that, at 1 week, the Muse cells still expressed the liver progenitor markers. At 2 weeks, the Muse cells integrated into appropriate tissue structures expressed additional markers of differentiation, such as human-specific HepPar-1, albumin, alpha-1-antitrypsin, CK7, and Lyve-1, but the majority no longer expressed liver progenitor markers (Fig. 12.6 and Table 12.1). At 4 weeks, the specificity of protein expression by the integrated Muse cells was clearly supported by species-specific RT-PCR, discriminating human Muse cells from host mouse liver cells, indicating that integrated cells expressed these markers were derived from human Muse cells [3].
Expression of human CK19, DLK, OV6, and AFP 1 week after GFP-labeled Muse cell administration. Arrowheads indicate staining-positive cells. Insets show high-power magnification of the region. PV portal vein. Scale bar, 50 μm. (The data are reproduced from Katagiri et al. [3])
Human HepPar-1, CK7, Lyve-1, and CD68 expression 8 weeks after GFP-labeled Muse cell administration. Insets show high-power magnification of the region. Scale bar, 20 μm (The data are reproduced from Katagiri et al. [3])
12.6 The Role of Cell Fusion in Extrahepatic Cell Integration into the Liver
Despite these accumulated findings for Muse cell integration, these phenomena could simply be due to cell fusion that occurs during liver regeneration [58]. Extrahepatic stem cell plasticity in the context of liver regeneration has been extensively studied using fumarylacetoacetate hydrolase (Fah) knockout mice and discussed in a series of publications by Grompe et al. and others [59,60,61,62,63,64,65]. The Fah-deficient mice developed severe liver malfunctions following withdrawal of 2-(2-nitro-4-trifluoromethylbenzoyl)-1,3-cyclohexanedione (NTBC), which is used to treat tyrosinemia in humans via inhibition of p-OH phenylpyruvate dioxygenase [66, 67]. A Fah knockout mouse transplanted with sex- and genotype-mismatched bone marrow cells exhibited “repopulation” of bone marrow-derived hepatocytes in the liver through the bloodstream, which was explained by stem cell plasticity through cell fusion [68]. With these knockout and bone marrow transplant systems, the repopulation of BM cells to the damaged liver may have at least partially occurred at low frequency by fusion instead of BM-derived stem cell transdifferentiation [69, 70]. Although BM-derived cells undergo spontaneous cell fusion at very low frequencies (2–11 clones per 106 BM cells), fused cells could nonetheless be a dominant population if they were to acquire growth or survival advantages by compensating organ dysfunction [71]. However, an experiment involving transplantation of human hepatocytes into Fah-deficient mice revealed that the majority of repopulated hepatocytes were purely of human origin that had not undergone fusion [66]. With respect to the therapeutic potential for BM-derived stem cells, studies have shown that the plasticity of these cells allows conversion to liver cells without fusion [72, 73]. More recently, fusion-derived polyploidy hepatocytes are suggested not to be predisposed to convert phenotypes but instead give rise to the genetic variations that form the broad background of hepatocyte ploidy variations in the liver [74,75,76]. Although these studies provided substantial information on how extrahepatic cellular resources integrate into damaged liver tissue under extreme situations, these findings may not be immediately relevant for patients with potentially curable liver diseases. Thus, investigation of clinically applicable models using retrospective human materials is needed in order for clinical applications to be realistic.
To investigate whether fusion plays a role in Muse cell integration into the injured liver, we performed a FISH experiment in the Muse-transplanted hepatectomy model [3]. Using serial sections of liver samples adjacent to the transection line, we could approximate protein expression and genotyping at the cellular level. This combinational technique allowed us to examine whether GFP-labeled Muse cells that express liver markers also carry mouse chromosome markers that are indicative of fusion. Interestingly, at day 2 post-PPHx, CK19-expressing Muse cells (i.e., cholangiocytes) possessed only human chromosomes, whereas other GFP-negative CK19-expressing cells (presumably endogenous mouse cholangiocytes participating in liver regeneration) possessed only mouse chromosomes (Fig. 12.7A). This finding seems to suggest that fusion does not occur, at least immediately, in response to liver injury. Subsequent follow-up FISH analysis at 4 weeks post-PPHx revealed that a small percentage (1.9%) of hepatocytes derived from Muse cells showed mouse chromosomes, suggesting that fusion is an infrequent event (Fig. 12.7B). Our quantitative analysis of hepatocyte-differentiated Muse cells counted 74.3% of all integrated Muse cells, again suggesting that the fraction of cells that underwent fusion during liver regeneration was extremely small.
Muse cell marker expression following transplantation. (A) Two days posttransplantation with human GFP-positive Muse cells, *1 cell is positive for GFP/CK19 and possesses only human chromosomes, where *2-*8 cells are negative for both GFP and CK19 and possess only mouse chromosomes. (B) At 4 weeks after transplantation of human GFP-positive Muse cells, among cells positive for both GFP and HepPar-1, *1 and *2 cells possess only human chromosomes, whereas *4 cell has both human and mouse chromosomes, *3 cell that has only human chromosomes is not reflected in the GFP/HepPar-1 section, and the *5 cell is negative for both GFP and HepPar-1 and has only mouse chromosomes. Mouse and human chromosomes are indicated by green and red signals, respectively. Scale bar, 20 μm. (The data are reproduced from Katagiri et al. [3])
We also used FISH to investigate the possibility of fusion in humans in long-term liver regeneration using sex-mismatched (female-to-male) LDLT patient samples [21]. Liver grafts from these cases exhibited chimerism at the tissue level, indicating that extrahepatic cells differentiated into liver components. There were no cells that showed evidence of cell fusion between endogenous liver component cells and extrahepatic cells. Polyploid cells were present, but they all carried only X chromosomes (i.e., derived from only the donor liver). Interestingly, cholangiocytes carrying Y chromosomes were more frequent than other cell types, suggesting that extrahepatic cells were integrated with preference during bile duct formation. This finding, together with that for AFP+/CK19+ double-positive cholangiocytes, could imply that extrahepatic cells contribute to liver regeneration via progenitor cells. Thus, we conclude that fusion is unlikely to be a predominant mechanism in liver regeneration, and extrahepatic cells, particularly cholangiocytes, substantially contribute to the formation of liver structures as multipotent LPCs.
12.7 Potential of Muse Cells for Treating Liver Disease
Cellular transplantation of extrahepatic origin (including hepatocyte transplantation) has provided evidence that cellular support is somewhat effective for treating liver disease [45]. Development of such approaches would have higher priority if the mechanism associated with cellular integration was fully elucidated and the method efficacy was guaranteed. Our study showed that the closer the injury front, Muse cells could preferentially accumulated to the damaged site. The finding that more than 70% of the integrated Muse cells in the injury front differentiated spontaneously into hepatocytes would support that this approach could have high therapeutic efficacy.
Similar to other stem cell resources, techniques to enrich Muse cell populations from BM-MSCs or, more practically, from BM cells are needed. Indeed, Muse cells represent only 2–3% of the BM-MSC population, meaning that a large number of BM cells are required to obtain Muse cells for treatment. Nonetheless, the high efficacy achieved by this approach implied that cell transplantation has good therapeutic potential. In practice, administration of Muse cells should be performed through the portal vein in patients who undergo hepatectomy. The challenge for therapeutic use of Muse cells is illustrated by the suggestion that “hepatocyte transplantation” for engraftment of extrahepatic cells to a damaged liver would require 2.5% of the entire liver weight [9].
Another important issue is what kind of liver diseases are indicated for cell therapy with Muse cells. The liver failure involved in our PPHx model was a local injury. In this model, Muse cells proliferated selectively at the liver transection line in the early time period after integration, but whether such proliferation would occur for other types of injuries, or in various liver diseases, remains to be clarified. Thus, potential applications of Muse cells for other liver diseases should be identified.
12.8 The Origin of Liver Stem Cells
The LDLT genotyping suggested that extrahepatic cells capable of differentiating into multiple cells could contribute in part to liver regeneration. However, the identity of these cells, how they initiate regenerative processes, and from where they ultimately originated in the liver microenvironment remains unclear. Under physiological conditions, new hepatocytes were shown to arise by simple replication from a small portion of existing hepatocytes during homeostatic renewal of the liver [77,78,79] (Fig. 12.8A). In contrast, in situations involving severe injury, such as fulminant hepatic failure [80], chronic viral hepatitis [81], alcoholic hepatitis [82], or murine PPHx induced with a harmonic scalpel [44], cells with intermediate hepatocyte-cholangiocyte phenotypes emerge and expand in the liver parenchyma [44, 80,81,82,83,84]. These cell populations are referred to by various terms, including “ductular hepatocytes,” “atypical ductal cells,” “intermediate hepatobiliary cells,” or perhaps the most frequently called “LPCs” [85] (Fig. 12.8B). In rodent models, such cells were historically known as “oval cells,” a term first coined by Farber et al. to describe non-parenchymal cells in the periportal region that could be observed after 2-acetylaminofluorene treatment followed by two-thirds partial hepatectomy (2-AAF/PH) in rats [86, 87]. After 2-AAF/PH, oval cells in rat models are induced, whereas in mouse models the oval cell equivalent emerged more effectively following treatment with 3,5-diethoxycarbonyl-1,4-dihydrocollidine (known as DDC) or feeding of a choline-deficient, ethionine-supplemented (CDE) diet [88, 89]. The emergence of oval cells in the portal field suggests that these cells originated in the terminal branches of the intrahepatic biliary system, the Canals of Hering [90], and then expanded into the parenchyma to form duct-like structures known as “ductular reactions” [44, 91]. Indeed, an extended biliary duct remodeling has been shown for liver regeneration in response to various liver injuries because it provides a niche for LPCs [92]. In periportal area, Thy1+ cells have been shown to constitute the niche for LPCs by producing FGF7 that can regulate the spread of LPCs [93].
Stem cells for liver regeneration. (A) Under physiological conditions, both new hepatocytes and cholangiocytes arise by simple replication from a small portion of existing hepatocytes and cholangiocyte, respectively, during the homeostatic renewal of the liver. (B) Upon severe liver injury, “liver progenitor cells (LPCs),” which have an intermediate hepatocyte-cholangiocyte phenotype, emerge and differentiate into new hepatocytes and cholangiocytes to compensate for the damaged tissues. (C) Muse cells can be mobilized upon liver injury from peripheral blood, bone marrow, and connective tissues. The mobilized Muse cells differentiate into liver component cells, including hepatocytes, cholangiocytes, and sinusoidal cells. Note that Muse cells differentiate into hepatocytes or cholangiocytes via “LPC”-like cells, whereas Muse cells can directly differentiate into sinusoidal endothelial cells. CoH Canals of Hering
Using inducible Cre recombinase, Furuyama et al. demonstrated that hepatocyte differentiation could be activated almost exclusively by “Sox9-positive precursors” in the duct during liver regeneration induced by carbon tetrachloride or bile duct ligation [62]. These Sox9-positive cells afforded near-complete turnover of hepatocyte mass within 6 months. Whereas these Sox9-positive cells can be considered as LPCs, their terminal differentiation into functional hepatocytes is dependent on the degree of liver damage and composition of the neighboring extracellular matrix [94]. These observations suggest that when severe injuries cannot be repaired by simple replication of existing hepatocytes, extrahepatic cells can play a role in liver regeneration. Thus, our observation that donor and recipient genotypes were mixed in LDLT grafts might be an indicator of the degree of operational invasiveness of the liver injury [3]. Recently, Raven et al. demonstrated that loss of β1-integrin in hepatocytes with liver injury induced a ductular reaction wherein 25% of cells had a non-hepatocyte derivation. In contrast, inhibition of hepatocyte proliferation by β1-integrin knockdown and p21 overexpression induced dominant proliferation of cholangiocyte-derived hepatocytes. Although these data were from short-term injury mouse models and may not be immediately applicable to humans, we do note that in LDLT cholangiocytes exhibited the highest frequency of extrahepatic (i.e., recipient) genotypes.
If extrahepatic cells do play a role in liver regeneration, then an intriguing question is what extrahepatic cell types participate. Katsuda et al. reported a new approach to generate LPCs that involved incubating mature hepatocytes ex vivo with three combinations of compounds to produce chemically induced liver progenitor cells (CLiPs) that can proliferate, differentiate, and form ductal structures [95]. The CLiPs study revealed that diploid hepatocytes that represent a minor fraction of mature hepatocytes become dominant during CLiP selection, suggesting that diploid cells are the major source for CLiPs. Since aneuploidy is a common characteristic of mature hepatocytes, the fact that diploid cells could play a major role in potential hepatocyte replacement led us to consider whether extrahepatic stem cells are a source for LPCs. Diploid stem cells, particularly HSCs, MSCs, or other stem cells, may be delivered via the blood stream from other normal tissues. In this situation, some dedicated cell fractions in the blood should increase in response to physical stress. Supporting this hypothesis, increased numbers of Muse cells were observed within 24 h after ischemic stroke of the brain and acute myocardial infarction (AMI) [54, 55]. Although ischemic stroke or AMI may not directly damage the liver, these studies indicate that in response to physical stress, the numbers of diploid Muse cells increase, as does the likelihood that these cells will localize in a damaged area where they could aid differentiation of diploid cells into needed cell types. Our genotyping of LDLT showing diploid cell-dominant potential for LPCs and circulating Muse cells in stressed conditions strongly supports the possibility that extrahepatic Muse cells are an important resource for liver regeneration (Fig. 12.8C).
12.9 Conclusion
Following transplantation of Muse cells into mice with damaged livers, only Muse cells contributed to liver regeneration. Although several issues, including enrichment method, administration pathway, and recommended indications, must be addressed before clinical application, Muse cells may be a practical candidate for cell therapy for a wide range of liver diseases.
References
Itoh T, Miyajima A (2014) Liver regeneration by stem/progenitor cells. Hepatology 59(4):1617–1626
Miyaoka Y, Ebato K, Kato H, Arakawa S, Shimizu S, Miyajima A (2012) Hypertrophy and unconventional cell division of hepatocytes underlie liver regeneration. Curr Biol 22(13):1166–1175
Katagiri H, Kushida Y, Nojima M, Kuroda Y, Wakao S, Ishida K et al (2016) A distinct subpopulation of bone marrow mesenchymal stem cells, muse cells, directly commit to the replacement of liver components. Am J Transplant 16(2):468–483
Liang TJ, Ghany MG (2013) Current and future therapies for hepatitis C virus infection. N Engl J Med 368(20):1907–1917
Rinella ME (2015) Nonalcoholic fatty liver disease: a systematic review. JAMA 313(22):2263–2273
Breitenstein S, Dimitroulis D, Petrowsky H, Puhan MA, Mullhaupt B, Clavien PA (2009) Systematic review and meta-analysis of interferon after curative treatment of hepatocellular carcinoma in patients with viral hepatitis. Br J Surg 96(9):975–981
Mitry RR, Hughes RD, Dhawan A (2011) Hepatocyte transplantation. J Clin Exp Hepatol 1(2):109–114
Dhawan A, Puppi J, Hughes RD, Mitry RR (2010) Human hepatocyte transplantation: current experience and future challenges. Nat Rev Gastroenterol Hepatol 7(5):288–298
Fox IJ, Chowdhury JR, Kaufman SS, Goertzen TC, Chowdhury NR, Warkentin PI et al (1998) Treatment of the Crigler-Najjar syndrome type I with hepatocyte transplantation. N Engl J Med 338(20):1422–1426
Muraca M, Gerunda G, Neri D, Vilei MT, Granato A, Feltracco P et al (2002) Hepatocyte transplantation as a treatment for glycogen storage disease type 1a. Lancet 359(9303):317–318
Forbes SJ, Gupta S, Dhawan A (2015) Cell therapy for liver disease: from liver transplantation to cell factory. J Hepatol 62(1 Suppl):S157–S169
Pontikoglou C, Deschaseaux F, Sensebe L, Papadaki HA (2011) Bone marrow mesenchymal stem cells: biological properties and their role in hematopoiesis and hematopoietic stem cell transplantation. Stem Cell Rev 7(3):569–589
Prockop DJ, Brenner M, Fibbe WE, Horwitz E, Le Blanc K, Phinney DG et al (2010) Defining the risks of mesenchymal stromal cell therapy. Cytotherapy 12(5):576–578
Tautenhahn HM, Bruckner S, Baumann S, Winkler S, Otto W, von Bergen M et al (2016) Attenuation of postoperative acute liver failure by mesenchymal stem cell treatment due to metabolic implications. Ann Surg 263(3):546–556
Chamberlain G, Fox J, Ashton B, Middleton J (2007) Concise review: mesenchymal stem cells: their phenotype, differentiation capacity, immunological features, and potential for homing. Stem Cells 25(11):2739–2749
Kuroda Y, Kitada M, Wakao S, Nishikawa K, Tanimura Y, Makinoshima H et al (2010) Unique multipotent cells in adult human mesenchymal cell populations. Proc Natl Acad Sci USA 107(19):8639–8643
Chiu KW, Nakano T, Chen KD, Hsu LW, Lai CY, Chiu HC et al (2013) Homogeneous phenomenon of the graft when using different genotype characteristic of recipients/donors in living donor liver transplantation. World J Hepatol 5(11):642–648
Chiu KW, Nakano T, Chen KD, Lai CY, Hsu LW, Chiu HC et al (2013) Pyrosequencing to identify homogeneous phenomenon when using recipients/donors with different CYP3A5*3 genotypes in living donor liver transplantation. PLoS One 8(8):e71314
Hove WR, van Hoek B, Bajema IM, Ringers J, van Krieken JH, Lagaaij EL (2003) Extensive chimerism in liver transplants: vascular endothelium, bile duct epithelium, and hepatocytes. Liver Transpl 9(6):552–556
Kleeberger W, Rothamel T, Glockner S, Flemming P, Lehmann U, Kreipe H (2002) High frequency of epithelial chimerism in liver transplants demonstrated by microdissection and STR-analysis. Hepatology 35(1):110–116
Ng IO, Chan KL, Shek WH, Lee JM, Fong DY, Lo CM et al (2003) High frequency of chimerism in transplanted livers. Hepatology 38(4):989–998
Makuuchi M (2013) Surgical treatment for HCC–special reference to anatomical resection. Int J Surg 11(Suppl 1):S47–S49
Hasegawa Y, Nitta H, Sasaki A, Takahara T, Itabashi H, Katagiri H et al (2015) Long-term outcomes of laparoscopic versus open liver resection for liver metastases from colorectal cancer: a comparative analysis of 168 consecutive cases at a single center. Surgery 157(6):1065–1072
Page AJ, Weiss MJ, Pawlik TM (2014) Surgical management of noncolorectal cancer liver metastases. Cancer 120(20):3111–3121
Roll GR, Parekh JR, Parker WF, Siegler M, Pomfret EA, Ascher NL et al (2013) Left hepatectomy versus right hepatectomy for living donor liver transplantation: shifting the risk from the donor to the recipient. Liver Transpl 19(5):472–481
Takahara T, Wakabayashi G, Hasegawa Y, Nitta H (2015) Minimally invasive donor hepatectomy: evolution from hybrid to pure laparoscopic techniques. Ann Surg 261(1):e3–e4
Akamatsu N, Sugawara Y, Nagata R, Kaneko J, Aoki T, Sakamoto Y et al (2014) Adult right living-donor liver transplantation with special reference to reconstruction of the middle hepatic vein. Am J Transplant 14(12):2777–2787
Duclos J, Bhangui P, Salloum C, Andreani P, Saliba F, Ichai P et al (2016) Ad Integrum functional and volumetric recovery in right lobe living donors: is it really complete 1 year after donor hepatectomy? Am J Transplant 16(1):143–156
Kogure K, Ishizaki M, Nemoto M, Kuwano H, Makuuchi M (1999) A comparative study of the anatomy of rat and human livers. J Hepato-Biliary-Pancreat Surg 6(2):171–175
Malarkey DE, Johnson K, Ryan L, Boorman G, Maronpot RR (2005) New insights into functional aspects of liver morphology. Toxicol Pathol 33(1):27–34
Hori T, Ohashi N, Chen F, Baine AM, Gardner LB, Jermanus S et al (2011) Simple and sure methodology for massive hepatectomy in the mouse. Ann Gastroenterol 24(4):307–318
Mitchell C, Willenbring H (2008) A reproducible and well-tolerated method for 2/3 partial hepatectomy in mice. Nat Protoc 3(7):1167–1170
Song GW, Lee SG (2014) Living donor liver transplantation. Curr Opin Organ Transplant 19(3):217–222
Brown RS Jr (2008) Pros and cons of living donor liver transplant. Gastroenterol Hepatol (N Y) 4(9):622–624
Katagiri HNS, Nitta H, Wakabayashi G (2014) Potential involvement of extrahepatic cells in liver regeneration. J Iwate Med Assoc 66(2):67–74
Haga J, Shimazu M, Wakabayashi G, Tanabe M, Kawachi S, Fuchimoto Y et al (2008) Liver regeneration in donors and adult recipients after living donor liver transplantation. Liver Transpl 14(12):1718–1724
Ibrahim S, Chen CL, Wang CC, Wang SH, Lin CC, Liu YW et al (2005) Liver regeneration and splenic enlargement in donors after living-donor liver transplantation. World J Surg 29(12):1658–1666
Kato Y, Shimazu M, Wakabayashi G, Tanabe M, Morikawa Y, Hoshino K et al (2001) Significance of portal venous flow in graft regeneration after living related liver transplantation. Transplant Proc 33(1–2):1484–1485
Kido M, Ku Y, Fukumoto T, Tominaga M, Iwasaki T, Ogata S et al (2003) Significant role of middle hepatic vein in remnant liver regeneration of right-lobe living donors. Transplantation 75(9):1598–1600
Michalopoulos GK, DeFrances MC (1997) Liver regeneration. Science 276(5309):60–66
Tanimizu N, Mitaka T (2014) Re-evaluation of liver stem/progenitor cells. Organogenesis 10(2):208–215
Isse K, Lesniak A, Grama K, Maier J, Specht S, Castillo-Rama M et al (2013) Preexisting epithelial diversity in normal human livers: a tissue-tethered cytometric analysis in portal/periportal epithelial cells. Hepatology 57(4):1632–1643
Schmelzle M, Duhme C, Junger W, Salhanick SD, Chen Y, Wu Y et al (2013) CD39 modulates hematopoietic stem cell recruitment and promotes liver regeneration in mice and humans after partial hepatectomy. Ann Surg 257(4):693–701
Suzuki Y, Katagiri H, Wang T, Kakisaka K, Kume K, Nishizuka SS et al (2016) Ductular reactions in the liver regeneration process with local inflammation after physical partial hepatectomy. Lab Investig J Tech Methods Pathol 96(11):1211–1222
Huebert RC, Rakela J (2014) Cellular therapy for liver disease. Mayo Clin Proc 89(3):414–424
Mitry RR, Hughes RD, Aw MM, Terry C, Mieli-Vergani G, Girlanda R et al (2003) Human hepatocyte isolation and relationship of cell viability to early graft function. Cell Transplant 12(1):69–74
Strom SC, Davila J, Grompe M (2010) Chimeric mice with humanized liver: tools for the study of drug metabolism, excretion, and toxicity. Methods Mol Biol 640:491–509
Dezawa M (2006) Insights into autotransplantation: the unexpected discovery of specific induction systems in bone marrow stromal cells. Cell Mol Life Sci 63(23):2764–2772
Ferraro F, Lymperi S, Mendez-Ferrer S, Saez B, Spencer JA, Yeap BY et al (2011) Diabetes impairs hematopoietic stem cell mobilization by altering niche function. Sci Transl Med 3(104):104ra1
Lin BL, Chen JF, Qiu WH, Wang KW, Xie DY, Chen XY et al (2017) Allogeneic bone marrow-derived mesenchymal stromal cells for hepatitis B virus-related acute-on-chronic liver failure: a randomized controlled trial. Hepatology 66(1):209–219
Suk KT, Yoon JH, Kim MY, Kim CW, Kim JK, Park H et al (2016) Transplantation with autologous bone marrow-derived mesenchymal stem cells for alcoholic cirrhosis: phase 2 trial. Hepatology 64(6):2185–2197
Wakao S, Akashi H, Kushida Y, Dezawa M (2014) Muse cells, newly found non-tumorigenic pluripotent stem cells, reside in human mesenchymal tissues. Pathol Int 64(1):1–9
Dezawa M (2016) Muse cells provide the pluripotency of mesenchymal stem cells: direct contribution of muse cells to tissue regeneration. Cell Transplant 25(5):849–861
Hori E, Hayakawa Y, Hayashi T, Hori S, Okamoto S, Shibata T et al (2016) Mobilization of pluripotent multilineage-differentiating stress-enduring cells in ischemic stroke. J Stroke Cerebrovasc Dis 25(6):1473–1481
Tanaka T, Nishigaki K, Minatoguchi S, Nawa T, Yamada Y, Kanamori H et al (2018) Mobilized muse cells after acute myocardial infarction predict cardiac function and remodeling in the chronic phase. Circ J 82(2):561–571
Wakao S, Kitada M, Dezawa M (2013) The elite and stochastic model for iPS cell generation: multilineage-differentiating stress enduring (Muse) cells are readily reprogrammable into iPS cells. Cytometry A 83(1):18–26
Wakao S, Kitada M, Kuroda Y, Shigemoto T, Matsuse D, Akashi H et al (2011) Multilineage-differentiating stress-enduring (Muse) cells are a primary source of induced pluripotent stem cells in human fibroblasts. Proc Natl Acad Sci USA 108(24):9875–9880
Dahlke MH, Popp FC, Larsen S, Schlitt HJ, Rasko JE (2004) Stem cell therapy of the liver—fusion or fiction? Liver Transpl 10(4):471–479
Grompe M, al-Dhalimy M, Finegold M, Ou CN, Burlingame T, Kennaway NG et al (1993) Loss of fumarylacetoacetate hydrolase is responsible for the neonatal hepatic dysfunction phenotype of lethal albino mice. Genes Dev 7(12A):2298–2307
Grompe M, Lindstedt S, al-Dhalimy M, Kennaway NG, Papaconstantinou J, Torres-Ramos CA et al (1995) Pharmacological correction of neonatal lethal hepatic dysfunction in a murine model of hereditary tyrosinaemia type I. Nat Genet 10(4):453–460
Grompe M, Strom S (2013) Mice with human livers. Gastroenterology 145(6):1209–1214
He Z, Zhang H, Zhang X, Xie D, Chen Y, Wangensteen KJ et al (2010) Liver xeno-repopulation with human hepatocytes in Fah-/-Rag2-/- mice after pharmacological immunosuppression. Am J Pathol 177(3):1311–1319
Huch M, Dorrell C, Boj SF, van Es JH, Li VS, van de Wetering M et al (2013) In vitro expansion of single Lgr5+ liver stem cells induced by Wnt-driven regeneration. Nature 494(7436):247–250
Li L, Zeng Z, Qi Z, Wang X, Gao X, Wei H et al (2015) Natural killer cells-produced IFN-gamma improves bone marrow-derived hepatocytes regeneration in murine liver failure model. Sci Rep 5:13687
Qi Z, Wang X, Wei H, Sun R, Tian Z (2015) Infiltrating neutrophils aggravate metabolic liver failure in fah-deficient mice. Liver Int 35(3):774–785
Azuma H, Paulk N, Ranade A, Dorrell C, Al-Dhalimy M, Ellis E et al (2007) Robust expansion of human hepatocytes in Fah-/-/Rag2-/-/Il2rg-/- mice. Nat Biotechnol 25(8):903–910
Grompe M, Overturf K, al-Dhalimy M, Finegold M (1998) Therapeutic trials in the murine model of hereditary tyrosinaemia type I: a progress report. J Inherit Metab Dis 21(5):518–531
Wang X, Willenbring H, Akkari Y, Torimaru Y, Foster M, Al-Dhalimy M et al (2003) Cell fusion is the principal source of bone-marrow-derived hepatocytes. Nature 422(6934):897–901
Vassilopoulos G, Wang PR, Russell DW (2003) Transplanted bone marrow regenerates liver by cell fusion. Nature 422(6934):901–904
Wang X, Montini E, Al-Dhalimy M, Lagasse E, Finegold M, Grompe M (2002) Kinetics of liver repopulation after bone marrow transplantation. Am J Pathol 161(2):565–574
Terada N, Hamazaki T, Oka M, Hoki M, Mastalerz DM, Nakano Y et al (2002) Bone marrow cells adopt the phenotype of other cells by spontaneous cell fusion. Nature 416(6880):542–545
Harris RG, Herzog EL, Bruscia EM, Grove JE, Van Arnam JS, Krause DS (2004) Lack of a fusion requirement for development of bone marrow-derived epithelia. Science 305(5680):90–93
Jang YY, Collector MI, Baylin SB, Diehl AM, Sharkis SJ (2004) Hematopoietic stem cells convert into liver cells within days without fusion. Nat Cell Biol 6(6):532–539
Duncan AW, Dorrell C, Grompe M (2009) Stem cells and liver regeneration. Gastroenterology 137(2):466–481
Duncan AW, Hickey RD, Paulk NK, Culberson AJ, Olson SB, Finegold MJ et al (2009) Ploidy reductions in murine fusion-derived hepatocytes. PLoS Genet 5(2):e1000385
Duncan AW, Taylor MH, Hickey RD, Hanlon Newell AE, Lenzi ML, Olson SB et al (2010) The ploidy conveyor of mature hepatocytes as a source of genetic variation. Nature 467(7316):707–710
Malato Y, Naqvi S, Schurmann N, Ng R, Wang B, Zape J et al (2011) Fate tracing of mature hepatocytes in mouse liver homeostasis and regeneration. J Clin Invest 121(12):4850–4860
Wang B, Zhao L, Fish M, Logan CY, Nusse R (2015) Self-renewing diploid Axin2(+) cells fuel homeostatic renewal of the liver. Nature 524(7564):180–185
Yanger K, Knigin D, Zong Y, Maggs L, Gu G, Akiyama H et al (2014) Adult hepatocytes are generated by self-duplication rather than stem cell differentiation. Cell Stem Cell 15(3):340–349
Demetris AJ, Seaberg EC, Wennerberg A, Ionellie J, Michalopoulos G (1996) Ductular reaction after submassive necrosis in humans. Special emphasis on analysis of ductular hepatocytes. Am J Pathol 149(2):439–448
Libbrecht L, Desmet V, Van Damme B, Roskams T (2000) Deep intralobular extension of human hepatic ‘progenitor cells’ correlates with parenchymal inflammation in chronic viral hepatitis: can ‘progenitor cells’ migrate? J Pathol 192(3):373–378
Sancho-Bru P, Altamirano J, Rodrigo-Torres D, Coll M, Millan C, Jose Lozano J et al (2012) Liver progenitor cell markers correlate with liver damage and predict short-term mortality in patients with alcoholic hepatitis. Hepatology 55(6):1931–1941
Roskams TA, Theise ND, Balabaud C, Bhagat G, Bhathal PS, Bioulac-Sage P et al (2004) Nomenclature of the finer branches of the biliary tree: canals, ductules, and ductular reactions in human livers. Hepatology 39(6):1739–1745
Turanyi E, Dezso K, Csomor J, Schaff Z, Paku S, Nagy P (2010) Immunohistochemical classification of ductular reactions in human liver. Histopathology 57(4):607–614
Miyajima A, Tanaka M, Itoh T (2014) Stem/progenitor cells in liver development, homeostasis, regeneration, and reprogramming. Cell Stem Cell 14(5):561–574
Farber E (1956) Similarities in the sequence of early histological changes induced in the liver of the rat by ethionine, 2-acetylamino-fluorene, and 3’-methyl-4-dimethylaminoazobenzene. Cancer Res 16(2):142–148
Evarts RP, Nagy P, Marsden E, Thorgeirsson SS (1987) A precursor-product relationship exists between oval cells and hepatocytes in rat liver. Carcinogenesis 8(11):1737–1740
Preisegger KH, Factor VM, Fuchsbichler A, Stumptner C, Denk H, Thorgeirsson SS (1999) Atypical ductular proliferation and its inhibition by transforming growth factor beta1 in the 3,5-diethoxycarbonyl-1,4-dihydrocollidine mouse model for chronic alcoholic liver disease. Lab Investig J Tech Methods Pathol 79(2):103–109
Akhurst B, Croager EJ, Farley-Roche CA, Ong JK, Dumble ML, Knight B et al (2001) A modified choline-deficient, ethionine-supplemented diet protocol effectively induces oval cells in mouse liver. Hepatology 34(3):519–522
Theise ND, Saxena R, Portmann BC, Thung SN, Yee H, Chiriboga L et al (1999) The canals of Hering and hepatic stem cells in humans. Hepatology 30(6):1425–1433
Roskams TA, Libbrecht L, Desmet VJ (2003) Progenitor cells in diseased human liver. Semin Liver Dis 23(4):385–396
Kaneko K, Kamimoto K, Miyajima A, Itoh T (2015) Adaptive remodeling of the biliary architecture underlies liver homeostasis. Hepatology 61(6):2056–2066
Takase HM, Itoh T, Ino S, Wang T, Koji T, Akira S et al (2013) FGF7 is a functional niche signal required for stimulation of adult liver progenitor cells that support liver regeneration. Genes Dev 27(2):169–181
Espanol-Suner R, Carpentier R, Van Hul N, Legry V, Achouri Y, Cordi S et al (2012) Liver progenitor cells yield functional hepatocytes in response to chronic liver injury in mice. Gastroenterology 143(6):1564–75.e7
Katsuda T, Kawamata M, Hagiwara K, Takahashi RU, Yamamoto Y, Camargo FD et al (2017) Conversion of terminally committed hepatocytes to culturable bipotent progenitor cells with regenerative capacity. Cell Stem Cell 20(1):41–55
Acknowledgment
This work was partially supported by a Grant-in-Aid for Scientific Research 16 K09370 (Y.T.) and 17 K10676 (H.K.); and Keiryokai Research Foundation No. 132 (Y.S.).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Japan KK, part of Springer Nature
About this chapter
Cite this chapter
Nishizuka, S.S., Suzuki, Y., Katagiri, H., Takikawa, Y. (2018). Liver Regeneration Supported by Muse Cells. In: Dezawa, M. (eds) Muse Cells. Advances in Experimental Medicine and Biology, vol 1103. Springer, Tokyo. https://doi.org/10.1007/978-4-431-56847-6_12
Download citation
DOI: https://doi.org/10.1007/978-4-431-56847-6_12
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-56845-2
Online ISBN: 978-4-431-56847-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)