Abstract
Colonoscopy is a gold standard in assessing disease severity of ulcerative colitis, and therefore efforts have been made in order to quantify the severity of inflammation by endoscopic indices. Most indices have been proposed to assess the efficacy of clinical trials, and therefore not been validated. Baron score, ulcerative colitis endoscopic index of severity (UCEIS), and ulcerative colitis colonoscopic index of severity (UCCIS) are validated. There are some scoring systems in which different factors are graded for each item separately [Baron score, Rachmilewitz score, endoscopic activity index (EAI, UCEIS and UCCIS), and others grading multiple aspects altogether (Matts’ endoscopic grading, the Mayo endoscopic subscore (MES)]. It is essential to understand both strength and weakness of each index and utilize appropriately, since different indices have been developed for different purposes. It should be also noted that none of these widely used indices takes extent of inflammation into account. Currently, MES is most widely used in clinical trials for its simplicity, and UCEIS may become more common in the future because of its lower inter-observer variability. Definition of mucosal healing in each index has not been established yet.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Endoscopy is a “gold standard” for assessing the severity of ulcerative colitis (UC), since the affected area is localized in the colon and therefore the entire diseased organ can be reached by conventional colonoscopy. The emerging concept of mucosal healing has made endoscopic evaluation more important. The evaluation includes disease extent, activity, phase, and response to the therapy. Difference in these aspects needs to be objectively stratified for the outcome measurement of clinical trials as well as directing the treatment strategy in clinical practice. There have been dozens of scoring systems proposed in the previous literature, however, many of them were developed for each specific clinical trial and then applied to other purposes. Therefore, there are only a few indices that have been appropriately validated. In this chapter, strength and weakness, clinical implication, and future direction of endoscopic indices currently used for UC are discussed.
2 Matts’ Endoscopic Grading
Matts’ endoscopic grading is one of the most conventional endoscopic indices, first described in 1961 and still used in clinical practice and clinical researches because of its simplicity [1]. In was originally developed to evaluate the significance of histological assessment of a biopsy specimen by looking at the correlation between endoscopic and histological grading systems. Its definition is focused on mucosal granularity and bleeding; however, it is not clear enough what the threshold is for distinguishing ‘mild’ granularity and bleeding from ‘marked’. Furthermore, presence of ulcers appears only in grade 4; therefore, severity of ulceration cannot be reflected in this scoring system (Table 16.1)
.
3 Baron Score
Baron JH et al. reported the first validated endoscopic index in 1964 [2]. They studied the variation between observers in describing mucosal appearances in UC, and concluded that interobserver agreement was better reached based on mucosal friability and spontaneous bleeding compared with other descriptors. Based on this finding, classification of endoscopic activity using these two factors is proposed with high interobserver agreement (Table 16.2).
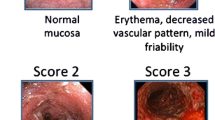
4 Mayo Endoscopic Subscore (MES)
Sutherland et al. established the Disease Activity Index using a quantitative rating scale with four variables including endoscopic mucosal appearance ranging from 0 to 3, which also utilizes friability and spontaneous bleeding [3]. A similar clinical disease activity index was defined by Schroeder et al. [4] for assessing the clinical efficacy of coated oral 5-ASA, with a more detailed description of mucosal appearance. This scoring system (called the Mayo score) is convenient for clinical trials, since it simultaneously reflects the overall clinical status as well as endoscopic mucosal appearance; however, it is of note that this endoscopic subscore itself has not been validated yet. The concept of mucosal healing is often defined as MES 0 and 1, which suggests the favorable long-term outcome (Table 16.3).
5 Rachmilewitz Score
The confusion in the indices described above is that they are graded based on multiple different aspects of mucosal appearance, such as vascular pattern, friability, bleeding, and ulceration, which are not always altered in parallel. These different factors may appear at different levels, especially in patients who are responding to therapeutic intervention. Therefore, Rachmilewitz proposed an endoscopic index in which four descriptors are independently taken into account (Table 16.4) [5].
6 Endoscopic Activity Index (EAI)
Naganuma et al. developed EAI, consisting of six descriptors so that early improvement of mucosal inflammation can be more sensitively detected [6]. It has been shown that EAI is superior to Matts’ score in differentiating responder and non-responder. Kobayashi et al. reported that decrease in EAI after 2-week intravenous cyclosporine inversely correlates to the first year colectomy, indicating that EAI is useful in stratifying early endoscopic improvement [7]. EAI is shown to have a wider range for severe cases, which may allow optimization of treatment based on severity even among patients graded identically as severe using the previous systems such as Matt’s or MES (Table 16.5).
7 Ulcerative Colitis Endoscopic Index of Severity (UCEIS) and Ulcerative Colitis Colonoscopic Index of Severity (UCCIS)
Travis SH et al. studied the intra- and inter- individual variation in ten endoscopic descriptors, and proposed UCEIS using three among them [8]. The UCEIS score incorporates vascular pattern (normal/patchy/complete obliteration), bleeding (none /mucosal/luminal mild/luminal moderate or severe), and erosions and ulcers (none/erosions/superficial/deep), each with precise definitions, which explained 90% of the variance in the overall assessment of endoscopic severity. It has been updated and validated with an independent [9] cohort of investigators, identifying it as one of the most well-validated endoscopic scores so far. One of the mechanisms helping UCEIS to avoid the variation is that each definition is very detailed, including size of the mucosal defects differentiating erosion (<5 mm) and ulcer (>5 mm).
UCCIS is another endoscopic severity index developed and validated recently. Thia et al. evaluated interobserver agreement in ten items and identified four (vascular pattern, granularity, ulcerations and bleeding–friability) as lesions demonstrating good agreements among endoscopic characteristics [10]. UCCIS was established using these four parameters and validated in a different cohort [11]. What makes UCCIS unique is that it is the only validated index that takes into account the extent of disease, and is weighted differently to each descriptor.
The other characteristics by which UCEIS and UCCIS are considered well-validated is the strong correlation with the visual analogue scale. This demonstrates that these indices well reflect the global assessment of severity by endoscopists, which might most directly prove the feasibility of these scores (Table 16.6).
8 Consideration and Clinical Implication
We should keep in mind that many of the endoscopic indices currently used are developed for measuring outcomes of clinical trials, but the primary purpose was not to establish the validated endoscopic severity index. Therefore, these indices have not been appropriately validated yet, except for Baron, UCEIS, and UCCIS. However, this does not necessarily mean that other indices are not acceptable. MES is indeed the simplest and most widely used in clinical trials, and therefore there are much more data available than for others. On the contrary, MES is not sensitive enough to detect early response with relatively small changes in some cases (e.g., the case shown in Fig. 16.1), which is also important in clinical practice. This issue arises mainly because the simplest scores such as MES were developed to define the inclusion criteria of severity of the patients recruited to the clinical trials, and/or are only sensitive enough to detect significant changes responding to the therapeutic interventions after a certain period of time. Scores grading different endoscopic items (e.g., ulcer, bleeding, friability, etc.) independently, such as EAI and UCCIS, may have solved this issue, but have become less simple, requiring more effort for endoscopists to score. So far, UCEIS is considered to be most “well-balanced” between accuracy, sensitivity, simplicity, and reproducibility. Much more clinical data are needed to make UCEIS as useful as MES in daily clinical practice.
Examples of scoring by MES, EAI, and UCEIS. a Endoscopic pictures of proximal (left) and distal (right) rectum of 35-year-old left-sided UC patients. MES, EAI, and UCEIS are 3, 11, and 6, respectively. b Endoscopic pictures of proximal (left) and distal (right) rectum of the same patient. MES, EAI, and UCEIS are 3, 14, and 7 respectively. MES is not altered, while EAI and UCEIS are higher than A because of the emergence of deep ulcers. c Endoscopic pictures of proximal (left) and distal (right) rectum 4 months after anti-TNF therapy and immunomodulator. MES, EAI, and UCEIS are 3, 10, and 6 respectively. MES is not altered, while EAI and UCEIS are lower than B. d Endoscopic pictures of proximal (left) and distal (right) rectum 10 months after continuing the treatment for a year. MES, EAI, and UCEIS are 1, 1, and 1 respectively
Simpler scores such as Matts’ and MES define the severity grades by multiple factors that are not always altered in parallel, especially in patients who is on the course of treatment. Furthermore, there could be a wide range of “severe” cases graded by these scores (e.g., any patients who have any ulcers should be scored as 3, since the definition only requires the presence but not the number or severity of ulceration). This lowers the potential ability to optimize the treatment options among severe cases, and the ability to detect the early response to treatment. Rachmilewitz, EAI, UCCIS, and UCEIS are theoretically expected to solve these disadvantages; however, these scores require more effort by the endoscopists than MES and other simpler scores, since there are more independent descriptors in the recent indices. An example of scoring by different systems is shown in Fig. 16.1.
There is also a discussion whether extent of disease should be included in the indices of endoscopic disease severity, especially because it is well known that extensive colitis is known to be an independent risk factor for colectomy [12, 13]. Therefore, patients with extensive colitis may need to be graded more severely compared with distally limited colitis; however, extent of disease is taken into account only in UCCIS among the indices described above. On the other hand, calculating sum of severity score from each segment of the colon makes the scoring process significantly more complicated. A list of strengths and weaknesses of each scoring system is summarized in Table 16.7.
What is the ideal index and what is the reality? There is no gold standard yet. In general, more complicated indices tend to be more sensitive to the alteration of severity. The most well-balanced score with an appropriate validation might be UCEIS; however, its feasibility in clinical trials as well as in daily clinical practice is still unknown. The current reality might be to learn the etiology of how each index was developed, and try to choose the right scoring system for the right purpose accordingly.
References
Matts SG. The value of rectal biopsy in the diagnosis of ulcerative colitis. Q J Med. 1961;30:393–407.
Baron JH, Connell AM, Lennard-Jones JE. Variation between observers in describing mucosal appearances in proctocolitis. Br Med J. 1964;1(5375):89–92.
Sutherland LR, Martin F, Greer S, Robinson M, Greenberger N, Saibil F, Martin T, Sparr J, Prokipchuk E, Borgen L. 5-aminosalicylic acid enema in the treatment of distal ulcerative colitis, proctosigmoiditis, and proctitis. Gastroenterology. 1987;92(6):1894–8.
Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987;317(26):1625–9. doi:10.1056/NEJM198712243172603.
Rachmilewitz D. Coated mesalazine (5-aminosalicylic acid) versus sulphasalazine in the treatment of active ulcerative colitis: a randomised trial. BMJ. 1989;298(6666):82–6.
Naganuma M, Ichikawa H, Inoue N, Kobayashi T, Okamoto S, Hisamatsu T, Kanai T, Ogata H, Iwao Y, Hibi T. Novel endoscopic activity index is useful for choosing treatment in severe active ulcerative colitis patients. J Gastroenterol. 2010;45(9):936–43. doi:10.1007/s00535-010-0244-2.
Kobayashi T, Naganuma M, Okamoto S, Hisamatsu T, Inoue N, Ichikawa H, Takayama T, Saito R, Sujino T, Ogata H, Iwao Y, Hibi T. Rapid endoscopic improvement is important for 1-year avoidance of colectomy but not for the long-term prognosis in cyclosporine a treatment for ulcerative colitis. J Gastroenterol. 2010;45(11):1129–37. doi:10.1007/s00535-010-0273-x.
Travis SP, Schnell D, Krzeski P, Abreu MT, Altman DG, Colombel JF, Feagan BG, Hanauer SB, Lemann M, Lichtenstein GR, Marteau PR, Reinisch W, Sands BE, Yacyshyn BR, Bernhardt CA, Mary JY, Sandborn WJ. Developing an instrument to assess the endoscopic severity of ulcerative colitis: the ulcerative colitis endoscopic index of severity (UCEIS). Gut. 2012;61(4):535–42. doi:10.1136/gutjnl-2011-300486.
Travis SP, Schnell D, Krzeski P, Abreu MT, Altman DG, Colombel JF, Feagan BG, Hanauer SB, Lichtenstein GR, Marteau PR, Reinisch W, Sands BE, Yacyshyn BR, Schnell P, Bernhardt CA, Mary JY, Sandborn WJ. Reliability and initial validation of the ulcerative colitis endoscopic index of severity. Gastroenterology. 2013;145(5):987–95. doi:10.1053/j.gastro.2013.07.024.
Thia KT, Loftus Jr EV, Pardi DS, Kane SV, Faubion WA, Tremaine WJ, Schroeder KW, Harmsen SW, Zinsmeister AR, Sandborn WJ. Measurement of disease activity in ulcerative colitis: interobserver agreement and predictors of severity. Inflamm Bowel Dis. 2011;17(6):1257–64. doi:10.1002/ibd.21480.
Samuel S, Bruining DH, Loftus Jr EV, Thia KT, Schroeder KW, Tremaine WJ, Faubion WA, Kane SV, Pardi DS, de Groen PC, Harmsen WS, Zinsmeister AR, Sandborn WJ. Validation of the ulcerative colitis colonoscopic index of severity and its correlation with disease activity measures. Clin Gastroenterol Hepatol. 2013;11(1):49–54. e41 doi:10.1016/j.cgh.2012.08.003.
Gower-Rousseau C, Dauchet L, Vernier-Massouille G, Tilloy E, Brazier F, Merle V, Dupas JL, Savoye G, Balde M, Marti R, Lerebours E, Cortot A, Salomez JL, Turck D, Colombel JF. The natural history of pediatric ulcerative colitis: a population-based cohort study. Am J Gastroenterol. 2009;104(8):2080–8. doi:10.1038/ajg.2009.177.
Romberg-Camps MJ, Dagnelie PC, Kester AD, Hesselink-van de Kruijs MA, Cilissen M, Engels LG, Van Deursen C, Hameeteman WH, Wolters FL, Russel MG, Stockbrugger RW. Influence of phenotype at diagnosis and of other potential prognostic factors on the course of inflammatory bowel disease. Am J Gastroenterol. 2009;104(2):371–83. doi:10.1038/ajg.2008.38.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Japan
About this chapter
Cite this chapter
Kobayashi, T. (2018). Endoscopic Indices for Ulcerative Colitis. In: Hibi, T., Hisamatsu, T., Kobayashi, T. (eds) Advances in Endoscopy in Inflammatory Bowel Disease. Springer, Tokyo. https://doi.org/10.1007/978-4-431-56018-0_16
Download citation
DOI: https://doi.org/10.1007/978-4-431-56018-0_16
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-56016-6
Online ISBN: 978-4-431-56018-0
eBook Packages: MedicineMedicine (R0)