Abstract
Neuroblastoma is unique in its biological heterogeneity. As a result, it is crucial that the therapies selected for its treatment are appropriate according to the patient’s classification based on several risk factors, including the patient’s age, staging, and the grade of the tumor’s biological malignancy. Surgery is one of the key options in the multidisciplinary therapies, with surgeries for neuroblastoma classified into three categories: radical primary resection, open biopsy, and radical second-look operations. It is necessary to select the appropriate surgery on an individual basis. Recently, the Japan Neuroblastoma Study Group (JNBSG) has been performing clinical studies using a classification system that includes three risk groups (low, intermediate, and high) based on the risk classifications of the Children’s Oncology Group (COG). The surgical guidelines combine the low and intermediate groups to create two groups of patients: the low- and intermediate-risk group and the high-risk group.
The figures in this chapter are reprinted with permission from Standard Pediatric Operative Surgery (in Japanese), Medical View Co., Ltd., 2013, with the exception of occasional newly added figures that may appear.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Neuroblastoma
- International Neuroblastoma Risk Group (INRG)
- Image-defined risk factors (IDRFs)
- Japan Neuroblastoma Study Group (JNBSG)
1 Preoperative Management
1.1 Low- and Intermediate-Risk Neuroblastoma
As a clinical staging system for neuroblastoma, the International Neuroblastoma Staging System (INSS), which is a postsurgical staging system, has been used in Japan for decades. Recently, a pretreatment staging system based on clinical criteria and pretreatment images has been developed into the new International Neuroblastoma Risk Group (INRG) staging system (Table 60.1) [1]. In this system, the image-defined risk factors (IDRFs) are used to evaluate the surgical risk for each patient and to determine the appropriate surgical procedures, such as whether to perform either resection or biopsy as a primary procedure. Pretreatment images (contrast CT or MRI) are analyzed to identify the presence or absence of IDRFs. It is recommended that radiological specialists analyze the images.
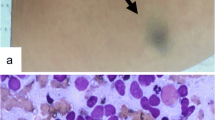
Images of each primary tumor are investigated for the existence of IDRFs. The tumors with at least one positive IDRF are defined as IDRF positive. Vessel factors are the most important risk factors in this system, with arteries that are “encased” in a tumor being defined as IDRF positive. The IDRF evaluation criteria for “contact” and “encasement” are illustrated in Figs. 60.1 and 60.2 [2].
A schematic illustration of the IDRF evaluation. Regarding the arteries, in cases where a vessel is completely surrounded by the tumor (total encasement), or more than half of the circumference of the vessel is surrounded by the tumor (contact ≧ 50 %), the vessel is considered to be “encased,” and the patient is considered to be IDRF positive. Vessel “contact” is defined by the surrounding of less than half of the artery circumference by the tumor; such cases are considered to be IDRF negative. In the case of veins, “encased” means the complete compression of the vessel with no visible lumen. “Contact” means that the lumen is visible and that case is IDRF negative
1.2 Guideline for Radical Primary Resection (for Localized Neuroblastoma)
In IDRF-negative cases, the localized tumor should be resected completely in the primary surgery, regardless of the origin, with the preservation of the adjacent organs. Lymph nodes involved in the tumor should be resected en bloc. However, in cases where the damage of the surrounding organs or major vessels is inevitable in the complete resection of the primary tumor, only an open biopsy should be performed, even if the patient has been evaluated as IDRF negative.
1.3 Guideline for Open Tumor Biopsy
A tumor biopsy should be performed safely and properly to obtain a sample of sufficient size for both the pathological diagnosis and the biological analysis of the tumor. A tissue sample of at least 1 cm2 in area is required for a precise diagnosis; thus, a needle biopsy is not recommended under this guideline.
It is recommended that the biopsy specimen be taken from the primary tumor. However, lymph nodes with obvious metastases are another option. In the cases where gross heterogenic regions are observed in one tumor, samples should be obtained from each region. Tumor tissue may be necrotic in the center; thus, the sample tissue should be resected sharply (avoiding compression), immediately under the tumor capsule.
Laparoscopic or thoracoscopic approaches might be considered for tumor biopsy since they are less invasive than an open biopsy. At present, there is insufficient evidence to support the recommendation of laparoscopic or thoracoscopic procedure for neuroblastoma biopsy.
1.4 High-Risk Neuroblastoma
For high-risk neuroblastoma, a tumor biopsy should be performed first, and a radical tumor resection should be performed after chemotherapy as a second-look operation. According to the JNBSG’s clinical study protocols for high-risk neuroblastomas, a radical operation should be performed as a delayed local therapy after the administration of high-dose chemotherapy. The patient is supposed to have a neutrophil count of more than 500/m3, and it is necessary to ensure that the conditions of the patient’s major organs (the heart, lung, liver, and kidneys) will tolerate general anesthesia. It is important to discuss the possible necessity of blood transfusions with anesthesiologists before surgery in order to maintain the patient in an appropriate condition for the surgery. Furthermore, we recommend preparing not only red cell concentrates but also platelet concentrates and fresh frozen plasma for transfusion during the surgery. The impairment of bone marrow function in patients who have undergone intensive chemotherapy must be taken into consideration. As a consequence, the patient’s recovery from a massive hemorrhage during surgery would be delayed in comparison to other surgical patients.
2 Points for Radical Surgery: Resection of the Primary Tumor
Organs surrounding the tumor must be preserved during the resection of the primary tumor regardless of its region. If possible, the lymph nodes involved in the tumor should be resected en bloc.
2.1 Tumors of Adrenal Gland or Retroperitoneal Origin
When the active invasion of the tumor into the kidney or the liver is observed during the surgery, the organs are partially resected together with the tumor. Renal function should be preserved to the extent that is possible. When the renal vessels are involved in the tumor and are difficult to detach from the tumor, the tumor capsule should be incised and the tumor should be resected to the extent that is possible. The renal blood flow should be preserved, and a nephrectomy should be avoided. When spasms of the renal vessels occur during surgery, the vessels should be wrapped in a piece of gauze soaked in Xylocaine, and the procedure should be continued with the maximum effort made to preserve the renal function. When the total resection of the tumor is impossible, even with renal resection, priority should be given to the preservation of renal function, while the tumor is resected to the extent that is possible. In the case that some of the major arteries from the abdominal aorta (such as the celiac or superior mesenteric artery) are involved in the tumor and are difficult to detach, the vessels should be preserved and the tumor should be resected to the extent that is possible, with an incision into the capsule. When a direct invasion into the spleen or splenic vessels is observed, a splenectomy should be considered together with the tumor resection for patients older than 5 years of age. In younger patients, the tumor should be resected to the extent that is possible while avoiding damage to the spleen.
2.2 Mediastinal Tumors
In cases where the tumor shows a dumbbell form, the nerve root should be resected at the level of the intervertebral foramen, avoiding the complication of the nervous systems. In principle, the resections of the vertebral arch or of tumors of retroperitoneal origin are not performed. However, in cases where the symptoms of spinal cord compression appear and it is possible to perform surgery within 72 h of the onset of symptoms, the resection of the tumor in the vertebral canal is allowed. In the case of an active invasion, the diaphragm should be resected. Otherwise, the diaphragm should be preserved to the extent that is possible.
2.3 Cervical Tumors
In the resection of tumors, damage to the major vessels such as the cervical artery or subclavian vein, and major nerves should be avoided. Tracheoplasty should be avoided during the tumor resection. Partial resection of the thyroid gland is performed in cases where active tumor invasion is found.
2.4 Presacral Tumors
Attention must be paid to preserving the nerve roots. Damage to the major vessels such as the intra- and extra-iliac arteries should be avoided in the resection of the tumor.
3 Radical Tumor Resection for Left Adrenal Neuroblastomas
An incision is made on the left upper abdomen (Fig. 60.3), with a Kent retractor helping to secure the operation field (Fig. 60.4).
Incising the peritoneum lateral to the descending colon and left colonic flexure, the tumor above the left kidney is exposed by mobilizing the descending colon to the right (Fig. 60.5). At this point, attention must be paid to avoid damage to the mesenteric vessels of the colon. If the colonic mesentery is damaged, it should be repaired before the abdomen is closed. In cases where it is difficult to identify the tumor border to the posterior side of the pancreas and to the splenic vein, the splenorenal ligament and splenodiaphragmatic ligament are dissected to expose the tumor, after which the organs may be mobilized to the right to remarkably improve the operation field. If it is possible to release the tumor adhesion from the kidney or renal vessels, the kidney should be reserved and the tumor should be dissected between the tumor capsule and the retroperitoneum by electrocoagulation (if it is difficult to achieve a complete tumor resection without damage to the kidney, a nephrectomy should be performed only in cases where it is possible to achieve the complete resection of the tumor).
For the resection, the tumor is approached from the top, bottom, and behind, mobilizing to the anterior and interior sides of the body (Fig. 60.6).
There are feeding blood vessels from the abdominal aorta, inferior diaphragmatic artery, renal artery, inferior vena cava, renal vein, and inferior diaphragmatic vein to the interior side of the tumor. They should be ligated and repeatedly dissected. In cases where the tumor edge is close to the renal hiatus, the dissection must be performed quite gently. It is also effective to spray a chemical such as papaverine to prevent the vessel spasm (surgeons should be especially careful in cases of right adrenal neuroblastoma, where the tumor is attached to the inferior vena cava, as the distance between the feeding vessels and the inferior vena cava is short). After all of the vessels are ligated and divided, the tumor should be removed with the surrounding fatty tissue (Fig. 60.7).
Systematic lymph node dissection is not ordinarily required; however, the lymph nodes surrounding the tumor should be dissected en bloc. Any obvious metastatic lymph nodes or lymph nodes of larger than 2 cm in size should also be dissected. When lymph node metastases are recognized in the pretreatment images, they should be dissected for sampling during the surgery. Chylous ascites sometimes occurs after surgery. Thus, care must be taken during the dissection of lymph nodes. The placement of metal clips which do not influence MRI examination at the top and the bottom of sampling site would be useful for the subsequent radiation therapy.
Drains must be placed in preparation for postoperative hemorrhage and chylous ascites after dissection of lymph nodes around the abdominal aorta.
As a precaution, an adhesion barrier film (Seprafilm®) should be placed under the surgical scar to prevent of adhesive ileus after surgery. The abdominal wall is then closed in layers with absorbable sutures.
4 Points of Postoperative Management
4.1 Infection Control
Neuroblastoma patients are expected to be at a high risk of general infection because of their low neutrophil count. The proper choice of antibiotics, based on the preoperative monitoring of bacterial cultures, is necessary, and the route of administration and the duration of antibiotic therapy should be carefully planned. When any symptoms of infection arise, gamma globulin should be administered without hesitation. For infection control while the bone marrow function is impaired, the infection control tactics must be planned in discussions between pediatric surgeons and pediatric oncologists.
4.2 Hemostasis and Coagulation
A decrease in the patient’s platelet transfused pre- and perioperative transfusion time is an indicator of a hemorrhage. Hemorrhages occur at the operation site; however, there is also a risk of intestinal, brain, and tracheal hemorrhage. It is necessary to monitor the patient’s hemostasis and coagulation and to perform platelet and fresh frozen plasma transfusions as appropriate.
4.3 Management of Ascites
Massive ascites may occur after surgery. Proper liquid infusion and blood transfusion are necessary to maintain the renal blood flow in patients with renal malfunction or reduced renal capacity. The retrograde contamination of the drainage tube can easily occur in these patients due to their impaired immune function.
4.4 Scar Management
When long-term chemotherapy and high-dose chemotherapy influence the patient’s nutritional status, wound healing will often be retarded, and close observation of the surgical scar is necessary. Careful scar management is required because the patient will be in an immunocompromised state, with a high risk of wound infection.
References
Monclair T, Brodeur GM, Ambros PF, et al. The International Neuroblastoma Risk Group (INRG) staging system: an INRG Task Force report. J Clin Oncol. 2009;27:298–7.
Brisse HJ, McCarville MB, Granata C, et al. Guidelines for imaging and staging of neuroblastic tumors: consensus report from the International Neuroblastoma Risk Group Project. Radiology. 2011;261:243–57.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Japan
About this chapter
Cite this chapter
Tajiri, T. (2016). Neuroblastoma. In: Taguchi, T., Iwanaka, T., Okamatsu, T. (eds) Operative General Surgery in Neonates and Infants. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55876-7_60
Download citation
DOI: https://doi.org/10.1007/978-4-431-55876-7_60
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55874-3
Online ISBN: 978-4-431-55876-7
eBook Packages: MedicineMedicine (R0)