Abstract
Vitellointestinal Fistula (Patent Omphalomesenteric Duct)
Failure of obliteration of the vitelline duct results in various anomalies such as umbilical enteric fistula, umbilical sinus, vitelline cyst, Meckel’s diverticulum, umbilical polyp, and obliterated omphalomesenteric duct. In a case of the patent vitelline duct (vitellointestinal fistula), the drainage of ileal contents to the umbilicus or the ileal mucosal prolapse through the umbilical sinus is recognized in the newborn period. The diagnosis of the patent vitelline duct is confirmed by a fistulography which demonstrates the direct communication between the umbilicus and the ileum. Treatment of this condition consists of the excision of the fistulous tract and closure of the ileal wall which communicates the fistula via transumbilical approach.
Urachal Remnant (Urachal Sinus/Cyst)
Although the urachus extends from the anterior dome of the bladder toward the umbilicus in early gestation, the lumen of the urachus is gradually occluded and becomes cordlike structure during fetal development. Failure of obliteration of the urachus results in patent urachus, urachal sinus, urachal cyst, urachal diverticulum, and alternating sinus. Completely patent urachus is usually recognized in the neonates due to drainage of the urine through the umbilicus. Surgical repair is accomplished through the subumbilical transverse incision or the infraumbilical U-shaped incision with excision of the urachal sinus. On the other hand, umbilical urachal sinus is recognized by periumbilical erythema, tenderness, and transumbilical purulent discharge, and urachal cyst is detected by tender lower midline mass in general. Excision of sinus or cyst with the rest of the urachal tract should be performed.
The figures in this chapter are reprinted with permission from Standard Pediatric Operative Surgery (in Japanese), Medical View Co., Ltd., 2013, with the exception of occasional newly added figures that may appear.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Vitellointestinal Fistula (Patent Omphalomesenteric Sinus)
1.1 Preoperative Management
1.1.1 Symptoms [1, 2]
-
1.
Drainage of ileal contents to the umbilicus
-
2.
Ileal mucosal prolapse through the umbilical sinus (Fig. 26.1)
1.1.2 Diagnosis
A fistulography demonstrates the direct communication between the umbilicus and the ileum (Fig. 26.2) [3].
1.2 Operations
1.2.1 Skin Incision (Fig. 26.3)
-
1.
Supra- or infraumbilical transverse incision
-
2.
U-shaped or inverted Ω incision around the umbilicus
-
3.
Circular incision within the umbilicus at the mucocutaneous junction (Fig. 26.3, right) [4]
1.2.2 Dissection, Resection of the Fistulous Tract, and Anastomosis
A circular incision between the umbilical skin and the ileal mucosa is made (Fig. 26.3, right), and dissection of the fistulous tract from the surrounding tissue is continued into the peritoneal cavity. Upon entering the peritoneal cavity, the ileum which is connected to the fistula is mobilized (Fig. 26.4). After a division of the mesodiverticular band, a wedge resection of the vitellointestinal tract is done and the ileum is closed in one or two layers with absorbable sutures (Fig. 26.5).
1.2.3 Wound Closure
The defect in the umbilical ring is sutured and the umbilical skin is closed by a subcuticular purse-string suture with absorbable suture.
1.3 Postoperative Management
-
1.
Feeding is started when flatus or stool passed.
-
2.
Postoperative complications: anastomotic leakage, anastomotic stenosis, wound infection, and adhesive intestinal obstruction.
2 Urachal Sinus/Urachal Cyst
2.1 Preoperative Management
2.1.1 Symptoms [5–7]
-
1.
Drainage of the urine through the umbilicus (completely patent urachus)
-
2.
Omphalitis: periumbilical erythema, tenderness, and transumbilical purulent discharge (umbilical urachal sinus)
-
3.
Tender lower midline mass (urachal cyst, pyourachus)
2.1.2 Diagnosis [7]
-
1.
Fistulography (Fig. 26.6)
-
2.
Retrograde cystography (Fig. 26.7)
-
3.
Ultrasonography (Fig. 26.8)
-
4.
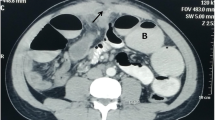
CT scan (Fig. 26.9)
-
5.
MRI
In case of a completely patent urachus, immediate surgery is needed, whereas operation should be performed after the infection subsides by antibiotic therapy or drainage in case of the pyourachus.
2.2 Operative Procedures
2.2.1 Skin Incision (Fig. 26.3)
-
1.
Subumbilical transverse incision (Fig. 26.10a)
-
2.
Lower abdominal midline incision (Fig. 26.10b)
-
3.
Infraumbilical U-shaped (Fig. 26.10c) or Y-shaped incision (Fig. 26.10d)
In case of a completely patent urachus and urachal cyst, the subumbilical transverse incision or the lower abdominal midline incision is suitable, whereas in case of the umbilical urachal sinus, the infraumbilical U-shaped or Y-shaped incision is excellent.
2.2.2 Dissection of the Urachus
After an adequate skin incision is made and the separation of the rectus fascia is done, the urachus is dissected away from the peritoneum. The urachus extends from the anterior dome of the bladder toward the umbilicus, adjacent to the medial umbilical folds (Fig. 26.11). In case of the umbilical urachal sinus, to probe from the umbilical orifice to the sinus facilitates the dissection.
2.2.3 Excision of the Urachus
Although the extraperitoneal excision of the urachal remnant is desirable, the urachus is resected with the peritoneum if the inflammatory adhesion is dense.
2.2.4 Closure of the Bladder and Excision of the Median Umbilical Fold
In case of a patent urachus, total excision of the urachal sinus with a cuff of bladder is required. The bladder is closed in two layers with absorbable sutures. In case of the umbilical sinus, the proximal sinus and the distal medial umbilical fold are resected.
2.2.5 Wound Closure
The defect in the umbilical ring is sutured and the abdominal wall is closed as usual fashion.
2.3 Postoperative Care
-
1.
Early postoperative feeding is possible in case of the extraperitoneal excision of the urachus, but in case of laparotomy, feeding is started when the flatus or the stool passed.
-
2.
Postoperative complications: wound infection and adhesive intestinal obstruction (in a case of laparotomy)
References
Fox PF. Uncommon umbilical anomalies in children. Surg Gynecol Obstet. 1951;92:91–100.
Moore TC. Omphalomesenteric duct malformations. Semin Pediatr Surg. 1996;5:116–23.
Ameh EA, Mshelbwala PM, Dauda MM, Sabiu L, Nmadu PT. Symptomatic vitelline duct anomalies in children. S Afr J Surg. 2005;43:84–5.
Hasegawa T, Sakurai T, Monta O, Tazuke Y, Ueda S, Iwasaki Y, Morimoto Y, Mizutani S, Sumimura J, Ban H, Dezawa T. Transumbilical resection and umbilical plasty for patent omphalomesenteric duct. Pediatr Surg Int. 1998;13:180–1.
Blichert-Toft M, Nielsen OV. Disease of the urachus simulating intraabdominal disorders. Am J Surg. 1971;122:123–5.
Naiditch JA, Radhakrishhan J, Chin AC. Current diagnosis and management of urachal remnants. J Pediatr Surg. 2013;48:2148–52.
Nagasaki A, Handa N, Kawanami T. Diagnosis of urachal anomalies in infancy and childhood by contrast fistulography, ultrasound and CT. Pediatr Radiol. 1991;21:321–3.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Japan
About this chapter
Cite this chapter
Handa, N. (2016). Vitellointestinal Fistula and Urachal Remnant. In: Taguchi, T., Iwanaka, T., Okamatsu, T. (eds) Operative General Surgery in Neonates and Infants. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55876-7_26
Download citation
DOI: https://doi.org/10.1007/978-4-431-55876-7_26
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55874-3
Online ISBN: 978-4-431-55876-7
eBook Packages: MedicineMedicine (R0)