Abstract
We describe microfluidic devices developed for producing heterogeneous hydrogel materials including sandwich-type hydrogel fibers, hydrogel fibers having a highly complex cross-sectional morphology, stripe-patterned hydrogel sheets, and yarn-ball-shaped hydrogel beads. Cells encapsulated within these hydrogel materials exhibit behaviors that are distinct from those of cells examined using conventional cell-culture techniques. The cells are rapidly encapsulated in the hydrogel materials, and the cell-containing materials obtained could function as unit structures in constructing large tissues. Here, we also briefly discuss the use of hydrogel-based microfluidic devices in the preparation of multilayer blood-vessel models.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
When tissues are closely examined in vivo, most of them can be observed to be composed of a 3-dimensional (3D) hierarchical assembly of cells and extracellular matrices (ECMs). For example, muscle is composed of precisely aligned muscle-cell filaments and embedded blood vessels. The liver, the largest organ in the human body, contains a parallel arrangement of cord-like unit structures called “hepatic cords,” each of which is composed of a row of parenchymal hepatocytes and surrounding sinusoidal endothelial cells. The pancreatic islet is composed of several types of major cells including α, β, and δ cells, and embedded vascular networks. To create such complex tissues in vitro, various types of tissue-engineering approaches have been developed. However, because most of the conventional platforms used for culturing animal cells are 2D, planar surfaces, critical differences exist between these in vitro environments and the tissues in vivo. Researchers have attempted to generate functional tissues or organ models that can be used in regenerative medicine, in cell-based drug-evaluation systems, and as platforms for studying cellular physiology in environments that mimic the in vivo setting. Because 3D cell cultures feature structures that are similar to in vivo tissue structures, cells cultivated in 3D can benefit from the upregulation of cellular functions and vitality, especially in the case of cells that are prone to lose their functions in vitro. New technologies are being developed to assemble multiple types of cells into large 3D tissues in which the positions of distinct types of cells and the appropriate arrangement of the ECMs can be controlled.
One of the strategies used most frequently for cultivating cells in 3D is the generation of spherical aggregates of cells, or “spheroids.” When suspended cells are seeded in non-cell-adhesive dishes or into microwells, the cells typically form spherical aggregates because of the contraction force between cells. Spheroids have been used as unit structures to create large tissue models such as blood vessel-like structures [1, 2]. However, one problem encountered with these cultures is that the cells located at the center of the aggregates are not viable when the spheroid size exceeds ~ 200 μm [3]. This example indicates that the size of the unit structures used for constructing tissues should be less than ~ 200 μm if specific vascular structures are not embedded. Moreover, the spherical shape of the cell aggregates does not necessarily represent the configuration most suitable for constructing large tissues; for example, toroidal aggregates could be suitable for constructing vascular-tissue models.
Hydrogels are materials that facilitate the culturing of cells in a 3D environment. The permeable matrices of hydrogels enable oxygen and nutrients to be transported to the cells embedded within the hydrogels. Various types of hydrogel materials have been used for culturing animal cells, including collagen, gelatin, alginate, gel-forming peptides, and synthetic polyethylene glycol (PEG)-based polymers. Cells are unlikely to be viable if they are embedded in large hydrogels at a high density, much as in the case of cell aggregates. Hence, techniques have been developed for encapsulating cells in small hydrogel constructs, and this helps avoid the problem of necrosis that is associated with hypoxia. For use in producing small-sized hydrogels, microfluidic technologies and microfabrication processes have attracted considerable interest in the field of hydrogel-based cell cultivation and tissue engineering [4]. Because the inherent laminar-flow profile formed within microchannels can be controlled accurately, microfluidic devices have been employed for preparing small but highly functional objects including particles, droplets, fibers, and sheets. For example, in the case of fabricating particulate materials, in addition to homogeneous and spherical particles, functional particles such as “Janus” particles and particles featuring complicated morphologies have been produced [5]. Furthermore, hydrogel materials such as beads and fibers featuring controlled morphologies have been produced, which successfully encapsulate cells within the hydrogel matrix [6–8]. Anisotropic hydrogel materials have also been produced, and these enable the precise encapsulation of multiple types of cells [9]. These studies clearly demonstrated the potential usefulness of micrometer-sized hydrogel materials as a novel platform for cell cultivation, in which the position, density, and compositions of cells can be precisely controlled. Moreover, these hydrogel materials can potentially be used as unit structures to construct large, complex tissues that mimic the structures of organs in vivo. In this chapter, we briefly introduce recent advances in the preparation of functional hydrogel materials including anisotropic hydrogel microfibers, functional hydrogel particles used for cell cultivation, and heterogeneous hydrogel sheets. We also present a brief overview of several studies in which microfluidic devices and microchambers made of hydrogel materials were used for cultivating cells in a 3D environment.
2 Anisotropic Hydrogel Fibers Used for 3D Cell Cultivation and Heterotypic Coculture Preparation
2.1 Preparation of Anisotropic Hydrogel Microfibers by Using Microfluidic Devices
Tissues and organs displaying microscale alignments of linear unit structures of cells are commonly detected in vivo, as in the case of, for example, multilayer vascular tissues, nerve bundles, skeletal muscles, and hepatic cord structures. Although these tissues appear “linear” in a microscopic view, most of them comprise multiple types of cells that are precisely aligned in regular patterns. The engineering of such linear tissues in vitro is likely to be facilitated by the use of linear but heterogeneous 3D microenvironments that encapsulate multiple cell types and concomitantly regulate the proliferation direction of the embedded cells. One of the most common methods of assembling multiple types of cells into linear colonies involves using patterned adhesive and non-adhesive surfaces on planar cell-culture plates. Various strategies have been proposed for this purpose, including photolithography [10], microcontact printing [11, 12], and microfluidics-based patterning techniques [13]. Conversely, the preparation of fibrous hydrogels has also been reported, which enables mammalian cells to be cultivated within 3D hydrogel matrices or on the hydrogel surface and also concomitantly allows the embedded cells to be efficiently supplied with oxygen and nutrients. Several studies have reported the preparation of alginate [14, 15] and chitosan [16] hydrogel fibers by using either a micronozzle or a double capillary. Although these studies demonstrated the potential suitability of hydrogel microfibers that were typically 10–1000 μm in diameter, most of the fibers used displayed homogeneous and uniform cross-sections. Unlike in the case of these fibers, not many reports have described the preparation of complex hydrogel fibers composed of multiple regions that exhibit distinct compositions in the cross-section.
To develop anisotropic fibrous hydrogel materials whose diameters are less than a few hundred micrometers, we recently prepared complex microfibers composed of multiple regions exhibiting divergent physicochemical characteristics [9]. For example, sandwich-type solid-soft-solid hydrogel fibers were prepared using microfluidic devices in which the proliferation direction of encapsulated cells was guided and thus linear cell colonies were formed. We employed sodium alginate (NaA) as the primary hydrogel material, because it offers the following remarkable advantages. (1) Alginate is gelled in the presence of multivalent cations, and thus its gelation does not require temperature control, especially heating. (2) Alginate gelation is extremely rapid. (3) Intact cells can be embedded in alginate gels at high densities. (4) The mechanical strength of the hydrogel matrix is high, and thus the gel can be handled easily. (5) The alginate polymer does not induce inflammation when transplanted in vivo. (6) Alginate hydrogels can be removed using cation chelators such as EDTA and citrate, or by enzymatically digesting the alginate polymer. Because of these characteristics, alginate hydrogels are widely used for preparing cell-embedding hydrogels that are employed in tissue engineering and regenerative medicine.
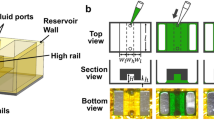
To engineer complex hydrogel microfibers, we used microfluidic devices (Fig. 8.1a). Microchannels featuring 5–7 inlets were used, which were prepared by employing soft lithography and replica-molding techniques and using polydimethylsiloxane (PDMS) as the microchannel material [17]. Gelation solutions containing CaCl2 or BaCl2, buffer solutions, and NaA solutions were continuously introduced from the outer, middle, and inner inlet channels, respectively (Fig. 8.1a), by using syringe pumps. By introducing NaA solutions of distinct compositions through separate inlet ports, micrometer-scale hydrogel fibers displaying complex cross-sectional morphologies were obtained. Two points are critical for stably obtaining Ca-alginate fibers that have uniform diameters: (1) thin buffer layers must be introduced between the NaA and CaCl2 solutions, because this controls the gelation speed of Ca-alginate hydrogels and prevents the microchannel from becoming clogged at the confluence point as a result of hydrogel formation; and (2) using a thickener such as dextran can help balance the viscosities of the introduced buffers/gelation solutions with the high viscosity of the NaA solution.
Preparation of anisotropic hydrogel microfibers and their use in culturing cells. a Microfluidic system used for producing anisotropic alginate hydrogel microfibers. b Hydrogel microfibers embedding particles of distinct colors. c A linear colony of PC12 cells formed within sandwich-type solid-soft-solid hydrogel microfibers. d Preparation of complex hydrogel fibers containing 8 soft regions in the periphery of the fiber. e Millimeter-long colonies of PC12 cells formed within the hydrogel fibers containing 8 soft regions. f, g Primary rat hepatocytes cultivated for 7 days f with and g without 3T3 cells within the sandwich-type fibers
In our study, we first examined whether Ca-alginate hydrogel fibers displaying complex cross-sectional morphologies were obtained. We introduced NaA solutions containing fluorescent particles into a microchannel (~ 400 μm wide and ~100 μm deep) that had 6 inlets. Figure 8.1b shows an example of a microfiber that had an average diameter of ~ 15 μm. Because a stable laminar flow forms within the microchannel, the gelation agent (Ca2+ or Ba2+ ions) diffused into the central flow region of the precursor solution (NaA solution) through the buffer flows and thus continuously transformed the precursor solution into the hydrogel. Consequently, we successfully obtained microfibers that were 5–100 μm in diameter and displayed a uniform cross-sectional morphology. The diameter of the obtained fibers could be tightly controlled by changing the flow rate of the NaA solutions and the microchannel dimensions: when broad microchannels (width and depth, 800 μm) were used, we obtained fibers that had diameters up to 200 μm; moreover, lowering the flow rate of the buffer solutions resulted in the formation of fibers whose widths were highly uniform.
To use the developed hydrogel fibers in cell cultures, we next prepared sandwich-type hydrogel fibers composed of 3 regions (containing distinctly colored particles) by using 7-inlet microchannels. To adjust the stiffness of the central region of the cross-section of the fibers, we used propylene glycol alginate (PGA), a non-gelling ester derivative of alginate. When an aqueous solution of NaA + PGA is used, the hydrogels obtained exhibit diminished stiffness. By introducing the NaA + PGA solution through the central inlet and NaA solutions from the neighboring inlets, we obtained sandwich-type hydrogel fibers that contained hard-soft-hard regions. Highly stiff alginate hydrogels are recognized to be unsuitable for cultivating highly proliferative cells [18]; however, we expected the cells encapsulated within the soft region of the fibers to proliferate and form intercellular networks along the fiber length. To demonstrate this, we encapsulated cells within the soft core and then observed the direction of cell growth. The soft core was made from 0.9 % PGA and 0.3 % NaA, whereas the solid shell was made from 2 % NaA. Moreover, the surface of the obtained fibers was coated with poly-L-lysine, which prevents the hydrogel fiber from swelling in the cell culture medium and thus keeps the cells from growing out of the hydrogel matrix. We cultured NIH-3T3 cells within the hydrogel fibers for 6 days (Fig. 8.1c); the cells were initially located within the core of the sandwich-type fibers, but then gradually grew along the soft region and finally formed linear, one-cell-thick colonies. By contrast, in control experiments in which homogeneous fibers made from 2 % NaA were used, spherical colonies were formed. Similar results were obtained when HeLa cells were cultivated. These results helped confirm that anisotropic hydrogel fibers serve as a suitable platform for cultivating cells in 3D environments and could potentially be applied for constructing linear tissues.
Next, we prepared hydrogel fibers whose cross-sectional morphologies were much more complex. Micronozzle array-combined microfluidic devices have been developed for generating hydrogel fibers composed of multiple soft and solid regions [19]. The patterns of the vertical micronozzles determine the cross-sectional morphology of the hydrogel microfibers. We fabricated 4-layer microfluidic devices made of poly(methyl methacrylate) employing numerical control (NC) micromachining and thermal-bonding processes. The microfibers obtained displayed 8 soft regions in the peripheral area of their cross-section, and the fiber diameter and the width of the soft regions were 60–100 and 10–20 μm, respectively (Fig. 8.1d). After confirming that 8 soft regions were successfully formed within the fibers, we encapsulated neuron -like cells (PC12 cells) in the peripheral soft regions of the fiber, and then cultured the cells under a differentiation condition in which the serum concentration in the medium was low and the medium contained nerve growth factor. Our results showed that the PC12 cells formed linear colonies and the outgrowth of their neurites was guided because of the presence of the solid-soft regions within the fiber. After cultivation for 14 days, millimeter-long cellular networks were formed (Fig. 8.1e). These heterogeneous fibers can serve as new tools for guiding cell proliferation and networking behaviors in 3D environments, and could potentially also be applied in regenerating damaged nerves and evaluating the behavior of neural cells in confined spaces.
2.2 Formation of Heterotypic Hepatic Microorganoids by Using Anisotropic Hydrogel Microfibers
Hepatocytes (parenchymal cells) perform major functions in the liver, including the metabolism of drugs, the production of plasma proteins, blood purification, and the storage of nutrients. Thus, engineering liver tissues by using hepatocytes can be critical for developing implantable hepatic constructs, preparing in vitro models for use in drug-metabolism and toxicity assays, and fabricating extracorporeal bioartificial liver devices for implantation in patients with liver insufficiency. Furthermore, hepatocyte-based tissue engineering could potentially be used as an alternate to whole-organ transplantation for the purpose of supporting hepatic functions. However, a major challenge faced in culturing primary hepatocytes in vitro is that hepatocytes do not proliferate and rapidly lose their functions and phenotypes, even though hepatocytes can efficiently regenerate in vitro. Therefore, new techniques designed for maintaining the functions and viability of hepatocytes in vitro are in high demand.
Various approaches have been tested to solve the problem of culturing hepatocytes in vitro. Generating spheroids by using non-adhesive surfaces/wells or patterned ECMs [20–24] is one of the most frequently used methods of upregulating hepatocyte functions, because this facilitates cell-cell interactions in a 3D environment. Hepatocytes have also been cocultured with other types of cells; for example, hepatocytes have been used in patterned cocultures prepared with fibroblasts or endothelial cells [25–31] and heterotypic cell sheets have been stacked [32, 33], and in both cases, heterotypic cellular interactions were reproduced. The human liver is composed of small unit structures called hepatic lobules, which comprise parenchymal hepatocytes and several types of non-parenchymal cells including liver sinusoidal endothelial cells (LSECs), stellate cells, and Kupffer cells. Within a lobule, hepatocytes are arranged in a cord-like linear structure, which is covered with a thin layer of LSECs. The space between the hepatocytes and LSECs is called Space of Disse, which contains various types of ECMs. This configuration allows hepatocytes to maintain close contact with the blood circulation through the fenestrations of the LSECs, and thus enables the efficient supply/exchange of nutrients, oxygen, and metabolic products. Based on considering this characteristic structure, we hypothesized that reconstructing similar microstructures composed of multiple types of cells will improve the functions and vitality of hepatocytes cultured in vitro. To fabricate such a 3D, heterotypic coculture system, we employed the anisotropic hydrogel microfibers that were produced using microfluidic devices; multiple types of cells were encapsulated close to each other within the microfibers [34].
Our strategy involved using sandwich-type, anisotropic alginate hydrogel microfibers . Hepatocytes were encapsulated in the center of the fiber, which was sandwiched by the hydrogel regions wherein non-parenchymal cells were embedded. In the core of the hydrogel fibers, hepatocytes gradually formed linear aggregates during cultivation, which then became gradually surrounded by non-parenchymal cells; this resulted in the formation of linear but 3D microaggregates (microorganoids) that closely mimicked the hepatic cord structures observed in the liver lobules.
In our study, we used Ba2+ ions instead of Ca2+ ions as the gelation agent for the alginate hydrogel, because the Ba2+ ions bind the alginate polymer more strongly than do the Ca2+ ions, and thus the swelling of the hydrogel is suppressed. We also included Type I collagen in the NaA solutions, which helps preserve the viability and functions of hepatocytes. The hepatocytes we used were primary hepatocytes that were isolated from male F344/N rats by using a collagenase-perfusion protocol. As a model of non-parenchymal cells, we used Swiss 3T3 cells, which are frequently used in coculture experiments as feeder cells. As in the experiments described in the preceding section, we used PDMS microchannels featuring gelation channels that were 400 μm wide and 160 μm deep. Hepatocytes and 3T3 cells were suspended separately in sterile, isotonic NaA solutions containing collagen. A high density of hepatocytes was used in the precursor solution (3 × 107 cells/mL) to ensure sufficient contact between hepatocytes. After preparing and recovering the cell-encapsulating alginate hydrogel fibers, cells were cultured for up to 90 days.
First, we examined the effect of O2 tension on the viability and functions of hepatocytes within the hydrogel fibers, because oxygen plays a critical role in hepatocyte cultures [35, 36]. We also investigated how coculturing hepatocytes with 3T3 cells affects hepatic functions and compared this with the effects measured using conventional plate cultures and hepatocyte-only cultures prepared in the hydrogel fibers. Figure 8.1f, g shows the obtained fibers containing hepatocytes with and without 3T3 cells 7 days of cultivation.
By adjusting the flow rates at which solutions were introduced, we effectively controlled the diameter of the cell-encapsulating microfibers. Hepatocytes were encapsulated in the core region that was ~ 50 μm wide, and 3T3 cells were embedded in the sandwiching shell regions. After cultivation for several days, we evaluated the viability of hepatocytes by using a dye-exclusion test. The hepatocytes and 3T3 cells formed linear aggregates within the hydrogel matrix (Fig. 8.1g); thus, hepatocyte viability remained above ~ 80 % when they were cocultured with 3T3 cells and the O2 concentration was high (35 %). By contrast, under normal O2 tension and in hepatocyte-only cultures, hepatocyte viability decreased rapidly, indicating that the O2 concentration was critical for maintaining the viability of hepatocyte in this culture system.
As mentioned in the preceding section, alginate hydrogels can be readily digested by using enzymes (alginate lyase) or chelating multivalent cations. We sought to recover the linear organoids by enzymatically digesting the alginate hydrogel. By using this procedure, we recovered intact linear organoids that were 200–1000 μm long. Immunohistological examination revealed that hepatocytes located in the center of the organoids were covered with a thin layer of 3T3 cells. Furthermore, by observing the ultrastructure of hepatocytes by using transmission electron microscopy, we confirmed that hepatocytes extended microvilli in the space between adjacent 3T3 cells. These characteristic morphologies resembled those observed in tissues in vivo, indicating that the heterotypic organoids closely mimicked the hepatic cord structures observed in the liver.
Lastly, we examined several hepatic functions, and compared the results with those obtained using conventional 2D plate cultures and 3D fiber cultures in which 3T3 cells were not included. First, albumin-production rates and urea synthesis were measured directly, which revealed that (relative to controls) albumin production was enhanced substantially under coculture conditions in the hydrogel fiber, and this high level was maintained for up to ~ 60 days. A similar trend was observed in the case of urea synthesis. Next, we performed quantitative PCR to evaluate hepatocyte-specific functions such as the expression of cytochrome P450 and coagulation factors. These genes were expressed at high levels in the cocultures prepared within the fibers. By contrast, the expression of these genes decreased rapidly in the 3D hepatocyte-only cultures and in the plate cultures. These results clearly demonstrated that using the microscale 3D coculture system, which closely mimics the sinusoidal structures present in vivo, is a highly effective strategy for maintaining hepatic functions in vitro. The aforementioned culture technique could be applied for developing liver-tissue models designed for hepatocyte-based drug development, toxicity assays, and bioartificial liver devices. Recently, several reports have described the preparation and application of micrometer-sized hydrogel fibers designed for tissue engineering and cell culture in a confined but 3D environment, and in these studies, alginate was used as the primary hydrogel materials [37, 38]. We expect that fibrous, microengineered hydrogel materials will be widely used in constructing linear tissue models.
3 Preparation of Patterned Hydrogel Sheets Designed for Coculturing Cells in 3D
In Sect. 2, we introduced microfabricated hydrogel fibers and their use in generating intercellular networks and cocultures of hepatocytes. These fibers feature one of the most suitable morphologies for preparing cell cultures in terms of the diffusion-based supply of oxygen and nutrients; by comparison, however, planar hydrogel sheets might be more suitable for generating complex cell assemblies that resemble in vivo tissues. Moreover, planar structures could be more effective than fibers are in serving as building blocks used for constructing large-scale 3D tissue models by means of stacking. Furthermore, the cell-encapsulation throughput and the production speed of hydrogels could be considerably higher for sheets than for fibers. In this section, we briefly describe our recent successful production of heterogeneous, stripe-patterned hydrogel sheets, which were prepared by using micronozzle-combined planar microfluidic devices. We also describe the coculture of hepatocytes (in this case, HepG2 cells) and feeder cells (3T3 cells).
The microfluidic device used for preparing heterogeneous hydrogel sheets encapsulating distinct types of cells is shown in Fig. 8.2a, and the cell-growth behaviors in the hydrogel sheet are shown in Fig. 8.2b. By introducing NaA solutions in the absence and presence of cells into the microchannel and by extruding the split/recombined streams into the gelation solution outside the microfluidic device, we can obtain hydrogel sheets incorporating arrays of parallel regions that contain distinct types of cells at high densities. By using PGA, we can control the stiffness of the hydrogel regions; cells are encapsulated in the soft regions of the sheet, and the solid regions prevent the cells from growing in the vertical direction, which results in the formation of rod-like heterotypic microorganoids. As an application, we cocultured hepatoma cells (HepG2 cells) and 3T3 cells and examined whether the functions of HepG2 cells were upregulated.
Preparation of heterogeneous hydrogel microsheets and their use in culturing cells. a Microfluidic system used for preparing patterned alginate hydrogel sheets. b Schematic representation of cell growth in patterned hydrogel sheets. c, d Stripe-patterned hydrogel sheets encapsulating 2 types of cells (non-stained cells: HepG2; red cells: 3T3). Arrays of linear colonies were formed within the hydrogel sheet after 7 days of cultivation (d)
In the experiment, we fabricated 3-layer PDMS microfluidic device s. The device featured 3 inlets: Inlet 1 was used for the NaA + PGA solution containing hepatocytes; Inlet 2, for the same alginate solution but with 3T3 cells; and Inlet 3, for the NaA solution that was used for the solid spacer region. The micronozzle exit was 2.5 mm wide. The flow stream containing HepG2 cells was divided into 16 streams, each of which was sandwiched by the flows containing the 3T3 cells. The flow in the spacer region separated the flows containing 3T3 cells. The encapsulated cells could proliferate along the soft-hydrogel regions, but the solid-hydrogel regions prevented the cells from growing in the horizontal direction; this resulted in the formation of rod-like, linear organoids that were composed of multiple types of cells.
First, we examined whether the stripe-patterned heterogeneous hydrogel sheets were precisely fabricated with controlled stripe width and hydrogel thickness. When we used 2 % NaA solutions containing distinctly colored microbeads (diameter, ~ 1 μm) as the precursor solution, flat hydrogel fibers of a uniform thickness were obtained. The hydrogel sheet (~ 2.0 mm wide) was slightly narrower than the micronozzle (2.5 mm wide) because the alginate hydrogel shrank during the gelation process. By controlling the ratio of the flow rates of the introduced solutions, we were able to precisely control the width of the stripe patterns, and by adjusting the ratio of the introduced flow rates and/or the extension speed by using the roller, we could precisely control the thickness of the hydrogel.
Next, to develop cultures that mimic the sinusoid structures of the liver, we used the microchannel system described herein to prepare hydrogel sheets incorporating HepG2 and 3T3 cells; these cells served as models of hepatocytes and non-parenchymal cells, respectively. In the microchannel system, the flows of HepG2 and 3T3 cells were focused into narrow streams within the microchannel by the spacer flow, because the viscosities of the introduced solutions were dissimilar. In total, 64 streams were combined in the microchannel and had a width of 2.5 mm, and then were extruded from the microchannel into the outer gelation bath through the micronozzle. The cell-encapsulating hydrogel sheets obtained are shown in Fig. 8.2c, d. The positions of the 2 types of cells were maintained throughout the gelation process, and the heterogeneous hydrogel sheets that were obtained incorporated HepG2 and 3T3 cells (stained with a red dye) at high densities. During cultivation, HepG2 cells grew within the soft region and formed linear organoids (Fig. 8.2c), because the solid spacer regions acted as barriers. By contrast, 3T3 cells did not proliferate substantially, probably because of the contact inhibition occurring within the hydrogel matrix, but these cells adhered on the surface of the linear colonies of HepG2 cells. We observed that the HepG2 cells located at the center of the colonies were surrounded by a layer of 3T3 cells after several days of cultivation, as in the case of the cocultures prepared within the alginate fiber. Lastly, we examined whether hepatic functions were enhanced in the cocultures by using quantitative PCR analysis and ELISAs. Our results showed that albumin secretion from the cocultures was higher than that from the single culture of HepG2 cells in the hydrogel fiber, which demonstrated that hepatic functions were effectively enhanced in the 3D cocultures. Moreover, the results of quantitative PCR assays revealed that several genes associated with the differentiation of HepG2 cells were upregulated. Compared with fiber-based cultivation, this microfluidic process developed for preparing stripe-patterned alginate hydrogel sheets might enable more efficient culturing multiple types of cells at high densities, because the process can be readily applied in constructing large tissue models.
4 A Microfluidic Process for Producing Functional Hydrogel Beads
4.1 A Microfluidic System Developed for Producing Yarn-Ball-Shaped Hydrogel Microbeads
Encapsulation of biological substances into hydrogel matrices is a promising technique that can be used in diverse bioengineering and medical applications. Specifically, cell-encapsulating hydrogel microbeads could serve as a favorable unit structure for constructing large tissue models, especially when the beads are used together with hydrogel fibers or sheets, or cell aggregates. To prepare cell-encapsulating hydrogel beads that are a few hundred micrometers in diameter, various approaches have been developed that involve using microfluidic devices [6] or micronozzle structures [7]. However, most of the previous approaches are not suitable for producing hydrogel beads that exhibit diverse morphologies; mostly spherical beads have been produced because of the minimal interfacial energy of the spherical droplets of the precursor solution. Although the preparation of hydrogel beads featuring more complex morphologies has been reported, the methods used require complicated microfluidic systems that incorporate in situ photolithographic processes [39, 40]. Furthermore, most of these photolithography-based techniques could only be used to prepare simple planar structures of uniform thickness. When cells are encapsulated within hydrogel beads, morphologies that have a high surface-to-volume ratio would be highly advantageous when considering the supply of oxygen and nutrients to cells. However, hydrogel microfibers, for example, are unlikely to be suitable for close packing in a flow-through reactor/chamber and for intravascular injection into host organs.
Recently, we developed a simple microfluidic process designed for producing yarn-ball-shaped hydrogel microbeads [41]. In this process, we employed the procedure used for preparing hydrogel fibers [9] that is described in the preceding sections and combined this with droplet-microfluidics technology. The mechanism by which the hydrogel microbeads are formed is illustrated in Fig. 8.3a. As in the preparation of hydrogel fibers, we employed parallel flows of aqueous solutions of a hydrogel precursor (NaA), a gelation agent, and a buffer solution. Incompletely gelled alginate hydrogel microfibers were generated at the confluence, where water-in-oil (w/o) droplets formed simultaneously. The fibers were fragmented during encapsulation and they folded into a yarn-ball-like shape. This yarn-ball-shaped morphology combines several advantages associated with both spherical beads and linear fibers: this unique morphology is compact but has a high surface-to-volume ratio, and thus can potentially enable efficient supply of oxygen and nutrients to encapsulated cells; moreover, if these yarn-ball-shaped particles are used as carriers for transplantation of cells (e.g., pancreatic islets or hepatocytes) and are transplanted intravascularly, the morphology is unlikely to strongly hinder the flow of blood because of the void space.
In our experiments, we first tested the fabrication of yarn-ball-shaped hydrogel beads by using a 1.8 % NaA solution as the precursor. The concentration of the gelation agent (CaCl2 or BaCl2) was varied to examine their effect on the generation of the yarn-ball-shaped hydrogel beads. The experimental procedures used were similar to those described for the production of hydrogel fibers, and to generate the w/o droplets, we introduced olive oil together with lecithin into the microchannels. When we tested CaCl2, we determined that at a concentration as high as 20 mM, the hydrogel fiber that was formed was not fragmented, because the gelation had already proceeded at the confluence point and the formed hydrogel fiber was highly solid. When the CaCl2 concentration was too low (5 mM), nearly spherical beads were obtained because droplets were formed and the inner contents were mixed before the formation of the hydrogel fiber. When the CaCl2 concentration was approximately 10 mM, the w/o droplets were generated at a point that was ~25 mm from the confluence. Incompletely gelled and fragmented hydrogel fibers were observed in the droplets, and we successfully obtained yarn-ball-shaped hydrogel beads. Based on these results, we concluded that the concentration of Ca2+ was critical for producing yarn-ball-shape beads. The beads were 200–300 μm in diameter, and the hydrogel fibers that formed the beads were 10–30 μm wide; these sizes could be adjusted by changing operational conditions such as the flow rates used. We were also able to produce Ba-alginate microbeads by using BaCl2 as the gelation agent; however, the optimal concentration of BaCl2 required for the formation of yarn-ball-shaped hydrogel beads was distinct from that of CaCl2 required for generating Ca-alginate microbeads. When a surfactant (1 % bovine serum albumin) was added in the gelation solution, the beads shrank and highly became uniform in size, because the surface tension between the water and oil phases was decreased.
To apply hydrogel microbeads in high-density cell cultivation, we incorporated animal cells (NIH-3T3 or HeLa cells) into the NaA solution and prepared cell-containing hydrogel microbeads (Fig. 8.3). The initial cell densities were 4.7 × 106 and 3.0 × 106 cells/mL for HeLa and NIH-3T3 cells, respectively. The cell viabilities remained high (> 80 %) even after the cells were encapsulated in the beads. The cells continuously proliferated and formed spherical colonies inside the hydrogel fibers, with the final cell densities reaching 2.4 × 107 cells/mL for HeLa cells on Day 7 and 3.8 × 107 cells/mL for NIH-3T3 cells on Day 15. This result indicated that the hydrogel beads contained voids that are suitable for high-density cell cultivation, which possibly enhanced the supply of oxygen and nutrients to the center of the beads. In summary, the fabricated hydrogel beads could be used as a new material for immobilizing and encapsulating biological materials and could potentially be applied in cell-transplantation therapies. Moreover, these hydrogel beads, which included large internal voids, could be suitable as artificial organ units that do not interrupt blood flow when injected into blood vessels. Lastly, these beads could also function as matrices for biological immobilization and cell cultivation.
4.2 Production of Micrometer-Sized Hydrogel Particles
Size is the most critical factor that determines the physicochemical characteristics of hydrogel beads. Small hydrogel beads are more suitable for biomedical application than large beads are, because chemicals are efficiently supplied and removed through their permeable matrices by means of diffusion. As mentioned in the preceding section, the production of alginate hydrogel beads by using microfluidic devices has been widely reported [6, 7]. However, the production of hydrogel beads whose diameters are in the single-micrometer size range remains challenging; this is because small droplets of highly viscous precursor solutions cannot be readily produced using a narrow microchannel or micronozzle. In this section, we describe a new approach we have developed for producing micrometer-sized hydrogel beads (diameter < 10 µm) by using a unique process of water molecule dissolution from w/o droplets into the continuous phase of a polar solvent [42]. This process enables the production of hydrogel microbeads that are considerably smaller than the droplets generated initially.
The process used for producing micrometer-sized hydrogel beads is shown in Fig. 8.4a. In this process, methyl acetate and an aqueous solution of the hydrogel precursor are introduced into the microchannels to generate w/o droplets at the first confluence. These droplets gradually shrink while flowing through the continuous phase of the polar solvent, and this occurs because of the dissolution of water molecules into the continuous phase. During this period, hydrophilic polymers are concentrated in the shrunk droplets, which are then gelled by introducing a gelation solution. Consequently, the hydrogel beads obtained are considerably smaller than the initial droplets. We prepared Ca-alginate beads and chitosan beads by using CaCl2 and NaOH solutions as the gelation agents, respectively. As the polar organic solvent, we mainly used methyl acetate, which exhibits a water solubility of 8 %.
In these experiments, we again used PDMS microchannels. The microchannel depth was uniformly 55 µm, and the droplet-generation channel (the first confluence) was 50 µm wide. The water-extraction and gelation channels were 70 and 75 mm long, respectively. To produce Ca-alginate hydrogel beads, 0.025–0.15 % NaA solution was used as the precursor solution and 0.01–1 M CaCl2 aq. was used as the gelation solution. To produce chitosan beads, 0.025 or 0.05 % chitosan solution in 0.1 M acetic acid was used as the precursor.
First, we confirmed that w/o droplets were generated at the confluence point and were in a non-equilibrium state. The droplets shrank while they flowed through the microchannel. When the flow rates of the precursor and methyl acetate were 0.9 and 30 µL/min, respectively, and the NaA concentration was 0.1 %, the initial average diameter of the droplets was ~ 70 µm; by contrast, the final average diameter at the time of saturation was ~ 9 µm (Fig. 8.4b). Thus, the volume of the droplets decreased to ~ 0.4 % of the volume of the initial droplets. We were able to adjust the microbead diameters by varying the initial NaA concentration: the diameter changed from 6 to 10 μm when the initial concentration of NaA was increased from 0.025 to 0.15 %, indicating that the NaA concentration in the droplet critically affects the bead size. These results demonstrated that the dissolution of water droplets in methyl acetate was possible, and this process was exploited for producing micrometer-sized hydrogel beads.
To determine whether the microbeads formed were composed of hydrogels, the microbeads were dried and re-swollen repeatedly; the beads shrank and deformed when they were dried, but recovered their initial spherical shape and volume when re-swollen by adding water, which indicated that the swollen beads contained water within their matrices. We used similar methods to prepare chitosan hydrogel beads and obtained monodispersed chitosan hydrogel beads featuring an average diameter of 10.1 µm (coefficient of variation (CV): 4.8 %) when 0.05 % chitosan solution was used (Fig. 8.4c). This result suggests that the process described here for producing micrometer-sized hydrogel beads can be applied on various types of hydrogel materials. These small hydrogel beads might be useful as tools for constructing complex tissue models and also as carriers or immobilization matrices for biological substances.
5 Preparation of Microfabricated Hydrogel Structures for Use in Tissue Engineering
In this section, we describe using microfluidic devices made of hydrogels to produce vascular-tissue models. Engineering vascular tissue is an approach that is essential for preparing artificial-artery grafts, fabricating large tissues embedded with capillary networks, and studying the cellular physiology associated with blood vessels such as cancer metastasis, angiogenesis, and thrombosis. Over the past decade, various strategies have been proposed for building vascular structures, including the rolling of cell sheets [43], the incorporation of cells into fibrous hydrogels [44], and the 3D deposition of cells by using inkjet printing [45]. However, preparing functional vascular tissues remains a challenge in terms of obtaining a multilayer configuration, branch structures, and thick walls; this is mainly because no techniques are available that can be used to effectively assemble multiple cell types into layered capillary structures. Specifically, vascular tissues are composed of inner endothelial cells on the lumen side, smooth muscle cells that provide physical support, and vascular tissue-specific ECM components such as elastin and collagen. Therefore, at least 2 types of cells have to be assembled into fabricated capillary to structurally mimic in vivo vascular tissues. Here, we present the approach we recently developed for assembling multiple types of cells into multilayer capillary structures [46]. In this procedure, multiple Ca-alginate hydrogel layers are deposited within hydrogel microchannels made of agarose.
The process used for preparing vascular tissue-like structures is presented schematically in Fig. 8.5a. In this approach, microchannels made of agarose hydrogel containing Ca2+ ions are first prepared by employing molding and physical-bonding processes. An aqueous solution containing NaA and cells is introduced into the agarose microchannel and then Ca2+ ions are supplied to the NaA solution through the permeable hydrogel matrix; this results in the formation of a Ca-alginate hydrogel layer on the microchannel surface. By repeating this deposition process with a solution of NaA that contains a different type of cells, multilayered Ca-alginate hydrogels incorporating distinct cell types are obtained. The tissues that are formed can be recovered from the hydrogels by detaching the bonded hydrogel plates.
a Schematic image showing the preparation of vascular tissue-like cell assemblies by using hydrogel microchannels and sodium alginate (NaA) solutions containing cells. First, the NaA solution containing Type 1 cells is introduced into the microchannel made of agarose and Ca2+ ions, and a Ca-alginate hydrogel layer is deposited within the microchannel. Next, the NaA solution containing cells of a distinct type (Type 2) is introduced, which results in the formation of a thick, multilayer, and heterotypic vascular-tissue model. b Photograph of a hydrogel microfluidic device incorporating a microchannel structure made of agarose hydrogel. c A multilayer vascular-tissue model prepared using 2 types of cells
We prepared agarose hydrogel microchannels containing Ca2+ ions in the matrix (Fig. 8.5b) by using a previously reported molding scheme [47]. An aqueous solution of 5 % agarose and 10 mM CaCl2 was poured onto a silicon mold with photoresist microstructures, and this was incubated at 4°C for 2 h to completely gel the agarose solution. Next, the hydrogel plate was peeled off from the mold and trimmed, a microstructured plate was physically bonded to the flat hydrogel plate to generate microchannel structures, and, lastly, inlet and outlet tubes were attached. The microchannels were uniformly 500 μm deep and wide.
Before introducing the NaA solution containing cell suspensions, the surface of the agarose microchannel was modified by introducing an aqueous solution of poly-L-lysine and 10 mM CaCl2, which can improve the attachment force of Ca-alginate hydrogels. To control the high gelation speed of alginate, an aqueous solution of a chelator (trisodium citrate) was introduced, after which we introduced 0.5–1 % NaA solutions containing cells or model particles into the microchannel by means of aspiration. After the cell-incorporating hydrogel structures were prepared, the agarose hydrogel microdevices were dipped in cell-culture medium overnight. We used several types of cells including human vascular endothelial cells (HUVECs), fibroblasts (NIH-3T3), and vascular smooth muscle cells; the cells were suspended separately in isotonic solutions of NaA at high densities (0.5–1 × 108 cells/mL). These NaA solutions containing the suspended cell were introduced stepwise into the microchannel, and the deposition of the hydrogel layers was observed using an inverted optical microscope. After the hydrogels had been deposited, complete gelation of the alginate hydrogels was further ensured by introducing a 10 mM CaCl2 solution. The cells were cultured under either fluid-perfusion or static-culture conditions for up to 2 weeks.
First, using a branched microchannel, we demonstrated the stepwise deposition and formation of multilayer Ca-alginate hydrogel structures within the agarose microchannel. After the first NaA solution was introduced into the agarose microchannel for 3 min at a flow rate of 20 µL/min, an approximately 150-μm-thick Ca-alginate hydrogel layer was formed on the microchannel surface. After we introduced the second NaA solution, double-layered Ca-alginate hydrogels were formed. When a particle suspension was introduced continuously, the particles were observed to flow through the hydrogel, which indicated that a hollow capillary structure was formed in a manner that depended on the microchannel geometry. Furthermore, we could control the thickness of the deposited Ca-alginate layer by changing the introduction period and the flow rate of the NaA solution.
Next, we used the NaA solutions containing suspended cells of distinct types and successfully constructed capillary-like tissues featuring double-layered hollow structures, through which we could observe the flow of fluorescent particles. Figure 8.5c shows an example of a capillary tissue that was formed and contained 2 types of cells. Using perfusion cultures resulted in improved viability and function of the embedded cells, as compared with the use of the static cultures. Moreover, the formed tissues could be readily recovered from the hydrogel microchannels by detaching the 2 bonded agarose hydrogel plates, and the tissues were adequately strong to allow them to be handled using tweezers. These results demonstrated that the method presented here enables the assembly of cells into 3D structures and the fabrication of multiple vascular-tissue models.
In summary, we have developed a new process that allows vascular-tissue models to be prepared easily and accurately. By changing the microchannel geometry, the flow rate, and the introduction period of the NaA solution, vascular-tissue models featuring diverse configurations can potentially be prepared. We expect this method to become a highly effective approach for use in vascular tissue engineering.
6 Conclusions and Perspectives
In this paper, we have briefly reviewed our recent progress in producing (1) cell-encapsulating hydrogel materials by using microfluidic devices and (2) capillary-like tissue models by using microfluidic devices made of hydrogels. These materials reproduced the in vivo microenvironment and provided a 3D cell-cultivation platform that enhanced cellular functions and vitality. Furthermore, the materials and tissues presented herein can potentially be used as unit structures for constructing larger tissue models through a bottom-up approach. We expect that by combining the use of the presented hydrogel materials with robotics and automation technologies, versatile strategies can be implemented that facilitate the construction of functional tissues, which will be valuable for use in regenerative medicine, cell-based assay systems designed for drug development, and physiological investigations on cells.
References
Dean DM, Napolitano AP, Youssef J, Morgan JR (2007) Rods, tori, and honeycombs: the directed self-assembly of microtissues with prescribed microscale geometries. FASEB J 21:4005
Norotte C, Marga FS, Niklason LE, Forgacs G (2009) Scaffold-free vascular tissue engineering using bioprinting. Biomaterials 30:5910
Anada T, Fukuda J, Sai Y, Suzuki O (2012) An oxygen-permeable spheroid culture system for the prevention of central hypoxia and necrosis of spheroids. Biomaterials 33:8430
Chung BG, Lee KH, Khademhosseini A, Lee SH (2012) Microfluidic fabrication of microengineered hydrogels and their application in tissue engineering. Lab Chip 12:45
Nisisako T, Torii T, Takahashi T, Takizawa Y (2006) Synthesis of monodisperse bicoloured Janus particles with electrical anisotropy using a microfluidic co-flow system. Adv Mater 18:1152
Tan WH, Takeuchi S (2007) Monodisperse alginate hydrogel microbeads for cell encapsulation. Adv Mater 19:2696
Sugiura S, Oda T, Izumida Y, Aoyagi Y, Satake M, Ochiai A, Ohkohchi N, Nakajima M (2005) Size control of calcium alginate beads containing living cells using micro-nozzle array. Biomaterials 26:3327
Sugiura S, Oda T, Aoyagi Y, Matsuo R, Enomoto T, Matsumoto K, Nakamura T, Satake M, Ochiai A, Ohkohchi N, Nakajima M (2007) Microfabricated airflow nozzle for microencapsulation of living cells into 150 micrometer microcapsules. Biomed Microdev 9:91
Yamada M, Sugaya S, Naganuma Y, Seki M (2012) Microfluidic synthesis of chemically and physically anisotropic hydrogel microfibers for guided cell growth and networking. Soft Matter 8:3122
He W, Halberstadt CR, Gonsalves KE (2004) Lithography application of a novel photoresist for patterning of cells. Biomaterials 25:2055
Zhang S, Yan L, Altman M, Lassle M, Nugent H, Frankel F, Lauffenburger DA, Whitesides GM, Rich A (1999) Biological surface engineering: a simple system for cell pattern formation. Biomaterials 20:1213
Kalinina S, Gliemann H, Lopez-Garcia M, Petershans A, Auernheimer J, Schimmel T, Bruns M, Schambony A, Kessler H, Wedlich D (2008) Isothiocyanate-functionalized RGD peptides for tailoring cell-adhesive surface patterns. Biomaterials 29:3004
Tourovskaia A, Figueroa-Masot X, Folch A (2005) Differentiation-on-a-chip: a microfluidic platform for long-term cell culture studies. Lab Chip 5:14
Su J, Zheng Y, Wu H (2009) Generation of alginate microfibers with a roller-assisted microfluidic system. Lab Chip 9:996
Sugiura S, Oda T, Aoyagi Y, Satake M, Ohkohchi N, Nakajima M (2008) Tubular gel fabrication and cell encapsulation in laminar flow stream formed by microfabricated nozzle array. Lab Chip 8:1255
Lee KH, Shin SJ, Kim CB, Kim JK, Cho YW, Chung BG, Lee SH (2010) Microfluidic synthesis of pure chitosan microfibers for bio-artificial liver chip. Lab Chip 10:1328
Duffy DC, McDonald JC, Schueller OJ, Whitesides GM (1998) Rapid prototyping of microfluidic systems in poly(dimethylsiloxane). Anal Chem 70:4974
Pokrywczynska M, Drewa T, Jundzill A, Lysik J (2008) Alginate is not a good material for growth of rapidly proliferating cells. Transplant Proc 40:1664
Kitagawa Y, Naganuma Y, Yajima Y, Yamada M, Seki M (2014) Patterned hydrogel microfibers prepared using multilayered microfluidic devices for guiding network formation of neural cells. Biofabrication 6:035011
Landry J, Bernier D, Ouellet C, Goyette R, Marceau N (1985) Spheroidal aggregate culture of rat liver cells: histotypic reorganization, biomatrix deposition, and maintenance of functional activities. J Cell Biol 101:914
Dvir-Ginzberg M, Elkayam T, Aflalo ED, Agbaria R, Cohen S (2004) Ultrastructural and functional investigations of adult hepatocyte spheroids during in vitro cultivation. Tissue Eng 10:1806
Fukuda J, Sakai Y, Nakazawa K (2006) Novel hepatocyte culture system developed using microfabrication and collagen/polyethylene glycol microcontact printing. Biomaterials 27:1061
Brophy CM, Luebke-Wheeler JL, Amiot BP, Khan H, Remmel RP, Rinaldo P, Nyberg SL (2009) Rat hepatocyte spheroids formed by rocked technique maintain differentiated hepatocyte gene expression and function. Hepatology 49:578
Fukuda J, Nakazawa K (2011) Hepatocyte spheroid arrays inside microwells connected with microchannels. Biomicrofluidics 5:22205
Bhatia SN, Yarmush ML, Toner M (1997) Controlling cell interactions by micropatterning in co-cultures: hepatocytes and 3T3 fibroblasts. J Biomed Mater Res 34:189
Corlu A, Ilyin G, Cariou S, Lamy I, Loyer P, Guguen-Guillouzo C (1997) The coculture: a system for studying the regulation of liver differentiation/proliferation activity and its control. Cell Biol Toxicol 13:235
Tsuda Y, Kikuchi A, Yamato M, Nakao A, Sakurai Y, Umezu M, Okano T (2005) The use of patterned dual thermoresponsive surfaces for the collective recovery as co-cultured cell sheets. Biomaterials 26:1885
Khetani SR, Bhatia SN (2007) Microscale culture of human liver cells for drug development. Nat Biotechnol 26:120
Hui EE, Bhatia SN (2007) Silicon microchips for manipulating cell-cell interaction. Proc Natl Acad Sci U S A 104:5722
Kidambi S, Sheng L, Yarmush ML, Toner M, Lee I, Chan C (2007) Patterned co-culture of primary hepatocytes and fibroblasts using polyelectrolyte multilayer templates. Macromol Biosci 7:344
Elloumi Hannachi I Itoga K Kumashiro Y Kobayashi J Yamato M Okano T (2009) Fabrication of transferable micropatterned-co-cultured cell sheets with microcontact printing. Biomaterials 30:5427
Harimoto M, Yamato M, Hirose M, Takahashi C, Isoi Y, Kikuchi A, Okano T (2002) Novel approach for achieving double-layered cell sheets co-culture: overlaying endothelial cell sheets onto monolayer hepatocytes utilizing temperature-responsive culture dishes. J Biomed Mater Res 62:464
Kim K, Ohashi K, Utoh R, Kano K, Okano T (2012) Preserved liver-specific functions of hepatocytes in 3D co-culture with endothelial cell sheets. Biomaterials 33:1406
Yamada M, Utoh R, Ohashi K, Tatsumi K, Yamatoc M, Okano T, Seki M (2012) Controlled formation of heterotypic hepatic micro-organoids in anisotropic hydrogel microfibers for long-term preservation of liver-specific functions. Biomaterials 33:8304
Kidambi S, Yarmush RS, Novik E, Chao P, Yarmush ML, Nahmias Y (2009) Oxygen-mediated enhancement of primary hepatocyte metabolism, functional polarization, gene expression, and drug clearance. Proc Natl Acad Sci U S A 106:15714
Cho CH, Park J, Nagrath D, Tilles AW, Berthiaume F, Toner M, Yarmush ML (2007) Oxygen uptake rates and liver-specific functions of hepatocyte and 3T3 fibroblast co-cultures. Biotechnol Bioeng 97:188
Onoe H, Okitsu T, Itou A, Kato-Negishi M, Gojo R, Kiriya D, Sato K, Miura S, Iwanaga S, Kuribayashi-Shigetomi K, Matsunaga YT, Shimoyama Y, Takeuchi S (2013) Metre-long cell-laden microfibres exhibit tissue morphologies and functions. Nat Mater 12:584
Kang E, Jeong GS, Choi YY, Lee KH, Khademhosseini A, Lee SH (2011) Digitally tunable physicochemical coding of material composition and topography in continuous microfibres. Nat Mater 10:877
Panda P, Ali S, Lo E, Chung BG, Hatton TA, Khademhosseini A, Doyle PS (2008) Stop-flow lithography to generate cell-laden microgel particles. Lab Chip 8:1056
Chung SE, Park W, Shin S, Lee SA, Kwon S (2008) Guided and fluidic self-assembly of microstructures using railed microfluidic channels. Nat Mater 7:581
Miyama A, Yamada M, Sugaya S, Seki M (2013) A droplet-based microfluidic process to produce yarn-ball-shaped hydrogel microbeads. RSC Adv 3:12299
Sugaya S, Yamada M, Hori A, Seki M (2013) Microfluidic production of single micrometer-sized hydrogel beads utilizing droplet dissolution in a polar solvent. Biomicrofluidics 7:54120
Yuan B, Jin Y, Sun Y, Wang D, Sun J, Wang Z, Zhang W, Jiang X (2012) A strategy for depositing different types of cells in three dimensions to mimic tubular structures in tissues. Adv Mater 24:890
Santos MI, Tuzlakoglu K, Fuchs S, Gomes ME, Peters K, Unger RE, Piskin E, Reis RL, Kirkpatrick CJ (2008) Endothelial cell colonization and angiogenic potential of combined nano- and micro-fibrous scaffolds for bone tissue engineering. Biomaterials 29:4306
Pataky K, Braschler T, Negro A, Renaud P, Lutolf MP, Brugger J (2012) Microdrop printing of hydrogel bioinks into 3D tissue-like geometries. Adv Mater 24:391
Iwase M, Yamada M, Seki M (2012) Construction of vascular tissues via multilayer cell deposition inside hydrogel microchannels. Proc MicroTAS 2012:572
Ling Y, Rubin J, Deng Y, Huang C, Demirci U, Karp JM, Khademhosseini A (2007) A cell-laden microfluidic hydrogel. Lab Chip 7:756
Acknowledgments
We would like to thank Dr. S. Sugaya, Dr. R. Utoh, Mr. M. Iwase, Mr. Y. Kitagawa, Ms. E. Yamada, Mr. Y. Nagamuna, Ms. A. Kobayashi, Ms. A. Miyama, Mr. Y. Yajima, Ms. A. Hori for their contribution in conducting experiments. This study was supported in part by Grants-in-aid for Scientific Research (KAKENHI 23106007, 23700554, and 30546784) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Japan
About this chapter
Cite this chapter
Yamada, M., Seki, M. (2015). High-Throughput Cell Assembly Featuring Heterogeneous Hydrogels Produced by Using Microfluidic Devices. In: Arai, T., Arai, F., Yamato, M. (eds) Hyper Bio Assembler for 3D Cellular Systems. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55297-0_8
Download citation
DOI: https://doi.org/10.1007/978-4-431-55297-0_8
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55296-3
Online ISBN: 978-4-431-55297-0
eBook Packages: EngineeringEngineering (R0)