Abstract
Recent data have provided important clues about the molecular mechanisms underlying retinal neurodegenerative diseases, including retinal detachment (RD). Photoreceptor cell death causes various types of cell death such as apoptosis, necrosis, autophagy, and necroptosis. Apoptosis is the major type of photoreceptor death in RD and is the most defined type in experimental and clinical settings. Most cell death in vertebrates proceeds via the mitochondrial pathway of apoptosis. Mitochondria contain proapoptotic factors such as cytochrome c and AIF in their intermembrane space. Furthermore, mitochondrial membrane permeabilization (MMP) is a critical event during apoptosis, representing the “point of no return” of the lethal process. Modern medicine is developing an increasing number of treatments for neurodegenerative disease, but no neuroprotective treatment has yet been established for RD. This chapter briefly reviews the mechanisms of cell death and neuroprotection for RD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keyword
1 Introduction
Photoreceptor cell death is the ultimate cause of visual loss in various retinal disorders including retinal detachment (RD) and has been thought to occur mainly through apoptosis. Photoreceptor cells die when they are physically separated from the underlying retinal pigment epithelium (RPE) and choroidal vessels, which provide metabolic support to the outer layer of the retina. Retinal detachment occurs in various retinal disorders, including age-related macular degeneration (AMD) [1], diabetic retinopathy [2], as well as rhegmatogenous, tractional, and exudative retinal detachment (RD) [3]. Although surgery is carried out to reattach the retina, only two-fifths of patients with rhegmatogenous RD involving the macula recover 20/40 or better vision [4]. Although various pathological changes occur in detached retina, studies on experimental models and human patient samples have shown that photoreceptor cell death is immediately induced as early as 12 h and peaks at around 2–3 days after RD [5]. Moreover, retinal imaging by optical coherence tomography has demonstrated that the microstructure of foveal photoreceptor cells is a critical factor predicting better visual function in patients who received successful RD repair [6]. These findings suggest that loss of photoreceptor cells may be an important cause of vision loss after RD. Therefore, identification of the mechanisms underlying photoreceptor cell death is critical to developing new treatment strategies for retinal disorders associated with RD. Apoptosis is the most characterized form of programmed cell death, where caspases play a central role for its induction. In experimental models of RD, dying photoreceptor cells exhibit the activation of caspases; however, there is a paradox that caspase inhibition alone does not provide a sufficient protection against photoreceptor cell loss, suggesting that there are other ways to die.
Therapeutic targeting of apoptosis may make more conceptual sense compared to necrosis, as apoptosis is a delayed event and an energy-dependent process. Mitochondria are considered as the central regulators of apoptotic cell death in vertebrates. In various paradigms of cell death, mitochondrial membrane permeabilization (MMP) delimits the frontier between life and death (Fig. 19.1). Mitochondria control the intrinsic pathway of apoptosis, in which MMP ignites the activation of caspases and other catabolic enzymes, and mitochondria participate in the extrinsic pathway of apoptosis, in which they amplify the self-destructive process [7–9]. Irrespective of its initiation at the inner or outer mitochondrial membrane, MMP culminates in the functional (dissipation of the mitochondrial membrane potential, shutdown of ATP synthesis, redox imbalance) and structural (reorganization of cristae, release of toxic intermembrane space proteins into the cytosol) collapse of mitochondria. MMP has a profound impact on cellular metabolism, activates caspase-dependent and caspase-independent executioner mechanisms, and finally results in the demise of the cell [10, 11]. The lethal consequences of MMP relate to the critical position occupied by the mitochondria in cellular bioenergetics and the release of proapoptotic proteins into the cytosol and the nucleus. Proapoptotic proteins liberated as a consequence of MMP include activators of the caspase cascade (e.g., cytochrome c) as well as caspase-independent death effectors (e.g., apoptosis-inducing factor (AIF) and endonuclease G) [12, 13]. Indeed, MMP is the main checkpoint of programmed cell death, and lethal pathways of signal transduction are often activated in neurodegenerative diseases. Hence, pharmacological agents that target mitochondria to subvert MMP are being evaluated as therapeutic approaches for treatment for neurodegenerative RD. Recent accumulating evidence also demonstrates that non-apoptotic forms of cell death, such as autophagic cell death and necrosis, are also regulated by specific molecular machinery, such as those mediated by autophagy-related proteins and receptor-interacting protein kinases, respectively. Here we summarize the current knowledge of cell death signaling and its roles in photoreceptor cell death after RD. A body of studies indicate that not only apoptotic but also autophagic and necrotic signaling are involved in photoreceptor cell death after RD. We summarized the important checkpoints of photoreceptor cell death and reviewed the current concepts on neuroprotection for RD.
2 Mechanism of Photoreceptor Apoptotic Cell Death
2.1 Mitochondrial Outer Membrane Permeabilization
MMP may originate at the outer membrane through at least two distinct mechanisms. These include the activation of proapoptotic proteins of the Bcl-2 family (e.g., Bax, Bak) to build up multimeric channels, allowing for the release of intermembrane space proteins [14], and formation of lipidic pores due to a direct interaction between proapoptotic Bcl-2 family members (e.g., Bax, truncated Bid) and lipids contained in mitochondrial membranes [11, 15, 16]. Outer membrane permeabilization also occurs upon its physical rupture, be it induced accidentally or as part of a regulated mechanism originating at the inner membrane (the so-called mitochondrial permeability transition). Outer membrane permeabilization culminates in the release of proapoptotic intermembrane space proteins, which trigger the execution process of apoptotic cell death.
2.2 Mitochondrial Inner Membrane Permeabilization
Mitochondrial membrane permeabilization may also start at the inner membrane. In contrast to the outer membrane, the inner membrane from healthy cells is nearly impermeable to small solutes and ions. When inner membrane impermeability is lost, for instance following the opening of the so-called permeability transition pore complex (PTPC), solutes enter the mitochondrial matrix, accompanied by a net influx of water. The resulting osmotic imbalance provokes swelling of the matrix, followed by the rupture of both mitochondrial membranes. This process is known as mitochondrial permeability transition.
2.3 Importance of Caspase-Dependent Pathways on Neurodegenerative Disease
Cysteine aspartate-specific proteases or caspases are the central molecules involved in initiation and execution of apoptosis [17]. Caspases are processed through proteolytic cleavage at the sites containing aspartate residue. Mitochondria contain cytochrome c and caspase-9 in the intermembrane space, and these are liberated into cytoplasm after apoptotic insults. Cytochrome c forms apoptosome in the presence of ATP along with Apaf-1 and caspase-9, initiating the activation of caspase cascade [7, 8, 18]. The “forebrain over growth” (fog) mutation leads to an autosomal recessive neural tube closure defect due to the near-to-complete lack of Apaf-1 expression [19, 20]. However, a complete deficiency in Apaf-1 usually results in perinatal lethality, while fog/fog mice readily survive into adulthood [20, 21], allowing to assess the role of Apaf-1 and Apaf-1-dependent cytochrome c-mediated caspase activation in neuronal apoptosis. Apaf-1 deficiency reduced the RD-induced neuronal photoreceptor apoptosis, as assessed by TUNEL staining [22]. Therefore capsizes and related molecules offer opportunity to salvage the apoptotic cells by targeting them using anti-caspase therapy for neuroprotection.
2.4 Importance of AIF in Caspase-Independent Pathways on Neurodegenerative Disease
AIF is a 67 kDa flavoprotein in mammals and highly conserved among mammalian species (>95 % amino acid identity between mouse and human) and bears a highly significant homology with flavoprotein oxidoreductases from all eukaryotic and prokaryotic kingdoms in its C-terminal portion [23, 24]. AIF is normally confined to the mitochondrial intermembrane space; however, AIF translocates to the cytosol and to the nucleus after apoptotic insults (Fig. 19.1) [23–25]. Harlequin (Hq) mice exhibit an X chromosome-linked ataxia due to the progressive degeneration of terminally differentiated cerebellar neurons [26, 27]. The Hq mutation has been identified as a proviral insertion in the apoptosis-inducing factor (Aif) gene, also known as programmed cell death 8 (pdcd8), causing about 80 % reduction in AIF expression [27]. In contrast to Aif knockout mice (which die in utero) [28], Hq mice are born at normal Mendelian ratios and are healthy until the age of 3 months. After the apoptotic insult mediated by RD, Hq/Y retinas exhibited significantly less TUNEL+ apoptotic neural cells than wild-type controls and exhibited a reduced cell loss in the retina [22]. The similar neuroprotective effects were observed in brain ischemia in adult [29] and neonate [30]. Further research on AIF and caspase-independent pathways may reveal novel therapeutic target for neuroprotection.
3 Mechanism of Non-apoptotic Cell Death
Autophagy (Greek for “self-eating”) is a process by which cell’s own components such as macromolecules (e.g., proteins, lipids, and nucleic acids) and organelles (e.g., mitochondria) are degraded by the lysosome [31]. Macroautophagy (hereafter referred to autophagy) is the best-characterized autophagy pathway and involves the formation of autophagosomes and autolysosomes. Autophagosome is a double- or multi-membrane vacuole that sequesters cytoplasmic materials and fuses with lysosomes to form autolysosome, where its content is degraded. It is induced by nutrient starvation in order to provide recycled energy and eliminate damaged organelles [32]. From the genetic screening of autophagy-defective mutants in yeast, Tsukada, Ohsumi, and colleagues discovered a set of autophagy-related (Atg) genes, most of which have mammalian homologues [31, 33]. Although previous morphological studies identified accumulation of numerous autophagosomes/autolysosomes in dying cells, the roles of autophagy, either promoting or protecting against cell death, have been controversial. In specific circumstances, autophagy appears to mediate cell death via excessive self-degradation. Nonetheless, accumulating evidence has shown that autophagy is crucial for cell survival by regulating the turnover of intracellular contents in normal and most pathological conditions.
Although necrosis (Greek for “dead”) was traditionally thought to be an uncontrolled process of cell death, it is now known to also have regulated components in certain instances. This regulated type of necrosis was discovered from the extensive studies of death receptor-induced cell death. Laster and colleagues observed that TNF-α caused not only apoptosis but also necrosis depending on cell types [34]. Intriguingly, Vercammen and colleagues demonstrated that, when death receptor-induced apoptosis is suppressed by the caspase inhibitor, the cells undergo an alternative necrotic cell death in murine L929 fibrosarcoma cells [35]. Twelve years later, Holler and colleagues identified that this death receptor-induced necrosis is mediated by the activation of receptor-interacting protein 1 (RIP1) [36]. Furthermore, three independent studies recently discovered that RIP3 is a crucial regulator of RIP1 kinase activation and subsequent necrosis. These advances in understanding the molecular basis of necrosis have revealed previously unrecognized roles of necrosis in health and various diseases including retinal degeneration [37, 38]. This RIP kinase-dependent regulated necrosis is termed as “necroptosis” or “programmed necrosis.” However, in order to avoid confusion, we here express it descriptively as “RIP kinase-dependent necrosis” according to recent studies [37–39].
4 Inflammation and Cell Death
Cytokines and chemokines are released in response to tissue injury and mediate cell survival/death and inflammation. The vitreous fluid from patients with RD contains substantially higher levels of TNF-α, IL-1β, IL-6, IL-8, and MCP-1, compared to samples from patients without RD. Furthermore, Nakazawa and colleagues showed that the mRNA levels of TNF-α, IL-1β, and MCP-1 are upregulated as early as 1 h after experimental RD, suggesting that these cytokines/chemokines may actively contribute to the pathology of RD [40, 41]. Indeed, as described above, TNF-α induces photoreceptor cell death after RD, along with the activation of caspase-8 and RIP kinase. In addition, blockade of TNF-α suppresses the retinal infiltration of macrophages and microglial cells [40]. Therefore, not only pro-death but also proinflammatory signals of TNF-α could be involved in the photoreceptor loss after RD. In another study by Nakazawa and colleagues, genetic deficiency of Mcp1 substantially reduces macrophage/microglia recruitment and attenuates photoreceptor cell loss after RD. In primary retinal mixed cultures, MCP-1 treatment induces photoreceptor cell loss; however, this cytotoxic effect is abolished by the removal of CD11b-positive macrophages/microglia from the retinal cultures [40]. These findings suggest that MCP-1 mediates photoreceptor cell death indirectly through activation and recruitment of macrophages/microglia after RD. Protection against RD-induced photoreceptor cell death is also obtained by genetic deletion of Cd11b/Cd18, an integrin critical for leukocyte recruitment, or the treatment with systemic steroids [40, 42], further confirming the pivotal role of inflammation in photoreceptor cell loss after RD. However, it should be noted that inflammation is not always detrimental, but also maintains tissue homeostasis by removing waste materials and dead cells.
Nucleic acids, proteins, and lipids released from dying or dead cells can initiate or modulate immune response, and these molecules are known as damage-associated molecular patterns (DAMPs). Among these, extracellular release of ATP is a key process to recruit macrophages to the site of injury (Fig. 19.2) [43]. ATP is secreted actively by exocytosis, anion channels, or transporters in an early phase of apoptosis or released passively via the loss of membrane integrity. ATP activates inflammasome through its action on P2X7 or mediates cell death via the formation of P2X7-dependent pore and caspase activation. Notomi and colleagues showed that intraocular injection of ATP induces photoreceptor cell death through the activation of P2X7 in mice and primary retinal cultures [44, 45]. In addition, extracellular ATP is substantially increased in the vitreous of AMD patients associated with subretinal hemorrhage [45]. High-mobility group box 1 (HMGB1), a nuclear protein that regulates transcription, has a divergent extracellular function as DAMP. HMGB1 is passively released from necrotic cells, but not from apoptotic cells. Arimura and colleagues showed that the extracellular release of HMGB1 occurs in human patients and experimental models of RD [46], suggesting that HMGB1 released from dying or dead photoreceptor cells may modulate retinal inflammatory response and degeneration after RD. Besides HMGB1, multiple proteins and nucleic acids such as S100, HSP, histones, DNA, and mRNA augment cytokine production and modulate tissue injury when they are released into the extracellular space. Investigating the roles of these DAMPs in retinal degeneration will lead to better understanding of the pathogenesis of the diseases and identification of novel therapeutic targets.
5 Neuroprotection Against Photoreceptor Cell Death for RD
5.1 MMP and Mitochondrial Release of Proapoptotic Factors
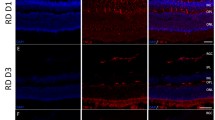
Mitochondrial membrane permeabilization (MMP) is a critical event during apoptosis, representing the “point of no return” of the lethal process. Cytochrome c is released from the mitochondria upon MMP and binds to cytosolic apoptotic protease-activating factor-1 (Apaf-1) to induce its dimerization and a conformational change [47]. Apaf-1 then oligomerizes into apoptosomes that recruit and activate caspase-9 followed by serial activation of caspase-3 and other apoptosis-execution molecules [48, 49]. However, MMP may cause cell death even if caspases are inhibited [50] and a broad caspase inhibitor, Z-VAD-fmk, fails to inhibit neuronal apoptosis [5, 51]. AIF is a caspase-independent apoptogenic factor and is normally confined to the mitochondrial intermembrane space [23]. During apoptosis, AIF translocates to the cytosol and then to the nucleus where it triggers peripheral chromatin condensation and interacts with cyclophilin A to generate a DNAse complex that is responsible for the so-called “large-scale” DNA degradation to fragments of approximately 50 kbp [23, 52]. AIF translocation has been reported for mammalian neural cells in numerous cases, for instance for photoreceptors upon retinal detachment (RD) [5], dopaminergic neurons in models of Parkinson’s disease [53] including phenylpyridinium toxicity [54], and photoreceptor cells in retinitis pigmentosa [55]. Pharmacological targeting of MMP inhibition may limit the release of these proapoptotic intermembrane space proteins into the cytosol (Fig. 19.1).
5.2 Growth Factor-Dependent Survival of Neuronal Cells
An increasing number of growth factors and nerve growth factor has been shown to support cell survival in various apoptotic insult in neuronal cells [56]. These include nerve growth factor family (NGF, BDNF, etc.), basic fibroblast growth factor (bFGF), and vascular permeability factor (VEGF). BDNF and bFGF have shown substantial neuroprotective effects in neuronal apoptosis of retinal detachment [5], brain ischemia, and Parkinson’s disease. These growth factors activated their counter receptors (i.e., NGF receptors) and stimulate cellular intrinsic pathways (i.e., activation of PI3K/Akt signaling pathways and mitogen-activated protein kinase (MAPK) pathways which leads to the upregulation of protein expression) [57]. Recently pigment epithelium-derived factor (PEDF) has also been reported to be neuroprotective in retinal degeneration in retinitis pigmentosa. While the receptor of PEDF remains unclear, lentivirus-mediated retinal gene transfer of PEDF inhibited MMP as examined by mitochondrial potential, inhibiting subsequent AIF translocation from mitochondria to nucleus in neural cells [51].
5.3 Overexpression of Bcl-2 Family Proteins for Inhibiting MMP for Neuroprotection
Bcl-2 family proteins are essential regulators of apoptosis and over 30 members have been discovered that share homology in Bcl-2 homology regions (BH1 to BH4) [18, 58]. These can be grouped into Bcl-2-like survival factors (antiapoptotic) [59, 60] and Bcl-2-like death factors (proapoptotic) [59, 61, 62]. The Bcl-2-like survival factors possess BH1–BH4 domains that mediate their prosurvival function and gate the release of apoptotic proteins by maintaining the MMP. The proapoptotic members of Bcl-2 family protein promote MMP via perturbation of mitochondrial membrane integrity and the interactions with other proapoptotic and antiapoptotic factors and hetero-dimerize with MMP-related proteins such as adenine nucleotide translocator (ANT) and voltage-dependent anion channel (VDAC). The overexpression of antiapoptotic members of Bcl-2 family protein has been reported to be neuroprotective [18]. Bcl-2 overexpression protects against neuron loss within the ischemic model, inhibiting cytochrome c accumulation and caspase-3 activation [63]. Moreover Bcl-2 transfection via herpes simplex virus blocks AIF translocation from mitochondria to nucleus [64]. The ratio of antiapoptotic and proapoptotic proteins may determine the fate of neurons by antagonizing and competing each other [15, 65].
5.4 A Cell-Permeable Peptide Corresponding to the BH-4 Domain of Bcl-XL Inhibits Neuronal Apoptosis via Blocking MMP
The recent reports indicate that (at least) two post-mitochondrial cell death pathways participate in neuronal apoptosis, namely, caspase-independent apoptosis (e.g., AIF and endonuclease G) and cytochrome c-dependent caspase activation in the apoptosome. Both AIF and the apoptosome are activated as a result of MMP. Recently, a cell-permeable MMP-inhibitory recombinant fusion protein, HIV-TAT BH4, composed of the HIV-TAT plasma membrane translocation domain and the antiapoptotic Bcl-XL-derived BH4 domain, has been reported to inhibit neuronal apoptosis [22, 66–68]. Cell-penetrating peptide constructs such as HIV-1 TAT basic domain and related peptides have been developed to deliver bioactive peptides into cells [67–73]. Rapid and receptor-independent uptake of TAT-conjugated peptides has been demonstrated to occur in vitro and in vivo [67]. Intraperitoneal injection of HIV-TAT protein led to its distribution into neuronal cells (in vivo), as this was seen after addition of HIV-TAT BH4 to primary neuronal cell cultures (in vitro) [22]. These fusion proteins resulted in robust protein transduction in neurons and inhibited caspase-3 activation in ischemic neurons [70], AIF translocation in neonatal brain damage [68], and AIF and cytochrome c translocation in retinal cells [22]. The Bcl-2 family proteins constitute a major life-or-death decisive point that can be manipulated to target the neuroprotective therapy.
5.5 A Novel Mechanism of HIV Protease Inhibitors for Neuroprotection Through Inhibition of Mitochondrial Apoptosis
HIV protease inhibitors (PIs) have originally been designed to block the formation of HIV viral proteins by viral proteases and are currently administered to millions of patients with HIV worldwide [74]. Recently, it has been reported that PIs do not only inhibit virus replication but also suppress CD4+ T lymphocyte apoptosis at concentrations similar to those that are achieved in the plasma of PI-treated patients [75]. In several cases, HIV-infected individuals recovered normal levels of circulating CD4+ T cells upon PI treatment although the therapy had no effects on the viral titers, suggesting that PIs might inhibit apoptosis of CD4+ T cells in vivo, independently from their effect on HIV replication [74, 76, 77]. Several groups investigated the mechanisms by which PIs inhibit apoptosis. Altered transcriptional regulation of regulatory proteins [78] and direct inhibition of caspase-1 [79] or calpain [80] have been reported. However, these proposed mechanisms may not explain the ability of PIs to block cell death induced by a wide range of apoptotic insults [75] and are not compatible with other studies reporting poor effects of PIs on effector caspases or the net synthesis of apoptosis regulators [81]. Recently, PIs were shown to inhibit the MMP-dependent release of cytochrome c [81, 82] via direct binding to and inhibition of the adenine nucleotide translocator, a protein from the inner mitochondrial membrane that can form pores and mediate MMP [83]. However the protective effects of PIs contrast with the observation that pharmacological caspase inhibitors largely fail to inhibit cell death [84]. PIs may simultaneously block caspase-dependent (e.g., activation of caspase-9 and caspase-3) and caspase-independent cell death pathways (e.g., AIF translocation) via blocking MMP, presumably inhibiting the adenine nucleotide translocator [22]. In our studies, PI had substantial antiapoptotic and neuroprotective effect on retinal photoreceptors after RD, in a non-virus-associated disease with excessive apoptosis. Paradoxically, PIs may also induce apoptosis, particularly of transformed cells, when used at higher doses [78, 85]. Further studies may provide the mechanistic insight of PIs effect on apoptosis and increased application for neuroprotection.
5.6 P2X7 Receptor (P2RX7) Blockade by Brilliant Blue G (BBG)
Recently, adenosine-5′-triphosphate (ATP) has been discovered as a major extracellular messenger that can contribute to lethal signaling [86]. Neuronal cells release intracellular ATP to extracellular space under stress or cell death. Extracellular ATP can act on purinergic receptors, which are classified into two classes, the ionotropic, ligand-gated P2X receptors and the metabotropic, G protein-coupled P2Y receptors [87]. Among the seven subtypes of mammalian P2X receptors, the P2X7 receptor (P2RX7) differs from other P2X receptor subtypes by its long cytoplasmic, carboxy-terminal tail (240 amino acids) and mediates cellular signals that can trigger cell death. In the retina, P2RX7 is expressed in both inner and outer retinal neurons, including retinal ganglion cells [88] and photoreceptors [89]. P2RX7 has physiological functions as a neurotransmitter receptor in the retina [89], while photoreceptors have been shown to undergo apoptosis by excessive ATP [44, 45, 90]. Recently, it has been shown that photoreceptor apoptosis involves P2RX7 activation with caspase-8 and caspase-9 cleavage and mitochondrio-nuclear translocation of AIF [44]. Moreover, photoreceptor apoptosis can be attenuated by Brilliant Blue G, a pharmacological P2RX7 antagonist, by blocking ATP acting on P2RX7 (Fig. 19.2) [45]. Indeed, BBG administration can confer neuroprotective effects in several models of Alzheimer’s disease, Parkinson’s disease, and spinal cord injury [37–39] as well as in the retina [35, 40, 41]. BBG is also known as an adjuvant approved for intraoperative use in ocular surgery. In chromovitrectomy, BBG is introduced to improve the visualization of intraocular tissues for specific procedures, such as internal limiting membrane (ILM) peeling during vitrectomy [42, 43]. Various retinal diseases could be linked to important elevations of extracellular ATP, accelerating neuronal cell death and irreversible tissue damage. Furthermore, any type of photoreceptor cell death could release ATP, making positive feed forward loop to worsen the surrounding tissue damage [45]. P2RX7 antagonists including BBG may have a potential neuroprotective therapeutic effect in RD and other retinal diseases with excessive extracellular ATP by blocking cell death loop.
5.7 A Novel Neuroprotection for Necrosis
Although apoptosis is a predominant form cell death after RD, previous morphological analysis described the presence of necrosis in RD-induced photoreceptor cell death [91]. However, necrosis was not considered as a therapeutic target for a long period, because of the general concept that necrosis is an uncontrolled process of cell death. During photoreceptor cell death after RD, death ligands such as TNF-α and Fas-L, which mediate not only apoptosis but also necrosis, are upregulated and contribute to photoreceptor cell loss [40, 92]. However, caspase inhibition by the pan-caspase inhibitor Z-VAD is not sufficient to prevent photoreceptor cell loss after RD [5]. Given the emerging roles of RIP kinase-dependent necrosis especially in conditions where caspase pathway is inhibited, we hypothesized that RIP kinase may act as an alternative pathway of photoreceptor cell death after RD. Trichonas and colleagues demonstrated that, while RIP3 is barely detectable in the normal retina, its expression increases over tenfold in the retina after RD [41]. Because the expression levels of RIP3 have been shown to correlate with necrotic responses in various cell lines, the increased RIP3 may sensitize cells to undergo necrosis in these pathological conditions. Furthermore, our morphological analysis using TEM showed that treatment with Z-VAD decreases apoptosis but substantially increases necrotic cell death of photoreceptors [38]. These necrotic changes after caspase inhibition are rescued by additional Nec-1 treatment or Rip3 deficiency. These findings clearly demonstrate that RIP kinase-dependent necrosis is an essential pathway for photoreceptor cell death after RD, which acts in concert with caspase-dependent apoptosis [38]. These findings suggest that RIP kinase is critical in medicating necrosis in RD and that targeting RIP kinase by itself or in combination with apoptosis inhibitors may be a potential strategy for treatment of retinal disorders.
6 Conclusions
MMP is a pivotal event in the pathogenesis of acute and chronic neurodegenerative disorders. Thus various neurodegenerative disorders that involve apoptosis could be amenable to drug- and gene-based therapies that target MMP. The existence of multiple cell death pathways with both overlapping and cross-talking molecular mechanisms may explain the observation that inhibition of one such pathway may enhance alternative ones. These information suggest that neuroprotection should optimally be directed at multiple and/or comprehensive targets. The therapeutic concept to target mitochondria, especially MMP, to block the release of multiple proapoptotic proteins and protect energy metabolism is substantially valuable for neuroprotection. A combination therapy with different approach targeting apoptosis, autophagy, necrosis, or inflammation may have additive effects for further application for neuroprotection. Photoreceptor cell death is the ultimate cause of vision loss in RD and other retinal disorders. The regulatory roles of mitochondria in each cell death mechanism and the interaction between cell death mechanisms during retinal degeneration warrant further investigation. We believe that further studies of the complex molecular mechanisms underlying photoreceptor cell death will lead to better understanding of the pathophysiology of RD and developing novel therapeutics for preventing vision deficits after RD.
References
Dunaief JL, Dentchev T, Ying GS, Milam AH (2002) The role of apoptosis in age-related macular degeneration. Arch Ophthalmol 120(11):1435–1442
Barber AJ, Lieth E, Khin SA, Antonetti DA, Buchanan AG, Gardner TW (1998) Neural apoptosis in the retina during experimental and human diabetes. Early onset and effect of insulin. J Clin Invest 102(4):783–791
Cook B, Lewis GP, Fisher SK, Adler R (1995) Apoptotic photoreceptor degeneration in experimental retinal detachment. Invest Ophthalmol Vis Sci 36(6):990–996
Campo RV, Sipperley JO, Sneed SR, Park DW, Dugel PU, Jacobsen J, Flindall RJ (1999) Pars plana vitrectomy without scleral buckle for pseudophakic retinal detachments. Ophthalmology 106(9):1811–1815, discussion 1816
Hisatomi T, Sakamoto T, Murata T, Yamanaka I, Oshima Y, Hata Y, Ishibashi T, Inomata H, Susin SA, Kroemer G (2001) Relocalization of apoptosis-inducing factor in photoreceptor apoptosis induced by retinal detachment in vivo. Am J Pathol 158(4):1271–1278
Schocket LS, Witkin AJ, Fujimoto JG, Ko TH, Schuman JS, Rogers AH, Baumal C, Reichel E, Duker JS (2006) Ultrahigh-resolution optical coherence tomography in patients with decreased visual acuity after retinal detachment repair. Ophthalmology 113(4):666–672
Kroemer G, Zamzami N, Susin SA (1997) Mitochondrial control of apoptosis. Immunol Today 18(1):44–51
Green DR, Reed JC (1998) Mitochondria and apoptosis. Science 281(5381):1309–1312
Hengartner MO (2000) The biochemistry of apoptosis. Nature 407(6805):770–776
Ferri KF, Kroemer G (2001) Mitochondria–the suicide organelles. Bioessays 23(2):111–115
Galluzzi L, Vitale I, Kepp O, Seror C, Hangen E, Perfettini JL, Modjtahedi N, Kroemer G (2008) Methods to dissect mitochondrial membrane permeabilization in the course of apoptosis. Methods Enzymol 442:355–374
Garrido C, Galluzzi L, Brunet M, Puig PE, Didelot C, Kroemer G (2006) Mechanisms of cytochrome c release from mitochondria. Cell Death Differ 13(9):1423–1433
Li LY, Luo X, Wang X (2001) Endonuclease G is an apoptotic DNase when released from mitochondria. Nature 412(6842):95–99
Zamzami N, Kroemer G (2001) The mitochondrion in apoptosis: how Pandora’s box opens. Nat Rev Mol Cell Biol 2(1):67–71
Green DR, Kroemer G (2004) The pathophysiology of mitochondrial cell death. Science 305(5684):626–629
Kroemer G, Galluzzi L, Brenner C (2007) Mitochondrial membrane permeabilization in cell death. Physiol Rev 87(1):99–163
Riedl SJ, Shi Y (2004) Molecular mechanisms of caspase regulation during apoptosis. Nat Rev Mol Cell Biol 5(11):897–907
Mehta SL, Manhas N, Raghubir R (2007) Molecular targets in cerebral ischemia for developing novel therapeutics. Brain Res Rev 54(1):34–66
Harris BS, Franz T, Ullrich S, Cook S, Bronson RT, Davisson MT (1997) Forebrain overgrowth (fog): a new mutation in the mouse affecting neural tube development. Teratology 55(4):231–240
Honarpour N, Gilbert SL, Lahn BT, Wang X, Herz J (2001) Apaf-1 deficiency and neural tube closure defects are found in fog mice. Proc Natl Acad Sci U S A 98(17):9683–9687
Yoshida H, Kong YY, Yoshida R, Elia AJ, Hakem A, Hakem R, Penninger JM, Mak TW (1998) Apaf1 is required for mitochondrial pathways of apoptosis and brain development. Cell 94(6):739–750
Hisatomi T, Nakazawa T, Noda K, Almulki L, Miyahara S, Nakao S, Ito Y, She H, Kohno R, Michaud N, Ishibashi T, Hafezi-Moghadam A, Badley AD, Kroemer G, Miller JW (2008) HIV protease inhibitors provide neuroprotection through inhibition of mitochondrial apoptosis in mice. J Clin Invest 118(6):2025–2038
Susin SA, Lorenzo HK, Zamzami N, Marzo I, Snow BE, Brothers GM, Mangion J, Jacotot E, Costantini P, Loeffler M, Larochette N, Goodlett DR, Aebersold R, Siderovski DP, Penninger JM, Kroemer G (1999) Molecular characterization of mitochondrial apoptosis-inducing factor. Nature 397(6718):441–446
Lorenzo HK, Susin SA, Penninger J, Kroemer G (1999) Apoptosis inducing factor (AIF): a phylogenetically old, caspase-independent effector of cell death. Cell Death Differ 6(6):516–524
Daugas E, Susin SA, Zamzami N, Ferri KF, Irinopoulou T, Larochette N, Prevost MC, Leber B, Andrews D, Penninger J, Kroemer G (2000) Mitochondrio-nuclear translocation of AIF in apoptosis and necrosis. FASEB J 14(5):729–739
Barber BR (1971) Research news. Mouse News Lett 45:34–35
Klein JA, Longo-Guess CM, Rossmann MP, Seburn KL, Hurd RE, Frankel WN, Bronson RT, Ackerman SL (2002) The harlequin mouse mutation downregulates apoptosis-inducing factor. Nature 419(6905):367–374
Joza N, Oudit GY, Brown D, Benit P, Kassiri Z, Vahsen N, Benoit L, Patel MM, Nowikovsky K, Vassault A, Backx PH, Wada T, Kroemer G, Rustin P, Penninger JM (2005) Muscle-specific loss of apoptosis-inducing factor leads to mitochondrial dysfunction, skeletal muscle atrophy, and dilated cardiomyopathy. Mol Cell Biol 25(23):10261–10272
Culmsee C, Zhu C, Landshamer S, Becattini B, Wagner E, Pellecchia M, Blomgren K, Plesnila N (2005) Apoptosis-inducing factor triggered by poly(ADP-ribose) polymerase and Bid mediates neuronal cell death after oxygen–glucose deprivation and focal cerebral ischemia. J Neurosci 25(44):10262–10272
Zhu C, Wang X, Huang Z, Qiu L, Xu F, Vahsen N, Nilsson M, Eriksson PS, Hagberg H, Culmsee C, Plesnila N, Kroemer G, Blomgren K (2007) Apoptosis-inducing factor is a major contributor to neuronal loss induced by neonatal cerebral hypoxia-ischemia. Cell Death Differ 14(4):775–784, Epub 2006 Oct 2013
Mizushima N, Noda T, Yoshimori T, Tanaka Y, Ishii T, George MD, Klionsky DJ, Ohsumi M, Ohsumi Y (1998) A protein conjugation system essential for autophagy. Nature 395(6700):395–398
Schworer CM, Mortimore GE (1979) Glucagon-induced autophagy and proteolysis in rat liver: mediation by selective deprivation of intracellular amino acids. Proc Natl Acad Sci USA 76(7):3169–3173
Tsukada M, Ohsumi Y (1993) Isolation and characterization of autophagy-defective mutants of Saccharomyces cerevisiae. FEBS Lett 333(1–2):169–174
Laster SM, Wood JG, Gooding LR (1988) Tumor necrosis factor can induce both apoptotic and necrotic forms of cell lysis. J Immunol 141(8):2629–2634
Vercammen D, Beyaert R, Denecker G, Goossens V, Van Loo G, Declercq W, Grooten J, Fiers W, Vandenabeele P (1998) Inhibition of caspases increases the sensitivity of L929 cells to necrosis mediated by tumor necrosis factor. J Exp Med 187(9):1477–1485
Holler N, Zaru R, Micheau O, Thome M, Attinger A, Valitutti S, Bodmer JL, Schneider P, Seed B, Tschopp J (2000) Fas triggers an alternative, caspase-8-independent cell death pathway using the kinase RIP as effector molecule. Nat Immunol 1(6):489–495
Murakami Y, Matsumoto H, Roh M, Suzuki J, Hisatomi T, Ikeda Y, Miller JW, Vavvas DG (2012) Receptor interacting protein kinase mediates necrotic cone but not rod cell death in a mouse model of inherited degeneration. Proc Natl Acad Sci U S A 109(36):14598–14603
Murakami Y, Notomi S, Hisatomi T, Nakazawa T, Ishibashi T, Miller JW, Vavvas DG (2013) Photoreceptor cell death and rescue in retinal detachment and degenerations. Prog Retin Eye Res 37:114–140
Green DR, Oberst A, Dillon CP, Weinlich R, Salvesen GS (2011) RIPK-dependent necrosis and its regulation by caspases: a mystery in five acts. Mol Cell 44(1):9–16
Nakazawa T, Hisatomi T, Nakazawa C, Noda K, Maruyama K, She H, Matsubara A, Miyahara S, Nakao S, Yin Y, Benowitz L, Hafezi-Moghadam A, Miller JW (2007) Monocyte chemoattractant protein 1 mediates retinal detachment-induced photoreceptor apoptosis. Proc Natl Acad Sci U S A 104(7):2425–2430
Trichonas G, Murakami Y, Thanos A, Morizane Y, Kayama M, Debouck CM, Hisatomi T, Miller JW, Vavvas DG (2010) Receptor interacting protein kinases mediate retinal detachment-induced photoreceptor necrosis and compensate for inhibition of apoptosis. Proc Natl Acad Sci U S A 107(50):21695–21700
Nakazawa T, Kayama M, Ryu M, Kunikata H, Watanabe R, Yasuda M, Kinugawa J, Vavvas D, Miller JW (2011) Tumor necrosis factor-alpha mediates photoreceptor death in a rodent model of retinal detachment. Invest Ophthalmol Vis Sci 52(3):1384–1391
Davalos D, Grutzendler J, Yang G, Kim JV, Zuo Y, Jung S, Littman DR, Dustin ML, Gan WB (2005) ATP mediates rapid microglial response to local brain injury in vivo. Nat Neurosci 8(6):752–758
Notomi S, Hisatomi T, Kanemaru T, Takeda A, Ikeda Y, Enaida H, Kroemer G, Ishibashi T (2011) Critical involvement of extracellular ATP acting on P2RX7 purinergic receptors in photoreceptor cell death. Am J Pathol 179(6):2798–2809
Notomi S, Hisatomi T, Murakami Y, Terasaki H, Sonoda S, Asato R, Takeda A, Ikeda Y, Enaida H, Sakamoto T, Ishibashi T (2013) Dynamic increase in extracellular ATP accelerates photoreceptor cell apoptosis via ligation of P2RX7 in subretinal hemorrhage. PLoS One 8(1):e53338
Arimura N, Ki-i Y, Hashiguchi T, Kawahara K, Biswas KK, Nakamura M, Sonoda Y, Yamakiri K, Okubo A, Sakamoto T, Maruyama I (2009) Intraocular expression and release of high-mobility group box 1 protein in retinal detachment. Lab Invest 89(3):278–289
Bao Q, Riedl SJ, Shi Y (2005) Structure of Apaf-1 in the auto-inhibited form: a critical role for ADP. Cell Cycle 4(8):1001–1003
Bao Q, Shi Y (2007) Apoptosome: a platform for the activation of initiator caspases. Cell Death Differ 14(1):56–65
Acehan D, Jiang X, Morgan DG, Heuser JE, Wang X, Akey CW (2002) Three-dimensional structure of the apoptosome: implications for assembly, procaspase-9 binding, and activation. Mol Cell 9(2):423–432
Bouchier-Hayes L, Lartigue L, Newmeyer DD (2005) Mitochondria: pharmacological manipulation of cell death. J Clin Invest 115(10):2640–2647
Murakami Y, Ikeda Y, Yonemitsu Y, Onimaru M, Nakagawa K, Kohno R, Miyazaki M, Hisatomi T, Nakamura M, Yabe T, Hasegawa M, Ishibashi T, Sueishi K (2008) Inhibition of nuclear translocation of apoptosis-inducing factor is an essential mechanism of the neuroprotective activity of pigment epithelium-derived factor in a rat model of retinal degeneration. Am J Pathol 173(5):1326–1338
Cande C, Vahsen N, Kouranti I, Schmitt E, Daugas E, Spahr C, Luban J, Kroemer RT, Giordanetto F, Garrido C, Penninger JM, Kroemer G (2004) AIF and cyclophilin A cooperate in apoptosis-associated chromatinolysis. Oncogene 23(8):1514–1521
Wang H, Shimoji M, Yu SW, Dawson TM, Dawson VL (2003) Apoptosis inducing factor and PARP-mediated injury in the MPTP mouse model of Parkinson’s disease. Ann N Y Acad Sci 991:132–139
Chu CT, Zhu JH, Cao G, Signore A, Wang S, Chen J (2005) Apoptosis inducing factor mediates caspase-independent 1-methyl-4-phenylpyridinium toxicity in dopaminergic cells. J Neurochem 94(6):1685–1695
Sanges D, Comitato A, Tammaro R, Marigo V (2006) Apoptosis in retinal degeneration involves cross-talk between apoptosis-inducing factor (AIF) and caspase-12 and is blocked by calpain inhibitors. Proc Natl Acad Sci U S A 103(46):17366–17371
Chaum E (2003) Retinal neuroprotection by growth factors: a mechanistic perspective. J Cell Biochem 88(1):57–75
Bogaerts V, Theuns J, van Broeckhoven C (2008) Genetic findings in Parkinson’s disease and translation into treatment: a leading role for mitochondria? Genes Brain Behav 7(2):129–151
Borner C (2003) The Bcl-2 protein family: sensors and checkpoints for life-or-death decisions. Mol Immunol 39(11):615–647
Boise LH, Gonzalez-Garcia M, Postema CE, Ding L, Lindsten T, Turka LA, Mao X, Nunez G, Thompson CB (1993) Bcl-x, a bcl-2-related gene that functions as a dominant regulator of apoptotic cell death. Cell 74(4):597–608
Gibson L, Holmgreen SP, Huang DC, Bernard O, Copeland NG, Jenkins NA, Sutherland GR, Baker E, Adams JM, Cory S (1996) Bcl-w, a novel member of the bcl-2 family, promotes cell survival. Oncogene 13(4):665–675
Oltvai ZN, Milliman CL, Korsmeyer SJ (1993) Bcl-2 heterodimerizes in vivo with a conserved homolog, Bax, that accelerates programmed cell death. Cell 74(4):609–619
Inohara N, Ding L, Chen S, Nunez G (1997) Harakiri, a novel regulator of cell death, encodes a protein that activates apoptosis and interacts selectively with survival-promoting proteins Bcl-2 and Bcl-X(L). EMBO J 16(7):1686–1694
Zhao H, Yenari MA, Cheng D, Sapolsky RM, Steinberg GK (2003) Bcl-2 overexpression protects against neuron loss within the ischemic margin following experimental stroke and inhibits cytochrome c translocation and caspase-3 activity. J Neurochem 85(4):1026–1036
Zhao H, Yenari MA, Cheng D, Barreto-Chang OL, Sapolsky RM, Steinberg GK (2004) Bcl-2 transfection via herpes simplex virus blocks apoptosis-inducing factor translocation after focal ischemia in the rat. J Cereb Blood Flow Metab 24(6):681–692
Kroemer G, Reed JC (2000) Mitochondrial control of cell death. Nat Med 6(5):513–519
Asoh S, Ohsawa I, Mori T, Katsura K, Hiraide T, Katayama Y, Kimura M, Ozaki D, Yamagata K, Ohta S (2002) Protection against ischemic brain injury by protein therapeutics. Proc Natl Acad Sci U S A 99(26):17107–17112
Dietz GP, Kilic E, Bahr M (2002) Inhibition of neuronal apoptosis in vitro and in vivo using TAT-mediated protein transduction. Mol Cell Neurosci 21(1):29–37
Yin W, Cao G, Johnnides MJ, Signore AP, Luo Y, Hickey RW, Chen J (2006) TAT-mediated delivery of Bcl-xL protein is neuroprotective against neonatal hypoxic-ischemic brain injury via inhibition of caspases and AIF. Neurobiol Dis 21(2):358–371
Shimizu S, Konishi A, Kodama T, Tsujimoto Y (2000) BH4 domain of antiapoptotic Bcl-2 family members closes voltage-dependent anion channel and inhibits apoptotic mitochondrial changes and cell death. Proc Natl Acad Sci U S A 97(7):3100–3105
Cao G, Pei W, Ge H, Liang Q, Luo Y, Sharp FR, Lu A, Ran R, Graham SH, Chen J (2002) In vivo delivery of a Bcl-xL fusion protein containing the TAT protein transduction domain protects against ischemic brain injury and neuronal apoptosis. J Neurosci 22(13):5423–5431
Schwarze SR, Ho A, Vocero-Akbani A, Dowdy SF (1999) In vivo protein transduction: delivery of a biologically active protein into the mouse. Science 285(5433):1569–1572
Sugioka R, Shimizu S, Funatsu T, Tamagawa H, Sawa Y, Kawakami T, Tsujimoto Y (2003) BH4-domain peptide from Bcl-xL exerts anti-apoptotic activity in vivo. Oncogene 22(52):8432–8440
Hotchkiss RS, McConnell KW, Bullok K, Davis CG, Chang KC, Schwulst SJ, Dunne JC, Dietz GP, Bahr M, McDunn JE, Karl IE, Wagner TH, Cobb JP, Coopersmith CM, Piwnica-Worms D (2006) TAT-BH4 and TAT-Bcl-xL peptides protect against sepsis-induced lymphocyte apoptosis in vivo. J Immunol 176(9):5471–5477
Staszewski S, Morales-Ramirez J, Tashima KT, Rachlis A, Skiest D, Stanford J, Stryker R, Johnson P, Labriola DF, Farina D, Manion DJ, Ruiz NM, Study 006 Team (1999) Efavirenz plus zidovudine and lamivudine, efavirenz plus indinavir, and indinavir plus zidovudine and lamivudine in the treatment of HIV-1 infection in adults. N Engl J Med 341(25):1865–1873
Phenix BN, Cooper C, Owen C, Badley AD (2002) Modulation of apoptosis by HIV protease inhibitors. Apoptosis 7(4):295–312
Deeks SG, Grant RM (1999) Sustained CD4 responses after virological failure of protease inhibitor-containing therapy. Antivir Ther 4(Suppl 3):7–11
Badley AD (2005) In vitro and in vivo effects of HIV protease inhibitors on apoptosis. Cell Death Differ 12(Suppl 1):924–931
Estaquier J, Lelievre JD, Petit F, Brunner T, Moutouh-De Parseval L, Richman DD, Ameisen JC, Corbeil J (2002) Effects of antiretroviral drugs on human immunodeficiency virus type 1-induced CD4(+) T-cell death. J Virol 76(12):5966–5973
Sloand EM, Kumar PN, Kim S, Chaudhuri A, Weichold FF, Young NS (1999) Human immunodeficiency virus type 1 protease inhibitor modulates activation of peripheral blood CD4(+) T cells and decreases their susceptibility to apoptosis in vitro and in vivo. Blood 94(3):1021–1027
Ghibelli L, Mengoni F, Lichtner M, Coppola S, De Nicola M, Bergamaschi A, Mastroianni C, Vullo V (2003) Anti-apoptotic effect of HIV protease inhibitors via direct inhibition of calpain. Biochem Pharmacol 66(8):1505–1512
Phenix BN, Lum JJ, Nie Z, Sanchez-Dardon J, Badley AD (2001) Antiapoptotic mechanism of HIV protease inhibitors: preventing mitochondrial transmembrane potential loss. Blood 98(4):1078–1085
Matarrese P, Gambardella L, Cassone A, Vella S, Cauda R, Malorni W (2003) Mitochondrial membrane hyperpolarization hijacks activated T lymphocytes toward the apoptotic-prone phenotype: homeostatic mechanisms of HIV protease inhibitors. J Immunol 170(12):6006–6015
Weaver JG, Tarze A, Moffat TC, Lebras M, Deniaud A, Brenner C, Bren GD, Morin MY, Phenix BN, Dong L, Jiang SX, Sim VL, Zurakowski B, Lallier J, Hardin H, Wettstein P, van Heeswijk RP, Douen A, Kroemer RT, Hou ST, Bennett SA, Lynch DH, Kroemer G, Badley AD (2005) Inhibition of adenine nucleotide translocator pore function and protection against apoptosis in vivo by an HIV protease inhibitor. J Clin Invest 115(7):1828–1838
Green DR, Kroemer G (2005) Pharmacological manipulation of cell death: clinical applications in sight? J Clin Invest 115(10):2610–2617
Gaedicke S, Firat-Geier E, Constantiniu O, Lucchiari-Hartz M, Freudenberg M, Galanos C, Niedermann G (2002) Antitumor effect of the human immunodeficiency virus protease inhibitor ritonavir: induction of tumor-cell apoptosis associated with perturbation of proteasomal proteolysis. Cancer Res 62(23):6901–6908
Ellis HM, Horvitz HR (1986) Genetic control of programmed cell death in the nematode C. elegans. Cell 44(6):817–829
Yuan J, Shaham S, Ledoux S, Ellis HM, Horvitz HR (1993) The C. elegans cell death gene ced-3 encodes a protein similar to mammalian interleukin-1 beta-converting enzyme. Cell 75(4):641–652
Dubyak GR, el-Moatassim C (1993) Signal transduction via P2-purinergic receptors for extracellular ATP and other nucleotides. Am J Physiol 265(3 Pt 1):C577–C606
Abbracchio MP, Burnstock G (1994) Purinoceptors: are there families of P2X and P2Y purinoceptors? Pharmacol Ther 64(3):445–475
Ferrari D, Los M, Bauer MK, Vandenabeele P, Wesselborg S, Schulze-Osthoff K (1999) P2Z purinoreceptor ligation induces activation of caspases with distinct roles in apoptotic and necrotic alterations of cell death. FEBS Lett 447(1):71–75
Erickson PA, Fisher SK, Anderson DH, Stern WH, Borgula GA (1983) Retinal detachment in the cat: the outer nuclear and outer plexiform layers. Invest Ophthalmol Vis Sci 24(7):927–942
Zacks DN, Boehlke C, Richards AL, Zheng QD (2007) Role of the Fas-signaling pathway in photoreceptor neuroprotection. Arch Ophthalmol 125(10):1389–1395
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Japan
About this chapter
Cite this chapter
Hisatomi, T. (2014). Neuroprotection for Retinal Detachment. In: Nakazawa, T., Kitaoka, Y., Harada, T. (eds) Neuroprotection and Neuroregeneration for Retinal Diseases. Springer, Tokyo. https://doi.org/10.1007/978-4-431-54965-9_19
Download citation
DOI: https://doi.org/10.1007/978-4-431-54965-9_19
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-54964-2
Online ISBN: 978-4-431-54965-9
eBook Packages: MedicineMedicine (R0)