Abstract
In recent years image-guided tumor ablation, which controls the tumor without performing surgery, has been tried as a treatment for localized, early-stage breast cancer. Radiofrequency ablation (RFA), high-intensity focused ultrasound (HIFU), and cryoablation are available as methods of image-guided tumor ablation that have been applied to the treatment of breast cancer, and clinical reports have been made in regard to each of them.
In this article we have explained the importance of breast imaging before and after nonsurgical ablation therapy. First, we provided a simple explanation of the difference in the meaning of the term “nonsurgical ablation” in Japan and abroad. Next, we described the advantages and limitations of ultrasonography during the performance of nonsurgical ablation therapy, and we explained the usefulness of MRI. Finally, we have explained the proper terminology that should be used in regard to imaging after performing nonsurgical ablation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
19.1 Terminology
“Nonsurgical ablation therapy” is a frequently used term in Japan. Performing cancer therapy without performing surgery (nonsurgical) is emphasized by this term, and it means that the technique is ablation. However, the term “image-guided tumor ablation” instead of “nonsurgical ablation” is usually used abroad [1]. The term “image-guided tumor ablation” does not include any mention of whether the breast cancer therapy is surgical or nonsurgical, and since the term simply means performing ablation during imaging, “image-guided tumor ablation” precisely expresses the fact that the technique is ablation. In Japan, an attempt to determine whether “image-guided tumor ablation” is a method of treatment that can replace current breast cancer surgery is being conducted by breast surgeons at several institutions. Consequently, the term “nonsurgical ablation” is being preferentially used in Japan for treatment in which surgery is not performed.
In this article we will explain breast tumor ablation using the term “image-guided tumor ablation” that is being used abroad.
19.2 Definition of “Image-Guided Tumor Ablation”
The term “tumor ablation” is defined as the direct application of chemical or thermal therapies to a specific focal tumor (or tumors) in an attempt to achieve eradication or substantial tumor destruction [1]. The term “direct” aims to distinguish chemical and thermal therapies used for tumor ablation from therapies that are administered orally or via an intra-arterial or peripheral venous route. Image guidance is critical to the success of direct tumor ablation therapies. Since most of direct tumor ablation therapies can be performed by using any of several imaging modalities, i.e., ultrasonography (US), computed tomography (CT), magnetic resonance imaging (MRI), fluoroscopy, and positron emission tomography (PET), unless a particular imaging modality is mandated as part of the technique, the more general term image guidance is preferred instead of using the name of a particular imaging modality. Theoretically, however, virtually all available ablation techniques can be used with more than one modality.
19.3 Five Steps Involved in Image-Guided Tumor Ablation
Five steps are involved in image-guided tumor ablation: planning, targeting, monitoring, controlling, and assessing treatment response [1]. Planning is the step that is performed before the ablation procedure, and assessing the response to ablation is performed after the procedure has been completed. Targeting, monitoring, and controlling are all performed during the procedure.
Planning
Imaging techniques, including US, CT, MRI, and, more recently, PET, are being used to help determine whether patients are suitable candidates for an ablation procedure. Imaging tasks that are particularly important consist of determining tumor size and shape, number, and location within the organ relative to blood vessels, as well as critical anatomical structures that might be at risk for injury during an ablation procedure.
Targeting
The term “targeting” is used to describe the step during an ablation procedure that involves placement of an applicator, e.g., a radiofrequency (RF) electrode or cryoprobe, into the tumors. While much of the current image-guided tumor ablation literature describes the use of modalities such as US and CT to target tumors for the purpose of ablating them, targeting is only one aspect of intraprocedural image guidance. The qualities of an ideal targeting technique are clear delineation of the tumor(s) and the surrounding anatomy, coupled with real-time imaging and multiplanar and interactive capabilities.
Monitoring
The term “monitoring” is used to describe the process by which the effects of therapy are viewed during a procedure. Changes in images that occur during a procedure are used to assess the effects of treatment. Important functions of monitoring include determining how well the tumor and/or target is being covered by the ablation zone and whether any adjacent normal structures are being affected. MRI is currently the only modality with well-validated techniques for real-time temperature monitoring [2–5]. The term “monitoring” is not used for the step in which the response to treatment is assessed; that step is called “assessing response to treatment.”
Controlling
This term is used to describe the intraprocedural tools and techniques that are used to control the treatment. To control an image-guided ablation procedure, the treatment should be monitorable, such so that the operator can utilize the image-based information obtained during monitoring to control it.
Assessing Treatment Response
Imaging used to assess an image-guided tumor ablation procedure is performed after the ablation procedure is completed, and this step is explained below in the “Terminology Used in Relation to Postprocedural Imaging” section.
19.4 Limitation of US for Image-Guided Tumor Ablation
In recent years, the effectiveness of image-guided tumor ablation of breast cancer has been reported [6–22]. Procedures such as radiofrequency ablation (RFA) [6–8] and high-intensity focused ultrasound (HIFU) [9–11] destroy tumor cells by heating. In contrast, cryoablation destroys cancer cells by cooling them with a cryoprobe [12–22]. Both thermal therapies are theoretically acceptable but still undergoing clinical investigation.
Regarding imaging modalities for image-guided tumor ablation of breast cancer, MRI is helpful for therapy planning, temperature monitoring, the delineation of the ablation zone, the detection of residual disease (assessing treatment response), and follow-up after treatment [8, 18, 22]. On the other hand, the widely adopted US-guided tumor ablation is most effective for only the targeting step.
One disadvantage of US-guided tumor ablation is the difficulty in visualizing the ablation zone. For instance, visualizing the area behind the ice ball is difficult in performing US-guided cryoablation because of acoustic shadowing. Only the surface of the ice ball facing the transducer can be delineated using US, possibly limiting evaluations of whether the tumor has been completely encased [17]. For these reasons, MRI-guided ablation may be more excellent than US-guided ablation. Particularly the inability to use it to evaluate the ablation zone (assessing treatment response) immediately after tumor ablation must be said to be the greatest shortcoming of US-guided tumor ablation in regard to cancer therapy. However, because of the technical convenience of US-guided needle insertion and limitations in the availability of MR-compatible devices, US-guided RFA or US-guided cryoablation is more commonly performed.
19.5 Importance of MRI for Image-Guided Tumor Ablation
Manenti et al. [8] reported that postablation MR images after RFA were strongly correlated with the results of histological analyses. Postablation MR images are helpful for measuring the ablation zone and evaluating the presence of any residual tumor. In addition, the ablation of appropriate margins beyond the borders of the tumor is necessary to achieve complete tumor destruction. Postablation MR images are also helpful for measuring the ablative margin.
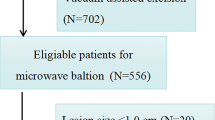
19.5.1 MRI-Guided Tumor Ablation (Cryoablation): Articles in the World
As for MRI-guided cryoablation, only two papers have been published [19, 20]. Morin et al. [19] studied the use of MRI-guided cryoablation for 25 invasive cancers (range, 12–60 mm; mean, 30 mm). They used a 0.5-T open-configuration MR system, and MR images were acquired with a standard transmit-receive linear surface square coil placed directly over the treated breast. The authors found that MRI was very adequate for discriminating between the tumor and the ice ball, and no viable tumor cells were found in any of the pathologic region covered by the ice ball. However, the MRI protocol used in their study, which lacked a dedicated breast coil, utilized a supine patient position, and a relatively thick imaging slice (5 mm) was insufficient for demonstrating the utility of MRI, compared with the current standard MRI protocol for the breast. High-resolution MR images using a dedicated breast coil may be even more helpful for therapy planning and verification of the nonsurgical ablation of breast cancer.
In another study on MRI-guided cryoablation, Pusztaszeri et al. [20] treated 11 patients with invasive breast cancers less than 25 mm in size. The treatment was unsuccessful in one case because of technical problems, and the tumor was found adjacent to the ablation zone during a histopathological examination in this case. However, the MRI sequences, MR coils, and technical details of cryoprobe insertion were not mentioned in their paper. In addition, skin ulceration and/or necrosis was observed in five patients. To avoid frostbite of the skin, the injection of saline under the skin near the ice ball has been reported to be useful [18].
19.5.2 MRI-Guided Cryoablation: Initial Experience in Kameda Hospital (Figs. 19.1, 19.2, and 19.3)
MRI-guided cryoablation (case 1). (a) The breast was moderately compressed using the compression plates. (b) Using the same technique of MRI-guided breast biopsy, the MR-compatible puncture needle was advanced to the appropriate depth. (c) The plastic tube of the puncture needle was left in the breast. (d) Transverse contrast-enhanced T1-weighted MR image shows an enhanced tumor (arrow) and the inserted plastic tube. (e) Transverse contrast-enhanced, fat-suppressed T1-weighted MR image shows that tumor is completely encased within the ablation zone (arrows)
MRI-guided cryoablation (case 2). (a) Transverse contrast-enhanced fat-suppressed T1-weighted MR image demonstrates a 12 mm-sized enhanced mass without surrounding intraductal extension. (b) Transverse contrast-enhanced fat-suppressed T1-weighted MR image shows that the non-enhanced tumor is completely encased within the ablation zone. Inset shows the border of the ablation zone (solid line), and the minimum ablative margin (dotted line) is 6.5 mm. (c) Coronal T1-weighted MR image obtained 9 weeks after cryoablation demonstrates the well-delineated ablation zone. (d) Sagittal fat-suppressed T2-weighted MR image obtained 9 weeks after cryoablation demonstrates the hypointense tumor encased within the ablation zone. (e) Sagittal contrast-enhanced fat-suppressed T1-weighted MR image obtained 9 weeks after cryoablation demonstrates a 12 mm-sized non-enhanced mass in the ablation zone with peripheral enhancement (benign periablational enhancement)
The cryoablation system and US were set up outside the MR room (Fig. 19.1). A 1.5-Tesla MR unit (Avanto; Siemens Medical Solutions, Erlangen, Germany) and dedicated breast coil (7-channel or 4-channel breast biopsy coil; Siemens Medical Solutions, Erlangen, Germany) were used. US (SSD-4000; Aloka, Tokyo, Japan) with a 10-MHz linear probe was performed before and during the cryoablation.
The actual procedure consisted of the following steps:
Therapy Planning
-
1.
The patient was placed in a prone position over the coil, and the breast was moderately compressed using the compression plates (Fig. 19.2a).
-
2.
Before the injection of the contrast material, sagittal and transverse three-dimensional volumetric interpolated breath-hold examination (3D-VIBE) sequences without fat suppression were performed (TR/TE, 4.3/1.4; flip angle, 15°; field of view, 16 cm; matrix size, 192 × 192; slice thickness, 1 mm; time of acquisition, 61 s).
-
3.
After the intravenous injection of 10 mL of Gd-DTPA from a 20-mL syringe (Magnevist®, Bayer Yakuhin Ltd., Japan), sagittal and transverse 3D-VIBE sequences with fat suppression were performed (TR/TE, 4.3/1.4; flip angle, 15°; field of view, 16 cm; matrix size, 192 × 192; slice thickness, 1 mm; time of acquisition, 66 s).
-
4.
The distances between the tumor margin and the surrounding tissue (skin and thoracic muscle) were calculated using three perpendicular planes (sagittal, transverse, and coronal multiplanar reconstruction images).
Targeting
-
5.
The patient was removed from the magnet.
-
6.
After cleansing the skin, a local anesthesia was applied and a skin nick was made with a scalpel. Using the same technique of MRI-guided breast biopsy [23], the MR-compatible puncture needle was advanced to the appropriate depth (Fig. 19.2b), and the plastic tube of the puncture needle was left in the breast (Fig. 19.2c).
-
7.
After verifying the appropriate location of the plastic tube (Fig. 19.2d), the cryoprobe was advanced into the tumor under US guidance.
-
8.
Central placement within the tumor was confirmed using two orthogonal planes.
Cryoablation
-
9.
Immediately after creation of the ice ball, breast compression was removed.
-
10.
We performed cryoablation using a double-freeze-thaw protocol. A passive thaw lasting 10 min was interposed between the two high freeze cycles, and an active thaw with helium gas was performed after the second freeze.
-
11.
During cyroablation, saline was injected under the skin near the ice ball as required to avoid causing frostbite on the skin.
-
12.
The cryoprobe was removed during the active thaw with helium gas.
Verification of Treatment
-
13.
After the completion of cryoablation, the patient was moved into the magnet again.
-
14.
Sagittal and transverse fat-suppressed T2-weighted images (TR/TE, 8750/94; field of view, 16 cm; matrix, 179 × 256; slice thickness, 3 mm; and time of acquisition, 79 s) were obtained. After verifying the creation of the ice ball (Fig. 19.2e), 3D VIBE sequence with fat suppression was performed before and after intravenous injection of the remaining 10 mL of Gd-DTPA in the 20-mL syringe.
One advantage of performing MRI immediately before cryoablation is therapy planning. MRI can be used to predict sites in danger of coming into contact with the increasing ice ball using three perpendicular images. In our protocol, the breast was temporarily compressed using compression plates to facilitate the insertion of the cryoprobe into the tumor. However, the breast compression was removed immediately after creation of the ice ball. Another advantage of MRI was the ability to verify the site of cryoablation. MR images obtained immediately after cryoablation are thought to be useful to both the operators and the patients.
Regarding cryoprobe insertion into the tumor (targeting), Morin et al. [19] reported that the breast was transfixed with an 18-gauge puncture needle through the long axis of the tumor under US guidance. Considering the indications of cryoablation, i.e., a small size (<15 mm) and localized tumor without surrounding DCIS, cryoprobe insertion under US guidance may be easier and safer than insertion under MRI guidance for US-visible breast cancers.
We used the MRI-guided breast biopsy technique to insert an MR-compatible puncture needle as far as the tumor margin. We then inserted the cryoprobe into the trocar, and inserted the cryoprobe inside the tumor, guided by US. The combination of needle insertion into the tumor under US guidance with therapy planning and verification of cryoablation using MRI may be a feasible and promising treatment protocol. If the MR-compatible cryoablation system is approved under the Pharmaceutical Affairs Act in Japan in the future, MRI-guided cryoablation may become more widely adopted. Moreover, this is an age when multiple cryoprobes are being used, and time and energy are being wasted by using a single cryoprobe as in this technique. Performing MRI-guided cryoablation with more than one cryoprobe in the future is definitely not a dream. When it becomes a reality, even broader indications are anticipated, and we hope that the number of breast cancer patients who receive the benefits of nonsurgical cryoablation will increase.
19.6 Terminology Used in Relation to Postprocedural Imaging
Ablation Zone
The term “ablation zone” is used to describe the radiologic region or zone where the effect of the ablation is visible, i.e., the area of gross tumor destruction visualized by imaging.
Ablative Margin
The term “ablative margin” is used for the margin beyond the border of the tumor that needs to be destroyed in order to achieve complete tumor destruction (Fig. 19.3b). For highly vascular organs, such as the kidney and liver, creation of an ablative margin results in low attenuation and absent perfusion zones that extend into the parenchyma.
Benign Periablational Enhancement
“Benign periablational enhancement” is a transient finding that is seen during both pathology examinations and contrast-enhanced imaging examinations, and its presence suggests a benign physiologic response to thermal injury in the form of reactive hyperemia initially and fibrosis and a giant cell reaction later [24]. Depending on the protocol used for contrast-enhanced imaging, i.e., the injection rate and scanning delay, benign periablational enhancement is seen immediately after the ablation procedure and may persist for as long as 6 months. It usually appears in the form of a penumbra, or a thin rim peripheral to the zone of ablation (Fig. 19.3e), that typically measures up to 5 mm acutely but most often measures 1–2 mm. It is a relatively concentric, symmetric, and uniform zone with smooth inner margins, and it needs to be differentiated from “irregular peripheral enhancement.”
Irregular Peripheral Enhancement
The term “irregular peripheral enhancement” is used to describe the imaging findings that are seen when residual tumor is present at the margin of the ablation zone. Residual unablated tumor often grows in a scattered, nodular, or eccentric pattern. Irregular peripheral enhancement indicates incomplete local treatment, i.e., the presence of residual unablated tumor. If left untreated, the residual tumor tends to continue to grow. Because of the delayed enhancement characteristics of many hypovascular tumors, this finding is often best appreciated by comparing delayed images with the baseline images.
19.7 Conclusion
In this article we have explained the importance of breast imaging before and after nonsurgical ablation therapy. First, we provided a simple explanation of the difference in the meaning of the term “nonsurgical ablation” in Japan and abroad. Next, we described the advantages and limitations of ultrasonography during the performance of nonsurgical ablation therapy, and we explained the usefulness of MRI. We have also stated our personal opinions regarding the current status and future prospects for MRI-guided tumor ablation, and we have interspersed our experience with cryoablation at our own institution into our explanation. Finally, we have explained the proper terminology that should be used in regard to imaging after performing nonsurgical ablation. Needless to say, “imaging” both before and after image-guided tumor ablation plays a very important role. We hope that this article will be useful in the proper popularization of image-guided tumor ablation.
References
Goldberg SN, Grassi CJ, Cardella JF, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. Radiology. 2005;235:728–39.
Silverman SG, Tuncali K, Adams DF, et al. MR imaging-guided percutaneous cryotherapy of liver tumors: initial experience. Radiology. 2000;217:657–64.
Quesson B, de Zwart JA, Moonen CT. Magnetic resonance temperature imaging for guidance of thermotherapy. J Magn Reson Imaging. 2000;12:525–33.
Lewin JS, Connell CF, Duerk JL, et al. Interactive MRI-guided radiofrequency interstitial thermal ablation of abdominal tumors: clinical trial for evaluation of safety and feasibility. J Magn Reson Imaging. 1998;8:40–7.
Vogl TJ, Muller PK, Hammerrstingl R, et al. Malignant liver tumors treated with MR imaging-guided laser-induced thermotherapy: technique and prospective results. Radiology. 1995;196:257–65.
Fornage BD, Sneige N, Ross MI, et al. Small (< or = 2-cm) breast cancer treated with US-guided radiofrequency ablation: feasibility study. Radiology. 2004;231:215–24.
Oura S, Tamaki T, Hirai I, et al. Radiofrequency ablation therapy in patients with breast cancers two centimeters or less in size. Breast Cancer. 2007;14:48–54.
Manenti G, Bolacchi F, Perretta T, et al. Small breast cancers: in vivo percutaneous US-guided radiofrequency ablation with dedicated cool-tip radiofrequency system. Radiology. 2009;251:339–46.
Wu F, Wang ZB, Cao YD, et al. A randomised clinical trial of high-intensity focused ultrasound ablation for the treatment of patients with localised breast cancer. Br J Cancer. 2003;89:2227–33.
Gianfelice D, Khiat A, Amara M, Belblidia A, Boulanger Y. MR imaging-guided focused US ablation of breast cancer: histopathologic assessment of effectiveness- initial experience. Radiology. 2003;227:849–55.
Furusawa H, Namba K, Thomsen S, et al. Magnetic resonance-guided focused ultrasound surgery of breast cancer: reliability and effectiveness. J Am Coll Surg. 2006;203:54–63.
Rand RW, Rand RP, Eggerding FA, et al. Cryolumpectomy for breast cancer: an experimental study. Cryobiology. 1985;22:307–18.
Staren ED, Sabel MS, Gianakakis LM, et al. Cryosurgery of breast cancer. Arch Surg. 1997;132:28–33.
Pfleiderer SO, Freesmeyer MG, Marx C, Kühne-Heid R, Schneider A, Kaiser WA. Cryotherapy of breast cancer under ultrasound guidance: initial results and limitations. Eur Radiol. 2002;12:3009–14.
Pfleiderer SO, Marx C, Camara O, Gajda M, Kaiser WA. Ultrasound-guided, percutaneous cryotherapy of small (< or = 15 mm) breast cancers. Invest Radiol. 2005;40:472–7.
Sabel MS, Kaufman CS, Whitworth P, et al. Cryoablation of early-stage breast cancer: work-in-progress report of a multi-institutional trial. Ann Surg Oncol. 2004;11:542–9.
Roubidoux MA, Sabel MS, Bailey JE, Kleer CG, Klein KA, Helvie MA. Small (<2.0-cm) breast cancers: mammographic and US findings at US-guided cryoablation-initial experience. Radiology. 2004;233:857–67.
Ozaki S, Fukuma E, Tozaki M, et al. The use of non-surgical cryoablation for minimal breast cancer. J Jpn Surg Assoc. 2008;69:3038–47. (Japanese with English abstract).
Morin J, Traoré A, Dionne G, et al. Magnetic resonance-guided percutaneous cryosurgery of breast carcinoma: technique and early clinical results. Can J Surg. 2004;47:347–51.
Pusztaszeri M, Vlastos G, Kinkel K, Pelte MF. Histopathological study of breast cancer and normal breast tissue after magnetic resonance-guided cryotherapy ablation. Cryobiology. 2007;55:44–51.
Littrup PJ, Jallad B, Chandiwala-Mody P, D’Agostini M, Adam BA, Bouwman D. Cryotherapy for breast cancer: a feasibility study without excision. J Vasc Interv Radiol. 2009;20:1329–41.
Tozaki M, Fukuma E, Suzuki T, Hoshi K. Ultrasound-guided cryoablation of invasive ductal carcinoma inside the MR room. Magn Reson Med Sci. 2010;9:31–6.
Tozaki M, Yamashiro N, Sakamoto M, Sakamoto N, Mizuuchi N, Fukuma E. MR-guided vacuum-assisted breast biopsy: results in 100 Japanese women. Jpn J Radiol. 2010;28:527–33.
Goldberg SN, Gazelle GS, Compton CC, Mueller PR, Tanabe KK. Treatment of intrahepatic malignancy with radiofrequency ablation: radiologic-pathologic correlation. Cancer. 2000;88:2452–63.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Japan
About this chapter
Cite this chapter
Tozaki, M. (2016). Importance of Breast Imaging Before and After Nonsurgical Ablation Therapy. In: Kinoshita, T. (eds) Non-surgical Ablation Therapy for Early-stage Breast Cancer. Springer, Tokyo. https://doi.org/10.1007/978-4-431-54463-0_19
Download citation
DOI: https://doi.org/10.1007/978-4-431-54463-0_19
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-54462-3
Online ISBN: 978-4-431-54463-0
eBook Packages: MedicineMedicine (R0)