Abstract
Transforming growth factor beta (TGF-β) is known to regulate numerous cell functions in the nervous system development, adult maintenance, and degeneration. TGF-β carries roles in neurons and glia and is involved in the regulation of proliferation, differentiation, neuron survival and death, as well as orchestrating its response to lesion. In the context of brain disorders the current understanding of TGF-β action is discussed for brain tumors, neurodegenerative disease, such as Alzheimers’ and Parkinson’s disease, in insults such as ischemia, stroke, and vascular damage, as well as changes in neuronal activity, such as hyperactivity as seen in epilepsy, or in neuronal depression.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cell cycle regulation
- ECM
- Neuroprotection
- Cell death
- Blood
- Neurons
- Astrocytes
- Microglia
- Myelination
- Neurogenesis
1 Introduction
The isolation and characterization of transforming growth factors-β (TGF-β) by Anita Roberts has introduced a versatile extrinsic signaling molecule affecting numerous events in the life of almost each cell (Roberts and Sporn 1990; Derynck et al. 1985). Best characterized events include the regulation of cell cycle, composition of the extracellular matrix (ECM), and thereby cell migration or differentiation, as well as regulation of cell survival and death. Imbalance of TGF-β availability is therefore likely to affect tissue development, maintenance, and homeostasis. This certainly also accounts for the nervous system. Once accepted that TGF-β is also expressed in the nervous system, the functional contribution of TGF-β is now more and more understood in numerous events in the development of the nervous system, its maintenance, and consequently also in the context of many brain diseases. This review will discuss the current knowledge of TGF-β in brain development and function and consequently in brain disorders.
Brain disorders include brain tumors, neurodegenerative disease, such as Alzheimers’ disease and Parkinson’s disease, insults such as ischemia and stroke, and vascular damage, as well as changes in neuronal activity, such as hyperactivity as seen in epilepsy, or neuronal depression.
2 TGF-β Expression in the Central Nervous System
Localisation of TGF-β isoforms in mice and rats has been performed by immunohistochemistry and in situ hybridization studies demonstrating a widespread distribution of TGF-β2 and TGF-β3 during development (Flanders et al. 1991; Pelton et al. 1991a, b; Unsicker et al. 1991). TGF-β1 is confined to meninges and choroid plexuses. During mouse development TGF-β2 and -β3 immunoreactivities become first detectable along peripheral nerves, in radial glial cells and along the central nervous system (CNS) axon tracts at embryonic age (E)12. Neuronal cell bodies become immunoreactive from E15 onwards. Most notably, TGF-β immunoreactivity is not detectable in the ventricular zone throughout the neural tube, suggesting that TGF-β may not be involved in the regulation of cell division of neural stem cells during development (Flanders et al. 1991). In contrast, on day E16, cells in the subventricular zone, subplate, and lamina I of the cortex stain positive for TGF-β. As they develop, astrocytes are also immunoreactive for TGF-β2 and -β3. In the adult nervous system both neurons and astroglia are immunoreactive for TGF-β2, -β3. Immunoreactive neuron populations include cortical layers 2, 3, and 5, hippocampus, piriform cortex, retinal ganglionic cells, hindbrain aminergic neurons, as well as spinal and hindbrain motoneurons (Unsicker et al. 1991). TGF-β1 is most prominent within the choroid plexus and meninges, it may, however, be expressed in other cells below levels of detectability. Upon lesioning, TGF-β1 may by upregulated in astrocytes as well as in neurons in vivo. TGF-β1 becomes also detectable in tissue culture, possibly mimicking a lesion-like situation. In primary neural tissue culture, treatment with all three TGF-β isoforms usually results in identical responses, suggesting that the recombinant proteins used have similar affinities for their shared receptor complex (Krieglstein and Unsicker 1994; Massague 2000).
In addition to the distribution of TGF-β within the peripheral nervous system (PNS) and CNS, its subcellular localization and mode of secretion is of importance in order to elaborate on its possible functions. Taking PC12 cells as a model to study sorting in the trans-Golgi network, Specht et al. (2003) could show that TGF-β2 may be sorted and released to a large proportion via the regulated path of secretion. Secretory vesicles provide a milieu of pH 5, which is suitable for TGF-β activation within the vesicle, enabling release of active TGF-β (Specht et al. 2003). Activity-depended release of TGF-β2 may suggest a function as a modulator for synaptic plasticity (Lacmann et al. 2007).
3 TGF-β in Brain Tumors
The role of TGF-β in cancer biology is complex and involves both aspects of tumor suppression (Bartholin et al. 2013; Seoane 2006) as well as tumor promotion (Wendt and Schiemann 2013; Joseph et al. 2013; Roberts and Wakefield 2003).
TGF-βs are well known for their capacity to regulate cell proliferation in a context-dependent manner. There are at least four scenarios in which regulation of cell proliferation is an important issue in nervous system development and maintenance: (a) neurogenesis, (b) proliferation of neuroblasts (neural crest cells), (c) proliferation of glial cells during development or upon lesioning, and (d) upon transformation in tumors.
Neurogenesis in the neural tube requires definite exit of the cell cycle to generate postmitotic neurons. In the past years there is increasing evidence for the role of TGF-β in developmental and adult neurogenesis (Vogel et al. 2010; Aigner and Bogdahn 2008). For some years there was indirect evidence available that neural stem cells in the neuroepithelium need to be protected from the action of TGF-β, in order to prevent premature growth retardation (Seoane et al. 2004; Hanashima et al. 2002). Seoane and coworkers have demonstrated on the basis of protein interaction analysis in human HaCaT keratinocytes that expression of the cyclin-dependent kinase (cdk) inhibitory protein 1 (p21Cip1) is regulated by TGF-β-dependent Smad complexes in combination with the Forkhead box (Fox) family member FoxO. This FoxO-Smad complex is inhibited by FoxG1, which has been shown to be essential for proliferation of telencephalic progenitor cells (Xuan et al. 1995). Indeed, FoxG1 mutants, which display reduced proliferation of telencephalic progenitor cell, premature differentiation and early depletion of the progenitor population (Xuan et al. 1995) show high levels of p21Cip1 expression in TGF-β-sensitive progenitor cells (Seoane et al. 2004). Exit from the cell cycle during terminal differentiation, as required for neurogenesis, has been described to be regulated by Ink4d and Kip1 inhibitors of cyclin-dependent kinases (Zindy et al. 1999; Cunningham and Roussel 2001). P27Kip1 has been identified as a TGF-β-dependent target gene; however, there is no evidence for a TGF-β-dependent regulation of p19Ink4d. This suggests that TGF-β may serve as an extracellular regulator to induce cell cycle arrest at the G1 phase in neural stem cells but may probably not be sufficient to regulate cell cycle exit required for terminal differentiation. In mouse hippocampal progenitor cells, TGF-β causes induction of p21Cip1 and downregulation of Cdk activators Ccnd1 and Ccnd2, leading to cell cycle exit and neuronal differentiation (Vogel et al. 2010). Along this line, TGF-β2/-β3 double knockout mice display increased cell proliferation and reduced numbers of neurons in the developing cerebral cortex and hippocampus, as the progenitor cells failed to differentiate into neurons because they did not exit cell cycle. Furthermore, TGF-β1 has been implicated as a negative modulator of adult neurogenesis (Wachs et al. 2006).
By affecting the cell cycle prior to terminal differentiation, TGF-β may, of course, regulate proliferation of neuroepithelial cells, including neuroblasts, neural crest cells, and glial progenitors (Zhang et al. 1997a; Anchan and Reh 1995). Furthermore, TGF-β2 has been shown to regulate cell proliferation in neural crest-derived chromaffin cells (Rahhal et al. 2004) with the capacity of lifelong proliferation.
Tumors of the CNS include primitive neuroectodermal tumors, such as gliomas and medulloblastomas (Fogarty et al. 2005; Nieder et al. 2003). They derive from dividing glial cells, or neural stem and progenitor cells. Glial brain tumors are further classified using grades I–IV to express the likelihood of increased growth and malignancy. CNS tumors are characterized by rapid and infiltrative growth, angiogenesis, and immune suppression. Due to the proliferative behavior of brain cells, brain tumors show a high occurrence not only during development affecting children but also during adulthood. Particularly adult neural stem cells with the capacity to provide new neurons and glia in regions with high plasticity, following injury, or in the context of specific diseases, may escape their physiological control machinery and transform into brain cancer stem cells (reviewed in Aigner and Bogdahn 2008).
Id4 (inhibitors of DNA binding/differentiation) has been shown to serve important functions in neural stem cell differentiation and its deregulation has been implicated in glial neoplasia (Dell’Orso et al. 2010). Deregulation could occur via functional point mutations or epigenetic silencing. Martini and coworkers (2012) were able to show that epigenetic silencing of Id4 via hypermethylation resulted in reduced expression of matrix GLA protein (MGP), TGF-β1 and vascular endothelial growth factor (VEGF) which was associated with a more favorable clinical outcome. However, there are many possibilities to circumvent this effect. First, as TGF-β actions are context-dependent, the presence of certain mitogens, such as TGF-α/epidermal growth factor (EGF) or platelet-derived growth factor (PDGF) may turn TGF-β into a growth stimulating factor (Roberts et al. 1981; Leof et al. 1986; Seoane 2006). Secondly, transformed cells may become insensitive to TGF-β due to overproduction of TGF-β or due to mutations of TGF-β receptors, their signaling components, or even their target genes responsible for G1 arrest (for example Rich et al. 1999; Lyons et al. 1990; Markowitz et al. 1995; Hahn et al. 1996; Seoane et al. 2004; Rich 2003 for review).
TGF-β´s ability to regulate ECM composition puts TGF-β at high risk in the regulation of tumor invasion and metastasis. In this context TGF-β has been shown to regulate integrin expression, for example integrin αVβ3 which has been shown to play a role in glioma propagation (Uhm et al. 1999). TGF-β has also been shown to upregulate matrix metalloprotease 2 (MMP-2) and MMP-9 expression at the cell surface (Rooprai et al. 2000) that may interact with αVβ3 integrin (for review, see Platten et al. 2001).
TGF-β is a potent immunosuppressive cytokine (Wahl and Chen 2003; Roth et al. 2012; Hau et al. 2011). Brain tumors are well known for their immunosuppressive properties allowing them to escape from the host’s immune surveillance. TGF-β2 and TGF-β3 are considered master molecules that upon secretion mediate this immunosupressive environment. This immunosuppressive role has been attributed to TGF-β2, which is also the preferentially expressed isoform by many glioblastomas, grade IV gliomas (Bodmer et al. 1989; Hau et al. 2011). On this basis, TGF-β2-specific antisense gene therapy strategies have been established to make tumor cells accessible to an effective anti-tumor immune response and counteract TGF-β-dependent tumor metastasis (Hau et al. 2009; Jachimczak et al. 1993; Lou 2004). Along this line, there is extensive research going on to identify TGF-β signaling inhibitors for cancer therapy (DaCosta et al. 2004; Yingling et al. 2004; Lahn et al. 2005).
4 Vascular Damage in the CNS
The blood–brain barrier (BBB) generates the specific milieu of the brain by building a tight boundary and thereby separating the components of the circulating blood from the brain. After injury or in neurologic diseases including trauma, ischemia/stroke, or Alzheimer’s disease (AD), leakage of the BBB results in the entry of blood constituents into the brain (Abbott et al. 2006). Plasma proteins such as albumin, immunoglobulins, amyloid-β, and fibrinogen, and vascular cells such as erythrocytes and leucocytes, leaking into the brain have been associated with inflammation and restriction of repair (for review, see Beck and Schachtrup 2012). Schachtrup and coworkers (2010) identified TGF-β as a vascular-derived protein. Specifically, they could demonstrate that the plasma-derived protein fibrinogen acts as a carrier of latent TGF-β. Its activation is mediated via avβ6 and avβ8 integrins present on the surface of astrocytes.
Increased levels of TGF-β1 has been described in human brains during trauma, multiple sclerosis (MS), Parkinson’s, AD, and stroke patients (Lippa et al. 1995). In patients suffering from severe head injury, high levels of TGF-β1 could be detected in the cerebrospinal fluid (CSF) within 1 day after injury (Csuka et al. 1999; Morganti-Kossmann et al. 1999). These observations strongly suggest that lesion-induced, vascular-derived TGF-β contributes to the corresponding degeneration and regeneration processes (Beck and Schachtrup 2012).
TGF-β has been profoundly investigated for its role in orchestrating the response to brain lesions (for review, see Flanders et al. 1998). With regard to astrocytes, this includes regulation of astrocytic growth, astroglial scar formation, and anti-inflammatory responses. In most contexts studied, TGF-β inhibits the growth of astrocytes (Flanders et al. 1993; Hunter et al. 1993). Most importantly, TGF-β counteracts mitogenic signals by astroglial mitogens such as fibroblast growth factor-2 (FGF-2) or PDGF. However, effects may vary depending on astrocyte culture conditions in vitro or may be brain region-dependent in vivo (Labourdette et al. 1990; Johns et al. 1992). TGF-β may also affect cell adhesion, migration, and ECM production by astrocytes, all being important steps in the cascade of shaping the reactive astrocyte phenotype. TGF-β-treated astrocytes show a slight increase in actin content, the appearance of actin stress fibers, a slight increase in the glial fibrillary acidic protein (GFAP), and an increased production of laminin and fibronectin (cf. Baghdassarian et al. 1993). Thus, treatment of cerebral wounds with anti-TGF-β2 antibodies was shown to lead to a marked reduction of glial scarring (Logan et al. 1999). Many effects of TGF-β on astroglia are anti-inflammatory and immunosuppressive, as TGF-β modulates the expression of important cytokines involved in CNS immune reactions. These include upregulation of interleukin-6 (IL-6) and nerve growth factor (NGF) (Spittau et al. 2012; Aderka et al. 1989; Lindholm et al. 1992), blocking interferon-γ mediated upregulation of major histocompatibility class (MHC) II (Dong et al. 2001), and the tumor necrosis factor α (TNF-α) and interleukin-1 β (IL-1 β)-mediated upregulation of intercellular adhesion molecule-1 (Shrikant et al. 1996).
5 TGF-β in Neuronal Survival and Death
TGF-β has been shown to promote survival of several neuronal populations in vitro (Krieglstein et al. 1995; Poulsen et al. 1994; Martinou et al. 1990). However, it is now well established that TGF-β may modulate the neurotrophic capacities of numerous growth factors including neurotrophins, such as NGF, brain-derived neurotrophic factor (BDNF), as well as ciliary neurotrophic factor (CNTF) (Krieglstein and Unsicker 1996) and, most importantly, glial cell line-derived neurotrophic factor (GDNF; Krieglstein et al. 1998b). GDNF was shown to crucially depend on TGF-β to exert its neurotrophic activities on peripheral as well as mesencephalic dopaminergic neurons in vitro. In vivo, GDNF’s neuroprotective effect on target-deprived pre-ganglionic sympathetic neurons, as well as 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-lesioned nigrostriatal dopaminergic neurons, also depends on the presence of TGF-β (Schober et al. 1999, 2007). GDNF/TGF-β cooperativity on chick ciliary ganglionic neurons has now been characterized in detail, whereby TGF-β is required for appropriate GDNF receptor (GFRα1) recruitment to the plasma membrane (Peterziel et al. 2002). Interestingly, TGF-β does not cooperate with Neurturin, a closely related factor to GDNF, and does not promote the recruitment of GFRα2 to the plasma membrane, suggesting high specificity in TGF-β/GDNF cooperativity (Peterziel et al. 2007).
Depending on the cellular context, TGF-β has also been shown to regulate ontogenetic neuron death. Upon immunoneutralization of all TGF-β isoforms in ovo (E6–E10), ontogenetic cell death of chick parasympathetic ciliary ganglionic neurons, sensory dorsal root ganglionic neurons as well as lumbar spinal motoneurons could be prevented (Krieglstein et al. 2000). Similarly, TGF-β regulates ontogenetic morphogenetic cell death in the developing retina of chick and mouse embryos (Dünker et al. 2001; Dunker and Krieglstein 2003). Another classical model for morphogenetic cell death during embryogenesis represents the removal of interdigital tissue to form individual fingers. Similarly, double deletion of TGF-β2 and -β3 in the mouse resulted in lack of cell death (Dunker et al. 2002). Furthermore, induced neuron death following embryonic limb bud ablation in chick embryos resulted in a significant neuroprotection upon immunoneutralization of TGF-β (Krieglstein et al. 2000). Together, these data suggest that TGF-β is a key regulator of ontogenetic cell death in vivo. Mechanistically, we recently identified that TGF-β-induced apoptosis in oligodendroglial progenitor cells (OLI-neu; Schuster et al. 2002) is characterized by downregulation of Bcl-xl. Furthermore, Fractin is produced as a caspase-specific cleavage product in oligodendroglial cells during TGF-β-mediated apoptosis, whereby Fractin binding to Bcl-xl induced downregulation of Bcl-xl protein levels (Schulz et al. 2009). Sorrentino and collaborators (2008) were able to show that the intracellular apoptotic cascade can be initiated via the type I receptor of TGF-β (TβR-I) and receptor-engaged TNF-α receptor associated factor 6 (TRAF6). Although TGF-β-induced apoptosis and underlying signaling pathways have been well characterized in many cells types, little is known about TGF-β-induced apoptosis in neurons (Schuster and Krieglstein 2002; Sanchez-Capelo 2005).
6 Cerebral Ischemia
Cerebral ischemia is caused by either a blood clot occluding a blood vessel in the brain (focal ischenia) or a more general reduction in brain blood flow (global ischemia) leading to insufficient blood flow and reduced oxygen levels in the respective brain areas, thus leading to death of brain tissue. Neuronal cell death may occur as necrosis or apoptosis. Thrombolysis is the approved treatment of stroke. TGF-β1 expressed at low levels in adult brain is rapidly upregulated following insults such as cerebral ischemia, excitatory injury, or traumatic brain injury (Klempt et al. 1992; Knuckey et al. 1996; Yamashita et al. 1999; Morganti-Kossmann et al. 1999; Zhu et al. 2000; Boche et al. 2003; Krieglstein 2006; Pál et al. 2012). TGF-β1 upregulation was observed primarily in microglial cells and in astrocytes, while TGF-β2 upregulation was seen in neurons. TGF-β3 was not upregulated; however, the levels of both TGF-β2 and TGF-β3 decreased subsequently. These data suggest a distinct spatiotemporal requirement of TGF-β isoforms action during cerebral ischemia (Pál et al. 2012). As TGF-β is a good candidate to organize the response of neurons to degeneration as well as mediating anti-inflammatory reactions, its neuroprotective potential has been widely analyzed (for review, see Flanders et al. 1998; Böttner et al. 2000; Dobolyi et al. 2012). Specifically, TGF-β1 applied either as recombinant protein or by adenoviral-based overexpression has been shown to reduce infarct size after focal cerebral ischemia and to prevent hippocampal neuronal damage after global ischemia (Gross et al. 1993; Prehn et al. 1993; Zhu et al. 2002; for review, see Buisson et al. 2003; Dhandapani and Brann 2003). Furthermore, TGF-β may also mediate tolerance of ischemic preconditioning towards subsequent ischemic insult (Boche et al. 2003). The molecular mechanism(s) by which TGF-β protects neurons from ischemic cell death relies on a signaling crosstalk between neurons and astrocytes (Prehn et al. 1994; Docagne et al. 1999) and involves the maintenance of Ca2+ homeostasis, modulation of the t-plasminogen activator (tPA)/plasminogen activator inhibitor (PAI-1) axis, as well as inhibition of pro-apoptotic pathways, such as Bad and caspase-3 (Zhu et al. 2001, 2002) and upregulation of anti-apoptotic proteins such as Bcl-2 (Prehn et al. 1994). An additional TGF-β-dependent anti-apoptotic pathways involving NF-κB activation has been described (Zhu et al. 2004). This pathway seems to be downstream of ALK1 (activin receptor-like kinase 1), an alternative TGF-β type I receptor first described on endothelial cells, which has been shown to be upregulated in neurons in an injury-dependent manner (Konig et al. 2005). Injury-dependent upregulation of ALK1, with signaling preference towards Smad1, may also explain numerous opposing effects of TGF-β in brain development and lesions.
7 Alzheimer’s Disease
Alzheimer’s disease (AD) is a degenerative brain syndrome characterized by a progressive decline in learning and memory, thinking, language, judgment, and other higher brain functions. Currently about 18 million people worldwide suffer from AD and it is estimated that in 2025, 34 million will be affected. The statistical risk of occurrence is 1.4 % at the age of 60 and doubles every 5 years thereafter (WHO; Huang and Mucke 2012).
AD is characterized by considerable brain shrinkage resulting in a large loss of brain weight and volume. The extent of brain volume loss suggests more general mechanisms such as shrinkage and loss of neuronal processes, including degeneration of specific neuron populations (Huang and Mucke 2012). Along this line, aberrant neuronal network activity, dysfunction, and loss of synapses may describe the cognitive decline in AD.
TGF-β has been implicated in the regulation of neurite outgrowth, transmitter synthesis as well as synapse formation (Krieglstein et al. 2011). TGF-β has been reported to cause neurite sprouting and elongation of hippocampal axons as well as promoting re-elongation of injured axons of hippocampal neurons in vitro (Ishihara et al. 1994; Abe et al. 1996). In the mouse neocortex, TGF-β can direct neuronal polarity by initiation of axon formation and neuronal migration via site-specific phosphorylation of the polarity protein Par6 (Yi et al. 2010). Extracellular signaling factors such as Wnt and TGF-βs are recognized as target-derived signals in synaptogenesis (Salinas 2005; Packard et al. 2003). In chick ciliary ganglionic neurons, developmental expression of KCa channels coincides with synaptogenesis. Dryer and coworkers have shown that target-derived TGF-β1 regulates the developmental expression of Ca2+-activated K+ currents in vitro and in vivo (Cameron et al. 1999). The acute effect of TGF-β1 relies on the translocation of KCa channels from intracellular stores to the plasma membrane involving signaling via the Ras GTPase, extracellular regulated kinases (Erk), and phosphoinositide 4′ (PI4) kinase (for review, see Dryer et al. 2003). In conclusion, TGF-β may well be suited to modulate synaptic plasticity and cognition (for review, see Krieglstein et al. 2011).
The pathogenesis of AD is focusing on amyloid β (Aβ) peptides, the main constituent in plaques, derived from amyloid precursor protein (APP) upon proteolylic cleavage (De Strooper et al. 2010; Bertram et al. 2010). There are several lines of evidence suggesting that TGF-β1 may contribute to the pathology of Alzheimer’s disease, particularly through promoting Aβ precursor expression and Aβ deposition (Burton et al. 2002; Wyss-Coray et al. 1997a, b; Flanders et al. 1995; van der Wal et al. 1993). Mice overexpressing TGF-β1 in astrocytes develop AD-like vascular and meningeal abnormalities with age (Gaertner et al. 2005). These chronic alterations could be correlated with reduced brain tissue perfusion, leading to an increased amount of fibrillar and soluble Aβ peptides. However, in brain parenchyma, astroglial TGF-β1 expression leads to a reduction of overall Aβ as well as decreased numbers of dystrophic neurites (Wyss-Coray et al. 2001). The reduced plaque burden in brain parenchyma is thought to depend on TGF-β-dependent microglial activation and microglial Aβ-clearance. Furthermore, a genetic association study of three polymorphisms of the human TGF-β1 gene with AD suggests that there is no correlation between TGF-β1 and AD on the basis of TGF-β1 gene variability (Araria-Goumidi et al. 2002).
Most recently, bioactive TGF-β has been shown to be associated with lipoproteins, specifically those containing ApoE3, but not ApoE4 (Tesseur et al. 2009). Association of TGF-β1 with lipoproteins may facilitate its diffusion and signaling and possibly also other biological functions of TGF-β1. This observation is of particular interest in this context as ApoE4 has been genetically linked with late-onset AD (Bertram et al. 2010). As TGF-β1 is a neuroprotective agent and may be beneficial in the AD condition, for example through reduction of plaque burden, the preferential binding of TGF-β1 to ApoE3 versus ApoE4 may put ApoE4 carriers on higher risk for developing AD (Tesseur et al. 2009).
Several lines of evidence suggest impairment of TGF-β-activated Smad signaling, with ectopic localization of phosphorylated Smad2/3 within amyloid plaques and neurofibrillary tangles (Lee et al. 2006; Tesseur et al. 2006; Ueberham et al. 2006; Chalmers and Love 2007a, b). Furthermore, AD patients have been shown to have reduced plasma levels of TGF-β1 (Mocali et al. 2004; Juraskova et al. 2010) as well as reduced neuronal expression of the TGF-β type II receptor (TβRII) (Tesseur et al. 2006). Lack of TβRII signaling via neuronal expression of kinase-deficient TβRII in AD transgenic mice promoted Aβ deposition and loss of dendrites (Tesseur et al. 2006), while Aβ may downregulate expression of TβRII via induction of miR-106b (Wang et al. 2010). Finally, injection of synthetic Aβ in combination with blocking TGF-β signaling via application of the TβRI kinase inhibitor SB431542 significantly increased the vulnerability of hippocampal neurons to Aβ, leading to neuronal degeneration (Caraci et al. 2008).
Together, as TGF-β1 signaling is beneficial in the AD environment, rescuing TGF-β1 levels and TGF-β signaling may represent a new strategy for neuroprotection in AD (Caraci et al. 2012).
8 Parkinson’s Disease
Parkinson’s disease (PD) is a neurodegenerative disease characterized by a progressive loss of nigrostriatal neurons and in consequence by marked reduction of striatal dopamine resulting in impaired voluntary movement (for review, see Braak et al. 2004; Dunnett and Björklund 1999). In addition to the loss of neurons, a further morphologic hallmark of PD is the presence of Lewy bodies and Lewy neurites (Forno 1996). The formation of these proteinaceous inclusions involves interaction of several proteins, including α-synuclein (Spillantini et al. 1998). The etiology of PD is likely due to combinations of environmental and genetic factors (for review, see, for example, Valente et al. 2012; Gasser et al. 2011).
TGF-β2 and TGF-β3 are expressed in adult nigral dopaminergic neurons (Unsicker et al. 1991), and TGF-β1 and -β2 were elevated in biopsies of PD patients (Nagatsu et al. 2000). TGF-βs have been shown to promote midbrain dopaminergic neuron survival in vitro and in vivo (Krieglstein and Unsicker 1994; Poulsen et al. 1994; Roussa et al. 2004), as well as protection against 1-methyl-4-phenylpyridinium (MPP+) intoxication (Krieglstein et al. 1995; Roussa et al. 2009). Most importantly, TGF-β cooperates with GDNF to promote dopaminergic neuron survival (Krieglstein et al. 1998b). GDNF is well known as a potential therapeutic agent coping with PD (for review, see Björklund and Lindvall 2000). However, also in vivo GDNF-dependent neuroprotective effects are based on the cooperativity with TGF-β, as shown in the MPTP-mouse model, an animal model of PD (Schober et al. 2007). This neuroprotective strategy has already been used incidentally by grafting extra-adrenal chromaffin cells obtained from Zuckerkandl’s organ in parkinsonian rats (6-hydroxydopamine model). The behavioral improvements of parkinsonia deficts were in addition to the supply of catecholamines attributed to the release of the survival promoting proteins GDNF and TGF-β1 (Fernandez-Espejo et al. 2005).
Most recently, a new animal model for PD has been introduced. Viral transformation of rats with α-synuclein showed a slow progression of nigral dopaminergic neurons (Ulusoy et al. 2010). Most interestingly, GDNF, for long considered as the gold standard in neurotrophic-based neuroprotection of PD, is not able to rescue α-synuclein-mediated degeneration of dopaminergic neurons (Decressac et al. 2011).
9 Epilepsy
Epilepsy is a common neurological disorder affecting 0.5–2 % of the population worldwide. Epilepsy is characterized by seizures resulting from abnormal neuronal activity. So far, there is no cure known for the disease. The mechanisms leading to the disease are only poorly understood. However, epilepsy is often seen following brain trauma, ischemic or infectious brain injury, or drug and alcohol misuse. These conditions may be accompanied by vascular damage and leakage of the blood–brain barrier (see above).
Cacheaux et al. (2009) have identified the involvement of TGF-β signaling in epileptogenesis. The group has previously demonstrated that serum albumin causes epileptic field potentials when exposed to brain slices in vitro (Ivens et al. 2007). Serum albumin was taken up by astrocytes leading to down regulation of inward-rectifying potassium (Kir 4.1) channels, resulting in reduced buffering of extracellular potassium in neuronal hyperexcitability and epileptiform activity. As the albumin uptake was shown to occur in a TGF-β receptor-mediated mechanism, blocking of the TβR in vivo reduced the likelihood of epiletogenesis in albumin exposed brains (Ivens et al. 2007). In follow-up experiments, the group was able to show that TGF-β1-mediated signaling is sufficient to induce epileptoforming activity (Cacheaux et al. 2009). These data strongly link the TGF-β pathway with epileptogenesis and identify the TGF-β pathway as a therapeutic target for the prevention of injury-induced epilepsy (Friedman 2011).
10 Depression
Major depressive disorder is a mental disorder characterized by low mood, low self-esteem, and reduced interest in enjoying pleasure. There is no clinical test for depression. Patients are treated with antidepressant drugs, which improves their mental condition after several weeks of treatment. Most antidepressant medications directly or indirectly increase the levels of one or more of the monoamines, such as serotonin, noradrenaline, and dopamine, in the synaptic cleft between neurons in the brain, suggesting that depression may be the consequence of reduced synaptic activity. In addition to neurotransmitters, also neuropeptides and neurotrophic factors such as BDNF and TGF-β have been shown to be released in an activity-dependent manner (Thoenen 1995; Specht et al. 2003; Lacmann et al. 2007). Notably, KCl stimulation caused Smad translocation into the nucleus and induced TGF-β-inducible early gene (Tieg1) expression, demonstrating that activity-dependent released TGF-β may exert autocrine actions and thereby activate the TGF-β-dependent signaling pathway (Lacmann et al. 2007). These results suggest an activity-dependent release and gene transcription of TGF-β in mouse hippocampal neurons in vitro as well as subsequent autocrine functions of the released TGF-β within the hippocampal network. TGF-β is also known to have a prominent role in long-term synaptic facilitation in isolated Aplysia ganglia (Zhang et al. 1997b). Within minutes, TGF-β1 stimulated MAPK-dependent phosphorylation of synapsin, which appeared to modulate synapsin distribution, and resulted in a reduced magnitude of synaptic depression (Chin et al. 2002). Most recently, Fukushima and coworkers (2007) were able to show that TGF-β modulates synaptic efficacy and plasticity in dissociated rat hippocampal neurons. Together, increasing evidence suggests that TGF-β may be involved in synaptogenesis, modulation of synaptic transmission, and synaptic plasticity.
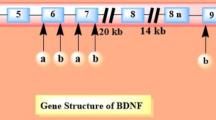
The delayed effects of antidepressants are thought to depend on indirect mechanisms, including the regulation of gene expression, for example antidepressant-induced upregulation of BDNF signaling, which then in turn promotes adaptive neuronal plasticity through effects on gene expression. Wibrand and coworkers (2006) identified five genes (Neuritin, Narp, Tieg1, Carp, and Arl4d) that are co-upregulated with Arc during BDNF-LTP. Tieg1 is a TGF-β-dependent immediate early gene that has also been shown to be upregulated in hippocampal neurons by TGF-β (Lacmann et al. 2007). As TGF-β has been shown to cooperate with BDNF in several scenarios, it may be quite likely that BDNF and TGF-β are the key players in antidepressant-mediated restoration of neuronal plasticity in patients suffering from major depressive disorders.
11 Motoneuron Disease
Amyotrophic lateral sclerosis (ALS) is a fatal disease, leading to paralysis and death. It is characterized by loss of motoneurons. Some ALS cases are due to mutation of the superoxide dismutase 1 (SOD1). TGF-β is a prominent motoneuron survival factor (McLennan and Koishi 2002; Martinou et al. 1990). Using SOD1 knockout mice as a model for ALS application of TGF-β2 caused a rapid and marked but transient improvement in the motoric performance of the mice (Day et al. 2005). In the past years, all components of the TGF-β signaling system have been localized in the presynaptic terminal of the neuromuscular junction, whereby TGF-β ligands are synthesized and localized on the postsynaptic side (McLennan and Koishi 2002; Toepfer et al. 1999). Furthermore, it has been shown that TGF-β2 alters the characteristics of the neuromuscular junction by regulating presynaptic quantal size (Fong et al. 2010).
Appropriate myelination is an important aspect of neuronal activity. Oligodendroglial cells are the myelinating cells of the CNS and Schwann cells of the PNS. Oligodendrocytes arise from a bipotential progenitor cell, the O2A progenitor. TGF-β restricts their PDGF-driven proliferation and induces oligodendroglial differentiation (McKinnon et al. 1993) but may also induce apoptosis (Schuster et al. 2002). In the PNS, TGF-β mediates developmental cell death of Schwann cells (Parkinson et al. 2001) and blocks Schwann cell myelination and expression of myelin-related proteins (Awatramani et al. 2002 and references therein). However, in adult mice TGF-β seems to stabilize compact myelin, as TGF-β1-null mice have grossly abnormal myelin (Day et al. 2003). Ski, a repressor of Smad-mediated TGF-β signaling controls Schwann cell proliferation and myelination, whereas absence of Ski abolished the formation of peripheral myelin, and myelinating Schwann cells upregulate Ski in development as well as during remyelination upon injury (Bonnon and Atanasoski 2012; Atanasoski et al. 2004).
12 Conclusions
TGF-β is a multifunctional and versatile molecule, effecting development, adult maintenance as well as aging of the brain. Although the prototype of a superfamily TGF-β is acting in the nervous system in a highly specific manner. In the context of brain tumors TGF-β is acting very much the way it as expected to by regulating cell cycle, adhesion, and immunosuppression. However, in all other disease scenarios TGF-β action is much more versatile reaching from orchestrating astrocyte and microglia activation to regulating growth factor responsiveness, uptake and release mechanisms, activity-dependent gene expression, and nerve myelination. TGF-β responsiveness may be mediated via alternative TβR-1 usage and may be blocked via the miRNA-dependent downregulation of TβR-II. A new and fascinating aspect is also evident from the modes of TGF-β delivery within the body through transport via lipoproteins or via fibrinogen. In conclusion, the role of TGF-β within brain disorders, either as cause or as key molecule orchestrating responses is only at the beginning of its understanding. Major open issues regard the specific action of individual TGF-β isoform, the context-specificity, the role of TGF-β activation to regulate TGF-β function and complexity of TGF-β signaling and crosstalk. This knowledge will then be also helpful to explain opposing actions of TGF-β such as promotion of survival/protection as to induction of cell death.
Abbreviations
- Aβ:
-
Amyloid β
- AD:
-
Alzheimer’s disease
- Alk:
-
Activin-receptor like kinase
- ALS:
-
Amyotrophic lateral sclerosis
- APP:
-
Amyloid precursos protein
- BBB:
-
Blood–brain barrier
- BDNF:
-
Brain-derived neurotrophic factor
- Cdk:
-
Cyclin-dependent kinase
- CNS:
-
Central nervous system
- CNTF:
-
Ciliary neurotrophic factor
- CSF:
-
Cerebrospinal fluid
- E:
-
Embryonic day
- ECM:
-
Extracellular matrix
- EGF:
-
Epidermal growth factor
- FGF:
-
Fibroblast growth factor
- Fox:
-
Forkhead box
- GDNF:
-
Glial cell line-derived neurotrophic factor
- GFAP:
-
Glial fibrillary acidic protein
- GFRα:
-
GDNF receptor
- Id4:
-
Inhibitors of DNA binding/differentiation
- TIEG:
-
TGF-β immediate early gene
- IL:
-
Interleukin
- Kir:
-
Inward recitfying potassium channels
- MGP:
-
Matrix GLA protein
- MHC:
-
Major histocompatobility class
- MMP:
-
Matrix metalloproteinase
- MPP+:
-
1-methyl-4-phenylpyridinium
- MPTP:
-
1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine
- MS:
-
Multiples sclerosis
- NGF:
-
Nerve growth factor
- PAI:
-
Plasminogen activator inhibitor
- PD:
-
Parkinson’s disease
- PDGF:
-
Platelet-derived growth factor
- PNS:
-
Peripheral nervous system
- SOD:
-
Superoxide dismutase
- TGF- β:
-
Transforming growth factor β
- TβR:
-
TGF-β receptor
- TNF-α:
-
Tumor necrosis factor α
- TRAF:
-
TNF-α receptor associated factor
- t-PA:
-
Tissue plasminogen activator
- VEGF:
-
Vascular endothelial growth factor
References
Abbott NJ, Rönnbäck L, Hansson E (2006) Astrocyte-endothelial interactions at the blood–brain barrier. Nat Rev Neurosci 7:41–53
Abe K, Chu PJ, Ishihara A, Saito H (1996) Transforming growth factor-β 1 promotes re-elongation of injured axons of cultured rat hippocampal neurons. Brain Res 723:206–209
Aderka D, Le JM, Vilcek J (1989) IL-6 inhibits lipopolysaccharide-induced tumor necrosis factor production in cultured human monocytes, U937 cells, and in mice. J Immunol 143:3517–3523
Aigner L, Bogdahn U (2008) TGF-β in neural stem cells and in tumors of the central nervous system. Cell Tissue Res 331:225–241
Anchan RM, Reh TA (1995) Transforming growth factor-β-3 is mitogenic for rat retinal progenitor cells in vitro. J Neurobiol 28:133–145
Araria-Goumidi L, Lambert JC, Mann DM, Lendon C, Frigard B, Iwatsubo T, Cottel D, Amouyel P, Chartier-Harlin MC (2002) Association study of three polymorphisms of TGF-β1 gene with Alzheimer’s disease. J Neurol Neurosurg Psychiatry 73:62–64
Atanasoski S, Notterpek L, Lee HY, Castagner F, Young P, Ehrengruber MU, Meijer D, Sommer L, Stavnezer E, Colmenares C, Suter U (2004) The protooncogene Ski controls Schwann cell proliferation and myelination. Neuron 43:499–511
Awatramani R, Shumas S, Kamholz J, Scherer SS (2002) TGFβ1 modulates the phenotype of Schwann cells at the transcriptional level. Mol Cell Neurosci 19:307–319
Baghdassarian D, Toru-Delbauffe D, Gavaret JM, Pierre M (1993) Effects of transforming growth factor-β1 on the extracellular matrix and cytoskeleton of cultured astrocytes. Glia 7:193–202
Bartholin L, Vincent DF, Valcourt U (2013) TGF-β as tumor suppressor: in vitro mechanistic aspects of growth inhibition. In: Moustakas A, Miyazawa K (eds) TGF-β in human disease. Springer, Tokyo, pp 113–138.
Beck K, Schachtrup C (2012) Vascular damage in the central nervous system: a multifaceted role for vascular-derived TGF-β. Cell Tissue Res 347:187–201
Bertram L, Lill CM, Tanzi RE (2010) The genetics of Alzheimer disease: back to the future. Neuron 68:270–281
Björklund A, Lindvall O (2000) Parkinson’s disease gene therapy moves towards the clinic. Nat Med 6:1207–1208
Boche D, Cunningham C, Gauldie J, Perry VH (2003) Transforming growth factor-β 1-mediated neuroprotection against excitotoxic injury in vivo. J Cereb Blood Flow Metab 23:1174–118
Bodmer S, Strommer K, Frei K, Siepl C, de Tribolet N, Heid I, Fontana A (1989) Immunosuppression and transforming growth factor-β in glioblastoma. Preferential production of transforming growth factor-β 2. J Immunol 143:3222–3229
Bonnon C, Atanasoski S (2012) c-Ski in health and disease. Cell Tissue Res 347:51–64
Böttner M, Krieglstein K, Unsicker K (2000) The transforming growth factor-βs: structure, signaling, and roles in nervous system development and functions. J Neurochem 75:2227–2240
Braak H, Ghebremedhin E, Rub U, Bratzke H, Del Tredici K (2004) Stages in the development of Parkinson’s disease-related pathology. Cell Tissue Res 318:121–134
Buisson A, Lesne S, Docagne F, Ali C, Nicole O, MacKenzie ET, Vivien D (2003) Transforming growth factor-β and ischemic brain injury. Cell Mol Neurobiol 23:539–550
Burton T, Liang B, Dibrov A, Amara F (2002) Transcriptional activation and increase in expression of Alzheimer’s β-amyloid precursor protein gene is mediated by TGF-β in normal human astrocytes. Biochem Biophys Res Commun 295:702–712
Cacheaux LP, Ivens S, David Y, Lakhter AJ, Bar-Klein G, Shapira M, Heinemann U, Friedman A, Kaufer D (2009) Transcriptome profiling reveals TGF-β signaling involvement in epileptogenesis. J Neurosci 29:8927–8935
Cameron JS, Dryer L, Dryer SE (1999) Regulation of neuronal K(+) currents by target-derived factors: opposing actions of two different isoforms of TGFβ. Development 126:4157–4164
Caraci F, Battaglia G, Busceti C, Biagioni F, Mastroiacovo F, Bosco P, Drago F, Nicoletti F, Sortino MA, Copani A (2008) TGF-β 1 protects against Aβ-neurotoxicity via the phosphatidylinositol-3-kinase pathway. Neurobiol Dis 30:234–242
Caraci F, Spampinato S, Sortino MA, Bosco P, Battaglia G, Bruno V, Drago F, Nicoletti F, Copani A (2012) Dysfunction of TGF-β1 signaling in Alzheimer’s disease: perspectives for neuroprotection. Cell Tissue Res 347:291–301
Chalmers KA, Love S (2007a) Neurofibrillary tangles may interfere with Smad 2/3 signaling in neurons. J Neuropathol Exp Neurol 66:158–167
Chalmers KA, Love S (2007b) Phosphorylated Smad 2/3 colocalizes with phospho-tau inclusions in Pick disease, progressive supranuclear palsy, and corticobasal degeneration but not with alpha-synuclein inclusions in multiple system atrophy or dementia with lewy bodies. J Neuropathol Exp Neurol 66:1019–1026
Chin J, Angers A, Cleary LJ, Eskin A, Byrne JH (2002) Transforming growth factor β1 alters synapsin distribution and modulates synaptic depression in Aplysia. J Neurosci 22:RC220
Csuka E, Morganti-Kossmann MC, Lenzlinger PM, Joller H, Trentz O, Kossmann T (1999) IL-10 levels in cerebrospinal fluid and serum of patients with severe traumatic brain injury: relationship to IL-6, TNF-α, TGF-β1 and blood–brain barrier function. J Neuroimmunol 101:211–221
Cunningham JJ, Roussel MF (2001) Cyclin-dependent kinase inhibitors in the development of the central nervous system. Cell Growth Differ 12:387–396
DaCosta BS, Major C, Laping NJ, Roberts AB (2004) SB-505124 is a selective inhibitor of transforming growth factor-β type I receptors ALK4, ALK5, and ALK7. Mol Pharmacol 65:744–752
Day WA, Koishi K, Nukuda H, McLennan IS (2005) Transforming growth factor-β 2 causes an acute improvement in the motor performance of transgenic ALS mice. Neurobiol Dis 19:323–330
Day WA, Koishi K, McLennan IS (2003) Transforming growth factor β 1 may regulate the stability of mature myelin sheaths. Exp Neurol 184:857–864
De Strooper B, Vassar R, Golde T (2010) The secretases: enzymes with therapeutic potential in Alzheimer disease. Nat Rev Neurol 6:99–107
Decressac M, Ulusoy A, Mattsson B, Georgievska B, Romero-Ramos M, Kirik D, Björklund A (2011) GDNF fails to exert neuroprotection in a rat α-synuclein model of Parkinson’s disease. Brain 134:2302–2311
Dell’Orso S, Ganci F, Strano S, Blandino G, Fontemaggi G (2010) ID4: a new player in the cancer arena. Oncotarget 1:48–58
Derynck R, Jarrett JA, Chen EY, Eaton DH, Bell JR, Assoian RK, Roberts AB, Sporn MB (1985) Human transforming growth factor-β cDNA sequence and expression in tumor cell lines. Nature 316:701–705
Dhandapani KM, Brann DW (2003) Transforming growth factor-β: a neuroprotective factor in cerebral ischemia. Cell Biochem Biophys 39:13–22
Dobolyi A, Vincze C, Pál G, Lovas G (2012) The neuroprotective functions of transforming growth factor β proteins. Int J Mol Sci 13:8219–8258
Docagne F, Nicole O, Marti HH, MacKenzie ET, Buisson A, Vivien D (1999) Transforming growth factor-β1 as a regulator of the serpins/t-PA axis in cerebral ischemia. FASEB J 13:1315–1324
Dong Y, Tang L, Letterio JJ, Benveniste EN (2001) The Smad3 protein is involved in TGF-β inhibition of class II transactivator and class II MHC expression. J Immunol 167:311–319
Dryer SE, Lhuillier L, Cameron JS, Martin-Caraballo M (2003) Expression of K(Ca) channels in identified populations of developing vertebrate neurons: role of neurotrophic factors and activity. J Physiol Paris 97:49–58
Dunker N, Krieglstein K (2003) Reduced programmed cell death in the retina and defects in lens and cornea of Tgfβ2(−/−) Tgfβ3(−/−) double-deficient mice. Cell Tissue Res 313:1–10
Dunker N, Schmitt K, Krieglstein K (2002) TGF-β is required for programmed cell death in interdigital webs of the developing mouse limb. Mech Dev 113:111–120
Dunker N, Schuster N, Krieglstein K (2001) TGF-β modulates programmed cell death in the retina of the developing chick embryo. Development 128:1933–1942
Dunnett SB, Björklund A (1999) Prospects for new restorative and neuroprotective treatments in Parkinson’s disease. Nature 399:A32–A39
Fernandez-Espejo E, Armengol JA, Flores JA, Galan-Rodriguez B, Ramiro S (2005) Cells of the sympathoadrenal lineage: biological properties as donor tissue for cell-replacement therapies for Parkinson’s disease. Brain Res Brain Res Rev 49:343–354
Flanders KC, Lippa CF, Smith TW, Pollen DA, Sporn MB (1995) Altered expression of transforming growth factor-β in Alzheimer’s disease. Neurology 45:1561–1569
Flanders KC, Ludecke G, Engels S, Cissel DS, Roberts AB, Kondaiah P, Lafyatis R, Sporn MB, Unsicker K (1991) Localization and actions of transforming growth factor-β s in the embryonic nervous system. Development 113:183–191
Flanders KC, Lüdecke G, Renzig J, Hamm C, Cissel DS, Unsicker K (1993) Effect of TGF-βs and bFGF on astroglial cell growth and gene expression in vitro. Mol Cell Neurosci 4:406–417
Flanders KC, Ren RF, Lippa CF (1998) Transforming growth factor-βs in neurodegenerative disease. Prog Neurobiol 54:71–85
Fogarty MP, Kessler JD, Wechsler-Reya RJ (2005) Morphing into cancer: the role of developmental signaling pathways in brain tumor formation. J Neurobiol 64:458–475
Fong SW, McLennan IS, McIntyre A, Reid J, Shennan KI, Bewick GS (2010) TGF-β2 alters the characteristics of the neuromuscular junction by regulating presynaptic quantal size. Proc Natl Acad Sci USA 107:13515–13519
Forno LS (1996) Neuropathology of Parkinson’s disease. J Neuropathol Exp Neurol 55:259–272
Friedman A (2011) Blood–brain barrier dysfunction, status epilepticus, seizures, and epilepsy: a puzzle of a chicken and egg? Epilepsia 52(Suppl 8):19–20
Fukushima T, Liu RY, Byrne JH (2007) Transforming growth factor-β2 modulates synaptic efficacy and plasticity and induces phosphorylation of CREB in hippocampal neurons. Hippocampus 17:5–9
Gaertner RF, Wyss-Coray T, Von Euw D, Lesne S, Vivien D, Lacombe P (2005) Reduced brain tissue perfusion in TGF-β 1 transgenic mice showing Alzheimer’s disease-like cerebrovascular abnormalities. Neurobiol Dis 19:38–46
Gasser T, Hardy J, Mizuno Y (2011) Milestones in PD genetics. Mov Disord 26:1042–1048
Gross CE, Bednar MM, Howard DB, Sporn MB (1993) Transforming growth factor-β 1 reduces infarct size after experimental cerebral ischemia in a rabbit model. Stroke 24:558–562
Hahn SA, Schutte M, Hoque AT, Moskaluk CA, da Costa LT, Rozenblum E, Weinstein CL, Fischer A, Yeo CJ, Hruban RH, Kern SE (1996) DPC4, a candidate tumor suppressor gene at human chromosome 18q21.1. Science 271:350–353
Hanashima C, Shen L, Li SC, Lai E (2002) Brain factor-1 controls the proliferation and differentiation of neocortical progenitor cells through independent mechanisms. J Neurosci 22:6526–6536
Hau P, Jachimczak P, Bogdahn U (2009) Treatment of malignant gliomas with TGF-β2 antisense oligonucleotides. Expert Rev Anticancer Ther 9:1663–1674
Hau P, Jachimczak P, Schlaier J, Bogdahn U (2011) TGF-β2 signaling in high-grade gliomas. Curr Pharm Biotechnol 12:2150–2157
Huang Y, Mucke L (2012) Alzheimer mechanisms and therapeutic strategies. Cell 148:1204–1222
Hunter KE, Sporn MB, Davies AM (1993) Transforming growth factor-βs inhibit mitogen-stimulated proliferation of astrocytes. Glia 7:203–211
Ishihara A, Saito H, Abe K (1994) Transforming growth factor-β 1 and -β 2 promote neurite sprouting and elongation of cultured rat hippocampal neurons. Brain Res 639:21–25
Ivens S, Kaufer D, Flores LP, Bechmann I, Zumsteg D, Tomkins O, Seiffert E, Heinemann U, Friedman A (2007) TGF-β receptor-mediated albumin uptake into astrocytes is involved in neocortical epileptogenesis. Brain 130(Pt 2):535–547
Jachimczak P, Bogdahn U, Schneider J, Behl C, Meixensberger J, Apfel R, Dorries R, Schlingensiepen KH, Brysch W (1993) The effect of transforming growth factor-β 2-specific phosphorothioate-anti-sense oligodeoxynucleotides in reversing cellular immunosuppression in malignant glioma. J Neurosurg 78:944–951
Johns LD, Babcock G, Green D, Freedman M, Sriram S, Ransohoff RM (1992) Transforming growth factor-β 1 differentially regulates proliferation and MHC class-II antigen expression in forebrain and brainstemastrocyte primary cultures. Brain Res 585:229–236
Joseph JV, Balasubramaniyan V, Walenkamp A, Kruyt FA (2013) TGF-β as a therapeutic target in high grade gliomas—promises and challenges. Biochem Pharmacol 85:478–485
Juraskova B, Andrys C, Holmerova I, Solichova D, Hrnciarikova D, Vankova H, Vasatko T, Krejsek J (2010) Transforming growth factor β and soluble endoglin in the healthy senior and in Alzheimer’s disease patients. J Nutr Health Aging 14:758–761
Klempt ND, Sirimanne E, Gunn AJ, Klempt M, Singh K, Williams C, Gluckman PD (1992) Hypoxia-ischemia induces transforming growth factor β 1 mRNA in the infant rat brain. Brain Res Mol Brain Res 13:93–101
Knuckey NW, Finch P, Palm DE, Primiano MJ, Johanson CE, Flanders KC, Thompson NL (1996) Differential neuronal and astrocytic expression of transforming growth factor β isoforms in rat hippocampus following transient forebrain ischemia. Brain Res Mol Brain Res 40:1–14
Konig HG, Kogel D, Rami A, Prehn JH (2005) TGF-{β}1 activates two distinct type I receptors in neurons: implications for neuronal NF-{κ}B signaling. J Cell Biol 168:1077–1086
Krieglstein K (2006) Transforming growth factor-βs in the brain. In: Lin R (ed) Handbook of neurochemistry and molecular neurobiology, neuroactive proteins and peptides. Springer, Heidelberg, pp 123–141
Krieglstein K, Farkas L, Unsicker K (1998a) TGF-β regulates the survival of ciliary ganglionic neurons synergistically with ciliary neurotrophic factor and neurotrophins. J Neurobiol 37:563–572
Krieglstein K, Henheik P, Farkas L, Jaszai J, Galter D, Krohn K, Unsicker K (1998b) Glial cell line-derived neurotrophic factor requires transforming growth factor-β for exerting its full neurotrophic potential on peripheral and CNS neurons. J Neurosci 18:9822–9834
Krieglstein K, Richter S, Farkas L, Schuster N, Dunker N, Oppenheim RW, Unsicker K (2000) Reduction of endogenous transforming growth factors β prevents ontogenetic neuron death. Nat Neurosci 3:1085–1090
Krieglstein K, Suter-Crazzolara C, Fischer WH, Unsicker K (1995) TGF-β superfamily members promote survival of midbrain dopaminergic neurons and protect them against MPP+ toxicity. EMBO J 14:736–742
Krieglstein K, Unsicker K (1994) Transforming growth factor-β promotes survival of midbrain dopaminergic neurons and protects them against N-methyl-4-phenylpyridinium ion toxicity. Neuroscience 63:1189–1196
Krieglstein K, Unsicker K (1996) Distinct modulatory actions of TGF-β and LIF on neurotrophin-mediated survival of developing sensory neurons. Neurochem Res 21:843–850
Krieglstein K, Zheng F, Unsicker K, Alzheimer C (2011) More than being protective: functional roles for TGF-β/activin signaling pathways at central synapses. Trends Neurosci 34:421–429
Labourdette G, Janet T, Laeng P, Perraud F, Lawrence D, Pettmann B (1990) Transforming growth factor type β 1 modulates the effects of basic fibroblast growth factor on growth and phenotypic expression of rat astroblasts in vitro. J Cell Physiol 144:473–484
Lacmann A, Hess D, Gohla G, Roussa E, Krieglstein K (2007) Activity-dependent release of transforming growth factor-β in a neuronal network in vitro. Neuroscience 150:647–657
Lahn M, Kloeker S, Berry BS (2005) TGF-β inhibitors for the treatment of cancer. Expert Opin Investig Drugs 14:629–643
Lee HG, Ueda M, Zhu X, Perry G, Smith MA (2006) Ectopic expression of phospho-Smad2 in Alzheimer’s disease: uncoupling of the transforming growth factor-β pathway? J Neurosci Res 84:1856–1861
Leof EB, Proper JA, Goustin AS, Shipley GD, DiCorleto PE, Moses HL (1986) Induction of c-sis mRNA and activity similar to platelet-derived growth factor by transforming growth factor β: a proposed model for indirect mitogenesis involving autocrine activity. Proc Natl Acad Sci USA 83:2453–2457
Lindholm D, Castren D, Kiefer R, Zafra F, Thoenen H (1992) Transforming growth factor-β1 in the rat brain: increase after injury and inhibition of astrocyte proliferation. J Cell Biol 117:395–400
Lippa CF, Smith TW, Flanders KC (1995) Transforming growth factor-β: neuronal and glial expression in CNS degenerative diseases. Neurodegeneration 4:425–432
Logan A, Green J, Hunter A, Jackson R, Berry M (1999) Inhibition of glial scarring in the injured rat brain by a recombinant human monoclonal antibody to transforming growth factor-β2. Eur J Neurosci 11:2367–2374
Lou E (2004) Oncolytic viral therapy and immunotherapy of malignant brain tumors: two potential new approaches of translational research. Ann Med 36:2–8
Lyons RM, Gentry LE, Purchio AF, Moses HL (1990) Mechanism of activation of latent recombinant transforming growth factor β 1 by plasmin. J Cell Biol 110:1361–1367
Markowitz S, Wang J, Myeroff L, Parsons R, Sun L, Lutterbaugh J, Fan RS, Zborowska E, Kinzler KW, Vogelstein B, Brattain M, Willson JKV (1995) Inactivation of the type II TGF-β receptor in colon cancer cells with microsatellite instability. Science 268:1336–1338
Martini M, Cenci T, D’Alessandris GQ, Cesarini V, Cocomazzi A, Ricci-Vitiani L, De Maria R, Pallini R, Maria Larocca L (2012) Epigenetic silencing of Id4 identifies a glioblastoma subgroup with a better prognosis as a consequence of an inhibition of angiogenesis. Cancer 119:1004–1012
Martinou JC, Le Van TA, Valette A, Weber MJ (1990) Transforming growth factor β 1 is a potent survival factor for rat embryo motoneurons in culture. Brain Res Dev Brain Res 52:175–181
Massague J (2000) How cells read TGF-β signals. Nat Rev Mol Cell Biol 1:169–178
McKinnon RD, Piras G, Ida JA Jr, Dubois-Dalcq M (1993) A role for TGF-β in oligodendrocyte differentiation. J Cell Biol 121:1397–1407
McLennan IS, Koishi K (2002) The transforming growth factor-βs: multifaceted regulators of the development and maintenance of skeletal muscles, motoneurons and Schwann cells. Int J Dev Biol 46:559–567
Mocali A, Cedrola S, Della Malva N, Bontempelli M, Mitidieri VA, Bavazzano A, Comolli R, Paoletti F, La Porta CA (2004) Increased plasma levels of soluble CD40, together with the decrease of TGF β 1, as possible differential markers of Alzheimer disease. Exp Gerontol 39:1555–1561
Morganti-Kossmann MC, Hans VH, Lenzlinger PM, Dubs R, Ludwig E, Trentz O, Kossmann T (1999) TGF-β is elevated in the CSF of patients with severe traumatic brain injuries and parallels blood–brain barrier function. J Neurotrauma 16:617–628
Nagatsu T, Mogi M, Ichinose H, Togari A (2000) Changes in cytokines and neurotrophins in Parkinson’s disease. J Neural Transm Suppl 60:277–290
Nieder C, Schlegel J, Andratschke N, Thamm R, Grosu AL, Molls M (2003) The role of growth factors in central nervous system tumors. Anticancer Res 23:1681–1686
Packard M, Mathew D, Budnik V (2003) Wnts and TGF β in synaptogenesis: old friends signalling at new places. Nat Rev Neurosci 4:113–120
Pál G, Vincze C, Renner E, Wappler EA, Nagy Z, Lovas G, Dobolyi A (2012) Time course, distribution and cell types of induction of transforming growth factor βs following middle cerebral artery occlusion in the rat brain. PLoS One 7:e46731
Parkinson DB, Dong Z, Bunting H, Whitfield J, Meier C, Marie H, Mirsky R, Jessen KR (2001) Transforming growth factor β (TGFβ) mediates Schwann cell death in vitro and in vivo: examination of c-Jun activation, interactions with survival signals, and the relationship of TGFβ-mediated death to Schwann cell differentiation. J Neurosci 21:8572–8585
Pelton RW, Johnson MD, Perkett EA, Gold LI, Moses HL (1991a) Expression of transforming growth factor-β 1, -β 2, and -β 3 mRNA and protein in the murine lung. Am J Respir Cell Mol Biol 5:522–530
Pelton RW, Saxena B, Jones M, Moses HL, Gold LI (1991b) Immunohistochemical localization of TGF β 1, TGF β 2, and TGF β 3 in the mouse embryo: expression patterns suggest multiple roles during embryonic development. J Cell Biol 115:1091–1105
Peterziel H, Paech T, Strelau J, Unsicker K, Krieglstein K (2007) Specificity in the crosstalk of TGFβ/GDNF family members is determined by distinct GFR α receptors. J Neurochem 103:2491–2504
Peterziel H, Unsicker K, Krieglstein K (2002) TGFβ induces GDNF responsiveness in neurons by recruitment of GFRα1 to the plasma membrane. J Cell Biol 159:157–167
Platten M, Wick W, Weller M (2001) Malignant glioma biology: role for TGF-β in growth, motility, angiogenesis, and immune escape. Microsc Res Tech 52:401–410
Poulsen KT, Armanini MP, Klein RD, Hynes MA, Phillips HS, Rosenthal A (1994) TGF β 2 and TGF β 3 are potent survival factors for midbrain dopaminergic neurons. Neuron 13:1245–1252
Prehn JH, Backhauss C, Krieglstein J (1993) Transforming growth factor-β 1 prevents glutamate neurotoxicity in rat neocortical cultures and protects mouse neocortex from ischemic injury in vivo. J Cereb Blood Flow Metab 13:521–525
Prehn JH, Bindokas VP, Marcuccilli CJ, Krajewski S, Reed JC, Miller RJ (1994) Regulation of neuronal Bcl2 protein expression and calcium homeostasis by transforming growth factor type β confers wide-ranging protection on rat hippocampal neurons. Proc Natl Acad Sci USA 91:12599–12603
Rahhal B, Dunker N, Combs S, Krieglstein K (2004) Isoform-specific role of transforming growth factor-β2 in the regulation of proliferation and differentiation of murine adrenal chromaffin cells in vivo. J Neurosci Res 78:493–498
Rich JN (2003) The role of transforming growth factor-β in primary brain tumors. Front Biosci 8:e245–e260
Rich JN, Zhang M, Datto MB, Bigner DD, Wang XF (1999) Transforming growth factor-β-mediated p15(INK4B) induction and growth inhibition in astrocytes is SMAD3-dependent and a pathway prominently altered in human glioma cell lines. J Biol Chem 274:35053–35058
Roberts AB, Sporn MB (1990) The transforming growth factor-β. In: Sporn MB, Roberts AB (eds) Handbook of experimental pharmacology, vol 95. Springer, Heidelberg, pp 419–472
Roberts AB, Anzano MA, Lamb LC, Smith JM, Sporn MB (1981) New class of transforming growth factors potentiated by epidermal growth factor: isolation from non-neoplastic tissues. Proc Natl Acad Sci USA 78:5339–5343
Roberts AB, Wakefield LM (2003) The two faces of transforming growth factor β in carcinogenesis. Proc Natl Acad Sci USA 100:8621–8623
Rooprai HK, Rucklidge GJ, Panou C, Pilkington GJ (2000) The effects of exogenous growth factors on matrix metalloproteinase secretion by human brain tumour cells. Br J Cancer 82:52–55
Roth P, Eisele G, Weller M (2012) Immunology of brain tumors. Handb Clin Neurol 104:45–51
Roussa E, von Bohlen und Halbach O, Krieglstein K (2009) TGF-β in dopamine neuron development, maintenance and neuroprotection. Adv Exp Med Biol 651:81–90
Roussa E, Farkas LM, Krieglstein K (2004) TGF-β promotes survival on mesencephalic dopaminergic neurons in cooperation with Shh and FGF-8. Neurobiol Dis 16:300–310
Salinas PC (2005) Signaling at the vertebrate synapse: new roles for embryonic morphogens? J Neurobiol 64:435–445
Sanchez-Capelo A (2005) Dual role for TGF-β1 in apoptosis. Cytokine Growth Factor Rev 16:15–34
Schachtrup C, Ryu JK, Helmrick MJ, Vagena E, Galanakis DK, Degen JL, Margolis RU, Akassoglou K (2010) Fibrinogen triggers astrocyte scar formation by promoting the availability of active TGF-β after vascular damage. J Neurosci 30:5843–5854
Schober A, Peterziel H, von Bartheld CS, Simon H, Krieglstein K (2007) Unsicker K GDNF applied to the MPTP-lesioned nigrostriatal system requires TGF-β for its neuroprotective action. Neurobiol Dis 25:378–391
Schober A, Hertel R, Arumae U, Farkas L, Jaszai J, Krieglstein K, Saarma M, Unsicker K (1999) Glial cell line-derived neurotrophic factor rescues target-deprived sympathetic spinal cord neurons but requires transforming growth factor-β as cofactor in vivo. J Neurosci 19:2008–2015
Schulz R, Vogel T, Mashima T, Tsuruo T, Krieglstein K (2009) Involvement of Fractin in TGF-β-induced apoptosis in oligodendroglial progenitor cells. Glia 57:1619–1629
Schuster N, Bender H, Philippi A, Subramaniam S, Strelau J, Wang Z, Krieglstein K (2002) TGF-β induces cell death in the oligodendroglial cell line OLI-neu. Glia 40:95–108
Schuster N, Krieglstein K (2002) Mechanisms of TGF-β-mediated apoptosis. Cell Tissue Res 307:1–14
Seoane J (2006) Escaping from the TGFβ anti-proliferative control. Carcinogenesis 27:2148–2156
Seoane J, Le HV, Shen L, Anderson SA, Massague J (2004) Integration of Smad and forkhead pathways in the control of neuroepithelial and glioblastoma cell proliferation. Cell 117:211–223
Shrikant P, Lee SJ, Kalvakolanu I, Ransohoff RM, Benveniste EN (1996) Stimulus-specific inhibition of intracellular adhesion molecule-1 gene expression by TGF-β. J Immunol 157:892–900
Sorrentino A, Thakur N, Grimsby S, Marcusson A, von Bulow V, Schuster N, Zhang S, Heldin CH, Landström M (2008) The type I TGF-β receptor engages TRAF6 to activate TAK1 in a receptor kinase-independent manner. Nat Cell Biol 10:1199–1207
Specht H, Peterziel H, Bajohrs M, Gerdes HH, Krieglstein K, Unsicker K (2003) Transforming growth factor β2 is released from PC12 cells via the regulated pathway of secretion. Mol Cell Neurosci 22:75–86
Spillantini MG, Crowther RA, Jakes R, Hasegawa M, Goedert M (1998) Alpha-synuclein in filamentous inclusions of lewy bodies from Parkinson’s disease and dementia with lewy bodies. Proc Natl Acad Sci USA 95:6469–6473
Spittau B, Zhou X, Ming M, Krieglstein K (2012) IL6 protects MN9D cells and midbrain dopaminergic neurons from MPP(+)-induced neurodegeneration. Neuromolecular Med 14:317–327
Tesseur I, Zhang H, Brecht W, Corn J, Gong JS, Yanagisawa K, Michikawa M, Weisgraber K, Huang Y, Wyss-Coray T (2009) Bioactive TGF-β can associate with lipoproteins and is enriched in those containing apolipoprotein E3. J Neurochem 110:1254–1262
Tesseur I, Zou K, Esposito L, Bard F, Berber E, Can JV, Lin AH, Crews L, Tremblay P, Mathews P, Mucke L, Masliah E, Wyss-Coray T (2006) Deficiency in neuronal TGF-β signaling promotes neurodegeneration and Alzheimer’s pathology. J Clin Invest 116:3060–3069
Thoenen H (1995) Neurotrophins and neuronal plasticity. Science 270:593–598
Toepfer M, Fischer P, Abicht A, Lochmuller H, Pongratz D, Muller-Felber W (1999) Localization of transforming growth factor β in association with neuromuscular junctions in adult human muscle. Cell Mol Neurobiol 19:297–300
Ueberham U, Ueberham E, Gruschka H, Arendt T (2006) Altered subcellular location of phosphorylated Smads in Alzheimer’s disease. Eur J Neurosci 24:2327–2334
Uhm JH, Gladson CL, Rao JS (1999) The role of integrins in the malignant phenotype of gliomas. Front Biosci 4:D188–D199
Ulusoy A, Decressac M, Kirik D, Björklund A (2010) Viral vector-mediated overexpression of α-synuclein as a progressive model of Parkinson’s disease. Prog Brain Res 184:89–111
Unsicker K, Flanders KC, Cissel DS, Lafyatis R, Sporn MB (1991) Transforming growth factor β isoforms in the adult rat central and peripheral nervous system. Neuroscience 44:613–625
Valente EM, Arena G, Torosantucci L, Gelmetti V (2012) Molecular pathways in sporadic PD. Parkinsonism Relat Disord 18(Suppl 1):S71–S73
van der Wal EA, Gomez-Pinilla F, Cotman CW (1993) Transforming growth factor-β 1 is in plaques in Alzheimer and Down pathologies. Neuroreport 4:69–72
Vogel T, Ahrens S, Büttner N, Krieglstein K (2010) Transforming growth factor β promotes neuronal cell fate of mouse cortical and hippocampal progenitors in vitro and in vivo: identification of Nedd9 as an essential signaling component. Cereb Cortex 20:661–671
Wachs FP, Winner B, Couillard-Despres S, Schiller T, Aigner R, Winkler J, Bogdahn U, Aigner L (2006) Transforming growth factor-β1 is a negative modulator of adult neurogenesis. J Neuropathol Exp Neurol 65:358–370
Wahl SM, Chen W (2003) TGF-β: how tolerant can it be? Immunol Res 28:167–179
Wang H, Liu J, Zong Y, Xu Y, Deng W, Zhu H, Liu Y, Ma C, Huang L, Zhang L, Qin C (2010) miR-106b aberrantly expressed in a double transgenic mouse model for Alzheimer’s disease targets TGF-β type II receptor. Brain Res 1357:166–174
Wendt KM, Schiemann WP (2013) The multifunctional roles of TGF-β in navigating the metastatic cascade. In: Moustakas A, Miyazawa K (eds) TGF-β in human disease. Springer, Tokyo, pp 169–188
Wibrand K, Messaoudi E, Håvik B, Steenslid V, Løvlie R, Steen VM, Bramham CR (2006) Identification of genes co-upregulated with Arc during BDNF-induced long-term potentiation in adult rat dentate gyrus in vivo. Eur J Neurosci 23:1501–1511
Wyss-Coray T, Borrow P, Brooker MJ, Mucke L (1997a) Astroglial overproduction of TGF-β 1 enhances inflammatory central nervous system disease in transgenic mice. J Neuroimmunol 77:45–50
Wyss-Coray T, Lin C, Yan F, Yu GQ, Rohde M, McConlogue L, Masliah E, Mucke L (2001) TGF-β1 promotes microglial amyloid-β clearance and reduces plaque burden in transgenic mice. Nat Med 7:612–618
Wyss-Coray T, Masliah E, Mallory M, McConlogue L, Johnson-Wood K, Lin C, Mucke L (1997b) Amyloidogenic role of cytokine TGF-β1 in transgenic mice and in Alzheimer’s disease. Nature 389:603–606
Xuan S, Baptista CA, Balas G, Tao W, Soares VC, Lai E (1995) Winged helix transcription factor BF-1 is essential for the development of the cerebral hemispheres. Neuron 14:1141–1152
Yamashita K, Gerken U, Vogel P, Hossmann K, Wiessner C (1999) Biphasic expression of TGF-β1 mRNA in the rat brain following permanent occlusion of the middle cerebral artery. Brain Res 836:139–145
Yi JJ, Barnes AP, Hand R, Polleux F, Ehlers MD (2010) TGF-β signaling specifies axons during brain development. Cell 142:144–157
Yingling JM, Blanchard KL, Sawyer JS (2004) Development of TGF-β signalling inhibitors for cancer therapy. Nat Rev Drug Discov 3:1011–1022
Zhang F, Endo S, Cleary LJ, Eskin A, Byrne JH (1997a) Role of transforming growth factor-β in long-term synaptic facilitation in Aplysia. Science 275:1318–1320
Zhang JM, Hoffmann R, Sieber-Blum M (1997b) Mitogenic and anti-proliferative signals for neural crest cells and the neurogenic action of TGF-β1. Dev Dyn 208:375–386
Zhu Y, Ahlemeyer B, Bauerbach E, Krieglstein J (2001) TGF-β1 inhibits caspase-3 activation and neuronal apoptosis in rat hippocampal cultures. Neurochem Int 38:227–235
Zhu Y, Culmsee C, Klumpp S, Krieglstein J (2004) Neuroprotection by transforming growth factor-β1 involves activation of nuclear factor-κB through phosphatidylinositol-3-OH kinase/Akt and mitogen-activated protein kinase-extracellular-signal regulated kinase1,2 signaling pathways. Neuroscience 123:897–906
Zhu Y, Roth-Eichhorn S, Braun N, Culmsee C, Rami A, Krieglstein J (2000) The expression of transforming growth factor-β1 (TGF-β1) in hippocampal neurons: a temporary upregulated protein level after transient forebrain ischemia in the rat. Brain Res 866:286–298
Zhu Y, Yang GY, Ahlemeyer B, Pang L, Che XM, Culmsee C, Klumpp S, Krieglstein J (2002) Transforming growth factor-β 1 increases bad phosphorylation and protects neurons against damage. J Neurosci 22:3898–3909
Zindy F, Cunningham JJ, Sherr CJ, Jogal S, Smeyne RJ, Roussel MF (1999) Postnatal neuronal proliferation in mice lacking Ink4d and Kip1 inhibitors of cyclin-dependent kinases. Proc Natl Acad Sci USA 96:13462–13467
Acknowledgments
Work from the author’s laboratory is supported by grants from the Deutsche Forschungsgemeinschaft (including SFB780, Kr1477/10 and 11).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer
About this chapter
Cite this chapter
Krieglstein, K. (2013). TGF-β in Brain Disorders. In: Moustakas, A., Miyazawa, K. (eds) TGF-β in Human Disease. Springer, Tokyo. https://doi.org/10.1007/978-4-431-54409-8_17
Download citation
DOI: https://doi.org/10.1007/978-4-431-54409-8_17
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-54408-1
Online ISBN: 978-4-431-54409-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)