Abstract
Presbycusis occurs mainly as a result of aging of the cochlea and the central auditory system. This chapter presents observations made using unconventional techniques to evaluate the nerve fibers in the organ of Corti, the basilar membrane, the stereocilia of the outer hair cells, and the stria vascularis in elderly people. Stained surface preparations of nerve fibers in the organ of Corti and the osseous spiral lamina were observed. Afferent and efferent nerve fibers were reduced in number in the lower basal turn in the elderly. Swellings of the efferent nerve fibers crossing the tunnel of Corti were occasionally observed. These swellings resembled the torpedoes seen in Purkinje cell degeneration. The medial fiber is considered an efferent fiber, and sometimes extends laterally beyond the outer hair cell area.
The stereocilia of the outer hair cells showed various types of degeneration with aging. Loss of individual hairs, fusion of several hairs, and giant cilia were common findings. After complete disappearance of the stereocilia, the surface of the cuticular plate showed remnants of equally-sized stumps, suggesting the breaking point of each hair.
In strial atrophy, the cells composing the stria vascularis disappeared with the strial capillaries. The basilar membrane of elderly people showed lipid deposits in the basal turn. These deposits were composed of neutral fat and cholesterol and were located along the filaments of the pars pectinata. As for prevention of presbycusis, an animal experiment revealed that caloric restriction prevented the age-related loss of spiral ganglion cells.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Nerve Fibers in the Osseous Spiral Lamina
The axons of the spiral ganglion cells leave Rosenthal’s canal, and join at the central bony axis, the modiolus, to form the cochlear nerve. The dendrites of the spiral ganglion cells pass between the upper and lower shelves of the osseous spiral lamina as they head toward the organ of Corti. Near the end of the spiral lamina are small foramina called habenula perforata, through which unmyelinated nerve fibers pass to the inner and outer hair cells.
In young people, the cochlea contains abundant nerve fibers leaving Rosenthal’s canal, their bundles gradually fanning out radially in the osseous spiral lamina (Fig. 8.1). Spiral fibers intermingle with the radial fibers in the osseous spiral lamina.
In elderly people, the cochlea shows loss of radial and spiral fibers, particularly in the lower basal turn, with less loss toward the apex (Fig. 8.2).
Myelinated nerve fibers in the osseous spiral lamina. Bundles of nerve fibers emerge from Rosenthal’s canal, and fan out in the osseous spiral lamina. (a) The radial and spiral fibers are densely intermingled in the lamina of the middle turn. (b) Both radial and spiral fibers are reduced in the basal turn. (c) Almost no fibers remain near the basal end. Seventy-five-year-old woman, Sudan Black B staining, ×10
Histochemical staining for acetylcholinesterase specifically stains the efferent nerve fibers, leaving the afferent fibers unstained. From spiral bundles, fibers radiate outward, eventually terminating primarily on the outer hair cells. In the organ of Corti, the outer spiral bundle shows acetylcholinesterase activity, though postmortem autolysis may obscure details (Fig. 8.3a, b) [1, 2]. In the lower basal turn of a 59-year-old man, most of the afferent and efferent nerve fibers had disappeared, with only a few fibers remaining (Fig. 8.3c). The course of the afferent fibers was relatively simple. By contrast, the efferent fibers followed a complicated course (Fig. 8.4). No efferent fibers were seen in the osseous spiral lamina of the cochlea (Fig. 8.5). Clinical data were not available for this individual.
Distribution of efferent fibers in the organ of Corti and osseous spiral lamina. (a) Strong staining at the top of the photograph indicates acetylcholinesterase activity in the organ of Corti (×45). (b) High power view of the organ of Corti. Sparse enzyme activity due to marked loss of the organ of Corti and postmortem changes. OSB outer spiral bundles (×160). (c) A single efferent fiber (white arrow) and a few afferent fibers (black arrow) remain in the lower basal turn (×160). Fifty-nine-year-old man, staining for acetylcholinesterase
Efferent and afferent fibers in the osseous spiral lamina. Because of the difficulty of pursuing the course of an individual fiber, an area with reduced fibers is selected for observation. Generally, the afferent fibers run radially, whereas the efferent fibers run spirally with a complicated course before taking a radial course to the organ of Corti. unstained fiber afferent fiber, stained fiber efferent fiber ×160
Gacek [3] reported a case in which the cochlea showed only efferent fibers.
8.2 Nerve Fibers in the Organ of Corti
It is difficult to follow nerve fibers in the organ of Corti in serial temporal bone specimens. However, they are easier to follow in properly stained surface specimens of the cochlea. When observed as a surface preparation, the tunnel of Corti is seen as a wide, clear belt because of its sparse cellularity. Individual nerve fibers can be clearly observed here (Figs. 8.6 and 8.7). The medial fiber and basilar fiber cross the tunnel of Corti. The medial fiber crosses the medial part of the tunnel, and is the efferent fiber [4]. The basilar fiber crosses the tunnel at its base and is the afferent fiber (Fig. 1.19).
According to Spoendlin [5], 90 % of the afferent fibers in the cat terminate on the inner hair cells, while 10 % terminate on the outer hair cells.
A similar finding was observed in a human organ of Corti, where only the basilar fiber was observed in the tunnel of Corti in a 6-month-old fetus after Holmes staining. The basilar fibers ran at the base of the tunnel, maintaining regular spacing. Evaluation revealed that 10–15 % of the nerve fibers crossed the tunnel to reach the outer hair cells after passing through the habenula perforata (Fig. 8.8) [6].
Basilar fibers crossing the tunnel, maintaining a regular interval. No medial fibers are seen [6]. ESB external (outer) spiral bundle, BF basilar fiber, HP habenula perforata. The basal direction is to the right in the figure. Six-month-old fetus, Holmes staining
Some efferent fibers have the appearance of a gigantic old tree. Perhaps the composing fibers loosen in the process of degeneration (Fig. 8.9).
A striking finding in the medial fibers is the presence of spindle-shaped swellings, similar in appearance to torpedoes (Figs. 8.10–8.12). These fibers are generally thick, and after forming a torpedo shape they bifurcate before joining the outer spiral bundles.
The spindle-shaped swelling observed in the efferent fibers appears similar to Purkinje cell axonal torpedoes. According to Louis et al. [7], a prominent finding in the cerebellum of patients with essential tremor is an abundance of torpedoes, swellings that result from the mis-accumulation of cell constituents. Immunoreactivity for phosphorylated neurofilament protein revealed clear labeling of torpedoes. On electron microscopy, torpedoes were packed with randomly arranged 10–12 nm neurofilaments. Mitochondria and smooth endoplasmic reticulum were abundant at the periphery of the torpedoes. The authors concluded that the torpedoes in essential tremor represent the mis-accumulation of disorganized neurofilaments and other organelles.
Efferent nerve fibers run spirally in the osseous spiral lamina toward the apex. In the cochlea of elderly people, both afferent and efferent fibers show the greatest loss in the lower basal turn. The torpedoes were rarely observed in aged cochleae, whereas they sometimes appear in younger individuals, where they are evenly distributed throughout the cochlea. The torpedoes might suggest a degenerative process of the nuclei of the efferent fibers.
8.3 Nerve Fibers Running Lateral to the Hair Cell Area
Occasionally, the medial fibers run laterally, away from the outer spiral bundles. The fibers bifurcate and run tortuously in the Hensen’s cell or Claudius’ cell area, but never extend to the spiral ligament. The termination of these fibers has not yet been determined (Figs. 8.13, 8.14, and 8.15).
8.4 Degeneration of Sensory Hairs on the Outer Hair Cells
Surface preparations of the organ of Corti of elderly people show loss of hair cells. The arrangement of hair cells and supporting cells becomes irregular with advancing age (Fig. 8.16). Details of the stereocilia cannot be clarified at the light microscopic level.
Surface specimen of the lower basal turn. Partial loss of inner and outer hair cells. Arrows point to areas of loss of inner hair cells and of outer hair cells in the first and third rows. IHC inner hair cell area, TC tunnel of Corti, OHC outer hair cell area. Seventy-one-year-old man, trichrome staining (×40)
One study evaluated the surface of the outer hair cells of elderly patients, aged 80–91 years, using a scanning electron microscope [8]. Fifteen temporal bones were studied within a 1–1.5 h postmortem interval. The organ of Corti from the upper basal turn to the middle turn was examined in this study.
The surface of the membrana reticularis showed normal stereocilia as well as hairs with varying degrees and types of degeneration (Fig. 8.17). Pathological changes of the stereocilia were mainly loss of hairs and giant cilia formation [8]. Cytoplasmic protrusion was another pathological change on the surface of the outer hair cells.
Changes in the stereocilia of the outer hair cells [8]. (a) Normal stereocilia of the outer hair cell. (b) Marked defect of the central stereocilia. Two giant stubs are seen at the center and a side of the stereocilia. (c) Marked loss of the central stereocilia around the giant cilium. (d) After loss of the stereocilia, remnants of equal size and shape are seen. Eighty-six-year-old woman, scale: 1 μm × 7500
Hair loss occurred in all regions of the stereocilia, i.e., in the peripheral area, the central area, or a mixture of the two. There was no particular pattern of loss distribution in different parts of the organ of Corti (Fig. 8.18).
Total hair loss was also seen, and this is a terminal stage before the stereocilia disappear. After disappearance of the stereocilia, remnants persisted on the surface of the cuticular plate. These were of uniform hemispherical shape and size, with a diameter of approximately 0.1 μm, suggesting a natural breaking point in each stereocilium. The remnants sometimes coexisted with a few remaining abnormal stereocilia.
A W-configuration could still be recognized in this case. As the degenerative process continues, the cuticular plate begins to disappear and the number of remnants decreases. The W-configuration becomes eccentric as surrounding cells invade the cuticular plate. Eventually, the hair cell surface is replaced by supporting cells. In this case there was a shallow depression indicating almost complete disappearance of the outer hair cells and replacement by the phalanx of Deiters’ cells and outer pillar cells (Fig. 8.19) [9]. The membrana reticularis consists of the cuticle, the phalanx of Deiters’ cells, and the outer pillar cells.
Repair of the membrana reticularis [9]. Two outer hair cells have disappeared in the second row. Eighty-six-year-old woman, scale: 5 μm, (×3,300)
A giant cilium is produced through fusion of hairs. Reorganization takes place within the fused hair. The length of the giant cilium is indicative of its growth. This can be interpreted as a premortem change rather than a postmortem change or artifact.
8.5 Strial Atrophy
Aging is one cause of degeneration of the stria vascularis. Schuknecht and Gacek [10] proposed defining strial presbycusis as the loss of at least 30 % of the strial tissue. Typically strial atrophy is patchy and is more pronounced in the middle and apical turns. On audiometry, flat elevations or slightly descending pure tone thresholds are seen in patients with strial atrophy, with preservation of good speech discrimination scores.
When fresh stria vascularis was stained for alkaline phosphatase and observed as a surface preparation, it was found that the remaining strial tissue always surrounded the strial capillary in the atrophic area. No strial capillary was found without surrounding strial tissue (Figs. 8.20, 8.21, and 8.22). Complete loss of a localized area of the stria vascularis suggests atrophy of the spiral prominence as a result of loss of the vas spirale (Fig. 8.23).
8.6 Lipidosis of the Basilar Membrane
Precipitates are found in the basilar membrane of elderly people.
Twenty-four human temporal bones from 20 patients ranging in age from 71 to 95 years were studied. After fixation in 10 % formalin and decalcification with a 5 % solution of trichloroacetic acid, the temporal bones were trimmed and the membranous labyrinth was exposed.
The following staining procedures were employed: 1. Osmium tetroxide-α-naphthylamine (OTAN) method, 2. Sudan III staining, 3. Nile blue sulfate method, 4. PAS reaction, 5. Smith-Dietrich reaction, 6. Observations under ultraviolet light and polarized light [11].
In some cases ultrasonic shaking was performed to disintegrate and detach the organ of Corti from the basilar membrane, before or after staining. Stained tissue was washed in distilled water and mounted as a flat specimen in polyvinyl pyrrolidone medium.
There were lipid deposits along the filamentous structure of the pars pectinata in the lower basal turn. Nine ears from 12 patients showed lipid deposits in the basilar membrane. Six cochleae from three younger patients, aged 1, 24, and 37 years, did not show any deposits at all. In specimens in which the organ of Corti was detached by ultrasonic shaking, the lipid deposits were more clearly observed. Deposits were most prominent in the basal turn from the vicinity of the basal end to the 5–10 mm area, and were more heavily distributed near the basal end than apically. The apical and middle turns failed to show deposits in the basilar membrane.
The following test results were obtained. The deposits were soluble in ether-alcohol. They were sudanophilic, stained pink by Nile blue sulfate, and showed partial birefringence under crossed nicols. Deposits were composed mainly of neutral fat with small amounts of cholesterol. No reaction was seen with the PAS or Smith-Dietrich methods, indicating the absence of glucolipid and phospholipid, respectively. Because the deposit did not fluoresce, the presence of lipofuscin was not likely. Formalin solution is not the best fixative for lipids, so it is possible that certain constituents were lost during fixation (Figs. 8.24, 8.25, and 8.26).
Lipidosis of the basilar membrane [11]. Left: 3 mm area of the lower basal turn. Right: 9 mm area. Marked lipid deposits are present in the 3 mm area. Eighty-six-year-old woman, osmium tetroxide-α-naphthylamine (OTAN) method (×400)
The basilar membrane is composed of ground substance, filaments, and a few connective tissue cells. The inner part, the pars tecta, is formed of radially arranged filaments, which are not grouped in bundles but lie side by side in scant ground substance. Beneath the filaments is cottony ground substance without filaments. The outer part of the basilar membrane, the pars pectinata, is thicker and striated. It is formed of compactly arranged, grouped filaments, all of which run radially. The space between filaments is filled with scant ground substance. The fibers are separated from each other by abundant cottony ground substance and are arranged in two strata [12, 13].
Mayer [14] reported that people over 60 years of age showed thickening of the basilar membrane. According to Mayer, calciferous deposits and occasional ossification was also observed in the thickened membrane. He believed that basilar membrane rigidity was the anatomical basis for presbycusis.
The basilar membrane is a tissue usually devoid of discernible lipids [15]. The formation of fat in tissue other than adipose tissue is called aberrant lipogenesis, which is thought to be related to fatty degeneration and atheromatosis [16].
It is not clear how lipids are deposited in the basilar membrane. The serum cholesterol levels of these patients had no correlation with the presence of lipid deposits. Because the deposits occurred in the lower basal turn, degeneration of the organ of Corti might be responsible for their formation. However, lipid deposits were also found in regions of the basilar membrane where the organ of Corti was intact. Because the basilar membrane from younger individuals did not show these deposits, aging may be closely related to the formation of the lipids. The motion of traveling waves in the basilar membrane may be influenced by the presence of the lipids, and the deposits may alter the membrane structure.
8.7 Prevention of Presbycusis
There is a paper suggesting that caloric restriction can prevent loss of spiral ganglion cells and hair cells in the organ of Corti. According to Lee et al. [17], most rodents demonstrate delayed onset of age-related pathological changes and have extended maximum lifespans when subjected to a long-term 20–50 % reduction in caloric intake without essential nutrient deficiency.
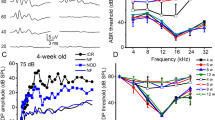
Someya et al. [18] observed the effects of caloric restriction on cochlear degeneration in mice. They restricted the caloric intake of experimental mice to 74 % that of control animals in early adulthood, and maintained this dietary regimen until the mice were 15 months of age. The mean weight of the 15-month-old caloric restriction mice was significantly lower than that of the 15-month-old control mice, but was not different from the mean weight of young control mice. ABR threshold measurements revealed that the young control mice exhibited normal hearing, whereas the 15-month-old control mice exhibited significant age-related hearing loss. In contrast, the 15-month-old caloric restricted mice displayed normal hearing.
The cochleae of the 15-month-old control mice showed the morphological characteristics of apoptosis, such as cell shrinkage and chromatin condensation in the spiral ganglion cells (Fig. 8.27b, e), indicating that apoptosis was associated with the development of presbycusis. The cochleae of the caloric restriction mice did not show cell shrinkage, but showed some chromatin condensation (Fig. 8.27c, f). The cochleae of young control mice showed no cell shrinkage or chromatin condensation (Fig. 8.27a, d).
Caloric restriction prevents presbycusis [18]. YC 4-month-old young control group, MC 15-month-old control group, CR 15-month-old caloric restricted group. Arrowheads in panels (a)–(c) indicate the spiral ganglion regions. Arrowhead in panel (d) indicates normal neurons. Arrowheads in panels (e) and (f) indicate neurons with marked chromatin condensation, a morphological characteristic of apoptosis. MC mice displayed severe degeneration of spiral ganglion cells, decreased cell body size, and chromatin condensation. CR mice displayed no significant degeneration of spiral ganglion cells, showing that caloric restriction prevented cochlear degeneration. CR mice showed no significant cell shrinkage, but did display some chromatin condensation ((c) and (f)). Scale: 50 μm (upper panel), 100 μm (lower panel) (Courtesy of Dr. Yamasoba)
Caloric restriction mice also showed a significant reduction in the number of TUNEL-positive cells and cleaved caspase-3-positive cells relative to the 15-month-old control mice. Microarray analysis revealed that caloric restriction down-regulated the expression of 24 apoptotic genes. Suppression of apoptosis by caloric restriction can prevent presbycusis.
References
Nomura Y, Kirikae I (1967) Innervation of the human cochlea. Ann Otol Rhinol Laryngol 76:57–68
Nomura Y, Kirikae I (1968) Presbyacusis. A histological-histochemical study of the human cochlea. Acta Otolaryngol 66:17–24
Gacek RR (1961) The efferent cochlear bundle in man. Arch Otolaryngol 74:690–694
Spoendlin H, Gacek R (1963) Electron microscopic study of the efferent and afferent innervation of the organ of corti in the cat. Ann Otol Rhinol Laryngol 72:660–686
Spoendlin H (1985) Anatomy of cochlear innervation. Am J Otolaryngol 6:453–467
Nomura Y (1976) Nerve fibers in the human organ of corti. Acta Otolaryngol 82:317–324
Louis ED, Yi H, Erickson-Davis C, Vonsattel JP, Faust PL (2009) Structural study of Purkinje cell axonal torpedoes in essential tremor. Neurosci Lett 450:287–291
Nomura Y, Kawabata I (1978) The pathology of sensory hairs in the human organ of corti, Scanning Electron Microscopy 1978/II. IITRI, Chicago, pp 417–422
Nomura Y, Kawabata I (1979) Loss of stereocilia in the human organ of corti. Acta Otorhinolaryngol 222:181–185
Schuknecht HF, Gacek MR (1993) Cochlear pathology in presbycusis. Ann Otol Rhinol Laryngol 102:1–16
Nomura Y (1970) Lipidosis of the basilar membrane. Acta Otolaryngol 69:352–357
Iurato S (1962) Functional implictions of the nature and submicroscopic structure of the tectorial membrane and basilar membrane. J Acoust Soc Amer 34:1386–1395
Iurato S (1967) Submicroscopic structure of the inner ear. Pergamon, Oxford
Mayer O (1920) Das anatomisches Substrat der Altersschwerhörighkeit. Arch Ohr Nas Kehlkopfheilk 105:1–13
Schätzle W, von Westernhagen B (1967) Lipidnachweis in der Cochlea. Pract Otorhinolaryngol (Basel) 29:75–84
Cogan DG, Kuwabara TK (1960) Aberrant lipogenesis. Nutr Rev 18:225–227
Lee CK, Klopp RG, Weindruch R, Prolla TA (1999) Gene expression profile of aging and its retardation by caloric restriction. Science 285:1390–1393
Someya S, Yamasoba T, Weindruch R, Prolla TA, Tanokura M (2007) Caloric restriction suppresses apoptotic cell death in the mammalian cochlea and leads to prevention of presbycusis. Neurobiol Aging 28:1613–1622
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Japan
About this chapter
Cite this chapter
Nomura, Y., Nomura, Y., Nomura, Y. (2014). Presbycusis. In: Morphological Aspects of Inner Ear Disease. Springer, Tokyo. https://doi.org/10.1007/978-4-431-54204-9_8
Download citation
DOI: https://doi.org/10.1007/978-4-431-54204-9_8
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-54203-2
Online ISBN: 978-4-431-54204-9
eBook Packages: MedicineMedicine (R0)