Abstract
All sensory hair cells of the inner ear exist in extracellular fluid, but in some areas the fluid has the characteristics of intracellular fluid, as far as concentrations of K+ and Na+ are concerned. The membranous labyrinth contains the intracellular fluid-like endolymph, and is surrounded by a distinct extracellular fluid, the perilymph. The sensory hair cells of the cochlea are surrounded by extracellular fluid called cortilymph in a separate compartment. Excessive accumulation or leakage of any of these fluids may affect the functions of the whole or partial inner ear.
This chapter is concerned with perilymphatic fistula, signs and symptoms of which mimic Meniere’s disease and sudden deafness. Because the pathophysiology of perilymphatic fistula formation is not clear, we have attempted to experimentally induce leakage of perilymph from the cochlear windows of guinea pigs by injecting artificial perilymph into the subarachnoid space or by suctioning a small amount of perilymph through the round window membrane. In these studies, the membranous labyrinth demonstrated various changes. The cochlea developed endolymphatic hydrops. The vestibular membranous labyrinth collapsed to a greater or lesser degree. In some experimental conditions, the organ of Corti showed cortilymphatic hydrops.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cerebrospinal fluid pressure
- Cochlear aqueduct
- Cortilymphatic hydrops
- Experimental perilymphatic fistula
- Perilymph
- Perilymphatic fistula
2.1 Inner Ear Fluid
2.1.1 Perilymph and Endolymph
In 1760, Domenico Cotugno (Italian anatomist, 1736–1822) discovered the presence of fluid in the inner ear, which was thereafter called the “liquid of Cotugno.” Later, Henri Marie Ducrotay de Blainville (French anatomist, 1777–1850) named the fluid “perilymph.” The fluid within the membranous labyrinth was called “endolymph of Breschet” (Gilbert Breschet, French anatomist, 1784–1845). The vestibular membrane was described in 1854 by Ernst Reissner (German anatomist, 1824–1878), and has been called Reissner’s membrane since that time.
2.1.2 Cortilymph
A third fluid space exists within the organ of Corti. Morphological studies have found no direct communication between the endolymphatic or perilymphatic spaces and the fluid within the organ of Corti. In 1960, Hans Engström [1] proposed the name “cortilymph” for the fluid filling the tunnel of Corti, the space of Nuel, the region around the hair cells, and the outer tunnel (Fig. 2.1).
The cortilymph occupies the space within the organ of Corti [1]. Engström H (1960) Acta Morphol Neerl Scand 3:195 Taylor & Francis Ltd. www.tandfonline.com
Schuknecht and Seifi [2] perfused the scala tympani of a cat with a histochemical acetylcholinesterase staining solution, and found deposits of reaction product extending from holes in the lower shelf of the osseous spiral lamina to inside the organ of Corti (Fig. 2.2). Schuknecht believed that these were communicating perilymph channels from the scala tympani to the organ of Corti. The holes in the lower shelf of the osseous spiral lamina were named the “canaliculi perforantes Schuknechtii.” They are located 0.2 mm from the habenula perforata in the cat. The staining solution flowed from the osseous spiral lamina through the habenula perforata into the organ of Corti. In a frozen specimen, however, no acetylcholinesterase reaction deposit could be found in the lower shelf of the osseous spiral lamina (Fig. 2.3).
Masuda et al. [3] demonstrated perilymphatic communication routes between the perilymph of the scala tympani and the cortilymph in guinea pigs by injecting inulin-methoxy-H3 through the round window membrane. Inulin accumulated not only in the habenula perforata and basilar membrane, but also in the cortilymph spaces, suggesting that the habenula perforata and basilar membrane are communication routes between the two spaces.
Nomura [4] perfused the scala tympani of guinea pigs using staining solution for succinic dehydrogenase with phenazine methosulfate. There were numerous holes in the lower shelf of the osseous spiral lamina through which the solution penetrated into the osseous spiral lamina (Fig. 2.4). Formation of reaction product, formazan, was rapid with phenazine methosulfate. Staining was observed along nerve fibers in the osseous spiral lamina. The staining solution passed from the osseous spiral lamina through the habenula perforata to the space in the organ of Corti (Fig. 2.5). The entire basilar membrane was eventually stained blue. But the first very rapid passage of solution into the organ of Corti was via a passageway between Deiters’ cells and Hensen’s cells (Fig. 2.6) [4]. According to Beagley [5], normal histological preparations showed fine canal-like intercellular spaces between Deiters’ cells and Hensen’s cells. Near the membrana reticularis, however, strong desmosomes join Hensen’s cells to the outermost phalangeal process of Deiters’ cells and this area seemed quite stable under the stress of acoustic trauma. By contrast, the base of the Hensen-Deiters’ junction showed a wide cleft in some acoustically stimulated guinea pigs. Beagley was of the opinion that the Hensen-Deiters’ split had protected the hair cells from acoustic stimuli.
Numerous holes (arrows) seen in the lower shelf of the osseous spiral lamina of the guinea pig. Staining solution for succinic dehydrogenase with phenazine methosulfate was introduced in the scala tympani (original ×16) [4]
Fluid passageway from the scala tympani to the organ of Corti. The solution entered through holes in the lower osseous spiral lamina to the inside the osseous spiral lamina of the guinea pig. The nerve fibers were stained. The solution entered the organ of Corti through the habenula perforata and basilar membrane (original ×6.5)
Fluid passageway through the basilar membrane. Marker solution rapidly passed through the localized area of basilar membrane, and entered the organ of Corti through the space between Deiters’ cell and Hensen’s cell in the guinea pig (arrow). Arrow indicates a route for fluid into the organ of Corti (original ×40) [4]
From an electron microscopic study, Ishiyama and Ishiyama [6] noted that there was a wide gap between Deiters’ cells and Hensen’s cells adjacent to the basilar membrane (Fig. 2.7).
There is a wide space between the junction (asterisk) of Deiters’ cell and Hensen’s cell. The inset shows the area of observation. Arrow indicates a route for fluid into the organ of Corti. HC Hensen’s cell, scale: 1 μm (Courtesy of Drs. Ishiyama and Ishiyama) [6]
In Nomura’s study, after perfusion of the solution containing phenazine methosulfate, the organ of Corti became hydropic. Hensen’s cells were pushed laterally, detached from the basilar membrane, and ballooned, so that there was a large space in the lateral part of the organ of Corti including the outer tunnel. This is the initial sign of formation of cortilymphatic hydrops. If hydropic conditions progress, the lateral portion of the membrana reticularis will be lifted (Fig. 2.8).
Cortilymphatic hydrops. The organ of Corti is stained blue. Hensen’s cell is detached from the basilar membrane. The split between Deiters’ cell and Hensen’s cell is enlarged. Hensen’s cells are ballooned (arrows). Lateral part of the membrana reticularis is lifted. The inner pillar cell is crushed. Perfusion of the solution for staining succinic dehydrogenase with phenazine methosulfate, Guinea pig, original ×40
The pillar cells and Deiters’ cells contain large numbers of tonofibrils. The pillar cells are firmly fixed to the basilar membrane. These cells together with the membrana reticularis strongly support the architecture of the organ of Corti. Hensen’s cells have no contact with Deiters’ cells at the base. The lateral aspect of the organ of Corti, where Hensen’s cells are found, is the weakest and least able to tolerate increased pressure. Although the functions of Hensen’s cells are not well understood, one role may be to release pressure within the organ of Corti.
As hydrops of the organ of Corti progresses with increasing osmotic pressure and/or diffusion from the scala tympani, the phalangeal processes of Deiters’ cells and the pillar cells become slender, and hair cells disappear. The membrana reticularis and Hensen’s cells become thin, but as a tough membrane they maintain the boundary of the organ of Corti (Fig. 2.9).
Schema showing the process of cortilymphatic hydrops formation. Fluid enters the organ of Corti through the Deiters–Hensen’s cell slit and habenula perforata. As the pillar cells and Deiters’ cells are hardy, Hensen’s cells are pushed laterally. As hydrops progresses, the pillar cells and Deiters’ cell become elongated. The outer hair cells disappear
Djeric and Schuknecht [7] reported two cases of Hensen’s cell cyst of the organ of Corti in human temporal bones. The cysts were bilaterally symmetrical. The authors postulated that the cysts might represent coalesced lipid droplets from Hensen’s cells.
2.1.3 The Cochlear Aqueduct
The cochlear aqueduct and fundus of the internal auditory canal are communicating routes between the cerebrospinal fluid (CSF) and the perilymph (Fig. 2.10). The internal aperture of the cochlear aqueduct is located near the round window and the inferior cochlear vein (Fig. 2.11).
Gopen et al. [8] evaluated 101 temporal bones from subjects aged 0–100 years, and reported that the mean diameter of the narrowest portion of the cochlear aqueduct was 138 ± 58 μm, which occurred 200–300 μm from the cochlear end of the aqueduct. They noted four types of aqueduct patencies: central lumen patent throughout the length of the aqueduct (34 %), lumen filled with loose connective tissue (59 %), lumen occluded by bone (4 %), and obliteration of the aqueduct (3 %). There was no correlation between age and narrowest diameter, or between age and type of patency.
The cochlear aqueduct is not a route for cerebrospinal fluid in cases of stapes gusher. Stapes gusher occurs in the cochlea when the fundus of the internal auditory canal is missing, and a wide communication exists between the internal auditory canal and the scala vestibuli (Fig. 2.12).
This temporal bone is from a patient with otopalatodigital syndrome. The bone shows fixation of the stapes, scala communis, defective modiolus, and a large communication between the internal auditory canal and scala vestibuli. No fundus of the internal auditory canal is observed. There is a risk of stapes gusher occurrence (Courtesy of Dr. Schuknecht)
2.1.4 Perilymph and the Limbus Spiralis
The portion of the limbus spiralis facing the scala vestibuli was named the vasculoepithelial zone by Borghesan [9]. The zone is believed to be related to the production of perilymph constituents and is lined by osmiophilic cells [6, 10, 11]. The cells have also been shown to have Na+/K+-ATPase activity [12].
Hsu and Nomura [13] demonstrated strong carbonic anhydrase activity in the vasculoepithelial zone (Fig. 2.13). Carbonic anhydrase is an enzyme that assists the rapid conversion of carbon dioxide and water into carbonic acid, hydrogen, and bicarbonate ions.
Carbonic anhydrase activity in the limbus spiralis. The vasculoepithelial zone demonstrates strong enzyme activity. The interdental cell and its vicinity show no reaction. Guinea pig [13]
Carbonic anhydrase is an important enzyme in the regulation of pH and fluid balance in different parts of the body, including the inner ear. Light and electron microscopic studies have shown diverse distribution of the enzyme in the inner ear. The stria vascularis and dark cells have strong carbonic anhydrase activity [13]. The neuroepithelia of the crista ampullaris show strong activity in the supporting cells, but sensory cells with nerve chalices show no activity, although the reaction products are found on the stereocilia (Fig. 2.14).
Carbonic anhydrase activity in the neuroepithelia of the crista ampullaris. Supporting cells show carbonic anhydrase activity. The sensory cell and nerve chalice show no activity. The stereocilia show deposits of reaction products. Guinea pig (original ×40) [13]
The inner ear maintains its functions through the actions of various cells and of enzymes such as carbonic anhydrase, Na+/K+-ATPase, and adenyl cyclase.
2.1.5 Endolymph
Endolymph is produced mainly in the stria vascularis and dark cell areas. Electrolyte concentrations in the endolymph are quite different from those in the perilymph. In 1954, Smith et al. [14] demonstrated a high potassium ion concentration and a low sodium ion concentration in the endolymph, while the reverse was found in the perilymph.
Unlike the utricle and ampullae of the semicircular canals, the saccule has no dark cell areas. Hydrops of the saccule is often quite marked in patients with Meniere’s disease. The origin of the endolymph in these cases is probably the stria vascularis.
The membrana reticularis divides the cortilymph from the endolymph. When the cuticular plate of the outer hair cells disappears, repair of the membrana reticularis will take place simultaneously. The area of the cuticular plate is tightly enclosed by the surrounding phalanxes of Deiters’ cells and the heads of the pillar cells, so that no contamination occurs between the endolymph and the cortilymph. When the stria vascularis is damaged by laser irradiation, rapid repair takes place to maintain the scala media.
Endolymphatic hydrops is described in the chapter on Meniere’s disease.
2.2 Perilymphatic Fistula
2.2.1 Clinical Aspects
Perilymph may leak into the tympanic cavity from the inner ear in cases of temporal bone trauma, including ear surgery. However, leakage can occur without apparent cause, leading to signs and symptoms of inner ear malfunction. This condition is called spontaneous perilymphatic fistula.
Perilymphatic fistula is suggested if any of the following symptoms is evident:
-
Tinnitus, hearing loss, fullness of the ear, dizziness, and disequilibrium, occurring immediately after straining, nose blowing, or any other physical activity that causes a rapid increase of cerebrospinal fluid (CSF) pressure. The same symptoms can also occur with a rapid change of atmospheric pressure that affects the middle ear pressure.
-
Sensorineural hearing loss developing over a period of hours or a few days.
-
Tinnitus or a sensation of running water within the ear.
-
Dizziness when pressure in the external ear is artificially increased or decreased.
-
Fullness of the ear, hearing loss, tinnitus, dizziness, and disequilibrium following a popping sound.
Perilymphatic fistula can also occur without hearing loss or dizziness. A definitive diagnosis can be made by confirming perilymph leakage or fluid from the oval and/or round window at exploratory tympanotomy or endoscopic inspection. The pathophysiology of perilymphatic fistula remains unclear, mainly because of the paucity of histopathological studies of the inner ear in patients with the disorder.
With exploratory tympanotomy, the areas near the oval and round windows can be reached. Fluid may be observed oozing around the stapes footplate without an apparent slit.
Because the round window membrane is nearly parallel to the floor of the external auditory canal in most cases, it is difficult to directly observe the membrane (Fig. 2.15). Furthermore, a round window niche membrane is often observed in that area. Nomura [15] evaluated 100 temporal bones and found that only 30 lacked a recognizable membranous structure in the round window niche. Of the remaining 70, 13 had closed niches, 54 were perforated, and 3 had a reticulated structure. The closed type niche membrane may be mistaken for the round window membrane [15] (Fig. 2.16).
The round window niche membrane closes the round window niche (closed type). The niche membrane may be mistaken for the round window membrane [15]
In the same study, rupture of the oval window or round window membrane was observed when pressure was applied through the cochlear aqueduct or scala tympani of cadaver temporal bones. In the round window membrane, a slit-like fistula was observed, running parallel to the direction of the round window membrane fibers [15, 16] (Figs. 2.17 and 2.18). Round fistulae were not detected [15].
Schema of the round window membrane (cross section). The membrane consists of three layers: the outer layer, which is a continuation of the mucosa of the tympanic cavity, the middle fibrous layer, and the inner mesothelial cell layer [16]
The middle layer of the human round window membrane. Bundles of collagen fibers are seen. The fibers fan out from the crista semilunaris toward the bony edge of the round window. Scale: 3 μm (original ×4,500) [15]
In cases of confirmed perilymph leakage, diagnosis of perilymphatic fistula can be made. In cases without confirmed perilymph leakage, can perilymphatic fistula be ruled out? The answer is “No.” The signs and symptoms of the condition depend on the underlying pathology of the membranous labyrinth. Therefore, if the pathology persists after the fistula has been closed, patients may show ongoing signs of inner ear disease. The condition should be diagnosed as perilymphatic fistula even without confirmed perilymph leakage.
It has recently been reported that cochlin-tomoprotein is specifically present in the perilymph and can thus be used as a perilymph marker. Serum and CSF do not contain cochlin-tomoprotein. Perilymph is a mixture of plasma filtrated through the blood-labyrinth barrier [17], CSF, and constituents produced in the inner ear. The volume of perilymph is about 150 μL. If perilymphatic fistula occurs, the first few microliters that leak from the inner ear contain cochlin-tomoprotein. However, if leakage persists, the fluid may no longer contain the protein, or the protein concentration may be below the cut-off value of the test. In such cases, plasma filtrate and CSF leak from the inner ear.
Taking these circumstances into consideration, a diagnosis of perilymphatic fistula should be made clinically without performing exploratory tympanotomy, just as we routinely diagnose sudden deafness and Meniere’s disease. Otherwise, clinical studies of perilymphatic fistula will not be promoted.
2.2.2 Changes of CSF and Middle Ear Pressures in Daily Life
Nose blowing is a not infrequent cause of perilymphatic fistula. Because patients usually do not recognize nose blowing as the cause of the condition, it is ignored. A diagnosis of spontaneous perilymphatic fistula may be made in such patients.
Goodhill [18] proposed the explosive and implosive routes in the pathogenesis of perilymphatic fistula. In the explosive route, high CSF pressure extends to the inner ear, resulting in fistula formation in the oval and/or round window. Conversely, high pressure in the middle ear exerts concomitant pressure on one or both of the windows, producing a fistula or fistulae via the implosive route.
2.2.2.1 Changes in CSF Pressure
To examine changes in CSF pressure in daily life, Sakikawa et al. [19] performed spinal taps on 23 hospitalized patients who required CSF examination for diagnosis of their medical problems. Their clinical diagnoses were vertigo (seven patients), sudden deafness (6), facial nerve paralysis (4), perilymphatic fistula (3), and other conditions (3).
During CSF pressure recording, the patients were asked to perform the following four actions: nose blowing with one nostril closed, nose blowing with both nostrils closed, breath holding, and sniffing. The results showed that nose blowing with both nostrils closed resulted in the greatest pressure elevation of the four actions. Resting CSF pressures ranged from 60 to 170 mmH2O (mean, 112) in the 20 patients without perilymphatic fistula, and from 60 to 120 mmH2O (mean, 120) in the three perilymphatic fistula patients. The mean value of maximum CSF pressure when nose blowing with both nostrils closed was 406 mmH2O (range: 177–666) in 20 patients without fistula, while it was 523 mmH2O (range: 449–598) in the three perilymphatic fistula patients.
Patients with perilymphatic fistula showed greater pressure changes than other patients (Fig. 2.19a). In some patients, nasopharyngeal pressure was measured in addition to CSF pressure (Fig. 2.19b). The study indicated that CSF pressure rose to more than 400 mmH2O with nose blowing with both nostrils closed in 10 of 23 cases (7 of 20 non-perilymphatic fistula cases, and all perilymphatic fistula cases). Conversely, sniffing lowered CSF pressure in all cases.
(a) Changes in cerebrospinal fluid pressure (CSF-P) with nose blowing and other actions in a 75-year-old woman with perilymphatic fistula. Maximum CSF-P (mmH2O) from the top: at rest, 136; nose blowing with one nostril closed, 381; nose blowing with both nostrils closed, 598; breath holding, 503; and sniffing, 290. Black bar indicates duration of actions. (b) Changes in CSF-P and nasopharyngeal pressure (NP-P) in a 70-year-old woman with facial palsy on the left side. When she blew her nose, both the CSF-P and NP-P increased equally. In breath holding, the NP-P was unchanged, while CSF-P increased. When she sniffed, both CSF-P and NP-P decreased [19]
2.2.2.2 Changes in Middle Ear Pressure
Changes in middle ear pressure in daily life have also been examined [20]. Eighteen patients with eardrum perforation were enrolled. Changes in middle ear pressure before and during nose blowing with both nostrils closed were recorded using a pressure monitor. Effects of sniffing and Eustachian catheterization were also examined.
During nose blowing with both nostrils closed, the mean pressure change was 252 mmH2O (range: 163–340 mmH2O). In 10 of 18 patients, middle ear pressure was unchanged during sniffing. These results suggest that sniffing only slightly influences middle ear pressure in people with competent Eustachian tubes. During Eustachian catheterization, the middle ear pressure changes ranged from 408 to 1,033 mmH2O (mean, 776 mmH2O).
The study showed that changes in middle ear pressure during nose blowing with both nostrils closed were large and rapid (Fig. 2.20). The amplitude of the pressure change in the middle ear during nose blowing was 230 mmH2O.
Changes in middle ear pressure (ME-P) in a 21-year-old man with traumatic perforation. Both ME-P and nasopharyngeal pressure (NP-P) increased during nose blowing with both sides closed, but the amplitude of change of ME-P was less than half that of NP-P. The passive opening pressure of the Eustachian tube was 450 mmH2O. When sniffing, NP-P decreased, while ME-P was unchanged. When politzerization was performed, ME-P increased slightly after NP-P increased to 400 mmH2O. Black bar indicates duration of actions: from the top, nose blowing with both sides closed, sniffing, and politzerization [20]
2.2.2.3 Pressure Gradient
Nose blowing influences CSF pressure as well as middle ear pressure. The mean maximum CSF pressure during nose blowing was more than 400 mmH2O. The mean middle ear pressure during nose blowing was 252 mmH2O. Therefore, the pressure gradient across the cochlear windows is about 150 mmH2O during nose blowing. During sniffing, middle ear pressure is unchanged. These results suggest that nose blowing may be an important cause of perilymphatic fistula via the explosive route, while sniffing is not likely to cause perilymphatic fistula.
Rupture of the cochlear windows was observed when artificial perilymph was injected into the subarachnoid spaces of guinea pigs. Ten of 14 ears showed cochlear window rupture. The pressure applied was 400 mmH2O in nine of ten ears. Three animals in which no rupture occurred with pressure increases of 400 mmH2O showed rupture of the round window membrane when the middle ear pressure decreased to −1,000 mmH2O. The pressure gradient across the round window membrane is very important in the development of perilymphatic fistula [15].
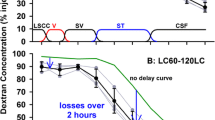
2.2.3 Experimental Perilymphatic Fistula
With Goodhill’s concept of explosive and implosive routes of fistula formation in mind, Hara et al. [21] injected artificial perilymph into the CSF of guinea pigs to produce high CSF pressure. This resulted in rupture of one or both windows on one or both sides. This method is an experimental perilymphatic fistula model of the explosive route. An alternate method of producing an explosive route model is suctioning a small amount of perilymph (4 μL) through the round window. Hara and colleagues found that these methods produce similar changes in the membranous labyrinth. The speed of injection or suction and the volume of injected artificial perilymph or suctioned perilymph are important factors affecting changes in the membranous labyrinth and should be measured. However, in the preliminary experiment, no measurements were made.
It is interesting that these procedures resulted in the formation of endolymphatic hydrops in the cochlea (Fig. 2.21). This condition appeared to be temporary and resolved by the time the fistula closed. The organ of Corti remained normal. Decreased perilymph pressure and relatively increased endolymph pressure may be responsible for the formation of hydrops. Not only bulging of Reissner’s membrane, but also bowing of the basilar membrane was observed in some animals (Fig. 2.22) [22]. The organ of Corti was compressed. The membrana reticularis showed a marked indentation between the first and second rows of the outer hair cells. The tectorial membrane was trapped and kinked. Another indentation occurred at the junction of the membrana reticularis and Hensen’s cells. The pillar cells and outer hair cells were markedly bent (Fig. 2.23) [23].
Endolymphatic hydrops produced by experimental perilymphatic fistula in a guinea pig (injection method) [21]
Indentation of the membrana reticularis with hydrops in the guinea pig. The tectorial membrane is trapped at the indentation of the membrana reticularis (arrow). The basilar membrane shows a downward bowing (apical turn: original ×6.5) [22]
Two notches (arrows) on the surface of the organ of Corti in the guinea pig. The right arrow indicates the area of the membrana reticularis between the first and second rows of outer hair cells. The tectorial membrane is trapped at the tip. The left arrow indicates the junction between the membrana reticularis and Hensen’s cells (injection method, 1 month post-injection) (original × 40) [23]
In one case, marked hydrops was found in a guinea pig two months after injection of artificial perilymph (Fig. 2.24) [24]. The scala vestibuli disappeared because of marked distension of Reissner’s membrane. The organ of Corti and stria vascularis were atrophic. A marked loss of connective tissue cells was observed in the limbus spiralis. The saccule was completely collapsed. This caused blockage of the longitudinal flow of endolymph, resulting in the formation of marked hydrops of the cochlea (Fig. 2.25).
Marked hydrops after experimental perilymphatic fistula formation in the guinea pig (injection method, 2 months post-injection). (a) The scala vestibuli is occupied by marked endolymphatic hydrops (arrows). The organ of Corti, limbus, and stria vascularis are atrophic. (b) Collapsed saccular wall covers the atrophic saccular macula [24]
Other findings observed in this series of experiments were collapse of Reissner’s membrane (Fig. 2.26a), degeneration of the organ of Corti (Fig. 2.26b) and cortilymphatic hydrops with a marked loss of the cellular elements of the organ of Corti (Figs. 2.9 and 2.27).
Marked cortilymphatic hydrops. Most of the cells within the organ of Corti have disappeared. A few Deiters’ cells and pillar cells remain in elongated shape. Marked loss of spiral ganglion cells. Massive hemorrhage remains in the scala tympani 1 month after injection (original ×16) [23]
2.2.4 Early Hearing Change with Perilymphatic Fistula
In clinical cases of perilymphatic fistula, most patients complain of ear fullness, tinnitus, hearing impairment, and hyperacusis. Pure-tone audiometry reveals every kind of hearing impairment.
Audiograms taken soon after onset show low-tone sensorineural hearing loss [25] (Fig. 2.28a). Fullness of the ear with low-tone hearing loss may lead to misdiagnosis of Eustachian tube disorder.
Hearing changes in patients with perilymphatic fistula. (a) Hearing of four patients soon after the onset of perilymphatic fistula [25]. (b) Recovery of hearing after closure of the fistula. (1) Sixteen hours after onset, (2) forty-eight hours after onset, (3) exploratory tympanotomy was performed on the fifth day. Leakage from the round window niche was confirmed. The niche was closed using a small piece of absorbable gelatin. Audiogram was taken on the 12th day after onset [26]
Recovery of acute hearing loss in a case of perilymphatic fistula is presented in Figure 2.28b. Audiogram 1 was taken 16 h after onset and audiogram 2 taken 48 h after onset. Exploratory tympanotomy was performed on the fifth day. Fluid leakage from the round window niche was confirmed. A small amount of absorbable gelatin was placed to cover the round window membrane. Audiogram 3 shows the patient’s hearing 12 days after onset. Low-tone sensorineural hearing loss and dominant negative SP in the electrocochleogram strongly suggest endolymphatic hydrops in the early stage of idiopathic perilymphatic fistula [25, 26].
2.2.5 Vestibular Changes in Experimental Perilymphatic Fistula
A characteristic finding of the vestibular labyrinth in cases of perilymphatic fistula is collapse. There is a trabecular mesh between the membranous labyrinth and surrounding bony wall in the pars superior of the inner ear (Fig. 2.29). When this mesh tears from the membranous labyrinth because of perilymph compromise, endolymph seepage occurs, resulting in collapse of the membranous labyrinth. The area and degree of collapse vary. The collapse of the pars superior can be classified as one of five types [27] (Fig. 2.30).
Schema showing several types of vestibular collapse. (a) Mild collapse of the utricle. (b) Moderately collapsed utricular wall attaching to the utricular macula. (c) Collapse of the ampulla. (d) Marked collapse of the ampulla with moderate utricular collapse. (e) Marked collapse of the utricle and ampulla [27]
When the utricular wall is slightly collapsed, the trabecular mesh in that area disappears. The utricular macula remains intact (Figs. 2.30a and 2.31). However, the collapsed wall may touch the utricular macula if the degree of collapse is severe. The collapsed wall may scrape the otolithic membrane, stimulating the sensory cells of the utricular macula (Figs. 2.30b and 2.32). As the perilymph leaks, the collapsed utricular wall may vibrate, stimulating the sensory epithelium, resulting in dizziness (floating [irritable] labyrinth) [28] (Fig. 2.33). In the clinical setting, dizziness is often resolved after closure of the fistula, probably because the vibration of the membranous labyrinth ceases. Complete collapse of the utricular wall will not induce vibration of the wall (Fig. 2.30e).
Mild collapse of the utricular wall after experimental perilymphatic fistula. The trabecular mesh disappears only in the collapsed area (arrow: original ×2.5) [28]
Utricular wall partly collapsed onto the normal neuroepithelium of the macula (original ×16) [28]
Concept of the floating (irritable) labyrinth. The collapsed utricular wall stimulates the macula, causing dizziness [28]
The semicircular ducts show various changes in cases of experimental perilymphatic fistula. Collapse of the semicircular duct is the most common finding, and is particularly severe in the posterior ampulla (Fig. 2.34a–c). Marked collapse of the ampullary wall covers the crista ampullaris (Fig. 2.35). This resembles the histopathology of vestibular atelectasis [29] (Fig. 2.36).
Separation of two layers of the ampullary wall was observed without collapse in guinea pigs immediately after injection of artificial perilymph. The mesothelial lining of the ampulla maintained its normal shape. No tear in the trabecular mesh was observed. It is interesting to observe that the top of the cupula pulled down the epithelial lining of the ampullary wall. Perhaps the endolymph within the semicircular duct was suctioned, so that the epithelial lining together with the cupula was pulled, resulting in dissociation of the ampullary wall. The tip of the cupula seemed to adhere fairly tightly to the epithelial lining of the ampullary wall (Fig. 2.37a, b).
Dissociation of ampullary wall. The epithelial cell layer is pulled from the mesothelial cell layer by the cupula. The trabecular mesh shows no change. (a) Anterior ampulla. The cochlea and saccule show mild hydrops. (original × 6.5) (b) Posterior ampulla. No change in the cochlea or other vestibular organs (immediately after injection). (original × 6.5) Guinea pigs
Caloric tests in guinea pigs with experimental perilymphatic fistulae revealed various changes: normal, no response, recovery, and caloric irregularity (Fig. 2.38). These responses may change with time. For example, no caloric response was observed 1 week after surgery in a particular animal, but it had recovered after another week [30–32] (Fig. 2.39).
Postoperative caloric test showing caloric irregularity. L Irregular waves of a longer duration are observed 1 week after surgery, R normal side, Upper trace: time base at 1 mark per second, Second trace: eye movement, Third trace: differentiated eye movements (eye velocity). Guinea pig (suction method) [22]
Canal paresis converts to normal caloric response in an electronystagmogram (ENG). The caloric test 1 week after experimental perilymphatic fistula showed canal paresis, which had normalized 1 week later. L operated side, R normal side, SPV slow-phase velocity. Calculated from ENG recordings of the original nystagmus curve. Upper trace: Time base at 1 mark per second Second trace: Eye movement Third trace: Differentiated eye movements (eye velocity). Guinea pig (suction method) [32]
Generally speaking, cochlear hydrops was observed with a normal vestibular system, although the saccule showed concomitant hydrops. Collapse of the vestibular system accompanied collapse of the scala media. However, the area and degree of collapse of the membranous vestibular labyrinth differs greatly from partial mild collapse to severe total collapse.
The experimental methods to produce perilymphatic fistulae described in this chapter are far from physiological conditions. Some of the results are difficult to understand. However, we can see mysteries hidden in the inner ear.
The variety of morphological changes observed in experimental perilymphatic fistula help us to consider the pathophysiology of inner ear disease when we see patients with the disorder. Keeping in mind the potential occurrence of the condition is of paramount importance.
References
Engström H (1960) The cortilymph, the third lymph of the inner ear. Acta Morphol Neerl Scand 3:195–204 Taylor & Francis Ltd. www.tandfonline.com
Schuknecht HF, Seifi AE (1963) Experimental observations on the fluid physiology of the inner ear. Ann Otol Rhinol Laryngol 72:687–712
Masuda Y, Sando I, Hemenway WG (1971) Perilymphatic communication routes in guinea pig cochlea. Arch Otolaryngol 94: 240–245
Nomura Y (1968) The cortilymph—in relation to perilymphatic space. Pract Oto-Rhino-Laryngol 61:469–474
Beagley HA (1965) Acoustic trauma in the guinea pig. I. Electrophysiology and histology, II. Electron microscopy including the morphology of cell junctions in the organ of Corti. Acta Otolaryngol 60:437–451
Ishiyama E, Ishiyama K (2012) Atlas of the inner ear morphology, 3rd edn. Sozo Shuppan, Tokyo
Djeric D, Schuknecht HF (1989) Hensen’s cell cyst of the organ of Corti. Acta Otolaryngol (Stockh) 108:55–61
Gopen Q, Rosowski J, Merchant SN (1997) Anatomy of the normal human cochlear aqueduct with functional implications. Hear Res 107:9–22
Borghesan E (1957) Modality of the cochlear humoral circulation. Laryngoscope 67:1266–1285
Ishiyama E, Keels EW, Weibel J (1970) New anatomical aspects of the vasculo-epithelial zone of the spiral limbus in mammals. Acta Otolaryngol (Stockh) 70:319–326
Kimura RS, Nye CL, Southard RE (1990) Normal and pathologic features of the limbus spiralis and its functional significance. Am J Otolaryngol 11:99–111
Schulte BA, Adams JC (1989) Distribution of immunoreactive Na, K-ATPase in gerbil cochlea. J Histochem Cytochem 37:127–134
Hsu CJ, Nomura Y (1985) Carbonic anhydrase activity in the inner ear. Acta Otolaryngol 418(Suppl):1–42
Smith CA, Lowry OH, Wu ML (1954) The electrolytes of the labyrinthine fluids. Laryngoscope 64:141–153
Nomura Y (1984) Otological significance of the round window. Adv Oto-Rhino-Laryngol 33:1–162
Nomura Y, Okuno T, Kawabata I (1983) The round window membrane. In: Pfaltz CR (ed) Modern perspectives in otology, vol 31. Adv Oto-Rhino-Laryngol, Karger, Basel pp 50–58
Juhn SK, Ryback LP (1981) Labyrinthine barriers and cochlear homeostasis. Acta Otolaryngol (Stockh) 91:529–534
Goodhill V (1971) Sudden deafness and round window rupture. Laryngoscope 81:1462–1474
Sakikawa Y, Kobayashi H, Nomura Y (1994) Changes in cerebrospinal fluid pressure in daily life. Ann Otol Rhinol Laryngol 103:959–963
Sakikawa Y, Kobayashi H, Nomura Y (1995) Changes in middle ear pressure in daily life. Laryngoscope 105:1353–1357
Hara M, Nomura Y, Saito K (1990) Histopathologic study of the perilymph-suctioned labyrinth. Ann Otol Rhinol Laryngol 99: 316–320
Nomura Y, Hara M, Young Y-H, Okuno T (1992) Inner ear morphology of experimental perilymphatic fistula. Am J Otolaryngol 13:32–37
Nomura Y, Hara M (1986) Experimental perilymphatic fistula. Am J Otolaryngol 7:267–275
Nomura Y, Hara M, Funai H, Okuno T (1987) Endolymphatic hydrops in perilymphatic fistula. Acta Otolaryngol (Stockh) 103:469–476
Fukaya T, Nomura Y (1988) Audiological aspects of idiopathic perilymphatic fistula. Acta Otolaryngol (Stockh) 456 (Suppl): 68–73
Fukaya T, Nomura Y (1987) Idiopathic perilymphatic fistula. Nippon Jibiinkoka Gakkai Kaiho (Tokyo) 91:233–239
Kukita N, Nomura Y (1994) Morphological changes of the vestibular labyrinth by experimental perilymph fistula. Showa Univ J Med Sci 6:97–103
Nomura Y, Okuno T, Hara M, Young Y-H (1992) “Floating” labyrinth: pathophysiology and treatment of perilymph fistula. Acta Otolaryngol (Stockh) 112:186–191
Merchant SN, Schuknecht HF (1988) Vestibular atelectasis. Ann Otol Rhinol Laryngol 97:565–576
Young Y-H, Nomura Y, Hara M (1992) Vestibular pathophysiologic changes in experimental perilymph fistula. Ann Otol Rhinol Laryngol 111:612–616
Young Y-H, Nomura Y, Hara M (1992) Caloric irregularity in experimentally induced perilymphatic fistula. Eur Arch Otorhinolaryngol 249:181–184
Young Y-H, Nomura Y (1995) Recovery of caloric function in experimental perilymph fistula. Ann Otol Rhinol Laryngol 104: 484–487
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Japan
About this chapter
Cite this chapter
Nomura, Y., Nomura, Y., Nomura, Y. (2014). Inner Ear Fluid. In: Morphological Aspects of Inner Ear Disease. Springer, Tokyo. https://doi.org/10.1007/978-4-431-54204-9_2
Download citation
DOI: https://doi.org/10.1007/978-4-431-54204-9_2
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-54203-2
Online ISBN: 978-4-431-54204-9
eBook Packages: MedicineMedicine (R0)