Abstract
Aortic aneurysm is the 13th leading cause of death in the United States. The prevalence of aortic aneurysms appears to be increasing, due in part to a higher level of awareness, advancement in imaging modalities, and an aging population. The incidence of thoracic aortic aneurysms is estimated to be around 10.4 cases per 100,000 person-years. In the future, it is likely that hybrid repair will be replaced by total endovascular techniques in most centers. Future applications may be for patients who are high risk for open TAAA repair, those who fail total endovascular repair or in centers with no access or experience with fenestrated and branched endografts. Keys for successful outcomes include patient selection, case planning, and knowledge of the technical aspects of the procedure.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Aortic aneurysm is the 13th leading cause of death in the United States [1]. The prevalence of aortic aneurysms appears to be increasing, due in part to a higher level of awareness, an advancement in imaging modalities, and an aging population [2]. The incidence of thoracic aortic aneurysms is estimated to be around 10.4 cases per 100,000 person-years [3].
Open surgical repair has been the treatment of choice for degenerative thoracic aortic aneurysms since the 1950s. Thoracic endovascular aortic repair (TEVAR) was first used in 1987 [4], and since that time, many publications have reported a lower mortality and morbidity in TEVAR compared to open repair of thoracic aortic aneurysm [5,6,7,8]. Hence, TEVAR has become the predominant method of treatment for most thoracic aortic pathologies, including aneurysms, traumatic injury, penetrating aortic ulcers, and aortic dissection.
Despite the significant advances in perioperative critical care, open surgical techniques, and endovascular therapy, there are still challenging situations in which conventional endovascular therapy is not applicable and open surgical repair carries a high perioperative risk.
In this chapter, we will discuss strategies for redo operations and hybrid procedures for descending thoracic aorta (DTA) and thoracoabdominal aortic aneurysm (TAAA).
2 Redo Strategies for DTA and TAAA Surgeries
Redo surgery for DTA and TAAA is often dreaded by surgeons due to its higher risk for morbidity and mortality compared to the primary surgery. This is due to respiratory complications and a higher risk of bleeding [9,10,11]. Multiple aortic aneurysms is not an uncommon scenario. In fact, Crawford et al. [12] reported that 59.6% of patients originally presenting with ascending, transverse arch or descending aortic aneurysms developed multiple aortic aneurysms in other segments. Other publications have reported that the most common reason for redo DTA or TAAA repair was new aneurysms or extension of disease (70–90%) [11,12,13].
3 Outcomes of Redo DTA and TAAA Surgeries
Information regarding redo surgery for DTA and TAAA is limited in the literature as few publications have reported outcomes of such complicated repairs. Earlier small series publications reported 25–28% early mortality rate [14,15,16]. More recent papers report a decrease in early mortality, 4.5–13.3% [10, 11, 17, 18].
Gloviczki and colleagues [9] reviewed the Mayo Clinic experience over two decades with 102 consecutive patients with multiple aortic aneurysms who underwent 201 aortic reconstructions. In 65 patients (63.7%), the initial operations involved the thoracic aorta; TAAA repair was performed as a subsequent procedure in 37 patients (36.3%). They found that overall operative mortality increased with the ordinal number of procedures: 4.4% for the first operation, 10.4% for the second, and 33.3% for the third.
Coselli et al. [18] reported their experience over 10 years, comparing patients who underwent TAAA repair with vs. without previous thoracic aortic aneurysm repair (PTAR). In all, 723 consecutive patients underwent TAAA repair, 179 of whom had PTAR. Although differences did not reach statistical significance, patients without PTAR tended toward increased in-hospital mortality (8.5% vs. 4.5%; p = 0.078) and postoperative paraplegia/paraparesis rates (6.5% vs. 2.8%; p = 0.069). More patients without PTAR had cardiac complications (11.3% vs. 5.6%; p = 0.028) and required chronic hemodialysis (5.9% vs. 1.1%; p = 0.009). In the PTAR, they reported pulmonary complications in 60/179 (33.5%), stroke in 5/179 (2.7%), and postoperative bleeding in 3/179 (1.6%) patients, and 37 (20.6%) underwent concurrent splenectomy. As a group, the patients with PTAR in this series were younger than those without PTAR and, consequently, had fewer comorbid factors. Rupture was also more common in the group without PTAR, likely explaining the better outcomes in the redo surgery group.
Kawaharada et al. [10] reported the experience in a single center in Japan, comparing a group of patients (70) who underwent elective TAAA repair without those with a history of previous DTA repair [30]. Major postoperative complications in the redo group included paraplegia (10%), renal failure requiring hemodialysis (20%), and respiratory failure (30%).
Etz et al. [11] reported their experience over 20 years with TAAA repair in patients with previous thoracic aneurysm repair through left thoracotomy. Between 1988 and 2007, 60 patients underwent redo thoracotomy for DTA or TAAA. Hospital mortality was 13.3%. Respiratory complications occurred in 13 patients (21.6%), 5 of whom needed tracheotomy and 1 required extracorporeal membrane oxygenation (ECMO). Permanent dialysis was required in two (3.3%), with one patient suffering from postoperative paraplegia (1.7%), and three (5%) had bleeding that required reoperation. There were no strokes [11].
4 Technical Consideration in Redo Repair of DTA and TAAA
In our institution, the redo repair is carried out in similar fashion to our standard DTA and TAAA repair [19]. After induction of anesthesia and placement of double-lumen endotracheal tube, we use cerebrospinal fluid (CSF) drainage in the majority of the cases, unless the patient is hemodynamically unstable or there is a concomitant infection. The chest is entered through a left thoracoabdominal incision (sixth intercostal space). In redo surgery, additional precautions are needed. This part of surgery could be difficult, due to extensive adhesions, and it could take a few hours until the descending aorta is dissected with adequate proximal and distal control. Therefore, we limit division of adhesions to those essential for obtaining the necessary aortic exposure for the planned repair, minimizing pulmonary trauma and bleeding.
Etz et al. have described a 2-day procedure in a few patients to allow bleeding to subside and clearance of pulmonary secretions before institution of cardiopulmonary bypass. We usually use left heart bypass for distal aortic perfusion by accessing the inferior pulmonary vein or the proximal descending aortic graft from previous surgery (Fig. 81.1). We establish the arterial inflow through an 8-mm Dacron graft (DuPont, Wilmington, DE) sutured end to side to the left common femoral artery (Fig. 81.2) or through the descending thoracic aorta if the distal anastomosis was completed first (distal-first approach) (Fig. 81.3). We use the distal-first approach in cases in which the left common femoral artery is not easily accessed for cannulation (i.e., previous aortobifemoral bypass, severely diseased vessel) [20, 21].
In redo cases due to visceral patch aneurysm (Fig. 81.4) in young patients and patients with genetic disorder (Marfan), we replace the graft with a side-branched thoracoabdominal aortic graft (STAG), which is a pre-sewn, multiple-branched woven Dacron graft that was designed by Dr. Hazim J. Safi in 1996 [22] (Fig. 81.5). For intercostal patch aneurysm, we reattach the intercostal arteries using a looped graft (Fig. 81.6).
Hypothermic circulatory arrest (HCA) can be used in cases where a placement of proximal aortic clamp is not feasible. Etz et al. reported the use of HCA in 30% of the redo repairs due to technical considerations. Lombardi and colleagues [17] utilized HCA in cases with visceral patch where they had to be converted from inclusion technique to separate bypasses to each vessel in the degenerated patch to provide additional visceral and renal protection during individual reconstruction of the visceral and renal vessels.
In the endovascular era, TEVAR is implemented in more complicated cases and with “off-label” use. This increases the risk for complications and a conversion to open repair at a later stage (Fig. 81.7) [23, 24]. Roselli et al. reported their experience from July 2001 to January 2012, with 50 patients who underwent TEVAR requiring additional open surgical repair, while HCA was required in 48%.
Redo repair of DTA and TAAA remains a challenge, with a higher risk for postoperative complications than the initial surgery. With increased expertise in endovascular surgery, more minimally invasive options, such as hybrid procedure, will likely become more appealing in treating those very complex cases.
5 Hybrid Procedures for DTA and TAAA
The conventional open repair for TAAA has evolved over the years, especially in the aspect of organ protection techniques, lowering the mortality and morbidity of this procedure in leading centers [19, 21, 22, 25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. However, it remains a great challenge for cardiothoracic and vascular surgeons, with significant rates of morbidity and mortality when performed in average centers.
Total endovascular repair of TAAA with fenestrated and branched stent graft has been described worldwide. Initial experience showed that this repair is safe and effective and reduces morbidity in patients with arch, thoracoabdominal, and pararenal aortic aneurysm [43,44,45,46,47]. The commercial devices for pararenal aortic aneurysms and TAAA extent II and III are with limited availability and still require 6–8 weeks for customization. There are “off-the-shelf” devices that allow treatment of more than 60–80% of patients with complex aneurysm. However, large series and long follow-up is lacking [48, 49]. These limitations have led a number of centers to come up with creative solutions for visceral artery bypasses using “chimney,” “sandwich,” “octopus,” and “periscope” techniques, as well as physician-modified endografts [50,51,52,53]. Those approaches are limited by “off-label” indications and a lack of long-term follow-up.
Furthermore, total endovascular repair of TAAA, specifically four visceral endovascular bypasses, requires a high degree of expertise and capabilities that only few centers possess. The search for a third alternative for treatment complex aortic aneurysms led to the development of “hybrid” repair, which includes an extra-anatomic bypass for visceral vessels (“debranching”), followed by placement of an endograft for aneurysm exclusion. The hybrid procedure includes known surgical techniques and available commercial devices. It also minimizes the surgical stress by avoiding one-lung ventilation, the need for cardiopulmonary bypass, hypothermia, and aortic cross-clamping. Therefore, in many centers, it has become the treatment of choice for patients with TAAA and who are at high risk for conventional open repair [54, 55].
6 Outcomes of Hybrid Repair of TAAA
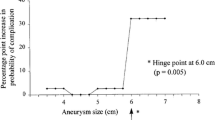
The outcomes of hybrid repair of TAAA remain with high morbidity and mortality in many centers. Oderich et al. [55] had reviewed many “single-center” experiences, with mortality ranging between 0 and 44% and morbidity between 3 and 69% [56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79]. Since this review, a few more centers have published results [54, 80,81,82]. The clinical outcomes of these published papers are summarized in Table 81.1.
There are few systematic reviews of the available literature that have been published on hybrid repair of TAAAs [83,84,85]. A recent review by Moulakakis et al. [85] included 528 patients and 14 reports published since 1999. There were 359 male (68%) and 169 female patients, with a mean age of 70.5 years. Aneurysm extent was classified as type I in 12.8%, type II in 23.2%, type III in 38%, type IV in 23.7%, and type V in 11.1%. A single-stage procedure was used in 47.5% and two-stage in 52.5%, with a mean period of 29.6 days between the two stages. Primary technical success, defined as completed visceral debranching and aneurysm exclusion by successful stent graft placement, was estimated as 95.4%. In all, 30-day or in-hospital mortality was 14.3%, and the most common causes of death were bowel ischemia, multisystem organ failure, respiratory complications, and aneurysm rupture prior to a second-stage procedure. Pooled rates of spinal cord injury were 7%, with irreversible paraplegia in 4.4%, and the pooled estimate of renal failure requiring dialysis was 7%. After a mean follow-up of 34.2 months, 21.1% of the patients had had endoleaks, and visceral graft patency was 96.5%.
The preliminary results of the North American Complex Abdominal Aortic Debranching (NACAAD) registry were presented at the 2011 Vascular Annual Meeting. Oderich et al. [55] summarized the results of this study. It included 208 patients treated for complex abdominal aortic aneurysms in 14 academic centers of North America. There were 118 male (57%) and 90 female (43%) patients with a mean age of 71 years. Aneurysm diameter averaged 6.6 ± 1.3 cm, and aneurysm extent included 163 TAAA (type I in 6%, type II in 25%, type III in 31%, and type IV) and 45 pararenal aneurysms. A single-stage debranching was performed in 92 patients (44%) and two-stage approach in 116 (56%). Arch debranching was needed in 22 patients (11%) to provide adequate proximal landing zone. The inflow for visceral reconstruction was based on the iliac arteries in 63%, aorta or aortic graft in 29%, or a hepatic/splenic artery in 8%.
Thirty-day or in-hospital mortality was 14% for all patients, 16% for TAAAs, and 9% for pararenal aneurysms. Morbidity occurred in 73% of the patients, most commonly pulmonary (22%), renal (19%), and gastrointestinal complications (14%). Spinal cord injury occurred in 21 patients (10%) and ischemic colitis in 13 (6%). After a median follow-up of 21 months, 70% of the patients had repeat aortic imaging. Endoleaks occurred in 23 patients (13%) and were classified as type I in 3%, type II in 8%, and type III in 1%. Primary visceral graft patency and freedom from reinterventions were 90 ± 2% and 85 ± 3% at 1 year, respectively.
7 Technical Considerations in Hybrid Repair of TAAA
The debranching procedure may be done through a midline incision, with transperitoneal or retroperitoneal approach. This is achieved in either a one- or two-stage fashion, with the aneurysm exclusion achieved by placement of the aortic stent graft. High-risk patients and those who have a difficult open reconstruction will benefit from the two-staged procedure. However, patients who don’t require an extensive aortic coverage might be suitable for a one-stage repair, eliminating the risk of rupture while waiting for the second stage [55]. Hughes et al. [2] published their experience in TAAA hybrid repair in 47 patients. They performed the one-stage repair in the initial 33 patients and a two-stage repair in the same hospital in the recent 14 patients. Tshomba et al. [80] described their experience with hybrid repair of TAAA in 52 high-risk patients; 37 (71.2%) had a simultaneous repair and 15 (21.8%) a staged procedures.
The source of inflow to the extra-anatomic bypass is usually retrograde, originating of the distal common iliac artery or proximal external iliac artery. Other sources have been described, such as infrarenal aorta, aortic graft in patients with previous aortic repair, and renal or splenic arteries [55]. Tshomba et al. [80] have described an antegrade bypass originating of the ascending aorta through a median sternotomy extended into median laparotomy approach in three patients.
Many graft configurations have been described in the literature. Oderich et al. [55] at the Mayo Clinic prefer to use a trifurcated graft from one of the common iliac arteries, with an added limb, depending on the patient’s anatomy. Lall et al. [1] have described using a bifurcated graft, which can be anastomosed with a short main body and graft limbs to the right renal and superior mesenteric arteries. To avoid kinks in prefashioned trifurcated grafts, separate graft limbs can be added for the celiac axis and left renal artery as needed. Hughes et al. [86] use a custom-designed, multibranched Dacron graft (Vascutek USA, Ann Arbor, Mich) with a 14-mm trunk, two 6-mm side limbs for the renal arteries, and two 8-mm side limbs for the visceral (celiac, SMA) arteries. In addition, there is a 10-mm side limb at the proximal end adjacent to the inflow anastomosis that is used as a conduit for the large sheaths during the delayed second endovascular stage.
Lachat et al. [58, 70] have described a modification of the technique, using VORTEC (Viabahn Open Rebranching TEChnique). It allows for a suture-less anastomosis using Viabahn stent grafts (W.L. Gore & Associates, Flagstaff, AZ) for the visceral bypasses.
8 Conclusion
In the future, it is likely that hybrid repair will be replaced by total endovascular techniques in most centers. Future applications may be for patients who are high risk for open TAAA repair and those who fail total endovascular repair or in centers with no access or experience with fenestrated and branched endografts. Keys for successful outcomes include patient selection, case planning, and knowledge of the technical aspects of the procedure.
References
Beckman JA. Aortic aneurysms: pathophysiology, epidemiology, and prognosis. In: Creager MA, Dzau VJ, Loscalzo J, editors. Vas Med. Philadelphia, PA: Saunders Elsevier Inc; 2006.
LaRoy LL, Cormier PJ, Matalon TA, Patel SK, Turner DA, Silver B. Imaging of abdominal aortic aneurysms. AJR Am J Roentgenol. 1989;152:785–92.
Clouse WD, Hallett JW Jr, Schaff HV, Gayari MM, Ilstrup DM, Melton LJ 3rd. Improved prognosis of thoracic aortic aneurysms: a population-based study. JAMA. 1998;280:1926–9.
Volodos NL, Karpovich IP, Shekhanin VE, Troian VI and Iakovenko LF. [A case of distant transfemoral endoprosthesis of the thoracic artery using a self-fixing synthetic prosthesis in traumatic aneurysm]. Grudn Khir 1988: 84-86.
Gopaldas RR, Huh J, Dao TK, et al. Superior nationwide outcomes of endovascular versus open repair for isolated descending thoracic aortic aneurysm in 11,669 patients. J Thorac Cardiovasc Surg. 2010;140:1001–10.
Cheng D, Martin J, Shennib H, et al. Endovascular aortic repair versus open surgical repair for descending thoracic aortic disease. a systematic review and meta-analysis of comparative studies. J Am Coll Cardiol. 2010;55:986–1001.
Hughes K, Guerrier J, Obirieze A, et al. Open versus endovascular repair of thoracic aortic aneurysms: A Nationwide Inpatient Sample Study. Vasc Endovascular Surg. 2014;
Arnaoutakis DJ, Arnaoutakis GJ, Abularrage CJ, et al. Cohort-comparison of thoracic endovascular aortic repair with open thoracic aortic repair using modern end-organ preservation strategies. Ann Vasc Surg. 2015;
Gloviczki P, Pairolero P, Welch T, et al. Multiple aortic aneurysms: the results of surgical management. J Vasc Surg. 1990;11:19–27.. discussion -8
Kawaharada N, Morishita K, Fukada J, Hachiro Y, Takahashi K, Abe T. Thoracoabdominal aortic aneurysm repair through redo leftsided thoracotomy. Ann Thorac Surg. 2004;77:1304–8.
Etz CD, Zoli S, Kari FA, et al. Redo lateral thoracotomy for reoperative descending and thoracoabdominal aortic repair: a consecutive series of 60 patients. Ann Thorac Surg. 2009;88:758–66.. discussion 67
Crawford ES, Cohen ES. Aortic aneurysm: a multifocal disease. Presidential address. Arch Surg (Chicago, IL: 1960). 1982;117:1393–400.
Carrel T, Pasic M, Jenni R, Tkebuchava T, Turina MI. Reoperations after operation on the thoracic aorta: etiology, surgical techniques, and prevention. Ann Thorac Surg. 1993;56:259–68.. discussion 69
Fox AD, Berkowitz HD. Thoracoabdominal aneurysm resection after previous infrarenal abdominal aortic aneurysmectomy. Am J Surg. 1991;162:142–4.
Curl GR, Faggioli GL, Stella A, D’Addato M, Ricotta JJ. Aneurysmal change at or above the proximal anastomosis after infrarenal aortic grafting. J Vasc Surg. 1992;16:855–9.. discussion 9-60
Edwards JM, Teefey SA, Zierler RE, Kohler TR. Intraabdominal paraanastomotic aneurysms after aortic bypass grafting. J Vasc Surg. 1992;15:344–50.. discussion 51-3
Lombardi JV, Carpenter JP, Pochettino A, Sonnad SS, Bavaria JE. Thoracoabdominal aortic aneurysm repair after prior aortic surgery. J Vasc Surg. 2003;38:1185–90.
Coselli JS, Poli de Figueiredo LF, LeMaire SA. Impact of previous thoracic aneurysm repair on thoracoabdominal aortic aneurysm management. Ann Thorac Surg. 1997;64:639–50.
Estrera AL, Sheinbaum R, Miller CC 3rd, Harrison R, Safi HJ. Neuromonitor-guided repair of thoracoabdominal aortic aneurysms. J Thorac Cardiovasc Surg. 2010;140:S131–5.. discussion S42-S46
Estrera AL, Sandhu H, Afifi RO, et al. Open repair of chronic complicated type B aortic dissection using the open distal technique. Ann Cardiothorac Surg. 2014;3:375–84.
Miller CC 3rd, Grimm JC, Estrera AL, et al. Postoperative renal function preservation with nonischemic femoral arterial cannulation for thoracoabdominal aortic repair. J Vasc Surg. 2010;51:38–42.
De Rango P, Estrera AL, Miller C 3rd, et al. Operative outcomes using a side-branched thoracoabdominal aortic graft (STAG) for thoraco-abdominal aortic repair. Eur J Vasc Endovasc Surg. 2011;41:41–7.
Chaer RA, Makaroun MS. Late failure after endovascular repair of descending thoracic aneurysms. Semin Vasc Surg. 2009;22:81–6.
Lima B, Roselli EE, Soltesz EG, et al. Modified and “reverse” frozen elephant trunk repairs for extensive disease and complications after stent grafting. Ann Thorac Surg 2012; 93: 103.-9; discussion 9.
Safi HJ, Estrera AL, Miller CC, et al. Evolution of risk for neurologic deficit after descending and thoracoabdominal aortic repair. Ann Thorac Surg 2005; 80: 2173.-9; discussion 9.
Coselli JS, Bozinovski J and LeMaire SA. Open surgical repair of 2286 thoracoabdominal aortic aneurysms. Ann Thorac Surg 2007; 83: S862.-4; discussion S90-2.
Safi HJ, Winnerkvist A, Miller CC 3rd, et al. Effect of extended cross-clamp time during thoracoabdominal aortic aneurysm repair. Ann Thorac Surg. 1998;66:1204–9.
Engle J, Safi HJ, Miller CC 3rd, et al. The impact of diaphragm management on prolonged ventilator support after thoracoabdominal aortic repair. J Vasc Surg. 1999;29:150–6.
Safi HJ, Miller CC 3rd. Spinal cord protection in descending thoracic and thoracoabdominal aortic repair. Ann Thorac Surg. 1999;67:1937–9.. discussion 53-8
Safi HJ, Subramaniam MH, Miller CC, et al. Progress in the management of type I thoracoabdominal and descending thoracic aortic aneurysms. Ann Vasc Surg. 1999;13:457–62.
Azizzadeh A, Huynh TT, Miller CC 3rd, et al. Postoperative risk factors for delayed neurologic deficit after thoracic and thoracoabdominal aortic aneurysm repair: a case-control study. J Vasc Surg. 2003;37:750–4.
Estrera AL, Miller CC, 3rd, Huynh TT, et al. Preoperative and operative predictors of delayed neurologic deficit following repair of thoracoabdominal aortic aneurysm. J Thorac Cardiovasc Surg 2003; 126: 1288-1294.
Safi HJ, Miller CC, 3rd, Huynh TT, et al. Distal aortic perfusion and cerebrospinal fluid drainage for thoracoabdominal and descending thoracic aortic repair: ten years of organ protection. Ann Surg 2003; 238: 372-80; discussion 80-1.
Hassoun HT, Miller CC, 3rd, Huynh TT, Estrera AL, Smith JJ and Safi HJ. Cold visceral perfusion improves early survival in patients with acute renal failure after thoracoabdominal aortic aneurysm repair. J Vasc Surg 2004; 39: 506-512.
Huynh TT, Miller CC, 3rd, Estrera AL, et al. Correlations of cerebrospinal fluid pressure with hemodynamic parameters during thoracoabdominal aortic aneurysm repair. Ann Vasc Surg 2005; 19: 619-624.
Huynh TT, van Eps RG, Miller CC 3rd, et al. Glomerular filtration rate is superior to serum creatinine for prediction of mortality after thoracoabdominal aortic surgery. J Vasc Surg. 2005;42:206–12.
Achouh PE, Madsen K, Miller CC 3rd, et al. Gastrointestinal complications after descending thoracic and thoracoabdominal aortic repairs: a 14-year experience. J Vasc Surg. 2006;44:442–6.
Estrera AL, Miller CC, Azizzadeh A and Safi HJ. Adjuncts during surgery of the thoracoabdominal aorta and their impact on neurologic outcome: distal aortic perfusion and cerebrospinal fluid drainage. Multimed Man Cardiothorac Surg 2006; 2006: mmcts 2006 001933.
Achouh PE, Estrera AL, Miller CC 3rd, et al. Role of somatosensory evoked potentials in predicting outcome during thoracoabdominal aortic repair. Ann Thorac Surg. 2007;84:782–7.. discussion 7-8
Winnerkvist A, Anderson RE, Hansson LO, et al. Multilevel somatosensory evoked potentials and cerebrospinal proteins: indicators of spinal cord injury in thoracoabdominal aortic aneurysm surgery. Eur J Cardiothorac Surg. 2007;31:637–42.
Miller CC 3rd, Villa MA, Achouh P, et al. Intraoperative skeletal muscle ischemia contributes to risk of renal dysfunction following thoracoabdominal aortic repair. Eur J Cardiothorac Surg. 2008;33:691–4.
Keyhani K, Miller CC, 3rd, Estrera AL, Wegryn T, Sheinbaum R and Safi HJ. Analysis of motor and somatosensory evoked potentials during thoracic and thoracoabdominal aortic aneurysm repair. J Vasc Surg 2009; 49: 36-41.
Roselli EE, Greenberg RK, Pfaff K, Francis C, Svensson LG, Lytle BW. Endovascular treatment of thoracoabdominal aortic aneurysms. J Thorac Cardiovasc Surg. 2007;133:1474–82.
Verhoeven EL, Katsargyris A, Bekkema F, et al. Editor’s Choice—Ten-year experience with endovascular repair of thoracoabdominal aortic aneurysms: results from 166 consecutive patients. Eur J Cardiothorac Surg. 2015;49:524–31.
Greenberg RK, Lu Q, Roselli EE, et al. Contemporary analysis of descending thoracic and thoracoabdominal aneurysm repair: a comparison of endovascular and open techniques. Circulation. 2008;118:808–17.
Greenberg R, Eagleton M, Mastracci T. Branched endografts for thoracoabdominal aneurysms. J Thorac Cardiovasc Surg. 2010;140:S171–8.
Haulon S, D’Elia P, O’Brien N, et al. Endovascular repair of thoracoabdominal aortic aneurysms. Eur J Cardiothorac Surg. 2010;39:171–8.
Sweet MP, Hiramoto JS, Park KH, Reilly LM, Chuter TA. A standardized multi-branched thoracoabdominal stent-graft for endovascular aneurysm repair. J Endovasc Ther. 2009;16:359–64.
Rodd CD, Desigan S, Cheshire NJ, Jenkins MP, Hamady M. The suitability of thoraco-abdominal aortic aneurysms for branched or fenestrated stent grafts--and the development of a new scoring method to aid case assessment. Eur J Cardiothorac Surg. 2011;41:175–85.
Lachat M, Veith FJ, Pfammatter T, et al. Chimney and periscope grafts observed over 2 years after their use to revascularize 169 renovisceral branches in 77 patients with complex aortic aneurysms. J Endovasc Ther. 2013;20:597–605.
Schwierz E, Kolvenbach RR, Yoshida R, Yoshida W, Alpaslan A, Karmeli R. Experience with the sandwich technique in endovascular thoracoabdominal aortic aneurysm repair. J Vasc Surg. 2014;59:1562–9.
Kolvenbach R. The role of periscopes and chimneys in complex aneurysm cases. J Endovasc Ther. 2011;18:661–5.
Oderich GS, Ricotta JJ 2nd. Modified fenestrated stent grafts: device design, modifications, implantation, and current applications. Perspect Vasc Surg Endovasc Ther. 2009;21:157–67.
Hughes GC, Andersen ND, Hanna JM, McCann RL. Thoracoabdominal aortic aneurysm: hybrid repair outcomes. Ann Cardiothorac Surg. 2012;1:311–9.
Oderich GS, Mendes BC, Gloviczki P, Kalra M, Duncan AA, Bower TC. Current role and future directions of hybrid repair of thoracoabdominal aortic aneurysms. Perspect Vasc Surg Endovasc Ther. 2012;24:14–22.
Quinones-Baldrich WJ, Panetta TF, Vescera CL, Kashyap VS. Repair of type IV thoracoabdominal aneurysm with a combined endovascular and surgical approach. J Vasc Surg. 1999;30:555–60.
Drinkwater SL, Goebells A, Haydar A, et al. The incidence of spinal cord ischaemia following thoracic and thoracoabdominal aortic endovascular intervention. Eur J Vasc Endovasc Surg. 2010;40:729–35.
Lachat M, Mayer D, Criado FJ, et al. New technique to facilitate renal revascularization with use of telescoping self-expanding stent grafts: VORTEC. Vascular. 2008;16:69–72.
Fulton JJ, Farber MA, Marston WA, Mendes R, Mauro MA, Keagy BA. Endovascular stent-graft repair of pararenal and type IV thoracoabdominal aortic aneurysms with adjunctive visceral reconstruction. J Vasc Surg. 2005;41:191–8.
Resch TA, Greenberg RK, Lyden SP, et al. Combined staged procedures for the treatment of thoracoabdominal aneurysms. J Endovasc Ther. 2006;13:481–9.
Black SA, Wolfe JH, Clark M, Hamady M, Cheshire NJ, Jenkins MP. Complex thoracoabdominal aortic aneurysms: endovascular exclusion with visceral revascularization. J Vasc Surg. 2006;43:1081–9.. discussion 9
Donas KP, Schulte S, Krause E, Horsch S. Combined endovascular stent-graft repair and adjunctive visceral vessel reconstruction for complex thoracoabdominal aortic aneurysms. Int Angiol. 2007;26:213–8.
Lee WA, Brown MP, Martin TD, Seeger JM, Huber TS. Early results after staged hybrid repair of thoracoabdominal aortic aneurysms. J Amer Coll Surg. 2007;205:420–31.
Gawenda M, Aleksic M, Heckenkamp J, Reichert V, Gossmann A, Brunkwall J. Hybrid-procedures for the treatment of thoracoabdominal aortic aneurysms and dissections. Eur J Vasc Endovasc Surg. 2007;33:71–7.
Ballard JL, Razavi M, Harward TR, Flanigan DP. Visceral/renal artery debranching for complex thoracoabdominal hybrid procedures via retroperitoneal abdominal aortic exposure: a preliminary report. Ann Vasc Surg. 2008;22:173–8.
van de Mortel RH, Vahl AC, Balm R, et al. Collective experience with hybrid procedures for suprarenal and thoracoabdominal aneurysms. Vascular. 2008;16:140–6.
Quinones-Baldrich W, Jimenez JC, DeRubertis B, Moore WS. Combined endovascular and surgical approach (CESA) to thoracoabdominal aortic pathology: A 10-year experience. J Vasc Surg. 2009;49:1125–34.
Biasi L, Ali T, Loosemore T, Morgan R, Loftus I, Thompson M. Hybrid repair of complex thoracoabdominal aortic aneurysms using applied endovascular strategies combined with visceral and renal revascularization. J Thorac Cardiovasc Surg. 2009;138:1331–8.
Da Rocha MF, Miranda S, Adriani D, Urgnani F, Riambau VA, Mulet J. Hybrid procedures for complex aortic pathology: initial experience at a single center. Rev Esp Cardiol. 2009;62:896–902.
Donas KP, Lachat M, Rancic Z, et al. Early and midterm outcome of a novel technique to simplify the hybrid procedures in the treatment of thoracoabdominal and pararenal aortic aneurysms. J Vasc Surg. 2009;50:1280–4.
Drinkwater SL, Bockler D, Eckstein H, et al. The visceral hybrid repair of thoraco-abdominal aortic aneurysms—a collaborative approach. Eur J Vasc Endovasc Surg. 2009;38:578–85.
Kabbani LS, Criado E, Upchurch GR Jr, et al. Hybrid repair of aortic aneurysms involving the visceral and renal vessels. Ann Vasc Surg. 2010;24:219–24.
Patel HJ, Upchurch GR Jr, Eliason JL, et al. Hybrid debranching with endovascular repair for thoracoabdominal aneurysms: a comparison with open repair. Ann Thorac Surg. 2010;89:1475–81.
Kuratani T, Kato M, Shirakawa Y, Shimamura K, Sawa Y. Long-term results of hybrid endovascular repair for thoraco-abdominal aortic aneurysms. Eur J Cardiothorac Surg. 2010;38:299–304.
Chiesa R, Tshomba Y, Marone EM, et al. Hybrid procedures for the treatment of thoracoabdominal aortic aneurysms and dissections. J Cardiovasc Surg (Torino). 2010;51:821–32.
Smith TA, Gatens S, Andres M, Modrall JG, Clagett GP, Arko FR. Hybrid repair of thoracoabdominal aortic aneurysms involving the visceral vessels: comparative analysis between number of vessels reconstructed, conduit, and gender. Ann Vasc Surg. 2011;25:64–70.
Lin PH, Kougias P, Bechara CF, et al. Clinical outcome of staged versus combined treatment approach of hybrid repair of thoracoabdominal aortic aneurysm with visceral vessel debranching and aortic endograft exclusion. Perspect Vasc Surgery Endovasc Ther. 2012;24:5–13.
Patel R, Conrad MF, Paruchuri V, Kwolek CJ, Chung TK, Cambria RP. Thoracoabdominal aneurysm repair: hybrid versus open repair. J Vasc Surg. 2009;50:15–22.
Chiesa R, Tshomba Y, Melissano G, et al. Hybrid approach to thoracoabdominal aortic aneurysms in patients with prior aortic surgery. J Vasc Surg. 2007;45:1128–35.
Tshomba Y, Melissano G, Logaldo D, et al. Clinical outcomes of hybrid repair for thoracoabdominal aortic aneurysms. Ann Cardiothorac Surg. 2012;1:293–303.
Hurie J, Patel HJ, Criado E, Eliason JL, Deeb GM, Upchurch GR Jr. Postoperative fluid collection after hybrid debranching and endovascular repair of thoracoabdominal aortic aneurysms. J Vasc Surg. 2011;54:1623–8.
Ham SW, Chong T, Moos J, et al. Arch and visceral/renal debranching combined with endovascular repair for thoracic and thoracoabdominal aortic aneurysms. J Vasc Surg. 2011;54:30–40.. discussion -1
Bakoyiannis C, Kalles V, Economopoulos K, Georgopoulos S, Tsigris C, Papalambros E. Hybrid procedures in the treatment of thoracoabdominal aortic aneurysms: a systematic review. J Endovasc Ther. 2009;16:443–50.
Moulakakis KG, Mylonas SN, Avgerinos ED, Kakisis JD, Brunkwall J, Liapis CD. Hybrid open endovascular technique for aortic thoracoabdominal pathologies. Circulation. 2011;124:2670–80.
Moulakakis KG, Mylonas SN, CN A, Liapis CD. Combined open and endovascular treatment of thoracoabdominal aortic pathologies: a systematic review and meta-analysis. Ann Cardiothorac Surg. 2012;1:267–76.
Hughes GC, Barfield ME, Shah AA, et al. Staged total abdominal debranching and thoracic endovascular aortic repair for thoracoabdominal aneurysm. J Vasc Surg. 2012;56:621–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer-Verlag GmbH Austria, part of Springer Nature
About this chapter
Cite this chapter
Afifi, R.O., Safi, H.J., Estrera, A.L. (2019). Hybrid and Redo Strategies for Descending and Thoracoabdominal Aorta. In: Stanger, O., Pepper, J., Svensson, L. (eds) Surgical Management of Aortic Pathology. Springer, Vienna. https://doi.org/10.1007/978-3-7091-4874-7_81
Download citation
DOI: https://doi.org/10.1007/978-3-7091-4874-7_81
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-4872-3
Online ISBN: 978-3-7091-4874-7
eBook Packages: MedicineMedicine (R0)