Abstract
Sarcocystis and pentastomes infections are uncommon zoonoses of worldwide distribution. In most of the cases, they were detected as an incidental finding at autopsy or necropsy. Recently, serious attention has been given to Sarcocystis when large human outbreaks have been reported in Malaysia. Similarly, the detection of a recent human pentastomiasis case in East Malaysia since nearly four decades ago has alerted that pentastomes should not be ignored by the medical and laboratory personnel. In addition, understanding the routes of infection is crucial in preventing further cases. This chapter will focus on sarcocystosis and pentastomiasis cases among humans and animals.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Intermediate Host
- Definitive Host
- Water Buffalo
- Southeast Asian Country
- Indirect Fluorescent Antibody Test
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
9.1 Sarcocystis
9.1.1 Introduction
Sarcocystis spp. are intracellular protozoa belonging to the family Sarcocystidae. The protozoan was first detected in striated muscles of a house mouse as white threadlike cysts by Miescher in 1843 [1]. It was initially referred as Miescher’s tubules for more than 50 years until the name Sarcocystis meisheriana was suggested for similar structures found in swine muscle [2]. Sarcocystis spp. are the etiological agents of sarcocystosis, an uncommon zoonosis of worldwide distribution. Majority of the human and animal cases were reported from Southeast Asian countries particularly Malaysia and Thailand [3, 4]. The life cycle of Sarcocystis is complex, involving asexual and sexual reproduction in intermediate (e.g. herbivores) and definitive (e.g. carnivores and omnivores) hosts respectively. Currently more than 130 Sarcocystis spp. have been identified from a variety of hosts including swine, birds, snake, rats, cattle, goats and monkeys. Interestingly humans may serve as both the definitive and intermediate (dead end) hosts [1]. Infection by Sarcocystis may cause be either a self-limiting intestinal infection or prolonged muscular infection in humans and animals [3, 5]. In most of the reported cases, sarcocystosis was detected as an incidental finding at autopsy or necropsy [6, 7].
9.1.2 Morphology
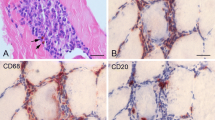
In general, there are three important Sarcocystis stages, namely the oocyst, sporocyst and sarcocyst. The oocysts are about 12–15 μm by 19–20 μm in size, containing a pair of sporocysts which are enclosed by a thin wall. Each of the sporocyst measures approximately 10 by 15 μm and contains four sporozoites and a granular residual body [1]. Both oocysts and sporocysts can be detected in the faeces of infected hosts but the oocysts are less commonly seen as their wall is very fragile and easily ruptured [1]. Sporocysts excreted from different hosts are usually morphologically indistinguishable [1]. Sarcocysts are usually found in striated muscles of the body including the tongue, oesophagus, diaphragm and cardiac muscle [8, 9]. They are spindle in shape with either a thin or thick wall surrounding them. The size of sarcocysts may vary depending on their age and range approximately 140–250 μm by 50–66 μm [8] (Fig. 9.1). Numerous infectious crescent-shaped bodies termed as bradyzoites are contained in each of the sarcocyst [8].
A thick wall sarcocyst with numerous bradyzoites stained with haematoxylin and eosin (×1,000) (adapted from [8] with permission from IeJSME)
9.1.3 Life Cycle
The life cycle of Sarcocystis is based on a prey–predator (intermediate–definitive) host relationship [1]. Asexual reproduction occurs in an intermediate host (e.g. cattle, pigs and goats) following ingestion of oocysts or free sporocysts from food or water contaminated with faeces from the infected definitive host (e.g. monkeys, baboons, dogs and reticulated pythons). In the small intestine, sporozoites are released from the sporocysts and migrate through the gut epithelium to the small arteries throughout the body. The first asexual generation begins at these sites, generating a large number of merozoites. Subsequent generations of merozoites develop in the direction of blood flow to arterioles, capillaries, venules and veins throughout the body and terminate with the formation of sarcocysts in muscles [10]. The sarcocysts would remain non-infectious for at least 2 months until the bradyzoites within the sarcocysts have matured and appeared as crescent shaped [1, 3].
Sexual reproduction occurs when meat containing sarcocysts from an infected intermediate host is eaten by a susceptible definitive host. In the intestine, the sarcocysts are ruptured, releasing the infectious bradyzoites. Male and female gametes are subsequently developed from each bradyzoite and fertilisation occurs. This results in the production of oocysts which are then being excreted in the faeces of the definitive host. Humans can become both the intermediate and definitive hosts. However, humans are usually the accidental intermediate hosts as we are unlikely to be eaten by other definitive hosts [1].
9.1.4 Disease Manifestations and Sarcocystis Cases in Southeast Asia
Infection in humans can result in intestinal and muscular sarcocystosis [1, 5]. Intestinal sarcocystosis can be acquired following consumption of raw or undercooked meat containing mature sarcocysts. The infection is usually self-limiting with symptoms such as nausea, loss of appetite, vomiting, stomach ache and diarrhoea. On the other hand, muscular sarcocystosis can be acquired from ingestion of water or food that has been contaminated with faeces from infected definitive hosts. Individuals with muscular sarcocystosis usually suffer from musculoskeletal pain, fever, rash and subcutaneous swelling, and these symptoms may last from months to years [5].
Muscular sarcocystosis in humans is rare and mostly reported from Southeast Asian countries particularly Malaysia [3, 11]. In Malaysia, the first human muscular sarcocystosis cases were reported in 1975 following incidental findings of sarcocysts in a laryngeal biopsy of a patient with hoarseness and an oropharyngeal biopsy of an Orang Asli girl [6, 12]. Subsequent human cases have been reported by Pathmanathan and colleagues in females and males from different ethnic groups (e.g. Malays, Indians, Chinese and Orang Asli) by examinations of autopsy or biopsy samples [3, 13]. Interestingly, more than 50 % of the infected individuals were associated with malignancies [13]. In a seroprevalence study done in 1978, almost 20 % of 243 individuals from Peninsular Malaysia were positive for Sarcocystis antibodies [14]. Prevalence of Sarcocystis infection was highest in the Orang Asli population followed by Malays, Indians and Chinese [14]. It is to be noted that Orang Asli are aboriginal peoples of Peninsular Malaysia and constitute almost 0.5 % of Malaysia’s total population [66]. Most of them live in poverty with poor environmental conditions and they hunt wild boar, deer and lizard for meat sources [67]. Hence, they are at a higher risk of getting the infection via consumption of water or food contaminated with sporocysts or eating raw meat of infected definitive hosts. In a separate prevalence study, Wong and Pathmanathan reported the detection of sarcocysts in 21 out of 100 tongues (21 %) collected during autopsies of individuals aged 16–57 years old [9].
In Malaysia, the first large outbreak was published in 1999 involving 7 of 15 US soldiers who had illness 1–3 weeks after returning from field operations in a remote area in 1993 [5]. All but one of them showed symptoms including fever, myalgias, bronchospasm, subcutaneous nodules, eosinophilia and elevated levels of muscle enzymes. Sarcocysts were also detected in muscle biopsies of one of the soldiers [5]. Albendazole was given to this index case patient to reduce the chronic sarcocystosis symptoms [5]. Subsequently a decade later, another 100 suspected muscular sarcocystosis cases were recognised in travellers returning from vacation in Tioman Island, East Coast of Peninsular Malaysia during the summer months of 2011 and 2012. Thirty-five cases were initially identified in travellers from Europe (i.e. Germany, France, Netherlands, Switzerland, Belgium and Spain) and Asia (i.e. Singapore); all had prolonged fever and muscle pain. Another 65 cases were recognised about 6–8 months later with two being asymptomatic [15, 16]. It is presumed that there may be more unreported cases from the outbreak especially from those individuals without any apparent symptoms. In 2012, there was also an unpublished outbreak in an island situated at the north-west of Peninsular Malaysia. In this outbreak, more than 90 suspected muscular sarcocystosis were identified, and sarcocysts were detected in muscle biopsies of three of the infected individuals (personal communication with Prof. Rohela Mahmud, Head of Parasitology Department, University of Malaya, Malaysia). It has been suggested that human muscular cases in Malaysia could be due to ingestion of food or water contaminated with sporocysts excreted from definitive hosts such as dogs, cats or pythons [3].
Besides muscular infection in humans, Sarcocystis sarcocysts have also been detected in muscle tissues of wild and domestic animals in Malaysia including rodents [8, 17–19], zoo animals [7], water buffaloes [20, 21], cattle [21], ovine [22], slow lories [23] and monkeys [24, 25]. Most of the infected animals were asymptomatic but pathological changes including haemorrhage and oedema of organs and muscle atrophy have been observed at necropsy [7]. Ambu and colleagues have reported the presence of sarcocysts in 73 out of 146 wild and peri-urban rodents collected in Peninsular Malaysia [8]. The number of sarcocysts detected per histological section varied from 1 to 136 and none could be seen by gross examination [8]. In another study involving 40 dead animals, sarcocysts were detected in three captive mammals and five birds of two zoos in Peninsular Malaysia [7]. Sarcocysts were detected mainly in the skeletal muscles (50 %) followed by the tongue and heart (37.5 %), diaphragm (25 %) and oesophagus (12.5 %) [7]. Thus far, no human intestinal sarcocystosis have been identified or published in Malaysia [3]. However, it is believed that most of the cases might be missed or misdiagnosed rather than absent as human intestinal infection is usually self-limiting and its clinical symptoms may mimic those of other diseases [1, 26].
In Thailand, consumption of raw infected beef and pork has been identified as the main sources of human intestinal sarcocystosis [4, 27]. This is supported by the detection of bradyzoites in 100 % of 300 swine cardiac muscle specimens collected from three markets in Samut Prakan Province [28]. Besides swine, Sarcocystis sarcocysts have also been identified in sections of tongues and muscles from a variety of other animals including cattle and water buffaloes [27]. In a prevalence study among 362 asymptomatic Thai labourers who were going abroad for work, 83.3 % were positive for Sarcocystis by stool examinations and most of them were from the northeastern Thailand [29]. It has been reported that Thai labourers particularly those from the northeastern are at higher risk of being infected with Sarcocystis due to their habit of eating raw or undercooked pork and poor hygiene practices [28, 29]. Recently, the first large prevalence study of human intestinal sarcocystosis was performed among 15,555 Thais, and sporocysts were detected in stool samples of 233 individuals [4]. Intestinal sarcocystosis have also been reported in 1.65 % of primary school children in Chiang Mai and 45 % of enterocolitis patients in Thailand [30, 31]. To date, only limited data is available regarding human muscular sarcocystosis in Thailand. In the late 1970s, a single study has reported the detection of sarcocysts in skeletal, laryngeal and cardiac muscle biopsies from 15 autopsy cases. Since then, no reports on human muscular sarcocystosis were published until 2011, when a single positive case was identified during histopathological review of 1,063 laryngeal biopsies obtained from 2000 to 2009 [32]. The Sarcocystis-positive biopsy belonged to a 66-year-old man who presented with voice hoarseness for 6 months. The patient was initially diagnosed with laryngeal carcinoma and underwent partial laryngectomy. Nonkeratinising squamous cell carcinoma with Sarcocystis sarcocysts were detected in his laryngeal biopsy. The patient was not given any antiprotozoal treatment, but he did not show any signs of recurrence during a 3-year follow-up [32].
In Singapore, there is a single species of Sarcocystis named after the country (i.e. S. singaporensis) following the detection of Sarcocystis from naturally infected pythons (Python reticulatus). As the life cycle of this species involves alternating sexual and asexual cycles in pythons and rodents, respectively, S. singaporensis has been currently used as an agent for biological control of rodents in agricultural habitats of Southeast Asia [33, 34]. Basically, rodents are artificially infected using pelleted bait containing high dosage of S. singaporensis sporocysts and a mixture of wheat flour, broken corn, oil and fish or coconut extracts as rodents attractants. Following consumption of the pelleted bait, the infected rodents will suffer from pneumonia and eventually die when infection with sporocysts exceeds a certain threshold [33, 34]. To date, at least three human muscular Sarcocystis cases have been reported in Singapore [11, 16].
In Indonesia, a Sarcocystis species named S. sulawesiensis has been detected in skeletal muscles of seven rodents from three different species (i.e. Bunomyschrysocomus, Bunomysfratrorum and Paruromys dominator) [35]. Sarcocystis sulawesiensis has thin-walled sarcocysts and their primary walls exhibit many hair-like structures [35]. What was unique about this species was it can only be detected in rodents collected in North Sulawesi but not in West Java, thus suggesting its limited geographical distribution [35]. In the same study, S. singaporensis was also detected in 13 rodents of six different species [35].
In the Philippines, many of the Sarcocystis cases were reported in animals. As early as 1916, Sarcocystis was first identified in meat of a water buffalo in the Luzon island [36]. In a separate study, sarcocysts have been identified in muscle tissues of 92 out of 142 (~65 %) water buffaloes. Some of the sarcocysts, identified as S. fusiformis, could be detected by gross examination and appeared as milk-white spindle-shaped structures in between of muscles [37]. Sarcocystis spp. have also been reported in beef sold in Manila [38], muscle tissues of Rattus spp. [39] and livestock animals including hogs, goats and chicken [40–42].
Thus far, only a single report is available on human intestinal sarcocystosis in Vietnam [68]. The study was not performed in Vietnam but Central Slovakia among 1,228 Vietnamese trainees who came to work in that republic in 1987–1989. Sporocysts were detected in 14 of the Vietnamese trainees but none of them reported any signs of gastrointestinal infection [68]. In Vietnam, muscular sarcocystosis was commonly reported in livestock animals particularly water buffaloes [43]. By using molecular approaches (i.e. PCR and DNA sequencing), S. fusiformis, S. cruzi, S. hominis and S. hirsuta were able to be identified in meat samples of water buffaloes slaughtered in the Son La Province [43]. In Ho Chi Minh, Vietnam, sarcocysts were detected in 396 out of 502 adult water buffaloes by gross and histological examinations. Higher sarcocystosis prevalence was reported among older water buffaloes (6–7 years old; 93 %) compared to the young animals (2–3 years old; 57 %) [44]. In addition, higher prevalence was also shown among water buffaloes originating from the northern part (89 %) than those from the southern part (69 %) of Vietnam [44].
To date, limited information is available on Sarcocystis infection in other Southeast Asia countries such as Myanmar and Laos. In Myanmar, a Sarcocystis infection has been diagnosed in a kitten with symptoms of depression and lethargy. Sarcocystis stages including the merozoites were found in the spinal cord of the kitten at necropsy [45]. In Lao PDR, the prevalence of human intestinal sarcocystosis among 1,008 individuals screened for intestinal parasites was approximately 10 % in group of individuals aged 20 years and above. Currently, there is no report on the presence of Sarcocystis spp. or human/animal sarcocystosis cases in Brunei Darussalam, Cambodia and Timor-Leste.
9.1.5 Diagnosis
Intestinal sarcocystosis should be suspected if individuals have a history of recent consumption of any raw or undercooked meat and exhibit symptoms such as nausea, stomach ache, vomiting and diarrhoea. Definitive diagnosis is usually based on the presence of oocysts or sporocysts in stool samples. For this, stool samples are initially concentrated by a floatation technique using combinations of high-density solutions (e.g. sodium chloride, cesium chloride, sucrose and Percoll) prior to viewing under a microscope. However, stool examination does not allow identification to species level due to morphological similarity of sporocysts of different Sarcocystis species [1].
For muscular sarcocystosis, the final diagnosis is usually made by microscopic detection of sarcocysts in muscle biopsies (e.g. tongue, oesophagus, diaphragm, heart and skeletal muscles) [44]. In most of the human cases, Sarcocystis was detected as incidental findings at autopsy [6, 9]. Tissue sections is commonly stained to facilitate visualisation and to differentiate Sarcocystis from other protozoa which have similar morphological structures [32, 46]. For example, periodic acid Schiff (PAS) can be used to differentiate bradyzoites of Sarcocystis (PAS negative) from those of Toxoplasma gondii (PAS positive except the nucleus) [32]. For ultrastructural studies of Sarcocystis sarcocysts and species identification, transmission electron microscope is regularly used [35]. In some Sarcocystis species, the sarcocysts are large in size and therefore can be detected by gross examination of the infected meat. In addition, the presence of infectious bradyzoites from sarcocysts can be microscopically examined from pellet of meat that has been ground, digested with chemicals (e.g. pepsin and hydrochloric acid) and centrifuged. Serological methods such as enzyme-linked immunosorbent assays and indirect fluorescent antibody test have also been used to determine Sarcocystis infection in humans and animals [5, 14, 47, 48]. Recently, polymerase chain reaction assays targeting the 18S rDNA gene and sequencing have been utilised for species identification [43, 49, 50]. In addition, the DNA sequences obtained can also be used for phylogenetic analysis and to determine the possible definitive hosts for the Sarcocystis species detected [51].
9.1.6 Conclusion
Sarcocystis was first discovered 170 years ago. However, less attention has been given to this protozoan until recently when large human outbreaks have been reported in Malaysia. Human sarcocystosis can be acquired following the consumption of raw or undercooked meat containing sarcocysts or ingestion of food or water contaminated with faeces from infected definitive hosts. Sarcocystosis may be undetected in asymptomatic cases, or in symptomatic cases, it may be misdiagnosed with other infections. Early identification of the infection is possible if clinicians and medical laboratory personnel are aware with its clinical symptoms, routes of infection, morphology of the organism and the use of suitable samples and diagnostic tools. As sarcocystosis is a zoonotic infection, screening of all pets, livestock animals and meat at abattoirs should be regularly performed. Prevention can also be done by adequate cooking of meat, freezing meat at −4 and −20 °C for 48 and 24 h, respectively, and boiling of water prior to use. In addition, adequate sanitation is important to avoid contamination of the environment and infection to susceptible intermediate hosts. For communities (e.g. aborigines) who have low hygiene practices and individuals who are going to Southeast Asian countries for vacation, public education should be given to increase their awareness on Sarcocystis infection.
9.2 Pentastomes
9.2.1 Introduction
Pentastomes are arthropods, considered to be related to crustaceans [52]. They are commonly known as tongue worms and are adapted for an endoparasite existence in the respiratory tract, especially the lungs of a variety of animals including amphisbaena serpents, lizards, crocodiles, birds, mammals and turtles. Adult Linguatula serrata inhabits the nasal passages of mammals. Pentastomes are blood feeders and several species have been seen in the nymphal stage in humans in several countries. Immature pentastomes have been reported from frogs, fishes, serpents, mammals and insects [53]. Pentastomes are included in two orders, namely the Cephalobaenida and the Porocephalida. The more evolved is the order Porocephalida which contains species of medical importance such as L. serrate, Armillifer armillatus, Armillifer grandis, Armillifer moniliformis, Armillifer agkistrodontis, Leiperia cincinnalis and Porocephalus crotali [54, 55]. The Cephalobaenida is a more primitive group and one of its genera, Raillietiella, is common in lizards and serpents in Malaysia [53], and one species Raillietiella hemidactyli has been reported in humans in Indochina. Dollfus and Canet [56] have documented cases of subcutaneous parasitism with this parasite. This resulted from the swallowing of small, live geckos as a folk remedy for conditions such as asthma and emphysema. In the Porocephalida where the life cycles are known, vertebrates are utilised both as definitive and intermediate hosts [57]. In the Cephalobaenida, Raillietiella spp. from house geckos, domiciliary cockroaches (Periplaneta americana, Periplaneta australasiae, Neostylopyga rhombifolia and Supella longipalpa) act as intermediate hosts [58, 59].
9.2.2 Morphology
In Malaysia, nymphal Armillifer moniliformis have been reported from humans. This is the only pentastome reported in humans from Malaysia [64]. Adult P. moniliformis is an elongated parasite. The parasite possesses a cephalothorax with two pairs of hooks situated lateral to the oral cadre and a cylindrical vermiform body with annular thickening. The anterior end is broad and wedge shaped. The posterior end tapers into a blunt-pointed cone. The annuli are characteristically thick and ring shaped. Nymphs from humans measure 10 mm in length and have 30 annuli while those from animals measure 15–20 mm in length and 1.5–1.6 mm in width and have 31–34 annuli. Males measure 24–30 mm in length and 2 mm in width and have 29–35 annuli. Females measure 60–72 mm in length and 3 mm in width and have 30–34 annuli [53].
9.2.3 Human Cases in Malaysia
Man is a dead-end host and acquires the condition through ingestion of contaminated water or vegetables eaten raw or by eating infected serpent poorly cleaned and cooked. Most of the cases reported throughout the world have been discovered at surgery and autopsy.
Prathap et al. [60, 61] found a 45.5 % incidence in a series of 30 consecutive autopsies on unclaimed bodies of Malaysian aborigines while a case each in a Dayak boy and a European woman was reported by Rail [62]. Subsequently, Ong [63] reported a case of pentastomiasis of the fallopian tube in an aborigine. After nearly a lapse of 40 years, a third case was reported in a 70-year-old aborigine farmer from rural Malaysian Borneo [64].
9.2.4 General Considerations
Although asymptomatic, symptomatic cases have been reported; serious illness that includes pneumonitis, peritonitis, meningitis, pericarditis, intestinal obstruction, nephritis and obstructive jaundice has been ascribed to heavy pentastome infection [53]. Adult A. moniliformis in Malaysia have been seen in pythons, Python reticulatus and Python curtus. The nymphs have been seen encapsulated in the liver, the liver mesenteries and omentum of a variety of vertebrates, including lower primates, Insectivora, carnivores, Rodentia and Artiodactyla [53]. Adults have also been collected from Python molurus in India and Python sebae in West Africa [65]. No cases are known to have been reported from other SEA countries except Malaysia.
9.2.5 Conclusion
Given that the nymphs of the parasite are very common in rodents and other mammals, the uncommon occurrence of human cases is fortuitous. However, extreme care should be exercised by those dealing with snakes. They should wash their hands properly after handling snakes. Those who consume python flesh should cook it properly.
References
R. Fayer, Sarcocystis spp. in human infections. Clin. Microbiol. Rev. 17(4), 894–902 (2004), table of contents
J.P. Dubey et al., Sarcocystis of Animals and Man (CRC, Boca Raton, FL, 1989)
S.P. Kan, R. Pathmanathan, Review of sarcocystosis in Malaysia. Southeast Asian J. Trop. Med. Public Health 22(Suppl), 129–134 (1991)
S. Nichpanit et al., First large scale of human Sarcocystis hominis in Thailand. Trends Res. Sci. Technol. 2(1), 1–5 (2010)
M.K. Arness et al., An outbreak of acute eosinophilic myositis attributed to human Sarcocystis parasitism. Am. J. Trop. Med. Hyg. 61(4), 548–553 (1999)
M.K. Kutty et al., Sarcocystis infection in an Orang Asli: the second human case from Malaysia. Southeast Asian J. Trop. Med. Public Health 6(3), 400–401 (1975)
B. Latif et al., Sarcocystosis among wild captive and zoo animals in Malaysia. Korean J. Parasitol. 48(3), 213–217 (2010)
S. Ambu et al., Prevalence of Sarcocystis spp. in rodents in Peninsular Malaysia. IeJSME 5(2), 29–38 (2011)
K.T. Wong, R. Pathmanathan, High prevalence of human skeletal muscle sarcocystosis in south-east Asia. Trans. R. Soc. Trop. Med. Hyg. 86(6), 631–632 (1992)
D.S. Lindsay et al., Sarcocystis spp. and Sarcocystosis. BAM 5(3), 249–254 (1995)
P.C. Beaver et al., Sarcocystis in man: a review and report of five cases. Am. J. Trop. Med. Hyg. 28(5), 819–844 (1979)
M.K. Kutty, A.S. Dissanaike, A case of human Sarcocystis infection in west Malaysia. Trans. R. Soc. Trop. Med. Hyg. 69(5–6), 503–504 (1975)
R. Pathmanathan, S.P. Kan, Three cases of human Sarcocystis infection with a review of human muscular sarcocystosis in Malaysia. Trop. Geogr. Med. 44(1–2), 102–108 (1992)
V. Thomas, A.S. Dissanaike, Antibodies to Sarcocystis in Malaysians. Trans. R. Soc. Trop. Med. Hyg. 72(3), 303–306 (1978)
CDC, Notes from the field: acute muscular Sarcocystosis among returning travelers Tioman Island, Malaysia, 2011. MMWR Morb. Mortal. Wkly Rep. 61(02), 37–38 (2012)
D.H. Esposito et al., Ongoing outbreak of an acute muscular Sarcocystis-like illness among travellers returning from Tioman Island, Malaysia, 2011-2012. Euro Surveill. 17(45), pii: 20310 (2012)
S.P. Kan, Ultrastructure of the cyst wall of Sarcocystis spp. from some rodents in Malaysia. Int. J. Parasitol. 9(5), 475–480 (1979)
S.P. Kan, A.S. Dissanaike, Ultrastructure of Sarcocystis sp. from the Malaysian house rat, Rattus rattus diardii. Z. Parasitenkd. 52(3), 219–227 (1977)
V. Zaman, F.C. Colley, Light and electron microscopic observations of the life cycle of Sarcocystis orientalis sp. n. in the rat (Rattus norvegicus) and the Malaysian reticulated python (Python reticulatus). Z. Parasitenkd. 47(3), 169–185 (1975)
A.S. Dissanaike et al., Demonstration of the sexual phases of Sarcocystis fusiformis (Railliet, 1897) and Sarcocystis sp. of the water buffalo (Bubalus bubalis) in the small intestines of cats and dogs. Trans. R. Soc. Trop. Med. Hyg. 71(3), 271 (1977)
B. Latif et al., Sarcocystosis among cattle and buffaloes in Selangor-Malaysia, in 49th Annual Conference of the Malaysian Society of Parasitology and Tropical Medicine (MSPTM), Kuala Lumpur, 19–20 Mar 2013, p. 23
O. Norlida et al., A histopathological appraisal of ovine Sarcocystosis in Kelantan. J. Adv. Biomed. Pathobiol. Res. 2(4), 137–142 (2012)
V. Zaman, Sarcocystis sp. in the slow loris, Nycticebus coucang. Trans. R. Soc. Trop. Med. Hyg. 64(1), 195–196 (1970)
S.P. Kan et al., Light and electron microstructure of a Sarcocystis sp. from the Malaysian long-tailed monkey, Macaca fascicularis. Am. J. Trop. Med. Hyg. 28(4), 634–642 (1979)
K. Prathap, Letter: Sarcocystis in the Malaysian long-tailed monkey, Macaca irus. Trans. R. Soc. Trop. Med. Hyg. 67(4), 615 (1973)
G. Juckett, R. Trivedi, Evaluation of chronic diarrhea. Am. Fam. Physician 84(10), 1119–1126 (2011)
S. Bunyaratvej et al., The Sarcocystis-cyst containing beef and pork as the sources of natural intestinal sarcocystosis in Thai people. J. Med. Assoc. Thai. 90(10), 2128–2135 (2007)
S. Nateeworanart et al., Prevalence of Sarcocystis spp in cardiac muscle of swine in Samut Prakan Province, Thailand. J. Southeast Asian Educ. 35(1), 82–83 (2004)
P. Wilairatana et al., Intestinal sarcocystosis in Thai laborers. Southeast Asian J. Trop. Med. Public Health 27(1), 43–46 (1996)
S. Bunyaratvej, P. Unpunyo, Combined Sarcocystis and gram-positive bacterial infections. A possible cause of segmental enterocolitis in Thailand. J. Med. Assoc. Thai. 75(Suppl 1), 38–44 (1992)
Y. Muangyimpong et al., Prevalence of Sarcocystis infection in primary school children in Changwat Chiang Mai, Northern Thailand. J. Trop. Med. Parasitol. 16(1), 22–24 (1993)
N. Larbcharoensub et al., Laryngeal sarcocystosis accompanying laryngeal squamous cell carcinoma: case report and literature review. Southeast Asian J. Trop. Med. Public Health 42(5), 1072–1076 (2011)
T. Jakel, Biological rodent control – TJ Homepage (2006), http://www.thomas-jaekel.homepage.t-online.de/brc/cycle.htm. Accessed 2/8/2013
T. Jakel et al., Biological control of rodents using Sarcocystis singaporensis. Int. J. Parasitol. 29(8), 1321–1330 (1999)
P.J. O’Donoghue et al., Ultrastructure of Sarcocystis spp. (Protozoa: Apicomplexa) in rodents from North Sulawesi and West Java, Indonesia. J. Wildl. Dis. 23(2), 225–232 (1987)
P.V. Arambulo et al., Sarcosporidiosis in Philippine buffaloes. Philipp. J. Vet. Med. 11, 53–59 (1972)
F.G. Claveria, M.J. Cruz, Sarcocystis levinei infection in Philippine water buffaloes (Bubalus bubalis). Parasitol. Int. 48(3), 243–247 (2000)
M. Tongson, M. Pelagio, A study on the incidence of Sarcocystis (SIC) trophozoites in ground meat sold as beef in Metro Manila. Philipp. J. Vet. Anim. Sci. 4, 253–269 (1978)
F.G. Claveria et al., Parasite biodiversity in Rattus spp caught in wet markets. Southeast Asian J. Trop. Med. Public Health 36(Suppl 4), 146–148 (2005)
F.G. Claveria, Survey of Sarcocystis spp. infection in Philippine livestock animals: light microscopic and ultrastructural studies. Research@DLSU-Manila: Continuing the Cycle, p. 100 (2007)
F.G. Claveria et al., Sarcocystis miescheriana infection in domestic pigs (Sus scrofa) in the Philippines. J. Parasitol. 87(4), 938–939 (2001)
F.G. Claveria et al., Sarcocystis capracanis infection in Philippine domestic goats (Capra hircus): ultrastructural studies. Philipp. J. Sci. 133(1), 33–37 (2004)
C. Jehle et al., Diagnosis of Sarcocystis spp. in cattle (Bos taurus) and water buffalo (Bubalus bubalis) in Northern Vietnam. Vet. Parasitol. 166(3–4), 314–320 (2009)
L.T. Huong, Prevalence of Sarcocystis spp. in water buffaloes in Vietnam. Vet. Parasitol. 86(1), 33–39 (1999)
D.D. Bowman et al., Feline Clinical Parasitology (Iowa State University Press, Ames, IA, 2002)
A.M. Baticados, W.N. Baticados, Histopathology of protozoal infection in animals: a retrospective study at the University of Philippines College of Veterinary Medicine (1972-2010). Vet. Ital. 48(1), 99–107 (2012)
Y.S. Habeeb et al., Serological diagnosis of extraintestinal Sarcocystosis. J. Egypt. Soc. Parasitol. 26(2), 393–400 (1996)
G. Savini et al., Sensitivities and specificities of two ELISA tests for detecting infection with Sarcocystis in cattle of Western Australia. Prev. Vet. Med. 32(1–2), 35–40 (1997)
Z.Q. Yang et al., Identification of Sarcocystis hominis-like (Protozoa: Sarcocystidae) cyst in water buffalo (Bubalus bubalis) based on 18S rRNA gene sequences. J. Parasitol. 87(4), 934–937 (2001)
Z.Q. Yang et al., Analysis of the 18S rRNA genes of Sarcocystis species suggests that the morphologically similar organisms from cattle and water buffalo should be considered the same species. Mol. Biochem. Parasitol. 115(2), 283–288 (2001)
M. Tian et al., Phylogenetic analysis of Sarcocystis nesbitti (Coccidia: Sarcocystidae) suggests a snake as its probable definitive host. Vet. Parasitol. 183(3–4), 373–376 (2012)
J. Riley et al., The phylogenetic relationships of the Pentastomida: the case for their inclusion within the crustacean. Int. J. Parasitol. 8, 245–254 (1978)
M. Krishnasamy et al., Some pentastomes from Malaysia, with special emphasis on those from Peninsular Malaysia. J. Malays. Soc. Health 5, 49–56 (1985)
J.T. Self et al., Pentastomes in Africa. Trop. Geogr. Med. 27, 1–13 (1975)
M.H. Yao et al., Human pentastomiasis in China: case report and literature review. J. Parasitol. 94, 1295–1298 (2008)
R.P. Dollfus, J. Canet, Sur en Pentastomide Raillietiella hemidactyli suppose susceptible de parasiter l’homme consecutivement a l’ingestion de lezards vivants. Bull. Soc. Pathol. Exot. 47, 401–407 (1954)
J.H. Ali, J. Riley, Experimental life-cycle studies of Raillietiella gehyrae Bovien, 1927 and Raillietiella frenatus Ali, Riley and Self. 1981: pentastomid parasites of geckos utilizing insects as intermediate hosts. Parasitology 86, 147–160 (1983)
J. Jeffery et al., Observation on the cockroach intermediate hosts and species and species of house gecko raillietiellid in peninsular Malaysia. J. Malays. Soc. Health 12, 57–65 (1994)
C. Rajamanickam, M.M.J. Lavoipierre, Periplaneta australasiae in an intermediate host of the pentastomid Raillietiella hemidactyli. Med. J. Malaya 20, 171 (1965)
K. Prathap et al., Pentastomiasis: a common finding at autopsy among Malaysian aborigines. Am. J. Trop. Med. Hyg. 18, 20–27 (1969)
J. Prathap et al., Hepatic and pulmonary porocephaliasis in Malaysian Orang Asli (Aborigine). Med. J. Malaya 23, 92–95 (1968)
G. Rail, Porocephaliasis: a description of two cases in Sabah. Trans. R. Soc. Trop. Med. Hyg. 61, 715–717 (1967)
H.C. Ong, An unusual case of pentastomiasis of the fallopian tube in an Aborigine woman. J. Trop. Med. Hyg. 77(8), 187–189 (1974)
B. Latif et al., Case report: human pentastomiasis caused by Armillifer moniliformis in Malaysian Borneo. Am. J. Trop. Med. Hyg. 85(5), 878 (2011)
J. Riley, J.T. Self, Some observation on the taxonomy and systematics of the pentastomid genus Armillifer (Sambos, 1922) in South East Asian and Australian snakes. Syst. Parasitol. 2, 171–179 (1981)
K. Wessendorf, The Indigenous World 2009 (IWGIA, Copenhagen, 2009)
K. Haemamalar Jr. et al., Nutritional status of orang asli (che wong tribe) adults in krau wildlife reserve, pahang. Malays. J. Nutr. 16(1), 55–68 (2010). Epub 2010/04/01
S. Straka et al., Sarcocystis species in Vietnamese workers. Ceskoslovenska epidemiologie, mikrobiologie, imunologie 40(4–5), 204–8 (1991). Epub 1991/11/01. Sarcocystis species u vietnamskych praktikantov
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Wien
About this chapter
Cite this chapter
Jeffery, J., Ahmad, A.F., Abdul-Aziz, N.M. (2013). Sarcocystis spp. and Pentastomes in Southeast Asia. In: Lim, Y., Vythilingam, I. (eds) Parasites and their vectors. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1553-4_9
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1553-4_9
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1552-7
Online ISBN: 978-3-7091-1553-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)