Abstract
The availability of advanced computer-aided robotized devices for the Gamma Knife (i.e., an automatic positioning system and PerfeXion) resulted in significant changes in radiosurgical treatment strategy. The possibility of applying irradiation precisely and the significantly improved software for treatment planning led to the development of the original concept of robotic Gamma Knife microradiosurgery, which is comprised of the following: (1) precise irradiation of the lesion with regard to conformity and selectivity; (2) intentional avoidance of excessive irradiation of functionally important anatomical structures, particularly cranial nerves, located both within the target and in its vicinity; (3) delivery of sufficient radiation energy to the tumor with a goal of shrinking it while keeping the dose at the margins low enough to prevent complications. Realization of such treatment principles requires detailed evaluation of the microanatomy of the target area, which is achieved with an advanced neuroimaging protocol. From 2003, we applied the described microradiosurgical concept in our clinic for patients with benign skull base tumors. Overall, 75 % of neoplasms demonstrated shrinkage, and 47 % showed ≥50 % and more volume reduction. Treatment-related complications were encountered in only 6 % of patients and were mainly related to transient cranial nerve palsy. Just 2 % of neoplasms showed regrowth after irradiation. In conclusion, applying the microradiosurgical principles based on advanced neuroimaging and highly precise treatment planning is beneficial for patients, providing a high rate of tumor shrinkage and a low morbidity rate.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
- Automatic positioning system
- Gamma Knife PerfeXion
- Gamma Knife radiosurgery
- Microradiosurgery
- Robotics
- Skull base tumor
Introduction
The concept of stereotactic radiosurgery as precise delivery of a single-fraction high-dose radiation to an imaging-defined target was originally developed by Professor Lars Leksell from Karolinska University in Stockholm, Sweden. In 1951, he performed the first radiosurgical procedure to treat a patient with trigeminal neuralgia. The technique involved focusing multiple beams of ionizing radiation in such a way that they collided at the same point in the three-dimensional (3D) space. Each beam contained a dose low enough to avoid altering normal brain, but at the point of intersection of all of the beams a destructive dose of radiation was delivered. Initially X-rays were used, but later they were replaced by radioactive cobalt emitting a form of high-energy radiation called gamma rays. Therefore, the new technique was designated Gamma Knife stereotactic radiosurgery (GKS).
At present, GKS is an approved and widely accepted management option for a variety of intracranial tumors, vascular malformations, and functional brain disorders. Around 50,000 patients undergo treatment each year worldwide, and the number is growing. Contemporary technological achievements have resulted in profoundly improved safety and clinical applicability of radiosurgery and currently permit administration of treatment with microsurgical precision and even better. Moreover, at the beginning of the new millennium, advanced computer-aided robotized devices were introduced into clinical practice, including an automatic positioning system (APS) and later the newest model of the Gamma Knife designated PerfeXion (Elekta Instruments AB, Stockholm, Sweden) (Fig. 1).
Advantages of the Modern Computer-Aided Robotized Devices for Gamma Knife Radiosurgery
The APS is a robotized computer-controlled device for automatic positional changes of the patient’s head fixed in a Leksell G stereotactic frame during radiosurgery using Gamma Knife model C or 4C (Elekta Instruments AB). The device provides extremely high mechanical precision, within 0.1 mm in any coordinate direction. The initial evaluation of the system after its introduction into clinical practice showed beneficial effects regarding the treatment time and significantly improved options for multi-isocenter radiosurgery with application of small collimators, which resulted in a prominent increase in the precision of GKS [20, 21, 26, 27, 36, 42]. Particularly, in cases of vestibular schwannomas, application of APS resulted in increased conformity and selectivity indices from 95 to 97 % and from 78 to 84 %, respectively [36], whereas in a cohort of cavernous sinus tumors utilization of the device led to a significant reduction of the radiation dose delivered to the optic chiasm [27]. It became possible to create radiosurgical treatment plans with more homogeneous high-dose distribution and avoid underdosed areas within the lesion [21]. Finally, there was a significant decrease of extracranial irradiation, which is important in patients with benign lesions and long life expectancy [26]. Among the limitations of APS is that technically it cannot be used in some cases, particularly for peripherally located intracranial lesions [26, 36, 42].
All of the above-mentioned treatment advantages associated with application of APS are augmented with the use of PerfeXion [29, 37, 46]. This fully robotized model of the Leksell Gamma Knife has several unique features that make it fundamentally different from its predecessors. First, it has an integrated permanent collimator system that incorporates openings for collimators of three diameters (4, 8, and 16 mm), which are separated into eight independently movable sectors around the circumference of the device. During treatment, the collimator size of each sector can be individually chosen or blocked off. The device allows generation of a single isocenter composed of different beam diameters (called a composite or hybrid shot) with optimized shape. This feature significantly increases conformity and selectivity of radiation delivery and is especially effective for complex targets located in the vicinity of critical anatomical structures [29, 46]. The improved dose homogeneity and greater precision of GKS permits its application to intracranial lesions of larger volume than traditionally considered suitable for such treatment. Additionally, modification of dose distribution is possible with “dynamic shaping.” It requires only delineation of the critical structure or area and its definition as a “risk volume” with resultant automatic blocking of the beams that pass through it [29, 46]. Second, improved dosimetry usually permits the treatment to be done as a single run [37]. This advantage, along with the ability to block all the beams during fast transition of coordinates from one isocenter to another, eliminates the need to remove the patient from the machine during GKS, which in turn results in relatively increased effective (beam on) treatment time, shortens the total treatment time, and reduces the extralesional (particularly extracranial) irradiation doses [29, 37]. Third, the coach itself represents the positioning system, which provides not only <0.05 mm mechanical accuracy but also greater comfort for the patient because no movements of the head are necessary during irradiation [37]. Fourth, the significantly increased volume of the radiation cavity and the change of its shape from hemispheric to cylindrical practically eliminates the possibility of collisions. It also has an important implication on the management of multiple brain metastases and avoids staged treatment with reapplication of the stereotactic frame even for patients with lesions located in the opposite intracranial areas [29, 37]. Moreover, at least theoretically, PerfeXion provides an opportunity to apply GKS to previously nonaccessible lesions of the external skull base, maxillofacial region, and cervical spine [29, 37]. Finally, full automatization and robotization of the device greatly alleviates the workload of the staff because establishing the gamma angle (70º, 90º, or 110º) remains the only manipulation that is set up manually [29]. It also results in significantly increased safety of the treatment because it eliminates the risk of human error during adjustment of the isocenter position [37]. The operator does not have a choice of switching to manual mode or blocking of the individual beams to protect distant structures (e.g., the lens) and these points represent potential disadvantages of the device. However, they are of limited if any clinical significance [29, 37]. It should be emphasized that despite technological complexity the technical failures during use of PerfeXion are exceptionally rare [29, 37, 46].
Availability of the described computer-aided robotizeddevices for GKS led to significant changes in the radiosurgical treatment strategy. The possibility of applying highly conformal and selective irradiation and the significantly improved software for treatment planning and dosimetry (Leksell GammaPlan; Elekta Instruments AB) permitted for us to create the concept of robotic Gamma Knife microradiosurgery [7, 40]. It was originally developed and then applied in practice after installation of the Leksell Gamma Knife model 4C with APS in our clinic (December 2002).
Concept of Robotic Gamma Knife Microradiosurgery
The concept of microradiosurgical treatment is based on three main principles: (1) precise irradiation of the lesion with regard to conformity and selectivity; (2) intentional avoidance of excessive irradiation of functionally important anatomical structures, particularly cranial nerves, located both within the target and in its vicinity; (3) delivery of sufficient radiation energy to the tumor with the goal of shrinking it while keeping the dose at the margins low enough to prevent complications. Realization of such treatment principles requires detailed evaluation of the microanatomy of the target area, which is performed using the advanced neuroimaging protocol.
Advanced Neuroimaging Protocol
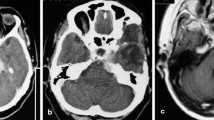
The original neuroimaging protocol for robotic Gamma Knife microradiosurgery requires access to high-resolution thin-sliced plain constructive interference in steady state (CISS) images, gadolinium-enhanced CISS images, and gadolinium-enhanced axial modified time-of-flight (TOF) images obtained with a 1.5 T clinical magnetic resonance imaging (MRI) scanner [11, 13, 19]. Usually for MRI examinations of benign skull base tumors, a single dose (0.1 mmol/kg) of the gadolinium-based contrast medium gadoteridol (ProHance®; Eisai, Tokyo, Japan) is administered intravenously. Additionally, thin-sliced plain, “bone window,” and contrast-enhanced axial computed tomography (CT) scans are obtained. The recognizable advantages of the CT scans include a low risk of image distortion artifacts and clear visualization of the osseous structures, which can be important during radiosurgery of skull base lesions [24, 35]. In some cases, metabolic information obtained with positron emission tomography (PET) or multivoxel proton magnetic resonance spectroscopy (1H-MRS) is used for radiosurgical treatment planning and can be particularly helpful during repeat GKS of recurrent tumors [24, 28].
Detailed Evaluation of the Target Neuroanatomy
All neuroimaging data are exported via the Intranet to Leksell GammaPlan (current version 8.3). This advanced software dedicated to planning the GKS and dosimetry provides an opportunity for highly accurate and precise co-registration and fusion of the various images obtained with different modalities and their magnification and reconstruction. It also allows for the surgeon to delineate various intracranial structures and to perform their evaluation from different angles and directions using 3D visualization [24].
After constructing the original workspace, the local neuroanatomy is assessed in detail. Identification of the cranial nerves either in the vicinity of the lesion or within its mass is especially emphasized. Plain CISS images permit clear visualization of the anatomical structures located intradurally or within the subarachnoid cisterns. Moreover, separate components of some cranial nerves can be differentiated from each other even with 1.5 T MR scanners. In the same time gadolinium-enhanced CISS images make the tumor “lucid” or half-tone but do not affect signal intensity of the adjacent cranial nerves. Therefore, the cranial nerves can be clearly delineated in the vicinity of the lesion (Figs. 2 and 3). Gadolinium-enhanced TOF proved helpful for 3D evaluation of the interrelations between the neoplasm and adjacent vessels. Fused “bone window” CT and MRI permit simultaneous visualization of soft tissue and bone structures [24, 35].
Gadolinium-enhanced multiplanar reconstructed (MPR) magnetic resonance (MR) images (upper row) and constructive interference in steady state (CISS) MR images (lower row) of a left cavernous sinus meningioma. Note the greater resolution of the CISS images, which permits detailed evaluation of the local neuranatomy
CISS images of a craniopharyngioma. Plain image (left) provides clear differentiation of the tumor border and subarachnoid cisterns, whereas administration of gadolinium (right) makes the tumor half-tone and facilitates determination of its border along adjacent cerebral structures, including visual pathways (from Yomo et al. [45])
Even with the advanced neuroimaging protocol and evaluation of images within the Leksell GammaPlan, delineation of the cranial nerves in the vicinity of large neoplasms is sometimes impossible. In such cases, identifying the tumor’s origin may allow the surgeon to presume the direction of its growth and the corresponding shift of adjacent anatomical structures. Therefore, their expected location can be predicted rather precisely and taken into consideration during radiosurgical treatment planning.
Principles of Microradiosurgical Treatment Planning
Microradiosurgical treatment planning is performed by referring to simultaneous onscreen displays of all obtained images in the 3D workspace of the Leksell GammaPlan. The dose plan is created with the use of multiple small isocenters, which are carefully positioned within the border of the mass with the goal of attaining its conformal and selective coverage with the prescribed isodose (Fig. 4). For GKS of benign skull base tumors, we usually try to attain a conformity index (CI) > 0.95 and a selectivity index (SI) > 0.90 [3, 46]. Although it requires a significant number of shots, it should not be an obstacle for treatment using robotized computer-aided devices such as APS or PerfeXion. Special emphasis is placed on avoiding projection of any isocenter on functionally important anatomical structures located nearby, particularly the cranial nerves. If the cranial nerves cannot be visualized, excessive irradiation of areas where they would presumably be located are intentionally avoided. It is easily done as Leksell GammaPlan allows adjustment of the isocenters’ coordinates with 0.1 mm precision.
Schematic (upper) and actual (lower) treatment planning for a Koos grade III right-sided vestibular schwannoma according to the concept of robotic Gamma Knife microradiosurgery. Note the use of multiple small isocenters, providing conformal and selective coverage of the lesion with a 50 % prescription isodose line, limited irradiation of the anterior border of the tumor for preventing facial nerve injury, and avoidance of extending the 80 % isodose area to the intracanalicular part of the neoplasm
Usually, a 50 % prescription isodose is applied to the border of the neoplasm. For benign skull base lesions, the dose at the margins varies from 10 to 14 Gy, depending on the lesion volume and location. In the vast majority of cases it constitutes 11–12 Gy. An exception to this guideline is hormone-secreting pituitary adenomas, which require larger irradiation doses to inhibit excessive hormone production. In such cases, a dose at the margins of, at least, ≥20 Gy seems necessary.
Specific Technique Directed at Tumor Shrinkage
The traditional goal of radiosurgery for intracranial tumors is growth control. However, reduction of the mass volume seems important for restoring the affected neuronal functions, particularly those related to direct compression of the cranial nerves. In fact, in one-third to two-thirds of cases, GKS results in shrinkage of benign skull base neoplasms (meningiomas, schwannomas, pituitary adenomas). Our experience demonstrated that reduction of the lesion volume after radiosurgery is directly associated with the amount of delivered radiation energy. Its variations may correspond to differences in the treatment effects despite the use of similar doses at the tumor margins [10, 16, 18]. This is in concordance with the experimental results of Massager et al. [30], which clearly showed that the presence of a “hot spot” within the target volume is likely to lead to the desired radiobiological result of GKS. It seemingly does not increase the risk of complications unless the radiosurgical treatment planning was insufficiently selective and the high-dose radiation extended to the adjacent normal tissue [2]. Therefore, in each case we try to attain a homogeneous dose distribution with creation of a wide 80 % prescription isodose area within the tumor while keeping a sufficiently low dose at the margins, which usually corresponds to a 50 % isodose. For skull base meningiomas, the suspected area of tumor origin on the dura mater is included in the high-dose irradiation area for possible obliteration of the feeding vessels [16].
To evaluate the high-dose area within the target, the homogeneity index (HI) is calculated as:
where TVpiv80 % and TV piv50 % correspond to target volumes covered by 80 % and 50 % prescription isodoses, respectively. During GKS of benign skull base tumors, we try to keep the HI at least at the level of 0.5. If the volume or distribution of the high-dose irradiation area in the target is considered insufficient, it can be optimized by adding additional small, low-weight isocenter(s). An original parameter, designated the unit energy (UE), reflects the average amount of radiation energy delivered to a unit of the tumor volume (mJ/cm3). The radiosurgical plan corresponding to current treatment standards and safety requirements, but providing the greatest possible UE, seems preferable because it provides greater probability of tumor shrinkage [10, 16, 18].
Safety Considerations
Low-dose GKS for skull base tumors provides optimal balance between good growth control and low risk of treatment-related morbidity, even for neoplasms of prominent size [4, 5, 23]. Additionally, use of multi-isocenter treatment with application of small isocenters provides a steep dose falloff outside the treated volume [21, 26, 29]. Even in relatively large skull base neoplasms, the described technique allows a gradient index far below 3, which is usually recommended for safe radiosurgical practice [3, 32].
To avoid complications, the maximum doses to specific functionally important structures should be kept within the safety range (Table 1). Particularly, excessive irradiation of the cranial nerves should be avoided. Although it is widely accepted that oculomotor, trochlear, and abducent nerves may safely tolerate doses up to 40 Gy [41], we prefer to keep their irradiation as low as possible. Therefore, if they are located within the target, which is not uncommon with cavernous sinus tumors, the treatment plan is preferably created in such a way that cranial nerves remain not covered by the high-dose irradiation area within a mass. A similar technique is used to protect the trigeminal nerve in the case of petroclival and Meckel’s cave neoplasms.
Additionally, the intratumoral 80 % prescription isodose area should not extend to the parts of the lesion located in strictly confined areas (e.g., internal acoustic canal, superior orbital fissure) to avoid possible compression of the adjacent cranial nerves during the period of temporary enlargement of the neoplasm after irradiation. The latter is a well-described phenomenon after GKS of vestibular schwannomas. It has also been demonstrated with nonvestibular schwannomas [15] and pituitary adenomas [33]. It usually appears 6–9 months after irradiation and does not require treatment unless symptomatic.
In more than half of the patients with cranial nerve dysfunction after GKS, the neuropathy is caused not by irradiation of the nerves themselves but by its effects on the the brain stem, which is usually associated with edema [1, 5]. This point strongly supports the need for precise dose planning and prevention of the inadvertent excessive irradiation of the functionally important brain structures. Higher selectivity of GKS with more rapid falloff of the dose outside the target is associated with less risk of adverse reactions in adjacent tissues [20, 23, 31].
Evaluation and Correction of Distortion Artifacts on MR Images
Targeting accuracy has a significant effect on the outcome of GKS. Although in general MRI allows detailed characterization of the intracranial lesion and allows creation of a precise radiosurgical treatment plan, mislocalization errors caused by distortion of the images during their acquisition and/or stereotactic transformation are possible [20]. Fusion with “bone window” CT allows 3D evaluation and correction of distortion artifacts on MRI scans, which is particularly important for GKS in the vicinity of functionally important anatomical structures [16, 35–37]. For this purpose, after completing the treatment planning and calculating the radiosurgical parameters (CI, SI, HI, UE), several anatomical landmarks in the vicinity of the target are defined and their position on MRI compared to that on CT is checked in the axial, sagittal, and coronal planes. If a difference is identified, it is considered the result of MRI distortion artifacts. Therefore, coordinates of all isocenters are shifted in a measured distance along the X, Y, or Z axes to compensate for mislocalization error.
Clinical Results
During the last decade the described microradiosurgical treatment strategy was consistently applied in our clinic for GKS of benign skull base tumors. Among cases with at least 2 years of follow-up after treatment, 75 % of neoplasms demonstrated shrinkage, and in 47 % of lesions ≥50 % volume reduction was noted. Occasionally, it was accompanied by definite improvement of the affected neurological functions. Treatment-related complications were encountered in only 6 % of patients, and they were mainly related to transient cranial nerve palsy. Just 2 % of neoplasms showed regrowth after GKS.
Benign Meningioma
The results of GKS for 66 benign skull base meningiomas, which were followed 26–80 months after treatment, were reported recently [16]. At the time of radiosurgery, the volume of the lesion varied from 0.3 to 50.6 cm3 (mean 6.6 cm3). Tumor growth control was attained in 99 % of cases. Shrinkage of the neoplasm was marked in 82 % of patients. Tumor volume reduction of ≥50 % and more was noted in 23 % of cases. Treatment-related morbidity was limited to transient abducent nerve palsy in one patient with a cavernous sinus tumor.
Vestibular Schwannoma
From December 2002, a total of 260 consecutive patients with a vestibular schwannoma underwent GKS in our clinic [10, 12, 18]. At the time of treatment, the tumor volume varied from 0.1 to 9.0 cm3 (mean 1.6 cm3). More than 3 years of follow-up data after irradiation were available for 182 patients. Tumor growth control was attained in 98 % of cases. Shrinkage of the neoplasm was marked in 76 % of patients. Tumor volume reduction of ≥50 % and more was noted in 55 % of cases. Postoperative complications included deterioration of hearing in 8 % of patients and occasional mild vertigo during the period of temporary enlargement of the neoplasm after irradiation.
Nonvestibular Schwannoma
Four patients with abducent nerve schwannoma were followed 7–43 months after GKS [15]. At the time of radiosurgery, the volume of the neoplasm varied from 1.7 to 4.9 cm3 (mean 3.0 cm3). Tumor growth control was attained in all cases. Shrinkage of the neoplasm was marked in three patients, who were followed at least 12 months after irradiation. Treatment-related morbidity included deterioration of vision with transient amaurosis (one case), transient (two cases) and permanent (one case) abducent nerve palsy, and formation of the intratumoral cyst (one case), which demonstrated spontaneous regression during long-term follow-up.
Recently, we analyzed results of GKS in six patients with a facial nerve schwannoma who were followed for 6–72 months after treatment. Tumor shrinkage was noted in three cases. None of the neoplasms regrew after irradiation. Transient facial nerve palsy after irradiation was marked in two patients.
Sellar Tumors
The results of GKS on 89 pituitary adenomas invading the cavernous sinus that were followed for 24–76 months after treatment were reported [14]. There were 43 nonfunctional and 46 hormone-producing tumors. Growth control was attained in 97 % of cases. Shrinkage of the lesion was marked in 64 % of cases. In 80 % of patients with secreting pituitary adenomas, radiosurgery resulted in normalization or improvement of endocrinological function. Treatment-related morbidity included transitory deterioration of the extraocular movements in two patients.
The results of GKS on 18 craniopharyngiomas followed for 12–52 months after treatment were analyzed as well [45]. Tumor growth control was attained in 94 % of cases. Shrinkage of the lesion was marked in 72 % of patients. There were no cases of treatment-related morbidity.
It should be specifically emphasized that none of the patients with a sellar tumor experienced diabetes insipidus, new pituitary hormone deficit, or deterioration of visual function after GKS.
Cavernous Sinus Hemangiomas
Cavernous sinus hemangiomas are rare benign skull base neoplasms for which surgical treatment is extremely difficult owing to abundant vascularization. It was demonstrated, however, that radiosurgery can be effective in these cases [22, 43, 44]. From December 2002, six patients with cavernous sinus hemangioma underwent GKS in our clinic and were followed for 30–78 months thereafter. Shrinkage of the neoplasm was marked in all of them. Reduced tumor volume of >50 % was noted in five cases (83 %). No treatment-related morbidity was noted.
Other Applications of Robotic Gamma Knife Microradiosurgery
With some modification, the described principles of robotic Gamma Knife microradiosurgery can be applied to parenchymal brain tumors [17, 39]. It has also been used to manage trigeminal neuralgia [9] and other intractable pain syndromes [6, 8].
Future Perspectives
The advent of modern technology and introduction of the described microradiosurgical treatment principles may change the paradigm of GKS for benign skull base neoplasms from attaining just tumor growth control to clinically meaningful reduction of lesion volume. The latter may lead to reversal of the neurological deficit, particularly that related to dysfunction of the cranial nerves. Further research should clarify optimal radiosurgical parameters for attaining such treatment goals with minimal risk of side effects and complications. Particularly, possible application of staged GKS for larger neoplasms requires thorough clinical evaluation.
Future advances of robotic Gamma Knife microradiosurgery will be definitely influenced by the development of new neuroimaging modalities and their application for treatment planning. Radiosurgical experience with functional MRI, diffusion-tensor imaging (DTI), and tractography has already demonstrated the high effectiveness of these methods in visualizing eloquent cortical areas and fiber tracts [24, 25, 34]. DTI is also helpful for identifying cranial nerves in cases of their being severely compressed by the tumor [38]. It may lead to prevention of excessive irradiation of functionally important anatomical structures and significantly increased treatment safety. Certainly, advanced MRI techniques can be effectively used with utilization of high-magnetic-field clinical scanners, which is usually considered unacceptable for GKS because of the high risk of distortion artifacts. Currently developing neuroimaging protocols directed at acquisition of geometrically accurate images may allow us to overcome this problem and pave the way for effective use of 3 T MRI for radiosurgical treatment planning [47].
The improved dose homogeneity and greater precision of GKS attained with available robotic devices may permit effective application of low-dose treatment to large-volume intracranial lesions [4, 5]. Nevertheless, the size of the neoplasm still represents the major limitation for radiosurgery [1, 2]. It should be noted, however, that large benign skull base tumors are frequently not suitable for total surgical resection because of the high risk of postoperative complications, particularly those related to injury of the cranial nerves. The best functional outcome in such cases can be attained with combined application of microneurosurgery and radiosurgery. Detailed 3D evaluation of the local neuroanatomy and treatment simulation within the Leksell GammaPlan may permit precise planning of combined management, with clear delineation of the part of the tumor amenable to safe resection and identification of the portion of the mass that is to be left in situ for subsequent irradiation.
Conclusion
The availability of robotic computer-aided devices for GKS led to significant changes in radiosurgical treatment strategy, particularly for benign skull base tumors. Application of the principles of Gamma Knife robotic microradiosurgery based on advanced neuroimaging and highly conformal and selective treatment planning is beneficial for patients, providing a high rate of tumor shrinkage and a low morbidity rate.
References
Davidson L, Zada G, Yu C, Petrovich Z, Pagnini PG, Zee CS, Giannotta SL, Zelman V, Apuzzo MLJ (2009) Delayed toxicity from gamma knife radiosurgery to lesions in or adjacent to the brainstem. J Clin Neurosci 16:1139–1147
Flickinger JC (2002) Radiobiological and dosimetric considerations in stereotactic radiosurgery. In: Pollock BE (ed) Contemporary radiosurgery: technique and evaluation. Futura, Armonk, pp 37–52
Ganz JC (2011) Gamma Knife neurosurgery. Springer, Wien, pp 101–102
Ganz JC, Reda WA, Abdelkarim K (2009) Gamma Knife surgery of large meningiomas: early response to treatment. Acta Neurochir (Wien) 151:1–8
Ganz JC, Reda WA, Abdelkarim K (2009) Adverse radiation effects after Gamma Knife surgery in relation to dose and volume. Acta Neurochir (Wien) 151:9–19
Hayashi M, Taira T, Chernov M, Fukuoka S, Liscak R, Yu CP, Ho RTK, Regis J, Katayama Y, Kawakami Y, Hori T (2002) Gamma knife surgery for cancer pain – pituitary gland – stalk ablation: a multicenter prospective protocol since 2002. J Neurosurg 97(Suppl):433–437
Hayashi M, Chernov M, Izawa M, Iseki H, Hori T, Takakura K (2003) Robotized micro Gamma Knife surgery for 21st century. In: The 12th annual meeting of the Japanese Society of Stereotactic Radiosurgery: program and abstracts, Kyoto, Jun 21–22, 2003, p 35 (in Japanese)
Hayashi M, Taira T, Ochiai T, Chernov M, Takasu Y, Izawa M, Kouyama N, Tomida M, Tokumaru O, Katayama Y, Kawakami Y, Hori T, Takakura K (2005) Gamma knife surgery of the pituitary: new treatment for thalamic pain syndrome. J Neurosurg 102(Suppl):38–41
Hayashi M, Ochiai T, Murata N, Nakaya K, Izawa M, Chernov M, Hori T, Regis J, Takakura K (2006) Gamma knife surgery for essential trigeminal neuralgia: advantages in new treatment strategy with robotized micro-radiosurgery. In: Kondziolka D (ed) Radiosurgery, vol 6. Karger, Basel, pp 260–267
Hayashi M, Ochiai T, Nakaya K, Chernov M, Tamura N, Maruyama T, Yomo S, Izawa M, Hori T, Takakura K, Regis J (2006) Current treatment strategy for vestibular schwannoma: image-guided robotic microradiosurgery. J Neurosurg 105(Suppl):5–11
Hayashi M, Ochiai T, Nakaya K, Chernov M, Tamura N, Yomo S, Izawa M, Hori T, Takakura K, Regis J (2006) Image-guided microradiosurgery for skull base tumors: advantages of using gadolinium-enhanced constructive interference in steady-state imaging. J Neurosurg 105(Suppl):12–17
Hayashi M, Tamura N, Maruyama T, Nakaya K, Ochiai T, Chernov M, Yomo S, Anami H, Izawa M, Ono Y, Okada Y, Hori T, Takakura K (2010) Current treatment strategy of Gamma Knife surgery for vestibular schwannoma: image-guided and robotized microradiosurgery. In: McDermott MW (ed) Radiosurgery, vol 7. Karger, Basel, pp 175–188
Hayashi M, Tamura N, Nakaya K, Ochiai T, Chernov M, Yomo S, Anami H, Izawa M, Okada Y, Ono Y, Hori T, Takakura K (2010) Image-guided micro Gamma Knife surgery for skull-base tumors to avoid underlying dysfunction of the surrounding vital structures using CISS with gadolinium enhancement. In: McDermott MW (ed) Radiosurgery, vol 7. Karger, Basel, pp 227–236
Hayashi M, Chernov M, Tamura N, Nagai M, Yomo S, Ochiai T, Amano K, Izawa M, Hori T, Muragaki Y, Iseki H, Okada Y, Takakura K (2010) Gamma Knife robotic microradiosurgery of pituitary adenomas invading the cavernous sinus: treatment concept and results in 89 cases. J Neurooncol 98:185–194
Hayashi M, Chernov M, Tamura N, Yomo S, Ochiai T, Nagai M, Tamura M, Izawa M, Muragaki Y, Iseki H, Okada Y, Takakura K (2010) Gamma Knife surgery for abducent nerve schwannoma: report of 4 cases. J Neurosurg 113(Suppl):136–143
Hayashi M, Chernov M, Tamura N, Izawa M, Muragaki Y, Iseki H, Okada Y, Takakura K (2011) Gamma Knife robotic microradiosurgery for benign skull base meningiomas: tumor shrinkage may depend on the amount of radiation energy delivered per lesion volume (unit energy). Stereotact Funct Neurosurg 89:6–16
Hayashi M, Chernov M, Tamura N, Tamura M, Izawa M, Muragaki Y, Iseki H, Okada Y (2011) “Donut’s shape” radiosurgical treatment planning for large cystic metastatic brain tumors. Minim Invasive Neurosurg 54:286–289
Hayashi M, Chernov MF, Lipski SM, Tamura N, Yomo S, Horiba A, Tsuzuki S, Izawa M, Okada Y, Muragaki Y, Iseki H, Ivanov P, Regis J, Takakura K (2013) Do we really still need an open surgery for treatment of patients with vestibular schwannomas? Acta Neurochir Suppl 116:25–36 (present volume)
Hayashi M, Chernov MF, Tamura N, Yomo S, Tamura M, Horiba A, Izawa M, Muragaki Y, Iseki H, Okada Y, Ivanov P, Regis J, Takakura K (2013) Usefulness of the advanced neuroimaging protocol based on plain and gadolinium-enhanced constructive interference in steady state images for Gamma Knife radiosurgery and planning microsurgical procedures for skull base tumors. Acta Neurochir Suppl 116:167–178 (present volume)
Herman MG, McCullough EC (2002) Physical aspects of cranial stereotactic radiosurgery. In: Pollock BE (ed) Contemporary radiosurgery: technique and evaluation. Futura, Armonk, pp 17–36
Horstmann GA, Van Eck AT (2002) Gamma Knife model C with automatic positioning system and its impact on the treatment of vestibular schwannomas. J Neurosurg 97(5 Suppl):450–455
Ivanov P, Chernov M, Hayashi M, Nakaya K, Izawa M, Murata N, Kubo O, Ujiie H, Muragaki Y, Nakamura R, Iseki H, Hori T, Takakura K (2008) Low-dose gamma knife radiosurgery for cavernous sinus hemangioma: report of 3 cases and literature review. Minim Invasive Neurosurg 51:140–146
Karlsson B (2002) Dose selection and prediction of stereotactic radiosurgery outcomes. In: Pollock BE (ed) Contemporary radiosurgery: technique and evaluation. Futura, Armonk, pp 53–73
Koga T, Maruyama K, Igaki H, Tago M, Saito N (2009) The value of image coregistration during stereotactic radiosurgery. Acta Neurochir (Wien) 151:465–471
Koga T, Maruyama K, Kamada K, Ota T, Shin M, Itoh D, Kunii N, Ino K, Terahara A, Aoki S, Masutani Y, Saito N (2012) Outcomes of diffusion tensor tractography-integrated stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 82:799–802
Kondziolka D, Maitz AH, Niranjan A, Flickinger JC, Lunsford LD (2002) An evaluation of the model C Gamma Knife with automatic patient positioning. Neurosurgery 50:429–432
Kuo JS, Yu C, Giannotta SL, Petrovich Z, Apuzzo MLJ (2004) The Leksell gamma knife model U versus model C: a quantitative comparison of radiosurgical treatment parameters. Neurosurgery 55:168–173
Levivier M, Massager N, Wikler D, Goldman S (2004) Modern multimodal neuroimaging for radiosurgery: the example of PET scan integration. Acta Neurochir Suppl 91:1–7
Lindquist C, Paddick I (2007) The Leksell Gamma Knife Perfexion and comparison with its Predecessors. Neurosurgery 61(3 Suppl):130–141
Massager N, Maris C, Nissim O, Devriendt D, Salmon I, Levivier M (2009) Experimental analysis of radiation dose distribution in radiosurgery: I. Dose hot spot inside target volume. Stereotact Funct Neurosurg 87:82–87
Massager N, Maris C, Nissim O, Devriendt D, Salmon I, Levivier M (2009) Experimental analysis of radiation dose distribution in radiosurgery: II. Dose fall-off outside the target volume. Stereotact Funct Neurosurg 87:137–142
Paddick I, Lippitz B (2006) A simple dose gradient measurement tool to complement the conformity index. J Neurosurg 105(Suppl):194–201
Pamir MN, Kilic T, Belirgen M, Abacioglu U, Karabekiroglu N (2007) Pituitary adenomas treated with Gamma Knife radiosurgery: volumetric analysis of 100 cases with minimum 3 year follow-up. Neurosurgery 61:270–280
Pantelis E, Papadakis N, Verigos K, Stathochristopoulou I, Antypas C, Lekas L, Tzouras A, Georgiou E, Salvaras N (2010) Integration of functional MRI and white matter tractography in stereotactic radiosurgery clinical practice. Int J Radiat Oncol Biol Phys 82:257–267
Regis J, David P, Wikler D, Porcheron D, Levrier O (2004) Stereotactic mapping for radiosurgical treatment of vestibular schwannomas. Neurochirurgie 50:270–281 (in French)
Regis J, Hayashi M, Porcheron D, Delsanti C, Muracciole X, Peragut JC (2002) Impact of the model C and automatic positioning system on Gamma Knife radiosurgery: an evaluation in vestibular schwannomas. J Neurosurg 97(5 Suppl):588–591
Regis J, Tamura M, Guillot C, Yomo S, Muraciolle X, Nagaje M, Arka Y, Porcheron D (2009) Radiosurgery with the world’s first fully robotized Leksell Gamma Knife PerfeXion in clinical use: a 200-patient prospective, randomized, controlled comparison with the Gamma Knife 4C. Neurosurgery 64:346–356
Roundy N, Delashaw JB, Cetas JS (2012) Preoperative identification of the facial nerve in patients with large cerebellopontine angle tumors using high-density diffusion tensor imaging. J Neurosurg 116:697–702
Takakura K, Hayashi M, Chernov MF, Tamura N, Izawa M, Okada Y, Tamura M, Muragaki Y, Iseki H (2013) Gamma Knife treatment strategy for metastatic brain tumors. Acta Neurochir Suppl 116:63–69 (present volume)
Takakura K, Iseki H, Chernov M, Hayashi M (2010) Development of a concept of Gamma Knife robotic microradiosurgery and its application in management of various intracranial diseases. In: IREIIMS achievement report 2005–2010. IREIIMS, Tokyo Women’s Medical University, Tokyo, p 50
Tishler RB, Loeffler JS, Lunsford LD, Duma C, Alexander E III, Kooy HM, Flickinger JC (1993) Tolerance of cranial nerves of the cavernous sinus to radiosurgery. Int J Radiat Oncol Biol Phys 27:215–221
Tlachacova D, Schmitt M, Novotny J Jr, Novotny J, Majali M, Liscak R (2005) A comparison of the Gamma Knife model C and the automatic positioning system with Leksell model B. J Neurosurg 102(Suppl):25–28
Wang X, Mei G, Liu X, Dai J, Pan L, Wang E (2012) The role of stereotactic radiosurgery in cavernous sinus hemangiomas: a systematic review and meta-analysis. J Neurooncol 107:239–245
Yamamoto M, Kida Y, Fukuoka S, Iwai Y, Jokura H, Akabane A, Serizawa T (2010) Gamma Knife radiosurgery for hemangiomas of the cavernous sinus: a seven-institute study in Japan. J Neurosurg 112:772–779
Yomo S, Hayashi M, Chernov M, Tamura N, Izawa M, Okada Y, Hori T, Iseki H (2009) Stereotactic radiosurgery of residual and recurrent craniopharyngioma: new treatment concept using Leksell Gamma Knife model C with automatic positioning system. Stereotact Funct Neurosurg 87:360–367
Yomo S, Tamura M, Carron R, Porcheron D, Regis J (2010) A quantitative comparison of radiosurgical treatment parameters in vestibular schwannomas: the Leksell Gamma Knife Perfexion versus model 4C. Acta Neurochir (Wien) 152:47–55
Zhang B, MacFadden D, Damyanovich AZ, Rieker M, Stainsby J, Bernstein M, Jaffray DA, Mikulis D, Menard C (2010) Development of a geometrically accurate imaging protocol at 3 Tesla MRI for stereotactic radiosurgery treatment planning. Phys Med Biol 55:6601–6615
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Wien
About this paper
Cite this paper
Hayashi, M. et al. (2013). Concept of Robotic Gamma Knife Microradiosurgery and Results of Its Clinical Application in Benign Skull Base Tumors. In: Chernov, M., Hayashi, M., Ganz, J., Takakura, K. (eds) Gamma Knife Neurosurgery in the Management of Intracranial Disorders. Acta Neurochirurgica Supplement, vol 116. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1376-9_2
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1376-9_2
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1375-2
Online ISBN: 978-3-7091-1376-9
eBook Packages: MedicineMedicine (R0)