Abstract
Total knee arthroplasty (TKA) is one of the most successful orthopedic procedures to date, and the number of TKAs performed worldwide continues to exponentially increase. Cementing using polymethylmethacrylate (PMMA) bone cement still is the most common method by which TKA prosthetic components are affixed to the bone. Unfortunately, a small percentage of TKAs will suffer from early failure due to infectious and non-infectious causes and require revision surgery. TKA revision surgery is costly, causes significant patient morbidity, and is not uniformly successful. Antibiotic-loaded bone cement is a material that has the potential to significantly reduce the burden of TKA revision and is, therefore, the focus of current research and debate. This chapter highlights evidence-based medicine (EBM) in favor of routine ALBC use for cemented TKA and briefly addresses the efficacy of other contemporary TKA local antimicrobial delivery strategies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
Total knee arthroplasty (TKA) is one of the most successful orthopedic procedures to date (Price et al. 2018). The number of TKAs performed worldwide continues to exponentially increase and has been estimated to be more than two million procedures per annum (Kurtz et al. 2011). When done for appropriate patients and conditions, TKA predictably reduces pain, improves function, and increases patient quality of life (Rocha de Silva et al. 2014).
Fixation of the TKA prosthesis to bone remains an area of active investigation and improvement. Cementing using polymethylmethacrylate (PMMA) bone cement still is the most common method by which TKA prosthetic components are affixed to the bone (Abdel and Berry 2019; National Joint Registry 2019; Australian Orthopaedic Association Joint Replacement Registry 2019a). When used for TKA, PMMA has demonstrated exemplary results. Currently, cemented TKA is the “gold standard” and accounts for greater than 95% of TKAs performed worldwide (National Joint Registry 2019; Australian Orthopaedic Association Joint Replacement Registry 2019b; Nugent et al. 2019).
Unfortunately, a small percentage of TKAs will suffer from early failure due to infectious and non-infectious causes and require revision surgery. Due to the large number of TKAs performed annually, the small percentage of TKAs requiring revision results in a substantial absolute number of revision surgeries. TKA revision surgery is costly, causes significant patient morbidity, and is not uniformly successful (Bozic et al. 2010; Salah et al. 2003). Consequently, surgical techniques and materials able to reduce the incidence of revision surgery are of paramount importance. Antibiotic-loaded bone cement (ALBC) is a material that has the potential to significantly reduce the burden of TKA revision and is, therefore, the focus of current research and debate.
2 Historical Context
Early arthroplasty surgeons noted prosthetic joint infection (PJI) was a relatively common and disastrous cause of THA and TKA failure. In the 1970s, it was noted ALBC use during THA could reduce the incidence of PJI (Buchholz et al. 1984). ALBC was also being used to treat THA PJI with great success (Buchholz et al. 1981). Therefore, it is not surprising that ALBC was later embraced during the development of modern cemented TKA techniques to both prevent and treat PJI (Best et al. 1998).
In the late 1970s and early 1980s, the incidence of early THA and TKA failures steadily decreased due to improvements in prosthetic design, biomaterials, and surgical techniques (Moran and Horton 2000). Additionally, adoption and standardization of prophylactic parenteral antibiotic administration prior to THA and TKA markedly decreased the incidence of PJI (Lidgren 2001). During this time, significantly different ALBC usage patterns emerged.
From the 1980s onward, many surgeons strongly advocated for routine ALBC use during all THA and TKA due to the excellent past performance of ALBC with respect to preventing THA PJI and revision. In contrast, other surgeons believed the impressive PJI and revision reductions that occurred were mainly attributable to improved surgical techniques and prophylactic antibiotic administration. Many of the same surgeons argued for the use of plain bone cement (PBC) without added antibiotics during cemented THA and TKA. This difference in opinion regarding appropriateness of ALBC utilization has persisted and continues to be debated (Parvizi et al. 2013).
It should be noted that these ALBC and PBC utilization and opinion differences evolved in an easily recognized geographic distribution. In general, most surgeons in Europe adopted routine use of ALBC for all THA and TKA surgeries while most US surgeons opted to perform THA and TKA using PBC. It is unlikely coincidental that the major PMMA producers in Europe were manufacturing predominantly ALBC while those in the United States were manufacturing predominantly PBC. It is highly probable that these commercial forces helped contribute to the current bone cement “transatlantic paradox” where ALBC is routinely used in Europe and much less commonly used in the United States (Sanz-Ruiz et al. 2017, 2020).
Such variations in ALBC opinion and utilization have set the stage for one of the premier questions and debates in THA and TKA: Should antibiotic-loaded bone cement be used routinely for all cemented THA and TKA?
The remainder of this chapter highlights evidence-based medicine (EBM) in favor of routine ALBC use for cemented TKA and briefly addresses the efficacy of other contemporary TKA local antimicrobial delivery strategies.
3 Current Consensus
There is wide divergence in opinion regarding the routine use of ALBC for THA and TKA PJI prophylaxis. This was documented at the 2nd International Consensus Meeting (ICM) on Periprosthetic Joint Infection where protracted debate concerning ALBC occurred amongst more than 500 PJI treatment experts. As with all topics addressed by the meeting, a team of expert topic authors (Fillingham et al. 2019) performed a systematic literature review of ALBC and formulated a response to a question posed by the Delphi Process. The evidence-based response was then presented to the attendees for a live consensus vote. The full 2018 ICM process and meeting document can be accessed at ► www.ICMPhilly.com.
2018 ICM ALBC question, response, and live attendee vote are detailed below:
-
Question: Is there sufficient evidence to support the use of antibiotic-loaded cement in primary total knee arthroplasty (TKA) or total hip arthroplasty (THA) to reduce the risk of surgical site infections/periprosthetic joint infections (SSIs/PJIs)?
-
Response: There is no conclusive evidence to demonstrate that routine use of antibiotic-loaded cement in primary TKA or THA reduces the risk of subsequent SSIs/PJIs. Recent high-level evidence and registry data have not demonstrated a reduction in SSI/PJIs. Furthermore, the added cost, the potential for the emergence of resistant organisms, and the potential adverse effect of antibiotics on the host provide adequate reasons to refrain from routine use of antibiotic-loaded cement during primary total joint arthroplasty.
-
Attendee vote: 38% Agree, 58% Disagree, and 4% Abstain.
The initial live vote demonstrated most PJI treatment experts in attendance believed antibiotic-bone cement could reduce the incidence of PJI. It also indicated the majority of attendees believed routine use of ALBC during THA and TKA was either acceptable or preferred. Because of the failure to reach a consensus statement with the first question, the MSIS ICM organizing committee elected to modify the question in hopes of clarifying the attendee’s views on ALBC use for primary THA and TKA. The modified question and response with attendee vote are detailed below:
-
Question: Is there a role for the use of antibiotic-impregnated cement in primary total joint arthroplasty (TJA)?
-
Response: Antibiotic-impregnated cement may be used during primary TJA to reduce the risk of surgical site infections/periprosthetic joint infections (SSIs/PJIs). The benefits of antibiotic-impregnated cement versus its cost and other potential adverse effects may be most justified in patients at high risk of infection.
-
Attendee vote: 93% Agree, 7% Disagree.
The supermajority and strong consensus of this vote undoubtedly shows that the 2018 ICM attendees agree that ALBC has a role in primary THA and TKA.
Furthermore, it suggests THA and TKA PJI experts agree ALBC utilization can decrease PJI incidence. Lastly, it demonstrates the potential costs and other theoretical negative aspects of ALBC usage are outweighed by ALBC benefits.
4 Products and Regulations
Many different commercially pre-mixed ALBC products are distributed and available for purchase in the world. The type of antibiotic contained and concentration of antibiotic vary significantly among the different products. Therefore, it is not surprising that the antibiotic elution characteristics of these pre-mixed commercially available bone cements are unique to each specific product and the intraoperative methods by which they are mixed (Kuehn 2014).
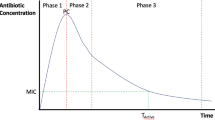
Prior investigations comparing elution of commercially pre-mixed ALBC have been performed. Squire et al. demonstrated that the in vitro antibiotic elution properties of 5 different commercially available ALBC products rapidly changed over time with high-viscosity brands producing significantly greater duration of antimicrobial activity as compared to lower-viscosity ALBC brands (◘ Fig. 46.1) (Squire et al. 2008).
Antimicrobial efficacy. (Squire et al. 2008, with permission from Elsevier)
Additionally, the investigation of Meyer et al. studying the antibiotic elution properties of 6 commercially available ALBC products showed that both ALBC brand and mixing regimen (vacuum vs. atmospheric) significantly influenced antibiotic elution intensity and duration (Meyer et al. 2011). This investigation indicates antibiotic elution of many ALBC products after 24 h is below the minimal inhibitory concentration (MIC) necessary to produce antibacterial efficacy whereas other products elute antibiotic concentrations above MIC for 3 or more days (◘ Fig. 46.2).
Comparison of average zone of bacterial growth inhibition (left) and antibiotic concentration (right) for vacuum-mixed bone cements during 5-day elution study. The horizontal line represents the 32 mg/L susceptibility threshold. (From Meyer et al. 2011, by courtesy of Wolters Kluwer Health, Inc.)
Assuming the in vitro studies above are translatable to the in vivo environment, differences in ALBC product antibiotic elution intensity and duration could have a significant impact on their ability to prevent SSI and/or PJI.
Regulatory approval for commercially pre-mixed ALBC products varies by country. While use of pre-mixed ALBC is the standard of care for primary THA and TKA in Europe and many other regions, in the United States, usage of pre-mixed ALBC is Food and Drug Administration approved only for use in the second stage of a two-stage revision for known septic THA and TKA. Therefore, in the United States, routine usage for primary THA and TKA is “off-label”.
ALBC can be constructed by “hand blending” of powdered antibiotics into PMMA not containing antibiotics.
Hand-blended ALBC suffers from inconsistencies introduced by human error and results in PMMA that has variable elution and mechanical characteristics (Ferraris et al. 2010; Dunne et al. 2007; Neut et al. 2003).
Importantly, a review of physician modification of FDA-approved devices concluded that “since the device had been modified after the manufacturing process and used outside the instructions for use, the manufacturer essentially became exempt from any product liability claim” (Starnes 2013), potentially enhancing the liability of the physician in cases where patient harm is realized. Because of the excellent pre-mixed commercial products currently available, the utility of hand blending ALBC for routine primary THA and TKA PJI prophylaxis is questionable.
It is the author’s opinion that hand blending of ALBC should be reserved for infrequent clinical situations requiring local delivery of more or different antibiotics than commercially pre-mixed ALBC products can provide.
5 Evidence
5.1 Retrospective
In 2003, investigators at a French hospital compared their experience with ALBC to PBC when used during primary TKA (Eveillard et al. 2003). In this review of TKAs, ALBC containing unknown concentration of gentamicin was utilized. Clean-air rooms, pre-incision parenteral antibiotics, and iodized alcohol skin preparation were also utilized for all patients. Incidence of comorbid conditions increasing PJI incidence was not detailed for the different groups. Minimum follow-up was 12 months and the outcome of interest was PJI. ALBC was utilized in 83 patients and PBC was utilized in 84 patients per the discretion of the faculty surgeon. PJI incidence in the ALBC group was 1.21% while the PJI incidence in the PBC group was 9.52%.
In this investigation, ALBC demonstrated protective efficacy against PJI (p = 0.03); however, it should be noted the incidence of PJI for the PBC cohort was much higher than expected for primary TKA.
In a 2009 non-randomized investigation, ALBC ability to reduce PJI in 1625 consecutive TKAs performed in a Canadian institution was assessed (Gandhi et al. 2009). Analysis of the ALBC and PBC groups showed them to be demographically and clinically similar. ALBC group (814 TKA) PJI incidence was 2.2% and PBC group (811 TKA) PJI incidence was 3.1%. There were 7 fewer PJIs at 1 year in the ALBC group which is a 30% reduction in PJI. Despite this, PJI difference between ALBC and PBC groups was deemed to not be statistically significant. Examination of the statistical methodology used demonstrates the investigation was constructed to detect a 50% PJI incidence change.
Therefore, failure to ascribe statistical significance to the observed 30% PJI reduction could very well represent a type II error and failure to recognize the efficacy of ALBC in preventing PJI.
The Kaiser Permanente Registry reported on the efficacy of ALBC from 2003 to 2007 using their large US community database of 22,889 TKAs (Namba et al. 2009). In this investigation, ALBC was used per the surgeon’s discretion in 8.9% of all TKAs (2030). In this investigation, TKA PJI incidence was noted to be 1.4% in the ALBC group vs. 0.7% in the PBC cohort, and use of ALBC was found to be an independent risk factor for development of TKA PJI.
Careful examination of the study reveals significant differences in the ALBC and PBC cohorts. The ALBC cohort had statistically greater percentages of diabetics (14.5% vs. 10.3%), individuals <55 years of age (10.3% vs 7.0%), diagnoses other than osteoarthritis (10.8% vs. 7.3%), and ASA III classification patients (41.9% vs. 35.3%). Multivariate analyses performed in this investigation demonstrated all of these patient characteristics were independent risk factors for development of TKA PJI. Increased selective ALBC utilization in patients demonstrated to be at high risk for PJI is a substantial methodological and statistical bias which most likely increased the PJI incidence among the ALBC cohort.
Despite being a large registry-driven investigation, the statistical consequences of not controlling for the above cohort disparities seriously call into question the conclusions drawn from comparing the ALBC and PBC groups.
A recent investigation published in the Journal of Arthroplasty details a European hospital’s PJI experience when changing from PBC to commercially pre-mixed ALBC (Sanz-Ruiz et al. 2017). As reported, PMMA type was the only surgical or infection control variable changed within the institution over the study period with PBC uniformly used from 2009 to 2010 and uniform ALBC utilization from 2011 to 2012. All patients receiving either a primary TKA, THA, or hemiarthroplasty, were enrolled consecutively, and assessed for PJI at 2-year minimum follow-up. Despite the retrospective design, this study included the institutional PJI incidence for cementless hemiarthroplasty and THA during the same time period which effectively serve as control groups. ALBC utilization significantly decreased PJI incidence for all cemented groups (TKA, THA, and hemiarthroplasty).
TKA PJI risk dropped from 3.3% to 1.3% which was a statistically significant overall risk reduction of 60%.
Similar statistically significant decreases in cemented THA and hemiarthroplasty PJI incidence were also noted. PJI incidence of the control groups (cementless THA and cementless hemiarthroplasty) demonstrated no statistical change throughout the study duration. This contemporary investigation indicates ALBC use can significantly decrease PJI incidence.
Risk stratified usage of ALBC was examined in the similarly named article published in the Journal of Orthopedics 2020 (Qadir et al. 2014). In this retrospective review of TKAs performed in a single center, the authors divided patients into 3 groups: PBC TKAs, ALBC TKAs, and selective ALBC TKAs (used per surgeon discretion in patient when deemed high risk). The 3 groups had statistically similar numbers of diabetics and patients with inflammatory arthritis; however, there was a trend for the selective ALBC group to have more patients with significant obesity within it.
There were no details given regarding group-to-group distribution of other patient characteristics (e.g., malnutrition) thought to increase PJI incidence.
This investigation noted the 30-day, 6 month, and 1 year incidence of PJI among the different groups was identical. Obese patients in group 3 demonstrated a trend for increased PJI although this was not statistically significant. The conclusion of this investigation was that ALBC did not decrease PJI incidence and even selective use may not be justified. Another interpretation of this data could be that the selective ALBC group which was at the highest theoretical risk for PJI did not demonstrate an increased risk of PJI; therefore, the selective ALBC use mitigated excess PJI risk and its use was indeed justified.
A very recent analysis of 1,180,270 US patients undergoing TKA strongly supports the selective use of antibiotic-loaded bone cement (Chan et al. 2019). This study leveraged the Premier Healthcare Database, which contains administrative claims data for 20–25% of all US hospitalizations. ALBC was used in 27% of patients and was associated with both PJI prevention and lower odds of early postoperative infection (OR = 0.89; 95% CI 0.83–0.96). The investigation is unique for its extremely large patient cohort and robust multi-variate analysis including a significant number of variables known to increase PJI risks such as age, anesthesia modality, concomitant medications, smoking, obesity, and the Quan adaptation of the Charlson-Deyo index. Raw data analysis in this investigation indicated ALBC use might be correlated with acute renal failure not requiring dialysis (OR = 1.06; 95% CI: 1.02–1.11).
However, after controlling for other variables known to cause renal failure, ALBC association with renal failure was no longer statistically significant. Likewise, ALBC use did not lead to statistically greater allergic complications or microbiome disruptions.
5.2 Randomized Controlled
Limited prospective randomized studies exist detailing ALBC efficacy for primary TKA PJI prevention. Existing studies have shown mixed results and are prone to type II statistical error as PJI occurs infrequently and extremely large patient cohorts are required to demonstrate a positive effect on PJI prevention.
Unfortunately, different ALBC products were used in different studies which could be the reason different results and conclusions were reached by the authors.
One of the first randomized prospective studies demonstrating efficacy of ALBC was performed by Chiu et al. in a patient cohort of diabetic patients undergoing TKA. He demonstrated that ALBC decreased PJI risk in this cohort by 13% (Chiu et al. 2001). Using another randomized prospective study, the same authors demonstrated that ALBC significantly decreased the incidence of PJI in a non-diabetic patient cohort (Chiu et al. 2002). Both studies indicated ALBC use decreased PJI incidence but critiques of both studies noted a relatively high baseline risk of infection.
In contrast, a Spanish group of investigators failed to find efficacy of hand-blended ALBC containing colistin and erythromycin for reducing TKA PJI in a randomized-controlled study design (Hinarejos et al. 2013). In this reasonably powered and well-designed study, PJI incidence for the ALBC and PBC groups were very similar (1.37% and 1.35%, respectively). However, the authors noted several times that even though this was a level I investigation, the results of the study are only specific to ALBC containing colistin and erythromycin and repeating the study with a different ALBC formulation might demonstrate ALBC ability to reduce the incidence of PJI.
Currently, a large prospective study entitled “Antibiotic Loaded Bone Cement in Prevention of Periprosthetic Joint Infections in Primary Total Knee Arthroplasty” is enrolling patients. In this randomized study where patients will either receive ALBC or PBC for primary TKA, the primary aim is to determine the rate of revision due to PJI for the two groups and the cost-effectiveness of ALBC. The study seeks to enroll over 11,000 patients based on power analyses demonstrating registry PJI incidence of 1.0% (ALBC) and 1.5% (PBC), respectively.
The results of this study will be invaluable to improving our understanding the role of ALBC in primary TKA.
5.3 Systematic Reviews and Meta-analyses
Use of ALBC has been examined in systematic reviews and meta-analyses and has yielded conflicting results (Wang et al. 2013; Zhou et al. 2015; Schiavone Panni et al. 2016; King et al. 2018; Zhang et al. 2019). Due to lack of control groups and other deficiencies in scientific rigor, there are very few investigations examining the effect of ALBC on PJI incidence that qualify for inclusion in systematic reviews or meta-analyses. Careful examination of this literature shows it spans a broad time range (1987–2015) over which surgical environmental conditions and techniques have remarkably changed potentially skewing results. Furthermore, the types of ALBC used in the studies are quite heterogeneous (different products, antibiotics, antibiotic concentrations, as well as ALBC preparation methods) potentially introducing a confounding influence on results. Lastly, because of the low number of quality studies available, subtle differences in investigation exclusion and inclusion criteria can produce profound differences in results and conclusions.
An Italian group of authors performed a systemic review of ALBC efficacy for reducing TKA PJI incidence in 2016 (Schiavone Panni et al. 2016). Literature search returned 260 articles which were then narrowed to 6 publications. The pooled patient number included in the review was 6300. Significant methodological deficiencies in the included studies were identified which included but were not limited to heterogeneity in ALBC product type, differences in patient comorbidities, as well as poor patient randomization and blinding practices. This systematic review concluded ALBC was not protective for preventing TKA PJI. Two included investigations demonstrated ALBC to be protective against TKA PJI (Chiu, Eveillard) while four studies did not (Gandhi, Namba, Hinarejos, Wang). Only two randomized controlled studies could be identified and were included in this systematic review, one of which demonstrated efficacy of ALBC for the prevention of TKA PJI (Chiu) and the other one did not (Hinarejos). It should be noted that more than two-thirds of the pooled patients included in this review were derived from two retrospective studies with the lowest methodological quality scores both of which did not demonstrate efficacy of ALBC for preventing TKA PJI (Namba, Wang).
The most recent meta-analysis on ALBC efficacy in PJI prevention was published in 2019 (Zhang et al. 2019). This investigation narrowed initial search from 1049 potential studies to 10 randomized controlled trials (RCT) or cohort studies providing 13,909 THA and TKA patients for analysis. The date range for the included studies was 1981–2017. Within this meta-analysis, there were 3 randomized controlled trials (RCT) with 2287 patients which compared SSI/PJI incidence between patient groups receiving prophylactic antibiotics at the time of surgery to those receiving ALBC but no systemic antibiotics at the time of surgery. While the PJI incidence was lower within this ALBC subgroup (OR 0.34, CI: 0.14–0.89) the SSI incidence was higher within the ALBC group (OR 1.53, CI: 1.11–2.11) as compared to the prophylactic antibiotic group.
-
When the studies not providing systemic prophylactic antibiotics were removed and compared ALBC+prophylactic antibiotics to prophylactic antibiotics alone, SSI odds ratio for the ALBC+prophylactic antibiotic group was 0.68 (CI: 0.52–0.88).
-
When all 10 studies were included comparing THA and TKA PJI incidence in patients receiving ALBC with those that did not receive ALBC the OR markedly favored the ALBC group (OR 0.52, CI: 0.39–0.71).
-
When only TKA PJI was considered, again the odds ratio favored ALBC (OR 0.62, CI: 0.45–0.87).
5.4 Registry
Registry Data
In 2017, the Australian Orthopaedic Association published a supplementary report on bone cement in hip & knee arthroplasty using their national registry (Australian Orthopaedic Association 2017). This report covered 293,025 primary TKA procedures and 9753 revisions between 1999 and 2015.
In this analysis of total knee replacements, use of plain cement was associated with a statistically higher rate of revision (HR = 1.06; p = 0.038) as compared to ALBC.
Recently, a review of the National Joint Registry of England and Wales including over 700,000 TKAs demonstrated use of ALBC was associated with a decreased risk of revision as compared to TKAs implanted with PBC (Jameson et al. 2019). In this study many variables thought to be potential biases were controlled and separately examined.
The conclusion of the article was that ALBC was associated with a 19% lower rate of septic and aseptic revisions as compared to PBC.
Importantly, this analysis allowed determination of the number of patients who would have to receive ALBC before one PJI was prevented. The so-called number-needed-to-treat (NNT) was 115, i.e., one PJI would be prevented for every 115 patients receiving ALBC. From this NNT, cost-effectiveness can be estimated for a large population.
Assuming the additional cost of ALBC per TKA case is $300–500 USD as compared to PBC, the additional cost of ALBC in 115 patients would be $34,000–57,000 USD. Because the average cost of treating one PJI is approx. $100,000 USD, use of ALBC in this study would result in significant cost savings.
A report on 43,149 knee replacement cases from the Finnish Registry examined the impact of antibiotic delivery on re-operations for infections in primary and revision knees (Jamsen et al. 2009). The investigators looked at the impact of different antibiotic delivery strategies. In this analysis, systemic administration with ALBC demonstrated the lowest risk of revision for PJI in both primary and revision TKA. When compared to the systemic antibiotic with ALBC group, primary TKAs performed with systemic antibiotics only demonstrated a hazard ratio of 1.42 (95% CI: 1.08–1.88) for re-operation due to PJI. For revision TKA, only using systemic antibiotics increased the odds of re-operation for PJI by 2.12 (95% CI: 1.14–3.92).
For completeness, it is important to acknowledge both the Canadian and New Zealand Registry data with respect to ALBC and primary TKA. Data from these registries have been cited as evidence that ALBC usage does not prevent PJI or improve TKA outcomes. Understanding ALBC utilization, statistical nuances, and idiosyncratic findings of these registries are important to better understand the role of ALBC for primary TKA.
The Canadian Registry examined 36,681 primary TKA cases from 2003 to 2008 of which 45% were implanted with ALBC (Bohm et al. 2013). The multi-variate analysis of this registry, which controlled for age, sex, diabetes, and Charlson Comorbidity Index score indicated ALBC did not statistically alter the odds of needing TKA revision at 2 years (HR = 1.066; 95% CI: 0.90–1.27). However, and importantly, this registry analysis noted the hazard ratio for primary TKA revision was lower for surgeons who uniformly utilized ALBC (HR 1.04, 95% CI: 0.86–1.44) as compared to surgeons selectively utilizing ALBC (HR 1.19, CI: 0.75–1.90).
This curious paradox indicates all confounding variables may not have been adequately identified or controlled during registry data analysis and could be used to promote increased ALBC usage in the Canadian TKA population.
The New Zealand registry examined 64,566 primary TKAs performed between 1999 and 2012. Approximately, two-thirds of the patients in the New Zealand registry received a low-viscosity ALBC product with less than optimal antibiotic elution characteristics. Multi-variate analysis of this registry data indicated ALBC was a significant predictor of PJI at 6 months (OR = 1.93; p = 0.008) but not at 12 months. Unfortunately, this investigation included few patient risk factors correlated with PJI (BMI and prior surgery) and the authors acknowledge the increased PJI hazard rate with ALBC use is likely a direct result of selective ALBC use in patients at increased risk for PJI.
Because of the ALBC product utilized and suboptimal statistical control of confounding variables known to be correlated with PJI, caution should be exercised when drawing ALBC efficacy conclusions from this investigation.
6 Cost-Effectiveness
The economic ramifications for ALBC utilization differ among geographic markets. The main variables required to compute ALBC cost-effectiveness are:
-
PJI incidence (hospital and/or health system),
-
PJI treatment cost ($100,000 USD),
-
ALBC product cost in comparison to PBC product.
In general, as the absolute price difference between ALBC and PBC decreases so does the institutional PJI incidence required to make the use of ALBC cost neutral or cost beneficial. Geographically, the cost of ALBC is the greatest in the US healthcare marketplace, which more likely than not accounts for US vs. non-US reported differences in ALBC cost-effectiveness.
ALBC pricing within the US healthcare marketplace has consistently trended downward so that the average cost difference of two ALBC packs compared to two PBC packs is now less than $300 (Mendenhall & Associates). Theoretically, at this cost, ALBC would have to decrease PJI incidence by one TKA per 333 TKAs (0.3%) to make its use cost neutral or to demonstrate cost savings.
7 Safety
The main safety concerns with use of antibiotic-loaded bone cement pertains to kidney damage and antibiotic resistance. As previously discussed, a study of 1,184,270 US TKA insurance claims found that ALBC use was associated with a slight increase in acute renal failure in one analysis (OR = 1.06; 95% CI: 1.02–1.11) but this finding could not be replicated in subsequent sensitivity analyses and ALBC was not associated with a significant increase in the need for acute dialysis (Chan et al. 2019).
In a separate study of 2775 arthroplasty procedures performed in Belfast, Northern Ireland, from 2015 to 2016, patients undergoing cementless arthroplasty received intravenous cefuroxime and gentamicin while patients with cemented arthroplasty received intravenous cefuroxime and localized administration of gentamicin via ALBC (Tucker et al. 2018).
Patients receiving systemic gentamicin were observed to have twice the rate of acute kidney injury as compared to patients receiving gentamicin-impregnated ALBC (OR = 2.118; p = 0.004).
In 2014, the Rothman Institute reported on how ALBC impacted antimicrobial resistance patterns among patients who developed PJI (Hansen et al. 2014). The Rothman Institute switched from PBC to ALBC in 2003 allowing comparison of a cementless THA cohort over the entire study duration, PBC cohort prior to 2003, and ALBC cohort after 2003. With the switch to ALBC, they observed a 65% institutional reduction in the incidence of PJI for cemented arthroplasties (2.0% to 0.7%). Over the same time period, the PJI incidence in cementless hips only decreased by 33% (0.6% to 0.4%).
Investigators also examined the change in infective organism and antimicrobial resistance profiles for patients who developed culture-positive PJI (nTKA = 120; nTHA = 54). After the initiation of routine ALBC use, the causative organism did not change significantly (p > 0.1). Additionally, while methicillin-resistance increased in cementless hips after 2003, the incidence of methicillin-resistant Staphylococcus aureus significantly decreased in patients receiving ALBC (40% vs. 18%, p = 0.048). The incidence of methicillin-resistant S. epidermidis was unchanged over this time period (p = 0.6). Non-significant decreases in tetracycline and erythromycin resistance rates were also observed.
A presentation at the 2019 AAOS Annual Meeting supports the findings of the Rothman Institute (Schmitt et al. 2019). This study from Loyola University also investigated causative organisms and antimicrobial resistance patterns amongst patients treated at their academic medical center over 20 years who developed PJI.
In 32 patients with 36 cases of PJI, ALBC was not observed to significantly alter the organism causative of PJI, increase the risk of antibiotic resistance, or alter the pattern of antimicrobial resistance.
8 Alternative Local Therapy
Wound cavity administration of antimicrobial and antibiotic compounds following TKA implantation but before arthrotomy closure is an area of active research. In essence, the goal of these treatments is similar to that of ALBC which is to sterilize the wound cavity and eradicate any bacteria introduced into the wound at the time of surgery. To date, limited evidence is available regarding the efficacy of such treatments (Edmiston et al. 2018; Heckmann et al. 2019).
Most investigations promoting such treatments suffer from very small patient numbers, inadequate follow-up intervals, retrospective study design, etc., which has significantly limited the ability to draw solid statistical conclusions from these studies.
The most popular topics discussed are the use of
-
povidone-iodine soaks,
-
intra-articular application of vancomycin powder,
-
dilute chlorhexidine irrigation.
All treatments have surgical literature that both supports and refutes their ability to modify SSI incidence and there is some literature to assess their effectiveness in altering the incidence of PJI (Brown et al. 2012; Cichos et al. 2019; Hart et al. 2019; Heckmann et al. 2019; Iorio et al. 2020). All treatments have advocates and opponents whose views are largely based upon expert opinion and anecdotal experience.
Intra-articular vancomycin application following TKA was recently noted to increase the wound complication rate with no ability to decrease PJI incidence, which is contrary to literature supporting its use in hip arthroplasty and spine surgery (Dial et al. 2018; Ghobrial et al. 2015). Povidone-Iodine irrigation for THA and TKA has been widely embraced but concerns regarding its preparation and efficacy remain (Hart et al. 2019). The combination of intra-articular povidone-iodine washes followed by vancomycin powder application prior to arthrotomy closure in high-risk THA patients has recently been investigated and the authors conclude this approach has the ability to decrease PJI incidence (Iorio et al. 2020). Dilute chlorhexidine irrigation has the potential to decrease bacterial contamination of the wound but its ability to decrease PJI incidence is to date unproven (Smith et al. 2015; Frisch et al. 2017; Driesman et al. 2020).
Because the soft tissue envelope around the knee is much more tenuous than the hip, adverse tissue responses to intra-articular treatments as described above can be disastrous (Osei et al. 2016). Allergies, sensitivities, and soft tissue compromise as a result of local administration of powdered vancomycin, povidone-iodine, and chlorhexidine have all been noted albeit rare (Krautheim et al. 2004; Ghobrial et al. 2015; Su et al. 2016).
Adoption of these strategies for PJI reduction should balance their potential ability to reduce PJI against potential for sterile field compromise during preparation and complications that can be precipitated by the treatment.
Take-Home Messages
-
Hand-blended ALBC suffers from inconsistencies introduced by human error and results in PMMA that has variable elution and mechanical characteristics.
-
Commercially premixed ALBCs have a predictable, uniform release.
-
According to registry data of Australian Orthopaedic Association (2017), the use of plain cement was associated with a statistically higher rate of revision (HR = 1.06; 0 = 0.038) as compared to ALBC.
-
Because the average cost of treating one PJI is approximately $100,000 USD, the use of ALBC in this study would result in significant cost savings.
-
The frequently discussed acute renal insufficiency finding could not be replicated in subsequent sensitivity analyses and ALBC was not associated with a significant increase in the need for acute dialysis.
-
ALBC was not observed to significantly alter the organism causative of PJI, increase the risk of antibiotic resistance, or alter the pattern of antimicrobial resistance.
References
Abdel MP, Berry DJ (2019) Current practice trends in primary hip and knee arthroplasties among members of the American Association of Hip and Knee Surgeons: a long-term update. J Arthroplast 34(7S):S24–S27
Australian Orthopaedic Association (2017) Supplementary report: cement in hip & knee arthroplasty. Figure C7: Cumulative percent revision of cemented primary total knee replacement by cement type (Primary Diagnosis OA). p 13
Australian Orthopaedic Association National Joint Registry (2019a) Annual report 2019. Figure KT4: Primary total knee replacement by fixation, p 210. https://aoanjrr.sahmri.com
Australian Orthopaedic Association National Joint Registry (2019b) Annual report 2019. Figures KT34–35: Cumulative percent revision of primary total knee replacement by fixation (Primary Diagnosis OA), pp 246–249. https://aoanjrr.sahmri.com
Best AJ, Fender D, Harper WM et al (1998) Current practice in primary total hip replacement: results from the National Hip Replacement Outcome Project. Ann R Coll Surg Engl 80(5):350–355
Bohm E, Zhu N, de Guia N et al (2013) Does adding antibiotics to cement reduce the need for early revision in total knee arthroplasty. Clin Orthop Relat Res 472(1):162–168
Bozic KJ, Kurtz SM, Lau E et al (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468:45–51
Brown NM, Cipriano CA, Moric M et al (2012) Dilute betadine lavage before closure for the prevention of acute postoperative deep periprosthetic joint infection. J Arthroplast 27(1):27–30
Buchholz HW, Elson RA, Engelbrecht E et al (1981) Management of deep infection of total hip replacement. J Bone Joint Surg Br 63-B(3):342–353
Buchholz HW, Elson RA, Heinert K (1984) Antibiotic-loaded acrylic cement: current concepts. Clin Orthop Relat Res 190:96–108
Chan JJ, Robinson J, Poeran J et al (2019) Antibiotic-loaded bone cement in primary total knee arthroplasty: utilization patterns and impact on complications using a national database. J Arthroplast 34(7S):S188–S194
Chiu FY, Lin CF, Chen CM et al (2001) Cefurozime-impregnated cement at primary total knee arthroplasty in diabetes mellitus: a randomized, prospective study. J Bone Joint Surg Br 839b:691–695
Chiu FY, Chen CM, Lin CFJ, Lo WH (2002) Cefuroxime-impregnated cement in primary total knee arthroplasty; a prospective, randomized study of three hundred and forty knees. J Bone Joint Surg Am 84(5):759–762
Cichos KH, Andrews RM, Wolschendorf F et al (2019) Efficacy of intraoperative antiseptic techniques in the prevention of periprosthetic joint infection: superiority of betadine. J Arthroplast 34(7S):S312–S318
Dial BL, Lampley AJ, Green CL, Hallows R (2018) Intrawound vancomycin powder in primary total hip arthroplasty increases rate of sterile wound complications. Hip Pelvis 30(1):37–44
Driesman A, Shen M, Feng JE et al (2020) Perioperative chlorhexidine gluconate wash during joint arthroplasty has equivalent periprosthetic joint infection rates in comparison to betadine wash. J Arthroplast 35(3):845–848
Dunne N, Hill J, Mcafee P et al (2007) In vitro study of the efficacy of acrylic bone cement loaded with supplementary amounts of gentamicin: effect on mechanical properties, antibiotic release, and biofilm formation. Acta Orthop 78(6):774–785
Edmiston CE, Spencer M, Leaper D (2018) Antiseptic irrigation as an effective interventional strategy for reducing the risk of surgical site infections. Surg Infect 19(8):774–780
Eveillard M, Mertl P, Tramier B, Francois EB (2003) Effectiveness of gentamicin-impregnated cement in the prevention of deep wound infection after primary total knee arthroplasty. Infect Control Hosp Epidemiol 24(10):778–780
Ferraris S, Miola M, Bistolfi A et al (2010) In vitro comparison between commercially and manually mixed antibiotic-loaded bone cements. J Appl Biomater Biomech 8(3):166–174
Fillingham Y, Greenwald AS, Grenier J et al (2019) Hip and knee section, local antimicrobials: proceedings of international consensus on orthopedic infections. J Arthroplast 34(2S):S289–S292
Frisch NB, Kadri OM, Tenbrunsel T et al (2017) Intraoperative chlorhexidine irrigation to prevent infection in total hip and knee arthroplasty. Arthroplast Today 3(4):294–297
Gandhi R, Razak F, Pathy R et al (2009) Antibiotic bone cement and the incidence of deep infection after total knee arthroplasty. J Arthroplast 24(7):1015–1018
Ghobrial GM, Cadotte DW, Williams K et al (2015) Complications from the use of intrawound vancomycin in lumbar spine surgery: a systematic review. Neurosurg Focus 39(4):E11
Hansen EN, Adeli B, Kenyon R, Parvizi J (2014) Routine use of antibiotic laden bone cement for primary total knee arthroplasty: impact on infecting microbial patterns and resistance profiles. J Arthroplast 29(6):1123–1127
Hart A, Hernandez NM, Abdel MP et al (2019) Povidone-iodine wound lavage to prevent infection after revision total hip and knee arthroplasty: an analysis of 2,884 cases. J Bone Joint Surg Am 101(13):1151–1159
Heckmann ND, Mayfield CK, Culvern CN et al (2019) Systematic review and meta-analysis of intrawound vancomycin in total hip and total knee arthroplasty: a call for a prospective randomized trial. J Arthroplast 34(8):1815–1822
Hinarejos P, Guirro P, Leal J et al (2013) The use of erythromycin and colistin-loaded cement in total knee arthroplasty does not reduce the incidence of infection: a prospective randomized study in 3000 knees. J Bone Joint Surg Am 95(9):769–764
Iorio R, Yu S, Anoushiravani AA et al (2020) Vancomycin powder and dilute povidone-iodine lavage for infection prophylaxis in high-risk total joint arthroplasty. J Arthroplast 35(7):1933–1936
Jameson SS, Asaad A, Diament M et al (2019) Antibiotic-loaded bone cement is associated with a lower risk of revision following primary cemented total knee arthroplasty. Bone Joint Surg Br 101-B:1331–1347
Jamsen E, Huhtala H, Puolakka T, Moilanen T (2009) Risk factors for infection after knee arthroplasty. J Bone Joint Surg Am 91(1):38–47
King JD, Hamilton DH, Jacobs CA, Duncan ST (2018) Antibiotic-loaded bone cement: a systematic review of clinical results and cost implications following total knee arthroplasty. J Arthroplast 33(12):3789–3792
Krautheim AB, Jermann THM, Bircher AJ (2004) Chlorhexidine anaphylaxis: case report and review of the literature. Contact Dermatitis 50(3):113–116
Kuehn KD (2014) PMMA cement as a drug carrier in PMMA cements. Springer, Berlin/Heidelberg/New York
Kurtz SM, Ong KL, Lau E et al (2011) International survey of primary and revision total knee replacement. Int Orthop 35(12):1783–1789
Lidgren L (2001) Joint prosthetic infections: a success story. Acta Orthop Scand 72:553
Meyer J, Piller G, Spiegel CA et al (2011) Vacuum-mixing significantly changes antibiotic elution characteristics of commercially available antibiotic-impregnated bone cements. J Bone Joint Surg 93(22):2049–2056
Moran CG, Horton TC (2000) Total knee replacement: the joint of the decade. BMJ 320(7328):820
Namba RS, Chen Y, Paxton EW et al (2009) Outcomes of routine use of antibiotic-loaded bone cement in primary total knee arthroplasty. J Arthroplast 24(6S):44–47
National Joint Registry for England, Wales, Northern Ireland and the Isle of Man (2019) Table 3.26: Kaplan-Meier estimates of cumulative revision (95% CI) by gender, age, fixation, constraint and bearing. 16th Annual Report 2019. p 128
Neut D, van de Belt H, van Horn JR et al (2003) The effect of mixing on gentamicin release from polymethylmethacrylate bone cements. Acta Orthop 74(6):670–676
Nugent M, Wyatt MC, Frampton CM, Hooper GJ (2019) Despite improved survivorship of uncemented fixation in total knee arthroplasty for osteoarthritis, cemented fixation remains the gold standard: an analysis of a National Joint Registry. J Arthroplast 34(8):1626–1633
Osei DA, Rebehn KA, Boyer MI (2016) Soft-tissue defects after total knee arthroplasty: management and reconstruction. J Am Acad Orthop Surg 24(11):769–779
Parvizi J, Gehrke T, Chen AF (2013) Proceedings of the international consensus on periprosthetic joint infection. Bone Joint J 95-B(11):1450–1452
Price AJ, Alvand A, Troelsen A et al (2018) Knee replacement. Lancet 392(10158):1672–1682
Qadir R, Sanbir S, Ochsner JL et al (2014) Risk stratified usage of antibiotic-loaded bone cement for primary total knee arthroplasty: short term infection outcomes with a standardized cement protocol. J Arthroplast 29(8):1622–1624
Rocha de Silva R, Santos AAM, Carvalho JS Jr, Matos MA (2014) Quality of life after total knee arthroplasty: systemic review. Rev Bras Ortop 49(5):520–527
Salah KJ, Hoeffel DP, Kassim RA, Burstein G (2003) Complications after revision total knee arthroplasty. JBJS 85-A(Suppl 1):71–74
Sanz-Ruiz S, Matas-Dies JA, Sanchez-Somolinos M et al (2017) Is the commercial antibiotic-loaded bone cement useful in prophylaxis and cost saving after knee and hip joint arthroplasty? The transatlantic paradox. J Arthroplast 32(4):1095–1099
Sanz-Ruiz P, Matas-Diez JA, Villanueva-Martínez M et al (2020) Is dual antibiotic-loaded bone cement more effective and cost-efficient than a single antibiotic-loaded bone cement to reduce the risk of prosthetic joint infection in aseptic revision knee arthroplasty? J Arthroplast 35(12):3724–3729. https://doi.org/10.1016/j.arth.2020.06.045
Schiavone Panni A, Corona K et al (2016) Antibiotic-loaded bone cement reduces risk of infections in primary total knee arthroplasty? A systematic review. Knee Surg Sports Traumatol Arthrosc 24(10):3168–3174
Schmitt D, Killen C, Murphy M et al (2019) The impact of antibiotic-loaded bone cement on antibiotic resistance in periprosthetic knee infections. AAOS Annual Meeting. Las Vegas, 12–16 March 2019; Abstract 3595
Smith DC, Maiman R, Schwechter EM et al (2015) Optimal irrigation and debridement of infected total joint implants with chlorhexidine gluconate. J Arthroplast 30(10):1820–1822
Squire MW, Ludwig BJ, Thompson JR et al (2008) Premixed antibiotic bone cement: an in vitro comparison of antimicrobial efficacy. J Arthroplast 23(6):1104
Starnes BW (2013) A surgeon’s perspective regarding the regulatory, compliance, and legal issues involved with physician-modified devices. J Vasc Surg 57(3):829–831
Su D, Zhao H, Hu J et al (2016) TRPA1 and TRPV1 contribute to iodine antiseptics-associated pain and allergy. EMBO Rep 17(10):1422–1430
Tucker A, Hegarty P, Magill PJ et al (2018) Acute kidney injury after prophylactic cefuroxime and gentamicin in patients undergoing primary hip and knee arthroplasty – a propensity score-matched study. J Arthroplast 33:3009–3015
Wang J, Zhu C, Cheng T et al (2013) A systematic review and meta-analysis of antibiotic-impregnated bone cement use in primary total hip or knee arthroplasty. PLoS One 8(12):e82745
Zhang J, Zhang XY, Jiang FL et al (2019) Antibiotic-impregnated cement for preventing infection in patients receiving primary total hip and knee replacement. Medicine (Baltimore) 98(49):e18068
Zhou Y, Li L, Zhou Q, Yuan S et al (2015) Lack of efficacy of prophylactic application of antibiotic-loaded bone cement for prevention of infection in primary total knee arthroplasty: results of a meta-analysis. Surg Infect 16(2):183–187
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer-Verlag GmbH, DE, part of Springer Nature
About this chapter
Cite this chapter
Squire, M.W. (2022). Antibiotic-Loaded Bone Cement: Pro. In: Hansen, E., Kühn, KD. (eds) Essentials of Cemented Knee Arthroplasty. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-63113-3_46
Download citation
DOI: https://doi.org/10.1007/978-3-662-63113-3_46
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-63112-6
Online ISBN: 978-3-662-63113-3
eBook Packages: MedicineMedicine (R0)