Abstract
Posterior shoulder dislocation makes 2–5% of all shoulder dislocations. This injury is very often overlooked or misdiagnosed resulting in severe disability. This article describes general approach to the patients with first time shoulder trauma resulting in posterior dislocation. An overview of clinical picture, imaging, and indications for conservative treatment indications of PSD (posterior shoulder dislocation) is presented.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Posterior dislocation of the shoulder
- Subluxation
- Conservative treatment
- Inverted Hill–Sacks
- Posterior instability
1 Introduction
This chapter describes the general approach to the patients with first-time shoulder trauma resulting in posterior dislocation or temporary posterior dislocation (subluxation) of the shoulder. Fracture dislocation or MDI is not considered. Clinical picture, examination diagnosis, and conservative treatment of posterior dislocation (PSD) are presented.
Full posterior dislocation of the shoulder joint (PSD) without fracture of the humeral head or glenoid is an extremely sparse case. Much more often in our practice, we deal with patients after an episode of sprain or subluxation and spontaneous reposition of dislocated humeral head. Posterior dislocation is usually associated with a fractured head of the inverted Hill–Sacks type [1] (McLaughlin lesion), some with subscapularis insertion lesion, and damage to the posterior–inferior acetabular labrum. Concomitant neurovascular or rotator cuff lesions are much less common after posterior dislocation compared to anterior dislocation [2, 3].
The spectrum of dislocation varies from acute to chronic traumatic dislocation, irreducible dislocation and in conjunction with proximal fractures of the humerus.
Usually, the cause of a posterior dislocation of the shoulder is a direct or indirect trauma to the anterior side of the shoulder, for example, in contact sports or falls on the adducted and extended arm in internal rotation. Electric shock or epilepsy may also create extreme muscle contraction with flexion, adduction, and internal rotation of the affected arm. These are pathognomonic factors of the posterior shoulder dislocation.
Considering the above, we will decrease the probability of overlooking the shoulder joint damage, which may lead to subsequent posterior instability and early degenerative changes.
2 Initial Assessment
Anamnesis:
-
High-energy direct or indirect trauma to the anterior side of the shoulder (e.g., contact sports) or.
-
fall on the adducted and extended arm in internal rotation (e.g., cycling or skiing accidents),
-
shoulder cluck or “out-of-the-socket experience”,
-
electric shock or epilepsy seizures, usually bilateral,
These are pathognomonic factors of the posterior shoulder dislocation.
Clinical picture of a patient with existing posterior dislocation of the shoulder joint:
-
very painful,
-
the shoulder may be swollen (hematoma) and its shape has changed,
-
the shoulder is put forward and high,
-
the scapula usually is rotated and leans forward to decrease pain and tension,
-
the humeral head may be visible posteriorly in skinny patients,
-
the coracoid is more prominent,
-
the arm in characteristic internal rotation (10–60°) and adduction,
-
the arm seems to be fixed in above-described position,
-
no active nor passive motion, especially external rotation is possible,
-
no ability to supinate the forearm when the arm is in flexion,
Clinical picture of a patient without existing posterior dislocation of the shoulder joint (after subluxation or dislocation with subsequent reposition):
-
less pain,
-
the shoulder may be swollen (hematoma) and its shape has changed,
-
the shoulder is leveled,
-
the scapula in normal position on the ribcage,
-
the humeral head in place,
-
the coracoid normal,
-
the arm in neutral rotation and some abduction,
-
the arm may be moved whilst hanging freely by doctor on examination,
-
active or passive motion is possible to some extent,
-
supination the forearm is possible with arm in flexion.
The main symptom is loss of movement of the affected shoulder, particularly external rotation.
3 Emergency
Immediate immobilization with simple, Velpeau or Desoult sling and painkillers.
4 Imaging
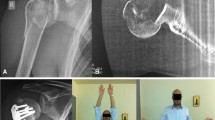
The cause of overlooking PSD by the physician is a failure to suspect the diagnosis and insufficient radiographic investigation. The key to diagnosis of this injury is to obtain proper X-ray. Diagnosis must be confirmed by two orthogonal X-rays of the affected shoulder joint, for example, anteroposterior (AP) and axial views. If the axial view is difficult to obtain due to abduction limitations and pain, the Y scapular or Velpeau view should be taken. I recommend an a–p view in internal rotation, which may reveal flattening of the humeral head at the subscapularis insertion (Fig. 29.1).
According to Wu Xu, only 11.4% cases of PSD were confirmed by AP radiographs only, but if axillary or Y view radiographs were taken at the initial investigation, the diagnosis was confirmed in all patients [4]. Ultrasound, CT, or MRI should also be considered if available.
Closed reduction of the dislocation should be attempted immediately under sedation, often successful, or under general analgesia with muscle relaxants [5]. The method of lateralization and ventralization of the humeral head, using the surgeon’s arm as a fulcrum is most commonly used. Alternatively an elevation of the internally rotated arm with longitudinal traction, is applied [6].
If closed reduction is not possible, additional imaging should be performed.
CT scan allows to asses the size of osteochondral impression fracture of the ventromedial articular surface of the humeral head (reversed Hill–Sacks lesion) and a state of the labrum or the bony glenoid rim [2, 7].
If PSD is not locked and reposition of the humeral head have been achived and stable, with defect of no more then 25% of the articular surface of the humeral head, patient can be treated by conservative methods.
An imperative condition to decide of nonoperative treatment is a stable joint after closed reduction. Patient has to be informed of long-term results, possible instability, or reconstructive surgery if necessary in case conservative management fails.
It is recommended to perform magnetic resonance imaging (MRI) after reposition of the joint, as it allows the assessment of soft tissues, with hematoma serving as a natural “contrast,” just like in artroMRI (Fig. 29.2).
This examination may unveil labral and chondral lesions, small fragment avulsion fractures of the subscapularis muscle tendon insertion, LHBT instability, or other rotator cuff pathology.
CT or MRI also may give important clues for possible residual posterior shoulder instability due to existing dysplasia, retroversion, or inclination of the glenoid (Figs. 29.3 and 29.4).
Coexisting neurovascular injuries or lesions of the rotator cuff occur much rarely after posterior dislocation. However, high-energy trauma to the shoulder often involves traction injury to the brachial plexus, which may be not seen at the initial examination.
This may be recognized later as a scapular dyskinesis, limb weakness, or proprioceptive position disorder, and thus compromise and extend the improvement process of rehabilitation up to the time of full brachial plexus recovery.
5 Aftercare
The arm should be immobilized for 6 weeks in neutral to 20° of internal rotation in abduction ER orthosis. This position ensures optimal healing conditions for the attachment of the subscapular muscle tendon and also is probably the best for healing damaged posterior capsule and labrum.
In case of patients with confirmed retroversion of the glenoid (CT or MRI), adequate correction of external rotation should be considered.
6 Rehabilitation
General rules of shoulder rehab apply. Rehabilitation plays a crucial role in maximizing the functional outcome. In the early phases of rehabilitation, it is necessary to protect the joint to allow healing. Pendulum movements of the shoulder to certain ranges of motion in sagittal plane are allowed. Orthosis/sling is removed only for rehabilitation exercises.
Isometric RC and scapular stabilizers strengthening exercises are introduced as soon as possible with pain settlement. Elbow, forearm, wrist and scapular active ROM exercise program, with emphasis on postural exercises, is introduced despite the use of an orthosis. Here, PowerBall and Swing Stick may be implemented, as these devices that allow muscle strengthening and proprioceptive training without changing position of the shoulder itself.
No shoulder internal rotation past neutral for 6 weeks and no shoulder internal rotation with abduction for 8 weeks.
Cardiovascular fitness has to be preserved: walking, stationary bike, avoid running and jumping until at least 8 weeks. Swimming breaststroke at 3–4 months.
Stretching of the posterior capsule (by internal rotation) avoided for 4 months.
Return to full activities is allowed at 6–8 months.
References
McLaughlin HL. Posterior dislocation of the shoulder. J Bone Joint Surg Am. 1952;24(3):584–90.
Roberts A, Wickstrom J. Prognosis of posterior dislocation of the shoulder. Acta Orthop Scand. 1971;42(4):328–37.
Mestdagh H, Maynou C, Delobelle JM, Urvoy P, Butin E. Traumatic posterior dislocation of the shoulder in adults. Apropos of 25 cases. Ann Chir. 1994;48(4):355–63.
Wu X, et al. Neglected posterior dislocation of the shoulder: a systematic literature review. J Orthop Translat. 2015;3(2):89–94.
Cicak N. Posterior dislocation of the shoulder. J Bone Joint Surg Br. 2004;86-B:324–32.
Benedikt S. Locked posterior shoulder dislocation: treatment options and clinical outcomes. Arch Orthop Trauma Surg. 2011;131:1127–34. https://doi.org/10.1007/s00402-011-1310-9.
Ovesen J, Söjbjerg JO. Posterior shoulder dislocation. Muscle and capsular lesions in cadaver experiments. Acta Orthop Scand. 1986;57(6):535–6.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 ESSKA
About this chapter
Cite this chapter
Surdziel, P.H. (2020). Conservative Treatment in Posterior Dislocation. In: Brzóska, R., Milano, G., Randelli, P., Kovačič, L. (eds) 360° Around Shoulder Instability. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-61074-9_29
Download citation
DOI: https://doi.org/10.1007/978-3-662-61074-9_29
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-61073-2
Online ISBN: 978-3-662-61074-9
eBook Packages: MedicineMedicine (R0)