Abstract
The anatomy of the glenohumeral joint allows for a wide range of motion at the expense of stability. It is the most commonly dislocated joint of the human body. The risk for instability is greatest in overhead sports and collision sports, especially football, rugby, and wrestling. While not a true collision or overhead sport, basketball necessitates physical contact and frequent overhead movements, which can lead to an increased risk of shoulder instability. After an instability event, the treating physician must help the patient decide between nonoperative and operative management. Many variables contribute to this decision, including the age of the patient, duration of symptoms, type of instability, number of instability events, radiological findings, and timing of the injury (i.e., in season or out of season). In general, operative treatment reduces recurrence rates while increasing successful return to play compared to conservative treatment. Therefore, operative management tends to be the preferred approach, especially in young athletes. The following chapter will provide a comprehensive review on shoulder instability in the basketball athlete with a special focus on diagnosis, management, and rehabilitation for successful return to play.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Anatomy: The shoulder is a ball and socket joint that allows for the largest arc of motion of any joint in the human body. This wide range of motion comes at the expense of decreased stability. The delicate balance between motion and stability is achieved by the intricate anatomy of the glenohumeral joint, including both static and dynamic stabilizers [1,2,3]. Bony static stabilizers include the glenoid, humeral head, and the proximal humerus. The articular conformity of the glenohumeral joint is relatively poor compared to other ball and socket joints. The glenoid is pear-shaped with the inferior aspect forming a true circle [4]. Contrarily, the humeral head is shaped like a sphere and has three times the surface area of the glenoid with only 25–30% of the humeral head articulating with the glenoid at any given position [3]. This poor bony congruency highlights the need for appropriately functioning soft tissue stabilizers about the shoulder joint.
Soft tissue static stabilizers include the glenoid labrum, glenohumeral ligaments, joint capsule, and negative intra-articular pressure. The labrum is a triangular rim of fibrocartilaginous tissue that deepens the glenoid articulation and increases shoulder stability by 10% [5, 6]. The capsular attachments to the labrum, known as the capsulolabral junction, adds further static stability to the glenohumeral joint. The most important components of the shoulder capsule are the glenohumeral ligaments. Each ligament provides static stability in addition to secondary dynamic stability based on the position of the shoulder. The inferior glenohumeral ligament (IGHL) is the most important ligament when considering anteroinferior and posteroinferior instability of the shoulder. The IGHL has an anterior and posterior band with a capsular bridge that acts like a “hammock” around the inferior proximal humerus (Fig. 24.1) [2, 7, 8]. The posterior band helps resist posterior instability by tightening when the arm is in the adducted, flexed, and internally rotated position. Conversely, the anterior band resists anteroinferior instability with the arm in the flexed, abducted, and externally rotated position. When the capsule and glenohumeral ligaments are intact, a negative-pressure “vacuum effect” is created, which further contributes to static stability of the shoulder [9, 10].
Dynamic stabilizers of the glenohumeral joint include the rotator cuff, deltoid, and long head of the biceps tendon. The rotator cuff is the most important dynamic stabilizer. It acts as a dynamic compressor of the humeral head against the glenoid, especially during the initiation of glenohumeral movement. Furthermore, direct attachment of the rotator cuff to the capsule increases articular tension while providing proprioceptive feedback [11, 12].
Pathoanatomy: The Bankart lesion is an anteroinferior labrum tear and is the classic, pathognomonic lesion of anterior shoulder instability. It was first described in 1923 by the English surgeon Arthur Bankart in his report of four cases that each demonstrated this lesion [13]. He stated that “the head shears off the fibrous capsule of the joint from its attachment to the fibro-cartilaginous glenoid ligament. The detachment occurs over practically the whole of the anterior half of the glenoid rim.” Bankart also acknowledged the importance of capsular laxity but maintained that the capsulolabral injury is the sentinel pathologic lesion of anterior shoulder instability, and this concept has largely stood the test of time.
Since its original description, variations of the Bankart lesion have been identified as well. A “bony Bankart” refers to a Bankart lesion that includes an associated anteroinferior glenoid fracture that becomes detached with the torn labrum. Another variation is the anterior labral periosteal sleeve avulsion (ALPSA) lesion, which occurs when a sleeve of the glenoid periosteum peels off with the Bankart lesion.
As described by Bankart, the anterior capsule and specifically the IGHL become injured and stretched during an anterior dislocation. In severe cases, the IGHL can become detached from its humeral attachment, known as a humeral avulsion of the inferior glenohumeral ligament (HAGL) lesion. This is a severe finding that necessitates surgical management, which will be discussed further in the treatment section. During an anterior dislocation, a Hill-Sachs lesion often develops, which is an impaction injury to the posterior humeral head from contact against the anterior glenoid.
The posterior side of the shoulder is slightly different in its pathoanatomy compared to the anterior side. A traumatic posterior dislocation can result in a labrum tear with an associated capsular injury. However, subtle posterior instability from repetitive trauma is more common because the posterior band of the IGHL is typically not as thick as the anterior band. Since ligamentous support of the posterior capsule is thinner and weaker compared to the more robust anterior side, repetitive trauma may alter the elasticity of the capsule, resulting in a more subtle instability pattern highlighted by capsular laxity.
Spectrum of Instability: Shoulder instability includes a broad spectrum of clinical presentations. Athletes may present after a complete dislocation, subluxation, or subtle micro-instability from repetitive trauma. A complete dislocation occurs when the humeral head no longer articulates with the glenoid surface and remains completely non-articulating. A full dislocation invariably requires the shoulder to be relocated with a reduction maneuver, which may be performed manually by the athlete or by a certified health professional. A subluxation is a partial dislocation that auto-reduces before full dislocation can occur. Athletes will often report a sliding sensation in his or her shoulder but will deny feeling the shoulder locked in a dislocated position. Subtle micro-instability from repetitive trauma usually does not have a traumatic mechanism. Instead, patients will report a gradual sensation of pain and/or not trusting the shoulder because of apprehension despite denying a true dislocation or subluxation event.
Epidemiology: Anterior shoulder instability most commonly occurs in the young and athletic population. Males have a much higher rate of shoulder instability compared to females with most studies reporting a 70–85% male predominance [14,15,16]. The incidence of anterior shoulder instability has been estimated between 8 and 23.9 per 100,000 person-years [17, 18]. This can be higher in athletes who participate in collision sports, including football, rugby, wrestling, and overhead throwing sports. Moreover, the incidence in military personnel has been estimated as 1.69 per 1000 person-years, which is even higher than contact athletes [17]. Owens et al. investigated 4080 glenohumeral instability events in National Collegiate Athletic Associate (NCAA) athletes during a 15-year period [15]. They reported an incidence of 0.12 injuries per 1000 athlete exposures. Dislocations were more likely to occur in male athletes (relative risk 2.67) and during collegiate games as opposed to practice (relative risk 3.50). More than 10 days of time lost from sport occurred after 45% of instability events.
Only a few studies have reported the epidemiology of shoulder instability in high-level basketball players. Recent studies have highlighted that basketball players have an increased risk of shoulder instability compared to many sports. This risk is often underappreciated because basketball is not considered a true contact or overhead sport. However, basketball necessitates low-velocity contact while performing frequent overhead maneuvers, leaving players in a potentially vulnerable position for shoulder injury. Recently, the Multicenter Orthopaedic Outcomes Network (MOON) Shoulder Instability Group investigated 863 patients after surgical management for primary shoulder instability [14]. They found that 709 patients (82%) were male and the average age was 24 years old. The primary direction of instability was anterior in both male (74%) and female (73%) patients, and posterior instability accounted for 23% of cases. The rate of shoulder dislocation requiring formal closed reduction was highest among male patients less than 20 years old. Moreover, a labrum tear (66%) and Hill-Sachs lesion (41%) were the most frequent concomitant injuries. Trauma from playing sports was the mechanism of injury for 644 patients (75%), and basketball was the second most common sport in which primary shoulder instability occurred, accounting for 13% of all dislocations.
Another recent epidemiological study by Kraeuter et al. compared rates of shoulder instability in high school and college athletes and found basketball to be a high-risk sport for shoulder instability, especially in college athletes [19]. Both male and female college basketball players had a significantly higher risk of shoulder dislocation (relative risk 2.99 and 2.28, respectively) compared to high school basketball players. Player to player contact was the most common mechanism, and dislocations were just as likely to occur in practice or competition.
An epidemiological database study of National Basketball Association (NBA) injuries found that shoulder instability accounted for 57 injuries over a 17-year period, which was only 0.5% of all injuries reported [20]. This seemingly low number is likely due to the extremely high rate of other, more common musculoskeletal injuries in basketball players, including lateral ankle sprains, patellofemoral inflammation, lumbar strains, and hamstring strains. Furthermore, NBA players are elite athletes that likely have the muscle strength, coordination, and proprioception to minimize shoulder instability compared to amateur basketball players. Nonetheless, Minhas et al. investigated the most common orthopedic procedures performed on NBA players and found shoulder instability surgery (46 cases) to be the fourth most frequent surgery performed, accounting for 13.2% of all cases [21].
Fact Box
-
The shoulder joint is a minimally constrained ball and socket joint that allows for a wide range of motion at the expense of stability.
-
The anteroinferior labrum and anterior band of the IGHL are the most commonly injured structures after an anterior instability event.
-
Shoulder instability occurs along a broad clinical spectrum, including complete dislocation, partial dislocation (i.e., subluxation), and repetitive micro-trauma.
-
Basketball necessitates low-velocity contact and frequent overhead movements, placing these athletes at a higher, often underappreciated, risk for shoulder instability.
2 Diagnosis
Evaluation of an athlete with shoulder instability should begin with a comprehensive history. Determining the type of instability event (i.e., dislocation, subluxation, or repetitive micro-trauma) is extremely important. The patient can often provide valuable information that will help the physician determine the exact nature of the instability event. The physician should always ask if the patient required a shoulder reduction, and if so, how the reduction was performed and who performed the reduction. The patient should also be asked how long the shoulder remained dislocated until the reduction was performed. Hand dominance, history of index injury, mechanism of injury, position of the shoulder at the time of injury, competitive level, position played, number of previous instability events, and goals for return to play should be assessed. Furthermore, the physician should document any other history of contralateral shoulder instability events or previous surgeries to either shoulder.
After acquiring the entire relevant history, a complete, detailed neurologic examination of both upper extremities should be performed. The examination should begin with inspection for any swelling or obvious deformity. Palpation of the entire shoulder girdle can reveal a concomitant injury to the sternoclavicular (SC) joint, acromioclavicular (AC) joint, clavicle, or proximal humerus. A concomitant fracture can accompany a shoulder dislocation in up to 18% of anterior shoulder dislocations [22]. Next, the examiner should assess both active and passive range of motion of the shoulder in forward flexion, abduction, internal rotation, and external rotation. Rotator cuff strength testing should be performed and any weakness should raise suspicion for possible rotator cuff tear or nerve injury. In a recent review, the incidence of axillary nerve injury after shoulder dislocation varied from 3.3% to 40% with most of the injuries being neuropraxic injuries that resolved spontaneously without special intervention [23, 24]. Every patient should also be assessed for hyperlaxity by testing for a sulcus sign and assessing Beighton’s criteria. Special tests should be performed last, including the apprehension test, Jobe relocation test, load and shift test, anterior jerk test, and posterior jerk test. The apprehension test and Jobe relocation test are particularly useful exam maneuvers when assessing anterior instability. A positive apprehension test is particularly useful as it has demonstrated a 96% positive predictive value for a Bankart tear [25].
While anterior instability is a relatively straight forward diagnosis, posterior instability can be more challenging because of its often-subtle presentation. Posterior instability has a wide spectrum of clinical manifestations from subtle subluxation to prominent dislocation. Symptoms include pain, inability to fully participate in athletic events, and inability to reach desired level of activity. Unlike patients who experience anterior instability, patients with posterior instability often present with a chief complaint of posterior shoulder pain as opposed to shoulder instability. Therefore, posterior instability can be an often-overlooked diagnosis. Whenever an athlete reports posterior shoulder pain during physical activity that loads the shoulder joint, a diagnosis of posterior instability should be considered. The diagnosis is often confirmed by provocative exam maneuvers, including the posterior jerk test, Kim test, posterior stress test, and the load and shift test [26, 27]. There is a 97% sensitivity to diagnose posterior instability when the Kim test and the jerk test are both positive [27].
Basic and advanced imaging of the affected shoulder should complement the history and physical examination. Any pre- and post-reduction shoulder radiographs must be reviewed. A radiographic shoulder series should include at least a true AP, scapular Y, and axillary views. Additional views, including a Stryker notch and West Point view, can provide further details on Hill-Sachs lesions and Bankart lesions, respectively. Magnetic resonance imaging (MRI) with or without arthrogram should be obtained to further evaluate the shoulder joint and any concomitant pathology. We prefer a non-arthrogram study at our institution to avoid distorting any injured structures in or around the shoulder joint. Special attention should be paid to the glenoid labrum, capsule, IGHL, and rotator cuff when evaluating the MRI. In the setting of a large, bony Bankart lesion or glenoid bone loss, a computed tomography (CT) scan should be obtained to better assess any bony deficiencies. A three-dimensional CT reconstruction of the glenoid and humerus can be particularly helpful in visualizing bone loss on both the glenoid and proximal humerus [28].
By paying careful attention to the patient’s history, physical examination, and imaging findings, the treating physician can make an accurate diagnosis. Once the correct diagnosis is determined, the physician can formulate a treatment plan that allows the athlete to safely return to sport with as little time lost from competition as possible. This will be the focus of the remaining sections.
Fact Box
-
Evaluation of a basketball athlete with shoulder instability should begin with a complete history, including descriptions of previous and current shoulder injuries.
-
The physical examination should start with painless, benign maneuvers and progress to more invasive, special testing at the end of the exam.
-
All basketball athletes should be asked about and tested for hyperlaxity at the time of evaluation as hyperlaxity is quite common in this population.
-
Advanced imaging is recommended for all patients to better appreciate the injury pattern and to help develop a treatment plan.
3 Treatment
The decision for how to treat a basketball player with shoulder instability is dependent on many factors, including the player’s age, level of competition, position, time of season, and history of previous dislocations. Educating the patient about various treatment options and mutual decision-making is important for successful treatment. The pros and cons of both nonsurgical and surgical management should be discussed with the patient and his or her family. It is imperative that the physician provides adequate information so an informed decision can be made. Elite athletes may have more complicated personal circumstances, including contract status, monetary incentives, and organizational expectations. Regardless, the physician should not be swayed by these additional factors. Instead, the focus should remain on helping the patient make the best decision that will optimize effective return to play and preserve the long-term health of his or her shoulder.
Regardless of the patient’s level of play, the physician’s first responsibility is the well-being of the patient, which requires choosing a treatment plan that reduces the risk of future instability events. While once regarded as a relatively benign event, a recurrent shoulder dislocation often causes further harm to the shoulder joint, including increased glenoid and humeral bone loss, worsening labrum tears, and increased capsular stretch [29, 30]. This can complicate the treatment algorithm and dictate more of a salvage-type procedure in the primary setting, which limits future options if the patient were to have a complication or fail primary surgery.
The first major decision to make is whether to choose nonoperative or operative management. If operative management is chosen, the next major decision is choosing the appropriate surgical procedure, i.e., arthroscopic Bankart repair, open Bankart repair, or a glenoid bone augmentation procedure, such as the Latarjet procedure. The rest of the section will focus on indications and results of the various treatment options for shoulder instability in basketball athletes.
Nonsurgical Management: Nonoperative treatment for shoulder instability has shown considerable variability in its effectiveness and remains controversial in the athletic population [15, 31,32,33,34,35]. Conservative management entails an initial period of brief sling immobilization (3–7 days) followed by a graduated physical therapy program focused on regaining shoulder range of motion and strength before returning to sport-specific drills [32, 36, 37]. Return to play is allowed once the patient demonstrates full, pain-free range of motion with full protective strength and no apprehension on physical exam. This usually takes 3–6 weeks but occasionally up to 8 weeks depending on the type of instability pattern [38]. A restrictive brace can be used by the athlete when returning to play, which can provide extra support to the shoulder and limit the athlete’s ability to place the arm in a vulnerable position. While bracing is a common practice because it provides subjective improvement in stability, there is no clinical evidence to support its use in preventing recurrent instability [33]. Furthermore, it is our experience that many basketball players find such a brace too restrictive and often decide against wearing one during competition.
The success of conservative management is extremely variable following a first-time, traumatic shoulder dislocation. While conservative management has the potential benefits of avoiding surgery and returning an athlete to play during the same season, it does have a significant risk of sustaining a recurrent instability event. This should not be overlooked and must be heavily considered by the treating physician because each recurrent dislocation risks further damage to the shoulder joint.
Age at the time of dislocation is one of the most important risk factors in determining the success of conservative treatment [34, 39,40,41,42]. Sachs et al. demonstrated that age under 25 years is a significant risk factor for re-dislocation following primary anterior shoulder instability [40]. Marans et al. revealed a 100% recurrent dislocation rate in adolescents treated with sling immobilization for 6 weeks [41]. This is consistent with a study from the United States Military Academy that reported a 92% recurrence rate in young athletes following conservative management [34]. Hovelius et al. reported a recurrence rate of 27% in patients older than 30 years but a 72% recurrence rate in athletes younger than 23 years, suggesting that appropriately chosen patients above the age of 30 may be amenable to nonoperative management [42]. Buss et al. showed an 86% return to sport rate without sling immobilization in a group of competitive high school and collegiate athletes, but 37% of the athletes experienced at least one recurrent instability event [32]. These athletes missed an average of 10.2 days (range 0–30 days) of sports participation with 27 of 30 athletes returning to play within 2–3 weeks.
Dickens et al. found that 73% of NCAA athletes were able to return to sport after an instability episode at a median of 5 days after injury [33]. However, 63% had a recurrent dislocation after returning to play. They found that athletes with a subluxation were 5.3 times more likely to return to sport compared to athletes with a dislocation. Similarly, Shanley et al. recently found that high school athletes who sustained a subluxation were three times more likely to successfully return to sport without recurrent instability after conservative management compared to athletes who sustained a dislocation [43].
Another study by Dickens et al. found that only 40% of athletes successfully returned to play without recurrence during a subsequent season following shoulder dislocation compared to 90% of athletes who successfully returned after surgical repair [33]. Athletes were 5.8 times more likely to successfully return for the following season after surgical repair. Return to play rates were the same between athletes who sustained one or multiple in-season dislocation events.
A recent meta-analysis of randomized clinical trials found a 52.9% re-dislocation rate after conservative management compared to a 7.9% re-dislocation rate after surgical repair [44]. They also found that arm position during immobilization (e.g., external rotation versus internal rotation) had no effect on re-dislocation rates.
It is our experience that the age of the athlete, physical exam findings, number of previous dislocations, competitive level, and timing within a season are the most important factors to consider when weighing the option of nonoperative management after a primary shoulder dislocation. Only patients who are at a low risk for recurrent dislocation should be indicated for possible conservative management. Therefore, the indications for conservative management are very narrow and include very young patients (i.e., age 10–13), a first-time dislocation, less than 10% glenoid bone loss, intact rotator cuff, and a non-engaging Hill-Sachs lesion. Relative indications for nonoperative management include recreational basketball players over the age of 30 who meet the above criteria and are willing to modify their activities during a trial of conservative management. The role of conservative management is less clear for athletes between the ages of 20 and 30. The recurrence rate for athletes younger than 30 after conservative treatment is three times higher than those having surgical repair [45, 46]. Similarly, we have found that athletes in this controversial age range are usually best treated surgically unless the patient is a casual, recreational player with a first-time dislocation who is willing to modify activities.
Conservative management is a particularly appealing option when a high-level athlete experiences a dislocation in the first half of a season since surgery would require missing the entire season. However, managing an isolated in-season dislocation in the elite athlete remains controversial with no clear guidelines available in the literature. Each case should be managed individually based on the athlete’s history, physical exam, imaging findings, and individual circumstances. Avoiding a lost season should not be the main motivator when managing an athlete after an in-season dislocation.
Contraindications to conservative management include age under 20 years old, presence of a concomitant operative injury such as rotator cuff tear or HAGL lesion, greater than 15% glenoid bone loss, history of more than one dislocation, generalized hyperlaxity, marked apprehension on physical exam, or failure to return to sport after previous conservative management. A decision-making algorithm for conservative management is presented in Fig. 24.2.
Surgical Management: Early operative treatment for anterior shoulder instability has gained popularity as a growing amount of evidence supports a high rate of successful return to play with decreasing recurrence rates, especially in young and active athletes [38, 44, 47,48,49,50]. Many physicians now favor early operative intervention within a few weeks of the initial injury, especially when the patient is not indicated for conservative management. Absolute indications for surgical management include an associated operative injury, including >50% rotator cuff tear, HAGL lesion, >15% glenoid bone loss, >25% humeral head articular surface defect, proximal humerus fracture requiring surgery, irreducible dislocation, or non-concentric reduction. Further indications for operative management include patient age less than 20 years, greater than two dislocations, participation in overhead or contact sports, injury near the end of a season, failure of conservative management, or inability to perform sport-specific drills without apprehension.
Determining the appropriate surgical procedure for each patient is a critical decision that can heavily influence the patient’s outcome. Historically, an open Bankart repair was the procedure of choice for anterior shoulder instability. This procedure allows the surgeon to directly visualize the detached labrum and then perform a labrum repair with a formal capsular shift. As shoulder arthroscopy gained popularity, many surgeons attempted arthroscopic Bankart repair with capsulorrhaphy. An arthroscopic approach offers the advantage of preserving the subscapularis attachment and reducing postoperative stiffness, especially loss of external rotation.
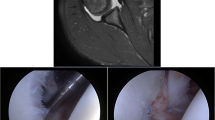
Regardless of the chosen technique, the main surgical goal is to restore normal capsulolabral anatomy. This requires (1) strong fixation of the labrum back onto the glenoid face to recreate the normal “bumper” effect of the labrum and (2) appropriate capsulorrhaphy to reduce the distorted capsular volume (Fig. 24.3). This was highlighted in a study by Speer et al., which demonstrated that isolated Bankart lesions are less likely to provoke complete dislocation unless there is a capsular injury [51].
Arthroscopic Bankart repair of a left shoulder in an 18-year-old female. (a) Identification of the Bankart lesion (arrow) and IGHL (double asterisk). (b) Placement of the arthroscopic probe into the Bankart lesion to signify adequate preparation of the labrum from the glenoid surface. (c) Bankart lesion fully prepared for fixation. (d) Insertion of initial suture tape through the labrum beneath the IGHL. (e) Placement of third suture for Bankart repair. Note that the second suture tape also captured the IGHL to achieve adequate capsular shift. (f) Final construct with labrum “bumper” effect restored with associated reduction of capsular volume. IGHL: inferior glenohumeral ligament
Initially, results following an arthroscopic repair were inferior to results after open repair, demonstrating higher re-dislocation rates [52,53,54]. However, with the evolution of advanced arthroscopic techniques and equipment, multiple modern studies have shown at least equal outcomes between open and arthroscopic Bankart repairs [48, 49, 55,56,57]. As a result, arthroscopic Bankart repair with capsulorrhaphy is now commonly the surgical method of choice for the majority of surgeons [58,59,60].
Owens et al. performed a randomized control trial comparing arthroscopic and open Bankart repair in young, competitive athletes who sustained only shoulder subluxations without any associated bone loss [61]. At 2-year follow-up, there was no difference in outcome scores or recurrent subluxation rates based on operative approach. Three patients in each group experienced recurrent subluxations and no dislocations. Outcomes scores were significantly better in patients with three or less subluxations prior to surgery compared to patients with greater than three subluxations prior to surgery, which advocates for early surgical management in this patient population.
While arthroscopic Bankart repair is a very successful surgery when performed for appropriate indications, the open Bankart repair is still a valuable surgery with distinct advantages over an arthroscopic repair, especially in the setting of chronic shoulder instability (>2 shoulder dislocations), revision stabilization surgery, collision athletes, generalized hyperlaxity, and significant capsular stretch that cannot be adequately reduced arthroscopically. In these instances, open procedures have demonstrated superior outcomes compared to arthroscopic repair [44, 62]. A recent meta-analysis by Kavaja et al. demonstrated decreased recurrence rate after open Bankart repair compared to arthroscopic repair in the setting of chronic shoulder instability (5.8% versus 13.4%, respectively) [44]. Similarly, a 2018 study by Su et al. revealed a 42% recurrent instability rate in patients who underwent a revision arthroscopic Bankart repair [62]. The presence of an engaging Hill-Sachs lesion, age less than 22 years, and ligamentous hyperlaxity were independent predictors of recurrence in their cohort.
To help stratify patients at risk for failing an arthroscopic Bankart repair, Balg and Boileau developed the Instability Severity Index Score (ISIS) to stratify a patient’s risk of failure following arthroscopic Bankart repair (Fig. 24.4) [39]. They reported the following risk factors for recurrence of instability following arthroscopic repair: age less than 20 years at the time of surgery, involvement in competitive/contact sports or those involving forced overhead activity, shoulder hyperlaxity, Hill-Sachs lesion present on anteroposterior radiograph with the shoulder in external rotation, and/or loss of the sclerotic inferior glenoid contour. This highlights that the decision to perform an open or arthroscopic repair should be largely dictated by extent of bony involvement, associated risk factors, and ultimately surgeon preference [63, 64].
The Instability Severity Index Score (ISIS) is a 10-point scale to help determine a patient’s risk for recurrent shoulder instability following arthroscopic Bankart repair. A score greater than 6 imparts a 70% chance of recurrent dislocation after arthroscopic repair (Reproduced with permission from: Balg F, Boileau P. The instability severity index score. A simple preoperative score to select patients for arthroscopic or open shoulder stabilization. J Bone Joint Surg Br. 2007;89 (11):1470–7)
In the setting of multiple dislocations, revision instability, and/or anterior glenoid bone loss greater than 15%, a glenoid bone augmentation procedure is usually the preferred treatment. The most commonly performed bone augmentation procedure is the Latarjet procedure, which transfers the coracoid process with the attached conjoint tendon to the anteroinferior glenoid. This creates a very stable construct that works through the “triple threat” mechanism of (1) glenoid bone augmentation, (2) sling effect from the conjoint tendon going over a subscapularis split, and (3) capsular shift/closure [65,66,67]. While the Latarjet procedure can be a very successful procedure, it does alter the normal anatomy and requires a steep learning curve. It also has a larger complication rate (15–30%) with a potentially more severe complication profile, including neurovascular injury, abrasion of humeral head cartilage against the bone block and screws, and bone lysis [68,69,70]. Many of these complications can be avoided with appropriate surgical experience and technique, and good patient outcomes with low recurrent instability rates are common after the Latarjet procedure [57, 67, 71,72,73,74].
Anterior glenoid augmentation with a free bone block is an alternative option in lieu of a Latarjet procedure or in the setting of a previously failed Latarjet procedure. The most commonly used bone blocks are either iliac crest autograft or distal tibial allograft [75,76,77,78]. There are multiple advantages of a free bone block procedure, including maintenance of normal coracoid anatomy and ability to salvage a failed Latarjet procedure. Drawbacks of the procedure include morbidity from iliac crest harvest, loss of the “sling effect” from the conjoint tendon, and bone block resorption, especially with allograft bone [79, 80]. In general, clinical results following glenoid augmentation with a free bone block are similar to results following a Latarjet procedure, making it a viable option in the primary or revision setting [81, 82].
In summary, we recommend meticulous assessment of each patient’s risk profile prior to selecting a surgical procedure. Most basketball athletes are amenable to an arthroscopic procedure, especially after a single shoulder dislocation [30]. Athletes who are younger or have sustained multiple instability events may warrant an open procedure depending on physical exam and imaging findings. In the setting of revision stabilization surgery or significant glenoid bone loss (>15%), a bone augmentation procedure should be performed as arthroscopic repair has demonstrated unacceptably high failure rates. A summary of surgical indications for the various procedures can be found in Fig. 24.5.
Return to Play After Surgery: Many post-surgical rehabilitation protocols allow a safe return to play following surgical correction of shoulder instability. These protocols often follow the same guidelines as conservative programs except the timeline is more prolonged to allow appropriate time for healing and return of full shoulder function. While protocols between surgeons will vary, most follow generally accepted guidelines of a graduated physical therapy program [83,84,85]. The initial phase focuses on a period of immobilization followed by pendulum exercises and isometric muscle contractions. This phase lasts about 4 weeks, at which time the athlete progresses to passive range of motion followed by active-assisted range of motion exercises without resistance. This phase also lasts approximately 4 weeks until the athlete transitions to regaining full active range of motion and progressive strength reacquisition. The final phase begins around 3 months after surgery and allows the athlete to progress with plyometric exercises, advanced upper extremity strengthening, and sport-specific exercises. Typically, the timeline for full return to play is 4–6 months, but it can take longer depending on the procedure and unique circumstances of the basketball athlete. It is our recommendation that athletes who must perform overhead movements with unplanned collisions, including basketball players, do not return to athletic competition until 6 months postoperatively.
Return to play rates following surgical shoulder stabilization are quite high with a reported rate between 63% and 93% depending on the type of athlete [14, 16, 21, 38, 47, 52]. Collision and overhead athletes are at the highest risk to experience surgical failure [86, 87]. Basketball players tend to do very well after surgical stabilization and appropriate rehabilitation. While many studies have investigated results of surgical repair for shoulder instability in contact and overhead athletes, minimal evidence is directly available for basketball players. Minhas et al. reported on 46 NBA players who underwent surgical stabilization for anterior shoulder instability [21]. They demonstrated a 93.5% return to play rate with increased games played and minimal change in post-injury player efficiency rating compared to players who underwent lower extremity surgery.
Fact Box
-
The decision for nonsurgical versus surgical management is made based on a patient’s history, physical examination, imaging findings, and overall risk factors for recurrent instability.
-
Young age (less than 20 years old), athletic participation that requires contact or overhead movements (including basketball), glenoid bone loss, and history of previous shoulder instability are significant risk factors for recurrent instability.
-
Conservative management after a shoulder dislocation is not recommended for most basketball athletes. The high incidence of contact in vulnerable overhead arm positions in basketball makes nonoperative management usually doomed to failure.
-
Surgical management for shoulder instability is the preferred treatment in young, competitive basketball players. Early surgical intervention is key to prevent additional dislocations in this population.
-
Arthroscopic Bankart repair is the most commonly performed procedure for primary, traumatic shoulder instability and allows minimally invasive restoration of normal shoulder anatomy.
-
Open Bankart repair or Latarjet procedure are the preferred treatments of choice in the setting of revision surgery or chronic shoulder instability. When there is glenoid bone loss >15% or an engaging Hill-Sachs lesion, then a bone augmentation procedure should be performed.
-
Postoperative rehabilitation protocols focus on an initial period of immobilization followed by gradual regaining of the athlete’s range of motion, strength, and ultimately sports performance.
-
Return to play rates are very high following surgical treatment, and most basketball athletes can return to full sports participation by 6 months postoperatively though timelines vary based on individual circumstances.
4 Conclusions
Shoulder instability is a common problem encountered by physicians who treat injured athletes. Basketball is a unique sport that allows for low-velocity contact with the arm in an overhead position. Therefore, basketball athletes are at higher risk for shoulder instability. Recognizing the pattern of shoulder instability from the athlete’s history, physical examination and imaging findings are the first steps in successful management. Understanding that the natural history of shoulder instability is a high propensity for recurrent dislocation, especially in the young athlete, is another vital component to developing a successful treatment plan. Surgical management is often the most appropriate treatment choice, especially in the young basketball player. Choosing the best surgical procedure is based on the patient’s age, number of previous dislocations, and presence or absence of glenoid bone loss. Return to play can usually occur within 6 months postoperatively. After appropriate treatment, basketball athletes can expect a high return to play rate at the previous level of competition.
References
Murray IR, Goudie EB, Petrigliano FA, Robinson CM. Functional anatomy and biomechanics of shoulder stability in the athlete. Clin Sports Med. 2013;32(4):607–24.
O’Brien SJ, Neves MC, Arnoczky SP, Rozbruck SR, Dicarlo EF, Warren RF, et al. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18(5):449–56.
Codman E. Tendinitis of the short rotators. In: The shoulder: Rupture of the suprasìnatus tendon and other lesions in or about the subacromial bursa. Boston: Thomas Todd; 1934. p. 78–215. https://scholar.google.at/scholar?q=E.A.+Codman+(Ed.),+The+shoulder,+rupture+of+the+supraspinatus+tendon+and+other+lesions+in+or+about+the+subacromial+bursa,+Krieger+Publishing,+Malabar,+FL+(1934),+pp.+313–331&btnG=&hl=de&as_sd.
Huysmans PE, Haen PS, Kidd M, Dhert WJ, Willems JW. The shape of the inferior part of the glenoid: a cadaveric study. J Shoulder Elb Surg. 2006;15(6):759–63.
Howell SM, Galinat BJ. The glenoid-labral socket. A constrained articular surface. Clin Orthop Relat Res. 1989;(243):122–5. http://www.ncbi.nlm.nih.gov/pubmed/2721051.
Halder AM, Kuhl SG, Zobitz ME, Larson D, An KN. Effects of the glenoid labrum and glenohumeral abduction on stability of the shoulder joint through concavity-compression: An in vitro study. J Bone Joint Surg Ser A. 2001;83(7):1062–9.
Burkart AC, Debski RE. Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthop Relat Res. 2002;(400):32–9. http://www.ncbi.nlm.nih.gov/pubmed/12072743
Itoigawa Y, Itoi E. Anatomy of the capsulolabral complex and rotator interval related to glenohumeral instability. Knee Surg Sports Traumatol Arthrosc. 2016;24:343–9.
Habermeyer P, Schuller U, Wiedemann E. The intra-articular pressure of the shoulder: An experimental study on the role of the glenoid labrum in stabilizing the joint. Arthroscopy. 1992;8(2):166–72.
Hurschler C, Wülker N, Mendila M. The effect of negative intraarticular pressure and rotator cuff force on Glenohumeral translation during simulated active elevation. Clin Biomech. 2000;15(5):306–14.
Lephart SM, Warner JJP, Borsa PA, Fu FH. Proprioception of the shoulder joint in healthy, unstable, and surgically repaired shoulders. J Shoulder Elb Surg. 1994;3(6):371–80.
Tibone JE, Fechter J, Kao JT. Evaluation of a proprioception pathway in patients with stable and unstable shoulders with somatosensory cortical evoked potentials. J Shoulder Elb Surg. 1997;6(5):440–3.
Bankart Blundell AS. Recurrent or habitual dislocation of the shoulder joint. Br Med J. 1923;2(3285):1132–3.
Trinh TQ, Naimark MB, Bedi A, Carpenter JE, Robbins CB, Grant JA, et al. Clinical outcomes after anterior shoulder stabilization in overhead athletes: An analysis of the MOON Shoulder Instability Consortium. Am J Sports Med. 2019;47(6):1404–10.
Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37(9):1750–4.
Kraeutler MJ, McCarty EC, Belk JW, Wolf BR, Hettrich CM, Ortiz SF, et al. Descriptive epidemiology of the MOON Shoulder Instability Cohort. Am J Sports Med. 2018;46(5):1064–9.
Owens BD, Dawson L, Burks R, Cameron KL. Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Ser A. 2009;91(4):791–6.
Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Ser A. 2010;92(3):542–9.
Kraeutler MJ, Currie DW, Kerr ZY, Roos KG, Mccarty EC, Comstock RD. Epidemiology of shoulder dislocations in high school and collegiate athletics in the United States: 2004/2005 through 2013/2014. Sports Health. 2017;10(1):85–91.
Drakos MC, Domb B, Starkey C, Callahan L, Allen AA. Injury in the National Basketball Association: a 17-year overview. Sports Health. 2010;2(4):284–90.
Minhas SV, Kester BS, Larkin KE, Hsu WK. The effect of an orthopaedic surgical procedure in the National Basketball Association. Am J Sports Med. 2015;44(4):1056–61.
Grimer RJ, Cool P. The prognosis following acute primary glenohumeral dislocation. J Bone Joint Surg Br. 2005;87-B(2):277.
Ward JP, Bradley JP. Decision making in the in-season athlete with shoulder instability. Clin Sports Med. 2013;32:685–96.
Avis D, Power D. Axillary nerve injury associated with glenohumeral dislocation. EFORT Open Rev. 2018;3(3):70–7. https://doi.org/10.1302/2058-5241.3.170003.
Kumar K, Makandura M, Leong NJJ, Gartner L, Lee CH, Ng DZW, et al. Is the apprehension test sufficient for the diagnosis of anterior shoulder instability in young patients without magnetic resonance imaging (MRI)? Ann Acad Med Singap. 2015;44(5):178–84.
Provencher MT, Leclere LE, King S, McDonald LS, Frank RM, Mologne TS, et al. Posterior instability of the shoulder: diagnosis and management. Am J Sports Med. 2011;39(4):874–86.
Kim SH, Park JS, Jeong WK, Shin SK. The Kim test: a novel test for posteroinferior labral lesion of the shoulder – a comparison to the jerk test. Am J Sports Med. 2005;33(8):1188–92.
Bishop JY, Jones GL, Rerko MA, Donaldson C. 3-D CT is the most reliable imaging modality when quantifying glenoid bone loss shoulder. Clin Orthop Relat Res. 2013;471(4):1251–6.
Duchman KR, Hettrich CM, Glass NA, Westermann RW, Wolf BR, Baumgarten K, et al. The incidence of Glenohumeral bone and cartilage lesions at the time of anterior shoulder stabilization surgery: a comparison of patients undergoing primary and revision surgery. Am J Sports Med. 2018;46(10):2449–56.
Dickens JF, Slaven SE, Cameron KL, Pickett AM, Posner M, Campbell SE, et al. Prospective evaluation of glenoid bone loss after first-time and recurrent anterior glenohumeral instability events. Am J Sports Med. 2019;47(5):1082–9.
Hayes K, Callanan M, Walton J, Paxinos A, Murrell GAC. Shoulder instability: management and rehabilitation. J Orthop Sport Phys Ther. 2013;32(10):497–509.
Buss DD, Lynch GP, Meyer CP, Huber SM, Freehill MQ. Nonoperative management for in-season athletes with anterior shoulder instability. Am J Sports Med. 2004;32(6):1430–3.
Dickens JF, Owens BD, Cameron KL, Kilcoyne K, Allred CD, Svoboda SJ, et al. Return to play and recurrent instability after in-season anterior shoulder instability: a prospective multicenter study. Am J Sports Med. 2014;42(12):2842–50.
Wheeler JH, Ryan JB, Arciero RA, Molinari RN. Arthroscopic versus nonoperative treatment of acute shoulder dislocations in young athletes. Arthroscopy. 1989;5(3):213–7.
Arciero RA, Wheeler JH, Ryan JB, McBride JT. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med. 1994;22(5):589–94.
Brumitt J, Sproul A, Lentz P, McIntosh L, Rutt R. In-season rehabilitation of a division III female wrestler after a glenohumeral dislocation. Phys Ther Sport. 2009;10(3):112–7.
Burns TC, Owens BD. Management of shoulder instability in in-season athletes. Phys Sportsmed. 2010;38:55–60.
Watson S, Allen B, Grant JA. A clinical review of return-to-play considerations after anterior shoulder dislocation. Sports Health. 2016;8(4):336–41.
Balg F, Boileau P. The instability severity index score. J Bone Joint Surg Br. 2007;89-B(11):1470–7. https://doi.org/10.1302/0301-620X.89B11.18962.
Sachs RA, Lin D, Stone ML, Paxton E, Kuney M. Can the need for future surgery for acute traumatic anterior shoulder dislocation be predicted? J Bone Joint Surg A. 2007;89(8):1665–74.
Marans HJ, Angel KR, Schemitsch EH, Wedgl JH. The fate of traumatic anterior dislocation of the shoulder in children. J Bone Joint Surg – Ser A. 1992;74(8):1242–4.
Hovelius L, Eriksson K, Fredin H, Hagberg G, Hussenius A, Lind B, et al. Recurrences after initial dislocation of the shoulder. Results of a prospective study of treatment. J Bone Joint Surg Am. 1983;65(3):343–9.
Shanley E, Thigpen C, Brooks J, Hawkins RJ, Momaya A, Kwapisz A, et al. Return to sport as an outcome measure for shoulder instability: surprising findings in nonoperative management in a high school athlete population. Am J Sports Med. 2019;47(5):1062–7.
Kavaja L, Lähdeoja T, Malmivaara A, Paavola M. Treatment after traumatic shoulder dislocation: a systematic review with a network meta-analysis. Br J Sports Med. 2018;52(23):1498–506.
Kirkley A, Griffin S, Richards C, Miniaci A, Mohtadi N. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder. Arthroscopy. 1999;15(5):507–14.
Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy. 2005;21(1):55–63.
Elsenbeck MJ, Dickens JF. Return to sports after shoulder stabilization surgery for anterior shoulder instability. Curr Rev Musculoskelet Med. 2017;10(4):491–8.
Abdul-Rassoul H, Galvin JW, Curry EJ, Simon J, Li X. Return to sport after surgical treatment for anterior shoulder instability: a systematic review. Am J Sports Med. 2019;47(6):1507–15.
Waterman BR, Burns TC, McCriskin B, Kilcoyne K, Cameron KL, Owens BD. Outcomes after Bankart repair in a military population: predictors for surgical revision and long-term disability. Arthroscopy. 2014;30(2):172–7.
Fabricant PD, Taylor SA, McCarthy MM, Gausden EB, Moran CJ, Kang RW, et al. Open and arthroscopic anterior shoulder stabilization. JBJS Rev. 2015;3:1.
Speer KP, Deng X, Borrero S, Torzilli PA, Altchek DA, Warren RF. Biomechanical evaluation of a simulated Bankart lesion. J Bone Joint Surg. 1994;76(12):1819–26.
Yong GR, Jeong HH, Nam SC. Anterior shoulder stabilization in collision athletes: arthroscopic versus open Bankart repair. Am J Sports Med. 2006;34(6):979–85.
Mohtadi NGH, Bitar IJ, Sasyniuk TM, Hollinshead RM, Harper WP. Arthroscopic versus open repair for traumatic anterior shoulder instability: a meta-analysis. Arthroscopy. 2005;21(6):652–8.
Freedman KB, Smith AP, Romeo AA, Cole BJ, Bach BR. Open Bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for recurrent anterior instability of the shoulder: a meta-analysis. Am J Sports Med. 2004;32(6):1520–7.
Harris JD, Gupta AK, Mall NA, Abrams GD, McCormick FM, Cole BJ, et al. Long-term outcomes after bankart shoulder stabilization. Arthroscopy. 2013;29:920–33.
Petrera M, Patella V, Patella S, Theodoropoulos J. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surg Sport Traumatol Arthrosc. 2010;18(12):1742–7.
Ialenti MN, Mulvihill JD, Feinstein M, Zhang AL, Feeley BT. Return to play following shoulder stabilization: a systematic review and meta-analysis. Orthop J Sports Med. 2017;5:2325967117726055.
Rugg CM, Hettrich CM, Ortiz S, Wolf BR, Baumgarten KM, Bishop JY, et al. Surgical stabilization for first-time shoulder dislocators: a multicenter analysis. J Shoulder Elbow Surg. 2018;27(4):674–85. https://doi.org/10.1016/j.jse.2017.10.041.
Bishop JY, Hidden KA, Jones GL, Hettrich CM, Wolf BRMSG. Factors influencing surgeon’s choice of procedure for anterior shoulder instability: a multicenter prospective cohort study. Arthroscopy. 2019;35(7):2014–25.
Kasik CS, Rosen MR, Saper MGZR. High rate of return to sport in adolescent athletes following anterior shoulder stabilisation: a systematic review. J ISAKOS. 2019;4(1):33–40.
Owens BD, Cameron KL, Peck KY, DeBerardino TM, Nelson BJ, Taylor DC, et al. Arthroscopic versus open stabilization for anterior shoulder subluxations. Orthop J Sport Med. 2015;3(1):1–4.
Su F, Kowalczuk M, Ikpe S, Lee H, Sabzevari S, Lin A. Risk factors for failure of arthroscopic revision anterior shoulder stabilization. J Bone Joint Surg Am. 2018;100(15):1319–25.
Phadnis J, Arnold C, Elmorsy A, Flannery M. Utility of the instability severity index score in predicting failure after arthroscopic anterior stabilization of the shoulder. Am J Sports Med. 2015;43(8):1983–8.
Boughebri O, Maqdes A, Moraiti C, Dib C, Leclère FM, Valenti P. Results of 45 arthroscopic Bankart procedures: does the ISIS remain a reliable prognostic assessment after 5 years? Eur J Orthop Surg Traumatol. 2015;25(4):709–16.
Yamamoto N, Muraki T, An KN, Sperling JW, Cofield RH, Itoi E, et al. The stabilizing mechanism of the latarjet procedure: a cadaveric study. J Bone Joint Surg Am. 2013;95(15):1390–7.
Wellmann M, De Ferrari H, Smith T, Petersen W, Siebert CH, Agneskirchner JD, et al. Biomechanical investigation of the stabilization principle of the Latarjet procedure. Arch Orthop Trauma Surg. 2012;132(3):377–86.
Mizuno N, Denard PJ, Raiss P, Melis B, Walch G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elb Surg. 2014;23(11):1691–9.
Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JJP. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94(6):495–501.
Gupta A, Delaney R, Petkin K, Lafosse L. Complications of the Latarjet procedure. Curr Rev Musculoskelet Med. 2015;8:59–66.
Griesser MJ, Harris JD, BW MC, Hussain WM, Jones MH, Bishop JY, et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg. 2013;22:286–92.
Zimmermann SM, Scheyerer MJ, Farshad M, Catanzaro S, Rahm S, Gerber C. Long-term restoration of anterior shoulder stability: a retrospective analysis of arthroscopic bankart repair versus open latarjet procedure. J Bone Joint Surg Am. 2016;98:1954–61.
Rossi LA, Bertona A, Tanoira I, Maignon GD, Bongiovanni SL, Ranalletta M. Comparison between modified Latarjet performed as a primary or revision procedure in competitive athletes: a comparative study of 100 patients with a minimum 2-year follow-up. Orthop J Sport Med. 2018;6(12):1–7.
An VVG, Sivakumar BS, Phan K, Trantalis J. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elbow Surg. 2016;25(5):853–63.
Bhatia S, Frank RM, Ghodadra NS, Hsu AR, Romeo AA, Bach BR, et al. The outcomes and surgical techniques of the Latarjet procedure. Arthroscopy. 2014;30:227–35.
Willemot LB, Akbari-Shandiz M, Sanchez-Sotelo J, Zhao K, Verborgt O. Restoration of articular geometry using current graft options for large glenoid bone defects in anterior shoulder instability. Arthroscopy. 2017;33(9):1661–9.
Provencher MT, Ghodadra N, LeClere L, Solomon DJ, Romeo AA. Anatomic osteochondral glenoid reconstruction for recurrent Glenohumeral instability with glenoid deficiency using a distal tibia allograft. Arthroscopy. 2009;25(4):446–52.
Frank RM, Romeo AA, Provencher MT. Glenoid reconstruction with distal tibia allograft for recurrent anterior shoulder instability. Orthopedics. 2017;40(1):e199–205.
Provencher MT, Frank RM, Golijanin P, Gross D, Cole BJ, Verma NN, et al. Distal tibia allograft glenoid reconstruction in recurrent anterior shoulder instability: clinical and radiographic outcomes. Arthroscopy. 2017;33(5):891–7.
Wong IH, King JP, Boyd G, Mitchell M, Coady C. Radiographic analysis of glenoid size and shape after arthroscopic coracoid autograft versus distal tibial allograft in the treatment of anterior shoulder instability. Am J Sports Med. 2018;46(11):2717–24.
Liwski CR, Dillman D, Liwski RS, Wong IH. Donor-specific human leukocyte antigen antibody formation after distal tibia allograft and subsequent graft resorption. Clin J Sport Med. 2019;1 https://doi.org/10.1097/JSM.0000000000000715.
Frank RM, Romeo AA, Richardson C, Sumner S, Verma NN, Cole BJ, et al. Outcomes of Latarjet versus distal tibia allograft for anterior shoulder instability repair: a matched cohort analysis. Am J Sports Med. 2018;46(5):1030–8.
Liu JN, Gowd AK, Garcia GH, Cabarcas BC, Nicholson GP, Cole BJ, et al. Return to sport following Latarjet versus distal tibia allograft for anterior shoulder instability: a matched cohort analysis. J Shoulder Elb Surg. 2019;28(6):e197–8.
Bottoni CR, Wilckens JH, DeBerardino TM, D’Alleyrand JCG, Rooney RC, Harpstrite JK, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30(4):576–80.
Pagnani MJ, Dome DC. Surgical treatment of traumatic anterior shoulder instability in American football players. J Bone Joint Surg Am. 2002;84(5):711–5.
Popchak A, Patterson-Lynch B, Christain H, Irrgang JJ. Rehabilitation and return to sports after anterior shoulder stabilization. Ann Joint. 2017;2:62.
Cho NS, Hwang JC, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: collision athletes versus noncollision athletes. Arthroscopy. 2006;22(9):947–53.
Dickens JF, Rue JP, Cameron KL, Tokish JM, Peck KY, Allred CD, et al. Successful return to sport after arthroscopic shoulder stabilization versus nonoperative management in contact athletes with anterior shoulder instability: a prospective multicenter study. Am J Sports Med. 2017;45(11):2540–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 ESSKA
About this chapter
Cite this chapter
Altchek, D.W., Carr, J.B., Cirdi, Y.U., Ergün, S., Karahan, M. (2020). Management of Shoulder Instability in Basketball Players. In: Laver, L., Kocaoglu, B., Cole, B., Arundale, A.J.H., Bytomski, J., Amendola, A. (eds) Basketball Sports Medicine and Science. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-61070-1_24
Download citation
DOI: https://doi.org/10.1007/978-3-662-61070-1_24
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-61069-5
Online ISBN: 978-3-662-61070-1
eBook Packages: MedicineMedicine (R0)