Abstract
Traumatic anterior dislocation of the shoulder is a relatively common injury in the young, active population. Most of the interest regarding these injuries has focused on recurrence as the primary complication. Recurrence is not typically a problem in the older population; prolonged morbidity secondary to associated rotator cuff injury is more common. In older individuals, the dynamic stabilizers are more likely to fail (rotator cuff), whereas in young individuals, it is more often the static restraints that fail (labrum). Additionally, with increasing age, the incidence of pre-existing, degenerative tears of the rotator cuff is increasing.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Traumatic anterior dislocation of the shoulder is a relatively common injury in the young, active population. Most of the interest regarding these injuries has focused on recurrence as the primary complication. Recurrence is not typically a problem in the older population; prolonged morbidity secondary to associated rotator cuff injury is more common. In older individuals, the dynamic stabilizers are more likely to fail (rotator cuff), whereas in young individuals, it is more often the static restraints that fail (labrum). Additionally, with increasing age, the incidence of pre-existing, degenerative tears of the rotator cuff is increasing.
When evaluating a patient who cannot abduct the arm after reduction of an anterior dislocation, the physician tends to assume that this inability is caused by an axillary nerve palsy. This assumption frequently results in an unnecessary delay in establishing the correct diagnosis of a ruptured rotator cuff, and the delay can result in a challenging reconstruction.
2 Literature Overview Summary: What Is Known
The association of a rotator cuff tear and dislocation in the older population is well documented. Ribbans et al. [1] reported a 63% rotator cuff tear rate in primary traumatic dislocation in a small number of patients older than 50 years. Hawkins and Mohtadi [2] reported a 90% rotator cuff tear rate in a similar patient population. Toolanen et al. [3] reported a 38% tear rate, and 47% of the patients still complained of shoulder dysfunction at 3 years postinjury. However, 65% of their patients had electromyogram-confirmed axillary nerve or brachial plexus injury, which may have contributed to their poor results. Neviaser et al. [4] reported a 100% rate of rotator cuff tears in patients older than 40 years with a primary traumatic anterior dislocation. However, this was a preselected group of patients, making the true incidence impossible to determine. In their study, most rotator cuff tears were initially misdiagnosed as axillary nerve injuries. They also reported a 30% recurrence rate and emphasized the importance of the rotator cuff to glenohumeral stability. This is consistent with Itoi et al. [5] who used a cadaver model to describe the importance of the rotator cuff muscles and the long head of the biceps, as dynamic stabilizers of the shoulder. Pevny et al. [6] studied 52 patients older than 40 years with a shoulder dislocation. Between these group of patients, 42 showed excellent or good outcomes, and 11 showed fair and poor outcomes. 18 patients out of a total of 52 showed a rotator cuff tear (35%), and only 11 (61%) of these patients obtained an excellent or good outcome. Of the 11 patients with a fair or poor result, seven (64%) had a rotator cuff tear. Of the patients with isolated cuff tears, 84% had an excellent or good result when treated surgically, compared with 50% when treated nonsurgically. These findings indicate that recurrence is not a frequent complication of traumatic anterior shoulder dislocation in this age group (4%). However, prolonged morbidity secondary to rotator cuff tear is more prevalent than in a younger population.
The most important concerns regarding this topic are related to the treatment. The dispute is about the type of treatment, conservative or surgical, open or arthroscopic. And finally on what to repair labral tear, cuff tear or both.
Pevny et al. [6] showed that patients treated surgically had 84% excellent/good results, compared with 50% excellent/good results when treated nonoperatively. In this series, most of the patients had open cuff repairs. Bassett and Coffield [7] also reported better results after surgical cuff repair in terms of functional outcome and pain relief following acute dislocations. In all studies available, the cuff repair was combined with an acromioplasty. Voos et al. [8] showed good clinical outcomes, restoration of motion, and high degree of patient satisfaction in patients treated arthroscopically with rotator cuff and Bankart lesion.
Operation is suggested by many authors, but there is discussion as to which structure should be repaired, only Bankart repair, only rotator cuff repair, or both. The Itoi’s results indicate that repair of a Bankart lesion is probably not necessary in older patients [5]. In the elderly, cuff tears are commonly associated with anterior dislocation, and repair of the cuff alone may be sufficient to achieve stability. Voos et al. [8] showed good clinical outcomes, restoration of motion, and high degree of patient satisfaction doing arthroscopic treatment of both labrum lesion and rotator cuff.
Porcellini et al. [9] in a case series stated that patient age and the number of dislocations do not appear to correlate with Bankart or capsular lesions, whereas posterosuperior cuff tears seem to be influenced by the number of dislocations. Although data from this study do not permit to conclude whether repair of the sole cuff tear can achieve shoulder stability nor whether shoulder stabilization alone can resolve the instability, treatment of both lesions should be performed arthroscopically, because the arthroscopic technique allows to treat capsular-labral and cuff lesions in the same procedure.
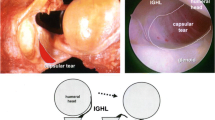
3 Anatomy
McLaughlin and MacLellan [10] suggested that anterior dislocation of the shoulder occurs either by disruption of the glenohumeral ligament (anterior mechanism) or by rupture of the rotator cuff (posterior mechanism). They believed that failure of the posterior support was more likely in patients who are older than 40 years, because the tendinous structure usually degenerates and weakens with age. Rupture of the musculotendinous cuff, particularly of the supraspinatus, infraspinatus, and teres minor, can permit anterior dislocation of the humeral head on an intact anterior soft tissue hinge and thus may be termed the posterior mechanism of anterior dislocation [11].
Hsu et al. [12] demonstrated in a cadaveric study that the displacement of the humeral head increases with an increase in tear size with or without translational forces applied and that a rotator interval tear is more crucial than a critical area tear from the viewpoint of instability.
4 Indication for This Surgery
Treatment regarding primary traumatic dislocation in the older patient is not well defined. Hawkins and Mohtadi [2] recommended physical therapy at 1 week followed by an arthrogram at 4 weeks if there was no clinical improvement. More recently, Sonnabend [13] recommended immobilization for 3 weeks followed by an arthrogram or ultrasound if pain and weakness were still present. In this kind of patients, 3 weeks of immobilization could be too long. This can lead to stiffness. Based on results present in the literature, the diagnosis of a rotator cuff tear should be approached aggressively at 7–10 days (after reduction) by an MRI or arthrogram if significant pain and weakness are still present. If the MRI is consistent with a rotator cuff tear, we recommend shoulder arthroscopy and arthroscopic or open repair. If the MRI is negative or the patient shows improved pain and weakness at 7–10 days, we recommend proceeding with a rehabilitation program aimed at strengthening the rotator cuff and scapular stabilizers. If after 3 weeks of rehabilitation the patient does not show significant improvement, an MRI should be ordered to evaluate the rotator cuff. Special attention should be directed to the subset with greater tuberosity fracture or axillary nerve involvement. If a rotator cuff tear is documented, prompt surgical repair should be pursued to optimize the long-term functional outcome in these patients.
5 Specific Points in Rehabilitation
In case of nonoperative management, a supervised rehabilitation program should be performed. The program consists of several steps: (1) pain was released by detonisation exercises combined with oral medication and (2) the flexibility and range of motion were restored by stretching exercises. The three steps involved restoration of strength of the internal and external rotators against resistance using a rubber tube or weights and improvement of the deltoid strength. After approximately 6 weeks, the fourth step consists of aerobic exercises and modification of work and sport activities.
In the case of surgical treatment of both rotator cuff tear and labrum damage, a physical therapy protocol was directed toward protecting the rotator cuff repair.
Rehabilitation protocols are not changed on the basis of the type of labrum repair performed. All patients had their arm placed in a sling and permitted passive range of motion in the scapular plane (maximum 90 ° forward flexion) and pendulum motion during the first 6 postoperative weeks. During weeks 6–12, passive range of motion is increased and active range of motion initiated. At 6 weeks, rotator cuff strengthening with a low-resistance TheraBand (the Hygenic Corporation, Akron, Ohio) was allowed. At 10–12 weeks, light weights are added. From week 12–6 months postoperatively, rotator cuff strengthening and scapular stabilizing exercises were progressed with unlimited return to activity at 6 months postoperatively.
6 Results
Only a few studies dealing with this subject are available in the literature. Pevny et al. [6] reported 84% of good results after early repair, as against only 50% after conservative treatment, and concluded that early surgical repair and treatment yielded better results than did conservative treatment of cuff tears. Bassett and Coffield [7] also reported better results after surgical cuff repair in terms of functional outcome and pain relief following acute dislocations.
Conclusion
Rotator cuff tear associated with anterior shoulder dislocation is well documented, although often the cuff injury is initially misdiagnosed. Brachial plexus injury has also been reported in association with rotator cuff tear in the setting of shoulder dislocation. This group of injuries could be considered the “terrible triad” of the shoulder.
The debate about the treatment of these patients is still open. The surgical treatment showed superior results to that conservative. It is not yet clear whether in these patients (elderly) it is better to treat either the injury or only the rotator cuff tear.
References
Ribbans WJ, Mitchell R, Taylor GJ. Computerised arthrotomography of primary anterior dislocation of the shoulder. J Bone Joint Surg Br. 1990;72(2):181–5.
Hawkins RJ, Mohtadi NG. Controversy in anterior shoulder instability. Clin Orthop Relat Res. 1991;272:152–61.
Toolanen G et al. Early complications after anterior dislocation of the shoulder in patients over 40 years. An ultrasonographic and electromyographic study. Acta Orthop Scand. 1993;64(5):549–52.
Neviaser RJ, Neviaser TJ, Neviaser JS. Anterior dislocation of the shoulder and rotator cuff rupture. Clin Orthop Relat Res. 1993;291:103–6.
Itoi E et al. Dynamic anterior stabilisers of the shoulder with the arm in abduction. J Bone Joint Surg Br. 1994;76(5):834–6.
Pevny T, Hunter RE, Freeman JR. Primary traumatic anterior shoulder dislocation in patients 40 years of age and older. Arthroscopy. 1998;14(3):289–94.
Bassett RW, Cofield RH. Acute tears of the rotator cuff. The timing of surgical repair. Clin Orthop Relat Res. 1983;175:18–24.
Voos JE et al. Outcomes of combined arthroscopic rotator cuff and labral repair. Am J Sports Med. 2007;35(7):1174–9.
Porcellini G et al. Shoulder instability and related rotator cuff tears: arthroscopic findings and treatment in patients aged 40 to 60 years. Arthroscopy. 2006;22(3):270–6.
McLaughlin HL, MacLellan DI. Recurrent anterior dislocation of the shoulder. II. A comparative study. J Trauma. 1967;7(2):191–201.
Craig EV. The posterior mechanism of acute anterior shoulder dislocations. Clin Orthop Relat Res. 1984;190:212–6.
Hsu HC et al. Influence of rotator cuff tearing on glenohumeral stability. J Shoulder Elbow Surg. 1997;6(5):413–22.
Sonnabend DH. Treatment of primary anterior shoulder dislocation in patients older than 40 years of age. Conservative versus operative. Clin Orthop Relat Res. 1994;304:74–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 ISAKOS
About this chapter
Cite this chapter
Franceschi, F., Franceschetti, E., Salas, E.A. (2017). Acute RCT as a Part of Dislocation. In: Imhoff, A., Savoie III, F. (eds) Shoulder Instability Across the Life Span. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-54077-0_28
Download citation
DOI: https://doi.org/10.1007/978-3-662-54077-0_28
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-54076-3
Online ISBN: 978-3-662-54077-0
eBook Packages: MedicineMedicine (R0)