Abstract
The entire nerves of hip, back, and leg are listed in detail – as far as they can be – which are affected by focal iatrogenic damage or by simple entrapment. Anatomy, some rare variants, damaging factors, and patient’s presentation of clinical symptoms with regard on each single nerve are first described. Next, each section contains details of electrodiagnostic testing and supplemental modern imaging techniques such as high resolution ultrasound and MRI. The high value of imaging is demonstrated in a lot of characteristic figures. The surgical approach for each single nerve is described as far as surgical decompression is possible.
Initially, a special outline is given of the worldwide problem with inguinal nerves after groin repair. The surgical approach differs from the usual entrapment cases: here, encouraging possibilities by neuromodulation are emphasized. The importance of imaging to establish the diagnosis of a space-occupying lesion preoperatively is argued. When a surgeon is unexpectedly confronted with intraneural ganglion cysts or a schwannoma he suddenly needs microsurgical equipment. Uncommon entrapment lesions such as pudendus, obturatorius, or saphenus neuralgia, anterior and media tarsal tunnel syndromes, and Morton’s metatarsalgia are delineated and illustrated by surgical instruction figures.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
9.1 Ilio-hypogastric, Ilio-inguinal, Genito-femoral Nerves
The following chapter about the three inguinal nerves will be short because efforts to expose the small nerves to try neurolysis macro-surgically, or even with a microscope, are useless. We therefore resort to describing anatomical details which we find in visceral surgical descriptions and reports. Nevertheless, there are new therapeutic concepts which can simply be applied to neuropathies as we will later describe in detail.
9.1.1 Damaging Factors
Painful focal nerve lesions of one or more of the inguinal nerves result almost always from hernia surgery. When we read “Hernia Repair Sequelae” in 2010, visceral surgeons worldwide claim about 10–15 % of post-operative painful discomfort [1]. It is interesting that the different authors never distinguish between the different types of groin pain. Local pain syndromes may be due to post-hematoma, fluid effusion or tumor-like fibrotic conditions as a reaction on prosthetic implants. Nerve damage-related groin pain of a radiating character can instead demonstrate various pain qualities as already described in Sect. 4.2. Independent of the type of hernia surgery, herniorrhraphy or hernioplasty with mesh grafts, the rate of painful complications remains the same. Most crucial are post-hernia neuropathic pain cases. Major risk factors related to developing such a pain syndrome are: age below 40 years, pre-existing pre-operative pain, and the male gender. The investigation of mesh explants in order to determine tissue reaction led to the result that younger patients displayed a significantly enhanced infiltration of macrophages after mesh implantation. Older patients were at lower risk of reacting with inflammation on mesh material [1].
Of great importance are, first, an Italian prospective multi-center study done by Alfieri and co-workers in 2006 [2] and second, a previous report by Izard and co-workers in 1996 [3]. Intra-operative identification of all three inguinal nerves during open inguinal hernia repair with or without mesh is reported there to be able to reduce chronic groin pain to less than 1 %.
Although the results of these analyses were published years ago, incapacitating pain syndromes are continuing to occur constantly and frequently. We have therefore to suppose that ligatures or clips for mesh graft fixation or inflammatory tissue reactions are the main causative factors. Industry thus tries to influence surgeons to apply lightweight macro-porous mesh implants to reduce inflammatory reactions on the one hand, and to avoid the possibility of mechanical nerve irritation on the other.
9.1.2 Clinical Symptoms
The symptoms consist of pain, with numbness remaining in the background, weakness is of course absent. The inguinal nerves mainly carry sensory fibers so that, compared to other skin nerves, pain is the leading complaint. It can mostly be manually triggered at the site where substantial damage exists in the abdominal wall. The nerve caliber is so small that intraneural destruction is of a high degree and, consequently, nerve axon regeneration can not be expected. The situation results in neuroma in continuity. The trigger point with radiating pain into the distribution area of the effected inguinal nerve indicates the site of the neuroma. Unfortunately, neuropathic pain types occur frequently. This pain has a burning character; slight touches are perceived as additionally painful (refer to Sect. 4.2). If causalgia occurs, the affected painful skin area is extended, a fact that no longer allows the conclusion which one of the inguinal nerves are really injured. Only the trigger point and the assessment of which skin area the pain then radiates into are helpful.
9.1.3 Electrodiagnostics
There is a significant lack of reports regarding electrodiagnostic testing of the ilio-hypogastric, ilio-inguinal, and genito-femoral nerves in the current literature. Some smaller recent studies or case reports have demonstrated abnormalities in nerve conduction velocities, needle electromyography of the abdominal muscles, reflexology (cremasteric) and somatosensory evoked potentials. All these electrophysiological studies require a technically skilled operator, but are not sufficiently sensitive and specific at the moment [4]. Whether these tests will become routine in general medical practice is uncertain.
Abnormalities in motor nerve conduction using conduction time to the cremasteric muscle, needle electromyography of the cremasteric muscle and cremasteric muscle reflex have been described in 47 % of patients which had undergone herniorrhaphy, whereas the 23 % of patients not treated surgically had problems with the genito-femoral nerve [5]. Similar results could be demonstrated under application of motor nerve conduction studies of the ilio-inguinal nerve [6]. Stand-alone needle electromyography of the abdominal muscles supplied by the ilio-hypogastric and ilio-inguinal nerves revealed signs of subacute or chronic axonal damage in 60 % of patients with definite entrapment and in 37 % with probable entrapment [7]. In future, high resolution ultrasound guided needle electromyography or needle-electrode placement may play a key role in increasing the sensitivity and specificity of these methods. In addition, the registration of somatosensory evoked potentials may be helpful in confirming diagnosis. Therefore, in a single case report the lateral cutaneous branch of the ilio-hypogastric nerve was used for stimulation [8]. Generally, if a unilateral affection is present a side to side comparison of the electrodiagnostic results described above may help and must be closely correlated with clinical findings.
9.1.4 Imaging
High resolution ultrasound provides a simple and cost-effective way to visualize both the ilio-inguinal and ilio-hypogastric nerves [9]. A diagnostic block can be more safely established when guided by ultrasound. It is increasingly important to apply this technique simultaneously, because in general, the diagnosis is assessed on the basis of pain relief within 10 min of local infiltration with anaesthetics [10]. Therefore, the ultrasound probe should be placed with its lateral end just above the anterior superior iliac spine (ASIS) with a perpendicular orientation to the inguinal line. Now the hyperechoic surface of the ASIS and its post-acoustic shadowing is clearly visible laterally. Medially underneath the subcutaneous fat, three layers of abdominal muscles appear (from the outside to the inside): external oblique (EO), internal oblique (IO) and transverse abdominal (TA). Below the transverse abdominal muscle, the peritoneum and the movement of bowels can be observed. Usually the ilio-inguinal and ilio-hypogastric nerves are visible between the layers of the TA and IO muscles, where a splitting of the fascia is normally present (Fig. 9.1b). Nevertheless, there also exist anatomical variants [11]. Sometimes, both nerves can pierce the IO and appear between the IO and EO muscles. They may run together or at a distance of approximately 10 mm. The technique for blocking the genital branch of the genito-femoral nerve under ultrasound guidance has not yet been published [10]. Furthermore, in some of our patients, we were able to demonstrate some pathological changes of the ilio-inguinal and ilio-hypogastric nerves. The most common reactions found included neuroma-formation and enlargement of the cross sectional area (Fig. 9.1a). Until now, major reports on 3 T-MRI of the three nerves are unavailable. In a recent case report on nerve injury locations due to retropubic sling procedures, MRI could not evaluate any abnormalities despite severe chronic pain in symptomatic individuals [12]. Recently Chhabra and Andreisek described the assessment of all three nerves using MRN [13].
Neuroma formation of the ilio-inguinal nerve after hernia surgery. (a) HRUS shows the stump neuroma (arrow) of the ilio-inguinal nerve (arrowheads) and scarring (asterisk) just above. (b) Normal anatomy. The arrowheads point on the ilio-inguinal and ilio-hypogastric nerves as well as on the deep circumflex iliac artery. ASIS anterior superior iliac spine, EOL + IOL external oblique and internal oblique muscle, TA transverse abdominal muscle
9.1.5 Treatment
Because neurolysis procedures have proved unsatisfactory and, of course, risk in resulting in hernia recurrence, circumscriptive neurotomy is performed worldwide, particularly as so-called “triple neurotomy” in the retroperitoneal space [1].
Neurosurgical pain surgeons have a completely new and comparably simple approach: the idea of pain relief by electrical stimulation of the involved peripheral nerve, a method that has been derived from the “Gate Control Theory” by Melzack and Wall in 1965 [14]. According to their concept, electrical stimulation of fast A-fibers is said to have the capacity to “gate out” pain stimuli conducted via slow C-fibers. It is well known that most pain input to the brain runs via the small unmyelinated and thinly myelinated C-fibers. This input and its transmission to the brain can be reduced by activating of fast running A-fibers. Currently, the concept of nerve stimulation is not only applied to sensory spinal cord fibers but just as successfully to injured peripheral nerves [15]. If the nerve caliber allows piercing of the epineurium, a small electrode is pushed slightly into the sub-epineurial space. We have demonstrated a case with superficial radial nerve branch pain in 2004 [16]. After an external test stimulation period of a few days, the external screener is changed into a pacemaker placed subcutaneously in chest or abdominal wall.
Due to their too small caliber, inguinal nerves do not allow one to advance electrodes into their sub-epineurial space. Experience can now demonstrate that electrodes which were directly beside or in the neighbourhood of nerves did work. With reference to triple neurotomy of hernia surgeons, laparoscopic approaches into the intra-abdominal and retro-peritoneal space were made in order to place electrodes a few centimeters under the peritoneum and beside the affected nerve [17]. The idea was derived from experience with extra-uterine endometriosis-related nerve pain.
Meanwhile, a far simpler approach seems to be the gold standard: so-called subcutaneous peripheral nerve stimulation (sPNS). In local anaesthesia, the electrode is percutaneously advanced near to the location of the assumed nerve injury whereby the trigger point helps to find the site exactly. The intra-operative test stimulation can induce pleasing paresthesias in the distribution area of the affected nerve. After a short external test stimulation period, the pacemaker is – then under general anaesthesia – placed into the abdominal wall about 10 cm from the electrode. This method achieves astonishing responses by the formerly painful conditions as recently reported. In this prospective study of our center, 21 patients are included with a follow up of nearly 10 years. Of these, 76 % had a successful long-term outcome and 24 % had to be considered as long-term failures [18]. Here, after all, sPNS is simple and nearly free of risk, especially if compared with intra- or extra-abdominal approaches. Furthermore, a recent evaluation of 61 spinal cord stimulation patients resulted in the interesting fact that responses did not differ whether the stimulator was used continuously or intermittently [19]. Several of these patients were even proud to have successfully extended their stimulation-out-periods more and more. They stimulated still only facultatively, and after a few years they even requested removal of the complete system. It can be emphasized that responses on post hernia neuropathic pain syndromes are also encouraging but, of course, cases need to be further analyzed.
9.2 Lateral Femoral Cutaneous Nerve
9.2.1 Anatomy
The nerve arises from the L2-root and remains within the retroperitoneal tissue. It exits the pelvis just medial to the anterior superior spine of the iliac crest. The exit point is formed by a split in the lateral attachment of the inguinal ligament at the bone. It then angulates sharply downward, especially in extended hip joint position. The small nerve remains under the fascia and crosses over the upper portion of the sartorius muscle a little to lateral. A few centimeters below the inguinal ligament, the nerve pierces the thick fascia lata. Variations occur frequently [20]. First, the nerve course can be situated more lateral so that it crosses over the iliac bone, second, the level of division into branches varies. It can easily be imagined that a very high ramification makes the exposure more difficult.
9.2.2 Damaging Factors
Most of focal neuropathies of the lateral femoral cutaneous nerve occur spontaneously. The passage between sheaths of the inguinal ligament predisposes the nerve to become compressed or angulated during hip extension. It is often said that symptoms disappear with weight loss, but we also saw underweight patients with the same neuropathy. To summarize, in most cases reliable causative factors cannot be identified. Less common is scarring in the neighbourhood of the nerve responsible for neuralgic pain. It can result from abdominal surgery, open or laparoscopic, and from injury during removal of iliac bone parts as grafts.
9.2.3 Clinical Symptoms
Symptoms are frequently perceived as electric current-like, often suddenly radiating into the distribution area of the nerve of the anterior and lateral aspects of the thigh. The pain does not include the knee and patella region. It is worsened or induced by standing and walking, and relieved by flexion of the hip joint. If the pain history runs long enough, patients complain of additional numbness during painless periods. Numbness unfortunately indicates advanced intra-neural damage within the small nerve, and it worsens the prognosis when neurolysis is done. The electric current-like pain can be provoked by deep manual palpation immediately medial to the anterior superior spine. The same radiating pain disappears if a local anaesthetic is injected at this point. Both of these tests, palpation and injection, serve as clinical proof of the neuropathy of “meralgia paresthetica” as it is usually called. However, this term has to be restricted to those cases with spontaneous onset rather than those related to prior surgery. Those tests also act as an aid to assess the differential diagnosis between a peripheral neuropathy and an L2- or L3-root compression. Both roots have sensory distribution areas similar to that of the lateral femoral cutaneous nerve.
9.2.4 Electrodiagnostics
The lateral femoral cutaneous nerve (LFCN) remained difficult to test reliably by electrophysiological means in the past, likely due to anatomic nerve variability and lack of response in asymptomatic obese subjects [21, 22]. However, recent studies with up to date electrophysiological equipment demonstrate that responses could be obtained in at least 92 % of subjects, even if they are obese [21]. Ultrasound-guided near-nerve needle placement and recording could provide a novel approach, especially when evaluation is critical and responses are difficult to obtain [23]. Orthodromic and antidromic sensory nerve conduction studies are frequently used in the clinical routine. The most appropriate stimulation site in an antidromic nerve conduction study is located 1 cm or more medial to the anterior superior iliac spine (ASIS) or 4 cm distal to the ASIS, whereas sensory nerve action potentials can be simultaneously recorded along an imaginary line between the ASIS and the lateral border of the patella and 2 cm medial to this line [24, 25]. However, normal values are variable and depend on the operator and recording technique. An alternative approach consists of orthodromic nerve conduction study of the lateral femoral cutaneous nerve distally to the ASIS. Of the 120 symptomatic subjects, 98 % had a side to side amplitude ratio greater than 2.3. Combined with the amplitude of the sensory nerve action potential that is lower than 3 μV, this yielded a specificity of 99 % [26]. Furthermore, recording of dermatomal somatosensory evoked potentials provides another option in the diagnosis of meralgia paresthetica. In a recent report, this technique was found to be superior to sensory nerve conduction studies: 81 % vs 65 % sensitivity [27].
9.2.5 Imaging
The lateral cutaneous femoral nerve can easily be identified in the intermuscular space between tensor fasciae latae and sartorius muscles by high resolution ultrasound [28]. Therefore, the sartorius muscle serves as an initial sonographic landmark (Figs. 9.2 and 9.3). Anatomical variations of the nerve course (e.g. piercing of the sartorius) can also be made visible. From this point, the nerve can be traced up to the inguinal ligament and to the anterior superior iliac spine. The cross sectional area of the lateral cutaneous femoral nerve move to behind 1.04 ± 0.44 mm2 [28]. In symptomatic individuals suffering from meralgia paresthetica, high resolution ultrasound was able to show the enlargement of the nerve diameter and cross sectional area [29]. In a recent study the optimal cut-off value for the diagnosis of lateral femoral cutaneous nerve entrapment was 5 mm2 [30]. In our own experience, even the demonstration of different sites of compression (e.g. below the inguinal ligament) with focal congestion of the nerve proximally to them is possible (Fig. 9.2). Moreover, high resolution sonography is not only useful in confirming the diagnosis of meralgia paresthetica but also in ultrasound guided treatment modalities. Whereas conventional techniques (blind or nerve stimulator guided) yielded an incomplete block-success, the ultrasound guided approach was successful in all subjects [31, 32]. Pain relief following application of an anaesthetic confirms the diagnosis at first (Fig. 9.3). After that, one single or two therapeutic perineural injections of 1 mL of methylprednisolone acetate (40 mg/mL) and 8 mL of mepivacaine 2 % can significantly reduce symptoms over a 2-month period [32]. There exist additional case reports on patients treated successfully by means of pulsed radiofrequency ablation, and this may provide in future a relevant therapeutic alternative to surgical interventions described below [33].
(a) Longitudinal sections of entrapment of the lateral femoral cutaneous nerve (arrowheads) at the level of the anterior superior iliac spine (ASIS) below the inguinal ligament (arrows). Note the proximal nerve swelling. (b) Shows the corresponding cross sections with proximal nerve swelling and effaced fascicles, compression below the inguinal ligament (arrows) and the course of the nerve within tendon of the sartorius muscle and the fat-filled tunnel (from right to left). Arrowheads: lateral femoral cutaneous nerve
(a) Several approaches of ultrasound guided injection of the lateral femoral cutaneous nerve (LFCN, arrowheads): Left: LFCN above the belly of the sartorius muscle. Middle: LCFN within a fat-filled tunnel. Right: LFCN below the inguinal ligament (arrows). ASIS anterior superior iliac spine. (b) Ultrasound guided injection of the LFCN using the “in-plane” scanning technique. Arrowheads: lateral femoral cutaneous nerve
Signal intensity alterations of the lateral femoral cutaneous nerve are difficult to visualize by MR imaging owing to the small size of the nerve [34]. Accordingly, MRI is not the first choice for the diagnosis of lateral femoral cutaneous neuropathy. However, a secondary etiology which is sometimes discussed from e.g. avulsion fractures of the ASIS, sartorius tendon injury, pelvic osteotomy, and acetabular fracture may be demonstrated by MRI [34].
9.2.6 Treatment
If conservative treatment fails (weight reduction, avoidance of tight clothing, drugs acting on neuropathic pain, ultrasound guided injections – see section above) [32], surgery is to be recommended. It consists of nerve release by transection of some parts of the lateral attachment of the inguinal ligament at the iliac bone. It sounds easy, but difficulties may occur with the small caliber of the nerve and its branches and with the above-mentioned anatomical anomalies. Therefore, repeated injections with corticosteroids or ultrasound-guided radiofrequency ablation are used and are also reported to be successful [32, 33]. Unfortunately, however, pitfalls of injection therapy trials can have a worsened prognosis if surgical neurolysis is in the end intended. First, the numbness is progressed, and, second, direct nerve substance damage can be caused by needles or injected substances. The prognosis is especially deteriorated when the character of the pain changes into a neuropathic one. We therefore prefer early surgery and perform it as neurolysis. We avoid a neurotomy so as not to risk a painful neuroma as a result (Fig. 9.4).
Surgical treatment of “Meralgia paresthetica”. (a) Skin incision. (b) First step: nerve exposure by splitting of the ventral limb fascia medial to the sartorius muscle. (c) Second step: nerve exposure to proximal aiming at transection of transverse inguinal ligament parts particularly inferior to the nerve
We personally prefer the approach which starts below the inguinal ligament. The skin incision is done anterior and a little superior of the spine and it then runs straight downward over a distance of about 4–5 cm. Next the fascia of the thigh is incised longitudinally. Beside the medial border of the sartorius muscle, the cutaneous nerve has to be identified as embedded in fat tissue; parallel to the nerve or its branches, a small venous vessel helps to find the thin nerve. After careful identification of the nerve or two or even three of its branches, we advance to proximal until the above-mentioned split between two parts of the inguinal ligament becomes visible. It is more important to transect the part which crosses under the angulated nerve than the part which covers the nerve course. During ligament fiber transection, the small nerve should be gently kept away a little. Particularly, if small bleedings appear at this moment, bipolar coagulation requires the nerve to be kept away. Surgical results of this approach are formally published [35].
As an alternative, some authors use a supra-inguinal approach which can facilitate nerve identification proximal to its ramification [36]. It needs the help of an assistant who keeps a retractor to medial manually whereas the infra-inguinal approach can be accomplished with self-holding retractors.
As we have experienced early recurrences following the surgery as outpatient management, we always advise hospitalization for a few days, and a suction drain to remain for no less than 3 days to avoid any re-bleeding or lymph fluid pad which likely occur in particular when the patient does not remain immobilized for long enough.
Pitfalls and pain recurrence depend on different factors, of course; on the efficiency of the inguinal ligament fiber transection, but also on the amount of intraneural damage that happened preoperatively, and, not to be neglected, on the preoperative pain type. Cases with hyperesthesia or even allodynia have a worse prognosis, whereas cases with a pain that can be triggered, and at the same time is without numbness, have the best prognosis. Injury to one of the small nerve branches can be followed by remaining neuropathic pain involving its small skin distribution, as experienced in rare cases.
9.3 Obturator Nerve
Focal neuropathies of the obturator nerve may commonly result from intra-pelvic trauma or surgery. As an intra-pelvic nerve exposure with neurolysis or proximal neurotomy seems to become unsatisfying, as described in comparable cases of inguinal nerve lesions in Sect. 9.1, we will neglect these almost incurable lesions in the following. However, several interesting experiences with spontaneous neuropathy exist, and they shall be covered in this chapter. Literature is rather lacking concerning these lesions.
9.3.1 Anatomy
The obturator nerve originates from the lumbo-sacral plexus (roots L2–L4). These are the same roots which contain all the fibers to the femoral nerve. It runs downward at the medial border of the psoas muscle, and then takes a vertical course to pierce the obturator membrane. At extra-pelvic level, the nerve at once divides into two branches, an anterior or superficial branch which supplies the adductor longus and gracilis muscles, and a posterior or deep branch, which supplies the adductor magnus and obturator externus muscles. Some sensory fibers represent sensation in a small skin area on the medial aspect of the thigh.
9.3.2 Damaging Factors
The possible relation of nerve injury to pelvic fractures or hip surgery has already been mentioned. Intra-pelvic malignancies may invade the nerve. Obturator hernias can involve the nerve. Newborns can suffer from obturator palsy; but they usually recover quickly [37]. Reliable factors which cause a compression syndrome with spontaneous onset are quite unknown. We could gain experience with the relatively easy exploration of the nerve’s exit site where the extra-pelvic course starts. We would like to emphasize the point that the split between obturator membrane and margin of the superior pubis bone branch is the location of a focal “spontaneously occuring” entrapment.
9.3.3 Clinical Symptoms
A small skin branch distributes a circumscriptive area at the medial and proximal aspect of the thigh. Pain is located there in the case of nerve entrapment. Numbness indicates a severe lesion and is therefore restricted to intra-pelvic nerve damage. Pathological potentials in the adductor muscles may be found in electromyography testing (see below). The diagnosis mainly consists of an infiltration with local anaesthesia at the point where we can elicit the pain by deep palpation, namely through the pectineus muscle. This test also helps to differentiate the obturator neuralgia from genital branch neuralgia.
9.3.4 Electrodiagnostics
Literature is rather sparse concerning nerve conduction studies of the obturator nerve and therefore limited in collaborative electrophysiological data. None of the few reported techniques on the subject are used routinely. A distal motor latency can be obtained by stimulating the obturator nerve at the inguinal ligament, while M-responses were recorded with needle electrodes from the gracilis muscle. An additional stimulation point – using needle electrodes at the level of the upper lumbar roots between L1–L2 vertebral laminae – generates a proximal conduction time [38]. In healthy individuals, the following normal values were reported: distal motor conduction latency 3.9 ± 0.7 ms, proximal conduction time 10.4 ± 0.3 m, and conduction velocity of the proximal segment 62 m/s [38]. An alternative method consists of magnetic stimulation of the paralumbar area, where the M-responses are recorded via needle electrodes placed in the adductor longus and adductor brevis muscles [39]. However, needle electromyography still remains the key method of evaluating obturator nerve function preexisting axonal damage. Due to the assessment of muscles only supplied by the obturator nerve, of muscles innervated by adjacent nerves, and of paraspinal muscles, a differentiation between an isolated obturator nerve neuropathy, lumbar plexopathy, or L3-root affection becomes feasible [40].
9.3.5 Imaging
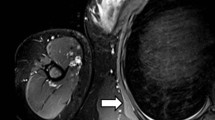
High resolution ultrasound is of subordinate importance in the diagnosis of obturator nerve neuropathy, because only the extra-pelvic nerve course can be assessed. The femoral vein and artery below the inguinal ligament serve as a landmark; by moving the probe medially and caudally to the pectineus muscle and then to the adductor muscles (consisting of the adductor longus, brevis and magnus from cranial to caudal) the nerve can easily be identified. The anterior branch of the obturator nerve with the adjacent vessels can be found in the fascia split between the pectineus, adductor longus and adductor brevis muscles, whereas the posterior branch with the accompanying vessels appears in the fascia split between the adductor brevis and magnus muscles. The following normal values (anterior-posterior diameter) have been reported so far: Anterior branch 1.4 ± 0.6 mm, posterior branch 1.7 ± 0.6 mm, main trunk 2.7 ± 1.2 mm [41, 42]. Tilting the probe cranially, the main trunk may be visible in slim individuals (Fig. 9.5). This technique is in use for ultrasound guided obturator nerve blocks [43]. As mentioned in the previous chapter, pain relief after infiltration with local anaesthetics again supports the diagnosis [40]. However, sonographical reports about extra-pelvic affections of the obturator nerve are missing at the moment. In contrast to that, 3 T-MRI allows the assessment of the entire course of the obturator nerve: the intra- and extra-pelvic parts. Particularly, by means of MRI, space-occupying lesions such as hematoma, bone fragments, bursa, nerve sheath tumor, malignancies, or osteo-synthesis materials as well as fat infiltration just proximal to and within the obturator canal can be assessed. On the other hand, muscle substance alternation related to acute or chronic denervation may be documented [34].
(a) Normal cross-sectional anatomy of the extra-pelvic course of the obturator nerve in HRUS. The main trunk (arrowhead) appears caudally between pectineus (PEC), adductor longus (AL) and adductor brevis (AB) muscles. (b) More distally the anterior branch (arrowhead) appears in the fascia split between adductor longus (AL) and the adductor brevis (AB) muscles whereas posterior branch (arrowhead) can be located in the fascia split between adductor brevis (AB) and adductor magnus (AM) muscles
9.3.6 Treatment
In the following, we restrict ourselves to describing the approach to the easily accessible extra-pelvic nerve part, the nerve segment, which may be involved in the sense of focal entrapment. We start with a skin incision parallel to the medial segment of the inguinal ligament and extend the incision vertically downward over 4–5 cm. The incision allows an approach between the long adductor muscle and the pectineus muscle. Of course, fibers of the pectineus muscle can also be split by blunt dissection. Underneath the layer of these two muscles, we enter a flat layer of fat tissue in which the two mentioned branches of the obturator nerve are embedded. These nerve branches and the concomitant obturator artery and its branches are gently isolated, and next we follow to proximal in order to find the exit point through the obturator membrane. By means of a small punch, the lower margin of the ramus superior ossis pubis is opened in an inverse U-shape always with the exiting nerve and artery in view. The only literature concerning this approach we believe to be available is from Millesi from 1992 [44]. However, interestingly his contribution does not consider spontaneous entrapment cases at all (Fig. 9.6a, b).
9.4 Sciatic Nerve
A focal entrapment of the sciatic nerve can rarely occur within the infra-piriforme foramen. Birch specifies the historical literature which we can find dealing with the so-called “piriformis syndrome” [45]. The term is controversial in that a lot of pain syndromes in neighbourhood of the hip joint are included by different authors. In the following, we restrict ourselves to applying this term to cases which are severely associated with pain radiating under the foot, indicating a sciatic nerve irritation.
9.4.1 Anatomy
The sciatic nerve leaves the pelvis together with the inferior gluteal nerve and vessels through the lower part of the great sciatic foramen. The foramen is divided into higher and lower openings by the transverse running piriformis muscle. Its tendon attaches at the great trochanter of the femur. Sometimes, the tendon is extended more than normal to medial so that a fibrotic structure crosses over the sciatic nerve. As anatomical variation, the nerve may be divided into two trunks with the piriformis muscle running between both. In these cases, the superior trunk leads fibers running into the peroneal nerve distribution whereas the lower trunk contains fibers of the tibial nerve. A surgeon should be aware of this variation which can frequently occur.
9.4.2 Damaging Factors
Completely comparable to the thoracic outlet syndrome, where fibrotic structures within the scalene muscles cause plexus irritation, here a fibrotic and too medially extended tendon within the piriformis muscle leads to discomfort. It is not the muscle belly itself, but its tendon. Small persons with little buttock substance are predisposed. Three times we have observed patients who always used to keep their purse in the same back pocket while sitting in a car or on a bicycle. They instinctively left it out sometimes and the pain progressively disappeared. Another time, we were confronted with a patient who presented with a subtotal foot drop and additional weakness of the plantar flexion on both sides after he had been confined to bed in a supine position for 2 weeks in an intensive care unit. On the other hand, cases with spontaneous onset or without any known cause have required us to find a solution.
Magnetic resonance imaging (MRI) has, of course, to exclude space-occupying lesions within the pelvic area. The main differential diagnosis is commonly a lumbar disk protrusion; the sign according to Lasegue is always pathognomic in root compression whereas likely to be negative in the case of a “piriformis syndrome”, but, unfortunately, also negative in the case of a narrowed root recess.
9.4.3 Clinical Symptoms
The patient suffers from electric current-like pain which radiates into the tibial and peroneal nerve distribution either spontaneously, or when we palpate the gluteal area deep enough and just medial to the hip joint. A palsy of foot extension and/or flexion appears rarely, but has to be taken into account as mentioned above.
Computerized tomography- or ultrasound-guided test injections can be used to differentiate between sciatica due to either spinal root compression or piriformis irritation: A nerve root infiltration influences the afferent input from both levels, from spinal and infrapiriforme ones, whereas an infiltration into the infrapiriforme foramen cannot influence afferent fibers which are compressed superiorly; thus, a positive effect in the periphery excludes a spinal root compression. Of course, magnetic resonance imaging (MRI) of the thoraco-lumbar spine and the pelvis is mandatory to use all possible means to exclude sciatica of alternative origin.
9.4.4 Electrodiagnostics
Electrodiagnostic testing may be of some assistance in determining nerve irritation. The sciatic nerve is stimulated proximally at the gluteal fold using a 75-mm monopolar needle, and distally at popliteal level, the peroneal and tibial nerves being stimulated separately. The recording electrodes are positioned over the extensor digitorum brevis and abductor hallucis muscles for examining the peroneal and tibial portions of the sciatic nerve. Motor nerve conduction velocities (MNCV) are, for the tibial nerve division 52.8 ± ms and, for the peroneal nerve division 54.3 ± 4.4 ms [46]. MNCV of the sciatic nerve can be measured at the gluteal segment by magnetic stimulation, proximally at L5 and S1 roots and distally at the sciatic nerve at the gluteal fold followed by recording at the corresponding muscles. The mean MNCV of the gluteal nerve segment in the L5 component was 55.4+/−7.8 m/s in patients with piriformis syndrome, which was slower than the mean value of 68.1+/−10.3 m/s obtained in healthy controls. The MNCV of the sciatic nerve in the S1 component showed no significant difference between patients and controls. A negative relation was found between the disease duration and the MNCV values in piriformis syndrome. It was concluded that magnetic nerve stimulation provides a painless, non-invasive and objective method to evaluate sciatic nerve function in patients with piriformis syndrome [47].
In clinical practice, however, commonly the electrodiagnostic studies include the sensory study of sural and further superficial peroneal nerves, and, of course, the motor studies of the peroneal and tibial nerves (see below). Abnormal SNAPs of sensory nerves imply an infraganglional lesion. H-reflexes and F-waves are unable to localize the lesion focus. Needle electromyography is the most informative in sciatic nerve lesions. Gluteal sciatic nerve irritation – such as in piriformis syndromes – can demonstrate slightly pathologic findings in semitendinosus and semimembranosus muscles, in the long head of biceps femoris, and in lower leg muscles [48].
9.4.5 Imaging
As previously mentioned in Sect. 6.1.3, the sciatic nerve course can be visualized well by means of high-resolution ultrasound distally of the gluteal fold, whereas the intrapelvic and gluteal regions hardly permit to obtain reliable information in ultrasound (Figs. 9.7, 6.8e and 6.22a).
The method of choice is MR neurography because the sciatic nerve is easily evaluated in all imaging planes due to its large size and abundant perineural fat (Figs. 6.21 and 6.22b). The nerve has intermediate signal intensity on T1-weighted images and mildly high signal intensity on fluid-sensitive images. It can be followed as it descends in the greater sciatic foramen and exits the pelvis under the inferior margin of the piriformis muscle. Direct MR imaging evidence of sciatic neuropathy includes course deviation, increased size and increased signal intensity. The latter is more easily detected than in lower extremity nerves owing to the large size of the sciatic nerve. Obliteration of the fat planes around the nerve trunk may also be noted [34]. However, imaging diagnosis of piriformis syndrome is problematic. Although the diagnosis can be commonly inferred from changes in the appearance of the affected nerve, evaluation of piriformis muscle size and its comparison with the contralateral side are less than satisfying, as muscle anomalies and significant variations in size are noted in symptomatic and asymptomatic individuals [34]. In a review of 100 patients with no history or clinical suspicion of piriformis syndrome, muscle size asymmetry of 2 mm was present in 81 % of patients. None of the patients with asymmetry of 4 mm or more had symptoms suggestive of piriformis syndrome [49].
Using MR neurography it was found that, of patients who responded well to piriformis surgery, 38.5 % had ipsilateral muscle hypertrophy and 15 % had muscular atrophy. Muscle asymmetry alone turned out to have a specificity of 66 % and sensitivity of 46 %, identifying patients with muscle-based piriformis syndrome. Conversely, ipsilateral nerve edema was 88 % associated with reproducible symptoms of piriformis syndrome. Use of both asymmetry of the piriformis muscle and increased nerve signal intensity improved the diagnostic ability of MR neurography, with 93 % specificity and 64 % sensitivity [50]. In a retrospectively reviewed MRN study of the sciatic nerve in the pelvis and thighs of 34 subjects, of which 17 had a final diagnosis of sciatic neuropathy according to electrodiagnostic or surgical confirmation, it was found that sciatic nerves of the affected sides exhibited higher nerve-to-vessel SI (signal intensity) ratios and, furthermore, higher incidences of T2 hyper-intensity, enlargement, and abnormal fascicular shape compared to sciatic nerves of the normal side. A cut-off value of nerve-to-vessel SI ratio of 0.89 exhibited high sensitivity and specificity in predicting sciatic neuropathy. In particular, calculation of the nerve-to-vessel SI ratio demonstrated excellent reliability. The authors conclude that both qualitative and quantitative criteria should be used to suggest the MRN diagnosis of sciatic neuropathy [51]. Nevertheless, most authorities agree that delineation of the neuromuscular relationship will turn out to become the most important goal of imaging. Until reproducible and reliable criteria have been established, piriformis syndrome will remain a diagnosis by exclusion [52].
9.4.6 Treatment
CT- or ultrasound-guided botulinum toxin injections into the piriforme muscle belly are performed repeatedly with success. However, the first surgical approach was described by Robinson in 1947 [53]. He sectioned the piriformis muscle a few centimetres beside its attachment at the great trochanter completely. He chose a lateral transection in order to assure the preservation of all major vessels which lie concomitant to the sciatic nerve and its branches. The same author describes several anatomical variations as existent in 10 % of specimens, e.g. the division of the sciatic trunk.
We prefer surgery and choose a skin incision parallel to the expected fibers of the gluteus maximus muscle; then the muscle fibers are split and separated to both sides and manually retracted. Fibers of the gluteus medius muscle which are situated underneath can be lifted up and also retracted. The sciatic nerve trunk can be felt medial to the hip joint as a longitudinally downward running structure of index finger diameter. It is embedded in fat tissue and accompanied by the inferior gluteal artery and a venous plexus. The dissection to proximal requires care to preserve as much of this plexus as possible. Transverse vessels have to be visualized before rupture, closed by bipolar coagulation far enough from nerve fibers, and finally transected. Vessel rupture immediately colours the operating field black. The sensory posterior femoral cutaneous nerve branch which runs downward and medial to the sciatic nerve has to be preserved; its injury can result in numbness or even neuropathic pain at the back of the thigh and in the perineum via a small perhaps not unimportant nerve branch. By proceeding to proximal, the transverse running fibrotic lower edge of the piriformis should come into view, and it then requires transection piece by piece above the exiting nerve. However, before doing so, the inferior gluteal nerve should be visualized; it curves around the lower edge of the piriformis and then upwards. The muscle belly itself can of course be preserved, comparably to the situation in the scalene notch, as muscle fibers do not irritate nerve structures at all.
It may rarely happen that a large venous convolute occurs within the infrapiriforme foramen on the left side. This rare phenomenon is related to the possible venous “pelvic congestion syndrome” which can occur by a so-called “nutcracker-phenomenon” – a compression of the left iliac vein between lumbar spine and left iliac artery or of the left renal vein between aorta and superior mesenteric artery [54, 55].
As it is almost impossible to preserve the whole venous plexus during surgery, a deeply advanced suction drain of large caliber is mandatory to avoid hematoma-complications, especially when the patient gets up. As a final remark concerning our indication, surgical treatment is only being considered when typical electric current-like radiating sciatica is present. Our goal cannot be anything else than decompression of a focal nerve entrapment. Pain syndromes which instead remain in the buttock – e.g. inflammatory tendopathies – do not offer any surgical option at the present time.
9.5 Pudendal Nerve
9.5.1 Anatomy
The pudendal nerve arises from the second, third and fourth sacral nerve roots, leaves the pelvis through the great sciatic foramen, and re-enters the pelvis through the lesser sciatic foramen. The fibrous canal between both foramens is referred to as the Alcock canal; therefore, neuropathies of the pudendal nerve were described as Alcock’s canal syndrome [56]. The nerve supplies half of the perineum and genital region with sensory fibers. Its focal entrapment evokes intractable pain attacks in this area. The clinically important fact that the perineum is also supplied by a small branch of the posterior femoral cutaneous nerve should never be neglected (Fig. 9.8a–d).
(a) Anatomy of the pudendal nerve course. (b) Anatomy after patient’s positioning on his back with lifted legs; nerve’s relation to sacrospinal and sacrotuberal ligaments. (c) Skin incision. (d) Nerve exposure and transection of the sacrotuberal ligament under the gluteus maximus muscle fibers; the ligament is, if existent, to be identified by your fingertip
9.5.2 Damaging Factors
Of course, trauma relation or iatrogenic damage and space-occupying lesions can affect the nerve. However, on the other hand, prolonged bicycle rides have been already repeatedly described [57]; similar histories have also been observed by us. This mechanism should be assessed as the main causative factor when a neuropathy seems to appear spontaneously. The nerve is then trapped between the ischial spine and the sacro-tuberous ligament. In particular, the falciforme lower edge of the ligament is able to pinch the nerve if pressure arises between body and bicycle saddle. A figure in Steward’s book gives us a reasonable impression of this entrapment site [58].
9.5.3 Clinical Symptoms
Patients describe unilateral, electric current-like, pain within the genital region and perineum with sudden onset comparable to the “tic doloureux” in a trigeminal neuralgia. Only one of our patients –a small person with little buttocks – suffered from alternating pain attacks on both sides.
A more or less continuous pain which remains restricted to the perineum might be of another origin: This restricted pain area can likely belong to the distribution of the perineal (cluneal) branch of the posterior cutaneous nerve, as mentioned in Sect. 9.4.
When the patient lies supine with his hip joint 90° flexed so that the leg stands vertically, the typical Tinel sign can be elicited about three fingertips beside the anus. It indicates the lower edge of the sacro-tuberous ligament. A careful test infiltration – perhaps ultrasound-guided – with local anaesthesia at this point removes the pain attacks for 2 h and creates a genital numbness instead. In a recent paper, these nerve blocks even resulted in therapeutic effects in 44 % of cases [59]. Only patients who satisfactorily responded to our test infiltration at the described site were selected for a small surgical decompression.
9.5.4 Electrodiagnostics
According to the anatomical course of the pudendal nerve, several sites of compression can lead to various clinical presentations of pudendal neuropathy [60]. As mentioned in Chap. 5, the unmyelinated C-fibers, carrying pain sensation are not assessable with conventional nerve conduction studies, whereas fecal and urinary incontinence, impotence and numbness of the skin area supplied by the nerve thereby may be relevant. In the past two decades, different electrodiagnostic techniques have been introduced, but most of them are not in general use. Needle electromyography of the anal sphincter, registration of terminal motor latency of the pudendal nerve after transrectal electrical stimulation, as well as somatosensory evoked potentials of the pudendal nerve may be helpful for making a diagnosis. In particular, a prolonged terminal motor latency and signs of anal sphincter denervation in needle electromyography suggest an involvement of the anal motor nerve, whereas changes in somatosensory evoked potentials of the pudendal nerve may verify a sensory neuropathy [61]. However, in 2008, a group of experts published five essential (exclusively clinical) diagnostic criteria for pudendal neuralgia by focal nerve entrapment (“Nantes criteria”): “(1) pain in the anatomical territory of the pudendal nerve; (2) worsened by sitting; (3) the patient is not woken at night by the pain; (4) no objective sensory loss on clinical examination; (5) positive effect by anaesthetic pudendal nerve block” [62]. In this set of criteria, electrodiagnostic testing plays only a subordinate role. We have unfortunately to realize that our electrodiagnostic techniques do not differentiate between entrapment and alternative nerve lesion (especially obstetrical damage in uni- or multiparous women). Therefore they do not give any direct information about pain etiology. Consequently, they have a rather limited sensitivity and specificity. In fact, they might perhaps be helpful before surgery in order to assess the quality of motor innervation of the nerve, and they might predict the outcome [63].
9.5.5 Imaging
In a recent report it has been shown that high resolution ultrasound can identify the pudendal nerve at the ischial spine when using a medial approach, and its terminal branches when using an anterior approach [64]. Unfortunately, its value in the diagnosis of different pathological processes involving the nerve, especially if entrapment is supposed, remains unclear at the moment. Until now, pain relief after blocking the pudendal nerve with anaesthetics is the superior diagnostic criterion in pudendal neuralgia [62]. Sonography may also be applied for ultrasound guided nerve blocks. Using colour Doppler to localize the internal pudendal artery at the ischium, in a second step, the sacro-spinous and sacro-tuberous ligaments have to be targeted. The pudendal nerve may be found in the plane between these two ligaments [10]. Regarding pudendal nerve entrapment and MR imaging, it was recently reported that the neurovascular bundle can be visualized by MR neurography between the ischial spine and the Alcock canal. In the case of entrapment, it is reported as typical to find asymmetric nerve swelling and hyperintensity on T2-weighted and fat-saturated images [65].
9.5.6 Treatment
Therapeutic concepts extend from repeated steroid injections via trans-vaginal approach, CT-guided trans-perineal injections [66], surgical decompression via trans-perineal approach [67], trans-gluteal approach with exposure of the entire Alcock’s canal [56], until neuro-modulation via electrodes on sacral nerve roots [68] or even on the spinal cord [69]. Of course, we have first to consider that a disorder of the pudendal nerve distribution can present a wide field of individual symptoms, and, second, that it is commonly combined with progressed social disintegration. Therefore, dedicated therapeutic approaches and options can only be offered where centers deal with all types of pudendal neuralgia [70]. Particular difficulties arise when the pain has achieved neuropathic character. Our own experience is exclusively restricted to those cases which could be manually triggered at the lower edge of the sacro-tuberous ligament, and which could be tested there by local anaesthetics.
The surgical approach to this focal entrapment site is very simple. It can be easily derived from anatomical figures [72]. The patient’s positioning is comparable to that needed in proctologic approaches. The skin incision is done approximately 3 cm beside the anus and a little bit dorsal to respectively below it. The lower edge of the gluteus muscle fibers is separated from fat tissue. At this point, the trapping ligament underneath the muscle should be palpated with a fingertip. In a few operated cases, the ligament as a solitary structure was absent, but instead, several transverse running fibrous bands could be palpated. The pudendal nerve exits upon the ligament or the fibrous bands when we bring to mind the patient’s position in the operating theatre. Identification of the pudendal nerve is not as easy as expected because it is embedded in abundant fat tissue and therefore difficult to survey. However, consideration of the pre-operatively discovered trigger point in relation to the position of the anus finally helps to isolate the nerve. The last surgical step is partial or complete transection of the sacro-tuberous ligament where it covers the nerve’s exit (Fig. 9.8c–d).
As mentioned, several specialized centers exist worldwide where experts of different disciplines work together in the field of pudendal neuropathy. However, around 60 % of these cases are suitable for trying the simple approach described above [70]. Our own experience is rather small, but at least it proved successful provided we remained restricted to neuralgias which originated from the nerve’s exit zone. This chapter shall not in any case cover the whole entity of pudendal neuropathies.
9.6 Femoral Nerve
The femoral nerve is never affected by a spontaneously occurring irritation or entrapment only. Pre-formed anatomical structures like tendons, ligaments or a narrowed channel which could irritate the nerve in a sense of focal neuropathy do not exist. Therefore, our description remains short.
9.6.1 Anatomy
The femoral nerve arises from the L3 and L4 spinal roots, and it then starts downward at the lateral aspect of the psoas muscle. Its course is covered by the iliacus fascia. Under the inguinal ligament it exits the pelvis lateral to the femoral artery and vein. Then it divides at once into several motor branches which supply the quadriceps muscles, and into sensory branches which innervate the skin of the ventral thigh medial to the area of the lateral femoral cutaneous nerve. One of its branches – the saphenous nerve – will be the subject of the next main section.
9.6.2 Damaging Factors
We have already mentioned that entrapments of focal character with spontaneous occurrence do not exist. Nontheless we once tried a single neurolyisis under the inguinal ligament in a patient with progressive loss of quadriceps muscle strength without success. The young man probably suffered from one of the inflammatory disorders we will describe in Chap. 12.
Reasonable femoral nerve impairments are instead the following: penetrating injuries in the groin, or below, at the thigh, lesions in association with pelvic fracture, inguinal node resection, femoral artery puncture, all kinds of intra-pelvic surgery, hip arthroplasty, hematoma or abscess beneath the iliacus fascia, false aneurysms following rupture of an aortic aneurysm, malignancies of the iliac bone or other space-occupying lesions like harmless cysts or ganglia. In 1934, anatomists described those rare cysts as originating from occasional communications with the hip joint [72]. In addition, in 1982, a possible way to evaluate these rare lesions by ultrasound was published; the paper again indicates that this type of investigation is easily applicable [73]. Therefore, in general, if a femoral neuropathy occurs, imaging seems mandatory to discover the reason before surgery is considered.
9.6.3 Clinical Symptoms
Patients always suffer from loss of muscle strength of the quadriceps. The disability more or less keeps the knee joint extended and impairs patients’ standing and walking. Numbness and paresthesias are not the main complaints, but rather the weakness. The knee reflex can be absent.
9.6.4 Electrodiagnostics
Motor evoked responses can be detected with surface electrodes located over the vastus medialis muscle using reference electrodes over the patella. The deep location of the nerve often requires high current intensities at the three recommended stimulation sites above and below the inguinal ligament and at Hunter’s canal along the medial aspect of the thigh. The distance between the proximal stimulation sites should be at least 5–6 cm. The latencies from above and below the inguinal ligament are 7.1 ± 0.7 ms and 6.0 ± 0.7 ms [46], respectively. Evaluating the CMAP from the two sites allows quantification of the degree of axonal loss. Femoral neuropathies which allowed estimation of its axonal loss of ≤50 % turned out to have a fine prognosis with improvement within 1 year; fewer than half the patients with axonal loss >50 % can expect to improve to some extent. Irrespective of the origin, spontaneous functional improvement was seen in two out of three patients; and assessment of amount of axonal loss was the only prognosis predicting factor [74]. In pure femoral neuropathy, the quadriceps and sartorius muscles show pathological results in needle electromyography, while the adductor muscles and the lower limb muscles remain normal. Additional involvement of the iliopsoas muscle reveals a lesion located more proximally. The differentiation from lumbar plexus lesions may be quite challenging and is needed to investigate paraspinal muscles, the adductor muscles, which are supplied by the obturator nerve, and also sciatic nerve innervated muscles [75].
9.6.5 Imaging
The femoral nerve can be visualized by high-resolution ultrasound (HRUS) in the inguinal region where it lies superficially. In a case report even a retroperitoneal femoral nerve injury after perforating injury at the lower abdomen could be demonstrated. A mass was observed in the retro-peritoneum, indicating a traumatic neuroma composed of disordered fascicles [76]. In our own experience, nerve lesion after angiography can easily be visualized (Fig. 9.9).
However, 3-T MRN as imaging seems to be the method of choice, because it can assess the nerve appearance in its pelvic course, where the sonography is uncertain (Fig. 6.17). A comprehensive review describes different types of abnormalities involving the femoral nerve and illustrates their 3-T MRN features with relevant case examples. Nerve compression may result from space-occupying lesions, such as hematoma, iliopsoas bursitis, neoplasm or psoas muscle abscess. Mild to moderate nerve abnormalities on MRN should be distinguished from nerve discontinuity resulting from severe injury which requires immediate surgery; fascicular morphologic abnormalities become very evident. Multiplanar reconstruction using 3D SPACE images is particularly helpful to differentiate between neuroma in continuity and physical nerve discontinuity. Extensor compartment muscle denervation changes serve as useful secondary signs of nerve abnormality [77].
9.6.6 Treatment
As the location of a focal femoral neuropathy is common within the pelvis and retroperitoneal, the approach nearly always requires opening of the retroperitoneal space. If unfamiliar with the exposure, a general surgeon should be requested to help. The approach also needs final proper wound closure to preclude an incisional hernia. For further details of this access refer to the work of Kline and Hudson from 1995 [78].
The management of trauma-related femoral nerve lesions needs extended nerve trunk exposure over its whole distance so that a two-portal approach above and below the inguinal ligament becomes unavoidable. However, it is not purpose of this book to describe the treatment of these extensive lesions related to the therapy of nerve traction during hip joint surgery. Iliacus hematomas, however, need prompt evacuation via the retroperitoneal approach, as recovery of nerve function then seems better than under more conservative treatment [79].
9.7 Saphenous Nerve with Infrapatellar Branch
9.7.1 Anatomy
The saphenous nerve arises from the femoral nerve a few centimeters below the inguinal ligament and runs downward alongside the femoral artery. In the lower third of the thigh, nerve and artery enter a channel of more or less 10 cm extension (Hunter’s channel). The nerve has an exclusively sensory function at the medial aspect of the lower leg. When exiting the channel the infrapatellar nerve leaves the saphenous nerve as a branch supplying the skin beneath the patella. Sometimes this branch pierces the facial roof of Hunter’s channel.
9.7.2 Damaging Factors
In our experience, older patients are commonly involved. Frequently, an arteriography of the femoral artery has previously been done to find or exclude peripheral arteriosclerotic occlusion, and sometimes interventional procedures of thrombus removal have been added. In any case, a severe femoral vessel sclerosis with loss of tissue elasticity has always been found during exposure. Nerve irritation then started between the sclerotic vessel and the channel’s roof. On the other hand, vein removal for use as arterial graft has sometimes resulted in saphenous pain syndrome [80].
Focal neuropathies of the infrapatellar branch mostly result from arthroscopic knee joint surgery. Unfortunately, substantial nerve tissue damage has then occurred with the frequent consequence that neuropathic pain appears under the patella.
9.7.3 Clinical Symptoms
Severe pain in the nerve distribution of the lower leg is the main complaint, perhaps aggravated by walking [81]. It can occur in the form of attacks, or it exists permanently, and it can be triggered with your fingertips at the level of the Hunter’s channel. Sometimes the triggered pain radiates retrograde to proximal. Test infiltrations into the channel to confirm the diagnosis involve risk of bleeding from the accompanied artery. In contrast to involvement of the lateral femoral cutaneous nerve, for instance, we avoid infiltrations.
The infrapatellar nerve branch commonly suffers from a severe intraneural lesion when it has been injured. The result is very frequently that either a neuroma pain type or, unfortunately, a neuropathic pain type appears (see Sect. 4.2). Simple entrapments are unknown in our experience.
9.7.4 Electrodiagnostics
In order to assess antidromic saphenous nerve conduction a proximal and a distal recording method has been developed. In the case of proximal recording, the nerve is activated along the medial aspect of the knee between the sartorius and gracilis tendons 1 cm proximal to the inferior border of the patella while the recording electrode is positioned 15 cm distal from the stimulation point at the medial border of the tibia. The values of peak-to-peak amplitudes are 10.2 ± 0.2 μV and of conduction velocity 58.8 ± 2.3 m/s [46]. In the case of distal recording, the nerve is activated between the medial border of the tibia and the gastrocnemius muscle – 14 cm proximally to the recording electrode of the previously described proximal method – while the recording electrode is positioned 3 cm proximal to the medial malleolus and posterior to the tibialis anterior tendon. The reference values of the peak-to-peak amplitudes are 9.0 ± 3.4 μV ms and of conduction velocity 41.7 ± 3.4 m/s [82].
9.7.5 Imaging
Ultrasound examination of the saphenous nerve is difficult because of its small size and anatomic variability. The sartorius muscle is identified first as an anatomic landmark. This long and flat muscle can be identified at once at the medial aspect of the knee: it is the only muscle located anterior to the gracilis and semitendinosus tendons. The muscle is then followed cranially. Attention is then focused on the deep surface of the muscle, where the saphenous nerve can be found running close to the deep fascia. In a more distal location the nerve can be visualized running between the sartorius and gracilis tendons to reach the subcutaneous tissue where they join the great saphenous vein. Detection of its thin infrapatellar branch can be very difficult [83]. In a cadaveric anatomical study, HRUS was performed on five cadavers and ten healthy volunteers. Useful landmarks to detect the nerve branch could be defined. Some anatomical variations were noted. It was concluded that the infrapatellar branch can be depicted by ultrasonographical means [84].
9.7.6 Treatment
Surgery on saphenous nerve entrapment requires opening of Hunter’s channel. A longitudinal skin incision is done over the lower third of the medial aspect of the thigh. The sartorius muscle covers Hunter’s channel and, when it is kept away, the surgeon’s fingertip feels pulsation of the femoral artery. Try first to isolate the artery, and afterwards the concomitant nerve where they enter the channel. With nerve and artery in view, the fascial roof of the channel is incised and finally sectioned transverse to its fibers as for the transverse carpal ligament fibers. The underlying sclerotic femoral artery has to be kept permanently in mind during nerve relief. Additional care should be taken to the infrapatellar nerve branch whose injury would induce the next pain syndrome. Wound closure needs to leave behind all fascial structures unclosed, and it needs a suction drain for 2 days (Fig. 9.10a, b).
The treatment of an injured infrapatellar branch remains controversial to date. Nerve repair can duplicate the pain intensity; the same holds true if a neuroma is exposed and removed. Shortening of the nerve branch is restricted up to the level where it arises from the saphenous nerve, a region where soft tissue is sufficiently lacking so that the new neuroma remains between skin and femur epicondyle. Nerve stimulation placed along the saphenous nerve below the inguinal ligament proved is more successful in such a case.
9.8 Common Peroneal Nerve at the Knee
9.8.1 Anatomy
The common peroneal nerve arises from the sciatic nerve at its mid-thigh level, turns a little to lateral and further superficially into the popliteal fossa, passes around the fibula bone about 1–2 cm below the tibio-fibula joint, and finally enters the compartment of the peroneal muscles. There it divides into two main branches, the superficial and deep ones. Both branches together supply muscles which extend the foot and toes. Further anatomical details have only importance when nerve repair is needed. Focal entrapments remain instead restricted to the site where the main nerve turns around the fibula and makes an almost 60° angled turn to ventral into the peroneal compartment.
9.8.2 Damaging Factors
The literature is full of causes or events that impair the common peroneal nerve at the above-mentioned exposed site [80]: external compression in operating theatres, due to plaster casts or braces, following habitual leg-crossing or sitting cross-legged, after prolonged kneeling, frequently in relation to special professions like floor-tilers. Trauma-related nerve lesions are mostly not focally restricted but far extended like typical traction lesions usually are.
The nerve may occasionally be compressed by a variety of space-occupying lesions like intraneural or extraneural ganglia, Baker’s cysts, hematomas or hypertrophic tibio-fibula joint arthrosis. With or without such lesions, patients often notice the symptom of a peroneal palsy after awakening from a normal sleep. Such palsy is probably the result of sleeping on one’s side. We remember a patient who used to press his knee against the left door continuously during professional car driving. However, most patients usually do not remember any possible causative factor. The physician therefore needs the patience to enquire about their habits, because a peroneal palsy almost never occurs really spontaneously.
9.8.3 Clinical Symptoms
One day during walking, the patient notices foot drop and finds himself in danger of stumbling. Slight paresthesias or numbness are additionally and often observed much later. The paresthesias can always be triggered at the typical compression site 2 cm below the prominent tibio-fibular joint. The typical occurrence of this Tinel sign is completely comparable to that just so often found in ulnar neuropathies at the elbow.
Ganglia cannot be detected by palpation because they are often hidden behind the fibular bone. Therefore, preoperative ultrasound imaging should be used in future, although, on the other hand, surgical exploration often enables to detect these lesions early. However, when we surprisingly find intraneural ganglia whose existence should always be considered, we will suddenly be confronted with the requirement for time consuming microsurgery (see Sect. 13.3.8).
Symptoms of “idiopathic” palsies and those related to space-occupying lesions do not differ from each other at all. Therefore, if preoperative differential diagnosis between both is required, and if uncomfortable findings during surgery are to be avoided, imaging becomes mandatory.
9.8.4 Electrodiagnostics
Demyelinating lesions of the peroneal nerve (e.g. due to compression neuropathy) across the fibular head are assessed with fractionated motor nerve conduction studies, whereby the recording electrode is placed over the extensor digitorum brevis (EDB) muscle, while nerve stimulation starts at the ankle and is then followed by stimulation below and above the fibular head [85]. Normal values have been published in 1999: distal motor latency 4.8 ms ±0.8, CMAP amplitude <40 years 6.8 mV ± 2.5, CMAP amplitude >40 years 5.1 mV ± 2.5, motor nerve conduction velocity 44–49 m/s ±4–5, normal amplitude difference from side to side 61 % [86]. A segmental delay of motor nerve conduction velocity by more than 10 m/s and/or a segmental drop in amplitude by more than 25 % (conduction block) are common findings in case of demyelinating lesions [85, 86]. However, in some previous studies, recording from the EDB was found to be less sensitive because only 33 % of affected cases were detected [87]. Thus, an additional motor nerve conduction study recording over the tibialis anterior muscle (TA) and stimulating below and above the fibular head has been suggested due to the fact that motor fibers supplying the EDB and TA may be damaged differently [85, 88, 89]. In addition, some anatomical variations can potentially disturb the motor nerve conduction study to EDB only. In fact, in 12.2 % of healthy individuals, an accessory deep peroneal nerve innervates the EDB. In this variability, no compound muscle action potential can be obtained while stimulating the nerve at the ankle, whereas stimulation below and above the fibular head generates a compound muscle action potential. Stimulation of the accessory deep peroneal nerve behind the lateral malleolus may solve this problem. Second, in 3.5 % of the healthy subjects, an agenesis of the EDB exists, and no compound muscle action potential can be obtained. Neither by stimulating the nerve at the ankle nor below and above the fibular head [90]. Finally, overlying diseases such as chronic compression by footwear or a polyneuropathy may affect the EDB.
Therefore, normal values for the tibialis anterior muscle have also been published in 2003: upper limit of distal motor latency to TA 4.9 ms, lower limit of CMAP amplitude 1.7 mV, lower limit of motor nerve conduction velocity 43 m/s, upper limit of side to side CMAP amplitude difference 50 %, upper limit of normal drop of amplitude from below to above fibular head stimulation 36 % [91]. A further alternative method, which is considered to be more specific, is the short segment stimulation after successive supramaximal stimuli of the nerve at 2 cm intervals, starting 4 cm distal and ending 6 cm proximal to the fibular head prominence [92].
As already explained in Chap. 5, a pure axonal peroneal nerve lesion will result as a drop or absence of compound muscle action potentials at all stimulation sites. Thus, no exact localization of the site of the nerve damage will be feasible with fractionated motor conduction studies. However, in this situation, needle electromyography is mandatory: the distribution of signs of denervation and chronic neurogenic changes in different muscles supplied either by the deep peroneal nerve (e.g. tibialis anterior, extensor halluces longus) or by the superficial peroneal nerve (e.g. peronaeus longus). or perhaps also by the peroneal part of the sciatic nerve (e.g. caput breve m. biceps femoris), by the lumbar plexus (e.g. gluteus medius), and, finally, by the L5-root innervated autochthonous para-vertebral muscles may localize the lesion. Needle myography will thus close the diagnostic gap [85].
The sensory function of the superficial peroneal nerve is easily assessable with an antidromic sensory nerve conduction study [85]. If the study is pathologically changed it indicates an infra-ganglionic lesion, whereas in the case of L5 radiculopathy, the SNAP should be preserved in the majority of cases. Furthermore, it has been recently demonstrated that even SNAPs of main branches of the superficial peroneal nerve, of both the medial and intermediate dorsal cutaneous sensory nerves, can easily be obtained by antidromic motor nerve conduction studies [93]. Technically more challenging and time-consuming are orthodromic nerve conduction studies with near nerve needle placement. This method is applicable on the superficial and deep peroneal nerves in certain patients, where the standard tools described above may not solve a complete differential diagnosis in common peroneal nerve neuropathy [87, 94].
In summary, if a peroneal nerve entrapment at the fibular head is assumed, initially, a fractionated motor nerve conduction study to the EDB may be helpful. If this does not localize the lesion, the peroneal motor nerve conduction study should be repeated recording the TA [85]. Finally, a fractionated orthodromic sensory nerve conduction study with near nerve needle placement could provide an alternative method, but it is more challenging and time-consuming [87, 94]. Axonal lesions are assessable with needle electromyography. By analysing the pattern of possible axonal damage in different muscles a mono-neuropathy of the peroneal nerve can be differentiated from other disorders, e.g. sciatic nerve neuropathy, lumbar plexopathy and L5 radiculopathy. Antidromic sensory nerve conduction studies are helpful in examining the superficial branch of the peroneal nerve and excluding a supra-ganglionic lesion. Furthermore, if a generalized and overlying disorder is supposed, extension of the examination including the opposite side and other peripheral nerves is mandatory [85].
9.8.5 Imaging
Both MR-neurography and sonography are applicable in focal peroneal neuropathy. With high resolution ultrasound, the main landmark is the fibular head of course. At this level, the common peroneal nerve can easily be obtained [95]. Tracing the nerve from this point proximally, it is first located below the short head of the biceps femoris muscle, and in front of it the lateral sural cutaneous nerve appears. More proximal, the common peroneal nerve runs medially and reaches the bifurcation of the sciatic nerve at variable depth and height. However, tracing the common peroneal nerve distally from the level at the fibular head, in our experience, the fascicles of the deep branch are located more distal, whereas the fascicles of the superficial branch can be found more proximal. The deep branch runs further deep below the peroneus longus muscle, and there it approaches the anterior tibial artery. Its terminal branches are difficult to detect within the surrounding muscles. The superficial branch first runs deep between the peroneus longus and extensor digitorum muscles. At the distal third of the lower leg (high variability!) the superficial peroneal nerve returns to the surface, pierces the crural fascia and now runs between the fascia of the two above-mentioned muscles and the subcutaneous fat-layer. Finally it reaches the back of the foot, where the nerve divides into its two terminal branches (high variability) [95]. The normal cross sectional area of the common peroneal nerve at the level of the fibular head is 0.10 ± 0.04 cm2 [95]. Recently a cut-off value for peroneal neuropathy >8 mm2 has been described [97].
In an epidemiological study, which involved our own patients (n = 2,071), the amount of subjects with a focal peroneal neuropathy was 2.8 % involving either the common peroneal nerve or its deep branch, and 0.33 % involving the superficial branch, respectively. Most frequently (67 %) the common peroneal nerve and its deep branch were affected by a traumatic nerve injury. High resolution ultrasound showed the typical signs already described in Chap. 6. Non-traumatic etiology included peripheral tumors of the peripheral nerve sheath, intra-neural ganglion cysts of the peripheral nerve sheath, compression by extraneural ganglion cysts, and compression below the peroneus longus muscle/fascia. Each of these lesions can be detected reliably using high resolution ultrasound (Figs. 6.12, 9.11, 9.12 and 9.13). Similar results are to be found in the literature [98–101]. Unfortunately, skin incisions resulting from different surgical interventions (varicose vein extraction, osteosynthesis, emergency compartment syndrome treatment, etc.) frequently painfully affect superficial peroneal nerve branches at the distal third of the lower leg. High resolution ultrasound enables to detect the compression by scar tissue or the stump neuroma/neuroma in continuity, and furthermore, an ultrasound guided diagnostic/therapeutic block can again be done [102]. Some examples are shown in Figs. 9.14, 9.15, and 9.16.
Chronic entrapment of the peroneal nerve below the peronaeus longus muscle in a patient with food drop lasting more than 9 months. (a) Ultrasound cross sections show a normal nerve (arrowhead) at level of the short head of the biceps femoris muscle (CB). At the fibular head (FH), a massive nerve swelling (arrowhead) appears. The left image demonstrates the compression of the peroneal nerve (arrowhead) between fibula (F) and peronaeus longus muscle (PL). (b) Corresponding MRN images showing increased nerve size on T1 weighted images at the fibular head (FH) as well as hyperintensity of single fascicles on 3D WATS (fluid) images (arrow). More distally, the site of compression is demonstrated between the tendon of peronaeus longus muscle (arrow) and fibula (F) (MRN courtesy of Karsten Stock, MD (department of radiology and neuroradiology, Dessau-Rosslau Hospital/Germany)). (c) Corresponding intraoperative images before (left) and after (right) decompression (arrows). After surgery symptoms disappeared within 3 months (Images courtesy of Werner Schneider, MD (department of hand and plastic surgery, Dessau Rosslau Hospital/Germany))
However, the 3 T-MR-neurography can also assess the common peroneal nerve and its branches as well as the muscles supplied by them. This kind of imaging can be of advantage in obese individuals, where sonography is inferior to MRI. Furthermore, cases where differential diagnosis between different neoplasia manifestations or intraneural ganglion cysts (refer to Sects. 6.1.7 and 6.2.7 and Chap. 13) is required, and where the administration of contrast agent is needed, profit from MRI more than from ultrasound imaging [34, 103, 104]. Please also refer to Figs. 6.19 and 9.12b. Not to be neglected are the diagnostic difficulties due to the “magic angle artefact” that can mimic a mild T2-lesion in MRI, a phenomenon that has already been described in Sect. 6.2.3).
9.8.6 Treatment
Surgery of trauma-related peroneal nerve lesions is done in the prone position as microsurgery in case of a tumor mass. Surgery of focal entrapment only can easily be fulfilled in supine position, with the body turned 30° to contralateral, knee joint about 90° angulated.
We prefer an incision using the skin crease of the knee joint, leading to the lateral aspect of the popliteal fossa, and finally turning around the prominent tibio-fibular joint into a distal direction. By doing so, a triangular skin flap is lifted up from popliteal fossa fascia and fascia over the peroneal compartment. The flap allows a final skin closure which keeps the nerve far away from overlying scar tissue. At first, the fascia of the popliteal fossa is gently opened parallel to the expected nerve course, whereby we have to be aware that the nerve here is located quite superficially and very closely connected to the fascia. With the identified nerve in view, further dissection leads around the fibular bone and finally to the most delicate point where superficial and deep branches enter the peroneal compartment. The common nerve trunk has to be lifted a little; both branches are separated from each other. Then, as a final step, the muscle fascia over the peroneal compartment has to be incised far enough so that both nerve branches enter the muscle compartment free of any more trapping structure. Sometimes a vertically downward running septum between muscle bellies can also be incised. Of course, a nerve transposition which would be desirable to prevent ongoing compression between fibula and skin is impossible. Finally, all incised fascias remain unclosed, the triangle skin flap is turned back, and skin stitches have to be good enough to tolerate flexion and extension movements of the knee joint when the patient gets up. A suction drain is mandatory because venous bleeding can occur when the patient gets up into vertical position. We have observed a few times re-bleeding 24 h postoperatively after mobilization leading to deterioration of the nerve function (Fig. 9.17a, b).
Surgery of space-occupying lesions is better done in the prone position because this facilitates the surgeon’s situation, especially if magnification of the operating field by microscope is required. With the patient supine one would create a situation comparable to acoustic-neurinoma surgery with semi-sitting patients.
Ganglia beside the tibio-fibular joint as the most common tumor-like mass can occur relatively frequently as mentioned above. It is entirely thanks to the work of Spinner that we understand that these ganglia always have a connection to the joint from which they originate [105]. The surgeon should therefore address these hidden connections and ligate them [106]. Nevertheless, nobody can guarantee that these cases will not recur. Everybody can imagine the importance and amount of pre-operative information that patients now need in order to understand the prognoses of their following treatments. Just as important seems preoperative imaging to reveal such comparably difficult lesions, although MRI findings not always succeed in describing how and where to find the small joint connection. It is very difficult for a radiologist to recognize them [107]. However, careful surgery that first skeletonises a nerve and then dissects around the ganglion cyst creates a situation which should allow the revelation of such a joint connection. Intraneural multi-cystic ganglion-like lesions which can also occur require magnification and real microsurgery which we will describe in Chap. 13 in detail. It is then much more difficult or even impossible to identify and ligate a joint communication. The same necessity of microsurgery holds true when imaging reveals a nerve sheath tumor in or below the popliteal fossa.
The question of how to treat injured and sometimes extremely painful terminal branches of the superficial peroneal nerve surgically remains unanswered. Perhaps, in future, experience and high resolution of ultrasound will improve in such a way that differentiation between extraneural compression by scar tissue and intraneural neuroma-formation becomes reliably possible. We must be enabled to rely on preoperative ultrasound findings, because surgical neurolysis when initiated can only succeed in the first kind of slight nerve injuries, and mostly not in one of the latter kind of nerve damage as described in Sects. 3.2 and 4.2. We need to remember the small caliber of superficial nerve branches which does not allow microsurgery, and if tried nevertheless, easily ends as duplicated neuropathic syndrome. However, sonographic imaging of superficial nerve branch lesions will gain greatly in value in making pain authentic, e.g. in the eyes of insurance companies. The prediction of eventual surgery outcome will furthermore depend on capabilities to visualize intraneural details.
9.9 Deep Peroneal Branch at the Ankle
9.9.1 Anatomy
The final course of the deep peroneal nerve branch runs alongside the anterior tibial artery between tendons of the extensor hallucis longus and tibialis anterior muscles. At ankle level, nerve and artery are covered by the retinaculum extensorum which can be divided into a superior and an inferior one. They serve as hypomochleon of the tendons. A terminal motor branch arises under the inferior retinaculum, turns to lateral and supplies the extensor hallucis brevis and extensor digitorum brevis muscles. A terminal sensory branch represents a small inter-digital area between the first and second toes, a situation that is comparable to the sensory distribution of the posterior interosseus nerve at the dorsal surface of the hand (see Sect. 8.10.1). A focal and painful entrapment rarely occurs under the retinaculum, and since 1963 it has been termed “anterior tarsal tunnel syndrome” [108].
9.9.2 Damaging Factors
The nerve crosses the anterior ankle beneath the extensor retinaculum, a preformed situation comparable to the carpal tunnel. Tight shoes, sprains, and bone dislocations after ankle fractures may narrow the canal and thus cause a focal nerve compression [109].
9.9.3 Clinical Symptoms
Impairment of the terminal motor branch usually remains unnoticed, but it can eventually be helpful to find the diagnosis by electromyographic testing. In contrast to the motor branch, involvement of the sensory branch often causes rather painful paresthesias which radiate into the first interdigital space. An electric current-like pain component can then be triggered either typically under the retinaculum extensorum, or, quite rarely, at the level where the branch passes under the tendon of the extensor hallucis muscle. The trigger point leads to the diagnosis.
9.9.4 Treatment
Before anaesthesia, the trigger point is marked in the operating theatre. A small skin incision is done longitudinally and lateral to the tibialis anterior tendon which can easily be palpated through the skin. Special care has to be taken immediately with branches of the superficial peroneal nerve running to the medial aspect of the dorsal foot surface. They are situated subcutaneously so that injury to these branches can again cause a pain syndrome comparable to injury of the skin branches of the superficial radial nerve at the wrist (see Sect. 9.8.6). Palpation of the anterior tibial artery between the long extensor tendons leads to the small anterior tarsal tunnel. The entrance of this tunnel is covered by a fascia which has to be opened very carefully, carefully because injury of the artery will produce a questionable result. The dissection then leads to distal and finally aims at transection of one or both extensor retinacula. Palpation with your the tip of your fifth finger can exclude additional compression sites either proximal or distal. Previous literature has even reported ganglia lying between the tibialis anterior and extensor digitorum longus tendons as a possible compression factor [110].
9.10 Tibial Nerve Below the Popliteal Fossa (“Soleal Sling”)
9.10.1 Anatomy
While the tibial nerve is most commonly entrapped in the tarsal tunnel (see Sect. 9.11), more proximal entrapment sites are increasingly appreciated as a potential cause of focal tibial neuropathy. Mastalgia et al. first described a tibial nerve entrapment by the tendinous arch of the soleus muscle origin in 1981, referred to as the soleal sling [111]. The fascial arch spanning its bilateral origin from the posterior aspect of the tibia and fibula forms a sling constituting a roof over the tibial neurovascular bundle which continues into a tunnel between the superficial and deep posterior compartments containing the tibialis posterior, flexor hallucis, and flexor digitorum longus muscles [112].
9.10.2 Clinical Symptoms
Symptoms of tibial nerve entrapment under the soleal sling include popliteal fossa and proximal calf pain, weakness of toe flexion, and sensory deficits in the foot sole that are aggravated by walking [113].
9.10.3 Imaging
High-resolution ultrasound experiences in depicting this rare focal neuropathy have not existed until now but will surely arise soon. However, it is capable of demonstrating other lesions of the tibial nerve (Figs. 9.18 and 6.25a). Incidentally, the last figure is remarkable insofar as we have been once more confronted with an unexpected manifestation of a Parsonage-Turner syndrome which we describe in Sects. 6.2.8 and 10.3 in general. While radiology literature regarding the MRN appearance of this particular neuropathy is also sparse, our own experience after all consists of the fact that direct visualization of an abnormally T2 hyperintense and flattened tibial nerve at the soleal sling with proximal nerve enlargement is well possible by means of 3 T MRI and dedicated MRN sequences (Fig. 6.25b). Secondary signs of gastrocnemius and soleus muscle denervation oedema can serve as additional important findings.
9.10.4 Treatment
Patients with soleal sling entrapment neuropathy can of course benefit from soleal sling release [114]. We do not ignore our own surgical experiences in nerve decompression but the surgical approach below the popliteal fossa should be quite easy. We would try to avoid surgery as outpatient management for the same reasons discussed in Sect. 9.8, although insurance companies tend to refuse hospitalization of cases needing a simple decompression.
9.11 Tibial Nerve at the Ankle
9.11.1 Anatomy
A second preformed narrow channel at ankle level is located behind the medial malleolus. It is therefore named the “posterior or medial tarsal tunnel” [115]; its roof is formed by one or two flexor retinacula. A few centimeters above the medial malleolus, the tibial nerve starts to divide into three branches, the medial and lateral plantar nerves and a small branch to the medial aspect of the heel. The latter can penetrate the flexor retinaculum [116]. Not to be neglected, and surgically important, is the fact that the posterior tibial artery runs along the nerve branches through the tunnel. When entering the sole of the foot, the artery divides into two main branches which supply all soft tissue structures of the sole. In the case of any surgery, preservation of both arterial branches is mandatory, comparable with the necessity of preserving the ulnar artery within the Guyon’s canal. The region under the flexor retinaculum contains not only the terminal tibial nerve branches and arteries just mentioned, but also, and within a separated compartment, both tendons of the flexor digitorum longus and tibialis posterior muscles.
If we try to compare the anatomy of arteries and nerves between hand and foot, we have to bear in mind that the posterior tarsal tunnel contains both structures of the carpal tunnel and Guyon’s canal. The medial plantar nerve branch is functionally comparable to the median nerve, the lateral plantar nerve branch to the ulnar nerve, and the posterior tibial artery to the ulnar artery. It is well known that preservation of all these structures is a mandatory precondition when the tarsal tunnel is entered surgically.
9.11.2 Damaging Factors
In 1978, Steward listed a large number of factors that cause functional impairment of the tibial nerve and its branches, such as posttraumatic fibrosis, tendon sheath cysts, tenosynovitis, rheumatoid arthritis, and acromegalia, and extraneural and intraneural ganglia [117]. Multiple intraneural ganglion cysts of the tibial nerve are a particular challenge to microsurgical ability [118]. Soft tissue alterations related to hypothyroidism have been reported in literature to be associated with multiple entrapments [119]. We observed two such patients with bilateral tarsal tunnel syndromes. Keck described findings like a varicocele in the tunnel in 1962 [120]. However, on the other hand, so-called idiopathic cases of tarsal tunnel syndrome can occur as unilateral and even bilateral disorders comparable to most carpal tunnel syndromes [121]. They have the best prognosis whereas ankle distortion-related cases likely develop intraneural fibrosis so that they often can no longer improve despite a careful external nerve decompression. Because of the large variability of damaging factors at this location, preoperative imaging has already been recommended in the early periods of imaging development [122].
9.11.3 Clinical Symptoms
It cannot be mentioned often enough that the tarsal tunnel comparably contains structures of carpal tunnel and Guyon’s canal together. For this reason, the tarsal tunnel syndrome looks similar to a combination of entrapments of the median and ulnar nerves at the wrist. Therefore, the associated symptoms are not so clearly distinguishable. All muscles of the sole are involved as well as the whole skin of the plantar surface. Patients commonly suffer from severe pain over the whole plantar skin, whereas weakness or muscle atrophy within the sole remains unremarkable in the patient’s eyes. We have no reliable explanation as to why a tibial nerve entrapment is almost always associated with severe pain, whereas, for instance, the common peroneal nerve entrapment at the knee is always associated with weakness and without pain, although both nerves are mixed ones [123]. In summary, the main disturbing symptoms are paresthesias, tingling, and pain restricted to the sole, and rarely pain that radiates back into the dorsal lower leg. Some patients observed deterioration after long walking tours. The physician should ask for a Hashimoto thyreoiditis in the patient’s history because it can promote multiple entrapments as just mentioned [119]. Although spontaneous onsets and slow deteriorations are reported in the majority of cases, severe entrapments can also be related to distortions involving the ankle joint. Pain then starts early subsequent to the distortion and increases more rapidly. The posttraumatic soft tissue reaction results in extraneural and intraneural fibrosis so that even one of the neuropathic pain types can occur. These trauma-associated cases need early surgical decompression if ever possible to prevent the patient from lifelong neuropathic pain. Unfortunately, trauma itself and the necessity for tight casts over a period of time cause situations where it seems impossible to differentiate pain type and location. Consequently, the final diagnosis of a posttraumatic tarsal tunnel syndrome is often considered much later.
Very rarely, cases can occur which present with either lateral plantar branch compression or medial plantar nerve compression only. The plantar nerves may normally be damaged within the tarsal tunnel as just described, but much more rarely, more distally in their course, where they enter the sole and pierce the fascia of the abductor hallucis muscle. This fascia forms an arcade comparable to that of the supinator muscle of the forearm. At this site, isolated involvements of one of both plantar branches can be observed with clinical symptoms like a carpal tunnel or Guyon’ canal syndrome. Another variant of symptoms is an entrapment of the first sensory branch of the lateral plantar nerve only, named Baxter’s neuritis. Pain is here restricted to the medial heel.
9.11.4 Electrodiagnostics
Concerning electrodiagnostic testing of the tarsal tunnel syndrome (TTS), one would expect a prolongation of the distal latency and a delayed or absent sensory response of the plantar branches (see Sects. 5.3.1 and 5.3.2). Reliable electrodiagnostic testing is nevertheless very difficult due to the high percentage of asymptomatic subjects who yet have abnormal sensory and motor results. In a study from 1980, 33 % of asymptomatic subjects older than 55 years presented with absent medial plantar sensory conduction, and 50 % of individuals had electromyography evidence of denervation in intrinsic muscles [124]. In a systematic evidence-based review of electrodiagnostic evaluation of tarsal tunnel syndrome cases, only four papers met criteria required to meet class III level of evidence. It was concluded that nerve conduction studies may somehow be useful confirming the diagnosis. Sensory NCSs turned out as more likely to be abnormal than motor NCSs, but the actual sensitivity and specificity could not be determined. The sensitivity of needle EMG abnormalities could not finally be determined [125]. In a recent review of the literature, the continuing controversial role of electrodiagnostic techniques in TTS was again assessed. As a conclusion, the role of NCS remains controversial insofar as the inability to predict which cases will respond to decompression [126].
9.11.5 Imaging
Ultrasound is a useful examination tool because it can be performed rapidly, and the tibial nerve and its main branches (medial and lateral plantar) can be visualized on transverse and longitudinal images. Ultrasound is reliable in measuring the cross-sectional area of the tibial nerve. Despite possible small measurement errors, a side-to-side difference of approximately 1.8 mm can be interpreted as meaningful in an individual patient [127]. In a recent report on 17 cases with tarsal tunnel syndrome, the preoperative sonography diagnosis was said to be intraoperatively confirmed in all cases. The neuropathy origins were ganglia (n = 10), talocalcaneal coalition (n = 1), talocalcaneal coalition associated with ganglia (n = 3) and varicose veins (n = 3). Among the cases involving ganglia, three ganglia were not clearly palpable before surgery, and they were revealed as small. Among the cases involving talocalcaneal coalition, ultrasonography indicated a beak-shaped bony process on the short axis images [128]. Ultrasound can provide direct evidence of nerve compression, because it then demonstrates focal nerve enlargement and changes in nerve echogenicity. A synovial cyst attached to the flexor hallucis tendon can play a role [129]. Hypertrophy of the abductor hallucis muscle is one of the reported further potential compression causes affecting either one or both tibial nerve branches. In a cadaveric study, nerve compression due to abductor hallucis muscle hypertrophy was evaluated by sonography. If ultrasonographic estimation of dorso-plantar thickness is >12.8 mm and medio-lateral width >30.66 mm, an abductor hallucis muscle hypertrophy associated compression neuropathy is said to be possibly suspected [130]. Some examples are shown in Fig. 9.19.
Tarsal tunnel syndrome caused by different pathologies in HRUS imaging. (a) Tendinopathy both of the tibialis posterior and flexor halluces tendons (asterisk) displacing the tibial nerve (arrowhead). (b) Multi-cystic ganglion (asterisk) between the two plantar branches of the tibial nerve (arrowheads). (c) Ganglion (asterisk) of the tendon sheath of the flexor hallucis tendon (arrow) compressing the tibial nerve (arrowheads)
Magnetic resonance (MR) imaging, including high-resolution MR neurography, allows detailed evaluation of the course and morphology of peripheral nerves, as well as accurate delineation of surrounding soft tissue and osseous structures that may contribute to tarsal tunnel narrowing (Fig. 9.20). Even the medial calcaneal nerve can be seen on axial images and, less commonly, on sagittal images as it separates from the tibial nerve proximal to the flexor retinaculum and continues toward its subcutaneous position along the medial aspect of the hind-foot. The medial and lateral plantar nerve branches are optimally to be visualized on axial images. Additionally, the inferior calcaneal nerve can often be followed as it takes off from the lateral plantar nerve and dives toward the abductor digiti minimi muscle [130]. The tibial nerve and its branches may be compressed in the tarsal tunnel owing to trauma (fracture, surgery and scarring), space-occupying lesions (tumor, ganglia, varicosities and anomalous muscles) and foot deformities (hind-foot valgus and – less typically – hind-foot varus, with fore-foot pronation, pes planus and tarsal coalition). However, in up to 40 % of patients, an underlying cause for the tarsal tunnel syndrome is not yet identified [130]. Nevertheless, accessory muscles within the tunnel (e.g. a supplementary flexor digitorum longus muscle) can be found.
Direct evidence of trauma-related tibial nerve damage may be difficult to detect due to the small nerve caliber, but increased signal intensity, increased size and nerve course deviation may occasionally be depicted. As tarsal tunnel entrapment usually manifests rather than motor deficits, muscle denervation is still rather later to be sensed, but when present, muscle atrophy is visible more distally at the mid- or fore-foot [130].
By means of MR-neurography (MRN), isolated mild T2 hyperintensity is frequently observed during routine evaluation, likely reflecting subclinical traction/friction neuritis. Therefore, in the literature, further signs of neuropathy such as enlarged nerve fascicles, encasing perineural fibrosis and potential denervation muscle changes should also be assessed before making diagnosis of tarsal tunnel syndrome [131].
MRN may be used in a post-operative setting to evaluate the etiology of failed surgical decompression due to incomplete decompression or encasing perineural fibrosis, or even neuroma-in-continuity formation if trauma associated, and possible persistent muscle denervation changes when compared with pre-operative settings [131]
9.11.6 Treatment
Surgical treatment has to aim at:
-
1.
Pain relief by adequate nerve decompression – widely known facts since 1962 [120, 121]
-
2.
Permanent pain relief by preservation of sliding soft tissue structures in a very delicate area [132]
The latter goal is particularly difficult to achieve in a region which is extremely moved and loaded by each step. After previous negative experiences, we refuse outpatient surgical procedures, hospitalize the patient for 4–5 days, and instruct them not to unroll the operated foot for 2–3 days. These precautions prevent postoperative hematoma and reactive fibrosis which destroy sliding abilities within the tunnels.
Surgery to the posterior tarsal tunnel syndrome should only be used if pathological electrodiagnostic testing can prove the indication. The differential diagnosis for similar diseases such as plantar fasciitis only succeeds by such means. In our experience, spontaneous occurring symptoms with pathological tests have the best prognosis, whereas traumatic traction damage to the tibial nerve has a rather controversial or even bad prognosis. Cases with a neuropathic pain type in the sole, particularly after trauma, need to be discussed thoroughly preoperatively if surgical decompression or even microsurgical neurolysis is considered.
The patient may lie supine or prone; when supine, he should be turned 30° so that the region behind the malleolus comes within easy reach. The skin incision is slightly curved behind the medial malleolus; it starts about 3 cm above the malleolus in order to enable to identify artery and nerve before entering the tarsal tunnel. Palpation of the arterial pulse is helpful and indicates where the lower leg fascia has to be opened longitudinally. We remain parallel to the course of artery and nerve. When afterwards proceeding downward, the surgeon is always prevented from entering into the wrong compartment; the hypomochleon of the posterior tibial and flexor digitorum longus tendons has to be preserved. The transection of the flexor retinaculum still follows, always with the nerve or its branches, artery and its branches, and sometimes tortuous venous vessels in view. An enlarged venous plexus should be considered as the source of re-bleeding when the patient gets up. The tibial artery often shows a serpentine course, and its branches intertwine with the plantar nerve branches. Small branching vessels should be tied with bipolar forceps, keeping far from the nerves, and then transected before being disrupted. The transection of the flexor retinaculum has, of course, to be complete. Medial and lateral plantar nerve branches now pierce a fascia which covers the abductor hallucis muscle. The entrance into the sole compartment should be dissected for both nerve branches and opened enough so that ongoing compression at these sites is excluded. This area is particularly delicate insofar as the tibial artery divides there into the medial and lateral plantar arteries to form the plantar vessel arch, comparable to the hand anatomy. Rare isolated compression syndromes of either the medial or the lateral plantar nerve branch have their origin at this far distal localization, and not under the flexor retinaculum. The surgeon should therefore bear in mind that the relief does not always succeed after retinaculum transection only. This important part of the decompression just described takes place far distal and needs to extend the skin incision slightly curved under the medial malleolus ahead and never into the plantar surface. We should avoid any skin incision which is later loaded by each step.
The surgical exposure needs time and therefore requires general or spinal anaesthesia. The surgeon has to be alert to expose unusual findings such as dilated veins, unusual tenosynovitis of tendons which pass through the tarsal tunnel and hypertrophy of the abductor hallucis muscle [116]. A particular challenge arises from intraneural or extraneural ganglia which have occult communications to neighboured joints [118]. The surgeon has to manage these lesions, especially the intraneural ones, if he is unexpectedly confronted with these not quite rare lesions. In our experience, it is seldom that the surgeon succeeds in identifying a joint communication in order to avoid recurrence. Therefore, a recurrence of extra or intraneural ganglia cysts have to be borne in mind (see Sect. 13.3.8) [118]. On the other hand, preoperative high resolution ultrasound imaging of the tarsal tunnel region will gain more and more importance as described above. It is well known that local anaesthesia is completely inadequate to manage all the previously mentioned possible findings. At the end of the operation we avoid subcutaneous stitches because they can strangle the tibial nerve. A drain, with or without suction, is inserted for 2 days, and the skin stitches remain for 14 days unconditionally. The need to avoid loading the foot by the patient’s body weight for a few days has already been mentioned above (Fig. 9.21).
Treatment of the tarsal tunnel syndrome. (a) Positioning of the lower leg and skin incision. (b) Exposure; concomitant vessels and the calcaneal nerve branch have to be preserved; transection of the flexor retinaculum as the first step. (c) Release of both nerve branches at the entrance into the sole of the foot as the second step
9.12 Plantar Digital Nerve Entrapment
9.12.1 Anatomy
Four common plantar digital nerves run between the five metatarsal bones and divide into two individual branches about 0.5 cm before the metatarso-phalangeal joints. These joints are connected with each other by inter-metatarsal ligaments. Joints or tendon sheaths can develop bursa cysts. The space between joints, transverse ligaments and sometimes additional cysts is extremely small so that a very acutely noticed pain syndrome can occur as already described in 1876 by Morton [133].
9.12.2 Damaging Factors
It is well known that anatomy variations can cause slight repeated sharp compression of the small nerves. The role of an additional bursa cyst is controversial, but exposures revealed that nerve fibers and cyst membrane could not be separated from each other, a situation reminiscent of typical intraneural ganglia (see Sect. 13.3.8).
9.12.3 Clinical Symptoms
The compression causes electric current-like extensive pain normally radiating into the distribution of the affected common plantar digital nerve, the space between two contiguous toes. Mostly, the interdigital space between the third and fourth toes is involved but, in our experience, all the other interdigital spaces can alternatively or additionally be affected. The pain is characteristically provoked by walking or manually pressing the toes against each other. This phenomenon serves as a clinical test to discover the diagnosis whereby the physician can add digital pressure from plantar [134]. Apparative diagnosis has again to be assumed controversial, because routine MR imaging mostly reveals diffuse signal alterations which probably indicate inflammation of a bursa or a tenosynovitis. Common imaging cannot reliably reveal a nerve neuroma in continuity as we likely would expect. We remember a case where a neurotomy was carried out through an interdigital space with such MRI findings, whereas the patient had affirmed pain within the neighbouring space; the neurotomy resulted in a neuropathic pain syndrome in the operated and in a remaining neuralgia in the neighbouring interdigital space. Our message is therefore at present to rely on the clinical presentation and on imaging findings not before they seem to provide security. The diagnosis consists, first, of a patient’s report that the pain repeatedly radiates into a certain interdigital space, second, of positive effects by provoking maneuvers, and third, of pain disappearing after installation of local anaesthesia into the interdigital space for a period of 1–2 h. Recent reports have, however shown that high resolution ultrasound is able to detect Morton neuroma. Of typical appearance would be a hypoechoic mass within the intertarsal region that does not abut against adjacent bony structures and has either well-defined borders or is poorly marginated. A biconcave appearance of the mass (“ginkgo leaf sign”) from compression by adjacent structures may be specific [135]. An example is shown in Fig. 9.22. Again, the future will answer questions as to how we can value HRUS findings in the interdigital foot space.
9.12.4 Treatment
We completely avoid a plantar approach to protect the patient from any plantar scar, and we additionally avoid a transection of the inter-metatarsal ligament to protect the patient from static alterations of the foot. Therefore, an approach from dorsal through the inter-metatarsal bones remains mandatory. It needs a microscope, a dissector and a blunt hook, small scissors, and a small suction device. We do not apply a neurolysis as sometimes recommended [136]. Instead we prefer a neurotomy because the surgeon cannot alter the narrow anatomical situation between two bony structures or perhaps enlarge the interosseous space. On the other hand, the neurotomy bears the risk of developing a new painful neuroma at the proximal nerve end. For this reason, the neuroma has to be located far proximal, within soft tissue with less risk of being newly irritated during walking.
The approach from the dorsal surface needs a 2- to 3-cm longitudinal incision. A small self holding retractor is helpful to enter between the two metatarsal bones. A microscope for magnification should be added in any case. The approach between bulging muscle fibers into the deep plantar compartment mostly proved more difficult than expected. The assistant cannot help, the suction in your left hand helps to dissect, and the instruments in your right hand are scissors, dissector or hook. Try to preserve the inter-metatarsal artery because the management of arterial bleeding from its stumps between bulging muscle fibers is difficult. At the end, the blunt hook is needed to isolate the nerve, lift it up and transect it. Sometimes during this maneuver, small tendons of plantar muscles can mimic the nerve. Their colour is quite similar to that of the nerve because of the commen soft tissue fibrosis in the sole. If you have such a tendon under your hook, it comes out as less elastic than a nerve structure. Try to remove a small piece from one nerve end so that the pathologist can tell the patient that a neurotomy was really done.
The surgery can be done as an outpatient procedure, but then questions are raised every time on how to manage bandaging with a foot that should not be loaded for several days. A small drain which ends in the compressing bandage, without suction, prevents a postoperative hematoma.
References
Schumpelick V, Fitzgibbons RJ, editors. Hernia repair sequelae. Berlin: Springer; 2010.
Alfieri S, Rotondi F, Di Giorgia A, Fumgalli U, Salzano A, Di Miceli D, Ridolfini MP, Sgagari A, Doglietto GB, Groin Pain Trial Group. Influence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic pain. Ann Surg. 2006;243(4):553–58.
Izard G, Gailleton R, Randriansolo S, Houry R. Treatment of inguinal hernias by McVay’s technique in a series of 1332 cases. Ann Chir. 1996;50(9):755–6.
Labat JJ, Delavierre D, Sibert L, Rigaud J. Electrophysiological studies of chronic pelvic and perineal pain. Prog Urol. 2010;20(12):905–10.
Bademkiran F, Tataroglu C, Ozdedeli K, Altay B, Aydogdu I, Uludag B, Ertekin C. Electrophysiological evaluation of the genitofemoral nerve in patients with inguinal hernia. Muscle Nerve. 2005;32(5):600–4.
Karakayali F, Karatas M, Ozcelik U, Ekici Y, Basaran O, Moray G, Haberal M. Influence of synthetic mesh on ilioinguinal nerve motor conduction and chronic groin pain after inguinal herniorrhaphy: a prospective randomized clinical study. Int Surg. 2007;92(6):344–50.
Knockaert DC, Boonen AL, Bruyninckx FL, Bobbaers HJ. Electromyographic findings in ilioinguinal-iliohypogastric nerve entrapment syndrome. Acta Clin Belg. 1996;51(3):156–60.
Dias RJS, de Souza L, de Morais WF, Carneiro AP. SEP diagnosing neuropathy of the lateral cutaneous branch of the iliohypogastric nerve. Arq Neuropsiquiatr. 2004;62(3-B):895–8.
Eichenberger U, Greher M, Kirchmair L, Curatolo M, Moriggl B. Ultrasound-guided blocks of the ilioinguinal and iliohypogastric nerve: accuracy of a selective new technique confirmed by anatomical dissection. Br J Anaesth. 2006;97(2):238–43.
Peng PWH, Tumber PS. Ultrasound-guided interventional procedures for patients with chronic pelvic pain a description of techniques and review of literature. Pain Physician. 2008;11(2):215–24.
Soneji N, Wenn Hsin Peng P. Ultrasound-Guided Pain Interventions – A Review of Techniques for Peripheral Nerves. Korean J Pain 2013; 26(2):111–124.
Fisher HW, Lotze PM. Nerve injury locations during retropubic sling procedures. Int Urogynecol J. 2011;22(4):439–41.
Chhabra A, Andreisek G. Magnetic resonance neurography. First Editionth ed. New Delhi/Panama City/London: Jaypee Brothers; 2012. p. 172–5. ISBN ISBN 978-93-5025-568-1.
Melzack R, Wall P. Pain mechanisms: a new theory. Science. 1965;150:971–9.
Shetter AG, Racz GB, Lewis R, Heavner JE. Peripheral nerve stimulation. In: North RB, Levy RM, editors. Neurosurgical management of pain. New York: Springer; 1997. p. 261–70.
Penkert G, Fansa H. Peripheral nerve lesions. Berlin: Springer; 2004. p. 123–4.
Possover M, Baeklandt J, Chiantera V. The Laparoscopic Implantation of Neuroprothesis-(LION) procedure to control intractable abdomino-pelvic neuralgia. Neuromodulation. 2007;10:18–23.
Winkelmüller M. Long term results of peripheral nerve stimulation in neuropathic pain. 8th Annual Meeting of the German Society of Neuromodulation (DGNM), Joint Meeting with the Neuromodulation Society of the United Kingdom and Ireland (NSUKI). Berlin. 23–24 Nov 2012.
Wolter T, Winkelmüller M. Continuous versus intermittant spinal cord stimulation: an analysis of factors influencing clincal efficacy. Neuromodulation. 2012;15:13–20.
Jefferson D, Eames RA. Subclinical entrapment of the lateral femoral cutaneous nerve: an autopsy study. Muscle Nerve. 1979;2:145–54.
Boon AJ, Bailey PW, Smith J, Sorenson EJ, Harper CM, Hurdle MF. Utility of ultrasound-guided surface electrode placement in lateral femoral cutaneous nerve conduction studies. Muscle Nerve. 2011;44(4):525–30.
Aszmann OC, Dellon ES, Dellon AL. Anatomical course of the lateral femoral cutaneous nerve and its susceptibility to compression and injury. Plast Reconstr Surg. 1997;100(3):600–4.
Deimel GW, Hurst RW, Sorenson EJ, Boon AJ. Utility of ultrasound-guided near-nerve needle recording for lateral femoral cutaneous sensory nerve conduction study: does it increase reliability compared with surface recording? Muscle Nerve. 2013;47(2):274–6.
Russo MJ, Firestone LB, Mandler RN, Kelly Jr JJ. Nerve conduction studies of the lateral femoral cutaneous nerve. Implications in the diagnosis of meralgia paresthetica. Am J Electroneurodiagnostic Technol. 2005;45(3):180–5.
Shin YB, Park JH, Kwon DR, Park BK. Variability in conduction of the lateral femoral cutaneous nerve. Muscle Nerve. 2006;33(5):645–9.
Seror P, Seror R. Meralgia paresthetica: clinical and electrophysiological diagnosis in 120 cases. Muscle Nerve. 2006;33(5):650–4.
el-Tantawi GA. Reliability of sensory nerve-conduction and somatosensory evoked potentials for diagnosis of meralgia paraesthetica. Clin Neurophysiol. 2009;120(7):1346–51.
Zhu J, Zhao Y, Liu F, Huang Y, Shao J, Hu B. Ultrasound of the lateral femoral cutaneous nerve in asymptomatic adults. BMC Musculoskelet Disord. 2012;13:227. doi:10.1186/1471-2474-13-227.
Aravindakannan T, Wilder-Smith EP. High-resolution ultrasonography in the assessment of meralgia paresthetica. Muscle Nerve. 2012;45(3):434–5.
Suh DH, Kim DH, Park JW, Park BK. Sonographic and electrophysiologic findings in patients with meralgia paresthetica. Clin Neurophysiol. 2013;124(7):1460–4. doi:10.1016/j.clinph.2013.02.003. Epub 2013 Mar 7.
Shannon J, Lang SA, Yip RW, Gerard M. Lateral femoral cutaneous nerve block revisited. A nerve stimulator technique. Reg Anesth. 1995;20(2):100–4.
Tagliafico A, Serafini G, Lacelli F, Perrone N, Valsania V, Martinoli C. Ultrasound-guided treatment of meralgia paresthetica (lateral femoral cutaneous neuropathy): technical description and results of treatment in 20 consecutive patients. J Ultrasound Med. 2011;30(10):1341–6.
Fowler IM, Tucker AA, Mendez RJ. Treatment of meralgia paresthetica with ultrasound-guided pulsed radiofrequency ablation of the lateral femoral cutaneous nerve. Pain Pract. 2012;12(5):394–8.
Petchprapa CN, Rosenberg ZS, Sconfienza LM, Cavalcanti CF, Vieira RL, Zember JS. MR imaging of entrapment neuropathies of the lower extremity. Part 1. The pelvis and hip. Radiographics. 2010;30(4):983–1000.
Mirzai S, Sepehrnia A, El Azm M, Penkert G, Samii M. Results of surgical treatment of meralgia paresthetica. In: Lorenz R, Klinger M, Brock M, editors. Advances in neurosurgery. Springer: Berlin; 1993. p. 268–73.
Aldrich EF, vd Heever CM. Suprainguinal ligament approach for surgical treatment of meralgia paresthetica. J Neurosurg. 1989;70:492–4.
Craig WS, Clark JMP. Obturator palsy in the newly born. Arch Dis Child. 1962;37:661–2.
Uludag B, Ertekin C, Turman AB, Demir D, Kiylioglu N. Proximal and distal motor nerve conduction in obturator and femoral nerves. Arch Phys Med Rehabil. 2000;81(9):1166–70.
Park BG. Obturator nerve conduction study using magnetic stimulation in healthy adults. J Korean Acad Rehabil Med. 1998;22(3):647–50.
Bradshaw C, McCrory P, Bell S, Brukner P. Obturator neuropathy: a cause of chronic groin pain in athletes. Am J Sports Med. 1997;25:402–8.
Soong J, Schafhalter- Zoppoth I, Gray AT. Sonographic imaging of the obturator nerve for regional block. Reg Anesth Pain Med. 2007;32(2):146–51.
Simeofori dou M, Bareka M, Basdekis G, Tsiaka K, Chantzi E, Vretzakis G. Peripheral nerve blockade as an exclusive approach to obturator nerve block in anterior cruciate ligament reconstructive surgery. Korean J Anesthesiol. 2013;65(5):410–7. doi: 10.4097/kjae.2013.65.5.410. Epub 2013 Nov 29.
Sinha SK, Abrams JH, Houle TT, Weller RS. Ultrasound-guided obturator nerve block: an interfascial injection approach without nerve stimulation. Reg Anesth Pain Med. 2009;34(3):261–4.
Millesi H. Chirurgie der peripheren Nerven. München: Urban & Schwarzenberg; 1992. p. 218–22.
Birch R, Bonney G, Wynn Parry CB. Surgical disorders of the peripheral nerves. Edinburgh: Churchill Livingstone; 1998. p. 288–9.
Ma DM, Liveson JA. Nerve conduction handbook. Philadelphia: F.A. Davis; 1983.
Chang CW, Shieh SF, Li CM, et al. Measurement of motor nerve conduction velocity of the sciatic nerve in patients with piriformis syndrome: a magnetic stimulation study. Arch Phys Med Rehabil. 2006;87(10):1371–5.
Dumitru CW, Amato A, Zwarts M. Electrodiagnostic medicine. 2nd ed. Philadelphia: Hanley Belfus; 2002. p. 873.
Russell JM, Kransdorf MJ, Bancroft LW, et al. Magnetic resonance imaging of the sacral plexus and piriformis muscles. Skeletal Radiol. 2008;37(8):709–13.
Filler AG, Haynes J, Jordan SE, et al. Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine. 2005;2(2):99–115.
Chhabra A, Chalian M, Soldatos T, et al. 3-T high-resolution MR neurography of sciatic neuropathy. AJR Am J Roentgenol. 2012;198(4):W357–64.
Pecina HI, Boric I, Smoljanovic T, et al. Surgical evaluation of magnetic resonance imaging findings in piriformis muscle syndrome. Skeletal Radiol. 2008;37(11):1019–23.
Robinson DR. Pyriformis syndrome in relation to sciatic pain. Am J Surg. 1947;73:355–8.
Hobbs JT. The pelvic congestion syndrome. Br J Hosp Med. 1990;73:355–8.
Desimpelaere JH, Seynaeve PC, Hagers YM, Appel BJ, Mortelmans LL. Pelvic congestion syndrome: demonstration and diagnosis by helical CT. Abdom Imaging. 1999;24:100–2.
Amarenco G, Lanoë Y, Perrigot M, et al. Un nouveau syndrome canalaire: la compression du nerf honteux interne dans le canal d’Alcock ou paralysie perineale du cycliste. Presse Med. 1987;16:399.
Goodson JD. Pudendal neuritis from biking. N Engl J Med. 1981;304:65.
Stewart JD. Focal peripheral neuropathies. New York: Elsevier; 1987. p. 275.
Vancaille T, Eggermont J, Armstrong G, Jarvis S, Liu J, Beg N. Response to pudendal nerve block in women with pudendal neuralgia. Pain Med. 2012;13(4):596–603.
Durante JA, Macintyre IG. Pudendal nerve entrapment in an ironman athlete: a case report. J Can Chiropr Assoc. 2010;54(4):276–81.
Lefaucheur JP. Neurophysiological testing in anorectal disorders. Muscle Nerve. 2006;33(3):324–33.
Labat JJ, Riant T, Robert R, Amarenco G, Lefaucheur JP, Rigaud J. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourol Urodyn. 2008;27(4):306–10.
Lefaucheur JP, Labat JJ, Amarenco G, Herbaut AG, Prat-Pradal D, Benaim J, Aranda B, Arne-Bes MC, Bonniaud V, Boohs PM, Charvier K, Daemgen F, Dumas P, Galaup JP, Sheikh Ismael S, Kerdraon J, Lacroix P, Lagauche D, Lapeyre E, Lefort M, Leroi AM, Opsomer RJ, Parratte B, Prévinaire JG, Raibaut P, Salle JY, Scheiber-Nogueira MC, Soler JM, Testut MF, Thomas C. What is the place of electroneuromyographic studies in the diagnosis and management of pudendal neuralgia related to entrapment syndrome? Neurophysiol Clin. 2007;37(4):223–8.
Tagliafico A, Perez MM, Martinoli C. High-resolution ultrasound of the pudendal nerve: normal anatomy. Muscle Nerve. 2012. doi:10.1002/mus.23537. Epub ahead of print.
Filler AG. Diagnosis and management of pudendal nerve entrapment syndromes: impact of MR neurography and open MR-guided injections. Neurosurg Q. 2008;18:1–6.
Hough DM, Wittenberg KH, et al. Chronic perineal pain caused by pudendal nerve entrapment: anatomy and CT-guided perineural injection technique. AJR Am J Roentgenol. 2003;181:561–7.
Bisschop E, Nundlall R. Surgical decompression of pudendal nerve by transperineal approach using a probe with a small balloon. J Gynecol Obstet Biol Reprod. 2011;40(3):225–30.
Richter EO, Abramowa MV, Aló KM. Percutaneous cephalocaudal implantation of epidural stimulation electrons over sacral nerve roots – a technical note on the importance of the lateral approach. Neuromodulation. 2011;14(1):62–7.
Rigoard P, Delmotte A, et al. Successful treatment of pudendal neuralgia with tricolumn spinal cord stimulation: case report. Neurosurgery. 2012;71(3):757–63.
Robert R, Labat J-J, Riant T, Louppe J-M, Hammel O. The pudendal nerve: clinical and therapeutic morphogenesis, anatomy, and pathophysiology. Neurochirurgie. 2009;55:463–9.
Putz R, Sobotta PR. Atlas der Anatomie des Menschen. 21st ed. München: Urban & Fischer; 2002; Figs. 1127, 1131.
Chandler SB. The iliospsoas bursa in man. Anat Rec. 1934;58:235–40.
Lavyne MH, Voorhies RM, Coll RH. Femoral neuropathy caused by an iliopsoas bursal cyst. J Neurosurg. 1982;56:584–6.
Kuntzner T, van Melle G, Regli F. Clinical and prognostic features in unilateral femoral neuropathies. Muscle Nerve. 1997;20(2):205–11.
Dumitru CW, Amato A, Zwarts M. Electrodiagnostic medicine. 2nd ed. Philadelphia: Hanley Belfus; 2002. p. 878.
Huang Y, Zhu J, Liu F. Ultrasound in diagnosis of retroperitoneal femoral nerve injury: a case report. J Plast Reconstr Aesthet Surg. 2013;66(2):e50–2. doi:10.1016/j.bjps.2012.11.023. Epub 2012 Dec 12.
Chhabra A, Faridian-Aragh N. High-resolution 3-T MR neurography of femoral neuropathy. AJR Am J Roentgenol. 2012;198(1):3–10. doi:10.2214/AJR.11.6676.
Kline DG, Hudson AR. Nerve injuries. Philadelphia: W B Saunders; 1995. p. 334–5.
Chiu WS. The syndrome of retroperitoneal hemorrhage and lumbar plexus neuropathy during anticoagulant therapy. South Med J. 1976;69:595–9.
Ledermann RJ, Breuer AC, Hanson MR, et al. Peripheral nervous system complications of coronary artery bypass graft surgery. Ann Neurol. 1982;12:297–301.
Mozes M, Ouakrisne G, Nathan H. Saphenus nerve entrapment simulating vascular disorder. Surgery. 1975;77:299–303.
Wainapel SF, Kim DJ, Ebel A. Conduction studies of the saphenous nerve in healthy subjects. Arch Phys Med Rehabil. 1978;59(7):316–9.
Bianchi S, Martinoli C, Demondion X. Ultrasound of the nerves of the knee region: technique of examination and normal US appearance. J Ultrasound. 2007;10(2):68–75. Published online 2007 June.
Le Corroller T, Lagier A, Pirro N, et al. Anatomical study of the infrapatellar branch of the saphenous nerve using ultrasonography. Muscle Nerve. 2011;44(1):50–4. doi:10.1002/mus.22004.
Masakado Y, Kawakami M, Suzuki K, Abe L, Ota T, Kimura A. Clinical neurophysiology in the diagnosis of peroneal nerve palsy. Keio J Med. 2008;57(2):84–9.
Buschbacher RM. Peroneal nerve motor conduction to the extensor digitorum brevis. Am J Phys Med Rehabil. 1999;78(6-Suppl):26–31.
Singh N, Behse F, Buchthal F. Electrophysical study of peroneal palsy. J Neurol Neurosurg Psychiatry. 1974;37(11):1202–13.
Raudino F. Electrophysiological study of peroneal nerve palsy at the fibular head. Electromyogr Clin Neurophysiol. 1996;36(7):439–40.
Katirji MB, Wilbourn AJ. Common peroneal mononeuropathy: a clinical and electrophysiologic study of 116 lesions. Neurology. 1988;38(11):1723–8.
Rayegani SM, Daneshtalab E, Bahrami MH, Eliaspour D, Raeissadat SA, Rezaei S, Babaee M. Prevalence of accessory deep peroneal nerve in referred patients to an electrodiagnostic medicine clinic. J Brachial Plex Peripher Nerve Inj. 2011;6(1):3. doi:10.1186/1749-7221-6-3.
Buschbacher RM. Reference values for peroneal nerve motor conduction to the tibialis anterior and for peroneal vs. tibial latencies. Am J Phys Med Rehabil. 2003;82(4):296–301.
Kanakamedala RV, Hong CZ. Peroneal nerve entrapment at the knee localized by short segment stimulation. Am J Phys Med Rehabil. 1989;68(3):116–22.
Kokotis P, Kolovou D, Papagianni A, Zambelis T, Karandreas N. The two sensory branches of the superficial peroneal nerve: electrophysiological differences and correlations with gender, age, height and BMI. Neurophysiol Clin. 2009;39(3):143–7.
Marchini C, Zambito Marsala S, Fabris F, Fornasier A, Ferracci F. Peroneal nerve orthodromic sensory conduction technique: normative data. Neurol Sci. 2009;30(3):201–5.
Lo YL, Fook-Chong S, Leoh TH, Dan YF, Tan YE, Lau WH, Chan LL. High-resolution ultrasound as a diagnostic adjunct in common peroneal neuropathy. Arch Neurol. 2007;64(12):1798–800.
Canella C, Demondion X, Guillin R, Boutry N, Peltier J, Cotten A. Anatomic study of the superficial peroneal nerve using sonography. AJR Am J Roentgenol. 2009;193(1):174–9.
Visser LH, Hens V, Soethout M, De Deugd-Maria V, Pijnenburg J, Brekelmans GJ. Diagnostic value of high-resolution sonography in common fibular neuropathy at the fibular head. Muscle Nerve. 2013;48(2):171–8. doi:10.1002/mus.23729. Epub 2013 Jun 26.
Vasudevan JM, Freedman MK, Beredjiklian PK, Deluca PF, Nazarian LN. Common peroneal entrapment neuropathy secondary to a popliteal lipoma: ultrasound superior to magnetic resonance imaging for diagnosis. PM R. 2011;3(3):274–9.
Jang SH, Lee H, Han SH. Common peroneal nerve compression by a popliteal venous aneurysm. Am J Phys Med Rehabil. 2009;88(11):947–50.
Rawal A, Ratnam KR, Yin Q, Sinopidis C, Frostick SP. Compression neuropathy of common peroneal nerve caused by an extraneural ganglion: a report of two cases. Microsurgery. 2004;24(1):63–6.
Visser LH. High-resolution sonography of the common peroneal nerve: detection of intraneural ganglia. Neurology. 2006;67(8):1473–5.
Snaith R, Dolan J. Ultrasound-guided superficial peroneal nerve block for foot surgery. AJR Am J Roentgenol. 2010;194(6):W538. doi:10.2214/AJR.09.3975; author reply W542.
Kim JY, Ihn YK, Kim JS, Chun KA, Sung MS, Cho KH. Non-traumatic peroneal nerve palsy: MRI findings. Clin Radiol. 2007;62(1):58–64.
Subhawong TK, Wang KC, Thawait SK, Williams EH, Hashemi SS, Machado AJ, Carrino JA, Chhabra A. High resolution imaging of tunnels by magnetic resonance neurography. Skeletal Radiol. 2012;41(1):15–31.
Spinner RJ, Atkinson JLD, Scheithauer BW, et al. Peroneal intraneural ganglia. The importance of the articular branch: clinical series. J Neurosurg. 2003;99:319–29.
Spinner RJ, Atkinson JLD, Tiel RL. Peroneal intraneural ganglia. The importance of the articular branch: a unifying theory. J Neurosurg. 2003;99:330–43.
Spinner RJ, Edwards PK, Amrami KK. Application of three-dimensional rendering in joint related ganglia. Clin Anat. 2006;19:312–22.
Kopell DM, Thomson WAL. Peripheral entrapment neuropathies. Baltimore: William and Wilkins; 1963. p. 171.
Gessini L, Jandolo B, Pietrangeli A. The anterior tarsal syndrome: report of four cases. J Bone Joint Surg. 1984;66 A:786–7.
Brooks DM. Nerve compression by simple ganglia: a review of thirteen collected cases. J Bone Joint Surg. 1952;34 B:391–400.
Subhawong TK, Wang KC, Thawait SK, et al. High resolution imaging of tunnels by magnetic resonance neurography. Skeletal Radiol. 2012;41(1):15–31. doi:10.1007/s00256-011-1143-1. Epub 2011 Apr 10.
Mastaglia FL, Venerys J, Stokes BA, Vaughan R. Compression of the tibial nerve by the tendinous arch of origin of the soleus muscle. Clin Exp Neurol. 1981;18:81–5.
Williams EH, Williams CG, Rosson GD, Dellon LA. Anatomic site for proximal tibial nerve compression: a cadaver study. Ann Plast Surg. 2009;62:322–5.
Mastaglia FL. Tibial nerve entrapment in the popliteal fossa. Muscle Nerve. 2000;23:1883–6.
Marinacci AA. Neurological syndromes of the tarsal tunnels. Bull Los Angeles Neurol Soc. 1968;33:90–100.
Edwards WG, Lincoln CR, Bassett TH, Goldner L. The tarsal tunnel syndrome. JAMA. 1969;207:716–20.
Stewart JD. Focal peripheral neuropathies. New York: Elsevier; 1987. p. 313–4.
Spinner RJ, Atkinson JCD, Harper CM, et al. Recurrent intraneural ganglion cysts of the tibial nerve. J Neurosurg. 2000;92:334–7.
Fritze J, Kountouris D. Hashimoto-Thyreoiditis mit Polyneuropathie und multiplen Engpaß-Syndromen. Nervenarzt. 1984;55:549–55 (German).
Keck C. The tarsal-tunnel syndrome. J Bone Joint Surg. 1962;44 A:180–2.
Lam SJS. A tarsal-tunnel syndrome. Lancet. 1962;2:1354–5.
Kerr R, Frey C. MR imaging in tarsal tunnel syndrome. J Comput Assist Tomogr. 1991;15(2):280–6.
Gerhard L, Reinhardt V, Koob E, Nau H-E. Morphological and pathogenetic considerations in entrapment syndromes. In: Samii M, editor. Peripheral nerve lesions. Berlin: Springer; 1990. p. 278–87.
Fealey RD, Litchy WJ, Daube JR. Plantar nerve stimulation in evaluation of peripheral nerves. Neurology. 1980;30:412.
Patel AT, Gaines K, Malamut R, Park TA, American Association of Neuromuscular and Electrodiagnostic Medicine, et al. Usefulness of electrodiagnostic techniques in the evaluation of suspected tarsal tunnel syndrome: an evidence-based review. Muscle Nerve. 2005;32(2):236–40.
Ahmad M, Tsang K, Mackenney PJ, Adedapo AO. Tarsal tunnel syndrome: a literature review. Foot Ankle Surg. 2012;18(3):149–52. doi:10.1016/j.fas.2011.10.007. Epub 2011 Dec 21.
Alshami AM, Cairns CW, Wylie BK, et al. Reliability and size of the measurement error when determining the cross-sectional area of the tibial nerve at the tarsal tunnel with ultrasonography. Ultrasound Med Biol. 2009;35(7):1098–102. doi:10.1016/j.ultrasmedbio.2009.01.011. Epub 2009 May 7.
Nagaoka M, Matsuzaki HJ. Ultrasonography in tarsal tunnel syndrome. J Ultrasound Med. 2005;24(8):1035–40.
Therimadasamy AK, Seet RC, Kagda YH, et al. Combination of ultrasound and nerve conduction studies in the diagnosis of tarsal tunnel syndrome. Neurol India. 2011;59(2):296–7. doi:10.4103/0028-3886.79152.
Ghosh SK, Raheja S, Tuli A. Potential sites of compression of tibial nerve branches in foot: a cadaveric and imaging study. Anat Clin. 2012. doi:10.1002/ca.22203.
Donovan A, Rosenberg ZS, Cavalcanti C. MR imaging of entrapment neuropathies of the lower extremity. Part 2. The knee, leg, ankle, and foot. Radiographics. 2010;30:1001–19.
Millesi H, Hausner T, Schmidhammer R, Trattnig S, Tschabitscher M. Anatomical structures to provide passive motility of peripheral nerve trunks and fascicles. Acta Neurochir Suppl. 2007;100:133–5.
Morton TG. A peculiar and painful affection about the fourth metatarsophalangeal articulation. Am J Med Sci. 1876;71:37–45.
Mulder JD. The causative mechanism in Morton’s metatarsalgia. J Bone Joint Surg. 1951;33 B:94–5.
Park HJ, Kim SS, Rho MH, Hong HP, Lee SY. Sonographic appearances of Morton’s neuroma: differences from other interdigital soft tissue masses. Ultrasound Med Biol. 2011;37(8):1204–9.
Gauthier GT. Morton’s disease : a nerve entrapment syndrome. A new surgical technique. Clin Orthop. 1979;142:90–2.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Böhm, J., Penkert, G., Schelle, T. (2015). Nerve Entrapment at Trunk and Leg. In: Focal Peripheral Neuropathies. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-54780-5_9
Download citation
DOI: https://doi.org/10.1007/978-3-642-54780-5_9
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-54779-9
Online ISBN: 978-3-642-54780-5
eBook Packages: MedicineMedicine (R0)