Abstract
Although generally considered benign, the biological behaviour of meningiomas varies considerably. The microscopic histopathological classification of the World Health Organization (WHO) cannot entirely predict the clinical behaviour of these tumours. Between 7 and 32 % of benign meningiomas recur after total resection, and between 19 and 50 % (or more) after subtotal removal. Quantifying the proliferative potential may help to predict the biological behaviour of individual tumours of comparable histology. The prognostic significance of various proliferative indices in meningiomas has already been assessed and it has been suggested that the tumour proliferative potential can predict the patient’s clinical course. The nuclear antigen Ki-67 expressed by proliferating cells has become available for routinely processed paraffin section. The Mib-1 antibody detects an epitope on the Ki-67 antigen, a nuclear protein present only during active phases of the cell cycle (G1, S, G2 and M).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Although generally considered benign, the biological behaviour of meningiomas varies considerably. The microscopic histopathological classification of the World Health Organization (WHO) cannot entirely predict the clinical behaviour of these tumours [21]. Between 7 and 32 % of benign meningiomas recur after total resection, and between 19 and 50 % (or more) after subtotal removal [6, 17]. Quantifying the proliferative potential may help to predict the biological behaviour of individual tumours of comparable histology. The prognostic significance of various proliferative indices in meningiomas has already been assessed and it has been suggested that the tumour proliferative potential can predict the patient’s clinical course [1, 35, 36, 38, 39]. The nuclear antigen Ki-67 expressed by proliferating cells has become available for routinely processed paraffin section [12]. The Mib-1 antibody detects an epitope on the Ki-67 antigen, a nuclear protein present only during active phases of the cell cycle (G1, S, G2 and M). The higher incidence of meningiomas among women, their behaviour during pregnancy and the reported epidemiological link between meningiomas and breast carcinomas have led to the assumption that sex steroid hormones may influence the growth of meningiomas [28, 34]. Supported by promising results in breast cancer therapy, new chemotherapeutic approaches based on hormone manipulation were tested in meningioma patients [25]. Meningiomas are highly vascularized tumours. Neoangiogenesis has been correlated to biological aggressiveness as it enables neoplasms to grow beyond the limits given by the host vessels [10]. Therefore, neoplasms able to produce angiogenetic factors are more prone to spread and recurrence. The quantity of neoangiogenesis is a prognostic parameter in several neoplasias [7, 49]. The prognostic value of angiogenesis also has been studied extensively in meningiomas using microvessel density or vascular endothelial growth factor (VEGF) [2, 3, 26, 42].
Decisions regarding patient management therefore rely on a variety of clinical, radiological and pathological prognosticators as the clinical behaviour of meningiomas with a tendency to recur led to the assumption that meningiomas cannot be classified as a benign entity despite their pathological classification.
1 Materials and Methods
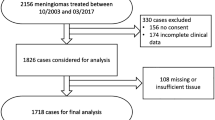
Based on a database of 1,766 meningiomas treated on at the Neurosurgical Department, Klinikum Hannover Nordstadt (1979–2002), and 953 meningiomas at University Hospital Tübingen (2004–2012), all of these tumours were analysed according to the current WHO classification. Five hundred eighty-eight paraffin blocks of 554 patients with intracranial meningiomas, operated between 1990 and 2000, were randomly retrieved from the archives of the Department of Pathology for immunohistochemical analysis. All of these patients were followed for a median of 74 months or until death. The material included 45 patients with neurofibromatosis type 2 disease (for a total of 62 tumours). Later on in Tübingen, cell culture studies were performed to further analyse growth behaviour and influence thereof.
Meningioma subtypes were defined according to the new WHO classification. Immunohistochemistry was performed with paraffin sections using Anti-Mib-1 and antihuman progesterone receptor 1A6. For Ki-67, the area of densest staining (‘hot spot’) was searched for and counting was performed in 10 contiguous fields. The average of the results in these fields determined the proliferative index (LI). The progesterone receptor status was determined by a semi-quantitative scoring scale according to the immunoreactive score (IRS) of Remmele et al., with respect to staining intensity and percentage of positive tumour cells [44].
1.1 Immunofluorescence
An immunocytochemical analysis was performed on primary cell culture growing in a monolayer fashion in culture. The cells were plated in 4-well glass slides and allowed to remain in growth media for 24 hours (h). After removal of the growth media, the slides were rinsed with PBS for 5 minutes (min) followed by fixation in methanol for 15 min at – 20 °C. The slides were rinsed with PBS and cells were blocked with 10 % horse serum in PBS for 30 min at room temperature (RT). Slides were incubated with primary antibodies overnight at 4 °C. Staining was developed using the secondary fluorescence antibody Alexa Fluor 488 (1:200) for 1 h at RT in the dark. The slides were mounted with DAPI-containing fluorescence mounting medium (Vector Laboratories, Burlingame, CA) (Fig. 3.1).
1.2 Immunocytochemical Staining
An immunocytochemical analysis was performed on meningioma cells growing in a monolayer fashion in culture. The cells were plated in 4-well glass slides and allowed to remain in growth media for 24 h. After removal of the growth media, the cells were rinsed with PBS for 5 min followed by fixation with ice-cold methanol for 10 min at – 20 °C. The slides were rinsed with PBS and incubated with 3 % H2O2 for 10 min at RT. All cells were blocked with 10 % rabbit serum in PBS for 30 min at room temperature. Slides were incubated with primary antibodies overnight at 4 °C. Staining was developed using the VECTASTAIN Elite ABC system and Vector® NovaRED™ (Vector Laboratories, Burlingame, CA). Sections were counterstained with haematoxylin and examined by light microscopic studies (Fig. 3.2).
1.3 Senescence-Associated β-Galactosidase Staining
Expression of senescent-associated β-galactosidase activity was analysed in different passages of primary meningioma cell cultures using the Cellular Senescence Detection Kit (BioVision, Milpitas, CA) (Fig. 3.3).
2 Results
The mean Mib-1 SI in male patients was 5.8 %, whereas that of female patients was 3.9 %; patients with NF-II show significant higher mean Ki-67 LI (6.2 %). Ki-67 LI in WHO I tumours was significantly lower than in WHO II (atypical) and WHO III (anaplastic) (p < 0.0001), but not within the subclassifications of WHO grading (meningotheliomatous 3.3 %, fibrous 3.9 %, transitional 2.9 %, psammomatous 1.1 %, angiomatous 3.0 %, clear cell 0.7 % or microcystic meningiomas 4.4 %) (Table 3.1). First time treated meningiomas had a mean Ki-67 LI of 3.9 % versus 6.9 % in recurrent meningiomas (P < 0.0001). Ki-67 LI increases from the initial tumour operation to its second, third and in 5 cases to its fourth local recurrence. There was a transformation from benign to atypical meningioma from second to third local recurrence in 16 % of the cases, whereas no dedifferentiation from WHO I to WHO III or WHO II to WHO III has been seen. Significantly lower PR expression in WHO II (atypical) and III (anaplastic) meningiomas, compared to WHO I meningiomas, has also been observed.
Excluding WHO II and III meningiomas, as well as partially resected meningiomas for survival analysis, in WHO I and SI resected meningiomas, no significant difference in survival according to different mean Ki-67 LI or PR status has been found. Combining two factors of proposed prognostic significance in benign meningiomas – proliferation index (Ki-67 LI < 4 % vs. ≥ 4 %) and PR status (neg. vs. pos.) – a significant decreased recurrence-free survival could be shown for negative PR status and Ki-67 LI ≥ 4 % (Fig. 3.4).
For proliferation and PR status analysis, multiple age groups for each sex have been examined as well (<40, 41–55, 56–70 and >70), but no significance has been seen (Fig. 3.5). No relationship between the calcifications, meningioma subtype or proliferation index could be established. Although recurrent meningiomas exhibit higher proliferation rates in general, no age dependency has been seen.
3 Discussion
Meningiomas are mostly benign tumours that usually do not invade the brain parenchyma. The WHO grading system aiming to describe different types of tumour frequently fails to determine the clinical behaviour of meningiomas. Even in cases of complete removal according to the Simpson classification the chance of recurrence is high [52]. Pathological specimens in those cases do not show either atypical features or histopathological signs of increased biological activity. Proliferation markers like BrdU or biochemical markers like telomerase and topoisomerase IIα have been used to describe the clinical course in meningioma patients [8, 51]. In the case of BrdU Gudjonssona et al. a PET study showed that BrdU is not suitable as proliferation marker [14]. Whereas telomerase is a potential predictor for recurrence in meningiomas [18, 30], there are conflicting results for topoisomerase IIα as predictor for recurrence in meningiomas [23, 24].
The Mib-1 monoclonal antibody, staining the Ki-67 antigen, has demonstrated its reliability in analysing meningioma growth and recurrence by several authors [1, 33, 36, 39, 47, 48].
Møller separated different resection grades and histology before survival analysis in 25 cases and could not give any significant prediction with Ki-67 immunohistochemistry as well [35]. Abramovich reported the absence of a significant difference in proliferation in 59 meningioma patients that had been radically operated, recognizing a clear overlap of the index range between the groups [1]. On the contrary, Ohta et al. showed a correlation with recurrence-free interval in 42 patients, but the follow-up time was 60 months and the statistics were performed without dividing the meningiomas according to the WHO classification [38]. Perry et al. showed values for interpretation of borderline atypical meningiomas in 425 meningiomas through multivariate analysis [39]. Brain invasion, mitosis count > 3/10 and a mean Ki-67 LI > 4.2 % correlated with decreased recurrence-free survival. Matsuno et al. and Nakasu et al. reported a 3.2 and 3 % cut-off point for higher recurrence tendency [33, 36]. However, 20–50 % of the recurrent meningioma groups were atypical, and all nonrecurrent meningiomas were WHO I. Survival analysis was performed taking all patients together without dividing for surgical resection or histological grade. The small number of patients in each group and the uneven distribution of histological grades might have additionally influenced the mean LI and the survival analysis. Failing to separate different histopathological and resection grades exposes these studies to the criticism that Ki-67 may simply describe a well-known phenomenon, in other words that more aggressive histology and less aggressive regression correlate with shorter disease-free survival times.
Elevated proliferative activity in recurrent meningiomas throughout the histological grouping has been shown [1, 33, 35, 36, 38]. A decrease of the LI has only been reported by Madsen et al. [29]. Caution is recommended when using the proliferation index as the sole prognostic indicator or as a substitute for morphological diagnosis due to the overlap in each group (WHO I mean Ki-67 LI 0–30 %, WHO II mean Ki-67 LI 3–35 % or WHO III mean Ki-67 LI 5–58 %) [19, 22, 27]. This might be due to the heterogeneity of biological activity within the tumour tissue. Proliferating cells in all histological grades were found to be distributed heterogeneously throughout the tumour, especially in recurrences [38]. It is debatable that the focal accumulation of proliferation may affect tumour recurrence for the ‘highest-area’ counting method. The ‘highest-area’ counting method is preferred to minimize missing of focal accumulation of biological activity within the meningioma tissue, as it is recommended by Nakasu et al. [36]. This is an important issue when considering modern neurosurgical techniques, where only small parts of tumour with unknown precise location of the tissue reach the pathologist’s hands. Indeed, it is debatable whether recognized areas of high mitotic activity in meningiomas determined with either counting method reflect the proliferation status of the whole tumour.
A substantial number of patients inherit mean Ki-67 LI of 1 % with recurrence times ranging from 11 to 148 month. Therefore, a cut-off value over which a tumour becomes suspicious cannot be given. Precise values from different laboratories are not applicable to other institutions because of differences in methodology, counting procedures and interpretation of the results as reflected by the relatively wide range of initial and recurrent Ki-67 LI determined by several investigators.
The role of steroid hormones in the progression of meningiomas is still a matter of controversy. Several studies, which included meningiomas of all grades, suggested a more favourable prognosis for PR-positive meningiomas [15, 16] with high progesterone receptor status being associated with lower recurrence rates and vice versa [9, 46]. However, these studies frequently included meningiomas with different resection grades and histological subtypes. Hsu and colleagues suggested that only a combination of three proposed prognostic factors for survival, that is, WHO grade, proliferative index and PR status, should be used to predict meningioma recurrence [16]. However, their model was tested containing atypical and malignant meningiomas and therefore did not demonstrate the true influence of PR status on survival. The focus of interest should be benign borderline cases where additional information is needed for prognostic considerations. Maiuri et al. compared two groups of completely resected WHO I meningiomas, with and without recurrence [31]. Patient age, tumour location, consistency, vascularity, histological subtype, oestrogen receptor, vascular endothelial growth factor (VEGF), and epidermal growth factor receptor (EGFR) were not correlated with tumour recurrence. Higher mitotic index and Ki-67 LI and PR negativity were predictive factors of recurrence of benign completely resected meningiomas. This study also showed a negative association between Bcl-2 and PR.
Data in the literature is pointing to a female preponderance in PR expression; however, these studies included a substantial number of atypical and malignant meningiomas [5, 9, 20]. These meningiomas are mostly devoid of PRs and more often found among male patients. After excluding atypical and malignant cases, no sex-related difference in PR expression could be found. Therefore, the previously reported sex-related difference might be due to particular selection criteria, which produced an inhomogeneous patient population.
Previous studies on the human endometrium have shown that progesterone plays a role in neovasculogenesis. High levels of progesterone receptors in meningiomas may indicate a similar situation. However, Fewings and Roser suggested that progesterone may inhibit angiogenesis, by enhancing the production of thrombospondin-1, an angiogenesis inhibitor [9, 46]. It is difficult to draw conclusions from these data, as the PRs in meningiomas are non-functional in the majority of cases [4]. Moreover, our observations come from a clinical and histopathological analysis and may well reflect a multifactorial situation with progesterone being only one variable in the process of tumour vascularization.
However, the PR status alone cannot be used to predict behaviour in benign meningiomas and should not influence the decision about follow-up intervals and therapeutic strategies. Moreover, Matsuda et al. demonstrated that the antitumoral effect of antiprogesterone agents on meningiomas, both in vitro and in vivo, exists regardless of the tumour’s PR status, suggesting that the antitumoral effect is mediated by other pathways [32]. This was supported by Verheijen and co-workers, who suggested that PR-like proteins do not have a biological function and may lead to the overestimation of the PR status for clinical purposes [54].
Analysing Ki-67 LI and PR status in spinal versus intracranial meningiomas, the former was found to be higher in spinal disease (the latter being almost identical) [45]. These findings were compared with recurrence-free survival at follow-up to determine if a relationship between these two biological indicators and clinical behaviour of the tumours could be seen. However, recurrence-free survival after total tumour resection was found to be very similar in both patient groups. The data suggest that spinal meningiomas differ from their intracranial counterpart in terms of proliferation as measured by the Ki-67 LI; however, they display similar clinical behaviour and PR status. The discrepancy between the Ki-67 LI and recurrence rates cannot be fully explained on the basis of the present data.
Meningiomas are highly vascularized tumours. Several studies have demonstrated that VEGF has a significant influence in the proliferation and migration in meningiomas [26, 43]. Whereas some groups observed a correlation between the degree of VEGF expression and meningioma histological grade [26, 50], Barresi and Pfister showed that VEGF expression and WHO grade did not correlate in meningiomas [3, 40]. VEGFR2 is the predominant mediator of VEGF-stimulated endothelial cell migration, proliferation, survival and enhanced vascular permeability [13]. The presence of an autocrine loop for VEGF and VEGFR2 has been demonstrated in several tumour cell lines, which resulted in increased proliferation [11, 53]. Pfister et al. showed that KDR expression is mostly low or absent in meningiomas, which suggests that mechanisms besides VEGFA signalling through KDR influence angiogenesis in meningiomas [40]. In addition, this study demonstrated that meningiomas display a high PDGFRβ expression. The combination of high PDGFRβ levels and low KDR and PDGFB expression in meningiomas indicates that PDGFRβ has a significant function in tumorigenesis in meningiomas. When meningiomas were stimulated with exogenous VEGFA in vitro, they displayed a significant higher proliferation rate. This proliferative stimulus was abolished once PDGFRβ was inhibited before administration of exogenous VEGFA.
The variety and distribution of benign meningioma subtypes are age independent with the exception of a higher percentage of psammomatous meningiomas among older patients [47]. Philippon et al. have suggested the higher percentage of calcified psammomatous meningiomas as a reason for lower recurrence rates in meningiomas [41]. Indeed, we found a significant higher percentage of psammomatous meningiomas in the elderly, but a relationship between psammomatous bodies and intratumoral calcification could not be established. Moreover, psammomatous meningiomas did not display lower proliferation rates than other benign subtypes. Proliferation rates and PR status, useful biological indicators of tumour activity, are age independent [47]. Survival measurements showed comparable outcome in both age groups within benign meningiomas. Different growth rates in different age groups cannot be explained by means of these two parameters alone.
Ongoing tissue research studies should focus on the growth behaviour of benign meningiomas to characterize specific alterations that could provide us with new diagnostic and prognostic criteria as a rational basis for treatment. The unsolved situation of clinical aggressive benign meningiomas (despite radiotherapy) should lead us to new concepts like chemotherapeutic agents which might play a role as radiosensitizers [37].
In histopathological borderline cases, with some but not convincing aspects of atypia, the Ki-67 LI, combined with the routine histopathological workup, can provide more insight in the behaviour of a meningioma, particularly in the presence of high vascularity, low PR status, subtotal resection and recurrence. PR status in combination with the proliferative index can be a useful prognostic tool for benign meningiomas. High scores of Ki-67 are worrisome and should lead to a closer follow-up for evidence of recurrent tumour, but the confidence in high LI should not interfere with the decisions for treatment plans as some authors recommend.
References
Abramovich CM, Prayson RA (1999) Histopathologic features and MIB-1 labeling indices in recurrent and nonrecurrent meningiomas. Arch Pathol Lab Med 123(9):793–800
Barresi V (2011) Angiogenesis in meningiomas. Brain Tumor Pathol 28(2):99–106
Barresi V, Tuccari G (2010) Increased ratio of vascular endothelial growth factor to semaphorin3A is a negative prognostic factor in human meningiomas. Neuropathology 30(5):537–546
Blankenstein MA, Verheijen FM, Jacobs JM, Donker TH, van Duijnhoven MW, Thijssen JH (2000) Occurrence, regulation, and significance of progesterone receptors in human meningioma. Steroids 65(10–11):795–800
Carroll RS, Glowacka D, Dashner K, Black PM (1993) Progesterone receptor expression in meningiomas. Cancer Res 53(6):1312–1316
Crompton MR, Gautier-Smith PC (1970) The prediction of recurrence in meningiomas. J Neurol Neurosurg Psychiatry 33(1):80–87
Ding S, Li C, Lin S, Yang Y, Liu D, Han Y et al (2006) Comparative evaluation of microvessel density determined by CD34 or CD105 in benign and malignant gastric lesions. Hum Pathol 37(7):861–866
Falchetti ML, Pallini R, Larocca LM, Verna R, D’Ambrosio E (1999) Telomerase expression in intracranial tumours: prognostic potential for malignant gliomas and meningiomas. J Clin Pathol 52(3):234–236
Fewings PE, Battersby RD, Timperley WR (2000) Long-term follow up of progesterone receptor status in benign meningioma: a prognostic indicator of recurrence? J Neurosurg 92(3):401–405
Folkman J (1995) Clinical applications of research on angiogenesis. N Engl J Med 333(26):1757–1763
Gee MFW, Tsuchida R, Eichler-Jonsson C, Das B, Baruchel S, Malkin D (2005) Vascular endothelial growth factor acts in an autocrine manner in rhabdomyosarcoma cell lines and can be inhibited with all-trans-retinoic acid. Oncogene 24(54):8025–8037
Gerdes J, Becker MH, Key G, Cattoretti G (1992) Immunohistological detection of tumour growth fraction (Ki-67 antigen) in formalin-fixed and routinely processed tissues. J Pathol 168(1):85–86
Gille H, Kowalski J, Li B, LeCouter J, Moffat B, Zioncheck TF et al (2001) Analysis of biological effects and signaling properties of Flt-1 (VEGFR-1) and KDR (VEGFR-2). J Biol Chem 276(5):3222–3230
Gudjonssona O, Bergström M, Kristjansson S, Wu F, Nyberg G, Fasth K-J et al (2001) Analysis of 76Br-BrdU in DNA of brain tumors after a PET study does not support its use as a proliferation marker. Nucl Med Biol 28(1):59–65
Gursan N, Gundogdu C, Albayrak A, Kabalar ME (2002) Immunohistochemical detection of progesterone receptors and the correlation with Ki-67 labeling indices in paraffin-embedded sections of meningiomas. Int J Neurosci 112(4):463–470
Hsu DW, Efird JT, Hedley-Whyte ET (1997) Progesterone and estrogen receptors in meningiomas: prognostic considerations. J Neurosurg 86(1):113–120
Jellinger K, Denk H (1974) Blood group isoantigens in angioblastic meningiomas and hemangioblastomas of the central nervous system. Virchows Arch A Pathol Anat Histol 364(2):137–144
Kalala JP, Maes L, Vandenbroecke C, de Ridder L (2005) The hTERT protein as a marker for malignancy in meningiomas. Oncol Rep 13(2):273–277
Karamitopoulou E, Perentes E, Diamantis I, Maraziotis T (1994) Ki-67 immunoreactivity in human central nervous system tumors: a study with MIB 1 monoclonal antibody on archival material. Acta Neuropathol (Berl) 87(1):47–54
Khalid H (1994) Immunohistochemical study of estrogen receptor-related antigen, progesterone and estrogen receptors in human intracranial meningiomas. Cancer 74(2):679–685
Kleihues P, Burger PC, Scheithauer B (1993) The new WHO classification of brain tumors. Brain Pathol 3:255–268
Kolles H, Niedermayer I, Schmitt C, Henn W, Feld R, Steudel WI et al (1995) Triple approach for diagnosis and grading of meningiomas: histology, morphometry of Ki-67/Feulgen stainings, and cytogenetics. Acta Neurochir (Wien) 137(3–4):174–181
Konstantinidou AE, Patsouris E, Korkolopoulou P, Kavantzas N, Mahera H, Davaris P (2001) DNA topoisomerase IIα expression correlates with cell proliferation but not with recurrence in intracranial meningiomas. Histopathology 39(4):402–408
Korshunov A, Shishkina L, Golanov A (2002) DNA topoisomerase II-α and cyclin A immunoexpression in meningiomas and its prognostic significance. Arch Pathol Lab Med 126(9):1079–1086
Lamberts SW, Tanghe HL, Avezaat CJ, Braakman R, Wijngaarde R, Koper JW et al (1992) Mifepristone (RU 486) treatment of meningiomas. J Neurol Neurosurg Psychiatry 55(6):486–490
Lamszus K, Lengler U, Schmidt NO, Stavrou D, Ergun S, Westphal M (2000) Vascular endothelial growth factor, hepatocyte growth factor/scatter factor, basic fibroblast growth factor, and placenta growth factor in human meningiomas and their relation to angiogenesis and malignancy. Neurosurgery 46(4):938–947
Langford LA, Cooksley CS, DeMonte F (1996) Comparison of MIB-1 (Ki-67) antigen and bromodeoxyuridine proliferation indices in meningiomas. Hum Pathol 27(4):350–354
Lieu AS, Hwang SL, Howng SL (2003) Intracranial meningioma and breast cancer. J Clin Neurosci 10(5):553–556
Madsen C, Schroder HD (1997) Ki-67 immunoreactivity in meningiomas–determination of the proliferative potential of meningiomas using the monoclonal antibody Ki- 67. Clin Neuropathol 16(3):137–142
Maes L, Lippens E, Kalala JPO, De Ridder L (2005) The hTERT-protein and Ki-67 labelling index in recurrent and non-recurrent meningiomas. Cell Prolif 38(1):3–12
Maiuri F, Caro MDB, Esposito F, Cappabianca P, Strazzullo V, Pettinato G et al (2007) Recurrences of meningiomas: predictive value of pathological features and hormonal and growth factors. J Neurooncol 82(1):63–68
Matsuda Y, Kawamoto K, Kiya K, Kurisu K, Sugiyama K, Uozumi T (1994) Antitumor effects of antiprogesterones on human meningioma cells in vitro and in vivo. J Neurosurg 80(3):527–534
Matsuno A, Nagashima T, Matsuura R, Tanaka H, Hirakawa M, Murakami M et al (1996) Correlation between MIB-1 staining index and the immunoreactivity of p53 protein in recurrent and non-recurrent meningiomas. Am J Clin Pathol 106(6):776–781
Michelsen JJ, New PF (1969) Brain tumour and pregnancy. J Neurol Neurosurg Psychiatry 32:305–307
Moller ML, Braendstrup O (1997) No prediction of recurrence of meningiomas by PCNA and Ki-67 immunohistochemistry. J Neurooncol 34(3):241–246
Nakasu S, Li DH, Okabe H, Nakajima M, Matsuda M (2001) Significance of MIB-1 staining indices in meningiomas: comparison of two counting methods. Am J Surg Pathol 25(4):472–478
Nathoo N, Barnett GH, Golubic M (2004) The eicosanoid cascade: possible role in gliomas and meningiomas. J Clin Pathol 57(1):6–13
Ohta M, Iwaki T, Kitamoto T, Takeshita I, Tateishi J, Fukui M (1994) MIB1 staining index and scoring of histologic features in meningioma. Indicators for the prediction of biologic potential and postoperative management. Cancer 74(12):3176–3189
Perry A, Stafford SL, Scheithauer BW, Suman VJ, Lohse CM (1998) The prognostic significance of MIB-1, p53, and DNA flow cytometry in completely resected primary meningiomas. Cancer 82(11):2262–2269
Pfister C, Pfrommer H, Tatagiba MS, Roser F (2012) Vascular endothelial growth factor signals through platelet-derived growth factor receptor [beta] in meningiomas in vitro. Br J Cancer 107(10):1702–1713
Philippon J, Cornu P, Grob R, Rivierez M (1986) Les meningiomes recidivantes. Neurochirurgie 32(Suppl 1):54–62
Preusser M, Hassler M, Birner P, Rudas M, Acker T, Plate KH et al (2012) Microvascularization and expression of VEGF and its receptors in recurring meningiomas: pathobiological data in favor of anti-angiogenic therapy approaches. Clin Neuropathol 31(5):352–360
Provias J, Claffey K, delAguila L, Lau N, Feldkamp M, Guha A (1997) Meningiomas: role of vascular endothelial growth factor/vascular permeability factor in angiogenesis and peritumoral edema. Neurosurgery 40:1016–1026
Remmele W, Stegner HE (1987) Recommendation for uniform definition of an immunoreactive score (IRS) for immunohistochemical estrogen receptor detection (ER-ICA) in breast cancer tissue. Pathologie 8(3):138–140
Roser F, Nakamura M, Bellinzona M, Ritz R, Ostertag H, Tatagiba MS (2006) Proliferation potential of spinal meningiomas. Eur Spine J 15(2):211–215
Roser F, Nakamura M, Bellinzona M, Rosahl SK, Ostertag H, Samii M (2004) The prognostic value of progesterone receptor status in meningiomas. J Clin Pathol 57:1033–1037
Roser F, Nakamura M, Ritz R, Bellinzona M, Dietz K, Samii M et al (2005) Proliferation and progesterone receptor status in benign meningiomas are not age dependent. Cancer 104(3):598–601
Roser F, Samii M, Ostertag H, Bellinzona M (2004) The Ki-67 proliferation antigen in meningiomas. Experience in 600 cases. Acta Neurochir (Wien) 146(1):37–44
Saad RS, El-Gohary Y, Memari E, Liu YL, Silverman JF (2005) Endoglin (CD105) and vascular endothelial growth factor as prognostic markers in esophageal adenocarcinoma. Hum Pathol 36(9):955–961
Sakuma T, Nakagawa T, Ido K, Takeuchi H, Sato K, Kubota T (2008) Expression of vascular endothelial growth factor-A and mRNA stability factor HuR in human meningiomas. J Neurooncol 88(2):143–155
Shibuya M, Hoshino T, Ito S, Wacker MR, Prados MD, Davis RL et al (1992) Meningiomas: clinical implications of a high proliferative potential determined by bromodeoxyuridine labeling. Neurosurgery 30(4):494–497
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20:22–39
Steiner H, Berger AP, Godoy-Tundidor S, Bjartell A, Lilja H, Bartsch G et al (2004) An autocrine loop for vascular endothelial growth factor is established in prostate cancer cells generated after prolonged treatment with interleukin 6. Eur J Cancer 40(7):1066–1072
Verheijen FM, Donker GH, Viera CS, Sprong M, Jacobs HM, Blaauw G et al (2002) Progesterone receptor, bc1-2 and bax expression in meningiomas. J Neurooncol 56(1):35–41
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Roser, F., Pfister, C. (2014). Proliferation Behaviour of Meningiomas. In: Ramina, R., de Aguiar, P., Tatagiba, M. (eds) Samii's Essentials in Neurosurgery. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-54115-5_3
Download citation
DOI: https://doi.org/10.1007/978-3-642-54115-5_3
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-54114-8
Online ISBN: 978-3-642-54115-5
eBook Packages: MedicineMedicine (R0)