Abstract
Disorders related to stress or trauma are common among patients with substance use disorders (SUD). In clinical samples of patients with SUD, the prevalence of lifetime Posttraumatic Stress Disorder (PTSD) ranges from 26 % to 52 %, and from 15 % to 41 % for current PTSD. A substantial number of these patients suffer from the consequences of severe and prolonged interpersonal trauma usually referred to as “Complex PTSD”. Another common consequence of repeated interpersonal trauma in childhood are dissociative symptoms that may or may not co-occur with PTSD in SUD patients. While several hypotheses can explain the relationships between SUD and PTSD, the self-medication hypothesis has the strongest empirical support. Patients with both disorders have a more severe clinical profile than SUD patients without PTSD, poorer adherence to treatment, a shorter duration of abstinence, and worse outcomes across a variety of measures. Their clinical needs often make a treatment approach necessary that integrates SUD specific and trauma specific interventions. Several trauma treatments focusing on the present (i.e. providing skills training and psycho-education) and, more recently, also past-focused (i.e. exposure-based) treatments have been evaluated in SUD patients with co-occurring PTSD. Some of them outperformed SUD treatment-as-usual on PTSD and/or substance use outcomes. Findings on the effects of medication in patients with SUD and co-occurring PTSD are scarce and remain inconclusive.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Trauma or stress-related disorders, especially Posttraumatic Stress Disorder (PTSD), have become one of the best-researched comorbidities in the field of substance abuse. What these disorders have in common is a history of trauma exposure. Patients with substance use disorders (SUD) report extensively high numbers of traumatic experiences. The majority of these patients was not traumatised by one discreet incident, such as a car accident, a rape, or a criminal assault, but was repeatedly exposed to traumatic stressors and many are still exposed to ongoing victimisation. Most patients report traumatic events in childhood, such as sexual and physical abuse, which can be followed by further experiences of interpersonal violence over the lifespan, often perpetuated by their ongoing substance abuse.
Traumatic exposure may be followed by a variety of clinical presentations grouped as posttraumatic stress disorders that are seen as a spectrum of disorders. The mental health consequences of traumatic experiences are of importance for both the development of SUD and for their course and outcome. In this chapter we will briefly outline the diagnostic criteria for trauma spectrum disorders. We will give an overview of findings related to their prevalence among patients with SUD, potential relationships between both groups of disorders, and clinical aspects, including evidence-based treatments for patients with this comorbidity. Given the large volume of literature on trauma and posttraumatic stress disorders, we restrict the term trauma to events that satisfy PTSD Criterion A according to DSM-5. Moreover, we focus on relationships between SUD and posttraumatic stress disorders rather than on trauma per se.
2 Posttraumatic Stress Disorder and Other Trauma-Related Disorders
Fortunately, many individuals show resilient responses to severe stress and potentially traumatic events. In a substantial number of people, however, these experiences lead to the development of posttraumatic stress disorders. The spectrum or continuum of trauma-related disorders includes Acute Stress Disorder (ASD), Posttraumatic Stress Disorder (PTSD), and reactions that typically arise from severe and prolonged experiences of interpersonal trauma that often begin already early in life, usually referred to as “Complex PTSD”. There is some overlap between this construct and the “dissociative subtype of PTSD” that has recently been included in DSM-5. Finally, high levels of dissociative symptoms, also in the absence of PTSD, and Dissociative Disorders are in most cases a consequence of early and complex trauma. In this short overview we will focus on the more severe clinical conditions (complex) PTSD and Dissociative Disorders.
2.1 Posttraumatic Stress Disorder
The most common diagnosis in the field of trauma-related disorders is Posttraumatic Stress Disorder (PTSD). A diagnosis of PTSD requires exposure to a traumatic event in which a person experiences or witnesses (an) event(s) that involves real or threatened bodily harm (DSM-5 American Psychiatric Association 2013). In DSM-IV, PTSD was defined by three trauma symptom clusters: intrusions (recurrent and intrusive distressing trauma memories including images, perceptions, thoughts, flashbacks and distressing dreams of the event, and a numbing of general responsiveness), avoidance (avoiding reminders of past trauma, an inability to recall an important aspect of the trauma, a diminished interest in significant activities, detachment from others, a restricted sense of affect, and a sense of foreshortened future), and hyperarousal and hypervigilance (sleeping difficulties, irritability, inability to concentrate, and exaggerated startle responses). To meet full criteria for a diagnosis of PTSD, the individual must experience symptoms for at least 1 month (after 3 months “chronic PTSD”) and the symptoms must cause clinically significant distress or impairment in social, occupational, or other areas of functioning. In DSM-5, the 3 clusters of DSM-IV symptoms are divided into 4 clusters: intrusions, avoidance, negative alterations in cognitions and mood (persistent and distorted blame of self or others, persistent negative emotional state) and alterations in arousal and reactivity (also including reckless or destructive behaviour). All of these symptoms may aggravate the clinical picture of traumatised SUD patients and interfere with treatment for substance abuse.
Research has clearly shown that the diagnosis of PTSD does not encompass the entirety of mental health consequences of trauma exposure, especially after repeated traumatisation and early adverse experiences prior to the onset of PTSD. As a consequence a “dissociative subtype of PTSD” has been included in DSM-5. Compared to individuals with PTSD alone (simple PTSD), patients with a diagnosis of the dissociative subtype of PTSD have higher levels of psychiatric comorbidity, especially comorbid personality disorders, increased functional impairment and increased suicidality. There is some overlap between this new subtype of PTSD in DSM-5 and the concept of “Complex PTSD” that has been proposed for ICD-11.
2.2 Complex PTSD
After repeated interpersonal traumatic experiences in childhood, PTSD symptoms may be complicated by sustained and pervasive disturbances in emotion regulation, in the experience of a diminished and defeated sense of self, altered systems of meaning, and in difficulties maintaining relationships. This syndrome has been labelled “PTSD with associated features” in DSM-IV-TR and “PTSD with personality change” in ICD-10 and is known by clinicians as “complex PTSD” or “Disorders of Extreme Stress Not Otherwise Specified (DESNOS)”. It has now been proposed to officially include this diagnosis into the section on disorders specifically related to trauma and stress in ICD-11 (Maercker et al. 2013). In addition to the three core elements of PTSD, the proposed diagnosis includes enduring disturbances in the domains of affect, self, and interpersonal relationships. It is assumed that Complex PTSD is distinguishable from personality disorders by its restricted symptom profile and its responsiveness to specific treatments that differ from those for personality disorders and from those for PTSD.
The recognition of the range of interrelated problems associated with a history of early severe interpersonal trauma is an important development with much relevance for the field of substance abuse. Complex PTSD may interfere with engagement in treatment, participation in and learning from structured treatment activities, and with the ability to inhibit substance cravings and impulsive substance-seeking behaviours while sustaining substance-free relationships, and relapse prevention behaviours.
2.3 Dissociative Disorders
Another common consequence of repeated interpersonal trauma in childhood are high levels of dissociative symptoms and, at the more extreme end of this symptom spectrum, dissociative disorders. According to the DSM-IV (APA 1994), the essential feature of dissociation is a disruption of the normal integrative functions of consciousness, memory, identity, and perception of the environment. DSM-IV recognises five distinct dissociative disorders, i.e. dissociative amnesia, dissociative fugue, dissociative identity disorder (DID), and depersonalization disorder as well as atypical dissociative disorders (i.e. dissociative disorder not otherwise specified; DDNOS). The DSM-5 classification reduces the number of these disorders by including dissociative fugue as specifier of dissociative amnesia rather than a separate diagnosis. Derealisation is included in the name and symptom structure of what was previously called depersonalisation disorder and is now called depersonalisation/derealisation disorder. Moreover, several changes to the criteria for dissociative identity disorder have been made: Certain possession-form phenomena and functional neurological symptoms to account for more diverse presentations of the disorder have been included; symptoms of disruption of identity may now be reported as well as observed; and gaps in the recall of events may occur for everyday events, not just for traumatic events.
Dissociative symptoms or disorders can, in the same way as simple and complex PTSD, aggravate the clinical picture of traumatised SUD patients and interfere with treatment for substance abuse. Dissociative symptoms or disorders can aggravate the clinical picture of traumatised SUD patients and interfere with treatment for substance abuse in the same way as simple and complex PTSD can.
3 Prevalence of the Dual Disorder of SUD and Posttraumatic Stress Disorders
3.1 SUD in Individuals with Posttraumatic Stress Disorders
Among people with lifetime PTSD, lifetime SUD is estimated at 21–43 %, compared to 8–25 % in those without PTSD (Jacobsen et al. 2001). According to US population data, among women who experience PTSD in their lifetime, 28 % develop an alcohol use disorder and 27 % develop a drug use disorder. Among men, 52 % and 35 % respectively, develop an alcohol or drug use disorder (Kessler et al. 1995). In a population-based study from Australia (Mills et al. 2006), 34 % of those with PTSD also had a substance use disorder, most commonly an alcohol use disorder (24 %). Even higher rates are found in clinical populations. For example, up to 75 % of combat veterans with lifetime PTSD also meet criteria for lifetime alcohol abuse or dependence (Jacobsen et al. 2001). In a study among women presenting for treatment with Complex PTSD and other severe consequences of childhood sexual abuse, one-third of the participants (33 %) had a lifetime history of substance abuse (Levitt and Cloitre 2005). And up to 59 % of patients with dissociative disorders also meet criteria for alcohol dependence (Langeland et al. 2005).
3.2 Posttraumatic Stress Disorders in Individuals with SUD
Conversely, the prevalence of PTSD is markedly elevated among individuals with SUD. In clinical SUD samples, the prevalence of lifetime PTSD ranges from 26 % to 52 % and from 15 % to 41 % for current PTSD (Schäfer and Najavits 2007). These rates are considerably higher than those observed in general population surveys where rates of current PTSD usually do not exceed 9 %. The prevalence of PTSD varies per sample. For example, current PTSD is more prevalent in females than in males—typically about twice the rate (e.g. Dom et al. 2007; Driessen et al. 2008). Moreover, some substances of abuse show a higher association with PTSD than others (e.g. “harder drugs” and polydrug use compared to alcohol or cannabis). In European samples, the prevalence of current PTSD among treatment seeking alcohol dependent patients was 15–25 % (e.g. Driessen et al. 2008; Schäfer et al. 2007), while the prevalence among patients with (additional) drug dependence was 29–36 % (Driessen et al. 2008).
As the diagnosis of complex PTSD (ICD-11) or a dissociative subtype (DSM-5) is just about to be included in the diagnostic systems, no studies using these categories in SUD patients exist so far. A wealth of studies, however, indicates that SUD patients reporting early and complex trauma (i.e. chronic exposure or exposure to different forms of childhood interpersonal trauma) suffer from characteristics of these diagnoses including disturbances in emotion regulation, interpersonal problems, altered sense of self, and chronic suicidality (Hien et al. 2005).
The few studies on the prevalence of dissociative disorders in patients with SUD need to be interpreted with care. A study from Turkey using the Structured Clinical Interview for DSM-IV dissociative disorders reported a current prevalence rate of 17 % (Karadag et al. 2005), others reported even higher rates. It has been proposed that lower levels of dissociative symptoms (and probably also dissociative disorders) are found in alcohol-dependent patients as compared to patients with drug use disorders (for overviews see Langeland et al. 2005; Schäfer et al. 2007). This was confirmed in a study among a larger sample of patients with different SUD where higher levels of dissociation were observed in patients with (additional) drug dependence as compared to patients with mere alcohol dependence (Schäfer et al. 2010). However, when severity of traumatic events in childhood, PTSD, age and gender were included in the analysis, the influence of the type of substance abuse did not prove to be statistically significant. The variable most strongly related to dissociative symptoms was severity of traumatic events in childhood, in particular emotional abuse, even after controlling for PTSD and other potential confounders.
4 Relationships Between Posttraumatic Stress Disorders and SUD
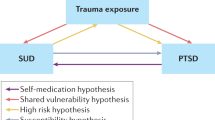
The question of pathways or mechanisms is crucial for understanding the relationship between trauma exposure, posttraumatic stress disorders, and substance use disorders (e.g. Hien et al. 2005). A better understanding of pathways from trauma to addiction and the complex symptom interplay that exists between trauma-related disorders and SUD can inform interventions addressing trauma and substance abuse. Four predominant hypotheses have been proposed to explain the ways in which PTSD or other trauma-related disorders often co-occur with SUD:
-
1.
Self-medication hypothesis: Individuals with trauma-related symptoms use substances to control their emotional pain.
-
2.
High-risk hypothesis: Substance use, drug use in particular, is a high-risk behaviour leading to a lifestyle that increases the risk for trauma exposure.
-
3.
Susceptibility hypothesis: Substance users, drug users in particular, are more susceptible to PTSD or other trauma-related disorders following exposure to traumatic events.
-
4.
Third factor hypothesis: There is no direct relationship, but the association appears because both conditions derive from a third common factor, such as genetics (influence of other variables).
Figure 12.1 depicts a model to explain ways in which posttraumatic stress disorders could lead to addiction problems.
While these models are not mutually exclusive, the self-medication model is the model with the strongest empirical support. Findings supporting the self-medication model come from different types of studies. A frequent approach is to compare the motivation for using substances in SUD patients with and without PTSD. In many studies, greater use of substances in patients with co-occurring PTSD was associated with situations involving unpleasant emotions, physical discomfort and interpersonal conflicts compared to situations involving pleasant or neutral situations. Similar associations were found between PTSD status and reasons for relapse in recently abstinent patients. In a series of laboratory studies, Coffey and colleagues found that clients who were alcohol and cocaine dependent with a comorbid diagnosis of PTSD reported greater drug and alcohol craving following the presentation of trauma-related stimuli as compared to neutral stimuli, and that PTSD severity was predictive of craving elicited by trauma-related stimuli and drug-related stimuli (Coffey et al. 2002). Moreover, alcohol craving and distress in response to trauma images decreased in patients receiving six sessions of trauma-focused imaginal exposure, but did not change in control patients (Coffey et al. 2002).
5 Clinical Aspects and Relationships with Outcome
5.1 Clinical Differences in Patients with PTSD
Patients with both PTSD and SUD have a more severe clinical profile than patients with SUD only, especially when trauma occurred early in their lives (see Schäfer and Najavits 2007). They have earlier onset of substance abuse and more years of problematic use, they report more polydrug use, and they have greater severity of current substance use. Patients with SUD and co-occurring PTSD also report worse physical health, lower well-being, and more interpersonal problems. Finally, patients with both disorders are more likely to meet criteria for additional psychiatric disorders, especially major depression and anxiety disorders (Langeland et al. 2004). Large epidemiological surveys also find high rates of other co-occurring disorders among those with PTSD and SUD. In one such study (Mills et al. 2006), almost two-thirds of those with PTSD and SUD had an additional affective disorder, and about half had a comorbid anxiety disorder. Personality disorders were also highly prevalent (62 %). All of these disorders were significantly more frequent in individuals with PTSD and SUD as compared to those with SUD alone or neither disorder. Also, consistent with findings from clinical studies, individuals with PTSD and SUD experienced poorer physical health and greater disability than those with SUD alone.
In addition to worse physical health and more psychiatric comorbidity, patients with complex PTSD present the typical manifestations of this disorder. They suffer from impulsivity and suicidal ideation, self-destructive behaviour, and vulnerability to revictimisation (Hien et al. 2005).
5.2 Treatment Utilisation and Outcome
Studies on the relationship between a history of trauma and treatment utilisation in patients with SUD are inconclusive. In a large sample of German outpatients with alcohol dependence, a history of sexual violence was related to higher use of SUD services in female but not in male victims (Schäfer et al. 2009). Victims of both genders were significantly younger at first contact with addiction treatment. Other authors reported that patients with a history of childhood sexual abuse seek less treatment for SUD, at least in institutional contexts (e.g. Peltan and Cellucci 2011). Simpson (2002) reported that with greater severity of childhood sexual abuse, the number of treatments for mental health problems increased, yet the number of substance abuse treatment episodes decreased. She suggested that there may not be a consistent relationship between childhood trauma and SUD treatment utilisation because of the relationship between traumatic experiences and utilisation of other services. While several studies reported a poorer outcome of treatment in patients with a history of childhood trauma (see Schäfer et al. 2009) others could not confirm this relationship. Recently contingency management (Petry et al. 2011) and self-help approaches (Makin-Byrd et al. 2011) have even been reported to have a higher efficacy in SUD patients with abuse histories. With regard to contingency management, one potential mechanism could be that this approach is especially effective in patients with more severe psychopathology, which is often the case in victims of sexual abuse (Petry et al. 2011).
In accordance with the findings among patients with other co-occurring disorders, there seems to be a relatively high lifetime utilisation rate of SUD services in substance abuse patients with PTSD (e.g. Najavits et al. 2004). When they engage in SUD treatment, patients with co-occurring PTSD have a poorer adherence to treatment than patients without the disorder, a shorter duration of abstinence, and worse outcomes across a variety of measures (Schäfer and Najavits 2007). Ouimette et al. (2003) conducted a 5-year follow-up study on one hundred male patients with co-occurring PTSD who attended SUD treatment. Patients who received PTSD treatment in the first 3 months following discharge and those who received treatment for a longer duration in the first year were more likely to be remitted 5 years later. The importance of treating symptoms of PTSD in SUD patients is further supported by studies showing that reductions of PTSD severity during treatment were likely to be associated with substance use improvement whereas substance use symptom reduction had little impact on symptoms of PTSD (e.g. Hien et al. 2010a, b). While the negative influence of comorbid PTSD on treatment outcome is clear, more research is needed on other potential factors. For instance, SUD patients with and without comorbid PTSD are also known to differ on other proximal determinants of treatment response, such as social support and coping strategies.
6 Assessment
The substantial prevalence rates of traumatic events among individuals with SUD point to the need to assess those entering substance abuse treatment programmes for traumatic experiences and trauma-related disorders. Asking if trauma has occurred can give clients a meaningful context to understand their behaviours and can empower them to search for and find the kind of help that best suits them. Many professionals, however, hesitate to assess for traumatic experiences and identify trauma-related disorders in their clients. The reasons include insufficient training, discomfort to ask about traumatic events, a high caseload, and fears that inquiring about trauma could cause harm to patients. With regard to the latter point, it is important to note that asking if a traumatic event has occurred and assessing its impact is not the same as opening up and exploring the trauma in detail, which should only be done by clinicians with more advanced training. If the difference between asking about trauma for screening and going into detail and “unpack” the trauma is clearly explained to the client, screening for trauma can be performed safely. When asking about trauma, especially about childhood abuse, it is essential to ask specific questions with clear examples, for instance “When you were a child, did an adult ever hurt or punish you in a way that left bruises, cuts or scratches?” or “When you were a child, did anyone ever do something sexual that made you feel uncomfortable?” (Read et al. 2007). Other principles of asking for trauma and responding to disclosures of trauma can be found in Box 12.1.
Box 12.1. Principles of asking and responding (mod. from Read et al. 2007)
Principles of Asking for Trauma
-
Ask all clients/patients
-
At initial assessment (or if in crisis, as soon as person is settled)
-
In context of a general psychosocial history
-
Preface with brief normalising statement
-
Use specific questions with clear examples of what you are asking about
-
Do not gather all the details, stop client empathetically if necessary
Principles of Responding to Disclosures of Trauma
-
Affirm that it was a good thing to tell
-
Offer support (make sure you know what is available)
-
Ask whether the client relates the abuse to their current difficulties
-
Check current safety—from on-going abuse
-
Check emotional state at end of session
-
Offer follow-up/“check-in”
With regard to the consequences of trauma, clinicians should consider the full context of a patient’s presentation when formulating their diagnosis. The diagnosis of PTSD may be appropriate in some cases, but not all, especially not in the aftermath of early traumatisation. Despite the evidence that a majority of women and many men who are seeking treatment for addictions have been exposed to early and multiple traumatic experiences, standard treatment programmes do not typically assess or target the associated impairments of PTSD, which greatly complicates the prognosis. In practice, integrating interventions that specifically target the associated features are often recommended for these patients.
For most types of assessments (screening tools, questionnaires, and interviews) there is good evidence that they are also valid and reliable in individuals with SUD (for overview see Winters et al. 2014). However, if patients are assessed when actively using substances or during the period of detoxification, the cut-scores of some measures, especially self-rating measures of PTSD and dissociation, need to be adapted. While PTSD symptoms and dissociative symptoms can decrease or increase during detoxification, it has been suggested that major changes in symptoms should be completed within two weeks after termination of active use. Nevertheless, it remains difficult to determine the exact effects of withdrawal or comorbid psychopathology on self-rating instruments. Symptoms of PTSD and dissociation should therefore be assessed repeatedly in the course of treatment to enhance the diagnostic validity. Moreover, it is recommended to give preference to diagnostic interviews over self-ratings. The gold standard for PTSD assessment is the Clinician-Administered PTSD Scale (CAPS) which is currently updated to match the DSM-5 criteria for PTSD. Further gold standard measures are the Structured Clinical Interview for Dissociative Disorders-Revised (SCID-D-R) for Dissociative Disorders, and the Structured Interview for Disorders of Extreme Stress (SIDES) for complex PTSD. Future clinical practice and research should include thorough assessment of trauma and neglect history and all DSM-5 trauma-related disorders as well as ICD-11 Complex PTSD, using validated instruments recommended in international guidelines (Cloitre et al. 2012; ISSTD 2011). The following website provides an overview of existing measures, many of which have been translated into different European languages: http://www.ptsd.va.gov/professional/pages/assessments/assessment.asp.
7 Psychotherapy for Posttraumatic Stress Disorders and SUD
7.1 General Principles of Treatment
Although effective treatments for both posttraumatic stress disorders (e.g. prolonged exposure, eye movement desensitisation, and reprocessing) and SUD (e.g. cognitive behavioural therapy, motivational enhancement techniques) are available, the literature for co-occurring posttraumatic stress disorders and SUD is still limited. The initial debate focused on the sequence of treatments. Early authors suggested that PTSD treatment should only be initiated after a period of abstinence had been achieved. More recently, preference is given to integrated treatments that conceptualise posttraumatic stress disorders and SUD as one large issue and plan treatment accordingly. While it is unclear if integrated treatments have a superior efficacy in patients with SUD and PTSD as compared to one efficacious treatment alone (Torchalla et al. 2012), the clinical needs of patients with SUD and posttraumatic stress disorders often make an integrated approach necessary. It has become widely accepted that the treatment of posttraumatic stress symptoms is a prerequisite for becoming abstinent in many patients. On the other hand, a certain stability of SUD is needed for some interventions, namely trauma exposure.
While SUD specific interventions are needed all along the way of treatment, a phase-based approach has been proven helpful to organise trauma-specific interventions. This approach follows the three stages of trauma therapy: (1) stabilising and managing responses; (2) grieving and processing traumatic memories; (3) reconnecting with the world. All patients need, and can benefit from, the present-focused interventions of the first phase of treatment. This phase includes getting a “road map” of the healing process, establishing safety, mobilising all available resources for healing, and learning how to regulate one’s emotions and manage symptoms. The second phase (including past-focused interventions, i.e. processing traumatic memories by means of trauma exposure) is essential to resolve symptoms of PTSD, but the moment when patients can enter this phase depends on the severity and complexity of the posttraumatic stress disorder. In more complex patients, a longer period of stabilisation will be necessary and in some patients (e.g. some patients with complex PTSD, DID or DDNOS) treatment is restricted to present-focused approaches. The following paragraphs summarise the available evidence for manualised present-focused and past-focused treatments of posttraumatic stress disorders in patients with SUD.
7.2 Present-Focused Treatments
Different treatment approaches focusing on the present (i.e. providing skills training and psycho-education) can be of help in SUD patients with posttraumatic stress disorders. Some of these programmes, e.g. “Dialectical Behaviour Therapy for patients with SUD” (Dimeff and Linehan 2008) have not yet been evaluated in patients with PTSD. In a recent overview, van Dam et al. (2012) could identify four present-focused treatments for concurrent PTSD and SUD with at least one effectiveness study: CBT for PTSD in SUD treatment, Substance dependency-posttraumatic stress disorder therapy, Transcend, and Seeking Safety. They conclude that the first three programmes showed no effects or that it was not possible to draw firm conclusions because of the design of the respective studies. A relatively good evidence base exists for the manualised group treatment Seeking Safety (Najavits 2002). The programme has been evaluated in a larger number of studies including six randomised controlled trials (RCTs). It offers 25 topics to teach coping skills for PTSD and SUD in four domains (cognitive, behavioural, interpersonal, and case management) and has been translated into several European languages (see www.seekingsafety.org). An important assumption of the programme is that safety has the highest priority when recovering from posttraumatic stress disorders and SUD. Safety is defined as abstinence from substances, reduction in self-destructive behaviour, establishment of a network of supportive people, and self-protection from dangers associated with the disorders (e.g., HIV-risk, and domestic violence). Randomised controlled trials showed that Seeking Safety can lead to significant improvements in SUD and PTSD symptom severity. In the RCTs, the programme was more effective than the usual treatment for substance abuse and of equal effectiveness as other cognitive–behavioural interventions for SUD. In some of the controlled trials, Seeking Safety outperformed the control on PTSD but not SUD, in another on SUD but not PTSD, and in some on both PTSD and SUD (Najavits and Hien 2013). An advantage of the treatment is the possibility to provide clients with trauma-specific stabilisation in an early phase of treatment, when abstinence is difficult to achieve or to maintain. It can be followed, if necessary, by past-focused (i.e. exposure-based) treatments.
7.3 Past-Focused Treatments
In recent years, several past-focused approaches have been evaluated in patients with PTSD and SUD. Most models (e.g. Mills et al. 2012; van Dam et al. 2013; Sannibale et al. 2013) took the approach of combining an existing empirically validated treatment developed for PTSD (such as prolonged exposure) and SUD (such as relapse prevention). More recently, the author of the present-focused model Seeking Safety developed a past-focused model (Creating Change) where exposure is broadened to a gentler version. It also includes extensive preparation and decision-making tools for deciding whether a client is ready for exposure (Najavits and Johnson 2014). It is important to note that all models with past-focused (i.e. exposure-based) components also incorporated present-focused approaches (Najavits and Hien 2013). They were delivered in individual rather than group modality, and most tended to be restricted to a more narrow sample than the studies on present-focused treatment approaches. All studies of past-focused models showed positive results but mainly on symptoms of PTSD. For instance, prolonged exposure combined with relapse prevention (COPE; Mills et al. 2012), outperformed the control SUD treatment-as-usual on PTSD at 9-month follow-up but did not outperform the usual treatment on the SUD variables. One of the most important results of the existing studies is that exposure-based models can be used with many SUD clients without notable negative outcomes when they are adapted to their needs.
To provide better guidance for the clinical management of patients with posttraumatic stress disorders and SUD, future studies need to address how these behavioural treatments can be optimally combined with pharmacological treatments.
8 Pharmacotherapy
So far, only few studies examined the effects of pharmacological treatments in patients with co-occurring PTSD and SUD. In one study, Trafton et al. (2006) assessed the effects of opioid substitution therapy among 255 opioid-dependent veterans. In this prospective observational trial, substitution therapy was as effective at reducing substance use in patients with comorbid PTSD as it was in patients without the disorder. One year after treatment both groups showed similar reductions in substance use, but PTSD patients received higher doses of opiate medication and attended more psychosocial treatment sessions. Another study found no significant benefit of the antidepressant sertraline over placebo in 94 alcohol-dependent patients with PTSD with regard to their alcohol consumption and symptoms of PTSD after 12 weeks of treatment (Brady et al. 2005). In a post-hoc cluster analysis of this study, a significant improvement became apparent in sertraline-treated participants with less severe alcohol dependence and early-onset PTSD.
Petrakis et al. (2006) compared the effects of disulfiram and naltrexone to placebo in male veterans with alcohol dependence and different comorbid psychiatric disorders. Patients received either disulfiram or no disulfiram and were, in addition to that, randomised to naltrexone or placebo, resulting in four different study groups. Of the 93 patients with co-occurring PTSD, individuals receiving naltrexone, disulfiram, or both medications had better outcomes after 12 weeks of treatment than the placebo group in terms of drinking days per week and consecutive days of abstinence. In addition, favourable effects on PTSD symptoms were observed in patients on disulfiram compared to those on naltrexone. However, as the authors point out, several limitations make the interpretation of these results difficult, including the potentially confounding effect of abstinence and the open administration of disulfiram. Nevertheless, the findings of this study suggest that both medications are safe and effective for alcohol-dependent patients with PTSD and should be considered for clinical management. In a more recent study of these authors (Petrakis et al. 2012), 88 patients with alcohol dependence and co-occurring PTSD received either paroxetine or desipramine and were, in addition to that, randomised to naltrexone or placebo. After 12 weeks, no differences were found between both antidepressants with regard to symptoms of PTSD but desipramine outperformed paroxetine on alcohol use outcomes. No additional effects of naltrexone were found.
Other promising pharmacotherapies of comorbid PTSD and SUD include, for instance, quetiapine, an antipsychotic medication (Monnelly et al. 2004) and topiramate, an antiseizure medication (Alderman et al. 2009), but the safety and efficacy of these medications for the treatment of posttraumatic stress disorders and SUD need to be tested in controlled clinical trials.
8 Conclusions
Trauma-related disorders are a common comorbidity among patients with SUD. Patients with both disorders have a more severe clinical profile and a worse overall outcome. Therefore, traumatic experiences and their clinical consequences should be routinely assessed in clinical practice and patients with trauma-related comorbidity should be offered specific treatments. Given that many patients suffer from the consequences of early and complex trauma, the typical features associated with these experiences need to be covered. Often, an integrated approach will be necessary to adequately address both disorders. While treatment approaches focusing on the present (i.e. providing skills training and psycho-education) will be beneficial for most patients, including those with dissociative disorders, past-focused (i.e. exposure-based) treatments should (additionally) be offered to SUD patients with co-occurring PTSD. More research is needed on the potential effects of medication in this group of patients.
References
Alderman CP, McCarthy LC, Condon JT, Marwood AC, Fuller JR (2009) Topiramate in combat-related posttraumatic stress disorder. Ann Pharmacother 43(4):635–641. doi:10.1345/aph.1L578
Brady KT, Sonne S, Anton RF, Randall CL, Back SE et al (2005) Sertraline in the treatment of co-occurring alcohol dependence and posttraumatic stress disorder. Alcohol Clin Exp Res 29(3):395–401
Cloitre M, Courtois CA, Ford JD, Green BL, Alexander P (2012) The ISTSS Expert Consensus Treatment Guidelines for Complex PTSD in Adults. www.istss.org/AM/Template.cf. Accessed: 27 Jan 2014
Coffey SF, Saladin ME, Drobes DJ, Brady KT, Dansky BS, Kilpatrick DG (2002) Trauma and substance cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug Alcohol Depend 65(2):115–127
Dimeff LA, Linehan MM (2008) Dialectical behavior therapy for substance abusers. Addict Sci Clin Pract 4(2):39–47
Dom G, De Wilde B, Hulstijn W, Sabbe B (2007) Traumatic experiences and posttraumatic stress disorders: differences between treatment-seeking early- and late-onset alcoholic patients. Compr Psychiatry 48(2):178–185. doi:10.1016/j.comppsych.2006.08.004
Driessen M, Schulte S, Luedecke C, Schaefer I, Sutmann F et al (2008) Trauma and PTSD in patients with alcohol, drug, or dual dependence: a multi-center study. Alcohol Clin Exp Res 32(3):481–488. doi:10.1111/j.1530-0277.2007.00591.x
Hien D, Cohen L, Campbell A (2005) Is traumatic stress a vulnerability factor for women with substance use disorders? Clin Psychol Rev 25(6):813–823
Hien DA, Campbell AN, Ruglass LM, Hu MC, Killeen T (2010a) The role of alcohol misuse in PTSD outcomes for women in community treatment: a secondary analysis of NIDA’s Women and Trauma Study. Drug Alcohol Depend 111(1–2):114–119. doi:10.1016/j.drugalcdep.2010.04.011
Hien DA, Jiang H, Campbell AN, Hu MC, Miele GM et al (2010b) Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA’s Clinical Trials Network. Am J Psychiatry 167(1):95–101. doi:10.1176/appi.ajp.2009.09091261
International Society for the Study of Trauma and Dissociation (ISSTD) (2011) Guidelines for treating dissociative identity disorder in adults, third revision: summary version. J Trauma Dissociation 12(2):115–187. doi:10.1080/15299732.2011.537247
Jacobsen LK, Southwick SM, Kosten TR (2001) Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. Am J Psychiatry 158(8):1184–1190
Karadag F, Sar V, Tamar-Gurol D, Evren C, Karagoz M et al (2005) Dissociative disorders among inpatients with drug or alcohol dependency. J Clin Psychiatry 66(10):1247–1253
Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB (1995) Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 52(12):1048–1060
Langeland W, Draijer N, van den Brink W (2004) Psychiatric comorbidity in treatment-seeking alcoholics: the role of childhood trauma and perceived parental dysfunction. Alcohol Clin Exp Res 28(3):441–447
Langeland W, van den Brink W, Draijer N (2005) Gender and the relationship between childhood trauma, dissociation and alcohol dependence. Zeitschrift für Psychotraumatologie und Psychologische Medizin 3:29–40
Levitt JT, Cloitre M (2005) A clinician’s guide to STAIR/MPE: treatment for PTSD related to childhood abuse. Cogn Behav Pract 12(1):40–52. doi:10.1016/s1077-7229(05)80038-0
Maercker A, Brewin CR, Bryant RA, Cloitre M, Reed GM et al (2013) Proposals for mental disorders specifically associated with stress in the International Classification of Diseases-11. Lancet 381(9878):1683–1685. doi:10.1016/S0140-6736(12)62191-6
Makin-Byrd K, Cronkite RC, Timko C (2011) The influence of abuse victimization on attendance and involvement in mutual-help groups among dually diagnosed male veterans. J Subst Abuse Treat 41(1):78–87. doi:10.1016/j.jsat.2011.02.001
Mills KL, Teesson M, Back SE, Brady KT, Baker AL et al (2012) Integrated exposure-based therapy for co-occurring posttraumatic stress disorder and substance dependence: a randomized controlled trial. JAMA 308(7):690–699
Mills KL, Teesson M, Ross J, Peters L (2006) Trauma, PTSD, and substance use disorders: findings from the Australian National Survey of Mental Health and Well-Being. Am J Psychiatry 163(4):652–658. doi:10.1176/appi.ajp.163.4.652
Monnelly EP, Ciraulo DA, Knapp C, LoCastro J, Sepulveda I (2004) Quetiapine for treatment of alcohol dependence. J Clin Psychopharmacol 24(5):532–535
Najavits LM (2002) Seeking safety: a treatment manual for PTSD and substance abuse. Guilford, New York
Najavits LM, Hien D (2013) Helping vulnerable populations: a comprehensive review of the treatment outcome literature on substance use disorder and PTSD. J Clin Psychol 69(5):433–479. doi:10.1002/jclp.21980
Najavits LM, Johnson KM (2014) Pilot study of creating change, a new past-focused model for PTSD and substance abuse. Am J Addict 23(5):415–422
Najavits LM, Sonn J, Walsh M, Weiss RD (2004) Domestic violence in women with PTSD and substance abuse. Addict Behav 29(4):707–715. doi:10.1016/j.addbeh.2004.01.003
Ouimette P, Moos RH, Finney JW (2003) PTSD treatment and 5-year remission among patients with substance use and posttraumatic stress disorders. J Consult Clin Psychol 71(2):410–414
Peltan JR, Cellucci T (2011) Childhood sexual abuse and substance abuse treatment utilization among substance-dependent incarcerated women. J Subst Abuse Treat 3:215–224. doi:10.1016/j.jsat.2011.03.004
Petrakis IL, Poling J, Levinson C, Nich C, Carroll K et al (2006) Naltrexone and disulfiram in patients with alcohol dependence and comorbid post-traumatic stress disorder. Biol Psychiatry 60(7):777–783. doi:10.1016/j.biopsych.2006.03.074
Petrakis IL, Ralevski E, Desai N, Trevisan L, Gueorguieva R et al (2012) Noradrenergic versus serotonergic antidepressant with or without naltrexone for veterans with PTSD and comorbid alcohol dependence. Neuropsychopharmacology 37(4):996–1004. doi:10.1038/npp.2011.283
Petry NM, Ford JD, Barry D (2011) Contingency management is especially efficacious in engendering long durations of abstinence in patients with sexual abuse histories. Psychol Addict Behav 25(2):293–300. doi:10.1037/a0022632
Read J, Hammersley P, Rudegeair T (2007) Why, when and how to ask about childhood abuse. Adv Psychiatr Treat 13:101–110
Sannibale C, Teesson M, Creamer M, Sitharthan T, Bryant RA et al (2013) Randomized controlled trial of cognitive behaviour therapy for comorbid post-traumatic stress disorder and alcohol use disorders. Addiction 108(8):1397–1410. doi:10.1111/add.12167
Schäfer I, Langeland W, Hissbach J, Luedecke C, Ohlmeier MD et al (2010) Childhood trauma and dissociation in patients with alcohol dependence, drug dependence, or both-A multi-center study. Drug Alcohol Depend 109(1–3):84–89. doi:10.1016/j.drugalcdep.2009.12.012
Schäfer I, Najavits LM (2007) Clinical challenges in the treatment of patients with posttraumatic stress disorder and substance abuse. Curr Opin Psychiatry 20(6):614–618. doi:10.1097/YCO.0b013e3282f0ffd9
Schäfer I, Reininghaus U, Langeland W, Voss A, Zieger N et al (2007) Dissociative symptoms in alcohol-dependent patients: associations with childhood trauma and substance abuse characteristics. Compr Psychiatry 48(6):539–545. doi:10.1016/j.comppsych.2007.05.013
Schäfer I, Verthein U, Oechsler H, Deneke C, Riedel-Heller S et al (2009) What are the needs of alcohol dependent patients with a history of sexual violence? A case-register study in a metropolitan region. Drug Alcohol Depend 105(1–2):118–125. doi:10.1016/j.drugalcdep.2009.06.020
Simpson TL (2002) Women’s treatment utilization and its relationship to childhood sexual abuse history and lifetime PTSD. Subst Abuse 23(1):17–30. doi:10.1023/a:1013678626447
Torchalla I, Nosen L, Rostam H, Allen P (2012) Integrated treatment programs for individuals with concurrent substance use disorders and trauma experiences: a systematic review and meta-analysis. J Subst Abuse Treat 42(1):65–77. doi:10.1016/j.jsat.2011.09.001
Trafton JA, Minkel J, Humphreys K (2006) Opioid substitution treatment reduces substance use equivalently in patients with and without posttraumatic stress disorder. J Stud Alcohol 67(2):228–235
van Dam D, Ehring T, Vedel E, Emmelkamp PM (2013) Trauma-focused treatment for posttraumatic stress disorder combined with CBT for severe substance use disorder: a randomized controlled trial. BMC Psychiatry 13:172. doi:10.1186/1471-244X-13-172
van Dam D, Vedel E, Ehring T, Emmelkamp PM (2012) Psychological treatments for concurrent posttraumatic stress disorder and substance use disorder: a systematic review. Clin Psychol Rev 32(3):202–214. doi:10.1016/j.cpr.2012.01.004
Winters LE, Karow A, Reimer J, Fricke S, Kuhnigk O, Schäfer I (2014) Psychometric properties of the Posttraumatic Diagnostic Scale (PDS) in alcohol-dependent patients. Subst Abus 35(3):262–267
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Schäfer, I., Langeland, W. (2015). Posttraumatic Stress Disorders and Addiction. In: Dom, G., Moggi, F. (eds) Co-occurring Addictive and Psychiatric Disorders. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-45375-5_12
Download citation
DOI: https://doi.org/10.1007/978-3-642-45375-5_12
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-45374-8
Online ISBN: 978-3-642-45375-5
eBook Packages: MedicineMedicine (R0)