Abstract
Hidradenitis suppurativa (HS, acne inversa) is a chronic and recurrent disease affecting the apocrine-bearing areas of skin. Although previously thought to arise from inflammation of the apocrine glands, evidence now points to follicular occlusion as the primary event, though the disease has distinct differences from acne vulgaris where occlusion also plays a role. Hidradenitis suppurativa varies in severity, ranging from occasional isolated inflammatory nodules to numerous painful inflammatory nodules with draining ulcers, sinus tracts, and scarring. While there is no cure for hidradenitis suppurativa, nor a standard protocol for treatment, therapy can help control the disease. Treatment options including oral antibiotics, hormonal therapy, immunosuppressants, biologics, and surgery are reviewed. In addition to medical and surgical therapy, supporting the psychosocial well-being of HS patients, especially adolescents, is very important, and HS support groups or referral for psychological evaluation can be helpful.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Hidradenitis suppurativa (HS), also known as acne inversa, is an inflammatory disease of the apocrine-bearing areas of the skin. HS is chronic, recurrent, difficult to treat, and potentially debilitating. Onset of HS typically occurs after puberty, but rare prepubertal cases have been reported [1]. Females are three times more likely to be affected than males. The prevalence is estimated to be 1–2 % in the general population [2]. It appears to be less prevalent among individuals 55 years and older, but more common among young adults, in which one study noted a prevalence of 4 % [3, 4].
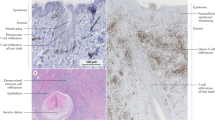
Verneuil first coined the term “hidradenitis suppurativa” in 1854 from the Greek words hidros for sweat and adne for gland, believing that the disease was caused primarily by purulent inflammation of apocrine glands. Since that time, the cause remains elusive, but histologic studies demonstrate that HS is a disease of the hair follicle. Follicular occlusion and dilation of the pilosebaceous unit lead to rupture and result in secondary inflammation of the apocrine glands. Along with acne conglobata, dissecting cellulitis, and pilonidal sinuses, HS is considered part of the follicular occlusion tetrad. Smoking, obesity, and mechanical friction are associated with HS and are exacerbating factors for some patients. HS commonly occurs in the intertriginous areas, typically the axillae, inguinal, anogenital, mammary, and inframammary regions, but other apocrine-prominent areas can be affected, such as the scalp, retroauricular skin, and chest. Double comedones and tender subcutaneous nodules are characteristic. The nodules are deeper than and lack the superficial purulent appearance of furuncles. Nodules often rupture, draining a foul-smelling purulent discharge, or become painful, deep dermal abscesses. As the disease progresses, sinus tracts, hypertrophic fibrotic scars, and dermal contractures can develop. Complications include infection, anemia, lymphedema, and fistulae to the urethra, bladder, or rectum in HS of the perineum.
Two methods of clinical staging for HS have been proposed. The Hurley staging system divides HS into three stages depending on the presence of sinus tracts and scars [5] (Table 4.1 and Figs. 4.1, 4.2, and 4.3). In contrast, the Sartorius system was developed to better assess treatment efficacy in clinical studies. This system scores regional and total disease severity based on involved anatomic regions, number and type of lesions, distance between lesions, and presence of normal skin between lesions.
Hidradenitis suppurativa, Hurley stage III. 16-year-old female with multiple inflammatory papules and nodules, chronically draining abscesses, and sinus tracts with exuberant granulation tissue in the axillae (shown here), inframammary region, and groin. Multiple systemic therapies, including doxycycline, minocycline, clindamycin and rifampin, and infliximab, have been unsuccessful. Because of coexistent medical conditions, dapsone, hormonal therapy, and oral retinoids were contraindicated
The psychosocial impact of HS can be profound. The chronic serous, bloody, and purulent exudate, pain, and physical deformity of private or hidden areas of the body are a tremendous psychological burden [2]. HS can disrupt school attendance, self-image, and employment. Patients lose an average of 2.7 workdays per year because of the disease, with women losing more days than males [6]. Patients with HS report a quality of life worse than those with alopecia, mild to moderate psoriasis, vascular anomalies of the face, and atopic dermatitis [7]. Younger patients are more likely to feel depressed, unworthy, and unlovable than older individuals, and this may explain the greater tendency for recall of alcohol abuse, suicidal ideation, and/or suicide attempts during adolescence [8]. In many cases, patients are told by medical professionals that nothing can be done for them, leading to more isolation and despair.
1 Management
There are few randomized controlled trials of therapy for HS and less data for pediatric patients. Treatment is guided by the severity and progression of disease. Patients must understand that as there is no cure for HS, the goals of therapy are to alleviate pain, minimize inflammation and scarring, maintain the disease at the early stages, and postpone the need for extensive surgery.
Treatment of localized, mild HS (Hurley I) consists of topical therapies and lifestyle changes. Smokers should be counseled on smoking cessation, and if obese, healthy weight loss strategies should be emphasized. Decreasing mechanical irritation through loose-fitting cotton clothing and avoidance of shaving, depilation, deodorants, heat, and humidity should be initiated early. Warm compresses or soaking baths can soothe inflamed lesions, and topical antibiotic/antiseptic or benzoyl peroxide soaps are appropriate. Topical clindamycin is a commonly used topical antibiotic agent to treat HS and can be effective in reducing the number of abscesses and pustules [9]. Combination topical therapies for acne, such as clindamycin-benzoyl peroxide preparations, are also useful. If these conservative measures are not enough, intralesional steroids are very helpful in alleviating painful nodules and halting progression to purulent, draining nodules. Other systemic therapy can be added, including oral antibiotics, if needed.
2 Systemic Antibiotics
Patients and physicians often view the purulent discharge from HS lesions as evidence of bacterial infection, but half of HS lesions are culture negative [10]. In culture-positive lesions, Staphylococcus epidermidis, Staphylococcus aureus, and coagulase-negative Staphylococci are most commonly isolated [10–12]. Often cultures are polymicrobial, with both gram-positive and gram-negative organisms. Gram-negative organisms such as Klebsiella, Proteus, and Escherichia coli may be frequently cultured from perineal HS [13]. Bacteria cultured from HS typically arise from secondary bacterial superinfection or represent colonization. Systemic antibiotics having anti-inflammatory and antibacterial properties can target the inflammation and bacterial superinfection that arise following follicular occlusion.
The tetracycline family (e.g., doxycycline and minocycline) and clindamycin are commonly used oral antibiotics for the treatment of HS and appear to be clinically helpful, though large studies supporting their efficacy are lacking. Tetracyclines are selected because of their anti-inflammatory and antibacterial properties and known efficacy in acne vulgaris. However, in one study comparing topical clindamycin to tetracycline 500 mg twice daily for at least 3 months, there was no significant difference in disease improvement between the two treatment arms [14]. Combination antibiotic therapy with clindamycin and rifampin has also been used in HS. Although there are no randomized controlled trials, there have been several case series of its efficacy in HS. Clindamycin 300 mg twice daily with rifampin 300 mg twice daily for at least 10 weeks decreased clinical severity, but diarrhea was a major side effect and can limit its use [15–17].
Combination antibiotic therapy with rifampin, moxifloxacin, and metronidazole has also been reportedly effective for HS. A series of 28 patients with severe HS were treated with rifampin 10 mg/kg/day, moxifloxacin 400 mg daily, and metronidazole 500 mg three times a day for 6 weeks, followed by rifampin and moxifloxacin therapy for 12 weeks [18]. Sixteen patients (57 %) had complete remission, with no active lesions at the end of the 18-week treatment course. Individuals with less severe disease (Hurley stage I and II) were more likely to achieve complete remission. Despite these promising results, the adverse effects were significant. Sixty-four percent of patients reported gastrointestinal side effects, predominantly nausea and diarrhea; 35 % of females reported vaginal candidiasis; and 14 % had moxifloxacin-associated tendonitis, which resulted in treatment termination.
Dapsone is an antibiotic effective in the treatment of neutrophilic dermatoses. Since HS has a prominent neutrophilic infiltrate, dapsone has been used as a treatment option, but the results have been mixed. A series of five patients responded to 25–150 mg of dapsone within 4–12 weeks of starting the medication [19]. A subsequent series of 24 patients treated with 50–200 mg of dapsone daily showed that only 38 % of patients had improvement, while 62 % had none. After cessation of treatment, the patients who responded reported a rapid recurrence of disease [20]. Prior to starting treatment with dapsone, patients should be screened for glucose-6-phosphate dehydrogenase (G6PD) deficiency and monitored for anemia during therapy.
3 Retinoids
Because early lesions of HS show follicular occlusion, acne therapies are commonly utilized for the treatment of HS. Unfortunately, the responsiveness of HS to such therapies often differs from acne vulgaris or nodulocystic acne. Isotretinoin has often been used to treat HS, but with very variable results. Early, small case reports were promising [21–24]. More recently, a retrospective review of 68 patients with moderate and severe HS treated with low-dose isotretinoin (mean dose 0.56 mg/kg/day) for 4–6 months demonstrated only 23.5 % of patients with clearance; an additional 20.6 % had marked improvement. Twenty-nine percent of patients dropped out before completing 4 months of treatment because of side effects and poor response to therapy [25]. Another review of 88 HS patients treated with isotretinoin showed that 77 % of them felt they had no improvement, and 6.9 % felt there was worsening of their disease following treatment [26].
Acitretin (mean dose 0.59 mg/kg/day) for 9–12 months was efficacious for severe HS in one small study [27]. The re-esterification of acitretin to etretinate in the presence of alcohol limits its use in the adolescent and adult populations, particularly in females, as both compounds are teratogens. Etretinate has an 80- to 160-day half-life, so if females of childbearing potential receive this drug, contraception is required not only during acitretin use but also for 3 years after discontinuation of treatment.
4 Hormones
Although the onset of HS usually corresponds with puberty, HS patients have normal androgen profiles and no difference in levels compared to age-, weight-, and hirsute-matched controls [28]. Altered end-organ sensitivity to androgens is postulated in HS, and antiandrogen treatments have been investigated as therapeutic options. Finasteride is a selective type II 5α-reductase inhibitor used for the treatment of benign prostatic hyperplasia and androgenetic alopecia in adult men. Finasteride has been tried in a small number of male and female patients with HS. A 5 mg daily dose produced significant clinical improvement in six of seven patients, with three having complete healing [29]. The multiple side effects of this medication, however, including breast tenderness, gynecomastia, irreversible sexual dysfunction, depression, anxiety, increased risk of prostate cancer in men, and teratogenicity limit the use of this medication.
Cyproterone acetate is an antiandrogen agent that has been used in female HS patients, but it is not available in the United States. Cyproterone acetate 50 mg/ethinyloestradiol 50 µg daily and cyproterone acetate 100 mg daily have both produced improvement in disease activity in females. [30, 31]
Several combination oral contraceptives with lower androgenic activity have gained FDA labeling for acne vulgaris. While quite effective for many female patients with resistant acne, oral contraceptives appear to have mixed efficacy in the treatment of HS in females. There are no controlled trials for this off-label use of oral contraceptives.
5 Immunosuppressants
Although HS has long been categorized as a form of acne, the lack of consistent improvement with acne therapies including isotretinoin argues that HS may be a different disease. More recently, HS has been considered to be an inflammatory disorder. The efficacy of intralesional steroid therapy to the inflamed sterile nodules of HS is supportive of this view. Systemic corticosteroids can provide temporary relief, but the multiple side effects of systemic steroids preclude long-term therapy. Several case reports have described improvement with cyclosporine of 3–6 mg/kg/day, but disease often recurs after treatment discontinuation, [32, 33] and long-term therapy is limited by the increased risk for hypertension and nephrotoxicity. Methotrexate at 12.5–15 mg weekly resulted in no clinical improvement of HS in one series of three patients [34]. Colchicine failed to reduce the severity of HS in patients treated with 0.5 mg twice daily for up to 4 months [35].
6 Biologics
Elevated tumor necrosis factor-alpha (TNFα) and interleukin(IL)-1β levels are noted in HS lesional and normal perilesional skin. Biologic agents that target the TNFα and IL-1β pathways have been used with promising results [36]. None of the biologics are approved by the Food and Drug Administration for the treatment of adult or pediatric HS. Of the few studies using biologics to treat HS, only a handful of patients under 18 years of age have been included [37, 38]. However, they have been used for other pediatric diseases: infliximab is approved for the treatment of pediatric inflammatory bowel disease in those age 6 years and older, etanercept is approved for the treatment of juvenile idiopathic arthritis in those age 2 years and older, and adalimumab is approved for the treatment of juvenile idiopathic arthritis in those age 4 years and older.
Infliximab, a chimeric monoclonal antibody to TNFα, has been the most studied of all the biologics in the treatment of HS. Several case reports and case series demonstrated that infliximab decreases clinical severity, but the long-term efficacy remains in question [37, 39–49]. Treatment regimens varied widely. Most studies utilized 5 mg/kg infusions at week 0, 2, and 6, with a variable number of infusions every 8 weeks thereafter. Some patients were given concurrent low-dose methotrexate to decrease the likelihood of developing neutralizing antibodies. Long-term disease control varied, with two studies reporting disease relapse 6 weeks to 4 months after stopping therapy [44, 45], while another showed no relapse in ten patients with follow-up of 4–24 months [46]. Reported adverse effects include an eczema-like eruption [47], abscess [47], abdominal pain caused by colon cancer [48], multifocal motor neuropathy with conduction block [48], severe allergic reaction with bronchospasm and urticaria [48], infliximab-induced lupus reaction [49], and hypersensitivity reaction to infliximab [49]. An 8-week randomized, placebo-controlled, crossover trial of 30 patients showed that a greater, though not statistically significant, number of patients treated with infliximab achieved at least a 50 % decrease in disease severity, but there was a significant improvement in patient-reported quality of life and visual analog scale scores [50].
Uncontrolled studies and case reports of etanercept showed that it was efficacious and well tolerated for HS, given at 50 mg weekly for at least 12 weeks [38, 51–53]. One study decreased dosing to 25 mg weekly after the initial treatment period [54], whereas another study started at 50 mg twice weekly for 24 weeks before decreasing to 25 mg twice weekly for another 24 weeks [55]. In contrast, a 12-week randomized, placebo-controlled trial of 20 patients found no significant difference between etanercept and placebo-treated patients in disease severity or quality of life [56]. No significant adverse effects from etanercept were reported in these studies.
After several case reports of successful control of HS with adalimumab were published [57–62], a 12-week randomized, placebo-controlled trial in 21 patients was performed. The dosing was based on standard psoriasis treatment: an initial dose of 80 mg, followed by 40 mg every other week. Compared to placebo, there was a significant decrease in clinical severity based on the Sartorius score, but nonsignificant decreases in quality of life and pain. Adalimumab was generally well tolerated, but the treatment group had a higher number of infections. As with etanercept, there was poor long-term control, as all patients relapsed by the 3-month follow-up [63].
Ustekinumab is a newer biologic agent that targets IL-12 and IL-23 cytokines in the Th1 immune pathway. A handful of HS cases successfully treated with ustekinumab have been reported [64, 65], but further larger-scale and placebo-controlled studies are needed to better assess safety and efficacy in treating HS.
7 Other Therapies
Cryotherapy has been reported for the treatment of individual inflammatory nodules. One study described ten patients with persistent, painful nodules treated with one freeze-thaw cycle of cryotherapy. Eight of the ten patients reported improvement in the treated nodules, but also had significant pain with treatment and long, painful healing complicated by infections and ulcerations [66].
Photodynamic therapy has shown mixed results in case reports. Some patients have noted complete clearance [67–70], but an equal number of patients saw no improvement [69, 71, 72]. A series of 13 patients treated with psoralen plus ultraviolet A (PUVA) therapy demonstrated that 38 % of patients cleared and 31 % had moderate clearance [73].
A single case report of botulinum toxin A injection for axillary HS showed complete remission of symptoms for 10 months [74]. The authors proposed that toxin inhibition of acetylcholine release decreases apocrine gland secretion, and with decreased accumulation of these secretions in an occluded follicle, the risk of follicular rupture and inflammation is decreased.
8 Laser Surgery
Ablative and nonablative laser therapy have been utilized as an alternative to surgical excision for HS. Several reports have shown successful localized treatment with carbon dioxide lasers. One of the first reports described the treatment of 24 patients with a stepwise horizontal vaporization technique with second-intention healing. Healing time was 4 weeks, and after a mean follow-up of 27 weeks, 92 % of patients reported no recurrence of disease in the treated areas [75]. Another early study treated seven patients with axillary and inguinoperineal disease with carbon dioxide laser and second-intention healing. After the 4- to 8-week healing time, patients were left with flat and linear scars, with only one patient experiencing a recurrence [76]. Three subsequent studies have shown similar positive responses [77–79]. Reported complications included axillary scar contracture [76, 79], hypertrophic granulation tissue [78], cellulitis [78], Sweet’s syndrome [78], and candidal wound infection [76].
Long-pulse neodymium:yttrium-aluminum-garnet (Nd:YAG) laser has shown some promise as a nonablative laser therapy for HS. As the chromophore for the Nd:YAG laser is the hair follicle, laser surgery might selectively halt the primary follicular occlusion process of early HS. A randomized controlled trial treated 17 patients with topical benzoyl peroxide wash 10 % and clindamycin 1 % lotion only versus these topical treatments plus Nd:YAG (using 4 monthly laser sessions). The entire affected area was treated with one pass, and inflammatory nodules, abscesses, and fistulae were treated with three stacked pulses. There was significantly more improvement in disease severity with adding Nd:YAG treatment and no reported adverse effects, [80] but more studies are needed to determine safety and efficacy.
9 Surgery
Patients with debilitating HS unresponsive to the therapies above should consider consultation for surgical treatment by a surgeon experienced in HS care. The best approach has yet to be determined, but surgical procedures can be divided into incision and drainage, unroofing of sinus tracts, and excision. Incision and drainage is often unsatisfactory. One study demonstrated 100 % recurrence after an average of 3 months [81].
Deroofing of sinus tracts can aid in tract healing. After the surgeon determines the extent of the tracts by exploring nodules and sinus tracts with a blunt probe, the roof of the tracts is surgically removed. The open tracts are allowed to heal by second intention; healing time averages 2 weeks. Two studies have shown this method to have a low recurrence rate and low complication rate, with the most common complication being postoperative bleeding [82, 83].
Wide excision is generally recommended over local excision for severe disease, because the recurrence rate is almost two times higher with local excision [81]. Several studies have shown that complete radical excision of the affected areas offers a low recurrence rate, with the inframammary, inguinogenital, and buttock being more likely to have recurrent disease [81, 84–86]. Complications include contractures [84, 85], suture dehiscence [87], bleeding or hematoma [85, 87], wound infection [85, 87], and pain [85]. Evidence also suggests that split-thickness skin grafts or flaps lead to lower recurrence rates compared to primary closure. A review of 72 patients who had excision demonstrated disease recurrence in 13 % of those closed with split-thickness grafts, 19 % of those closed with flaps, and 54 % of those with primary closure [88]. A subsequent review of 106 patients after excision showed no recurrence for those closed with flaps or split-thickness skin grafts versus 70 % recurrence in patients who had primary closure [89].
10 Approach to Managing Pediatric Hidradenitis Suppurativa
HS is a chronic, inflammatory, scarring disease that has no cure. There are no FDA-approved treatments, and formal guidelines do not exist for the treatment of HS. Although some pediatric patients have mild disease that remits with minimal intervention, many patients suffer from recurring painful nodules, ulcers, and scars. HS can have a significant impact on quality of life, lifestyle, and self-esteem. Many do not seek medical attention due to embarrassment or lack of past treatment efficacy. Moreover, painful lesions can limit activity and exercise, contributing to obesity, which in turn can exacerbate HS.
Management of HS is challenging because the data for treatment is limited and even more so in children, with few randomized controlled trials and with most treatment modalities having mixed results. Currently, the treatment of HS is as much art as science, and therapy should be selected bearing in mind the age of the patient, the disease activity, and risk-benefit ratio of the intervention, with the goal being to limit disease activity and postpone higher-risk procedures such as surgery. Multimodal management is often needed. Table4.2 reviews the dosing and side effects of selected systemic medications.
Mild HS (Hurley Stage I) may be treated with antimicrobial washes (e.g., benzoyl peroxide cleansers) and topical clindamycin. Combination products such as benzoyl peroxide-clindamycin gel have less impact on microbial resistance and may provide beneficial comedolytic effects. Clindamycin-tretinoin gel is another off-label option. Tender inflammatory nodules often respond well to low-strength intralesional steroid injections, particularly if early lesions are injected. If multiple nodules frequently recur, oral tetracycline antibiotics can be added to the regimen, such as doxycycline or minocycline 100 mg twice daily or sustained release minocycline, which is expensive but well tolerated and convenient with single daily dosing. If inadequate response is seen after 10–12 weeks, or if progression to Stage II disease occurs, clindamycin 300 mg and rifampin 300 mg twice daily for at least 10 weeks should be considered. Dapsone and isotretinoin are helpful in some patients, but data for these agents is less convincing. Surgical deroofing of sinus tracts can supplement systemic therapy as well.
If the above treatments are insufficient or if the disease progresses to Hurley Stage III, surgical consultation for partial or complete excision or ablative or nonablative laser treatment may be considered. Alternatively, systemic biologics can be considered, with infliximab being the most studied therapy for HS at this time.
For women who have flares of HS with their menstrual cycle, a trial of an oral contraceptive can be helpful. The oral contraceptives with FDA labeling for acne vulgaris are preferable as they are low in androgenic activity. As discussed earlier, patients who are obese should be counseled on healthy weight loss, and smokers should be directed to cessation strategies. Support groups or professional counseling can be very helpful for patients living with chronic HS. Lastly, teratogenic medications, such as isotretinoin and acitretin, should be used with extreme caution in the adolescent female population, with concomitant reliable contraception and serial pregnancy tests.
Pediatric HS remains an orphan disease and a therapeutic challenge needing further investigation.
Key Points
-
Hidradenitis suppurativa (HS) is a chronic disorder due to follicular occlusion and secondary inflammation of the apocrine glands.
-
Although some have mild disease, others progress to having numerous painful nodules with draining ulcers, sinus tracts, and scarring.
-
Treatment goals are to limit disease activity and psychosocial impact and to postpone higher-risk procedures such as surgery. Systemic agents (e.g., oral antibiotics, hormonal therapy, immunosuppressants, and biologics) along with laser treatments may be utilized for moderate to severe cases.
-
Most data for therapies are extrapolated from adult disease, and pediatric HS needs further attention and study.
Abbreviations
- FDA:
-
Food and Drug Administration
- HS:
-
Hidradenitis suppurativa
- Kg:
-
Kilogram
- Mg:
-
Milligram
- Nd:YAG:
-
Neodymium:yttrium-aluminum-garnet
- PUVA:
-
Psoralen plus ultraviolet A
References
Mengesha YM, Holcombe TC, Hansen RC. Prepubertal hidradenitis suppurativa: two case reports and review of the literature. Pediatr Dermatol. 1999;16(4):292–6.
Jemec GB. Medical treatment of hidradenitis suppurativa. Expert Opin Pharmacother. 2004;5:1767–70.
Revuz JE, Canoui-Poitrine F, Wolkenstein P, et al. Prevalence and factors associated with hidradenitis suppurativa: results from two case–control studies. J Am Acad Dermatol. 2008;59:596–601.
Jemec GB, Heidenheim M, Nielsen NH. The prevalence of hidradenitits suppurativa and its potential precursor lesions. J Am Acad Dermatol. 1996;35:191–4.
Hurley HJ. Axillary hyperhidrosis, apocrine bromhidrosis, hidradenitis suppurativa, and familial benign pemphigus: surgical approach. In: Roenigk RK, Roenigk HH, editors. Dermatologic surgery. New York: Marcel Dekker; 1989. p. 729–39.
Jemec GB, Heidenheim M, Nielsen NH. Hidradenitis suppurativa – characteristics and consequences. Clin Exp Dermatol. 1996;21:419–23.
Von der Werth JM, Jemec GB. Morbidity in patients with hidradenitis suppurativa. Br J Dermatol. 2001;144:809–13.
Esmann S, Jemec GB. Psychosocial impact of hidradenitis suppurativa: a qualitative study. Acta Derm Venereol. 2011;91:328–32.
Clemmensen OJ. Topical treatment of hidradenitits suppurativa with clindamycin. Int J Dermatol. 1983;22:325–8.
Jemec GB, Faber M, Gutschik E, et al. The bacteriology of hidradenitis suppurativa. Dermatology. 1996;193:203–6.
Lapins J, Jarstrand C, Emtestam L. Coagulase-negative staphylococci are the most common bacteria found in cultures from the deep portions of hidradenitis suppurativa lesions, as obtained by carbon dioxide laser surgery. Br J Dermatol. 1999;140:90–5.
Sartorius K, Killasli H, Oprica C, et al. Bacteriology of hidradenitis suppurativa exacerbations and deep tissue cultures obtained during carbon dioxide laser treatment. Br J Dermatol. 2012;166:879–83.
Shaughnessy DM, Greminger RR, Margolis IB, et al. Hidradenitis suppurativa. A plea for early operative treatment. JAMA. 1972;222:320–1.
Jemec GB, Wendelbow P. Topical clindamycin versus systemic tetracycline in the treatment of hidradenitis suppurativa. J Am Acad Dermatol. 1998;39:971–4.
Mendonça CO, Griffiths CEM. Clindamycin and rifampicin combination therapy for hidradenitis suppurativa. Br J Dermatol. 2006;154:977–8.
Van der Zee HH, Boer J, Prens EP, et al. The effect of combined treatment with oral clindamycin and oral rifampicin in patients with hidradenitis suppurativa. Dermatology. 2009;219:143–7.
Gener G, Canoui-Poitrine F, Revuz JE, et al. Combination therapy with clindamycin and rifampicin for hidradenitis suppurativa: a series of 116 consecutive patients. Dermatology. 2009;219:148–54.
Join-Lambert O, Coignard H, Jais JP, et al. Efficacy of rifampin-moxifloxacin-metronidazole combination therapy in hidradenitis suppurativa. Dermatology. 2011;222:49–58.
Kaur MR, Lewis HM. Hidradenitis suppurativa treated with dapsone: a case series of five patients. J Dermatolog Treat. 2006;17:211–3.
Yazdanyar S, Boer J, Ingvarsson G, et al. Dapsone therapy for hidradenitis suppurativa: a series of 24 patients. Dermatology. 2011;222:342–6.
Jones DH, Cunliffe WJ, King K. Hidradenitis suppurativa—lack of success with 13-cis-retinoic acid. Br J Dermatol. 1982;107:252.
Dicken CH, Powell ST, Spear KL. Evaluation of isotretinoin treatment of hidradenitis suppurativa. J Am Acad Dermatol. 1984;11:500–2.
Norris JFB, Cunliffe WJ. Failure of treatment of familial widespread hidradenitis suppurativa with isotretinoin. Clin Exp Dermatol. 1986;11:579–83.
Brown CF, Gallup DG, Brown VM. Hidradenitis suppurativa of the anogenital region: response to isotretinoin. Am J Obstet Gynecol. 1988;158:12–5.
Boer J, van Gemert M. Long-term results of isotretinoin in the treatment of 68 patients with hidradenitis suppurativa. J Am Acad Dermatol. 1999;40:73–6.
Soria A, Canoui-Poitrine F, Wolkenstein P, et al. Absence of efficacy of oral isotretinoin in hidradenitis suppurativa: a retrospective study based on patients’ outcome assessment. Dermatology. 2009;218:134–5.
Boer J, Nazary M. Long-term results of acitretin therapy for hidradenitis suppurativa. Is acne inversa also a misnomer? Br J Dermatol. 2011;164:170–5.
Barth JH, Layton AM, Cunliffe WJ. Endocrine factors in pre-and postmenopausal women with hidradenitis suppurativa. Br J Dermatol. 1996;134:1057–9.
Joseph MA, Jayaseelan E, Ganapathi B, et al. Hidradenitis suppurativa treated with finasteride. J Dermatolog Treat. 2005;16:75–8.
Mortimer PS, Dawber RP, Gales MA, et al. A double-blind controlled cross-over trial of cyproterone acetate in females with hidradenitis suppurativa. Br J Dermatol. 1986;115:263–8.
Sawers RS, Randall VA, Ebline FJ. Control of hidradenitis suppurativa in women using combined antiandrogen (cyproterone acetate) and oestrogen therapy. Br J Dermatol. 1986;115:269–74.
Roase RF, Goodfield MJ, Clark SM. Treatment of recalcitrant hidradenitis suppurativa with oral cyclosporine. Clin Exp Dermatol. 2006;31:154–6.
Buckley DA, Rogers S. Cyclosprin-responsive hidradenitis suppurativa. J R Soc Med. 1995;88:289P–90.
Jemec GB. Methotrexate is of limited value in the treatment of hidradenitis suppurativa. Clin Exp Dermatol. 2002;27:523–9.
Van der Zee HH, Prens EP. The anti-inflammatory drug colchicine lacks efficacy in hidradenitis suppurativa. Dermatology. 2011;223:169–73.
Van der Zee HH, de Ruiter L, van den Broecke DG, et al. Elevated levels of tumor necrosis factor (TNF)-α, interleukin (IL)-1β and IL-10 in hidradenitis suppurativa skin: a rationale for targeting TNF-α and IL-1β. Br J Dermatol. 2011;164:1292–8.
Adams DR, Gordon KB, Devenyi AG, et al. Severe hidradenitis suppurativa treated with infliximab infusion. Arch Dermatol. 2003;139:1540–2.
Cusack C, Buckley C. Etanercept: effective in the management of hidradenitis suppurativa. Br J Dermatol. 2006;154:726–9.
Sullivan TP, Welsh E, Kerdel FA, et al. Infliximab for hidradenitis suppurativa. Br J Dermatol. 2003;149:1046–9.
Alecsandru D, Padilla B, Izquierdo JA, et al. Severe refractory hidradenitis suppurativa in an HIV-positive patient successfully treated with infliximab. Arch Dermatol. 2010;146:1343–5.
Moschella SL. Is there a role for infliximab in the current therapy of hidradenitis suppurativa? A report of three treated cases. Int J Dermatol. 2007;46: 1287–91.
Fernandez-Vozmediano JM, Armario-Hita JC. Infliximab for the treatment of hidradenitis suppurativa. Dermatology. 2007;215:41–4.
Thielen AM, Barde C, Saurat JH. Long-term infliximab for severe hidradenitis suppurativa. Br J Dermatol. 2006;154:1105–7.
Brunasso AM, Delfino C, Massone C. Hidradenitis suppurativa: are tumor necrosis factor-α blockers the ultimate alternative? Br J Dermatol. 2008;159:761–3.
Lasocki A, Sinclair R, Foley P, et al. Hidradenitis suppurativa responding to treatment with infliximab. Australas J Dermatol. 2010;51:186–90.
Mekkes JR, Bos JD. Long-term efficacy of a single course of infliximab in hidradenitis suppurativa. Br J Dermatol. 2008;158:370–4.
Delage M, Samimi M, Atlan M, et al. Efficacy of infliximab for hidradenitis suppurativa: assessment of clinical and biological inflammatory markers. Acta Derm Venereol. 2011;91:169–71.
Fardet L, Dupuy A, Kerob D, et al. Infliximab for severe hidradenitis suppurativa: transient clinical efficacy in 7 consecutive patients. J Am Acad Dermatol. 2007;56:624–8.
Usmani N, Clayton TH, Everett S, et al. Variable response of hidradenitis suppurativa to infliximab in four patients. Clin Exp Dermatol. 2007;32:204–5.
Grant A, Gonzalez T, Montgomery MO, et al. Infliximab therapy for patients with moderate to severe hidradenitis suppurativa: a randomized, double-blind, placebo-controlled crossover trial. J Am Acad Dermatol. 2010;62:205–17.
Sotiriou E, Apalla Z, Ioannidos D. Etanercept for the treatment of hidradenitis suppurativa. Acta Derm Venereol. 2009;89:82–3.
Giamarellos-Bourboulis EJ, Pelekanou E, Antonopoulou A, et al. An open-label phase II study of the safety and efficacy of etanercept for the therapy of hidradenitis suppurativa. Br J Dermatol. 2008;158:567–72.
Pelekanou A, Kanni T, Savva A, et al. Long-term efficacy of etanercept in hidradenitis suppurativa: results from an open-label phase II prospective trial. Exp Dermatol. 2010;19:538–40.
Lee RA, Dommasch E, Treat J, et al. A prospective clinical trial of open-label etanercept for the treatment of hidradenitis suppurativa. J Am Acad Dermatol. 2009;60:565–73.
Zangrilli A, Esposito M, Mio G, et al. Long-term efficacy of etanercept in hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2008;22:1260–2.
Adams DR, Yankura JA, Fogelberg AC, et al. Treatment of hidradenitis suppurativa with etanercept injection. Arch Dermatol. 2010;146:501–4.
Moul DK, Korman N. Severe hidradenitis suppurativa treated with adalimumab. Arch Dermatol. 2006;142:1110–1.
Blanco R, Martinez-Taboada VM, Villa I, et al. Long-term successful adalimumab therapy in severe hidradenitis suppurativa. Arch Dermatol. 2009;145:580–4.
Sotiriou E, Apalla Z, Vakirilis E, et al. Efficacy of adalimumab in recalcitrant hidradenitis suppurativa. Eur J Dermatol. 2009;19:180–1.
Amando M, Grant A, Kerdel FA. A prospective open-label clinical trial of adalimumab for the treatment of hidradenitis suppurativa. Int J Dermatol. 2010;49: 950–5.
Arenbergerova M, Gkalpakiotis S, Arenberger P. Effective long-term control of refractory hidradenitis suppurativa with adalimumab after failure of conventional therapy. Int J Dermatol. 2010;49:1445–9.
Sotiriou E, Goussi C, Lallas A, et al. A prospective open-label clinical trial of efficacy of the every week administration of adalimumab in the treatment of hidradenitis suppurativa. J Drugs Dermatol. 2012;11(Suppl):15–20.
Miller I, Lynggaard CD, Lophaven S, et al. A double-blind placebo-controlled randomized trial of adalimumab in the treatment of hidradenitis suppurativa. Br J Dermatol. 2011;165:391–8.
Gulliver WP, Jemec GB, Baker KA. Experience with ustekinumab for the treatment of moderate to severe hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2012;26(7):911–4.
Sharon VR, Garcia MS, Bagheri S, et al. Management of recalcitrant hidradenitis suppurativa with ustekinumab. Acta Derm Venereol. 2012;92:320–1.
Bong JL, Shalders K, Saihan E. Treatment of persistent painful nodules of hidradenitis suppurativa with cryotherapy. Clin Exp Dermatol. 2003;28:241–4.
Guglielmetti A, Bedoya J, Acuna M, et al. Successful aminolevulinic acid photodynamic therapy for recalcitrant severe hidradenitis suppurativa. Photodermatol Photoimmunol Photomed. 2010;26:110–1.
Saraceno R, Teoli M, Casciello C, et al. Methyl aminolaevulinate photodynamic therapy for the treatment of hidradenitis suppurativa and pilonidal cysts. Photodermatol Photoimmunol Photomed. 2009;25: 164–5.
Schweiger ES, Riddle CC, Aires DJ. Treatment of hidradenitis suppurativa by photodynamic therapy with aminolevulinic acid: preliminary results. J Drugs Dermatol. 2011;10:381–6.
Gold M, Bridges TM, Bradshaw VL, et al. ALA-PDT and blue light therapy for hidradenitis suppurativa. J Drugs Dermatol. 2004;3:S32–5.
Sotiriou E, Apalla Z, Maliamani F, et al. Treatment of recalcitrant hidradenitis suppurativa with photodynamic therapy: report of five cases. Clin Exp Dermatol. 2009;34:e235–6.
Strauss RM, Pollock B, Stables GI, et al. Photodynamic therapy using aminolaevulinic acid does not lead to clinical improvement in hidradenitis suppurativa. Br J Dermatol. 2005;152:803–4.
Shareef M, Dawe R. Bath psoralen plus ultraviolet A for hidradenitis suppurativa: a review of 13 patients. Br J Dermatol. 2011;164:895–6.
O’Reilly DJ, Pleat JM, Richards AM. Treatment of hidradenitis suppurativa with botulinum toxin A. Plast Reconstr Surg. 2005;116:1575–6.
Lapins J, Marcusson JA, Emtestam L. Surgical treatment of chronic hidradenitis suppurativa: CO2 laser stripping-secondary intention technique. Br J Dermatol. 1994;131:551–6.
Finley EM, Ratz JL. Treatment of hidradenitis suppurativa with carbon dioxide laser excision and second-intention healing. J Am Acad Dermatol. 1996;34:465–9.
Lapins J, Sartorius K, Emtestam L. Scanner-assisted carbon dioxide laser surgery: a retrospective follow-up study of patients with hidradenitis suppurativa. J Am Acad Dermatol. 2002;47:280–5.
Hazen PG, Hazen BP. Hidradenitis suppurativa: successful treatment using carbon dioxide laser excision and marsupialization. Dermatol Surg. 2010;36:208–13.
Madan V, Hindle E, Hussain W, et al. Outcomes of treatment of nine cases of recalcitrant severe hidradenitis suppurativa with carbon dioxide laser. Br J Dermatol. 2008;159:1309–14.
Mahmoud BH, Tierney E, Hexsel C, et al. Prospective controlled clinical and histopathologic study of hidradenitis suppurativa treated with the long-pulsed neodymium:yttrium-aluminium-garnet laser. J Am Acad Dermatol. 2010;62:637–45.
Ritz JP, Runkel N, Haier J, et al. Extent of surgery and recurrence rate of hidradenitis suppurativa. Int J Colorectal Dis. 1998;13:164–8.
Van Hattem S, Spoo JR, Horvath B, et al. Surgical treatment of sinuses by deroofing in hidradenitis suppurativa. Dermatol Surg. 2012;38:494–7.
Van der Zee HH, Prens EP, Boer J. Deroofing: a tissue-saving surgical technique for the treatment of mild to moderate hidradenitis suppurativa lesions. J Am Acad Dermatol. 2010;63:475–80.
Bohn J, Svensson H. Surgical treatment of hidradenitis suppurativa. Scand J Plast Reconstr Surg Hand Surg. 2001;35:305–9.
Bieniek A, Matusiak L, Okulewicz-Gojlik D, et al. Surgical treatment of hidradenitis suppurativa: experiences and recommendations. Dermatol Surg. 2010;36:1998–2004.
Buyukasik O, Hasdemir AO, Kahramansoy N, et al. Surgical approach to extensive hidradenitis suppurativa. Dermatol Surg. 2011;37:835–42.
Rompel R, Petres J. Long-term results of wide surgical excision in 106 patients with hidradenitis suppurativa. Dermatol Surg. 2000;26:638–43.
Watson JD. Hidradenitis suppurativa – a clinical review. Br J Plast Surg. 1985;38:567–9.
Mandal A, Watson J. Experience with different treatment modules in hidradenitis suppurativa: a study of 106 cases. Surgeon. 2005;3:23–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Jen, M., Chang, M.W. (2014). Hidradenitis Suppurativa. In: Tom, W. (eds) Severe Skin Diseases in Children. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-39532-1_4
Download citation
DOI: https://doi.org/10.1007/978-3-642-39532-1_4
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-39531-4
Online ISBN: 978-3-642-39532-1
eBook Packages: MedicineMedicine (R0)