Abstract
Crescentic glomerulonephritis is not a specific disease but rather is a manifestation of severe glomerular injury that can be caused by many different etiologies and pathogenic mechanisms. The major immunopathologic categories of crescentic glomerulonephritis are immune complex-mediated, anti-glomerular basement membrane (anti-GBM) antibody-mediated, and pauci-immune, which usually is antineutrophil cytoplasmic autoantibody (ANCA)-mediated [1]. Table 9.1 shows the relative frequency of these immunopathologic categories of crescentic glomerulonephritis. Crescentic glomerulonephritis can occur as a renal-limited process or as a component of systemic small-vessel vasculitis, such as IgA vasculitis (Henoch-Schönlein purpura), cryoglobulinemic vasculitis, Goodpasture’s syndrome, or ANCA vasculitis [2–5]. In addition to small-vessel vasculitis, the kidneys also are a frequent site of involvement by other forms of vasculitis, such as polyarteritis nodosa, Kawasaki disease, giant cell arteritis, and Takayasu arteritis [3, 5] (Table 9.2).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Kawasaki Disease
- Giant Cell Arteritis
- Takayasu Arteritis
- Polyarteritis Nodosa
- Crescentic Glomerulonephritis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction/Clinical Setting
Crescentic glomerulonephritis is not a specific disease but rather is a manifestation of severe glomerular injury that can be caused by many different etiologies and pathogenic mechanisms. The major immunopathologic categories of crescentic glomerulonephritis are immune complex-mediated, anti-glomerular basement membrane (anti-GBM) antibody-mediated, and pauci-immune, which usually is antineutrophil cytoplasmic autoantibody (ANCA)-mediated [1]. Table 9.1 shows the relative frequency of these immunopathologic categories of crescentic glomerulonephritis. Crescentic glomerulonephritis can occur as a renal-limited process or as a component of systemic small-vessel vasculitis, such as IgA vasculitis (Henoch-Schönlein purpura), cryoglobulinemic vasculitis, Goodpasture’s syndrome, or ANCA vasculitis [2–5]. In addition to small-vessel vasculitis, the kidneys also are a frequent site of involvement by other forms of vasculitis, such as polyarteritis nodosa, Kawasaki disease, giant cell arteritis, and Takayasu arteritis [3, 5] (Table 9.2).
2 Anti-Glomerular Basement Membrane Disease
Anti-GBM disease is a small-vessel vasculitis that affects the glomerular capillaries and pulmonary alveolar capillaries [6, 7]. It may occur as an isolated glomerulonephritis or as the renal component of a pulmonary-renal syndrome. In the latter instance, the term Goodpasture’s syndrome is appropriate.
2.1 Pathologic Findings
2.1.1 Light Microscopy
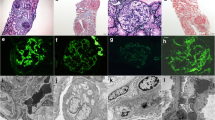
By light microscopy, the acute glomerular lesion is characterized by segmental to global fibrinoid necrosis with crescent formation in over 90 % of patients [1]. Periodic acid-Schiff (PAS) and silver stains demonstrate breaks in the GBM in areas of necrosis (Fig. 9.1). Glomerular segments that do not have necrosis often are remarkably normal or have a slight increase in neutrophils. Marked neutrophil infiltration is observed in association with the necrosis in occasional specimens. Features of aggressive immune complex glomerulonephritis are notably absent, such as marked capillary wall thickening and endocapillary hypercellularity. Often there are breaks in Bowman’s capsule, occasionally with associated reactive multinucleated giant cells.
With time, foci of glomerular necrosis evolve into glomerular sclerosis, and cellular crescents become fibrous crescents. Acute tubulointerstitial inflammation that is centered on necrotic glomeruli evolves to more regional or generalized interstitial fibrosis with chronic inflammation and tubular atrophy.
2.1.2 Immunofluorescence Microscopy
Immunohistology demonstrates intense linear staining of the GBM (Fig. 9.2), predominantly for immunoglobulin G (IgG) along with more granular and discontinuous staining for C3 (Fig. 9.3). Immunoglobulin A (IgA)-dominant anti-GBM disease is very rare [8]. Irregular staining for fibrin occurs at sites of fibrinoid necrosis and within crescents. In some specimens, the fibrinoid of glomeruli is so extensive that identification of linear staining along intact segments of GBM is difficult. Care must be taken not to misinterpret anti-GBM disease with extensive destruction of GBMs as pauci-immune disease.
2.1.3 Electron Microscopy
Electron microscopy reveals no immune complex-type electron-dense deposits unless there is concurrent immune complex glomerulonephritis. Glomerular basement membrane gaps are present in areas of necrosis and crescent formation. Cellular crescents typically contain electron-dense fibrin tactoid strands.
2.1.4 Clinicopathologic Correlations
Anti-GBM disease is caused by autoantibodies directed against the α3 chain in the noncollagenous domain of type IV collagen [9]. Serologic confirmation of anti-GBM disease should be sought, but approximately 10–15 % of patients with anti-GBM disease have negative results. About a quarter to a third of patients with anti-GBM disease also have ANCA [10]. Thus, all anti-GBM patients should be tested for ANCA. Patients with both anti-GBM and ANCA have an intermediate prognosis that is worse than ANCA alone but better than anti-GBM alone. Anti-GBM antibodies characteristically occur as one episode that clears with immunosuppressive therapy, whereas ANCA disease is characterized by more persistent antibodies and frequent recurrence of disease. Patients with combined disease may have permanent remission of the anti-GBM disease with recurrence of the ANCA disease alone.
Approximately half the patients with anti-GBM disease present with rapidly progressive glomerulonephritis without pulmonary hemorrhage, and the other half have pulmonary-renal syndrome (Goodpasture’s syndrome). However, most patients with pulmonary-renal syndrome have ANCA disease rather than anti-GBM disease [11].
Anti-GBM is the most aggressive form of crescentic glomerulonephritis and has the worst prognosis, especially if aggressive immunosuppressive treatment is not instituted quickly before the serum creatinine is >6 mg/dL [1, 7, 12]. The serum creatinine at the time treatment is begun is a better predictor of outcome than any pathologic feature. The current approach to treatment uses high-dose cytotoxic agents combined with plasma exchange [6, 7, 12].
3 Pauci-immune and ANCA Glomerulonephritis and Vasculitis
3.1 Introduction/Clinical Setting
Antineutrophil cytoplasmic autoantibody disease is a form of small-vessel vasculitis [2–4, 13–15]. Small-vessel vasculitides have a predilection for capillaries, venules, and arterioles, although arteries may be affected [2, 13, 14]. The major immunopathologic categories of small-vessel vasculitis are anti-GBM disease, immune complex small-vessel vasculitis, and pauci-immune small-vessel vasculitis. Pauci-immune small-vessel vasculitis is characterized by an absence or paucity (<2+) of vessel staining for immunoglobulin, which is distinct from the conspicuous linear staining in anti-GBM disease and prominent granular staining in immune complex disease. Approximately 85 % of active untreated pauci-immune crescentic glomerulonephritis and vasculitis is associated with ANCA in the circulation. The major clinicopathologic expressions of pauci-immune and ANCA-associated vasculitis are renal-limited vasculitis (pauci-immune necrotizing and crescentic glomerulonephritis), microscopic polyangiitis, granulomatosis with polyangiitis (Wegener’s granulomatosis), and eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome) (Table 9.2) [2, 3, 13, 14].
3.2 Pathologic Findings
3.2.1 Light Microscopy, Immunofluorescence, and Electron Microscopy
Histologically, the glomerular lesion in all four clinicopathologic categories is identical and is characterized by fibrinoid necrosis and crescent formation (Figs. 9.4, 9.5, and 9.6). In less than 10 % of specimens, the glomerulonephritis may be accompanied by necrotizing arteritis (Fig. 9.7) (usually in the interlobular arteries) or medullary angiitis affecting the vasa rectae (Fig. 9.8).
By light microscopy and electron microscopy, pauci-immune crescentic glomerulonephritis cannot be distinguished from anti-GBM crescentic glomerulonephritis; however, immunofluorescence microscopy readily distinguishes the two. Pauci-immune crescentic glomerulonephritis, by definition, has no or low-intensity immunostaining for immunoglobulin; however, often there is some staining for immunoglobulin [16]. A reasonable approach is to draw the line at 2+ or less immunoglobulin staining on a scale of 0–4+ for pauci-immune disease. Pauci-immune crescentic glomerulonephritis often has irregular segmental or global staining for fibrin at sites of fibrinoid necrosis and crescent formation (Fig. 9.9). Electron microscopy may show no electron-dense deposits, or there may be a few small electron-dense deposits, especially if immunofluorescence microscopy revealed staining for immunoglobulin. Glomerular basement membrane breaks often can be identified.
Microscopic polyangiitis (MPA) is necrotizing vasculitis with few or no immune deposits affecting small vessels, that is, capillaries, venules, or arterioles [4, 13, 14, 17]. Necrotizing arteritis occurs in some but not all patients. Approximately 90 % of patients with microscopic polyangiitis have glomerulonephritis. Hemorrhagic pulmonary alveolar capillaritis is common in patients with microscopic polyangiitis. Histologically, the acute vascular lesions, for example, affecting dermal venules or small visceral arteries, are characterized by segmental fibrinoid necrosis, and mural and perivascular neutrophilic infiltration with leukocytoclasia (Figs. 9.7 and 9.8). Within a few days, the predominant inflammatory cells in the vasculitic lesions evolve from neutrophils to mononuclear leukocytes, and the fibrinoid necrosis transforms into fibrosis.
Granulomatosis with polyangiitis (Wegener’s granulomatosis) (GPA) is characterized by granulomatous inflammation that frequently is accompanied by necrotizing vasculitis affecting capillaries, venules, arterioles, and small- to medium-sized arteries [4, 13, 14]. Necrotizing granulomatous inflammation is observed most often in the upper and lower respiratory tract but occasionally in other tissues, such as the orbit, skin, and kidneys. The granulomatous lesions typically have extensive necrosis with infiltrating mononuclear and polymorphonuclear leukocytes with scattered multinucleated giant cells. Necrotizing glomerulonephritis is common (Fig. 9.4). The vasculitis in the lungs and elsewhere can involve arteries, arterioles, veins, venules, and capillaries and can be granulomatous or nongranulomatous. The latter is histologically identical to the necrotizing vasculitis of MPA and eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome) (EGPA).
EGPA is characterized by eosinophil-rich granulomatous inflammation involving the respiratory tract and necrotizing vasculitis affecting small- to medium-sized vessels that is associated with asthma and blood eosinophilia [13, 14]. The vasculitis of EGPA cannot be definitively differentiated by histology from the vasculitis of GPA or MPA; however, there is a tendency for more eosinophils among the infiltrating leukocytes. Likewise, the necrotizing granulomatous inflammation of EGPA resembles that of GPA but tends to have more eosinophils. The vasculitis of EGPA most often affects the lungs, heart, peripheral nervous system, skin, gut, and kidneys. The pauci-immune focal necrotizing glomerulonephritis of EGPA usually is less severe than the glomerulonephritis in GPA or MPA but is histologically indistinguishable.
3.3 Etiology/Pathogenesis
Overall, approximately 90 % of patients with pauci-immune crescentic glomerulonephritis or pauci-immune small-vessel vasculitis have circulating ANCA [4, 15]. The two major antigen specificities of ANCA are for proteinase 3 (PR3-ANCA) or myeloperoxidase (MPO-ANCA). Either specificity can occur in any clinicopathologic variant of ANCA disease, but MPO-ANCA is most prevalent in renal-limited disease and PR3-ANCA is most prevalent in GPA. Overall, <50 % of patients with EGPA have ANCA; however, >90 % of EGPA patients with crescentic glomerulonephritis have ANCA, usually MPO-ANCA. In Asia, MPO-ANCA is much more frequent than PR3-ANCA in all clinicopathologic variants [18]. Genetic associates and important disease characteristics, such as response to therapy and frequency of relapses, correlate better with ANCA specificity than with clinicopathologic phenotype [19].
There is compelling in vitro and animal model experimental data showing that ANCA IgG causes glomerulonephritis and vasculitis, probably by direct interaction with neutrophils (and possibly monocytes) resulting in neutrophil activation with release of complement-activating factors, lytic enzymes, and reactive oxygen radicals that cause the inflammatory injury to glomeruli and vessels [20, 21]. Clinical support is provided by the observation that a neonate developed pulmonary hemorrhage and nephritis following transplacental transfer of maternal MPO-ANCA IgG [22] as well as the effectiveness of therapy that reduce circulating antibody levels, such as immunosuppressive drugs, anti-B antibodies, and plasma exchange [15].
3.4 Clinicopathologic Correlations
All variants of pauci-immune small-vessel vasculitis and glomerulonephritis are treated with high-dose corticosteroids and immunosuppressive agents when there is active and progressive glomerulonephritis [15, 23, 24]. Remission of glomerulonephritis and other vasculitic manifestations can be induced in approximately 80 % of patients. However, a third or more of patients may have one of more relapses within 5 years. Nevertheless, the 5-year renal and patient survival approaches 80 % if treatment is instituted early enough. As with anti-GBM disease, the renal outcome in ANCA disease correlates best with the serum creatinine at the time treatment was begun. A pathologic classification system categorizes pauci-immune crescentic glomerulonephritis as focal (50 % or more histologically normal glomeruli), crescentic (50 % or more crescents), sclerotic (50 % or more global sclerosis), or mixed (<50 % normal, crescentic, and sclerotic glomeruli) [25]. Renal function at presentation and the outcome is best for the focal class and worst for the sclerotic class.
4 Polyarteritis Nodosa
4.1 Introduction/Clinical Setting
Polyarteritis nodosa is a medium-vessel vasculitis because it primarily affects medium-sized arteries rather than smaller vessels [3, 5, 13, 14]. The other major category of medium-vessel vasculitis is Kawasaki disease (Table 9.2). Medium-vessel vasculitides have a predilection for main visceral arteries, such as the coronary, hepatic, renal, and mesenteric arteries and their major first- and second-order branches. These same vessels, however, also can be involved with large-vessel vasculitides and small-vessel vasculitides. In the kidney, the major targets of polyarteritis nodosa and Kawasaki disease are the interlobar and arcuate arteries, whereas ANCA small-vessel vasculitis primarily targets interlobular arteries, arterioles, vasa rectae, and glomerular capillaries [3].
The term polyarteritis nodosa has been used quite variably over the years [2]. Some definitions have allowed involvement of vessels smaller than arteries, including glomerulonephritis. However, the Chapel Hill nomenclature system confined the term to necrotizing arteritis that affects arteries but does not involve vessels smaller than arteries and thus does not cause glomerulonephritis [13, 14]. If pauci-immune necrotizing arteritis is associated with glomerulonephritis, this would be categorized as microscopic polyangiitis by the Chapel Hill nomenclature system.
4.2 Pathologic Findings
4.2.1 Light Microscopy
By light microscopy, polyarteritis nodosa is characterized by segmental transmural fibrinoid necrosis and accompanying inflammation (Fig. 9.10), which initially has predominantly neutrophils and sometimes eosinophils but within several days has predominantly mononuclear leukocytes. The segmental inflammation and necrosis in artery walls may produce an aneurysm (actually a pseudoaneurysm) by eroding through the artery wall into the perivascular tissue. Infarction and hemorrhage are the major consequences of renal involvement by polyarteritis nodosa.
Polyarteritis nodosa is treated with high-dose corticosteroids, often in combination with cytotoxic drugs such as cyclophosphamide [26]. Polyarteritis nodosa is less likely to recur after induction of remission than is microscopic polyangiitis.
5 Kawasaki Disease
The sine qua non of Kawasaki disease is the mucocutaneous lymph node syndrome, which includes fever, cutaneous and oral mucosal erythema and sloughing, and lymphadenopathy [5, 13, 14, 27]. Kawasaki disease is a disease of childhood that rarely occurs after the age of 5 years. The vasculitic lesions of Kawasaki disease involve predominantly small- and medium-sized arteries, with a special predilection for the coronary arteries [27]. The histologic lesions are characterized by segmental transmural edema and necrosis with infiltration by monocytes and neutrophils (Fig. 9.11). The necrotizing lesions of Kawasaki disease have less fibrinoid material and more edema than the necrotizing lesions of polyarteritis nodosa.
Kawasaki disease rarely causes clinically significant renal disease; however, postmortem examination demonstrates substantial involvement of renal arteritis in many patients who die from Kawasaki disease [27].
The arteritis of Kawasaki disease responds very well to treatment with aspirin and high-dose intravenous immunoglobulin [28].
6 Large-Vessel Vasculitis
6.1 Introduction/Clinical Setting
Large-vessel vasculitis affects the aorta and its major branches with transmural chronic inflammation that is characterized even in the acute phase by infiltration of predominantly mononuclear leukocytes, often with accompanying multinucleated giant cells [5, 13, 14]. The two major clinicopathologic variants are giant cell arteritis and Takayasu arteritis. The best distinguishing feature between these two variants is the age of the patient [13, 14]. Giant cell arteritis rarely occurs before 50 years of age, and Takayasu arteritis virtually always occurs prior to the age of 50. Postmortem examination reveals that pathologic involvement of the kidneys by large-vessel vasculitis is much more common than clinically significant involvement [3]. The most common clinical manifestation is renovascular hypertension, which results from involvement of the main renal artery or its major branches, especially the lobar (interlobar) arteries [29].
6.2 Pathologic Findings
The pathologic hallmark of large-vessel vasculitis is transmural infiltration of artery walls by mononuclear leukocytes accompanied by variable numbers of multinucleated giant cells (Fig. 9.12) [5]. This often results in thickening of the intima and narrowing of the lumen, which causes ischemia to the tissue supplied by the artery. Involvement of the renal artery can cause a pattern of renal artery stenosis atrophy in the renal parenchyma that is characterized by marked reduction in the size of the tubules and resultant clustering of glomeruli close to one another. This pattern of atrophy has much less interstitial fibrosis and inflammation than the ischemic atrophy of hypertensive arterionephrosclerosis.
Large-vessel vasculitis that is causing substantial ischemic injury is treated with corticosteroids [30, 31]. Patients with severe disease or steroid toxicity require other immunosuppressive agents, e.g., cyclophosphamide, mycophenolate mofetil, or azathioprine. Reconstructive vascular surgery (stent or bypass) may be required to improve flow to ischemic tissues.
References
Jennette JC (2003) Rapidly progressive and crescentic glomerulonephritis. Kidney Int 63:1164–1172
Jennette JC, Falk RJ (1997) Small vessel vasculitis. N Engl J Med 337:1512–1523
Jennette JC, Falk RJ (1994) The pathology of vasculitis involving the kidney. Am J Kidney Dis 24:130–141
Jennette JC, Thomas DB (2007) Pauci-immune and antineutrophil cytoplasmic autoantibody glomerulonephritis and vasculitis. In: Jennette JC, Olson JL, Schwartz MM, Silva FG (eds) Heptinstall’s pathology of the kidney, 6th edn. Lippincott Williams & Wilkins, Philadelphia, pp 643–674
Jennette JC, Singh H (2007) Renal involvement in polyarteritis nodosa, Kawasaki disease, giant cell arteritis and Takayasu arteritis. In: Jennette JC, Olson JL, Schwartz MM, Silva FG (eds) Heptinstall’s pathology of the kidney, 6th edn. Lippincott Williams & Wilkins, Philadelphia, pp 675–700
Tarzi RM, Cook HT, Pusey CD (2011) Crescentic glomerulonephritis: new aspects of pathogenesis. Semin Nephrol 31:361–368
Cui Z, Zhao MH (2011) Advances in human antiglomerular basement membrane disease. Nat Rev Nephrol 7:697–705
Borza DB, Chedid MF, Colon S, Lager DJ, Leung N, Fervenza FC (2005) Recurrent Goodpasture’s disease secondary to a monoclonal IgA1-kappa antibody autoreactive with the alpha1/alpha2 chains of type IV collagen. Am J Kidney Dis 45:397–406
Pedchenko V, Bondar O, Fogo AB, Vanacore R, Voziyan P, Kitching AR, Wieslander J, Kashtan C, Borza DB, Neilson EG, Wilson CB, Hudson BG (2010) Molecular architecture of the Goodpasture autoantigen in anti-GBM nephritis. N Engl J Med 363:343–355
Short AK, Esnault VL, Lockwood CM (1995) Anti-neutrophil cytoplasm antibodies and anti-glomerular basement membrane antibodies: two coexisting distinct autoreactivities detectable in patients with rapidly progressive glomerulonephritis. Am J Kidney Dis 26:439–445
Niles JL, Böttinger EP, Saurina GR, Kelly KJ, Pan G, Collins AB, McCluskey RT (1996) The syndrome of lung hemorrhage and nephritis is usually an ANCA-associated condition. Arch Intern Med 56:440–445
Levy JB, Turner AN, Rees AJ, Pusey CD (2001) Long-term outcome of antiglomerular basement membrane antibody disease treated with plasma exchange and immunosuppression. Ann Intern Med 134:1033–1042
Jennette JC, Falk RJ, Andrassy K, Bacon PA, Churg J, Gross WL, Hagen EC, Hoffman GS, Hunder GG, Kallenberg CG et al (1994) Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum 37:187–192
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen EC, Hoffman GS, Jayne DR, Kallenberg CG, Lamprecht P, Langford CA, Luqmani RA, Mahr AD, Matteson EL, Merkel PA, Ozen S, Pusey CD, Rasmussen N, Rees AJ, Scott DG, Specks U, Stone JH, Takahashi K, Watts RA (2013) 2012 revised International Chapel Hill Consensus Conference Nomenclature of the Vasculitides. Arthritis Rheum 65:1–11
Kamesh L, Harper L, Savage CO (2002) ANCA-positive vasculitis. J Am Soc Nephrol 13:1953–1960
Harris AA, Falk RJ, Jennette JC (1998) Crescentic glomerulonephritis with a paucity of glomerular immunoglobulin localization. Am J Kidney Dis 32:179–184
Jennette JC, Thomas DB, Falk RJ (2001) Microscopic polyangiitis (microscopic polyarteritis). Semin Diagn Pathol 18:3–13
Chen M, Cui Z, Zhao MH (2010) ANCA-associated vasculitis and anti-GBM disease: the experience in China. Nephrol Dial Transplant 25:2062–2065
Lyons PA, Rayner TF, Trivedi S, Holle JU, Watts RA, Jayne DR, Baslund B, Brenchley P, Bruchfeld A, Chaudhry AN, Cohen Tervaert JW, Deloukas P, Feighery C, Gross WL, Guillevin L, Gunnarsson I, Harper L, Hrušková Z, Little MA, Martorana D, Neumann T, Ohlsson S, Padmanabhan S, Pusey CD, Salama AD, Sanders JS, Savage CO, Segelmark M, Stegeman CA, Tesař V, Vaglio A, Wieczorek S, Wilde B, Zwerina J, Rees AJ, Clayton DG, Smith KG (2012) Genetically distinct subsets within ANCA-associated vasculitis. N Engl J Med 367:214–223
Jennette JC, Falk RJ, Gasim AH (2011) Pathogenesis of antineutrophil cytoplasmic autoantibody vasculitis. Curr Opin Nephrol Hypertens 20:263–270
Jennette JC, Xiao H, Falk RJ (2006) The pathogenesis of vascular inflammation by antineutrophil cytoplasmic antibodies. J Am Soc Nephrol 17:1235–1242
Bansal PJ, Tobin MC (2004) Neonatal microscopic polyangiitis secondary to transfer of maternal myeloperoxidase-antineutrophil cytoplasmic antibody resulting in neonatal pulmonary hemorrhage and renal involvement. Ann Allergy Asthma Immunol 93:398–401
Bacon PA (1994) Therapy of vasculitis. J Rheumatol 21:788–790
Nachman PH, Hogan SL, Jennette JC, Falk RJ (1996) Treatment response and relapse in ANCA-associated microscopic polyangiitis and glomerulonephritis. J Am Soc Nephrol 7:33–39
Berden AE, Ferrario F, Hagen EC, Jayne DR, Jennette JC, Joh K, Neumann I, Noël LH, Pusey CD, Waldherr R, Bruijn JA, Bajema IM (2010) Histopathological classification of ANCA-associated glomerulonephritis. Kidney Int 21:1628–1636
Guillevin L, Lhote F (1998) Treatment of polyarteritis nodosa and microscopic poly-angiitis. Arthritis Rheum 41:2100–2105
Naoe S, Takahashi K, Masuda H, Tanaka N (1991) Kawasaki disease. With particular emphasis on arterial lesions. Acta Pathol Jpn 41:785–797
Kuo HC, Yang KD, Chang WC, Ger LP, Hsieh KS (2012) Kawasaki disease: an update on diagnosis and treatment. Pediatr Neonatol 53:4–11
Lagneau P, Michel JB (1985) Renovascular hypertension and Takayasu’s disease. J Urol 134:876–879
Koening CL, Langford CA (2006) Novel therapeutic strategies for large vessel vasculitis. Rheum Dis Clin North Am 32:173–186
Seko Y (2007) Giant cell and Takayasu arteritis. Curr Opin Rheumatol 19:39–43
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Fogo, A.B., Cohen, A.H., Colvin, R.B., Jennette, J.C., Alpers, C.E. (2014). Crescentic Glomerulonephritis and Vasculitis. In: Fundamentals of Renal Pathology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-39080-7_9
Download citation
DOI: https://doi.org/10.1007/978-3-642-39080-7_9
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-39079-1
Online ISBN: 978-3-642-39080-7
eBook Packages: MedicineMedicine (R0)