Abstract
Extracranial carotid disease is the leading cause of ischemic stroke. Several randomized controlled trials performed in the 1990s demonstrated a significant benefit in carotid endarterectomy for risk reduction of ischemic stroke and overall mortality, when compared to medical management alone. Unfortunately, not all patients are candidate for carotid revascularization with carotid endarterectomy. Transluminal carotid angioplasty and stenting has been found to be a “non-inferior” alternative to surgery in selected patients. The technology and methods used for angioplasty and stenting have evolved substantially over the last two decades and can be safely performed in most patients. Although percutaneous revascularization is unlikely to fully supplant its surgical counterpart, carotid angioplasty and stenting has become a reasonable option of carotid disease and assists in further individualizing patient care.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Internal Carotid Artery
- Carotid Stenosis
- Carotid Disease
- North American Symptomatic Carotid Endarterectomy Trial
- Carotid Angioplasty
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Cerebrovascular disease is the third leading cause of death in industrialized countries and accounts for the most common cause of hospitalization for all neurological diseases (Wolf et al. 1999). Stroke is the leading cause of adult disability. In the United States alone, an estimated $30 billion are lost due to disability per year (US Disability 2009). C. Miller Fisher first described the relationship between carotid artery disease and stroke (Fisher 1951). Extracranial vascular disease (ECVD) is a common cause of ischemic strokes (ISs) with approximately one-third of strokes caused by extracranial carotid disease (Brott et al. 2011; Liapis et al. 2009). Atherosclerotic disease represents the most common cause of ECVD, while arterial dissection, cystic medial necrosis, fibromuscular dysplasia, and vasculitis are other etiologies. Patients with atherosclerotic disease are at risk for myocardial infarction and peripheral vascular disease.
The treatment of carotid artery disease has undergone a significant evolution over the past three decades. Before the growing popularity of endovascular therapy with angioplasty and stenting, the North American Symptomatic Carotid Endarterectomy Trial (NASCET) and the European Carotid Surgery Trial (ECST) defined the benefits and risks of carotid endarterectomy in patients with symptomatic disease (NASCET 1991a; ECST 1991b). Although first described in 1979, percutaneous transluminal techniques were not widely used until the mid-1990s (Mathias et al. 1983; Mathias 1977). Since the first randomized trial, the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS), which completed in 1997, there have been several randomized studies to further define the indications and techniques for carotid angioplasty and stenting (CAS) (CAVATAS 2001).
In this chapter, we will discuss the history and evidence for open surgical treatment of ECVD (Note: a more detailed discussion of the indications and techniques of surgical treatment will be discussed in another chapter). Also, the evolution of carotid angioplasty and stenting (CAS), the growing indications, and technique for CAS will be described. And finally, anticipated complications and procedure limitations will be reviewed.
Carotid Endarterectomy
Historical Background : From Eastcott and DeBakey to NASCET and ECST
The first successful carotid endarterectomy (CEA) was described by Felix Eastcott (Eastcott et al. 1954) (Fig. 1). However, Michael DeBakey claimed to perform the operation earlier than Eastcott in 1953 (DeBakey 1996). Because of anecdotal reports of efficacy, the CEA gained significant popularity to treat ECVD to the point that an estimated 100,000 operations were being performed per year until 1985 (DeBakey 1975; Rob 1978; VA Cooperative Study 1986).
Criticism of unacceptable rates of mortality and morbidity regarding the procedure surfaced as the popularity increased (Winslow et al. 1988). In addition, concerns over appropriateness of the indication for surgery were raised. One report found that only 33 % of CEAs over the study period were found to have “appropriate” indications (Findlay et al. 2002). These concerns were established as the enthusiasm behind CEA was blunted, and the United States saw an approximate 40 % drop in absolute number of operations performed from 1985 to 1991 (Halm et al. 2003).
The reports of unfavorable results and inconsistent indications motivated neurologists, vascular surgeons, and neurosurgeons to design and carry out prospective randomized clinical studies in the United States and Europe. The initial results of the NASCET and ECST, published in 1991, demonstrated a significant benefit when compared to medical management alone in selected patients (Table 1). This resulted in a renewed enthusiasm for the CEA. In 1999, approximately 131,000 procedures were performed in the United States alone (Gross et al. 2000; Halm et al. 2003).
Randomized Control Trials
Fifty centers from Canada and the United States participated in NASCET from 1988 to 1991 while enrolling 2,885 patients, 2,226 with 30–69 % stenosis and 659 with 70–99 % stenosis. Altogether, 1,453 patients were randomized to the surgical arm of the NASCET. The investigators found a significant benefit in incidence of ipsilateral stroke within 2 years of randomization in patients with symptomatic severe carotid stenosis treated surgically (9 %) when compared to the medically managed group (26 %) (NASCET 1991c). Additionally, a clinical benefit was found in those patients with moderate (50–69 %) symptomatic stenosis with 15.7 % of surgically treated patients and 22.2 % of medically treated patients suffering an ipsilateral stroke during the 5-year study period (Barnett et al. 1998). The 8-year results of 5.7 % risk of disabling ipsilateral stroke and a 17.1 % risk of any ipsilateral stroke further demonstrated the long-term durability of the procedure (Ferguson et al. 1999).
Similarly, the ECST enrolled greater than 3,000 patients, with 1,811 patients randomized to surgery and 1,213 allocated to the medical control group. The investigators found a significant reduction in major stroke and death at 3 years in patients with 80 % or greater luminal carotid stenosis that underwent surgery (14.9 %), when compared to those randomized to the medical control group (26.5 %). They found an operative risk of 7 % for nonfatal stroke and death (ECST 1991b, 1998).
In 1999, Ferguson et al. published the data regarding the surgical complications of CEA in NASCET in Stroke (Ferguson et al. 1999). They found the total risk of disabling stroke and death at 90 days was approximately 2 %. Five statistically significant risk factors of increased risk of perioperative stroke or death were identified and include presenting hemispheric transient ischemic attack (TIA) versus retinal TIA (RR = 2.3), left-sided procedure (RR = 2.3), presence of contralateral carotid occlusion (RR = 2.2), ipsilateral ischemic lesion on presenting CT scan (RR = 1.8), and ulcerated or irregular plaque found on angiography (RR = 1.5). Approximately 9.3 % of surgeries were complicated by postoperative hematomas with less than half of hematomas requiring a return to the operating room or resulting in significant decline, and 8.6 % of patients suffered a cranial nerve (CN) injury with CEA.
Although the evidence for obtaining a significant benefit in patients with symptomatic carotid artery stenosis was confirmed with three large randomized control trials, the role of operative intervention for asymptomatic carotid disease remained controversial and ill defined (Mayberg et al. 1991; NASCET 1991a; ECST 1991b). The Veterans Affairs (VA) Cooperative Study enrolled 444 men with asymptomatic stenosis of 50 % or greater studied angiographically and randomized them to the surgical arm with CEA and aspirin (ASA) therapy or ASA therapy alone (Hobson et al. 1993). Eleven VA medical centers participated from 1983 to 1991. Patients were followed for a mean period of 47.9 months. The 30-day perioperative risk of disabling stroke or death was 4.7 %, which included morbidity and death from arteriography. The investigators found a significant reduction in ipsilateral neurological events in the surgical group (8.0 %) when compared to the medical arm (20.6 %). However, this was offset by the perioperative risk of disabling stroke or death, and statistical significance was not demonstrated. The most common cause of death in this study population was cardiac related (Hobson et al. 1993).
In 1995, the highly anticipated Asymptomatic Carotid Atherosclerosis Study (ACAS), which enrolled 1,662 patients from 39 centers, reported the 5-year risk for ipsilateral stroke or perioperative IS or death for patients randomized to CEA versus optimal medical management, which was 325 mg of ASA daily (Walker et al. 1995). Patients with carotid stenosis greater than 60 % who underwent surgery were found to have a perioperative stroke and death risk and 5-year ipsilateral stroke risk of 5.9 %. Patients who were randomized to the medical control group were found to have an 11 % 5-year ipsilateral stroke risk, and an absolute risk reduction of 1.2 % per year was defined. When only disabling strokes were evaluated, the 5-year absolute risk reduction decreased to 2.6 %. These results were determined with a 30-day morbidity and mortality (2.3 %) of CEA, which was exceedingly low when compared to NASCET (3.7 %) and ECST (3.8 %).
Some authors have found the modest to minimal benefit of CEA in asymptomatic patients, with the low incidence of neurological events, the significant improvements in “medical management,” and the significant cost of surgery to be difficult to justify the indication of CEA in asymptomatic ECVD (Abbott 2009; Mathias and Gissler 2002). These concerns may be justified as the risks of CEA have been found to vary by source of publication and practice. In 1996, Rothwell et al. performed a systematic review of the risks of IS and death related to CEA (Rothwell et al. 1996). The investigators found systematic heterogeneity when the risk of IS or death was reported by neurologists (7.7 %) versus surgeons (2.3 %). Also, Wennberg et al. reported significant variability in the risks of perioperative death among trial hospitals (1.4 %) and nontrial hospitals (2.5 %) (Wennberg et al. 1998). This has led some authors to conclude the risks of major perioperative IS and that mortality rates in randomized trials should not be extrapolated to reflect everyday practice (Mathias and Gissler 2002; Wholey et al. 1998).
Rational for Endovascular Treatment
Despite the well-established efficacy of open surgical treatment for ECVD, there are many patients who cannot safely undergo a CEA secondary to technical factors or because of severe comorbid medical illnesses, such as coronary artery disease and heart failure (Table 1) (Goldstein et al. 1994; Goldstein et al. 1998; Rothwell et al. 1996; Rothwell et al. 1997). With the significant risks of perioperative IS, death, and cardiac insults related to CEA and the growing popularity and efficacy of percutaneous angioplasty for coronary, renal, and peripheral disease during the late 1980s, it was inevitable that endovascular techniques be applied to ECVD.
Egas Moniz described the first successful cerebral angiogram in 1927, and Charles Kerber performed the first transluminal angioplasty of the carotid artery in 1980 (Doby 1992; Kerber et al. 1980). The popularity of endovascular therapy for ECVD continued to increase, and the first randomized controlled comparison of CEA versus CAS, CAVATAS, was performed from 1992 to 1997 (CAVATAS 2001). Since CAVATAS, several randomized trials have been performed with the indications of CAS continuously defined, and as endovascular techniques and instruments have evolved, it is clear that CEA and CAS should complement each other in individualizing patient care.
Carotid Angioplasty and Stenting
Early Randomized Control Trials and Embolic Protection Devices
As stated above, CAVATAS was the first randomized trial, which assigned patients to either treatment (as determined by the local investigators), CEA or endovascular treatment (CAVATAS 2001). Of the 504 patients enrolled, 97 % of who were symptomatic, 251 patients were assigned to endovascular treatment and 253 to CEA. There were no statistically significant differences in the rate of death or stroke at 30 days or in the rate of ipsilateral stroke at 3 years between the two treatment options. However, stenting was used in only 26 % of the percutaneously treated patients, and distal protection devices were not used, as they were not commercially available. The rates of severe (70–99 %) restenosis assessed by ultrasound at 1 year were significantly different, 14 % in the endovascular group versus 4 % in the CEA group. The endovascular group did, however, show expected improvements in rates of cranial nerve deficits (0 %) and neck hematomas (1.2 %), when compared to open surgery, 8.7 % and 6.7 %, respectively. As in NASCET and ECST, patients who were found to have high surgical risks because of premorbid factors were excluded from trial enrollment.
Another pair of early, randomized clinical trials underlined the variability of outcomes in CAS prior to the routine use of embolic protection devices (EPDs). The Wallstent trial was a randomized equivalency trial comparing CEA to CAS for patients with carotid stenosis greater than 60 % (Alberts 2001). The investigators found a 12.1 % rate of any stroke or death at 30 days with CAS and a 4.5 % rate in the CEA group. The 30-day and 1 year primary outcomes were not achieved. The study was terminated after only 209 patients were randomized because of the inferiority of CAS. Similarly, another randomized trial featuring the Wallstent compared patients undergoing CAS versus CEA for symptomatic carotid disease of greater than 70 % (Naylor et al. 1998). The primary end point was any stroke or death within 30 days of the procedure. Only 23 patients were randomized (17 underwent treatment) before the trial was suspended secondary to the high morbidity of the CAS group. None of the endovascular practitioners used EPDs in either of these two studies (Alberts 2001; Naylor et al. 1998).
In 1984, Theron and Bockenheimer developed the first commercially available balloon protection device designed for embolic protection during CAS (Theron et al. 1996). As techniques for CAS evolved, many physicians found significant benefits with embolic protection in preventing perioperative morbidity (Cremonesi et al. 2003; Jaeger et al. 2002; Al-Mubarak et al. 2002; Zhou et al. 2011). The three main principles of cerebral protection from embolism are:
-
Proximal blood flow arrest and reversal for cerebral protection
-
Distal blood flow arrest for cerebral protection
-
Filtering of blood flow distal to CAS
Flow arrest through the internal carotid artery (ICA) can be accomplished through proximal and distal balloon blockade (Fig. 2). Kachel first described proximal occlusion and temporary flow reversal with the use of a balloon in the common carotid artery (CCA) in 1991 (Kachel et al. 1991). Juan Parodi would later refine the technique with the now known Parodi Anti-Embolic System (Gore Neuro Protection System, W.L. Gore & Associates, Flagstaff, Arizona, United States) (Adami et al. 2002). This device consists of a long sheath with a balloon at its end for blockade of the CCA and a guidewire with a second balloon for the flow arrest in the external carotid artery (ECA). With inflation of both balloons, blood flow in the ICA will reverse down the sheath, be filtered, and be reinfused into the femoral vein. With this technique, the main advantage is a protected initial passage of the stenosis. With other embolic protection devices, at least one unprotected passage of the diseased segment is required prior to deploying the device. Some patients will not tolerate the temporary balloon occlusion, and the device is quite bulky, which can be cumbersome in some patients with tortuous anatomy. Two European series with a total of 86 patients found no major ISs or deaths at 30 days when the flow-reversal technique was employed for CAS (Adami et al. 2002; Rabe et al. 2006). This device is commercially available in Europe and limited to investigational use in the United States.
Proximal flow arrest for embolic protection. A patient with a symptomatic intraluminal thrombus refractory to anticoagulation treatment underwent CAS with proximal flow arrest. A pretreatment arteriogram (a, b) demonstrates intraluminal thrombus (white arrowheads). An arteriogram (c) with proximal balloon occlusion (white arrow) demonstrates arrest of flow during the procedure. A final arteriogram (d) after the stent has been deployed
The MO.MA Proximal Cerebral Protection Device (Medtronic, Minneapolis, Minnesota, United States) is a single catheter system with similar functionality of the Parodi Anti-Embolic System without the connection to the femoral vein. One multicenter trial found a 98.2 % device success rate with an exceedingly low 30-day major stroke rate (0.9 %) (Ansel et al. 2010). One difficulty with this system is the large 9 Fr introducer sheath recommended for use, as most current systems can be performed with much smaller sheaths. The MO.MA device received FDA approval in 2009. Another flow-reversal and proximal occlusion embolic protection device, the GORE Flow Reversal System (W.L. Gore & Associates, Flagstaff, Arizona, United States) was approved by the FDA in 2009 after the prospective, multicenter clinical EMPiRE trial (Clair et al. 2011). Investigators found a 30-day IS, death, and myocardial infarction rate of 3.7 %.
Theron and Bockenheimer independently developed the first embolic protection device with a flow-arrest style distal ICA balloon (Theron et al. 1996). Although this technology has evolved since its first inception, the principles remain the same. A balloon mounted on a guidewire is inflated with diluted contrast distal to the diseased segment, preferably in a straight vertical segment of the cervical ICA. Once inflated, a test injection is performed to confirm flow arrest, and then the operator can proceed with treating the diseased segment. Once stent angioplasty is completed, the segment proximal to the balloon is cleared of embolic material with flushing and aspiration. Flushing should be done with a low volume as to not “spill” proximal to the aspirating catheter. The alternating sequence of flushing and aspiration should be performed until the aspirate is clear of debris. This protection device should not be performed if the arteriogram demonstrates retrograde collateral flow from the ECA to the brain. Low operative morbidity and high technical success rates have been reported in clinical trials with such distal balloon protection devices (Kawarada et al. 2007; Theron et al. 1996; Tübler et al. 2001). Technical difficulties with the use of the device result from having to pass a potentially friable atheromatous lesion prior to deploying distal protection and with the continuous flushing and aspiration required to clear the debris (Mathias and Gissler 2002; Tübler et al. 2001). Few patients will not be able to tolerate temporary carotid occlusion. In one series, approximately 8 % of patients could not tolerate temporary occlusion because of immediate, although transient, neurological deterioration (Kawarada et al. 2007). Some authors believe patients with greater than 90 % stenosis will have a greater tolerance of temporary balloon occlusion (Mathias and Gissler 2002). Nonapproved distal flow-arrest balloon devices include the PercuSurge Guardwire (Medtronic, Minneapolis, Minnesota, United States) and the TriActive System (Kensey Nash, Exton, Pennsylvania, United States).
An alternative measure of distal cerebral protection involves blood filtration. Several distal filters have been developed with different filter shapes and pore sizes. Flow arrest is not required, although a balloon guide catheter can be used in conjunction for aspiration, if embolic material has completely obstructed the ICA proximal to the filter, although it has been reported that filter obstruction is not associated with increased risk of suffering a periprocedural IS (Maldonado et al. 2008). Frequent angiographic injections are recommended during the procedure after the filter is deployed to detect any embolic material or stagnation of contrast proximal to the filter. If a large thrombus is caught in the filter, the filter should not be recaptured in the usual way as this can dislodge embolic material distally. If this happens, the guide catheter should be advanced to the filter, then the catheter should be withdrawn into the descending aorta, and at this point, the filter should be withdrawn.
Although embolic filters require crossing the diseased segment prior to protection, use of this device is associated with a significant decrease in periprocedural reversible neurological events, when compared to distal balloon protection (0 % versus 10 %) (Powell et al. 2006). As stated several distal filters have been developed and include five FDA-approved devices: the Accunet (with the Acculink stent), the FilterWire EZ (Boston Scientific, Natick, Massachusetts, United States) (Fig. 3a), the SpiderFX (ev3, Plymouth, Minnesota, United States) (Fig. 3b), the AngioGuard (with the Precise stent, Cordis, Warren, New Jersey, United States), and the Emboshield (with the Xact stent, Abbott Vascular, Redwood City, California, United States). The advantages of the filter embolic protection systems include ease of deployment, good trackability, and increased flexibility of the guidewire.
To date, no single EPD or embolic protection strategy has been found to be superior to another in large, randomized trials (Lam 2009; Powell et al. 2006). Intraluminal thrombus, severe symptomatic stenosis, and a tortuous cervical ICA would make proximal balloon occlusion and flow reversal a more logical choice of EPD for CAS. A prospective European registry, Imaging in Carotid Angioplasty and Risk of Stroke (ICAROS), demonstrated a significant increase of embolic strokes after CAS in patients with carotid plaques found to have gray-scale median scores of less than 25, indicating a softer plaque that is more likely to embolize during the procedure (Biasi et al. 2004). Some operators believe that patients with gray-scale median scores less than 25 may be better served with a proximal EPD or with CEA. However, it should be noted that operator preference of EPD and familiarity are significant factors for procedural success. Although no consensus exists regarding the mandatory use of EPDs, some operators believe that CAS would not have become an acceptable alternative to CEA without their development (Lam 2009).
Contemporary Randomized Control Trials
Since CAVATAS, multiple clinical trials have been performed or are in process comparing CAS to CEA for various indications (Andziak 2006; Brott et al. 2010; CARESS Steering Committee 2003; Gaines and Randall 2005; International Carotid Stenting Study investigators et al. 2010; Rudarakanchana et al. 2009; SPACE Collaborative Group et al. 2006; Yadav et al. 2004). The Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy (SAPPHIRE) trial randomized high-risk symptomatic (>50 % stenosis) and asymptomatic patients (>80 % stenosis) to CEA or CAS with distal protection (Yadav et al. 2004). Criteria for high risk included clinically significant cardiac disease, severe pulmonary disease, contralateral carotid occlusion, contralateral laryngeal nerve palsy, previous radical neck surgery or neck radiation, recurrent stenosis after prior CEA, and age of over 80 years. Operators performed CAS with EPDs. Three hundred and thirty-four patients were evenly divided between CEA and CAS, although 7 % did not actually receive their assigned treatment. The rate of death, stroke, or myocardial infarction within 30 days or death or ipsilateral stroke at 1 year was 12.2 % for the patients assigned to CAS and 20.1 % for those assigned to CEA (P = 0.05). By 3 years there was no significant difference between the two treatments (Gurm et al. 2008). The rates of IS in patients with asymptomatic disease were 10.3 % in the CAS group and 9.2 % in the CEA group. While the major difference seen in the early time points is likely due to rates of periprocedural myocardial infarction, SAPPHIRE nevertheless supports the position that CAS is not inferior to CEA for high-risk patients.
In order to determine the “real-world” application of CAS, the Carotid Revascularization Using Endarterectomy or Stenting Systems (CaRESS) trial was performed (CARESS Steering Committee 2003). This was a multicenter, prospective, nonrandomized trial comparing CAS with distal protection to CEA in symptomatic and asymptomatic patients with carotid stenosis. The choice of treatment (CEA or CAS) was based solely on physician and patient preference. Three hundred and ninety-seven patients were enrolled (254 CEA and 143 CAS), and there was no significant difference in the primary end point of death and stroke at 30 days and a 1-year end point of death, IS, or MI. The 4-year data from CaRESS showed no differences in outcomes of all-cause mortality, IS, and MI (Zarins et al. 2009). The failure to reach statistical significance or “clinical equivalence” would suggest that the operators were able to assign patients to the appropriate treatment.
Two randomized European trials of symptomatic patients, Endarterectomy versus Angioplasty in Patients with Symptomatic Severe Carotid Stenosis (EVA-3S) and Stent-Supported Percutaneous Angioplasty of the Carotid artery versus Endarterectomy (SPACE), failed to show non-inferiority of CAS to CEA (Mas et al. 2008; SPACE Collaborative Group et al. 2006). Both trials showed a higher 30-day IS or death rate in patients treated with CAS, although there has been criticism of both trials regarding endovascular surgeon experience and technique (Andziak 2006). In EVA-3S surgeons performing CEA were required to have performed at least 25 operations in the preceding year, while interventionists were required to have performed as little as 5 CASs (Mas et al. 2008). Also, there was significant heterogeneity in the periprocedural management of antiplatelet therapy and intraprocedural anticoagulation. And finally, there were significant differences in 30-day IS or death rate in patients treated with or without an EPD during CAS (7.9 % versus 25 %, respectively).
The Carotid Revascularization Endarterectomy versus Stenting Trial (CREST) was published in 2010 (Brott et al. 2010). In this study, 2,502 patients with symptomatic (>50 % stenosis) and asymptomatic (>80 % stenosis) disease were randomly assigned to CAS or CEA from December 2000 to July 2008. The mean follow-up was 2.5 years with 1,271 enrolled to the CAS treatment group and 1,251 enrolled to CEA. To maintain a more rigorous monitoring of the interventionists allowed to enroll patients into CREST, operators were asked to submit their personal series of CAS procedures with notes and narrative summaries (Hobson et al. 2004). Four hundred and twenty- seven physicians applied to participate in CREST. Of those, 238 operators were selected by the Interventional Management Committee to participate for training and the lead-in phase of the trial, 73 were found to have satisfactory experience and were allowed to randomize patients without training, and 116 physicians did not qualify for training (Hopkins et al. 2010). During the lead-in phase, approved interventionists were monitored for up to 20 procedures using study devices, which included the Acculink stent and Accunet embolic protection system. The credentialing and monitoring process to ensure an acceptable baseline of experience in the participating interventionists of CREST has been more rigorous than any preceding randomized trial.
The CREST study was initially designed for patients with symptomatic lesions but was later modified to recruit asymptomatic patients as well. Additionally, the degree of stenosis required for enrollment varied according to the imaging modality. The primary end point was stroke, MI, or death within 30 days or any ipsilateral stroke within 4 years (Table 2). Stroke was defined as an increased NIH Stroke Scale of at least two points, while MI was defined as an increase in serum troponin, chest pain, and electrocardiographic changes. In other words, stroke was more likely to have a greater impact on health and quality of life compared to MI. Over a median follow-up of 2.5 years, there was no significant difference in primary end point between CAS (7.2 %) and CEA (6.8 %). However, the 30-day rate of stroke was significantly higher in CAS (4.1 %) compared to CEA (2.3 %), while the risk of myocardial infarction was lower (1.1 % versus 2.3 %). Additionally, in symptomatic patients, CAS had a significantly higher periprocedural stroke and death rate (6 %) compared to CEA (3.2 %). Investigators found an increased risk of stroke in older patients who underwent CAS (Voeks et al. 2011). Additionally, age was found to be a treatment effect modifier in CAS with increased risk of stroke with increasing age in 10-year increments. This effect was not found in patients who underwent CEA. Also, costs and cost-effectiveness were evaluated for each procedure in CREST (Vilain et al. 2012). Although CAS cost $1,025 more per patient, investigators estimated this increase to be trivial at 10 years in overall healthcare costs and quality-adjusted life expectancy impact, suggesting that cost should not be weighed significantly in deciding which of the two procedures should be performed.
There are currently three prospective, randomized trials enrolling low-risk patients for CAS. The Asymptomatic Carotid Stenosis Stenting versus Endarterectomy Trial (ACT1) is a North American trial currently enrolling low-surgical risk patients with asymptomatic stenosis (>80 % stenosis) to CAS or CEA. There is no pure medical arm to this trial. Similarly, the Asymptomatic Carotid Surgery Trial-2 (ACST-2) is comparing CAS to CEA in asymptomatic patients with high-grade stenosis. It is an international study that hopes to enroll 5,000 patients. Recent advances in medical therapy and the debate that asymptomatic carotid disease is best managed with medical therapy have led to the Transatlantic Asymptomatic Carotid Interventional Trial (TACIT) (Abbott 2009, 2010; Schneider and Naylor 2010). TACIT is a multicenter, international, prospective trial with three treatment arms (Gaines and Randall 2005). Patients with asymptomatic carotid stenosis of greater than 60 % found on duplex ultrasonography will be randomized to medical management alone, medical management with CAS, or medical management with CEA. Medical management consists of antiplatelet, lipid-lowering, and antihypertensive therapies, in addition to glucose control, smoking-cessation assistance, and lifestyle modification.
Patient Selection and Indications
Carotid stenosis is usually found either as the result of an evaluation for a patient who has suffered a stroke or TIA or in a screening test of an asymptomatic patient. The noninvasive diagnostic measures (Fig. 4), computed tomographic angiography (CTA), magnetic resonance angiography (MRA), and Doppler ultrasonography, are all capable of providing information on the degree of stenosis, but the gold standard test remains catheter angiography.
Noninvasive imaging for carotid stenosis. An axial image (a) and coronal (b) and sagittal (c) reconstructions of a CTA demonstrate focal carotid stenosis (white arrow in the axial image) at the ICA origin. An axial image (d) and a 3D reconstruction (e) of the left carotid artery demonstrate a focal high-grade stenosis of the CA (white arrowhead in the axial image). A Doppler ultrasonogram (f) demonstrates focal moderate stenosis with change in velocity across the lesion (white arrow)
The NASCET method for calculating the degree of stenosis measures the luminal diameter at the level of the stenotic lesion (R) compared with the diameter of the normal distal internal carotid artery beyond the carotid bulb (D) where the walls of the internal carotid artery first become parallel to each other (NASCET 1991c). The NASCET formula is: stenosis = (1–R/D) × 100 % (Fig. 5a). The NASCET method is frequently used in the United States, although it tends to underestimate the degree of stenosis, especially in the setting of near occlusion. An alternative measure of carotid stenosis is with the ECST method, where stenosis is measured using the most stenotic lumen (R) and a subjectively calculated normal lumen (N). The ECST formula is: stenosis = (1–R/N) × 100 % (Fig. 5b). We recommend that the degree of stenosis be calculated by the NASCET method applied to catheter angiography.
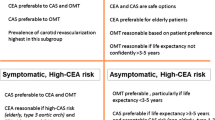
Based on the results of multiple prospective, randomized studies, the following guidelines are proposed for the use of CAS. These evidence-based treatment recommendations were assessed according to the criteria published by the American Heart Association/American Stroke Association (AHA/ASA) and the University of Oxford’s Center for Evidence-Based Medicine (CEBM) (Furie et al. 2011):
-
1.
CAS should be considered in patients with symptomatic severe stenosis (>70 %) who are high risk for CEA (AHA/ASA Class IIb; Level of Evidence B, CEBM Level 2b, Grade B) (Furie et al. 2011).
-
2.
For patients with symptomatic carotid disease with 50–69 % stenosis, CEA is recommended. CAS is considered an alternative to CEA for patients at average or low risk for endovascular surgery and for those that are high risk (>6 % morbidity and mortality) for CEA (AHA/ASA Class I; Level of Evidence B, CEBM Level 1b, Grade B). Factors considered high risk for endovascular surgery include severely elongated, calcified and/or atherosclerotic aortic arch, lesion length >10 mm, marked tortuosity or angulation of internal carotid artery, coexisting common carotid artery lesions, subtotal occlusion (“string sign”) of internal carotid artery, severe concentric calcification of target lesion, and intraluminal thrombus (Carotid Stenting Trialists’ Collaboration et al. 2010; Faggioli et al. 2007; Furie et al. 2011; Kastrup et al. 2008; Naggara et al. 2011). While patients 80 years or older were considered high risk for CEA in the SAPPHIRE trial, CREST showed a benefit for age < 70 years with CAS, perhaps due to anatomic factors such as abnormal aortic arch anatomy. We suggest that age alone should not be considered in determining CEA versus CAS and that other patient-specific factors should be considered (Table 3).
-
3.
The benefit of CAS in asymptomatic patients is less clear, and there is uncertainty regarding CAS over CEA (AHA/ASA Class IIb; Level of Evidence B, CEBM Level 2b, Grade B) (Goldstein et al. 2011).
-
4.
For patients with carotid stenosis < 50 %, there is no indication for CEA or CAS (AHA/ASA Class III; Level of Evidence B, CEBM Level 1b, Grade B) (Furie et al. 2011).
Table 3 Factors associated with high periprocedural risks for CEA
Carotid Angioplasty and Stenting Procedure
Procedural Preparation
Prior to the procedure, a baseline neurological examination should be performed and documented. Imaging of the target lesion with a catheter arteriogram as well as full diagnostic cerebral arteriogram should be done before the decision of treatment modality is made. Preprocedure antiplatelet therapy should be started three to five days prior the procedure with aspirin and clopidogrel. A typical regimen is aspirin 325 mg per day and clopidogrel 75 mg per day started 3 days prior to the procedure (Holmes 2006). Alternatively, a loading dose of 300–600 mg of clopidogrel can be substituted on the day of the procedure. Clopidogrel is administered for 6 weeks, while the patient should continue to take aspirin indefinitely, if possible, but at for at least 6 months. Also, a recent, European-based, randomized study demonstrated patients may benefit from loading with atorvastatin 80 mg at 12 h and 40 mg at 2 h prior to the start of the procedure (Patti et al. 2013). For patients who have suffered a previous allergic reaction to iodinated contrast, a pretreatment regimen of prednisone 50 mg every 6 h for three doses ending 1 h prior to the start of the procedure coupled with one dose of diphenhydramine 50 mg at 1 h prior should reduce the risk of significant allergic reactions (Greenberger et al. 1981).
Some patients are unresponsive to clopidogrel inhibition and at greater risk for suffering a periprocedural ischemic stroke, as the target moiety of platelets, P2Y12, has been shown to have a variable response to clopidogrel (Gurbel et al. 2009; Müller-Schunk et al. 2008). The real-time evaluation of platelet inhibition with the VerifyNow P2Y12 assay is a measure some interventionists use to guide therapy (Maruyama et al. 2011). However, no standard of care has been established regarding the medication regimen to be used in patients found to be unresponsive to standard clopidogrel inhibition. At our institution, we typically double the daily dose of clopidogrel to 150 mg in divided doses, while others have advocated the addition of cilostazol or ticlopidine to standard clopidogrel therapy (Maruyama et al. 2011).
Prior to starting the procedure, the patient should have two peripheral intravenous lines, a Foley catheter, and an arterial line for monitoring of periprocedural blood pressure. Arterial lines are useful in postprocedure care as well, as strict blood pressure is necessary acutely after the procedure to prevent a reperfusion syndrome. CAS can be performed under general anesthesia or awake, depending on premorbid factors and the operator’s preference. If the procedure is performed without endotracheal intubation, the patient must be able to remain arousable enough to follow commands.
Procedure Overview: Key Points and Intraprocedural Complication Avoidance
The techniques for CAS have evolved significantly since its first inception and, as with any procedure, there will be variable nuances between operators’ practice. Below, we outline the typical steps performed in CAS with a filter wire used as the EPD. We will briefly discuss the technicalities of CAS while using a flow-reversal EPD with proximal occlusion.
Typical access for CAS occurs through the femoral artery. In selected patients, brachial or radial artery access may be more beneficial (Taha et al. 2007; Tietke et al. 2008). Some authors have described a direct carotid puncture; however, this requires a high carotid bifurcation and has known significant risks including increased risk of ischemic complications and symptomatic access site hematomas (Matsumoto et al. 2004; Taha et al. 2007). Initially, a 5 French (Fr) introducer sheath should be placed femorally. Once access is obtained, the patient is given heparin 50–60 Un/Kg for a goal activated clotting time of approximately 250 s.
Next, diagnostic angiography of the diseased segment should be performed. With the diagnostic catheter in the CCA, a road map of the ICA and ECA should be performed. An exchange-length 0.035 in. wire is then advanced into a branch of the ECA. The diagnostic catheter is then exchanged for a 6 Fr Cook shuttle. At this point, control over the exchange wire is emphasized. While pulling the wire back into the carotid, bifurcation can cause devastating ischemic complications, and uncontrolled antegrade movement can perforate vessels of the ECA (Ecker et al. 2005). Alternatively, in patients that have undergone diagnostic angiography prior to the procedure, exchange and placement of the shuttle can occur in the descending aorta. Once placed in the descending aorta, the shuttle can be advanced into the CCA over a selector catheter.
Prior to advancing the EPD (such as the SpiderFX, FilterWire EZ, or the AngioGuard) past the lesion, an ideal view of the stenosis should be obtained. An adequate road map that demonstrates the largest opening around the stenosis will facilitate crossing with the microwire and EPD. The EPD catheter should be placed in a straight segment of the distal cervical ICA. The filter wire is then deployed. The filters are sized so they can approximate the lumen of the landing zone and circumferential opposition with the vessel can be obtained (Fig. 6). In some cases of severe stenosis, the lesion cannot be crossed without angioplasty.
Once the filter wire and EPD catheter are in place, a coaxial balloon, such as the Sterling Balloon Dilatation catheter (Boston Scientific, Natick, Massachusetts, United States), is advanced to the stenotic segment. The maximal diameter of the balloon should be approximately 1–2 mm smaller than the diameter of distal, nondiseased ICA. Balloon inflation should be performed with an insufflator to accurately measure the inflating pressure. Angioplasty is performed with smooth insufflation and deflation over the entire diseased segment. Arteriography is then performed to evaluate the treated stenosis and for any embolic material in the filter wire. With lesions at the carotid bifurcation, angioplasty can cause significant stimulation of the carotid body, which will rarely result in significant bradycardia. If this is encountered, the bradycardia is usually self-limited, but atropine and vasopressors should be readily available. Similarly, patients who were previously hypertensive may have a significant decline in blood pressure in the postoperative period. Rarely, do we require sympathomimetic medications to stabilize their blood pressure.
There are several carotid stents available, including balloon-expandable and nitinol self-expandable stents (Fig. 7). Few patients will suffer from an allergic reaction of the nickel of nitinol stents (Giménez-Arnau et al. 2000). The stent diameter should be sized according to the maximal diameter of the segment of the blood vessel the stent will cover. While a tapering, oversized stent may cover a longer portion of the blood vessel than initially anticipated, an undersized stent, “floating” in the blood vessel, has significant thrombogenicity and should be avoided.
Self-expandable stents. Note the open-cell design of the Protégé RX Carotid Stent System ((a) Courtesy of ev3, Plymouth, Minnesota, United States) and the closed-cell design of a partially deployed Carotid Wallstent Monorail Endoprosthesis ((b) Courtesy of Boston Scientific, Natick, Massachusetts, United States)
Once the stent is deployed, post-stenting angioplasty may be performed to improve wall apposition of the stent. This maneuver, however, should be done with caution and sparingly as it can induce emboli. At this point, the filter wire is partially captured into the microcatheter. Full retrieval of the filter wire into the catheter can embolize material that has been “caught” in the filter during the procedure.
When attempting to retrieve the filter wire past the newly placed stent, the EPD catheter or filter wire can become entangled with the stent, especially open-cell stents. If this occurs, care must be taken not to aggressively withdraw the microcatheter as this can dislodge the stent. Usually, the devices can be untethered with gentle advancement and withdrawal of the device. Rarely, dynamic maneuvers, such as having the patient turn his or her head, are needed to straighten the blood vessel and facilitate retrieval of the filter. If these measures fail, a smaller diagnostic catheter (4 to 5 Fr) can be used to pass over the microcatheter and recapture the filter. Once the catheter is retrieved, final cervical and cranial arteriography should be performed.
In rare occasions, an intraluminal thrombus or mobile segment of a ruptured plaque can complicate carotid stenosis. Although no randomized trials exist, initial treatment with systemic anticoagulation appears to be efficacious (Pelz et al. 1986; Vellimana et al. 2013) (Fig. 8). In patients with continued symptoms and failure of anticoagulation therapy, CAS may be indicated (Kwon et al. 2011). In these cases, proximal occlusion with flow reversal is often more ideal than distal embolic protection.
Intraluminal thrombus complicating carotid artery disease. A 48-year-old female presented with several days of headache. On nonenhanced head CT, (a) cortical subarachnoid hemorrhage was found (black arrow). An MR (b) image showed diffusion restriction in the same location (white arrowhead). Arteriograms of the left carotid cervical (c) and cranial (d) vasculature demonstrated an intraluminal thrombus (white arrow) and absence of arterial filling (white ellipsoid), respectively. The patient was successfully managed with anticoagulation therapy
As stated earlier, the MO.MA and Gore flow-reversal system are two FDA-approved devices. The MO.MA uses inflatable balloons in the CCA and ECA to prevent proximal and distal retrograde flow (Fig. 9). With the balloons properly insufflated, angioplasty and stenting may proceed. Once CAS is completed, the embolic and particulate material within the lumen is aspirated. The Gore flow-reversal system utilizes a two-balloon flow-arrest technique similar to the MO.MA, except that the arterial blood is shunted to the venous system with access to the femoral vein. These two systems have the benefit of not having to cross a lesion with an EPD prior to CAS. Also, in patients with tortuous carotid arteries, there is the proposed benefit of not having to place a filter wire in an unsuitable landing zone. Recent evidence suggests these systems have a high technical success rate and low complication rate (Ansel et al. 2010). Some patients, however, will not have sufficient collateral intracranial circulation to tolerate temporary balloon occlusion.
Neurological complications can occur at any time after access is obtained. Having patients awake while intermittently checking gross neurological functions can alert the team to a new neurological deficit. If a deficit is suspected, a more detailed neurological exam can localize the area of ischemia or hemorrhage. For patients that are obtunded or are otherwise unable to protect their airway, general endotracheal intubation should be performed. Once the patient is stable, a diagnostic cerebral arteriogram of the suspected vascular territory should be performed to evaluate for evidence of large vessel occlusion or stagnation of blood flow. If a large vessel occlusion is found, attempts to revascularize the vessel should be carried out without delay. If there is no appreciable difference noted on angiography from the patient’s baseline study, an immediate CT of the head should be performed. Protamine should be readily available and the anticoagulation reversed if a hemorrhage is found. Patients should be evaluated for craniotomy and surgical evacuation of the hematoma. For patients with relatively small intracranial hemorrhages, conservative therapy with blood pressure control, serial CT scans of the head, and frequent neurological assessments may suffice without surgery. In patients without evidence of hemorrhage on CT scan but stagnation of blood flow through distal cerebral arteries, such as in the cases of multiple small, distal emboli, the patient should be started on an intravenous glycoprotein IIb/IIIa inhibitor such as eptifibatide (Integrilin, Millennium Pharmaceuticals, Cambridge, Massachusetts, United States).
Once the procedure is completed, hemostasis of the access site should be obtained with a closure device such as the Angio-Seal Vascular Closure Device (St. Jude Medical, Minnetonka, Minnesota, United States), the StarClose SE Vascular Closure System (Abbott Vascular, Abbott Park, Illinois, United States), or the Mynx Closure Device (AccessClosure, Santa Clara, California, United States). Operators should be familiar with the use of several closure devices as each has its own indications based on size of access system and patient anatomy. If hemostasis is attempted, the sheath should be left until the activated clotting time is less than 150 s and the blood pressure is less than 160/90 mmHg.
Postprocedure Care
In the majority of cases, patients will not suffer an intraoperative complication but should be transferred to the intensive care unit or intermediate care unit for an overnight observation. Patients are hydrated overnight with intravenous fluids while undergoing frequent neurological, access site, and peripheral vascular assessments. A majority of neurological complications will occur in the angiography suite, but reperfusion hemorrhage and ischemic complications from a carotid dissection may manifest within the 24 h following the procedure (Meyers et al. 2000). Patients with bilateral high-grade carotid stenosis, who have poorly controlled blood pressure in the postprocedure setting, may have increased risk of a reperfusion hemorrhage (Abou-Chebl et al. 2004). Patients that suffer a neurological deterioration after the procedure should undergo an immediate CT scan of the head. If no hemorrhage is found, they should immediately be taken to the angiography suite for evaluation of patency of the stent, possible carotid dissection, or distal embolization.
Access-related complications comprise a significant source of complications for all endovascular procedures and should not be trivialized. Local hematomas, pseudoaneurysms, and arteriovenous fistulae should be investigated in patients with new swelling, lower extremity pain, decrease in peripheral pulses, or new bruit. In patients that suffer postprocedure hypotension and concerns for acute anemia of blood loss, a CT of the abdomen and pelvis should be obtained to investigate a potential retroperitoneal hematoma.
Potential systemic complications include MI, contrast-induced nephropathy, allergic complications of iodinated contrast, and seizures. All patients should undergo baseline electrolyte and glomerular filtration rate evaluation prior to and immediately after the procedure. Also, continuous pulse oximetry and cardiac monitoring should be utilized in all patients while in the immediate postprocedure phase.
Follow-Up and Long-Term Results
All patients who undergo CAS should have baseline carotid Doppler ultrasonography performed before discharge, again at 6 months, and then annually. Again, clopidogrel therapy should be continued for at least 6 weeks, and aspirin therapy should continue for at least 6 months. Patients should be seen by a neurologist or primary care physician to fully evaluate other potentially modifiable risk factors such as tobacco use, dyslipidemia, and diabetes.
The durability of CAS has been a concern since its inception. CAVATAS found a restenosis rate of 14 % at 1 year in patients treated with CAS, which was significantly worse than the 4 % found in patients treated with CEA (CAVATAS 2001). Similarly the 4-year outcomes of patients in CaRESS demonstrated a twofold increase in patients who underwent CAS (Zarins et al. 2009), although symptomatic restenosis did not seem to vary significantly. With improvements in techniques in CAS and closer attention to treatment of modifiable risks of stroke, the rate of restenosis of CAS may be improving. The largest randomized trial to date, CREST, did not find a high rate of restenosis in CAS at 2 years (6.0 %) or a significant difference when compared to CEA (6.3 %) (Lal et al. 2012). Some practitioners have found cilostazol to improve rates of restenosis in patients undergoing CAS, when compared to those undergoing CAS with clopidogrel therapy (Takayama et al. 2012). The rates of restenosis appear to be improving with experience, and the durability of CAS should not significantly impact the decision making when practitioners decide between surgical or endovascular therapies.
Illustrative Cases
Case 1 (Bilateral Carotid Stenosis )
A 68-year-old man with a remote history of left hemispheric ischemic stroke (Fig. 10a) was found to have severe bilateral carotid stenosis on CTA. His past medical history included hypertension, coronary artery disease, and diabetes. His examination was significant for mild right residual hemiplegia and mild aphasia. Diagnostic angiography confirmed the bilateral atherosclerotic lesions with his right ICA having 90 % stenosis and the left ICA demonstrating 95 % stenosis as calculated by the NASCET criteria (Fig. 10b, c). The patient was found to be at high risk for CEA, so endovascular treatment with CAS under monitored anesthesia was recommended.
Case 1. Prior to presentation, the patient had suffered an IS with MR imaging (a) showing diffusion restriction. A pretreatment arteriogram (b, c) demonstrated focal high-grade stenosis (95 %) at the level of the carotid bifurcation. With a 6F shuttle placed in the distal CCA (d), the EPD can be seen distal to the lesion. After initial angioplasty and stenting, residual stenosis and poor wall apposition can be visualized (e). A final arteriogram (f) after repeat angioplasty demonstrated successfully CAS
After positioning a 6 Fr shuttle in the distal CCA, a FilterWire EZ was deployed distal to the lesion (Fig. 10d). Pre-stenting angioplasty was performed with a 3.5 × 30 mm Sterling Balloon. An 8 × 21 mm Wallstent was positioned from the CCA to the proximal ICA covering the entire length of the lesion (Fig. 10e). A portion of the atheroma remained eccentric to the wall, preventing good wall apposition of the stent. Post-stenting angioplasty was performed with a 4.5 × 30 mm Sterling Balloon (Fig. 10f). The EPD was retrieved without difficulty, and final cervical and cranial angiograms were performed. Hemostasis was obtained with a Mynx Closure Device. The patient was transferred to the intensive care unit in stable condition. He was discharged the following morning at his baseline neurological condition.
Case 2 (Restenosis After CEA)
A 58-year-old man with a history of symptomatic carotid stenosis was treated with a left CEA 7 years prior to presentation. Routine Doppler ultrasonography demonstrated increased velocities of the previously treated ICA, concerning for restenosis. At presentation, the patient was found to be neurologically intact. Endovascular treatment with CAS was recommended. The initial arteriogram demonstrated a dissection with an intimal flap resulting in approximately 90 % stenosis of the proximal ICA and delayed filling of the distal ICA (Fig. 11a, e). After positioning a 6 Fr shuttle in the distal CCA, a 3 mm Spider FX filter wire was deployed distal to the lesion for protection (Fig. 11b). Next, with the aid of a 5 × 30 mm Sterling Balloon Dilatation catheter, angioplasty was performed (Fig. 11c). Then, a 6 × 22 mm Wallstent was advanced over the filter wire with the proximal portion in the CCA and the distal portion landing in the ICA beyond the flap (Fig. 11d).
Case 2. Delayed filling can be seen in the left carotid cervical (a) and cranial (e) arteriograms. The procedure was performed with a filter wire EPD (b). Post-angioplasty (c) and stenting (d) arteriograms demonstrate successful treatment of the restenosis after CEA (e). A final cranial arteriogram (f) demonstrates improved flow with the anterior cerebral artery (white arrowheads) and middle cerebral artery (white arrow) territories
While attempting to retrieve the filter wire, the EPD became entangled with the tines of the stent. After gentle manipulations of the wire failed, the patient was asked to turn his head to the contralateral side while an assistant applied gentle pressure to his neck in the area of interest under fluoroscopy. This maneuver released the entanglement, and the filter wire could be retrieved without further incident. Hemostasis was obtained with a StarClose closure device. The patient tolerated the procedure well and was transferred to the intensive care unit for overnight monitoring. He was discharged the following morning after baseline Doppler ultrasounds were performed.
Conclusions
The treatment of ECVD has significantly changed during the past three decades. During this time period, the indications for CEA became more clearly defined with a significant benefit found in multiple randomized trials. The endovascular treatment of carotid disease has similarly evolved over the last 15 years with further indications defined and techniques improved. The risks and benefits of both procedures are similar, but current data suggests that each procedure can be tailored to individual patients based on their specific indications and/or contraindications. Thus, the modalities should complement each other as potential options for patients found to have ECVD. For this reason, the endovascular modality is unlikely to supplant its surgical counterpart, although CAS has been found to be “not inferior” to CEA.
Endovascular technologies will continue to evolve at a rapid pace, allowing operators to have several options for devices such as EPDs, angioplasty balloons, and stents. While these advances will likely improve the technical success of CAS, further data regarding the long-term durability and the treatment’s role in asymptomatic ECVD, when compared to optimal medical management, will be welcomed. For a minority of patients, the role of CAS versus CEA remains unclear, but for most, we are moving toward an era where patient care will truly be individualized.
Cross-References
Abbreviations
- Antiplatelet drug:
-
A class of drugs used to decrease the affinity of platelets to aggregate. Multiple target moieties exist, such as the cyclooxygenase, adenosine diphosphate receptors, and glycoprotein IIB/IIIA receptors. Often used in the treatment of ischemic stroke and for periprocedural antiplatelet management during treatment of carotid stenosis.
- Carotid angioplasty and stenting:
-
Endovascular, catheter-based, treatment of carotid stenosis to prevent future ischemic strokes with balloon-angioplasty and delivery of an intraluminal stent.
- Carotid endarterectomy:
-
A surgical procedure used to correct carotid stenosis, to prevent future ischemic strokes by removing the material, most often atherosclerotic disease, within the internal or common carotid arteries.
- Carotid stenosis:
-
Narrowing, often atherosclerosis, within the extracranial internal or common carotid arteries, which is often associated with ischemic stroke and transient ischemic attack.
- Computed tomography angiography:
-
Noninvasive computed tomography-based evaluation of the intracranial and extracranial blood vessels with iodinated contrast.
- Diagnostic cerebral arteriography:
-
Invasive, catheter-based angiography of the to evaluate intracranial and extracranial cerebrovascular pathology. It is the “gold standard” measure of carotid stenosis.
- Doppler ultrasonography:
-
Using a probe extracutenously, subcutaneous tissues may be evaluated noninvasively with ultrasound. Can be used to evaluate extracranial carotid artery disease, specifically stenosis.
- Embolic protection devices:
-
Endovascular instruments used to prevent distal embolization during angioplasty and/or stenting. When used in carotid angioplasty and stenting, they are often distal, “filter-type” devices or proximal devices used to arrest or reverse flow during the procedure.
- Extracranial vascular disease:
-
Extracranial carotid artery and to a lesser extent extracranial vertebral artery disease predisposing patients to thromboembolic complications including transient ischemic attack and ischemic stroke.
- Ischemic stroke:
-
A permanent neurological deficit caused by inadequate perfusion of a region of brain, most often caused by a blocked blood vessel.
- Magnetic resonance angiography:
-
Noninvasive magnetic resonance-based evaluation of the intracranial and extracranial blood vessels. Extracranial evaluations are often aided with an intravenous gadolinium infusion.
- Randomized controlled trial:
-
The “gold standard” for clinical trials, whereby patients are randomized to one of two or more treatment arms and confounding variables are controlled for. Often used to test the efficacy or effectiveness of various types of medical treatments within a patient population.
- Transient ischemic attack:
-
Transient neurological dysfunction secondary to focal ischemia without permanent infarction.
- ACST-2:
-
Asymptomatic Carotid Surgery Trial-2
- ACT1:
-
Asymptomatic Carotid Stenosis Stenting versus Endarterectomy Trial
- AHA:
-
American Heart Association
- ASA:
-
American Stroke Association
- CaRESS:
-
Carotid Revascularization Using Endarterectomy or Stenting Systems trial
- CAS:
-
Carotid angioplasty and stenting
- CAVATAS:
-
Carotid and Vertebral Artery Transluminal Angioplasty Study
- CCA:
-
Common carotid artery
- CEA:
-
Carotid endarterectomy
- CEBM:
-
University of Oxford’s Center for Evidence-Based Medicine
- CREST:
-
Carotid Revascularization Endarterectomy versus Stenting Trial
- CTA:
-
Computed tomography angiography
- ECA:
-
External carotid artery
- ECST:
-
European Carotid Surgery Trial
- ECVD:
-
Extracranial vascular disease
- EPD:
-
Embolic protection device
- EVA-3S:
-
Endarterectomy versus Angioplasty in Patients with Symptomatic Severe Carotid Stenosis
- ICA:
-
Internal carotid artery
- IS:
-
Ischemic stroke
- MI:
-
Myocardial infarction
- MRA:
-
Magnetic resonance angiography
- NASCET:
-
The North American Symptomatic Carotid Endarterectomy Trial
- NIH:
-
National Institute of Health
- RR:
-
Relative risk
- SAPPHIRE:
-
The Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy trial
- SPACE:
-
Stent-Supported Percutaneous Angioplasty of the Carotid artery versus Endarterectomy
- TACIT:
-
Transatlantic Asymptomatic Carotid Interventional Trial
- TIA:
-
Transient ischemic attack
- VA:
-
Veterans Affairs
References
(1986) Role of carotid endarterectomy in asymptomatic carotid stenosis. A Veterans Administration Cooperative Study. Stroke J Cereb Circ 17:534–539
(1991a) Clinical alert: benefit of carotid endarterectomy for patients with high-grade stenosis of the internal carotid artery. National Institute of Neurological Disorders and Stroke, Stroke and Trauma Division. North American Symptomatic Carotid Endarterectomy Trial (NASCET) investigators. Stroke J Cereb Circ 22:816–817
(1991b) MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70–99 %) or with mild (0–29 %) carotid stenosis. European Carotid Surgery Trialists’ Collaborative Group. Lancet 337:1235–1243
(1991c) Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 325:445–453. doi: 10.1056/NEJM199108153250701
(1998) Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 351:1379–1387
(2001) Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): a randomised trial. Lancet 357:1729–1737
(2009) Prevalence and most common causes of disability among adults--United States, 2005. Mmwr Morb Mortal Wkly Rep 58:421–426
Abbott AL (2009) Medical (nonsurgical) intervention alone is now best for prevention of stroke associated with asymptomatic severe carotid stenosis: results of a systematic review and analysis. Stroke J Cereb Circ 40:e573–e583. doi:10.1161/STROKEAHA.109.556068
Abbott AL (2010) Current medical intervention alone is now the best solution for asymptomatic carotid stenosis. Letter to the editors of Journal of Vascular Surgery and the European Journal of Vascular and Endovascular Surgery regarding trans-atlantic debate no. 1. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg 40:678–679; author reply 679. doi: 10.1016/j.ejvs.2010.07.026
Abou-Chebl A, Yadav JS, Reginelli JP et al (2004) Intracranial hemorrhage and hyperperfusion syndrome following carotid artery stenting: risk factors, prevention, and treatment. J Am Coll Cardiol 43:1596–1601. doi:10.1016/j.jacc.2003.12.039
Adami CA, Scuro A, Spinamano L et al (2002) Use of the Parodi anti-embolism system in carotid stenting: Italian trial results. J Endovasc Ther Off J Int Soc Endovasc Spec 9:147–154. doi: 10.1583/1545-1550(2002)009<0147:UOTPAE>2.0.CO;2
Alberts MJ (2001) Results of a multicenter prospective randomized trial of carotid artery stenting vs. carotid endarterectomy. The publications committee of WALLSTENT (abstract). Stroke 32:325
Al-Mubarak N, Roubin GS, Vitek JJ, Iyer SS (2002) Microembolization during carotid stenting with the distal-balloon antiemboli system. Int Angiol J Int Union Angiol 21:344–348
Andziak P (2006) Commentary to the articles: SPACE Collaborative Group. 30 day results from the SPACE trial of stent-protected angioplasty versus carotid endarterectomy in symptomatic patients: a randomised non-inferiority trial. Lancet 368:1239–1247
Ansel GM, Hopkins LN, Jaff MR et al (2010) Safety and effectiveness of the INVATEC MO.MA proximal cerebral protection device during carotid artery stenting: results from the ARMOUR pivotal trial. Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv 76:1–8. doi:10.1002/ccd.22439
Barnett HJ, Taylor DW, Eliasziw M et al (1998) Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 339:1415–1425. doi:10.1056/NEJM199811123392002
Biasi GM, Froio A, Diethrich EB et al (2004) Carotid plaque echolucency increases the risk of stroke in carotid stenting: the Imaging in Carotid Angioplasty and Risk of Stroke (ICAROS) study. Circulation 110:756–762. doi:10.1161/01.CIR.0000138103.91187.E3
Brott TG, Hobson RW 2nd, Howard G et al (2010) Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 363:11–23. doi:10.1056/NEJMoa0912321
Brott TG, Halperin JL, Abbara S et al (2011) 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. Circulation 124:489–532. doi:10.1161/CIR.0b013e31820d8d78
CARESS Steering Committee (2003) Carotid revascularization using endarterectomy or stenting systems (CARESS): phase I clinical trial. J Endovasc Ther Off J Int Soc Endovasc Spec 10:1021–1030. doi: 10.1583/1545-1550(2003)010<1021:CRUEOS>2.0.CO;2
Carotid Stenting Trialists’ Collaboration, Bonati LH, Dobson J et al (2010) Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: a preplanned meta-analysis of individual patient data. Lancet 376:1062–1073. doi:10.1016/S0140-6736(10)61009-4
Clair DG, Hopkins LN, Mehta M et al (2011) Neuroprotection during carotid artery stenting using the GORE flow reversal system: 30-day outcomes in the EMPiRE Clinical Study. Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv 77:420–429. doi:10.1002/ccd.22789
Cremonesi A, Manetti R, Setacci F et al (2003) Protected carotid stenting: clinical advantages and complications of embolic protection devices in 442 consecutive patients. Stroke J Cereb Circ 34:1936–1941. doi:10.1161/01.STR.0000081000.23561.61
DeBakey ME (1975) Successful carotid endarterectomy for cerebrovascular insufficiency. Nineteen-year follow-up. JAMA J Am Med Assoc 233:1083–1085
DeBakey ME (1996) Carotid endarterectomy revisited. J Endovasc Surg Off J Int Soc Endovasc Surg 3:4. doi: 10.1583/1074-6218(1996)003<0004:CER>2.0.CO;2
Doby T (1992) Cerebral angiography and Egas Moniz. AJR Am J Roentgenol 159:364. doi:10.2214/ajr.159.2.1632357
Eastcott HH, Pickering GW, Rob CG (1954) Reconstruction of internal carotid artery in a patient with intermittent attacks of hemiplegia. Lancet 267:994–996
Ecker RD, Guidot CA, Hanel RA et al (2005) Perforation of external carotid artery branch arteries during endoluminal carotid revascularization procedures: consequences and management. J Invasive Cardiol 17:292–295
Faggioli G, Ferri M, Gargiulo M et al (2007) Measurement and impact of proximal and distal tortuosity in carotid stenting procedures. J Vasc Surg 46:1119–1124. doi:10.1016/j.jvs.2007.08.027
Ferguson GG, Eliasziw M, Barr HW et al (1999) The North American Symptomatic Carotid Endarterectomy Trial: surgical results in 1415 patients. Stroke J Cereb Circ 30:1751–1758
Findlay JM, Nykolyn L, Lubkey TB et al (2002) Auditing carotid endarterectomy: a regional experience. Can J Neurol Sci J Can Sci Neurol 29:326–332
Fisher M (1951) Occlusion of the internal carotid artery. Ama Arch Neurol Psychiatry 65:346–377
Furie KL, Kasner SE, Adams RJ et al (2011) Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke J Cereb Circ 42:227–276. doi:10.1161/STR.0b013e3181f7d043
Gaines PA, Randall MS (2005) Carotid artery stenting for patients with asymptomatic carotid disease (and news on TACIT). Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg 30:461–463. doi:10.1016/j.ejvs.2005.07.002
Giménez-Arnau A, Riambau V, Serra-Baldrich E, Camarasa JG (2000) Metal-induced generalized pruriginous dermatitis and endovascular surgery. Contact Dermatitis 43:35–40
Goldstein LB, McCrory DC, Landsman PB et al (1994) Multicenter review of preoperative risk factors for carotid endarterectomy in patients with ipsilateral symptoms. Stroke J Cereb Circ 25:1116–1121
Goldstein LB, Samsa GP, Matchar DB, Oddone EZ (1998) Multicenter review of preoperative risk factors for endarterectomy for asymptomatic carotid artery stenosis. Stroke J Cereb Circ 29:750–753
Goldstein LB, Bushnell CD, Adams RJ et al (2011) Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke J Cereb Circ 42:517–584. doi:10.1161/STR.0b013e3181fcb238
Greenberger PA, Patterson R, Simon R et al (1981) Pretreatment of high-risk patients requiring radiographic contrast media studies. J Allergy Clin Immunol 67:185–187
Gross CP, Steiner CA, Bass EB, Powe NR (2000) Relation between prepublication release of clinical trial results and the practice of carotid endarterectomy. JAMA J Am Med Assoc 284:2886–2893
Gurbel PA, Antonino MJ, Tantry US (2009) Recent developments in clopidogrel pharmacology and their relation to clinical outcomes. Expert Opin Drug Metab Toxicol 5:989–1004. doi:10.1517/17425250903107772
Gurm HS, Yadav JS, Fayad P et al (2008) Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med 358:1572–1579. doi:10.1056/NEJMoa0708028
Halm EA, Chassin MR, Tuhrim S et al (2003) Revisiting the appropriateness of carotid endarterectomy. Stroke J Cereb Circ 34:1464–1471. doi:10.1161/01.STR.0000072514.79745.7D
Hobson RW 2nd, Weiss DG, Fields WS et al (1993) Efficacy of carotid endarterectomy for asymptomatic carotid stenosis. The Veterans Affairs Cooperative Study Group. N Engl J Med 328:221–227. doi:10.1056/NEJM199301283280401
Hobson RW 2nd, Howard VJ, Roubin GS et al (2004) Credentialing of surgeons as interventionalists for carotid artery stenting: experience from the lead-in phase of CREST. J Vasc Surg 40:952–957. doi:10.1016/j.jvs.2004.08.039
Holmes DR Jr (2006) Antiplatelet therapy after percutaneous coronary intervention. Cerebrovasc Dis Basel Switz 21(Suppl 1):25–34. doi:10.1159/000090359
Hopkins LN, Roubin GS, Chakhtoura EY et al (2010) The Carotid Revascularization Endarterectomy versus Stenting Trial: credentialing of interventionalists and final results of lead-in phase. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc 19:153–162. doi:10.1016/j.jstrokecerebrovasdis.2010.01.001
International Carotid Stenting Study Investigators, Ederle J, Dobson J et al (2010) Carotid artery stenting compared with endarterectomy in patients with symptomatic carotid stenosis (International Carotid Stenting Study): an interim analysis of a randomised controlled trial. Lancet 375:985–997. doi:10.1016/S0140-6736(10)60239-5
Jaeger HJ, Mathias KD, Hauth E et al (2002) Cerebral ischemia detected with diffusion-weighted MR imaging after stent implantation in the carotid artery. Ajnr Am J Neuroradiol 23:200–207
Kachel R, Basche S, Heerklotz I et al (1991) Percutaneous transluminal angioplasty (PTA) of supra-aortic arteries especially the internal carotid artery. Neuroradiology 33:191–194
Kastrup A, Gröschel K, Schnaudigel S et al (2008) Target lesion ulceration and arch calcification are associated with increased incidence of carotid stenting-associated ischemic lesions in octogenarians. J Vasc Surg 47:88–95. doi:10.1016/j.jvs.2007.09.045
Kawarada O, Yokoi Y, Takemoto K, Morioka N (2007) Double-wire technique in balloon-protected carotid artery stenting. J Intervent Cardiol 20:55–62. doi:10.1111/j.1540-8183.2007.00218.x
Kerber CW, Cromwell LD, Loehden OL (1980) Catheter dilatation of proximal carotid stenosis during distal bifurcation endarterectomy. Ajnr Am J Neuroradiol 1:348–349
Kwon TH, Kim BM, Nam HS et al (2011) Carotid stenting in acute ischemic stroke patients with intraluminal thrombus. Neuroradiology 53:773–778. doi:10.1007/s00234-010-0788-0
Lal BK, Beach KW, Roubin GS et al (2012) Restenosis after carotid artery stenting and endarterectomy: a secondary analysis of CREST, a randomised controlled trial. Lancet Neurol 11:755–763. doi:10.1016/S1474-4422(12)70159-X
Lam RC (2009) Contemporary review of embolic distal protection strategies in carotid artery stenting. J Invasive Cardiol 21:413–414
Liapis CD, Bell PRF, Mikhailidis D et al (2009) ESVS guidelines. Invasive treatment for carotid stenosis: indications, techniques. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg 37:1–19. doi:10.1016/j.ejvs.2008.11.006
Maldonado TS, Loh S, Fonseco R et al (2008) Incidence and outcome of filter occlusion during carotid artery stent procedure. Ann Vasc Surg 22:756–761. doi:10.1016/j.avsg.2008.08.004
Maruyama H, Takeda H, Dembo T et al (2011) Clopidogrel resistance and the effect of combination cilostazol in patients with ischemic stroke or carotid artery stenting using the verify now P2Y12 assay. Intern Med Tokyo Jpn 50:695–698
Mas J-L, Trinquart L, Leys D et al (2008) Endarterectomy Versus Angioplasty in patients with symptomatic severe carotid stenosis (EVA-3S) trial: results up to 4 years from a randomised, multicentre trial. Lancet Neurol 7:885–892. doi:10.1016/S1474-4422(08)70195-9
Mathias K (1977) A new catheter system for percutaneous transluminal angioplasty (PTA) of carotid artery stenoses. Fortschr Med 95:1007–1011
Mathias K, Gissler HM (2002) Carotis artery disease: percutaneous approach. In: Lanzer P, Topol EJ (eds) Panvascular medicine integrated clinical management. Springer, Berlin\Heidelberg\New York, pp 1302–1316
Mathias K, Bockenheimer S, von Reutern G et al (1983) Catheter dilatation of arteries supplying the brain. Radiologe 23:208–214
Matsumoto H, Fujita K, Miki J et al (2004) Direct carotid approach for carotid angioplasty and stenting with a small incision: a technical case report. No Shinkei Geka 32:735–740
Mayberg MR, Wilson SE, Yatsu F et al (1991) Carotid endarterectomy and prevention of cerebral ischemia in symptomatic carotid stenosis. Veterans Affairs Cooperative Studies Program 309 Trialist Group. JAMA J Am Med Assoc 266:3289–3294
Meyers PM, Higashida RT, Phatouros CC et al (2000) Cerebral hyperperfusion syndrome after percutaneous transluminal stenting of the craniocervical arteries. Neurosurgery 47:335–343, discussion 343–345
Müller-Schunk S, Linn J, Peters N et al (2008) Monitoring of clopidogrel-related platelet inhibition: correlation of nonresponse with clinical outcome in supra-aortic stenting. Ajnr Am J Neuroradiol 29:786–791. doi:10.3174/ajnr.A0917
Naggara O, Touzé E, Beyssen B et al (2011) Anatomical and technical factors associated with stroke or death during carotid angioplasty and stenting: results from the endarterectomy versus angioplasty in patients with symptomatic severe carotid stenosis (EVA-3S) trial and systematic review. Stroke J Cereb Circ 42:380–388. doi:10.1161/STROKEAHA.110.588772
Naylor AR, Bolia A, Abbott RJ et al (1998) Randomized study of carotid angioplasty and stenting versus carotid endarterectomy: a stopped trial. J Vasc Surg 28:326–334
Patti G, Tomai F, Melfi R et al (2013) Strategies of clopidogrel load and atorvastatin reload to prevent ischemic cerebral events in patients undergoing protected carotid stenting. Results of the randomized ARMYDA-9 CAROTID (Clopidogrel and Atorvastatin Treatment During Carotid Artery Stenting) study. J Am Coll Cardiol 61:1379–1387. doi:10.1016/j.jacc.2013.01.015
Pelz DM, Buchan A, Fox AJ et al (1986) Intraluminal thrombus of the internal carotid arteries: angiographic demonstration of resolution with anticoagulant therapy alone. Radiology 160:369–373
Powell RJ, Alessi C, Nolan B et al (2006) Comparison of embolization protection device-specific technical difficulties during carotid artery stenting. J Vasc Surg 44:56–61. doi:10.1016/j.jvs.2006.03.035
Rabe K, Sugita J, Gödel H, Sievert H (2006) Flow-reversal device for cerebral protection during carotid artery stenting–acute and long-term results. J Intervent Cardiol 19:55–62. doi:10.1111/j.1540-8183.2006.00105.x
Rob C (1978) Occlusive disease of the extracranial cerebral arteries. A review of the past 25 years. J Cardiovasc Surg (Torino) 19:487–498
Rothwell PM, Slattery J, Warlow CP (1996) A systematic review of the risks of stroke and death due to endarterectomy for symptomatic carotid stenosis. Stroke J Cereb Circ 27:260–265
Rothwell PM, Slattery J, Warlow CP (1997) Clinical and angiographic predictors of stroke and death from carotid endarterectomy: systematic review. BMJ 315:1571–1577
Rudarakanchana N, Dialynas M, Halliday A (2009) Asymptomatic Carotid Surgery Trial-2 (ACST-2): rationale for a randomised clinical trial comparing carotid endarterectomy with carotid artery stenting in patients with asymptomatic carotid artery stenosis. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg 38:239–242. doi:10.1016/j.ejvs.2009.05.010
Schneider PA, Naylor AR (2010) Transatlantic debate. Asymptomatic carotid artery stenosis–medical therapy alone versus medical therapy plus carotid endarterectomy or stenting. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg 40:274–281. doi:10.1016/j.ejvs.2010.05.004
SPACE Collaborative Group, Ringleb PA, Allenberg J et al (2006) 30 day results from the SPACE trial of stent-protected angioplasty versus carotid endarterectomy in symptomatic patients: a randomised non-inferiority trial. Lancet 368:1239–1247. doi:10.1016/S0140-6736(06)69122-8
Taha MM, Sakaida H, Asakura F et al (2007) Access site complications with carotid angioplasty and stenting. Surg Neurol 68:431–437. doi:10.1016/j.surneu.2006.11.036
Takayama K, Taoka T, Nakagawa H et al (2012) Effect of cilostazol in preventing restenosis after carotid artery stenting using the carotid wallstent: a multicenter retrospective study. Ajnr Am J Neuroradiol 33:2167–2170. doi:10.3174/ajnr.A3127
Theron JG, Payelle GG, Coskun O et al (1996) Carotid artery stenosis: treatment with protected balloon angioplasty and stent placement. Radiology 201:627–636
Tietke MW, Ulmer S, Riedel C, Jansen O (2008) Carotid artery stenting via transbrachial approach. Röfo Fortschritte Auf Dem Geb Röntgenstrahlen Nukl 180:988–993. doi:10.1055/s-2008-1027707
Tübler T, Schlüter M, Dirsch O et al (2001) Balloon-protected carotid artery stenting: relationship of periprocedural neurological complications with the size of particulate debris. Circulation 104:2791–2796
Vellimana AK, Kadkhodayan Y, Rich KM et al (2013) Symptomatic patients with intraluminal carotid artery thrombus: outcome with a strategy of initial anticoagulation. J Neurosurg 118:34–41. doi:10.3171/2012.9.JNS12406
Vilain KR, Magnuson EA, Li H et al (2012) Costs and cost-effectiveness of carotid stenting versus endarterectomy for patients at standard surgical risk: results from the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST). Stroke J Cereb Circ 43:2408–2416. doi:10.1161/STROKEAHA.112.661355
Voeks JH, Howard G, Roubin GS et al (2011) Age and outcomes after carotid stenting and endarterectomy: the carotid revascularization endarterectomy versus stenting trial. Stroke J Cereb Circ 42:3484–3490. doi:10.1161/STROKEAHA.111.624155
Walker MD, Marler JR, Goldstein M et al (1995) Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Jama J Am Med Assoc 273:1421–1428
Wennberg DE, Lucas FL, Birkmeyer JD et al (1998) Variation in carotid endarterectomy mortality in the Medicare population: trial hospitals, volume, and patient characteristics. JAMA J Am Med Assoc 279:1278–1281
Wholey MH, Wholey M, Bergeron P et al (1998) Current global status of carotid artery stent placement. Cathet Cardiovasc Diagn 44:1–6
Winslow CM, Solomon DH, Chassin MR et al (1988) The appropriateness of carotid endarterectomy. N Engl J Med 318:721–727. doi:10.1056/NEJM198803243181201
Wolf PA, Clagett GP, Easton JD et al (1999) Preventing ischemic stroke in patients with prior stroke and transient ischemic attack : a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke J Cereb Circ 30:1991–1994
Yadav JS, Wholey MH, Kuntz RE et al (2004) Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 351:1493–1501. doi:10.1056/NEJMoa040127
Zarins CK, White RA, Diethrich EB et al (2009) Carotid revascularization using endarterectomy or stenting systems (CaRESS): 4-year outcomes. J Endovasc Ther Off J Int Soc Endovasc Spec 16:397–409. doi:10.1583/08-2685.1
Zhou W, Zareie R, Tedesco M et al (2011) Risk factors predictive of carotid artery stenting-associated subclinical microemboli. Int J Angiol Off Publ Int Coll Angiol Inc 20:25–32. doi:10.1055/s-0031-1272546
Further Reading
Mas JL, Chatellier G, Beyssen B, EVA-3S Investigators, et al (2006) Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med 355:1660–1671. Kardiol Pol 64:1458–1460; discussion 1460–1461
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this entry
Cite this entry
Ikeda, D.S., Shaw, A., Sauvageau, E., Powers, C.J. (2015). Endovascular Management of Extracranial Carotid Disease . In: Lanzer, P. (eds) PanVascular Medicine. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-37078-6_93
Download citation
DOI: https://doi.org/10.1007/978-3-642-37078-6_93
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-37077-9
Online ISBN: 978-3-642-37078-6
eBook Packages: MedicineReference Module Medicine