Abstract
The disease process of atraumatic osteonecrosis was first described as ischemic necrosis of the hip [1]. This pathological process can lead to destructive arthritis in multiple joints, most commonly occurring in the hips, knees, shoulders, and ankles [1]. Currently, there is no consensus on the pathophysiological mechanism of osteonecrosis, but it is thought to be multifactorial in nature. However, there are certain direct risk factors implicated in the development of osteonecrosis such as trauma, radiation, Caisson’s disease, and sickle cell disease [2]. In addition, various other risk factors have been shown to have a direct correlation with osteonecrosis such as corticosteroids, habitual alcohol intake, hyperlipidemia, chemotherapeutic agents, systemic lupus erythematosus, lipid storage diseases, and inflammatory bowel disease [3, 4].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Systemic Lupus Erythematosus
- Systemic Lupus Erythematosus Patient
- Sickle Cell Disease
- Pulse Therapy
- Severe Acute Respiratory Syndrome
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The disease process of atraumatic osteonecrosis was first described as ischemic necrosis of the hip [1]. This pathological process can lead to destructive arthritis in multiple joints, most commonly occurring in the hips, knees, shoulders, and ankles [1]. Currently, there is no consensus on the pathophysiological mechanism of osteonecrosis, but it is thought to be multifactorial in nature. However, there are certain direct risk factors implicated in the development of osteonecrosis such as trauma, radiation, Caisson’s disease, and sickle cell disease [2]. In addition, various other risk factors have been shown to have a direct correlation with osteonecrosis such as corticosteroids, habitual alcohol intake, hyperlipidemia, chemotherapeutic agents, systemic lupus erythematosus, lipid storage diseases, and inflammatory bowel disease [3, 4].
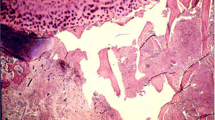
In 1958, Chandler and Wright described the adverse effects of high-dose intra-articular corticosteroid injection [5]. Later in 1960, Heimann and Freiberger noticed similar results seen with high-dose oral corticosteroids on the femoral and humeral head [6]. Although there are several theories behind corticosteroid-induced osteonecrosis, it is generally thought to be caused by vascular compromise to the femoral head. The most widely accepted mechanism of corticosteroid-induced osteonecrosis results from adipocyte hypertrophy which increases intraosseous pressure causing extramural compression of the vasculature to the femoral head [7]. This leads to a disruption in blood flow, which causes a lack of delivered vital nutrients. In addition, corticosteroids have been found to cause a decrease in osteoclast and osteoblast activity, which subsequently results in decreased bony turnover, trabecular width, density, and formation [8].
Recently, numerous studies have shown there to be a direct correlation between the use of high-dose corticosteroids and the increased risk of osteonecrosis. It is widely accepted that doses greater than 2 g over a 3-month interval impart the greatest risk for the development of corticosteroid-induced osteonecrosis [2]. This chapter therefore aims to evaluate the effects of corticosteroids on the incidence of osteonecrosis of the hip , particularly in relation to dosing, and duration of treatment, and the effects of pulse therapy.
2 Treatment Dosing
Current studies demonstrate that there is a direct correlation between the incidence of osteonecrosis and the use of corticosteroids. A recent study by Felson et al. demonstrated that the incidence of corticosteroid-induced osteonecrosis may be increasing due to higher dosing regimens. The authors found there to be a 4.6 % increase in incidence of osteonecrosis with every 10 mg/day increase in corticosteroid use. Additionally, it was seen that the daily dose of corticosteroid may be one of the greatest risk factors for osteonecrosis (R 2 = 0.75) [9]. Similarly, the incidence of osteonecrosis has been reported to be higher with a mean daily dose of > 40 mg/day. Shigemura et al. in a prospective randomized study found a fourfold increase in the risk of osteonecrosis with the use >40 mg/day of corticosteroids (OR = 4.2; p = 0.001). This study showed that an increase in the mean daily dose may result in an increased incidence of osteonecrosis [10].
In a prospective study of 45 patients diagnosed with systemic lupus erythematosus (SLE), Nagasawa et al. examined the dose–response relationship with development of osteonecrosis over a 5-year period. During this period patients had magnetic resonance imaging (MRI) evaluations every year following initiation of 40 mg/day of corticosteroid therapy. The authors demonstrated that the cohort who developed osteonecrosis had a significantly higher proportion of patients who received >1,000 mg/day of corticosteroids than that group of patients who demonstrated no radiographic evidence of the disease (87 % versus 37 %; p < 0.01) [11].
Studies have also demonstrated that patients receiving a cumulative dose of corticosteroids >2 g are at a higher risk for developing osteonecrosis. A retrospective study by Nakamura et al., who examined 201 SLE patients over a 13-year period, demonstrated that 15 % of patients who received high corticosteroid doses had increased risks of developing osteonecrosis [4].
The cumulative corticosteroid dosage has been shown to have a direct association with the risk of osteonecrosis. In particular, a study by Shjibatani et al. found that patients who have had renal transplantation are at a potentially higher risk of developing osteonecrosis. The authors found that patients who received ≤1,795 mg and >1,795 mg of cumulative steroid dosing over an 8-week period after renal transplantation had higher risks of developing osteonecrosis compared to those who received less than 1,400 mg of corticosteroids (hazards ratio, 2.9 and 3.2, respectively; p = 0.07 and 0.07, respectively) [12].
Despite the positive correlation seen in the previous studies, a prospective study by Ono et al. showed that there may be no correlation between corticosteroid use and development of osteonecrosis. This study consisted of 62 patients with SLE who were treated with 30 mg/day of corticosteroids for at least 30 days. The authors found no significant correlation between the mean dose, the total cumulative usage, and the duration of high-dose corticosteroids and the subsequent risk of developing osteonecrosis [13]. It is possible that limiting corticosteroid use to the lowest dose possible that is medically effective may minimize the risk of osteonecrosis.
3 Treatment Duration
Another independent risk factor associated with an increased risk of osteonecrosis is the duration of corticosteroid treatment. A study by Nakamura et al. observed the risk of osteonecrosis in relation to the dose and duration in 201 SLE (537 joints) patients over a 13-year period [4]. This study demonstrated a direct association between osteonecrosis risk and longer duration of corticosteroid use, as well as with increased doses required for patients who had recurrent episodes. The authors found that 238 out of the 537 joints developed osteonecrosis at an average of 26 years of age. Additionally, a study by Li et al. evaluated the correlation between osteonecrosis and corticosteroid in 539 patients with severe acute respiratory syndrome. In relation to duration of treatment, the authors found that patients who developed osteonecrosis received corticosteroids for a significantly longer duration when compared to patients who did not develop the disease (38 ± 17 versus 27 ± 15 days; p < 0.01) [14].
However, no studies were found refuting that increased duration of treatment increased the risk of osteonecrosis. It is postulated that this could have been a compounding variable with higher dosages as well. Therefore, it may be important to minimize treatment to the shortest duration feasible.
4 Pulsed Therapy
Pulsed therapy refers to the intermittent administration of corticosteroids at suprapharmacologic dosages intravenously [15]. A study by Ce et al. compared 60 patients who had multiple sclerosis and were treated with corticosteroids to a group who had multiple sclerosis but did not receive corticosteroid treatment. The authors found from MRI evaluation that patients had a significantly higher risk for developing osteonecrosis with treatment of >10 g of cumulative pulsed corticosteroid dose, compared to the matched group (15.5 % versus 0 %; p = 0.043) [16]. However, it is uncertain whether the positive correlation seen in this study is from the treatment with pulsed corticosteroids or the higher cumulative dose. Similarly, a study by Lausten et al. of 374 renal transplant patients found that patients who were treated with pulsed corticosteroid therapy (n = 34) had a significantly higher rate of osteonecrosis when compared to treatment without pulsed therapy (n = 22; p < 0.05) [17].
However, a study by Oinuma et al. of 72 patients with SLE showed that there was no significant difference in the incidence of osteonecrosis with the use of pulsed therapy. The authors found that 45 % (18 of 40) of patients who had osteonecrosis received pulsed corticosteroid therapy when compared to 53 % (17 of 32) of patients without osteonecrosis who received pulsed therapy. However, this study failed to mention the dosage of pulsed corticosteroid therapy [18].
The current use of pulsed therapy has shown to have conflicting results in association with the development of osteonecrosis. Due to a lack of concordance between studies, larger prospective randomized studies are needed to determine a cause-effect relationship between pulsed therapy and osteonecrosis.
5 Conclusion
Treatment with corticosteroids may have up to a tenfold increase in the risk of developing osteonecrosis. Additionally, patients receiving higher mean doses have been shown to be at an even higher increased risk of osteonecrosis. However, it is uncertain whether corticosteroid duration and cumulative dose have an effect on the incidence of osteonecrosis. It is believed that it may be a compounding factor along with the underlying disease. Furthermore, the reported studies demonstrate the pulsed corticosteroids may also increase the risk of osteonecrosis. Based on the current literature, it is believed that minimizing the dosage and duration of corticosteroid treatment may potentially minimize the risk of developing osteonecrosis. Due to paucity of reports, we believe that larger prospective studies are needed to assess the effects of corticosteroids on the incidence of osteonecrosis. Furthermore, molecular studies may be important in elucidating the pathogenetic mechanism of corticosteroids and osteonecrosis.
References
Johnson AJ, Mont MA, Tsao AK, Jones LC. Treatment of femoral head osteonecrosis in the united states: 16-year analysis of the nationwide inpatient sample. Clin Orthop Relat Res. 2013. doi:10.1007/s11999-013-3220-3.
Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88(5):1117–32. doi:10.2106/JBJS.E.01041. 88/5/1117 [pii].
Seguin C, Kassis J, Busque L, Bestawros A, Theodoropoulos J, Alonso ML, Harvey EJ. Non-traumatic necrosis of bone (osteonecrosis) is associated with endothelial cell activation but not thrombophilia. Rheumatology (Oxford). 2008;47(8):1151–5. doi:10.1093/rheumatology/ken206.
Nakamura J, Harada Y, Oinuma K, Iida S, Kishida S, Takahashi K. Spontaneous repair of asymptomatic osteonecrosis associated with corticosteroid therapy in systemic lupus erythematosus: 10-year minimum follow-up with mri. Lupus. 2010;19(11):1307–14. doi:10.1177/0961203310372951. 0961203310372951 [pii].
Chandler GN, Wright V. Deleterious effect of intra-articular hydrocortisone. Lancet. 1958;2(7048):661–3.
Heimann WG, Freiberger RH. Avascular necrosis of the femoral and humeral heads after high-dosage corticosteroid therapy. New Engl J Med. 1960;263:672–5. doi:10.1056/NEJM196010062631404.
Sheng H, Sheng CJ, Cheng XY, Zhang G, Lee KM, Leung KS, Qu S, Qin L. Pathomorphological changes of bone marrow adipocytes in process of steroid-associated osteonecrosis. Int J Clin Exp Pathol. 2013;6(6):1046–50.
Powell C, Chang C, Gershwin ME. Current concepts on the pathogenesis and natural history of steroid-induced osteonecrosis. Clin Rev Allergy Immunol. 2011;41(1):102–13. doi:10.1007/s12016-010-8217-z.
Felson DT, Anderson JJ. Across-study evaluation of association between steroid dose and bolus steroids and avascular necrosis of bone. Lancet. 1987;1(8538):902–6.
Shigemura T, Nakamura J, Kishida S, Harada Y, Ohtori S, Kamikawa K, Ochiai N, Takahashi K. Incidence of osteonecrosis associated with corticosteroid therapy among different underlying diseases: prospective mri study. Rheumatology (Oxford). 2011;50(11):2023–8. doi:10.1093/rheumatology/ker277.
Nagasawa K, Tada Y, Koarada S, Horiuchi T, Tsukamoto H, Murai K, Ueda A, Yoshizawa S, Ohta A. Very early development of steroid-associated osteonecrosis of femoral head in systemic lupus erythematosus: prospective study by MRI. Lupus. 2005;14(5):385–90. doi:10.1191/0961203305lu2103oa.
Shibatani M, Fujioka M, Arai Y, Takahashi K, Ueshima K, Okamoto M, Yoshimura N, Hirota Y, Fukushima W, Kubo T. Degree of corticosteroid treatment within the first 2 months of renal transplantation has a strong influence on the incidence of osteonecrosis of the femoral head. Acta Orthop. 2008;79(5):631–6. doi:10.1080/17453670810016641.
Ono K, Tohjima T, Komazawa T. Risk factors of avascular necrosis of the femoral head in patients with systemic lupus erythematosus under high-dose corticosteroid therapy. Clin Orthop Relat Res. 1992;277:89–97.
Li ZR, Sun W, Qu H, Zhou YX, Dou BX, Shi ZC, Zhang NF, Cheng XG, Wang DL, Guo WS. Clinical research of correlation between osteonecrosis and steroid. Zhonghua wai ke za zhi [Chin J Surg]. 2005;43(16):1048–53.
Sinha A, Bagga A. Pulse steroid therapy. Indian J Pediatr. 2008;75(10):1057–66. doi:10.1007/s12098-008-0210-7.
Ce P, Gedizlioglu M, Gelal F, Coban P, Ozbek G. Avascular necrosis of the bones: an overlooked complication of pulse steroid treatment of multiple sclerosis. Eur J Neurol. 2006;13(8):857–61. doi:10.1111/j.1468-1331.2006.01375.x.
Lausten GS, Jensen JS, Olgaard K. Necrosis of the femoral head after renal transplantation. Acta Orthop Scand. 1988;59(6):650–4.
Oinuma K, Harada Y, Nawata Y, Takabayashi K, Abe I, Kamikawa K, Moriya H. Osteonecrosis in patients with systemic lupus erythematosus develops very early after starting high dose corticosteroid treatment. Ann Rheum Dis. 2001;60(12):1145–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Cherian, J.J., Kapadia, B.H., Banerjee, S., Jauregui, J.J., Mont, M.A. (2014). Corticosteroid Usage and Osteonecrosis of the Hip. In: Koo, KH., Mont, M., Jones, L. (eds) Osteonecrosis. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-35767-1_12
Download citation
DOI: https://doi.org/10.1007/978-3-642-35767-1_12
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-35766-4
Online ISBN: 978-3-642-35767-1
eBook Packages: MedicineMedicine (R0)