Abstract
In thyroid cancer 18F-FDG is well established for detection of noniodine-avid disease in patients with elevated Tg levels. From a prognostic perspective it is known that patients with FDG-avid, high-volume disease (>125 mL) as assessed with CT and PET have markedly reduced survival. Thus FDG PET is a tool for assisting in the clinical decision making for either localized or systemic therapy other than the use of 131I in patients with negative iodine scans and elevated hTg and in patients with suspected local recurrence after thyroidectomy. One important prerequisite of using 18F-PET-CT for this patient is that when using it combined with a 131I-scan or when potentially a radio-iodine-therapy is planned no intravenous contrast should be administered for the diagnostic CT. Here PET-MR can offer the possibility to add a diagnostic morphological dataset to the PET-examination as Gd-based contrast media do not interfere with the use of a 131I-scan or therapy. Additionally PET-MR is expected to be a useful tool in surgical planning and radioactive iodine therapy decisions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Thyroid and Endocrine Tumors
In thyroid cancer 18F-FDG is well established for detection of noniodine-avid disease in patients with elevated Tg levels [1, 2]. This has led to a substantial improvement of patient management especially for cases of recurrent tumor [3]. From a prognostic perspective it is known that patients with FDG-avid, high-volume disease (>125 mL) as assessed with CT and PET have markedly reduced survival [4]. Thus FDG PET is a tool for assisting in the clinical decision making for either localized or systemic therapy other than the use of 131I in patients with negative iodine scans and elevated hTg and in patients with suspected local recurrence after thyroidectomy [5]. One important prerequisite of using 18F-PET/CT for these patients is that no intravenous contrast media should be administered when combined with a 131I-scan or when potentially a radio-iodine-therapy is planned no intravenous contrast should be administered for the diagnostic CT [6, 7]. Here PET/MR can offer the possibility to add a diagnostic morphological dataset to the PET/examination as Gd-based contrast media do not interfere with the use of a 131I-scan or therapy. Additionally PET/MR is expected to be a useful tool in surgical planning and radioactive iodine therapy decisions.
For neuroendocrine tumors of the abdomen the use of PET/MR offers potential advances especially for detection of the primary tumor and potential liver metastases. Recently studies [8, 9] showed that 68Ga- radiolabeled somatostatin analog and combination of PET and MR performed significantly more accurate (sensitivity, specificity, NPV, and PPV of 91, 96, 87, and 97 %) compared to PET/CT (74, 88, 69, and 93 %, respectively). It is assumed that MRI compensates for the drawbacks in PET in small hepatic lesions where diffusion-weighted imaging can provide high lesion-to-liver contrast. Additional gain in diagnostic performance is also expected for determining the extent primary pancreatic tumors and thus helping in therapeutic decisions [10, 11]. Especially for neuroendocrine pancreatic cancer MR is often superior to CT in the detection of small lesions implying an important role of PET/MR in this patient population [12, 13].
Metastatic Pulmonary Carcinoid
Clinical History
Twenty-nine-year-old male patient with a neuroendocrine tumor of the right upper lobe of the lung, bilobectomy was performed 6 years ago. Resection of a bone metastasis in the proximal right tibia was performed 3 years ago.
Imaging Technique
Whole body PET/MR images acquired 42 min after i.v. injection of 131 MBq [68Ga]-DOTATOC, weight 82 kg. 8 bed positions × 4 min (head to lower legs). MR-Sequences: Whole body: Dixon for attenuation correction, cor T1 TSE. Liver: ax/cor T2 BLADE.
Left column: Two axial slices (top row and bottom row) showing somatostatin-receptor positive liver metastases with intense tracer uptake (PET). Middle column: T2-weighted MR images show multiple hyperintense masses in the liver, corresponding to the areas of increased somatostatin receptor expression, consistent with liver metastases. Furthermore, additional multiple smaller hyperintense lesions are seen on the MR images, also suspicious for malignancy. Right column: PET/MR fusion
Examples of the multiple bone metastases in this patient. Top row: coronal PET/MR fusion. Bottom row: coronal T1-weighted MR images. Left column: Metastasis in the right clavicle showing intense somatostatin receptor overexpression. Middle column: Metastasis in the right acetabulum, showing a a clear hypointense correlate in the T1w MR image. Right column: multiple somatostatin-receptor positive bone metastases in the right proximal tibia. Additionally, a large hypointense defect is observed in the T1w MR images in the lateral part of the proximal right tibia, showing no tracer uptake, consistent with postoperative changes
Findings
PET shows disseminated bone metastases with avid tracer uptake, correlating with suspicious hypointense signal alterations on the T1-weighted MR images. Additionally, multiple somatostatin-receptor positive liver metastases are seen, showing hyperintense correlates in the T2-weighted MR images.
Teaching Points
Somatostatin receptor PET/MR is feasible for whole-body staging of patients with neuroendocrine tumors. This patient underwent peptide receptor radiotherapy (PRRT) with Lu-177-DOTATATE.
Metastatic Medullary Thyroid Cancer
Clinical History
Eighty-six-year-old male patient with history of total thyroidectomy (medullary thyroid cancer) 12 years ago and radiotherapy of a bone metastasis (4th lumbar vertebra) 2 years ago. Currently ongoing therapy with somatostatin analogs.
Imaging Technique
Whole body PET/MR images acquired 103 min after i.v. injection of 107 MBq [68Ga]-DOTATOC, weight 67 kg. 3 bed positions × 4 min (head to pelvis). MR-Sequences: Partial body: Dixon for attenuation correction, cor T1 TSE. Liver: ax/cor T2 BLADE, ax T1 VIBE, ax DWI.
Two coronal views (top and bottom row) showing a bone metastasis in the 4th lumbar vertebra (lumbalization of the 1st sacral vertebra). Left: PET shows intense overexpression of the somatostatin receptor. Middle: Hypointense mass in the 4th lumbar vertebra with extrasseous soft tissue extension to the right side. Right: PET/MR fusion
Two axial slices (left and right column) showing multiple liver metastases. Top: some metastases show low to moderate expression of the somatostatin receptor (PET). Middle: diffusion-weighted MRI (DWI, b = 800) additionally shows disseminated small, receptor negative metastases. Bottom: PET/MR fusion
Findings
Local recurrence and bone metastases showing intense overexpression of the somatostatin-receptor. Disseminated liver metastases are also observed, showing only low to moderate receptor expression.
Teaching Points
DOTATOC PET/MR can be used for assessment of somatostatin-receptor expression of neuroendocrine tumors. Especially in the liver, DWI can help to identify small or receptor-negative lesions.
Benign Finding on Somatostatin Receptor PET/MR
Clinical History
Fifty-one-year-old male patient after resection of a medullary thyroid carcinoma (left thyroid lobe, T2 N0 M0 R0) including neck dissection two years ago. The serum calcitonin was 72 ng/ml at the time of PET/MR imaging.
Imaging Technique
Partial body PET/MR images acquired 84 min after i.v. injection of 129 MBq [68Ga]-DOTATOC, weight 70 kg. 3 bed positions × 4 min (head to pelvis). MR-Sequences: Dixon for attenuation correction, cor T1w, sag T1w (spine) and sag T2w (spine) sequences.
The lesion in the 8th thoracal vertebra is also hyperintense on the fat-weighted Dixon images (acquired for attenuation correction), consistent with high fat content, consistent with a hemangioma. Left: coronal fat-weighted Dixon image. Middle: sagittal fat-weighted Dixon image. Right: sagittal PET/MR fusion
Findings
Moderate tracer accumulation in the 8th thoracal vertebra. No further foci of pathological tracer accumulation. The finding correlates with a hyperintensity in the T1w images and in the fat-weighted Dixon images, corresponding to an hemangioma. The study was rated negative for metastases.
Teaching Points
MRI is useful to further characterize bone lesions, which may increase sensitivity for bone metastases, but on the other hand may also increase specificity by identifying false positive lesions.
Papillary Thyroid Cancer
Clinical History
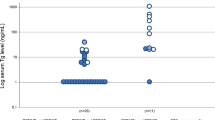
Twenty-three-year-old male patient with papillary thyroid cancer pT3pN1R0 (03/2012). He received 131I therapy for ablation in April 2012. He presented with increased Tg levels (hTg: 3.6 ng/ml, TSH > 100 μIU/ml) and therefore 131I scintigraphy after administration of 40 MBq 131I was performed (Fig. 11.14). To exclude FDG-avid, 131I negative metastases, 18F-FDG PET/MR was performed while planning a second 131I therapy.
Imaging Technique
PET/MR 97 min p.i. of 317 MBq 18F-FDG, 70 kg, 5 bed positions 4 min per bed position. T1 VIBE Dixon for attenuation correction.
MR component: neck: ax T2 STIR, ax T1 TSE −/+ Gd cor T1 SPIR post Gd trunk: ax T1 VIBE fs.
Findings
Diagnostic 131I scan (Fig. 11.14) and 18F-FDG PET/MR (Fig. 11.15) do not exhibit any pathological increased focal uptake. However in the 131I planar and SPECT/CT scan performed after treatment with 206 mCi of 131I increased focal 131I uptake is shown in right cervical lymph nodes (Fig. 11.16). The lymph nodes cannot be distinguished on CT images of SPECT/CT, however they can be identified on MR images of PET/MR (Fig. 11.17).
Teaching Points
When exact anatomical localization of thyroid cancer manifestations is an issue, the MR component of PET/MR can be a valuable tool as the diagnostic performance of CT is limited in this condition due to the inability to use contrast enhancement. Latter would lead to iodine contamination limiting treatment with 131I. Further, iodine negative 18F-FDG avid lesions could be identified with PET/MR.
Lymph Node Metastasis of Thyroid Cancer
Clinical History
Seventy-six-year-old male patient after thyreoidectomy and ablative radioiodine treatment because of papillary thyroid cancer pT3pN1b(2/37)R0. Patient is referred for restaging due to a sonographically conspicuous lymph node in the left supraclavicular region. Thyreoglobulin in serum is not elevated, however there are thyreoglobulin antibodies. Diagnostic 131I scintigraphy (planar and SPECT/CT) with 379 MBq 131I and 18F-FDG PET/MR were performed.
Imaging Technique
PET/MR 78 min p.i. of 428 MBq 18F-FDG, 91 kg, 4 bed positions 4 min per bed position. T1 VIBE Dixon for attenuation correction.
MR component: Neck: ax T2 STIR, ax T1 TSE −/+ GD, cor T1 SPIR post GD, cor T1 TSE, trunk: ax T1 VIBE fs.
Findings
131I scintigraphy did not show any pathological focal uptake, however CT component of SPECT/CT demonstrates an enlarged lymph node in the left supraclavicular region (Fig. 11.18). PET/MR confirms the enlarged lymph node exhibiting an increased glucose utilization, suspicious for malignancy. No other lesions suspicious for malignant manifestations were shown (Figs. 11.19 and 11.20). Whole body PET/MR showed suspicion of a singular metastasis of thyroid cancer. Surgical lymph node excision followed, histopathology confirmed metastasis of papillary thyroid cancer.
Teaching Points
PET/MR is a valuable tool for evaluating iodine negative thyroid cancer. The whole body imaging capability of this technique allows better screening of distant lesions and adjustment of targeted therapy.
Hürthle Cell Thyroid Cancer
Clinical History
Restaging of a 67 year old male patient with Hürthle cell thyroid carcinoma after thyroidectomy, pT4pN0(0/16)R1, and radioiodine treatment for ablation, presenting with increasing thyreoglobulin levels (4 ng/ml) and negative posttherapeutic 131I scintigraphy.
Imaging Technique
PET/MR 90 min p.i. of 448 MBq 18F-FDG, 92 kg, 4 bed positions 4 min per bed position. T1 VIBE Dixon for attenuation correction.
MR component: neck: ax T2 STIR, ax T1 TSE −/+ Gd cor T1 STIR post Gd cor T1 TSE.
Upper row: image of ax T2 STIR, ax T1 TSE and ax T1 TSE post Gd showing a T2 hyperintense signal alteration in the formal right thyroid bed enhancing after contrast media application (arrows). Lower row: image of ax PET and ax PET/MR fusion as well as cor T1 SPIR post Gd showing a contrast enhancing signal alteration in the formal thyroid bed (arrow) corresponding to the hypermetabolic lesion demonstrated in PET. Please note the very high tumor/background ratio in the PET image facilitating detection of local recurrence
Findings
Increased focal 18F-FDG uptake in the region of the formal right thyroid bed indicating local recurrence of the thyroid carcinoma (Figs. 11.21 and 11.22). No other suspicious lesions were observed.
Teaching Points
This case emphasizes the value of PET/MR in iodine negative manifestations of thyroid cancer such as in Hürthle cell carcinoma. The excellent tumor/background ratio of the lesion demonstrated in the PET component of PET/MR facilitates detection of the lesion.
References
Macapinlac HA (2001) Clinical usefulness of FDG PET in differentiated thyroid cancer. J Nucl Med 42(1):77–78
Schlüter B, Bohuslavizki KH, Beyer W, Plotkin M, Buchert R, Clausen M (2001) Impact of FDG PET on patients with differentiated thyroid cancer who present with elevated thyroglobulin and negative 131I scan. J Nucl Med 42(1):71–76
Wang W, Macapinlac H, Larson SM, Yeh SDJ, Akhurst T, Finn RD et al (1999) [18F]-2-Fluoro-2-deoxy-d-glucose positron emission tomography localizes residual thyroid cancer in patients with negative diagnostic 131I whole body scans and elevated serum thyroglobulin levels. JCEM 84(7):2291–2302
Grünwald F, Kälicke T, Feine U, Lietzenmayer R, Scheidhauer K, Dietlein M et al (1999) Fluorine-18 fluorodeoxyglucose positron emission tomography in thyroid cancer: results of a multicentre study. Eur J Nucl Med 26(12):1547–1552
Seiboth L, Van Nostrand D, Wartofsky L, Ousman Y, Jonklaas J, Butler C et al (2008) Utility of PET/neck MRI digital fusion images in the management of recurrent or persistent thyroid cancer. Thyroid 18(2):103–111
Mosci C, Iagaru A (2011) PET/CT imaging of thyroid cancer. Clin Nucl Med 36(12):e180–e185
Abraham T, Schöder H (2011) Thyroid cancer—indications and opportunities for positron emission tomography/computed tomography imaging. Semin Nucl Med 41(2):121–138
Buchmann I, Henze M, Engelbrecht S, Eisenhut M, Runz A, Schäfer M et al (2007) Comparison of 68Ga-DOTATOC PET and 111In-DTPAOC (Octreoscan) SPECT in patients with neuroendocrine tumours. Eur J Nucl Med Mo Imaging 34(10):1617–1626
Schreiter NF, Nogami M, Steffen I, Pape U-F, Hamm B, Brenner W et al (2012) Evaluation of the potential of PET/MRI fusion for detection of liver metastases in patients with neuroendocrine tumours. Eur Radiol 22(2):458–467
Ruf J, Lopez Hänninen E, Böhmig M, Koch I, Denecke T, Plotkin M et al (2006) Impact of FDG-PET/MRI image fusion on the detection of pancreatic cancer. Pancreatology 6(6):512–519
Tatsumi M, Isohashi K, Onishi H, Hori M, Kim T, Higuchi I et al (2011) 18F-FDG PET/MRI fusion in characterizing pancreatic tumors: comparison to PET/CT. Int J Clin Oncol 16(4):408–415
Kalra MK, Maher MM, Mueller PR, Saini S (2003) State-of-the-art imaging of pancreatic neoplasms. Br J Radiol 76(912):857–865
Fidler JL, Johnson CD (2001) Imaging of neuroendocrine tumors of the pancreas. Int J Gastrointest Cancer 30(1–2):73–85
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Eiber, M., Gärtner, F., Scheidhauer, K., Souvatzoglou, M. (2013). Thyroid and Endocrine Tumors. In: Ratib, O., Schwaiger, M., Beyer, T. (eds) Atlas of PET/MR Imaging in Oncology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-31292-2_11
Download citation
DOI: https://doi.org/10.1007/978-3-642-31292-2_11
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-31291-5
Online ISBN: 978-3-642-31292-2
eBook Packages: MedicineMedicine (R0)