Abstract
Variability in exposure to a drug leads to variability in the clinical response across a patient patient population (Rowland et al. 1985). Estimating the variability of the PK (pharmacokinetics) across a patient population requires data obtained from a large study, typically including more than 100 patients. For ethical and practical reasons, pharmacokinetic properties of a drug are difficult to study in large numbers of patients using the traditional approach.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Mixed Effect Modeling
- Concentration Time
- Population Pharmacokinetic
- Intraindividual Variability
- Unbalanced Data
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
PURPOSE AND RATIONALE
Variability in exposure to a drug leads to variability in the clinical response across a patient patient population (Rowland et al. 1985). Estimating the variability of the PK (pharmacokinetics) across a patient population requires data obtained from a large study, typically including more than 100 patients. For ethical and practical reasons, pharmacokinetic properties of a drug are difficult to study in large numbers of patients using the traditional approach.
The PPK (population pharmacokinetic) population approach was suggested by Sheiner et al. (1977) for investigating the typical PK of a drug in a large target population using sparse and unbalanced data obtained without any additional cost during routine care of patients. The PPK approach aims to quantitate the effect of various physiologic factors on drug PK with the overall goal of explaining as much variability as possible.
Using the PPK approach in the development of a new drug has the advantage that the relevant pharmacokinetic parameters for a reasonably large population can be obtained from only a few blood samples per subject. The PPK approach is the method of choice in all situations when only sparse and unbalanced data sparse can be obtained. This situation exists when the PK needs to be studied in elderly, critically ill, and pediatric patients, but also very often in preclinical studies investigating the effects of the drug in animals.
Once such a mathematical model is available, the concentration time courses for various scenarios of administration can be predicted. The dosage can be adjusted to achieve a specific clinical goal like drug exposure within the therapeutic concentration window in the whole population or, if necessary, for special subpopulations characterized by their individual physiology. Following the learning and confirming approach (Sheiner 1997), the predicted clinical success for these optimized dose regimens needs to be confirmed in the next clinical study.
The PPK approach estimates the joint distribution of population-specific pharmacokinetic model parameters for a given drug. Fixed effect parameters quantify the relationship, e.g., of clearance to individual physiology like function of liver, kidney, or heart. The volume of distribution is typically related to body size. Random effect parameters quantify the intersubject variability which remains after the fixed effects have been taken into account. Then, the observed concentrations will still be randomly distributed around the concentration time course predicted by the model for an individual subject. This last error term called residual variability needs to be estimated. As fixed and random effects are included, this method is called mixed effects modeling.
The essential features of a population pharmacokinetic study are summarized in a guideline (FDA 1999).
PROCEDURE
The NONMEM (nonlinear mixed effects modeling) software (Beal et al. 1992), mostly used in population pharmacokinetics, was developed at the University of California and is presently distributed by Globomax. For data management, postprocessing, and diagnostic plots, the software S-plus (Mathsoft) is frequently used.
Before starting model fitting, all available information obtained in previous studies should be assembled (prior knowledge). The analysis starts with an exploration of the data to generate hypotheses for the model: a statistical summary of demography, plots of the logarithm of the concentration versus time indicate the number of pharmacokinetic compartments involved. With the help of plots of individual time courses in a common coordinate system, subgroups in the population may be identified. Normalizing the curves to unit doses should indicate dose linearity or nonlinearity.
Prior knowledge and various hypotheses are condensed into models. NONMEM determines the parameter vector including fixed and random effects of each model using the maximum likelihood algorithm. NONMEM uses each model to predict the observed data set and selects the best PPK parameter vector minimizing the deviation between model prediction and observed data. Comparing model fits by the criteria discussed in the section “Evaluation” should decide which hypothesis is the most likely. As a general rule, the model should be as simple as possible, and the number of parameters should be at a minimum.
The situation after an IV bolus for a system described by a one compartment model with first order elimination can serve to illustrate the procedure. The observed concentration ci,j of an individual i at the time tj can be modeled as
with \( {{\text{k}}_{\text{i}}} = \frac{{{\text{C}}{{\text{L}}_{\text{i}}}}}{{{{\text{V}}_{\text{i}}}}} \), where CLi and Vi are the individual clearance and the individual volume of subject i. εi,j is the residual error drawn from a normal distribution with zero mean and variance σ2 (covariance matrix describing the within subject or residual variability), the intraindividual variability.
The pharmacokinetic parameters themselves are modeled like
where θCL is a population mean clearance and \( {{{\eta }}_{{{\text{C}}{{\text{L}}_{\text{i}}}}}} \)is again a random variable representing the deviation from the population mean of the clearance for the i-th subject. \( {{{\eta }}_{{{\text{C}}{{\text{L}}_{\text{i}}}}}} \) is normally distributed with zero mean and variance ω2 (covariance matrix describing the between subject variability). The unexplained intersubject variability acts as random effect \( {\eta_{{{\text{C}}{{\text{L}}_{\text{i}}}}}} \) on the clearance.
It is important to emphasize that all pharmacokinetic, fixed effect, and random parameters, i.e., θ, ω2, and σ2, are fitted in one step as mean values with standard error by NONMEM. A covariance matrix of the random effects can be calculated. For a detailed description of the procedure, see Grasela and Sheiner (1991) and Sheiner and Grasela (1991).
In a subsequent step, the modeler tries to explain part of the unexplained interindividual variability. Fitted individual parameters (or the variable part expressed by η) are plotted against physiological parameters like weight or indicators of renal or metabolic functionality. Identified dependencies should enter into the model. For example, clearance is very often modeled as depending on the covariate CLCR (creatinine clearance):
In this equation, \( {\text{C}}{{\text{L}}_{{{\text{C}}{{\text{R}}_{\text{i}}}}}} \) is the actual creatinine clearance of subject i. The fixed effect parameters are now θCL corresponding to the clearance of a person with a CLCR of 4 l/h the and \( {\theta_{{{\text{C}}{{\text{L}}_{\text{CR}}}}}} \) as an exponent describing the increase of CLi with CLCR.
The relevance of CLCR for clearance is tested using the likelihood ratio test (Beal et al. 1992). The so-called full model l (alternative hypothesis) given in Eq. 46.3 is tested against the reduced model with \( {\theta_{{{\text{C}}{{\text{L}}_{\text{CR}}}}}} = 0 \) (null hypothesis) characterized by Eq. 46.2.
The more complex full model is accepted only if the objective function obtained with the full model is more favorable than the objective function obtained with the reduced model (see “Evaluation”).
Concentration time courses can be simulated by the model and the demographic parameters for different dose regiments. The final administration of the drug has to be adjusted so that, e.g., 95% of the target population falls into the therapeutic window. If subpopulations differ too much, adjusted administration regiments have to be considered.
EVALUATION
The following criteria determine about the best model:
-
1.
The OF (objective function: negative log of probability, −2 ln(Prob)), calculated by NONMEM, is a measure for the deviation between the model prediction and the observed data. It enters into the likelihood ratio test as follows: if the OF of the full model minus the OF of the reduced model is smaller than −3.84, then the full model can be accepted at a significance level of p < 0.05 (Beal et al. 1992).
-
2.
The observed concentrations plotted against the predicted concentrations had to be more randomly distributed around the line of unity.
-
3.
The weighted residuals and the individual residuals plotted against the predicted concentrations had to show the most symmetric distribution around zero.
In order to validate the final model, the data set can be split randomly into two parts. The model is developed with one part, the index data set. With this model and the demographic data of the second part, the validation data set, observations for the validation data set can be predicted. The difference of predicted data and observations is a measure of the accuracy of the model. An alternative is the bootstrap method (Efron 1981).
MODIFICATION OF THE METHOD
Data from individuals drawn from a target population are not completely independent. Concentration time curves (longitudinal data) of a subject are considered to be driven by a functionality depending on individual parameter values. But what is the connection between the same parameters in different persons? Parts of it may be described by a functionality depending on demographic variables. In any case, unexplained intra- and interindividual random effects remain. Mixed effect modeling clearly distinguishes between these two sources of randomness.
Modifications of the method differ in the way they deal with these different levels of random effects, i.e., how they distribute or confound them. It should be noted that the different handling of random effects has also consequences for the fixed effects.
-
1.
In a situation with many data from each individual drawn in an intersubject balanced manner, a two-stage method is very often used: each individual is fitted individually without considering the interindividual dependencies. In a second step, the parameters are resumed as population mean and standard deviation, often considered as interindividual variability. (STS (standard two-stage method), (Steimer et al. 1985)).
-
2.
If only a few data per subject are available, they are sometimes pooled and considered as coming from one hyperanimal. If several observations are available at the same time, they are averaged, and means and standard deviations can be calculated. In a second step, the mean values are fitted to a pharmacokinetic model. (NAD (naive averaging data method) (Steimer et al. 1985)). A different naive technique is the NPD (naive pooled data) method proposed by Sheiner (Sheiner and Beal 1980). Again, all data are pooled but fitted in one step to a pharmacokinetic model. In both cases, intra- and interindividual random effects are confounded. An influence of covariates cannot be determined by this approach.
-
3.
Mixed effect modeling deals with the situation in between. Inter- and intraindividual variabilities are separated and calculated within the same step. Interindividual random effects are calculated for those parameters for which this information can be drawn from the data set. In general, only one residual error is calculated. The method is very well suited for sparse and unbalanced data situations.
Population pharmacokinetics can be extended to pharmacodynamics and PK/PD modeling using a link model like an effect compartment (Sheiner et al. 1979). In huge clinical trials, only a limited number of patients can be included in a pharmacokinetic satellite study. The model is developed in this satellite. Knowing the demographic covariates of the patients in the whole study, concentration time curves and even effect time curves can be predicted.
Alternative software like NPEM uses nonparametric procedures for the statistical part of the models (Jelliffe et al. 1990).
CRITICAL ASSESSMENT OF THE METHOD
The NAD and NPD methods confound several sources of variability and very often give biased estimates of the mean values of the pharmacokinetic parameters (Steimer et al. 1985). But when the population is very homogeneous, the naive approaches already give reasonable results. The widespread STS method requires the estimation of a large number of parameters, reducing the degree of freedom and leading to over parametrization (large SEMs).
Mixed effect modeling is a very flexible one-step method. It can cope with many situations. It is the only method which can deal with sparse data and unbalanced data sparse situations. The method can start in preclinical phases with animal data. In phase I with a homogeneous population and many observations per individual, the structural model, dose linearity, and bioavailability are determined. In phase II and phase III, patients are investigated, and the demographic parameters should spread over a large range in order to determine the variability in the target population. The method is well suited to perform meta-analysis of several studies.
It should be emphasized that models are not the truth and that different models can describe the same data with the same accuracy. Whereas interpolation for doses or covariates is in general possible, extrapolations should be considered with care. Extrapolation with different models, if available, can give a feeling about the range for the observations to be expected.
Simulations should be used for the design of the next experiment (trial). The new observations should be compared to the prediction allowing improvement of the model in an iterative manner (Sheiner 1997).
EXAMPLE
Introduction
Levofloxacin is the l-isomer of the racemate ofloxacin, a quinolone antibacterial agent used worldwide to treat a wide range of infections. The PK profile of levofloxacin was first characterized in healthy volunteers. The following prior knowledge was obtained before the clinical study presented below. Levofloxacin is primarily excreted renally. Increasing doses of levofloxacin showed linear PK over the investigated dose range between 50 and 600 mg. The PPK of levofloxacin used in patients with respiratory tract infections was investigated by Tanigawara et al. (1995).
Objective
Can 500-mg levofloxacin given twice daily achieve the therapeutic goal of plasma levels above 2 mg/l, the MIC (minimum inhibitory concentration) in male and in female patients?
Materials and Methods
The PPK were analyzed in a subpopulation of 44 out of 314 patients with pneumonia being treated with levofloxacin. Patients received two daily doses of 500 mg for 10 to 15 days. Initially, the drug was given intravenously as an infusion for approximately 60 min. The switch from IV to oral treatment was suggested after a minimum of four IV doses. Three to five blood samples were taken from each patient, 199 blood samples in total.
The available concentration time data is typical for a clinical study: there are relatively few observations on each of a large number of patients, and samples are not taken at the same time points (sparse and unbalanced data). Neither the NAD method nor the STS method can be used. A one compartment model with absorption compartment and first order elimination was fitted to the data by mixed effect modeling with NONMEM. Clearance and volume of distribution were described by
(Eq. 46.3 with \( {\theta_{{{\text{C}}{{\text{L}}_{\text{CR}}}}}} = 1 \))
The model uses CLCR, WT (body weight [kg]), and SEX (1 = male and 2 = female) as covariates.
Alternatively, the volume model was simplified using LBM (lean body mass in kg) instead of WT and SEX. LBM is related to WT, HT (height in cm), and SEX in the following equation:
The model for V (volume of distribution) given as
needs one parameter, θSEX, less than the model given in Eq. 46.5. Now, the PPK model uses in total only two covariates, i.e., CLCR and LBM.
RESULTS
PK Differences Between Male and Female Patients?
The volume given in Eq. 46.5 as a full model (A) changes with θSEX = 0 to a reduced model reduced model (B). To perform the likelihood ratio test, both models were fitted with NONMEM, and the OF of the full model (A) was 6.39 points lower than the OF obtained for the reduced model (B). This difference is highly significant, so the full model (A) is preferred when compared to a reduced model (B).
WT and SEX are combined in LBM. To simplify the model, we described the fixed effect on V only with LBM as a single measure of body size. Using Eq. 46.7 in model (C), we repeated the NONMEM fit and compared the OF obtained for model (C) with the previous two fits. Model (A) was still 3.1 points better than model (C). We preferred model (C) because it uses only body size while model (A) uses body size and sex as demographic covariates in the V model. Table 46.1 resumes the values of the PPK parameter vector including θ (vector of parameter, describing the fixed effect model), ω2, and σ2 calculated for model (C).
Concentration time curves for three individuals with different kidney functions CLCR are shown in Fig. 46.1. The broken lines CLCR represent the time-dependent CLCR as a measure of the kidney function. For the subject shown in the center panel, the CLCR decreases at 3.5 days causing a steep increase in the drug concentration. Dots are observations CONC (observed concentration), and full lines PRED (model predictions for the population with η = 0) correspond to the model predictions for a typical individual with a specific set of mean covariates CLCR, WT, and SEX (fixed effects). The broken lines IPRE (model predictions for the individual subject with random ηi) are the individual predictions for the subject taking the random effects on volume and clearance into account.
Once the model is in place, simulations can be performed in order to find or to verify the optimal dose regimen.
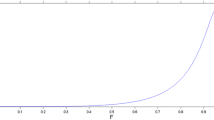
In Fig. 46.2, mean Css (concentration at steady state), given in Eq. 46.8, as a function of CLCR is shown.
Mean concentrations at steady state after twice daily 500-mg levofloxacin. The circles and crosses correspondent to the individual CL estimates in male and female patients, respectively. Three filled circles correspond to patients which PK is shown in Fig. 46.1. The lines are calculated using the fit parameters given in Table 46.1 and Eq. 46.2 for the 2.5, 50, and 97.5% quantiles. All except two individuals are within these limits. The vertical solid lines mark patients with creatinine clearances of 30 ml/min and 70 ml/min, curves stop at 150 ml/min
The circles correspond to the observations. The lines are calculated using the fit parameters and Eq. 46.2 for the 2.5%, 50%, and 97.5% quantiles. All except two individuals are within these limits. As reveals from Fig. 46.2, the selected dose regimen of 500 mg twice daily achieves even in more than 95% of male and female patients with normal kidney function Css concentrations above the MIC of 2 mg/l.
Figure 46.3 shows the joint distribution of V and CLtot (total clearance) for males and females as calculated by the model (C). Volume and clearance are distributed around mean values (center of the ellipse), and they are slightly correlated to each other. The 95% contour line of their joint probability of occurrence is shown as ellipses for male and female.
Joint distribution of V and CLtot. Ellipse joint 95% prediction interval in a subpopulation of male patients (CLCR = 72.53 ml/min and LBM = 57.63 kg) and in a subpopulation of female patients (58.32 ml/min and 43.12 kg). The individual V and CLtot estimates calculated by NONMEM are grouped according to the degree of renal failure
Simulations of the concentration time course under steady state conditions as predicted by the model for a 500-mg twice daily dose regimen are shown in Fig. 46.4. The broad line corresponds to the typical male and female patients. All other lines are calculated using only CL and V pairs of the 95% contour line of their joint probability of occurrence as shown in Fig. 46.3 as ellipses. As reveals from Fig. 46.4, concentration time courses remain within an interval describing the concentrations expected in 95% of male or female patients.
Simulations of the concentration time course under steady state conditions as predicted by the model (C) for a 500-mg twice daily dose regimen. The broad line corresponds to the typical male (CLCR = 72.53 ml/min and LBM = 57.63 kg) and female (58.32 ml/min and 43.12 kg) patients. All other lines are calculated using only CL and V pairs of the 95% contour line of their joint probability of occurrence as shown in Fig. 46.3 as ellipses. The horizontal solid line marks the MIC of 2 mg/l
DISCUSSION
The PPK approach uses all the data observed at all sampling times and from all subjects enrolled in the satellite study in a single step to extract the information necessary to optimize a dose regimen.
For the example of levofloxacin given twice daily 500 mg, 95% of male and female patients achieved the therapeutic goal and showed concentrations above 2 mg/l (MIC) for more than 10 hours of the 12-h dose interval. Due to their smaller volume of distribution, peak concentrations are higher, and half-lives are shorter in female patients. The different extents of accumulation as an effect of differences in half-lives become evident when comparing the through levels. The highest concentrations reached are still below the safety limits. Therefore, the same dose regimen for male and female patients was recommended.
References
Beal S, Sheiner L (1992) NONMEM user guide. University of California, San Francisco
Efron B (1981) Nonparametric estimates of standard error: the jackknife, the bootstrap and other methods. Biometrika 68:589–599
FDA (ed) (1999) Guidance for industry: population pharmacokinetics. CP1
Grasela T, Sheiner L (1991) Pharmacostatistical modeling for observational data. J Pharmacokin Biopharm 19(3):25S–37S
Jelliffe R, Gomis P, Schumitzky A (1990) A population model of genamicin made with a new nonparametric EM algorithm. Technical report 90-4, Laboratory of Applied Pharmacokinetics. University of Southern California School of Medicine, Los Angeles
Mathsoft (ed) (2002) S-Plus 6.0 for UNIX users guide. Mathsoft, Seattle
Press W, Flannery B, Teukolsky S, Vetterling W (1988) Numerical recipes in C, the art of scientific computing. Cambridge University Press, Cambridge, pp 551–553
Rowland M, Sheiner L, Steimer J (eds) (1985) Variability in drug therapy: description, estimation, and control. Raven, New York
Sheiner L (1997) Learning versus confirming in clinical drug development. Clin Pharmacol Ther 61:275–291
Sheiner L, Beal S (1980) Evaluation of methods for estimating population pharmacokinetic parameters I Michaelis–Menten model: routine clinical pharmacokinetic data. J Pharmacokinet Biopharm 8(6):553–571
Sheiner L, Grasela T (1991) An introduction to mixed effect modeling: concepts, definitions, and justification. J Pharmacokinet Biopharm 19(3):11S–24S
Sheiner L, Rosenberg B, Barathe V (1977) Estimation of population characteristics of pharmacokinetic parameters from routine clinical data. J Pharmacokinet Biopharm 5(5):445–479
Sheiner L, Stanski D, Vozeh S et al (1979) Simultaneous modeling of pharmacokinetics and pharmacodynamics: application to d-tubocurarine. Clin Pharmacol Ther 25(3):358–371
Steimer J, Mallet A, Mentre F (1985) Estimating interindividual pharmacokinetic variability. In: Rowland M et al (eds) Variability in drug therapy: description, estimation and control. Raven, New York
Tanigawara Y, Nomura H, Kagimoto N, Okumura K, Hori R (1995) Premarketing population pharmacokinetic study of levofloxacin in normal subjects and patients with infectious diseases. Biol Pharm Bull 18(2):315–320
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this entry
Cite this entry
Weber, W., Rüppel, D. (2013). Population Pharmacokinetics. In: Vogel, H.G., Maas, J., Hock, F.J., Mayer, D. (eds) Drug Discovery and Evaluation: Safety and Pharmacokinetic Assays. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-25240-2_50
Download citation
DOI: https://doi.org/10.1007/978-3-642-25240-2_50
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-25239-6
Online ISBN: 978-3-642-25240-2
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences