Abstract
Nephrotoxicity is an important and preventable cause of nephrotoxin induced acute kidney injury (AKI) as well as chronic kidney disease (CKD). Drugs and toxins may cause renal injury based on several pathophysiological mechanisms. The spectrum of injury may vary from subtle to severe. The diagnosis of nephrotoxic injury requires a high index of suspicion. The common endogenous toxins like hemoglobin, myoglobin, and uric acid as well as exogenously administered drugs, heavy metals, and contrast agents are discussed in this chapter. The risk factors for nephrotoxicity; the various mechanisms of nephrotoxicity such as alteration of renal hemodynamics, acute tubular injury, acute interstitial nephritis, and tubular obstruction; the clinical features; and the relevant investigations are outlined. Various aspects of management and prevention, specific to each of these drugs and toxins, are also discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Chronic Kidney Disease
- Acute Kidney Injury
- Acute Tubular Necrosis
- Nephrogenic Systemic Fibrosis
- Aristolochic Acid
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
16.1 Introduction
-
Nephrotoxins are an important cause of acute kidney injury (AKI) in children. They may also be the cause for chronic kidney disease (CKD).
-
There are several factors which increase vulnerability of the kidney to nephrotoxic injury. The kidney is an important site for metabolism of various drugs. The large blood flow through glomeruli and peritubular vessels, the large surface area available for uptake of nephrotoxic compounds, the high concentration of drugs within the tubular lumen which promotes intracellular uptake and precipitation and crystallization within tubules, multiple transport systems which concentrate the drug or its metabolite within tubular cells, and the high metabolic rate of renal tubular cells which makes it susceptible to injury with mild oxygen depletion are some of them.
-
Endogenous substances like hemoglobin, myoglobin, and uric acid are toxic to the tubules and cause AKI. Commonly used drugs like NSAIDs and antibiotics can be toxic to the kidney. Often, there may be more than one drug which contributes to kidney injury. Renal injury associated with drugs may involve more than one mechanism. Critically ill children, neonates, and children with preexisting renal disease are at maximum risk of nephrotoxicity.
Risk Factors for Nephrotoxicity
Extremes of age |
Volume depletion |
Concomitant use of several nephrotoxic medications |
Compromised renal function |
Drug dose, frequency, and duration related |
-
The spectrum of nephrotoxicity can vary from subtle manifestations to severe kidney injury. Though AKI is the most common renal injury produced by nephrotoxic agents, prolonged exposure to certain drugs may predispose to chronic kidney disease, e.g., NSAIDs.
-
The diagnosis of nephrotoxicity is often missed or delayed due to the presence of coexisting risk factors, subtle manifestations, and lack of availability of early markers. A high index of suspicion; use of urinary biomarkers of renal injury, e.g., β-2 microglobulin, retinol-binding protein, and neutrophil gelatinase-associated lipocalin (NGAL) in early stages; and monitoring of drug levels may help in early diagnosis and prompt treatment of nephrotoxicity.
-
Pseudonephrotoxicity must be suspected when drugs which inhibit tubular secretion of creatinine (e.g., cimetidine, trimethoprim) or drugs which interfere with the laboratory estimation of creatinine (e.g., cefoxitin, flucytosine) cause a rise in creatinine in the absence of other manifestations of renal injury.
Mechanisms of Nephrotoxicity
Alteration of renal hemodynamics/vasoconstriction resulting in decreased renal perfusion: |
Nonsteroidal anti-inflammatory drugs (NSAIDs), angiotensin-converting enzyme inhibitors (ACE inhibitors), calcineurin inhibitors, norepinephrine, radiocontrast agents, and diuretics |
Acute tubular injury: |
Aminoglycosides, amphotericin B, vancomycin, NSAIDs, contrast media, acetaminophen, cyclosporin, cisplatin, IV immunoglobulin, mannitol, heavy metals |
Acute interstitial nephritis: |
Ciprofloxacin, methicillin, penicillin G, ampicillin, cephalosporins, rifampicin, sulfonamides, NSAIDs, contrast media, thiazides, furosemide, phenytoin, allopurinol, cimetidine |
Tubular obstruction: |
Sulfonamides, methotrexate, methoxyflurane, triamterene, acyclovir, ethylene glycol, protease inhibitors, pigments (hemoglobin, myoglobin), statins (rhabdomyolysis) |
Hypersensitivity angiitis: |
Penicillin G, ampicillin, sulfonamides |
Thrombotic microangiopathy: |
Mitomycin C, cyclosporine, oral contraceptives |
Glomerulopathy: NSAIDs, gold, penicillamine |
Papillary necrosis: NSAIDs |
Nephrocalcinosis: Furosemide |
16.2 Endogenous Nephrotoxins
16.2.1 Hemoglobinuria
16.2.1.1 Causes of Hemoglobinuria
-
Genetic defects: Glucose-6-phosphate dehydrogenase deficiency, paroxysmal cold hemoglobinuria, march hemoglobinuria
-
Infections: Malaria, clostridia
-
Transfusion reaction
-
Chemical agents: Quinine sulfate, benzene, hydralazine, fava beans
-
Venoms: Snakes, spiders
-
Traumatic/mechanical destruction: Prosthetic valves, disseminated intravascular coagulation, extracorporeal circulation
-
Miscellaneous: Heatstroke
16.2.2 Myoglobinuria
16.2.2.1 Causes of Myoglobinuria
-
Traumatic muscle injury: Crush injury, pressure necrosis, severe burns
-
Drugs/toxins: Barbiturates, benzodiazepine, HMG-CoA reductase inhibitors, fibric acid derivatives, salicylates, carbon monoxide, ethylene glycol, snake and insect venoms, succinylcholine, propofol
-
Genetic disorders: Phosphorylase deficiency, phosphofructokinase deficiency, α-glucosidase deficiency, carnitine palmitoyl transferase deficiency
-
Infections: Influenza, tetanus, gas gangrene, Coxsackie virus, leptospirosis, HIV
-
Excessive muscular activity: Vigorous exercise, status epilepticus, tetany
-
Ischemia: Arterial occlusion
-
Electrolyte and endocrine/metabolic disorders: Hypokalemia, hypophosphatemia hypothyroidism, hypothermia, and hyperthermia
-
Immunologic diseases: Polymyositis, dermatomyositis
16.2.3 Clinical Presentation of Hemoglobinuria and Myoglobinuria (Pigment Nephropathy)
The presenting features of pigment-induced nephrotoxicity include oliguria and reddish urine; oliguria lasts for 7–10 days. Urine analysis shows acidic pH, no RBCs in the urine, and positive benzidine test suggesting hemoglobinuria/myoglobinuria. Granular casts/pigment casts may also be seen. Hyperkalemia disproportionate to renal failure is usually seen in case of massive hemolysis/rhabdomyolysis. Fractional excretion of sodium is generally low. In case of hemolysis and hemoglobinuria, pallor is seen. There will be evidence of hemolysis in the form of elevated reticulocyte count, peripheral smear showing features of hemolysis and elevated LDH, and low serum haptoglobin suggesting intravascular hemolysis. In case of myoglobinuria, there may be evidence of muscle injury and history of drug intake along with elevated LDH and CPK levels.
16.2.4 Pathophysiology of Pigment Nephropathy
The cause of pigment-associated acute tubular necrosis (ATN) is not well defined. The proposed mechanisms are (a) hypovolemia and ischemia, (b) direct tubular toxicity, and (c) tubular obstruction with pigment casts.
16.2.5 Treatment of Pigment Nephropathy
-
Forced alkaline diuresis: Give fluids intravenously or orally, a one and a half to two times the maintenance rate depending on the condition of the child to target a normal central venous pressure and urine output of >3 ml/kg/h. Sodium bicarbonate (50–100 mmol) can be added to 1 l of 0.45 NS with dextrose, with the aim of maintaining the urine pH >6.5.
-
Mannitol: Ensures good diuresis, acts as a free radical scavenger, and increases renal blood flow. It can be given at 3–5 ml/kg/dose every 8 h. Check plasma osmolality and osmolal gap while on mannitol and consider stopping mannitol if signs of fluid overload or if plasma osmolal gap exceeds 55 mOsm/kg.
-
Consider renal replacement therapy if there is resistant hyperkalemia, rapidly rising serum potassium, oligoanuria, volume overload, or severe metabolic acidosis (pH <7.1).
-
Recovery is usually complete.
16.2.6 Uric Acid Nephropathy
-
Acute uric acid nephropathy is seen in patients with leukemias/lymphomas who develop massive cell lysis (tumor lysis syndrome) resulting in release of uric acid. Hyperuricemia causes uricosuria and uric acid crystal deposition and obstruction of renal tubules.
-
Risk factors for uric acid nephropathy include urine pH less than 5.0, dehydration, rapid response to chemotherapy, elevated serum uric acid, and preexisting renal dysfunction.
-
Lesch-Nyhan syndrome is a genetic disorder of uric acid metabolism which can result in uric acid calculi and nephropathy.
-
Uric acid nephropathy is characterized by elevations in blood urea nitrogen, creatinine, potassium, uric acid, and phosphate concentrations and a decrease in the serum calcium levels.
-
Acute kidney injury due to acute uric acid nephropathy is oliguric. Elevations in BUN and serum creatinine typically develop 2 days after the initiation of chemotherapy and return to baseline after 7–10 days.
-
The urinary uric acid-to-creatinine ratio greater than 1 is consistent with acute uric acid nephropathy.
-
Prophylaxis as well as treatment of tumor lysis syndrome includes the use of xanthine oxidase inhibitors, forced diuresis, and urinary alkalinization. Dialysis may be required in some cases.
-
Rasburicase, a recombinant form of urate oxidase, is an option for treatment of uric acid nephropathy. It is given in the dose of 0.2 mg/kg/day as an IV infusion over 30 min.
-
-
Prophylaxis:
Prior to chemotherapy, ensure hydration. Measure uric acid and creatinine levels. If renal function is normal, start with fluids at twice the maintenance rate (3 l/m2/day). Monitor intake-output strictly and watch for signs of fluid overload. Diuretics may be used to maintain a good urine output. Allopurinol can be added prophylactically in patients with hyperuricemia or if there is high tumor burden.
Urinary pH should be maintained above 7.0, titrating intravenous bicarbonate therapy.
-
Prophylaxis:
-
Fluid overload, refractory hyperkalemia, hyperphosphatemia, and acidosis may be indications to initiate dialysis.
-
Recovery is usually complete.
16.3 Exogenous Nephrotoxins
16.3.1 NSAIDs (Nonsteroidal Anti-inflammatory Drugs)
16.3.1.1 Acute Kidney Injury
-
NSAIDs precipitate acute kidney injury in conditions with impaired GFR due to inhibition of the compensatory vasodilatation caused by prostaglandins at the efferent arteriole.
-
Volume depletion, neonatal period, congestive cardiac failure, and hypoalbuminemia are risk factors.
-
The renal toxicity is dose, drug, and duration related. Aspirin is least likely and indomethacin is most likely to cause AKI. Ibuprofen, diclofenac, and naproxen have an intermediate nephrotoxicity.
-
COX-2 selective NSAIDs (rofecoxib, celecoxib) also induce renal dysfunction especially in high-risk patients.
-
Onset is usually 1–5 days after ingestion and may be oligoanuric or nonoliguric.
-
Usually renal failure is reversible upon discontinuation of NSAIDs. If NSAIDs must be used in a child who has poor renal perfusion, a drug with a short half-life should be used (e.g., aspirin, sulindac).
-
NSAIDs also cause tubulointerstitial nephritis which may present as acute kidney injury.
-
Typically manifests as oliguric or nonoliguric AKI with nephrotic range proteinuria and eosinophiluria or leukocyturia.
-
AKI is usually reversible.
16.3.2 Antibiotics
16.3.2.1 Aminoglycosides
-
Aminoglycosides are eliminated unchanged almost entirely by the kidneys. They are highly charged cations which bind to tubular epithelial cells of S1 and S2 segments of proximal tubules from where they are reabsorbed by pinocytosis via megalin and are translocated into the lysosomes. Accumulation induces an injury cascade, phospholipid hydrolysis, formation of electron dense myeloid bodies, and progression to cell necrosis.
-
Risk factors for aminoglycoside toxicity:
-
Patient-related factors: Newborns, preexisting renal disease, intravascular volume depletion, and Mg, K, Ca deficiency
-
Drug-related factors: Recent aminoglycoside therapy, large doses, treatment for more than 15 days
-
Concomitant use: Amphotericin B, cisplatin, cephalosporin, and furosemide
-
-
Nephrotoxicity is drug, dose, and duration related. The order of relative toxicity of aminoglycosides, from the most toxic to the least, is neomycin, gentamicin, tobramycin, and amikacin.
-
A variety of tubular dysfunction syndromes, Fanconi syndrome, hypomagnesemia and hypokalemia, and antidiuretic hormone resistance, are observed.
-
Clinical manifestations: Usually nonoliguric, starts within 5–10 days following exposure to drug.
-
Enzymuria is the first indicator of aminoglycoside toxicity. Tubular proteinuria and glycosuria may be seen. Hypokalemia and hypomagnesemia are common. The other significant toxicity is ototoxicity, to which there may be a genetic predisposition.
-
Usually, the acute kidney injury is reversible but may take days to weeks.
-
Serum aminoglycoside levels must be checked in all patients who are on therapy for 3–5 half-lives (2–3 doses) of the drug. The trough level is checked 30 min prior to the dose and peak level is checked after 30 min of intravenous infusion. The peak and trough levels are specific for each drug and also the conditions for which the drug is being administered. Recommended peak and trough levels for amikacin are 20–30 mcg/ml and <10 mcg/ml, respectively.
Prevention of Aminoglycoside Toxicity
Identify risk factor – patient- and drug-related factors |
Single daily dose |
Administer as an infusion and not as a bolus |
Minimum duration of treatment |
Avoid other concomitant nephrotoxic drugs |
Avoid dehydration |
Corrected doses if reduced GFR |
Estimate trough blood levels and titrate dose |
Use alternative non-nephrotoxic drugs if possible |
16.3.2.2 Beta-Lactam Antibiotics
-
Penicillins, cephalosporins, and carbapenems are all associated with nephrotoxicity. Cephaloridine and imipenem are most nephrotoxic.
-
Cefotaxime, ceftazidime, and meropenem are nephrotoxic and require dose adjustments in renal failure.
-
Ceftriaxone and cefoperazone are not nephrotoxic and hence do not require dose adjustments in renal failure.
-
Clinical features: Usually an idiosyncratic response. They may present as oliguric or nonoliguric renal failure. Acute tubulointerstitial nephritis presents as nonoliguric renal failure and may be associated with systemic manifestations like fever, rash, and arthralgia. Urinalysis shows tubular proteinuria, pyuria, and eosinophiluria.
-
Lipid peroxidation, acylation, inactivation of tubular proteins, and inhibition of mitochondrial respiration are the major mechanisms of nephrotoxicity.
-
Acute tubulointerstitial nephritis (TIN) due to hypersensitivity can also cause renal failure, especially with drugs like methicillin.
-
Generally resolves spontaneously; steroids may be helpful in acute TIN.
-
Administration of probenecid may help to reduce the nephrotoxic effect of beta-lactam antibiotics.
16.3.2.3 Glycopeptide Antibiotics (Vancomycin)
-
Usually asymptomatic and manifests only as rise in serum creatinine levels.
-
The exact mechanism of action is not known. Accumulation in the lysosomes of the proximal tubule contributes to nephrotoxicity.
-
Nephrotoxicity is related to the dose and duration of therapy.
-
Risk factors are high baseline serum creatinine, concomitant nephrotoxic drugs, and existing liver disease.
-
Nephrotoxicity is usually reversible.
-
Therapeutic drug monitoring helps to titrate therapy in high-risk groups. The target trough level is 10 mcg/ml.
16.3.2.4 Others
-
Sulfonamides and their acetylated metabolites are poorly soluble in acidic urine and may precipitate leading to intrarenal obstruction. This can be prevented by adequate fluid intake and alkalinization of urine.
-
Trimethoprim can cause hyperkalemia by blocking amiloride-sensitive channels. It blocks tubular secretion of creatinine causing pseudonephrotoxicity.
16.3.3 Antifungals
16.3.3.1 Amphotericin B
-
The drug interacts with membrane cholesterol at the distal tubule and leads to formation of aqueous pores resulting in increased permeability and back diffusion of H+, Na+, and Cl− resulting in “backleak” type of distal renal tubular acidosis and vasopressin-resistant polyuria. It also causes reduced GFR secondary to afferent arteriolar vasoconstriction.
-
The toxicity is related to the cumulative dose, dosing frequency, duration, and formulation (lipid and liposomal formulations are less nephrotoxic).
-
The risk factors for nephrotoxicity are salt depletion, concomitant use of diuretics, cyclosporine or aminoglycoside antibiotics, abnormal renal functions, and young age.
-
It clinically manifests as distal renal tubular acidosis, hypokalemia, hypomagnesemia, and decreased GFR secondary to afferent arteriolar vasoconstriction.
-
Salt supplementation reduces the incidence and severity of nephrotoxicity. Normal saline infusion (10–15 ml/kg) pre- and post-amphotericin B dose is recommended. Use of lipid-based formulations of amphotericin B may produce less nephrotoxicity, without affecting clinical effectiveness.
16.3.4 Antivirals
16.3.4.1 Acyclovir and Ganciclovir
-
The toxicity of these drugs may be due to direct tubular toxicity or due to intrarenal obstruction due to crystal deposits. These drugs are excreted by glomerular filtration and tubular secretion. They form insoluble crystals which precipitate in the distal tubule.
-
Risk factors include high doses of intravenous acyclovir, volume depletion, and preexisting renal disease.
-
Clinical features: Usually asymptomatic; however, symptoms may develop within 24–48 h after starting therapy. Nausea, vomiting, flank pain, or abdominal pain may occur. Urinary findings include crystalluria (needle shaped crystals), hematuria, pyuria, and proteinuria.
-
The renal insufficiency is generally reversible and renal function returns to normal by 1 week.
-
Infusing the drug slowly over 1–2 h and hydrating the child adequately to maintain a high urinary flow help lower the risk for renal toxicity. Probenecid coadministration may reduce the tubular secretion of acyclovir.
16.3.4.2 Other Antivirals
-
Foscarnet: Drug toxicity profile is similar to acyclovir. It also causes functional renal tubular defects like hypophosphatemia, hypokalemia, and nephrogenic diabetes insipidus.
-
Cidofovir: Causes proximal tubular necrosis and renal failure.
-
Tenofovir: Presents with proximal tubular dysfunction resulting in Fanconi syndrome.
-
Indinavir: Causes crystalluria resulting in obstruction and renal failure. It may also present as renal calculi and chronic renal dysfunction. The crystals appear as flat rectangular plates in fan-shaped or starburst aggregates.
16.3.5 Chemotherapeutic Drugs
16.3.5.1 Cisplatin
-
Cisplatin is an inorganic platinum compound that may induce acute and chronic renal toxicity. Carboplatin is less nephrotoxic when compared to cisplatin. Cisplatin decreases the GFR and also acts as a direct tubular toxin.
-
The nephrotoxicity is dose related.
-
Clinical features: Usually presents with polyuria, tubular proteinuria, and tubular loss of potassium, magnesium, sodium, phosphate, and amino acids.
-
Hypomagnesemia is a striking feature of cisplatin toxicity and may take weeks to improve.
-
Prevention of nephrotoxicity: Infusion of mannitol and saline has been used to maintain good urine output and reduce nephrotoxicity. Dosage should not exceed 25–33 mg/m2/week. The administration of cisplatin in hypertonic saline is associated with better tolerability.
-
Sodium thiosulphate administration also protects the kidneys. The role of amifostine, a free radical scavenger, has been approved for use with cisplatin. N-Acetylcysteine, free radical scavengers, and liposomal formulations are being tried to reduce the nephrotoxic effects of platinum compounds.
16.3.5.2 Ifosfamide
-
Unlike cyclophosphamide, ifosfamide is associated with significant nephrotoxicity. Ifosfamide and its metabolites like chloroacetaldehyde have been found to be toxic to cells.
-
The incidence is variable and depends on cumulative dose (>60 g/m2), rapidity of administration, concomitant nephrotoxic drugs like platinum compounds, and age of patient.
-
Clinical features: Presents with features of tubular injury resulting in nonoliguric renal failure, associated with tubular wasting of glucose, phosphate, low molecular weight proteins, and bicarbonate and loss of concentrating ability.
-
Though usually reversible, chronic hypophosphatemia, rickets, and chronic kidney disease also have been found as late consequences of ifosfamide toxicity.
-
Mesna which is used to prevent hemorrhagic cystitis does not offer any protection against nephrotoxic effects of ifosfamide.
16.3.5.3 Cyclophosphamide
-
Though cyclophosphamide is not a nephrotoxic drug, it can cause hemorrhagic cystitis.
-
Syndrome of inappropriate antidiuresis (SIAD) may also be seen with cyclophosphamide.
16.3.5.4 Methotrexate
-
The nephrotoxicity has been attributed to the precipitation of the drug and its metabolites within the tubular lumen and also due to direct tubular toxicity.
-
Clinical presentation: Methotrexate toxicity is associated with decrease in GFR and increase in serum creatinine.
-
Usually reversible and may require about 2 weeks for recovery.
16.3.6 Calcineurin Inhibitors (Cyclosporine and Tacrolimus)
-
Mechanism of action: The nephrotoxic effects may be acute or chronic.
-
Acute nephrotoxicity: Hemodynamically mediated, dose dependent, reversible reduction in GFR due to afferent arteriolar vasoconstriction. Damage to the vascular endothelium may result in hemolytic uremic syndrome resulting in acute kidney injury. Proximal tubular defect includes impaired secretion of uric acid and urea, hyperkalemia, and hyperchloremic metabolic acidosis. It can also cause hypomagnesemia.
-
Chronic nephrotoxicity: Defined as 20 % or greater irreversible reduction in GFR. It is characterized by morphological changes including tubular atrophy, striped interstitial fibrosis, vascular hyalinosis, and glomerular sclerosis. This may not be dose dependent and not reversible.
-
-
Drugs like ketoconazole, macrolides, and metoclopramide which inhibit the metabolism of calcineurin inhibitors may potentiate toxicity.
-
Clinical features: May be asymptomatic and recognized only by monitoring of creatinine levels. May manifest as delayed graft function in the post-transplant period. It may be difficult to distinguish calcineurin toxicity from graft rejection. In children with nephrotic syndrome, calcineurin toxicity may be a differential diagnosis for progression of focal segmental glomerulosclerosis. Monitoring of serum levels may help in titrating the dose of calcineurin inhibitors.
-
Acute nephrotoxicity usually resolves spontaneously with cessation of therapy.
16.3.7 Angiotensin-Converting Enzyme (ACE) Inhibitors and Angiotensin Receptor-Blocking Agents (ARB)
-
Clinical features: Oliguria and hyperkalemia are common manifestations.
-
Usually reversible on reduction of dose or cessation of the drug.
-
Fetopathy and severe oliguric renal failure in newborn have been reported with maternal ingestion of ACE inhibitors.
-
The main mechanism of acute renal dysfunction is due to inhibition of the afferent arteriolar dilatation and efferent arteriolar constriction which is a compensatory autoregulatory response of angiotensin II in order to maintain the GFR.
-
Risk factors for renal dysfunction are dehydration, hypovolemia, congestive cardiac failure, renal artery stenosis, and concomitant use of other nephrotoxic medications like NSAIDs. They must be used with caution in patients with solitary kidney and renal artery stenosis.
16.3.8 Paracetamol
-
Usually presents as AKI due to acute tubular necrosis with proteinuria, granular casts in the urine, hematuria, and pyuria.
-
Paracetamol/acetaminophen: Though hepatotoxicity is the most common manifestation of paracetamol poisoning, nephrotoxicity is also known.
-
Nephrotoxicity is attributed to the depletion of sulfates and glutathione resulting in the accumulation of the toxic metabolite N-acetyl-p-benzoquinone imine (NAPQI).
-
The serum creatinine peaks at 7 days and returns to normal within a month.
-
N-acetylcysteine may be considered in the management of nephrotoxicity.
16.3.9 Radiocontrast Agents
-
Radiocontrast agents are tri-iodinated benzoic acid derivatives which are freely filtered at the glomerulus.
-
Clinical features: Nonoliguric renal failure characterized by an elevation in serum creatinine within 24 h of exposure is typical. Rarely, it may be oliguric. The serum creatinine peaks at 3–5 days and returns to baseline within 14 days. Urine analysis may show tubular proteinuria and granular casts. Fractional excretion of sodium remains low (<1 %).
-
An absolute rise of serum creatinine of ≥0.5 mg/dl within 48 h of exposure to a contrast or a 25 % increase in serum creatinine from baseline within 48 h of exposure is defined as contrast-induced nephropathy (CIN). Other sensitive markers like cystatin C and NGAL (neutrophil gelatinase-associated lipocalin) are being studied as early indicators of renal dysfunction.
-
Mechanism of action: Renal medullary ischemia due to vasoconstriction is the most important pathophysiological mechanism resulting in tubular cell hypoxia and damage. Hyperviscosity of the contrast media and osmolar load also result in medullary hypoxia. Free radical injury may contribute to worsening of renal failure.
-
Risk factors for CIN: Preexisting renal dysfunction, congestive cardiac failure, hypovolemia, younger age, concomitant NSAIDs, and diuretics are known risk factors. Diabetes mellitus and myocardial infarction are important risk factors in adults.
-
Pharmacokinetic properties of contrast media which predispose to CIN: High osmolality, high viscosity, and higher volumes of contrast are known risk factors. Low-osmolar agents (iohexol, iodixanol) may have benefit over iso-osmolar agents in reducing the risk of CIN.
-
Usually recovery is spontaneous, with <1 % requiring dialysis.
-
Prevention:
-
(a)
Intravenous hydration: Hydration with isotonic saline prior to contrast administration has been found to be useful in reducing the risk of CIN.
-
(b)
Sodium bicarbonate has been shown to be effective in reducing the risk of CIN.
-
(c)
N-acetylcysteine: Has shown significant reduction in the risk of CIN.
-
(d)
Diuretics may be used only in situations of fluid overload. There is no role for use of mannitol.
-
(e)
The role of theophylline, dopamine, and acetazolamide in preventing CIN is unclear.
-
(a)
Protocol for Prevention of Contrast-Induced Nephropathy
Ensure adequate hydration – isotonic saline started at 1 ml/kg/h at least 2 h prior to contrast administration and continued for 6–12 h following the procedure. |
Sodium bicarbonate – 3 ml/kg bolus over 1 h prior to the procedure and 1 ml/kg/h for 6 h after the procedure. |
N-acetylcysteine 1,200 mg/1.73 m2 twice a day, orally on the day before and on the day of the procedure. |
16.3.9.1 Nephrogenic Systemic Fibrosis (NSF)
-
Nephrogenic systemic fibrosis is the result of systemic toxicity in patients with impaired renal function who have subsequent impaired clearance of gadolinium and related compounds.
-
Gadolinium is a non-iodinated contrast agent used for magnetic resonance angiography and digital subtraction angiography. The risk of nephrotoxicity with gadolinium was thought to be minimal, and hence, it was considered to be a substitute for iodinated contrast agents in high-risk groups. Later, it was discovered that NSF could be a complication of using gadolinium in patients with renal insufficiency.
-
Nephrogenic systemic fibrosis is a condition seen in patients with renal dysfunction exposed to gadolinium. Gadolinium-based agents are rapidly excreted by normal kidneys. In patients with CKD, the time for these agents in circulation is increased and they dissociate into linear chelates. The free gadolinium chelates are responsible for NSF. This primarily involves the skin resulting in fibrosis and myxedema-like features. The early changes are pain, pruritus, erythema, and edema which usually begin over the legs and later progress to involve the entire body, sparing the head and neck. Usually seen within 18 months following exposure to gadolinium, this condition may also affect the liver, heart, and skeletal muscle. In late stages, there can be severe contractures resulting in deformities.
-
The proposed mechanism of action is release of free gadolinium ions which deposit in the skin resulting in fibrosis.
-
It can be fulminant and fatal in <5 % cases.
-
Prevention:
-
(a)
Avoid use of gadolinium-based contrast in children with renal dysfunction.
-
(b)
Use of low-dose gadolinium.
-
(c)
Hemodialysis initiated following exposure may be helpful in clearance of gadolinium in patients with GFR <30 ml/1.73 m2/min. Peritoneal dialysis is not effective.
-
(a)
-
Treatment of nephrogenic systemic fibrosis are as follows:
Corticosteroids, sodium thiosulfate, intravenous immunoglobulin, phototherapy, and ultraviolet radiation have been used as modalities for the treatment of nephrogenic systemic fibrosis.
16.3.10 Miscellaneous
16.3.10.1 Herbal Medications
-
Chinese herbal medicines use aristolochic acid derived from Aristolochia plant species which is known to cause aristolochic acid nephropathy, endemic Balkan nephropathy, and reversible renal Fanconi syndrome.
-
Aristolochic acid nephropathy and endemic Balkan nephropathy present with tubular proteinuria, proximal tubulopathy, sterile pyuria, and anemia. It causes chronic kidney disease and can predispose to urothelial malignancies. The progress to ESRD is rapid in aristolochic acid nephropathy (1–2 years) as compared to endemic Balkan nephropathy (15–20 years).
-
Traditional medicinal products contain several plant products and heavy metals which can induce various renal problems like acute tubular necrosis, acute or chronic interstitial nephritis, Fanconi syndrome, dyskalemia, arterial hypertension, papillary necrosis, and urolithiasis and urothelial cancer. Glycyrrhiza (licorice) may induce arterial hypertension and hypokalemia.
-
Mushrooms (Cortinarius species) are known to cause acute kidney injury due to the toxic substance orellanine. Acute tubular necrosis and acute interstitial nephritis are seen.
16.3.10.2 Ethylene Glycol and Methanol
-
Ethylene glycol (EG) and methanol are components of antifreeze or transmission fluid. The ingestion, usually accidental or suicidal, results in severe high anion gap metabolic acidosis and AKI.
-
Untreated, three phases have been described as follows: (1) neurologic stage, with hallucinations, stupor, and coma; (2) cardiovascular toxicity with cardiac failure; and (3) renal failure due to acute tubular necrosis.
-
The compounds are not themselves toxic, but their metabolites are. Metabolism is initiated by alcohol dehydrogenase (ADH) and results in oxalate and organic acids for ethylene glycol and formic acid and formaldehyde for methanol.
-
Oxalic acid combines with calcium to form calcium oxalate crystals in the renal tubules.
-
Other laboratory findings: Calcium oxalate crystalluria, hematuria, and hypocalcemia.
-
Ethanol and fomepizole are specific antidotes which inhibit alcohol dehydrogenase and prevent metabolism of ethylene glycol into toxic metabolites.
-
Mild cases may require only symptomatic treatment.
-
In moderate to severe cases, criteria for antidotal therapy in EG poisoning are the following:
-
EG concentration in serum above 200 mg/l
-
Patient’s history of ingestion of a toxic dose of EG and an osmolar gap of more than 10 mOsm/kg
-
Suspicion of EG poisoning by history or clinical symptoms and two of the following criteria: Arterial blood pH <7.3, serum bicarbonate concentration <20 mmol/l, osmolar gap >10 mOsm/kg, and crystals of calcium oxalate in urine sediment
-
Fomepizole is better tolerated in children; loading dose of 15 mg/kg, followed by four bolus doses of 10 mg/kg every 12 h
-
-
Hemodialysis is recommended if the EG serum level is above 500 mg/l.
16.3.10.3 Heavy Metals
-
Lead: Lead toxicity may be acute or chronic. It has several systemic manifestations like abdominal pain, cognitive deficits, peripheral neuropathy and arthralgia, a lead line at the junction between tooth and gum, and anemia with basophilic stippling. The nephrotoxic effects may manifest as a Fanconi syndrome with damage to the proximal tubule.
The acute effects of lead on the kidney are generally reversible. Chronic lead toxicity results in progressive tubular atrophy and interstitial fibrosis resulting in chronic kidney disease. It can also cause nephrotic syndrome, hyperuricemia, and hypertension.
-
Cadmium: Chronic exposure to cadmium causes chronic kidney disease and osteoporosis.
-
Mercury: Acute mercury poisoning can cause tubular necrosis and AKI. Long-term exposure can cause membranous nephropathy.
16.3.10.4 Animal Toxins
-
Snake envenomation (refer to Chap. 13).
-
Animal stings: Sting by animals (e.g., spiders, arthropods, scorpions) can induce nephrotoxicity in the form of acute tubular necrosis, acute interstitial nephritis, hemolytic uremic syndrome, nephrotic syndrome, and, rarely, pigment nephropathy. Marine animals (e.g., carp, jellyfish, and sea anemones) can also induce acute tubular necrosis, proteinuria, and nephrotic syndrome.
16.3.10.5 Melamine Poisoning
Melamine formaldehyde is an adulterant in powdered milk formula to increase the nitrogen content of the food. The “outbreak” of renal stones in children following consumption of adulterated milk in China has brought melamine poisoning into light. Cyanuric acid, the metabolite of melamine, is implicated in the nephrotoxicity. The toxic effects can be acute or chronic. It can present with nephrolithiasis and AKI. The usual clinical features are hematuria, flank pain, and dysuria. The symptoms are due to renal stones (melamine, uric acid, and triple ammonium phosphate) and due to urinary tract infections. The symptoms are seen within 3–6 months following consumption of melamine. Hypertension, edema, and acute kidney injury may be seen in severe cases. Melamine stones are radiolucent and are usually multiple and bilateral. Urine analysis shows microscopic hematuria with or without proteinuria. Melamine crystals appear as fan-shaped crystals on microscopy. Long-term exposure to melamine can cause bladder calculi and transitional cell carcinoma. Treatment for renal calculi and AKI is conservative. Rarely, surgical removal of calculi is indicated. Food and Drug Administration (FDA) gives a safety limit of exposure to melamine and its structural analogues as <0.63 mg/kg/day.
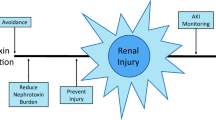
Conclusions
Nephrotoxic renal injury is an important and preventable cause of AKI as well as CKD in children. The spectrum of nephrotoxicity is varied and requires a high index of suspicion for early diagnosis. Most common cause for nephrotoxic renal injury is “drug toxicity.” A drug may cause nephrotoxicity by several mechanisms and different drugs may share common mechanism of nephrotoxicity. Altered hemodynamics, acute tubular necrosis, or acute interstitial nephritis contributes to acute kidney injury. Nephrotoxic injury can be prevented by appropriate dose reduction in renal failure, avoiding concomitant use of nephrotoxic medications, and monitoring of drug levels, whenever possible. The drug toxicity may also present as chronic kidney disease.
Suggested Reading
Bacchetta J, Dubourg L, Juillard L, Cochat P (2009) Non-drug-induced nephrotoxicity. Pediatr Nephrol 24:2291–2300
Cronin RE (2010) Contrast induced nephropathy: pathogenesis and prevention. Pediatr Nephrol 25:191–204
Hau AK, Kwan TH, Li PK (2009) Melamine toxicity and the kidney. J Am Soc Nephrol 20(2):245–250
Lopez-Novoa JM, Quiros Y, Vicente L, Morales AI, Lopez-Hernandez FJ (2011) New insights into the mechanism of aminoglycoside toxicity: an integrative point of view. Kidney Int 79:33–45
Patzer L (2008) Nephrotoxicity as a cause of acute kidney injury in children. Pediatr Nephrol 23:2159–2173
Penfield J (2008) Nephrogenic systemic fibrosis and the use of gadolinium based contrast agents. Pediatr Nephrol 23:2121–2129
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Vasudevan, A., Kamath, N. (2014). Nephrotoxicity. In: Phadke, K., Goodyer, P., Bitzan, M. (eds) Manual of Pediatric Nephrology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-12483-9_16
Download citation
DOI: https://doi.org/10.1007/978-3-642-12483-9_16
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-12482-2
Online ISBN: 978-3-642-12483-9
eBook Packages: MedicineMedicine (R0)