Abstract
Reoperation may be needed for a number of reasons following repair of esophageal atresia (EA) with or without a tracheoesophageal fistula (TEF). Although not all complications require reoperation, one may be desirable either because of the severity or to bring the problem to a close if nonoperative treatment has been unsuccessful. The judgments about the severity of the problem or the risk of reoperation will vary considerably among practitioners, consequently, so will treatment plans. For many surgeons, a reoperation understandably seems daunting and clearly requires experience and a center that is able to support complex procedures. Currently, there is a lack of clear definitions and guidelines for what deserves reoperation; nevertheless, with these variables in mind, we will present our approach for significant complications which we believe justify an operative solution.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Esophageal atresia
- Tracheoesophageal fistula
- Postoperative results
- Redo operations
- Recurrent fistulas
- Leaks
- Strictures
- Diverticula
- Intrathoracic stomach
Introduction
Reoperation may be needed for a number of reasons following repair of esophageal atresia (EA) with or without a tracheoesophageal fistula (TEF). Although not all complications require reoperation, one may be desirable either because of the severity or to bring the problem to a close if nonoperative treatment has been unsuccessful. The judgments about the severity of the problem or the risk of reoperation will vary considerably among practitioners, consequently, so will treatment plans. For many surgeons, a reoperation understandably seems daunting and clearly requires experience and a center that is able to support complex procedures. Currently, there is a lack of clear definitions and guidelines for what deserves reoperation; nevertheless, with these variables in mind, we will present our approach for significant complications which we believe justify an operative solution.
Reoperation may solve the problem more quickly and effectively than other approaches, and this chapter will discuss why and how they are done. Among the significant complications of EA repair, the literature reports an anastomotic leak rate of up to 25 % and a recurrent TEF (recTEF) incidence of up to 15 % [1–6]. Postoperative anastomotic strictures are also common although the frequency has not been established because, to some degree, it is a subjective diagnosis without an agreed-upon definition. These problems as well as residual tracheal pouches, diverticula from a previous myotomy, and a partially intrathoracic stomach from whatever cause often deserve reoperation. The literature has shown that the significant early complications are more frequent in repairs of long-gap EA (LG-EA); however, even apparently successful short-gap repairs may have chronic problems worthy of reoperation [1–14].
From the literature, the majority of leaks apparently heal spontaneously, but some do not and may require reoperation to close a chronic lesion. A recTEF, in contrast, is unlikely to heal on its own because a mucosa-lined track usually forms which prevents spontaneous closure. Several endoscopic methods to treat a recTEF including stripping off the mucosa and/or plugging the track with various materials have been described [15]. Success, based on the patients referred to us, is unpredictable and the recTEFs often persist. Furthermore, a stricture in combination with either a leak or a recTEF presents an even more difficult problem because the usual methods of dilating the stricture will also likely keep either the anastomotic hole or the recTEF open. For these problems, reoperation will often be the best solution.
There are several other lesions following an EA repair which may be best treated by a reoperation. Occasionally, a residual pouch left in the tracheal membranous septum at the site of a lower segment fistula may enlarge, collecting mucous and bacteria which produce symptoms [12]. Although attempts to reduce the pouch have been made endoscopically, at present, a reoperation will likely be more successful [16].
Two other problems which result from techniques used to facilitate an anastomosis are a diverticulum from a circular myotomy or reflux from a partially intrathoracic stomach. Doing one or more myotomies or pulling the stomach part way up through the hiatus to allow a primary anastomosis in a longer-gap defect may have seemed like a good idea at the time; however, there may be unfavorable consequences. A myotomy may result in a large unsupported diverticulum which hinders food passage, continues to enlarge, and may even cause airway problems [13, 17]. For a partially intrathoracic stomach with the GE junction is in the chest, whether high or low, it is subjected to negative pressures, and significant reflux is predictable as are the consequences. These are difficult and reliably progressive problems which are very unlikely to be effectively treated without a corrective operation.
Most structural complications, with the exception of some anastomotic leaks, are unlikely to resolve without intervention and left untreated, usually produce significant symptoms. Consequently, for persistent problems resistant to nonoperative strategies, the indications for a reoperation will include large anastomotic leaks, recurrence of a TEF, a membranous tracheal pouch, significant GER, a recalcitrant stricture which does not relent with dilations and/or short-term stent placement, a large esophageal diverticulum, or a partially intrathoracic stomach. These are often complicated clinical situations and may require some combination of esophageal, tracheal, stomach, and diaphragm repair.
Reoperations, however, with predictable, often “dense” adhesions, the uncertain quality of the tissues to be repaired, and a lack of experience with difficult reoperations all may temper the surgeon’s enthusiasm. The trepidation about reoperation may lead to a continued search for other solutions, to the detriment of the patient. Consequently, sending a patient with a significant chronic problem to a center where sufficient experience and expertise exists will make sense [11].
Reoperation, as a result, will fall to some surgeons, and the purpose of this chapter is to describe the surgical details which should aid in carrying out repeat thoracotomies with successful repair of the problems encountered.
The Surgical Technique for Reoperations
Timing of the Reoperation
The timing of the reoperation in relation to the previous thoracotomy or laparotomy will affect the ease of reentry. If the reoperation is done within about 10–12 days after the previous operation, reentry through the interspace and dissection throughout the pleural space will be relatively easy. Increasingly after this time and until at least 5–6 weeks later, the neovasculature that accompanies adhesion formation will insure blood loss during reoperation. After about 6 weeks’ time, the vascularity will have largely regressed and, as the adhesions become filmy in nature, bleeding during reoperation will be less.
The Incision, the Interspace, and the Dissection
With the patient in a straight lateral position, perhaps tipped a little forward, the previous skin incision is usually reopened which will allow access to virtually any interspace. Presumably, the original opening was correct for the initial lesion, and the recurrent problem will likely be in the same area and related to its repair. The same interspace is usually also reopened, but if one needs to be higher or lower inside the chest, a different interspace can be chosen. Admittedly, it will often be easier to enter through another interspace; however, the more interspaces entered, the greater the potential for fusion of multiple ribs, one of the causes of thoracic deformity [18].
A redo thoracotomy is more difficult for several reasons. Entering an interspace for the second or third time often means encountering fused ribs unless a piece of folded thin Silastic sheeting has been left between them. The rib fusion may be so dense that an osteotome will be required to separate them to gain entrance into the chest cavity. Only one corner of the osteotome should be used at a shallow angle to limit the depth of the cutting surface and avoid incising the adherent lung below.
Once the intercostal division is underway, the assistant elevates and pulls the ribs apart with two vein retractors, sturdy tissue hooks or similar instruments, creating a potential space which allows the lung to be dissected off the chest wall ahead of the osteotome. The dissection will be carried anteriorly and posteriorly in the line of incision and also superiorly and posteriorly to open the pleural space. The separation of the lung from the chest wall should be done as broadly as possible to avoid the disadvantages of working down in a tunnel. Elevating the rib cage, as described, makes the dissection easier, and at some point, a small chest retractor can be placed and it too can be elevated.
Carrying Out the Dissection
The general principle that will greatly aide achieving the preoperative goals will be to take down essentially all adhesions between the lung and the chest wall and, more posteriorly, with the esophagus. Depending on the location of the lesion and the size of the patient, it may not be necessary in a larger patient to take down all the adhesions medially between the lung and diaphragm.
The adhesions between the lung and parietal pleura are best taken down broadly and sharply under direct vision unless they are very filmy. The temptation will be to lyse as few adhesions as possible and go directly to the presumed site of the problem, whether it is esophageal or airway or both. This approach unfortunately results in a long, relatively narrow tunnel with the problem at the bottom. Effective repair, however, requires both good visualization of the lesion and mobility of the tissues to be brought together for closure. Consequently, dissecting the lung free and separating it from the esophagus will be important to success.
As noted, the dissection should proceed broadly anteriorly, superiorly, and inferiorly to prepare for the important posterior dissection. Then, lifting up the lung brings the dissection as much as possible up into the area of the incision and aids the lysis of the posterior adhesions by putting them on stretch. The lung can be elevated by using a small round peanut sponge held by a clamp, and, as the dissection progresses, a clamped larger tonsil or thumb sponge can be used to help separate the structures. In general, elevating the lung and bringing it and other structures up anteriorly rather than pushing them downward and medially will facilitate the dissection as it proceeds posteriorly. Elevation will create a potential space between structures which becomes realized as the dissection proceeds.
Completely freeing up these structures has at least two advantages. The nature of the problem will be better revealed, allowing lesions, such as fistulas to more remote parts of the bronchial tree, to be easily found. Secondly, and importantly, it will also provide the necessary mobility for effective esophageal and tracheal repairs. These repairs are much more difficult when the problem is seen at the bottom of a deep hole and hindered by the constraints of surrounding tissues and scarring. With experience, the dissection, which may seem daunting initially, becomes more straightforward and can be reliably done in reasonable time. This experience, nevertheless, will more likely be acquired at a center specializing in these problems.
Dissection of the Esophagus and Airway
With the lung essentially completely mobilized, it can be elevated and retracted medially revealing the esophagus and much of the posterior (membranous) aspect of the airway. The area of the anastomosis is usually the site of the problem whether it is a leak, a stricture, or the presence of a recTEF, and the dissection will be easier if this site is not approached first. A relatively normal portion of the esophagus, usually closer to the diaphragm, is chosen and dissected free (at least the anterior surface), and, if helpful, a loop is passed around it. The posterior and medial adhesions to the esophagus will also be put on stretch by the loop making them easier to divide. The looped esophagus is pulled toward the surgeon allowing its contour to be visualized and the surface followed precisely up to the problem area, avoiding a new injury to either esophagus or airway.
A fistula into the airway, whether proximal or distal, will become obvious by the air leak when it is divided. A recTEF in a larger patient may not require full mobilization of the esophagus if the communication is small; nevertheless, the entire anterior surface should be free for a tension-free closure of the esophageal end of the fistula. A stricture alone or in combination with a recTEF, however, will require complete and extensive mobilization of the esophagus to enable a well-constructed anastomosis to be created after the resection.
Nonoperative Closure of Anastomotic or Post-dilation Leaks
From literature reports, many esophageal leaks close spontaneously with adequate chest tube drainage, but sometimes they do not and a procedure may be required to close the hole and allow feeding to begin. Several endoscopic methods have been used and are usually the first approach if the hole is not large. The endoscopic results so far have been variable and success is generally inversely related to the size of the hole. As with any new technique, however, improvement can be expected.
Through the endoscope, the edges of the hole may be clipped together, and this is most likely to be successful if the hole is small or a vertical split as might occur after a dilation. Larger holes or those with edges that cannot be pulled together easily by clips will be unlikely to benefit from this technique and might be made worse by the effort.
Another endoscopic approach is the short-term placement of covered stents which allow closure to take place. Because these stents have had some success, they will likely be used increasingly in the future as more experience is gained. Stents also have the advantage of holding the lumen open while the hole closes and may limit the consequences of the stricturing tendency present early after completion of the anastomosis. A stricture may still form after stent removal, however, which poses a difficult problem because of the presence of the healed leak site with its potential for reopening if dilations are used. In this case, reoperation with the excision of both the stricture and leak site will be the best solution.
Finally, it has been claimed that a nasogastric tube can be placed down the esophagus and guided out the hole into the cavity providing a form of internal drainage. The abscess cavity may close down satisfactorily, which would allow the tube to be slowly withdrawn; nevertheless, this procedure would only be used in very unusual circumstances. No reports of the use of this technique have appeared in the pediatric literature.
In summary, each of these endoscopic techniques has succeeded and each has failed. Predictably with experience and better techniques, success will come more frequently; nevertheless, there will be leaks that require reoperation.
Suturing Techniques for Leaks or the Difficult Anastomosis
The repair of a leak will obviously be influenced by the size of the hole which will usually be either at the anastomotic site or a longitudinal split from dilation. With the lung mobilized and retracted, the leak site will be exposed. An effective repair will require joining viable, full-thickness esophageal walls trimmed of any obviously infected, necrotic tissue. The suturing techniques will be similar to those used for a first time primary anastomosis. For larger holes, whose closure will be under tension, the intraoperative technique of gradually bringing the edges together to allow closure can be used. All the sutures for closure are accurately placed and tagged (Fig. 40.1). When all are placed, the sutures are crossed and used to gradually pull the edges together. When the edges are touching and held in position, individual sutures are tied off tension with the knots brought down carefully, keeping the edges in apposition.
Alignment of the esophageal wall edges to promote accurate healing is very important for successful closure of a hole or for the creation of an anastomosis. If the edges are not aligning well, then suturing techniques can be used to overcome the malalignment. Lembert-type stitches in which the very edge of the mucosa is caught by the suture will align the walls (Fig. 40.2). If one edge is turned up or down, angling of the needle as it passes through the wall will help correct this by lowering or raising the edge. The needle is held by a Castro-Vejho needle holder, which can be used like a pen to compose the anastomosis and make up for alignment deficiencies between the two ends. By angling the needle during placement of the stitch to include more outer wall and less mucosa will depress the edge of the esophagus (Fig. 40.3a, c). Similarly, angling the needle to include less wall near the outer surface and more on the mucosa side, it will elevate the cut edge of the esophagus (Fig. 40.3b, d). Careful sewing techniques such as these will align the edges of the esophagus for a successful closure of a defect or to produce a well-constructed anastomosis (Fig. 40.3c, d).
Esophageal wall alignment disparity corrected by using angled needle and suture placement. (a) A wider tissue bite on the outer surface of the esophagus and narrow on the mucosal side will drop the edge and align as shown. (b) A narrower tissue bite on the outer wall and a wider bite at the mucosal side will elevate the cut edge. (c, d) When tied, the sutures placed as described above align the cut edges to promote accurate healing
The Recurrent Tracheoesophageal (Airway) Fistula
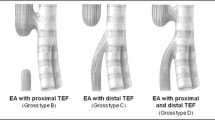
The literature indicates that in about 5–15 % of repaired EA cases, a fistula will later develop between the esophagus and the airway [1, 2, 4]. Most commonly, this is a recurrence of the original fistula between the lower esophageal segment and the back of the trachea or the proximal right main stem bronchus as found in the common form of EA (type C). Typically, recTEF becomes apparent within a few months of the original repair.
The mechanism of recurrence presumably relates to the esophageal anastomotic line and the repair site of the airway being close together and vulnerable to the microabscesses which may appear in suture lines. An abscess will tend to migrate to a cavity, a lumen, or the outside. In the cases of the recTEF, the abscess migrated in order to drain, both into the trachea and back into the esophagus. Rarely, a similar inflammatory mechanism with a different location may result in the fistula entering the left main stem bronchus.
A recTEF is usually signaled by coughing, significant aspiration episodes, and pulmonary infections. In general, the more proximal and larger the TEF, the easier are the diagnosis and location established [4, 15, 19, 20]. The more distal recTEFs tend to be smaller and often require a careful contrast study to demonstrate a communication with the airway and provide an explanation for the pulmonary symptoms. The partial outlining of the distal trachea by an esophagram, done without spill over from above, satisfactorily confirms its presence and may identify the location. A fistula into a smaller bronchus can cause continued contamination of the airway; however, demonstrating it and localizing the site preoperatively can be difficult (Fig. 40.4). A small blush of contrast material from the esophagus into the lung field will establish the cause of the pulmonary problems, but may not provide much information on the location of the fistula into the airway.
When a fistula between the esophagus and airway is suggested because of the signs and symptoms and has been confirmed by a blush of contrast, the question becomes one of treatment. A recTEF, or even a de novo TEF, will pose problems and a conservative approach is unlikely to be effective [4, 19, 20]. The recTEF will soon be lined with mucosa which tends to preserve the lumen and prevent spontaneous closure. Furthermore, the presence of both a TEF and an accompanying stricture creates a difficult problem because adding dilations may also enlarge the TEF or at least keep it open.
The Later Appearing, More Remote Recurrent Tracheoesophageal Fistula
A smaller percentage of fistulas, however, occur at sites remote from the original TEF or develop following an EA repair even though none was present originally. The more distal airway fistulas may be less clear as to their cause, but likely began with a small abscess where the lung was adherent to the esophagus. Although the process may begin more peripherally near the surface of the lung, it can still find its way into a segmental bronchus and produce problems (Fig. 40.4).
In one case, a previously asymptomatic patient developed an occasional cough, not related to drinking liquids, 8 years after an uncomplicated repair of pure EA (type A). Contrast material injected into a small esophageal opening flowed through the peripheral lung parenchyma in an irregular path until it reached a small bronchus. The irregular path through the lung slowed the drainage of liquids; consequently her cough was sporadic and did not appear to be triggered by drinking.
Presumably, the recTEF began with the formation of an abscess in the peripheral part of the right lung which was adherent to the esophagus after the two earlier thoracotomies for the growth procedure. Again, the abscess migrated both to the esophagus and eventually to a small bronchus. Treatment required a reoperation with simple closure of the small esophageal opening and a more generous over sewing of the adherent pulmonary end. With a relatively small area of very chronic pneumonia adherent to the esophagus, it may be desirable to remove this portion of lung.
Nonoperative Methods to Close the Recurrent Fistula
The operative treatment of a recTEF may seem daunting because of predictable adhesions obliterating the pleural space and, often, because of its uncertain location. Consequently, a number of endoscopic methods have been devised to strip the mucosa and close the track, but these may not work and even might make the hole larger [15]. The methods range from laser treatments to plugging the fistula with artificial tissue membranes. More recently, tissue sealants in combination with the temporary placement of covered stents in the esophagus at the site of the fistula have achieved some successes with the more proximal recTEFs. The tissue sealants and implants do not seem to make the situation worse; however, they have not been reliable, are expensive, and may only delay resolution of the problem. Once the recTEF is established, the mucosa-lined fistulas resist closure and endoscopic procedures may not suffice for closure and reoperation will be necessary [15]. Other nonoperative methods of fistula closure will continue to be sought, however, and may, eventually, prove to be satisfactory and reliable.
Localization of the Fistula
If the fistula is a recurrence of the original TEF from the lower segment of esophagus (type C), its identification in the membranous portion of the trachea is reassuring as to where it will be at reoperation. For a fistula into the right main stem bronchus or even further out, the possibility of identifying and localizing it by bronchoscopy becomes progressively less even though the esophageal opening may be found. Because a TEF occasionally occurs more distally, it is useful to understand how the TEF can be effectively located and treated despite the uncertainty and apparent difficulty it presents.
When the fistula can be visualized by bronchoscopy and an operative repair is planned, it has been frequently recommended that a catheter or wire be placed across the fistula to aid in locating it during the operative procedure [4, 19–23]. Although many surgeons have followed this advice which seems to have logic on its side, we have not found it either necessary or even helpful. The bronchial end of a distal fistula which is producing symptoms and problems, moreover, may be difficult to locate preoperatively by endoscopy causing consternation and even leading to the conclusion that “nothing more can be done.” Beginning in Minnesota, where we were referred many recTEF cases and, more recently, in Boston where even a larger number have been treated, the operative approach to be described effectively revealed fistulas of any location and size without wire localization and allowed reliable closure.
Reoperation for Recurrent TEF
The operative approach is designed to insure the esophageal-airway fistula is found and divided no matter how small in size or distal in location. Once divided, this technique also maximizes the likelihood of a satisfactory repair with little chance of another recurrence. To accomplish these goals, the reoperation begins by opening the previous incision and dissecting the lung free, virtually to the diaphragm, so it can be elevated and the esophagus located. After the esophagus is first reached, usually well below the anastomotic site, the dissection follows the surface of the esophagus superiorly up into the thoracic inlet which will necessarily divide the recTEF. The separation of the lung and airway from the esophagus will efficiently reveal the divided fistula by the bubbling with ventilation at the site of the bronchial communication. Complete separation of the esophagus and the airway will also allow both ends of the fistula to be repaired under better visualization and, importantly, with less resulting tension imposed by inflexible, scarred surrounding structures.
The only fistula that could be missed by this technique would be in the cervical region; however, in this location, the preoperative studies would have identified it and the approach would be by a neck incision. And, although approaching a recTEF from the left side has been advocated, full mobilization of the structures would be made much more difficult by this approach which encounters the aorta [24].
The holes in a recTEF are typically small. A single generous, horizontal mattress suture should straddle the hole and incorporate almost the full wall up to the submucosa. When tied carefully, but not too tightly, the suture will provide a secure closure. A second more widely placed stitch can be used to reinforce closure but it must be tied even less tightly.
Another advantage of generous mobilization of the esophagus and tracheobronchial tree is that after the recTEF has been divided and repaired at each end, the two suture lines tend to lie some distance apart, further diminishing the chance of recurrence. If the two suture repairs remain close together, however, two or three relatively superficial sutures can be placed in the esophageal wall and posteriorly into the chest wall fascia to roll the esophageal closure further away from the tracheal repair.
As with the anastomosis, we believe the use of nonreactive sutures will minimize the inflammatory response. A simple repair using fine nonabsorbable monofilament sutures which are the least reactive material will minimize the occurrence of small abscesses. The choice between fine monofilament absorbable and nonabsorbable sutures will be made by the surgeon, but we have settled on the least reactive. Even absorbable sutures set up some local reaction with hydrolysis which helps make the case for a fine, nonabsorbable monofilament suture. Braided sutures are even more prone to microabscesses and silk sutures which are inherently very reactive would be the worst choice.
A 6-0 suture should be satisfactory for closure of the small fistulas. The knot should begin with two similar throws so it can be carefully tightened to bring the tissues together before a squaring throw locks it. The knot should be only composed of four to five throws, and back pulling on the last throw will further lock the knot. The ends should be cut short to minimize the adverse effects of the suture material. These steps are done to minimize the occurrence of small abscesses which can enlarge and migrate toward the lumens of the trachea and esophagus, producing the dynamics which will result in a recTEF. This operative technique has been used successfully and without later recurrence in 38 consecutive cases in Minnesota and Boston where recTEF is a problem commonly referred for treatment [25].
A case has also been made in the literature for inserting tissue such as intercostal muscle or pleural or pericardial flaps between the suture lines to reduce the possibility of another recurrence. Again, although this may appear to be a helpful idea, the reported results seem no better than repairs without a flap and, compared to our experience, not as good [23, 26]. Any mobilization of flap tissue, moreover, may produce areas of necrosis and/or foster formation of microabscesses which add to the potential for a recTEF.
In summary, reoperation for a recTEF requires extensive mobilization and elevation of the lung and airway of the esophagus. This frees up a generous amount of the esophageal surface which will divide the connection and allows easy visualization of the holes, extensively mobilizing the esophageal wall so that an accurate and effective closure can be carried out. The tracheal repair should neither reduce the lumen size nor leave behind an unsupported pouch which may increase in size, harbor infection, and promote refistulization.
Strictures
As noted, clinical judgments about the severity of a stricture vary, but our definition has been that any visible anastomotic narrowing on a contrast study is at least a mild stricture. Even a mild stricture will likely produce some degree of dysphagia and perhaps episodes of food sticking. To function normally, the esophagus will need to be supple enough to allow the passage of solids of a larger diameter than the lumen collapsed at rest. Without distensibility, even a mild narrowing will limit the passage of some solids and be unpleasant for the patient. If a stricture is considered significant only when the lumen is clearly narrowed, patients with a lesser but real stricture will have to compensate by eating small bites of solids, with careful chewing to avoid food being caught at the site.
These two viewpoints are at the ends of a spectrum on how strictures are judged and treated. Because there is no agreed-upon definition of what constitutes a significant stricture, variation in the diagnoses and recommended treatments will continue to exist. The methods and vigor of the treatment will vary both from the judgments of the stricture and the experience and capability of those dealing with them. Mild strictures may not be addressed beyond the early postoperative period as the patients seem to be “doing well,” and, as a probable consequence, dysphagia is very common even in adults who have had the common-type C EA/TEF repair in infancy [9, 10].
We believe a successful outcome of EA repair, however, does not include dysphagia, and these symptoms deserve evaluation and treatment. Dilations and, more recently, stent placement remain the first line of stricture treatment. The Minnesota experience has suggested relatively early, and frequent dilations seem more likely to encourage the stricturing tendency to relent rather than beginning dilations after more severe symptoms develop and the stricture is tighter [27, 28]. A more severe stricture will require more vigorous dilations, stirring up the mechanisms which lead to this problem.
Strictures, however defined, occur more commonly following repairs of longer-gap EA under tension and in patients with continuing gastroesophageal reflux (GER) [1, 2, 27–29]. The presence of GER will also be a persisting obstacle to effective stricture treatment, and, because late dysphagia is so common, the problem and treatment of strictures will be presented in detail.
Resection of Short Strictures
A variable of importance is the length of the stricture. Although most anastomotic strictures are relatively short and can be resected, the more recalcitrant ones may be relatively long making operative treatment including resection with primary anastomosis more difficult. For long strictures, the principle of growth induction by axial tension has been used to allow staged resection and eventual primary esophageal repair.
For relatively short, recalcitrant strictures, there are two operative options which preserve the esophagus. The first and most straightforward method is complete excision and reanastomosis. Even for a stricture length of 1.5 cm, however, complete excision will leave a gap of at least 4 cm after the ends retract, increasing the difficulty of the reanastomosis. This predictable situation is why surgeons may resort to a pull-up procedure for even a modest sized stricture. In experienced hands, however, resection and primary anastomosis keeping the GE junction below the diaphragm can be reliably accomplished and will prove to be increasingly beneficial over the succeeding years (Fig. 40.5a, b).
When making the decision to resect a stricture, several considerations should be kept in mind. The extent of the fibrous stricture may be longer than anticipated which, together with the retraction of for the divided esophagus, might make the resulting gap much longer than anticipated. The reoperation therefore should be approached in a flexible manner which does not prevent an eventual primary esophageal anastomosis and avoids a shift to a “rescue” gastric interposition. Finally, the entire stricture must eventually be resected; otherwise, the symptoms will persist and little will have been gained.
If there is uncertainty about the actual length of the stricture, the flexible approach would be to divide the esophagus in the center of the stricture and then systematically resect more until the surgeon believes that no more can be taken without jeopardizing the ability to accomplish an anastomosis. Once the esophagus has been divided and at least a portion of the stricture has been resected, there are three general possibilities for completion of the operation: (1) do a primary anastomosis even if the stricture has not been completely resected and plan on a second resection to remove the remainder in 7–10 days (2) close the ends or at least close the lower end and bring out a spit fistula, or (3) bring up an interposition graft. Only the first result, however, would be a completely acceptable outcome.
Resection of a stricture should be done carefully so that a primary anastomosis remains possible. A partial resection should be done initially and then more taken if an anastomosis under tension can still be accomplished. Sutures can be placed through the cut ends, tagged, and crossed to limit retraction. Under very special circumstances, the stricture can be 75–80 % resected, leaving a strip of back wall, which will somewhat limit retraction and may add a sense of security. A complete resection of the stricture will be more desirable.
With more experience and careful attention to the details of creating an anastomosis, complete resection of a relatively short stricture will be reliably done. For longer strictures, a primary anastomosis will still be possible after using growth induction as part of a staged resection.
Stricturoplasty (Vertical Incision for a Short Stricture)
The second method, applicable for a relatively short lesion, consists of a longitudinal incision through the stricture with transverse closure. Although this will have the apparent advantage of largely eliminating the effect of retraction and preserving the back of the wall, it poses difficulties and leaves the original stricture in place, affecting perhaps 60–70 % of the eventual circumference. To effectively relieve the stricture, the longitudinal incision must extend well above and below it; otherwise, even a transverse closure will not open up the lumen satisfactorily. It is the length of the vertical incision that determines how much the stricture will be opened. The upper and lower ends of the vertical incision will be brought together as the middle point of the transverse closure and consequently this distance may be much greater than the ends following a simple excision. The mid portion of the closure, therefore, may be under significant tension and difficult to bring together. This consideration limits this approach.
To accomplish this approach, after a suitably long opening has been made, closure begins by placing a suture at the midpoint on each side of the longitudinal incision. These sutures are tagged and pulled laterally to set up the transverse closure (Fig. 40.6a). Additional sutures to accomplish the transverse closure are placed, tagged, crossed, and put under increasing traction to bring the edges together. This method will be satisfactory if the midpoints are not too far apart (Fig. 40.6b). Once the midpoints are essentially in apposition, the tying can proceed from laterally to medially on each end until the closure is complete. In this approach, a complete, full-thickness esophageal repair is desirable to avoid the use of a patch to complete the closure. The use of tissue patches to widen the lumen has been reported, and although colon patches will open up the area, their wall strength may not be adequate over the long term and a diverticulum may form [30]. Once formed, a diverticulum will have a tendency to enlarge, compounding the problem.
In summary, this technique of a longitudinal incision with transverse closure may appear useful under certain circumstances. In general, however, despite its initial appeal, it will only be workable for short strictures which are usually better served by resection.
Longitudinal Stricturoplasty
Another technique has been described which features a long incision through the fibrous portion of the stricture but only down to the mucosal layer [31]. The result resembles a pyloromyotomy for hypertrophic pyloric stenosis with mucosa bulging out between the edges of the split stricture. Given the probable need for a fundoplication and the sporadic contractile function of the lower esophagus following EA repair, the outpouching mucosa may begin to expand because of the slow emptying. Once the mucosa has begun to enlarge, the outpouching may continue to increase in size. Follow-up studies are not available in the literature; however, it does not seem likely that this method will provide a satisfactory long-term solution.
Residual Tracheal Pouch
If the tracheoesophageal fistula in the common form of EA (type C) is not repaired flush with the tracheal wall using tissue of good holding power, a pouch may develop. The pouch will tend to retain mucous and bacteria, leading to aspiration and other symptoms [12–16]. Although the natural history of these residual lesions from an EA/TEF repair is variable, because the pouches are relatively unsupported, they will often continue to enlarge, increasing the problem. Only local scarring associated with the original repair might impede this progression; consequently, when symptoms appear, the likelihood is that they will only increase in size and reoperation will eventually be needed.
To close the pouch, an essentially complete dissection is carried out and the lower trachea and esophagus separated. Because the wall of the diverticulum will be thin and easily entered, its location should be determined as the dissection proceeds superiorly. The light from a fine bronchoscope in the pouch usually provides the necessary information to safely continue the dissection upward.
Once the pouch has been dissected out and the esophagus retracted away, the decision on the specifics of the repair can be made. The repair will be carried out in a vertical direction and individual sutures on each side of the pouch should include a rim of the membranous septum. Although the membranous septum is relatively thin, the tissue is stronger than that of the residual pouch and a vertical closure will heal well and solve this problem. A vertical repair is desirable because the tracheal cartilages will prevent a horizontal closure of even a medium-sized defect.
The size of the pouch will affect the method of repair. If the pouch is small, endoscopic closure may suffice [16]. Larger pouches will likely require reoperation [12]. If the pouch is too big to be simply reefed up as the sutures are tied, it should be unroofed to leave less tissue folded into the closure itself; otherwise, later remodeling and regression of the wrapped up tissue might leave loose sutures and increase the potential for recurrence. There are no established guidelines; however, if the pouch is large and it appears too much tissue will be incorporated in the repair, a portion should be excised. These are the general principles; nevertheless, this repair is not without potential difficulties.
Esophageal Diverticulum
Following one or more circular myotomies, the unsupported mucosal wall of the esophagus will tend to enlarge, interfering with the esophageal emptying, and may even become a significant mass in the mediastinum impinging on the airway and causing ventilatory problems (Fig. 40.7a) [13, 17].
Repair requires reestablishment of a full-thickness esophageal wall; however, simple excision of a large diverticulum followed by anastomosis of the esophageal ends may be difficult. Given the tendency of the esophagus to retract, the excision of a 3–4 cm long diverticulum may result in a 6–8 cm gap between the esophageal ends and preclude an anastomosis. This variation of the long-gap problem can be remedied by first inducing growth of the esophagus above and below the diverticulum. Horizontal mattress sutures of 5-0 pledgeted Prolene are placed in the esophageal wall above and below the diverticulum, crossed and anchored either into the paraspinal ligaments or into the chest wall on the other side of the diverticulum. When these sutures are tied, the diverticulum will collapse and the normal esophagus will be stimulated to grow (Fig. 40.8). This approach uses the basic principles of axial tension to stimulate growth combined with not entering the esophageal lumen until one is ready for a primary anastomosis. After 5–7 days of this form of internal traction, a primary esophageal anastomosis will be much easier to achieve (Fig. 40.7b).
When the upper and lower portions of the esophagus are sufficiently close for a full-thickness anastomosis, then the diverticulum can be treated in one of two general ways. If the diverticulum was large, it is better excised. Generous suture bites are taken for the reanastomosis and placed in a Lembert fashion to bring the mucosal edges together (Figs. 40.2 and 40.3). In some cases of a relatively small diverticulum, however, the mucosa may be imbricated carefully with the sutures not entering the lumen. In this situation, the mucosal folds, if relatively small, can be expected to remodel and regress. The holding power will come from generous tissue bites in the esophageal wall as in any anastomosis.
By using one of these methods, a very satisfactory repair can be achieved. This overall approach will have the substantial long-term benefit of avoiding an interposition graft.
The Partially Intrathoracic Stomach
Whether by design to allow a primary anastomosis, or as a consequence of a large esophageal hiatus, from the result of traction sutures used to induce lower esophageal growth or from an esophageal anastomosis under significant tension, the GE junction and part of the stomach may be above the diaphragm. This configuration is detrimental for the long term because it insures GE reflux with its long-term adverse consequences. For the short term which may be 1 or even 5 or even 10 years, this problem may be treated in a symptomatic degree by antacid therapy; nevertheless, the effects of chronic bile reflux will prove to be increasingly detrimental, making unlikely the goal of 70 good years [31]. This unsatisfactory sequence of events will likely also be seen following gastric pull-up procedures, but the return to the abdomen in these cases will require a jejunal interposition to restore continuity.
The difficulty in correcting the partially intrathoracic stomach will be in rough proportion to how much is above the diaphragm. If the stomach has been brought up through the hiatus to allow an esophageal anastomosis, a significant amount may be in the chest. Even an unplanned hiatal hernia, however, may be relatively large and pose problems. Anatomic and physiologic correction will require bringing the GE junction at least 2 cm below the diaphragm, and the esophagus will likely be “too short” for this to be easily accomplished causing a similar deficiency problem as found in long-gap EA.
Two methods have been used by us to return the GE junction below the diaphragm. The first is relatively straightforward and consists of full mobilization of the esophagus and placing a 3-0 monofilament suture superficially around the GE junction. The GE junction can usually be identified by surface characteristics of the esophagus in contrast to the stomach, as well as the presence of a branch from the vagus nerve which crosses the GE junction transversely along with a vein. This localization is important so that the subsequent wrap is around the esophagus and not the upper stomach. With downward traction on the 3-0 Prolene suture, and continued freeing up of the esophagus as it is pulled downward, the GE junction may be brought far enough below the diaphragm to allow a proper fundoplication to be done (Fig. 40.9). After reducing the hiatal opening and completing the wrap, the 3-0 Prolene suture is removed.
Sufficient mobilization of the esophagus may also require reopening the thoracotomy incision and, although this increases the magnitude of the operation, we believe that a partially intrathoracic stomach is so detrimental over the decades that the combined incisions are more than justified to return the GE junction to the abdomen where it belongs.
The second method has not been described to our knowledge and may seem to be unorthodox; however, it is relatively straightforward and effective. This technique can be successfully used when the GE junction cannot otherwise be brought below the diaphragm.
The concept is simple enough. If the GE junction can’t be brought below the diaphragm, the diaphragm can be moved above the GE junction (Fig. 40.10). Normally, the diaphragm dips downward posteriorly with the esophageal hiatus located well below the apex. The diaphragm can be detached along its posterior aspect, and when a sufficient length has been freed-up, it is anchored higher on the chest wall, well above the GE junction with nonabsorbable pledgeted horizontal mattress sutures (usually 4-0 Tevdek). The edge of the diaphragm will need to be split at an angle for a short distance which will place a strip of muscle between the esophagus and the posterior chest wall. The diaphragm will be closed around the esophagus to fashion a new hiatus. The innervation of the diaphragm is from the phrenic nerve which fans out from its central location; therefore, detaching the diaphragm posteriorly will not interfere with function.
This operative maneuver is not difficult, and small, posterior remnants of the crura may be left behind in the abdomen which will indicate the previous location of the esophageal hiatus. With the diaphragmatic opening higher on the esophagus, a fundoplication can be carried out in the usual fashion with the wrap and GE junction within the abdomen (Fig. 40.10).
In contrast to these methods, a partially intrathoracic stomach is in adults commonly treated by a Collis procedure in which the upper stomach is cut downward in the line of the esophagus and the resulting piece of greater curvature used to complete a type of fundoplication below the diaphragm. Obviously, this leaves the true GE junction in the chest along with the length of stomach which remains above the fundoplication. Although this may seem to provide a solution, the presence of gastric mucosa in the chest and the frequent lack of an effective pressure zone producing a physiological GE junction means acid production and reflux will continue to occur. For the long term, this situation will likely be very detrimental, and even the short-term results have been unsatisfactory [32].
Growth Procedure Following Previous Attempts at Repair of Esophageal Atresia
A patient who has had a failed EA repair which has included several operations may have little remaining esophagus. The choice will be between an interposition graft and a growth procedure. Although the prospect for a growth procedure can be daunting, it may still be possible to locate sufficient esophagus to produce an effective growth response, leading to a primary repair with the GE junction below the diaphragm. In such a case, the less desirable interposition may be avoided (Fig. 40.11a, b).
Growth procedure following multiple operations for EA: (a) gastric contrast study of a 2-year-old who after eight operations, including cervical esophagostomy revisions, appeared to have completely lost her lower esophagus. The gap length to the upper pouch was 16.5 cm. (b) At laparotomy, a nubbin of the esophagus was found, and by axial tension, a very satisfactory lower esophagus was grown. The arrows indicate the edges of the new lower esophagus. After a primary esophageal repair, she eats normally
Summary
Reoperation, as discussed in this chapter, may be the best solution to a difficult and persistent problem. Avoiding a reoperation may have its appeal, but postponing effective treatment in these situations may be quite detrimental to the patient. The technical details for the successful treatment of several problems are presented, and, where a significant esophageal gap may result from the procedure, the methods to induce sufficient growth are also discussed. Reoperation, however, requires experience and may be best undertaken at a suitable center, where the approach can be adequately carried out.
References
Leendertse-Verloop K, Tibboer D, Huzebroek FWJ, et al. Postoperative morbidity in patients with esophageal atresia. Pediatr Surg Int. 1987;2:2–5.
McKinnon LJ, Kosloski AM. Prediction and prevention of anastomotic complications of esophageal atresia and tracheo-esophageal fistula. J Pediatr Surg. 1990;25:778–81.
Chittmittrapap S, Spitz L, Kiely EM, et al. Anastomotic leakage following surgery for esophageal atresia. J Pediatr Surg. 1992;127:29–32.
Ein SH, Stinger DA, Stephens CA, et al. Recurrent tracheoesophageal fistulas-a seventeen year review. J Pediatr Surg. 1983;18:436–41.
Ak B, Tam PK. Measurement of gap length in esophageal atresia: a simple predictor of outcome. J Am Coll Surg. 1996;182:41–5.
Borruto FA, Impellizzeri P, Montalto AS, Antonuccio P, Santacaterina E, Scalfari G, Arena F, Romeo C. Thoracoscopy versus thoracotomy for esophageal atresia and tracheoesophageal fistula repair: Review of the literature and meta-analysis. Eur J Pediatr Surg. 2013;22:415–9.
Hagberg S, Rubenson A, Sillen U, Werkmaster K. Management of long-gap esophagus: experience with end-to-end anastomosis under maximal tension. Prog Pediatr Surg. 1986;19:89–92.
Chavin K, Field G, Chandler J, Tagge E, Othesen HB. Save the child’s esophagus: management of major disruption after repair of esophageal atresia. J Pediatr Surg. 1996;31:48–52.
Kovesi T, Rubin S. Long-term complications of congenital esophageal atresia and/or tracheoesophageal fistula. Chest. 2004;126:915–25.
Sistoner S, Koivusalo A, Nieminen U, et al. Esophageal morbidity and function in adults with repaired esophageal atresia with tracheoesophageal fistula. Ann Surg. 2010;251:1167–73.
Spitz L. Oesophageal atresia treatment: a 21st-centruy perspective. J Pediatr Gastroenterol Nutr. 2011;52:S12.
Gaissert H, Grillo H. Complications of the tracheal diverticulum after division of congenital tracheoesophageal fistula. J Pediatr Surg. 2006;41:842–4.
Otte JB, Gianello P, Wese FX, et al. Diverticulum formation after circular myotomy for esophageal atresia. J Pediatr Surg. 1984;19:68–71.
Myers NA, Beasley SW, Auldist AW. Secondary esophageal surgery following repair of esophageal atresia with distal tracheoesophageal fistula. J Pediatr Surg. 1990;25:773–7.
Meier JD, Sulman CG, Almond PS, Holinger LD. Endoscopic management of recurrent congenital tracheoesophageal fistula: a review of techniques and results. Int J Pediatr Otorhinolaryngol. 2007;71:691–7.
Cheng ATL, Gazali N. Acquired tracheal diverticulum following repair of tracheo-oesophageal fistula: endoscopic management. Int J Pediatr Otorhinolaryngol. 2008;72:1269–74.
Siegel M, Sheckelford GD, McAllister WH, Bell MJ. Circular esophageal myotomy simulating a pulmonary or mediastinal pseudocyst. Pediatr Radiol. 1980;136:365–8.
Jaureguizar E, Vazquez J, Murcia J, Diez PJ. Morbid musculoskeletal sequelae of thoracotomy for tracheoesophageal fistula. J Pediatr Surg. 1985;20:511–4.
Kafrouni G, Baick C, Woolley MM. Recurrent tracheoesophageal fistula: a diagnostic problem. Surgery. 1970;68:889–94.
Kiser JC, Peterson TA, Johnson FE. Chronic recurrent tracheoesophageal fistula. Chest. 1972;62:222–4.
Filston HC, Rankin JD, Kirks DR. The diagnosis of primary and recurrent tracheoesophageal fistulas: value of selective catheterization. J Pediatr Surg. 1982;17:144–8.
Hotta Y, Uezono S, Segaw O, et al. Precise localization of a recurrent tracheo-oesophageal fistula using retrograde guide wire placement. Paediatr Anaesthesiol. 2002;12:541–3.
Bruch SW, Hirschl RB, Coran AG. The diagnosis and management of recurrent tracheoesophageal fistulas. J Ped Surg. 2010;45:337–40.
Slim MS, Tabry IF. Left extrapleural approach for the repair of recurrent tracheoesophageal fistula. J Thorac Cardiovasc Surg. 1974;68:654–7.
Smithers CJ, Hamilton T, Jennings R, Foker JE. Operative repair for recurrent tracheo-esophageal fistula. (Submitted; 2014).
Briganti V, Mangia G, Ialongo P. Usefulness of large pleural flap for the treatment of children with recurrent tracheoesophageal fistula. Pediatr Surg Int. 2009;25:587–9.
Best C, Sudel B, Foker JE, Krosch T, Dietz C, Khan K. Esophageal stenting in children: indications, application, effectiveness, and complications. Gastrointest Endosc. 2009;70:1248–53.
Khan K. Endoscopic management of strictures in pediatrics. Tech Gastrointest Endosc. 2013;15:25–31.
Guo W, Fonbalsrud EW, Swaniker F, Kodner A. Relationship of esophageal anastomotic tension to the development of gastroesophageal reflux. J Pediatr Surg. 1997;32:1337–40.
Othersen Jr B, Parker E, Chandler J, Smith C, Tagge E. Save the child’s esophagus, Part II: colic patch repair. J Pediatr Surg. 1997;32:328–33.
Anderson K, Acosta J, Meyer M, Sherman N. Application of the principles of myotomy and strictureplasty for treatment of esophageal strictures. J Pediatr Surg. 2002;37:403–6.
DeMeester TR, Peters JH, Bremner CG, Chandrasoma P. Biology of gastro-esophageal reflux disease: pathophysiology relating to medical and surgical treatment. Annu Rev Med. 1999;50:496–506.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Foker, J.E. (2017). Reoperations After Esophageal Atresia Repair (for Significant Leaks, Recurrent Fistulas, Strictures, Residual Tracheal Pouches, Large Diverticula, Partially Intrathoracic Stomachs, and Failed Repairs). In: Till, H., Thomson, M., Foker, J., Holcomb III, G., Khan, K. (eds) Esophageal and Gastric Disorders in Infancy and Childhood. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-11202-7_40
Download citation
DOI: https://doi.org/10.1007/978-3-642-11202-7_40
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-11201-0
Online ISBN: 978-3-642-11202-7
eBook Packages: MedicineMedicine (R0)