Abstract
The continued rise of prescription drug spend, in particular specialty drugs has created the need for high-quality, low-cost options for biologics. The passage of the Affordable Care Act (ACA) created an FDA approval pathway for biosimilars, but that is the tip of the iceberg as it pertains to how a biosimilar will actually get to the patient. As a general rule, legislation contains very little detail and requires much regulatory guidance by various government agencies to be developed to facilitate a product coming to market. The Centers for Medicare and Medicaid Services (CMS) is the primary federal agency to provide guidance on the Medicare coverage, coding and payment for biosimilars in the US. CMS will also provide some guidance on the use of biosimilars in state Medicaid programs; however, much of that detail will be determined by the state program. Commercial health plans will also weigh in with their own coverage decisions, but typically follow the coding of biosimilars as set forth by CMS. This chapter will assess the existing reimbursement landscape for biosimilars and will address key considerations and implications around current decisions that will impact biosimilars’ market entry in the US.
In many ways, payers, governmental and commercial, will determine the ultimate success of biosimilars in the US by developing benefit designs and provider and patient incentives to drive biosimilar use. This chapter will explore how lessons on biosimilar incentive structures can be gleaned from the European experience and highlight what payer activity we have seen to date with marketed biosimilars in the US.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Medicare
- Medicaid
- Reimbursement
- Biosimilars
- Commercial payers
- Payment
- Coding
- Physicians
- Patients
- Manufacturers
- Interchangeability
- J-code
- Coverage gap
In the US, specialty drug spend continues to increase; a trend which many stakeholders believe is unsustainable to support future innovation. With both the rise in available specialty medications as well as conditions like cancer becoming more chronic, long-term conditions, spending has exceeded targets for the past several years. Additionally, specialty drug approvals by the Food and Drug Administration (FDA) have risen significantly over the past several years, with 2010 beginning the first of several years where the number of approved specialty drugs exceeded traditional small molecule drugs (PwC Health Research Institute 2016). First, let’s begin by defining a specialty drug. A specialty drug is a prescription product that has one or more of the following: special conditions for storage, handling or administration and/or monitoring. Typically, specialty drugs are biologics, injectable or infused, though increasingly they may also be oral (Health Affairs–Health Policy Briefs 2013). In part because of their handling requirements, but also their development, specialty drugs are often more costly than traditional small-molecule drugs. Why is this trend significant to biosimilars? Biosimilars represent the most significant way to increase competition and bring lower cost alternatives to market.
Reimbursement Overview
Reimbursement is a broad term that typically encompasses the coverage, coding and payment for a specific product. It is a critical issue for both specialty drugs broadly and specifically biosimilars. Let’s walk through each component as a foundation of understanding.
Coverage
Typically means any requirements put in place by a health plan or payer that the patient must meet in order to access the drug. Coverage will be primarily determined by the benefit in which it is covered—either the medical or pharmacy benefit (Table 3.1).
Coding
Drug codes can come in a variety of different forms and are the primary communication between the healthcare provider (HCP) and the payer. Codes are used to communicate which drug the patient is receiving.
Healthcare Common Procedure Coding System (HCPCS) Level II codes are used for medical benefit drugs. J-code is the most common of the HCPCS codes used for drugs. J-codes are alpha-numeric, five digit codes that being with “J” and are followed by four numbers. The Centers for Medicare and Medicaid Services (CMS) own the HCPCS coding process, meaning CMS controls the development and implementation of drug-specific coding. All payers—including commercial and Medicaid programs typically follow CMS’ lead on use of J-codes. Typically a product only has one J-code, and it is often designated at the appropriate strength, for example, “1 mg” or “10 mg”level. For example, the J-code for Remicade® is J1745—“Injection, infliximab, excludes biosimilar, 10 mg” (Janssen Pharmaceuticals 2016). Physicians will utilize the J-code and bill the appropriate number of units, utilizing the Remicade example, if the doctor dosed 100 mg, they would bill 10 units.
Pharmacy benefit codes for drugs are different; pharmacy claims typically utilize National Drug Codes (NDCs). NDCs are generated and maintained by the FDA upon approval and/or introduction of new formulations/dosing. NDCs are very specific and a single drug can have multiple NDCs underneath them based on the number of available products.
Payment
Payment is perhaps the most critical component of reimbursement; however, the first two components ultimately drive the accuracy and timeliness of a payment.
Payment for medical benefit drugs encompasses two components: (1) what the HCP is paid and (2) what the patient owes. As outlined in the table above, typically payment for medical benefit drugs is based on ASP. ASP is based on a series of data points including rebates and discounts and is updated quarterly by CMS. Manufacturers of medical benefit drugs submit quarterly information to CMS and CMS releases a file of all medical benefit drugs with ASPs. Similar to the coding process, CMS owns this calculation process; however, other payers including commercial and Medicaid programs utilize ASP to pay for products.
Patients cost share will be highly dependent on their specific plan. However, typically medical benefit cost-share is a percentage—example, 20% is owed by the patient for in-network drugs and services.
Payment for pharmacy benefit drugs is similar with two main components: (1) what the pharmacy is paid and (2) what the patient owes. Pharmacy benefit drugs are typically based on a negotiated price (e.g., rebates and discounts) between the payer (or pharmacy benefit manager—PBM) and adjudicated upon the pharmacy submitting the claim for payment. This is the general process whether it is retail or SP submitting the claim.
Patient cost-share depends on a variety of factors—including tier placement and benefit design. For small molecule drugs—the patient will typically pay a flat copayment amount determined by tier (e.g., tier 1: $5; tier 2: $20). Increasingly, high-cost, specialty drugs covered on the pharmacy benefit require a coinsurance from the patient. Coinsurance is often based on the list-price (or WAC), which is pre-discounts. So a patient could have a 20% coinsurance monthly on a specialty medication until they hit their annual out-of-pocket (OOP) limit for the year. Coinsurance can be quite costly for patients who are also juggling coinsurance on any medical benefit services or drugs as well.
In summary, reimbursement is a complex set of considerations and highly dependent on the payer and their requirements.
Medicare Reimbursement and Biosimilars
Now that we have a basic foundation for reimbursement in the US system, it is time to dive into biosimilar reimbursement considerations by payer. In many ways, CMS is a top decision-maker in terms of reimbursement policy for biosimilars.
Medicare Part B
Medicare Part B is the benefit that covers services within the physician office and hospital outpatient setting. Additionally—as discussed, the Part B benefit includes payment for physician-administered drugs that are administered in either the physician office or hospital outpatient department.
Coverage
As with other parts of Medicare, CMS national provides regulatory guidance to its’ Medicare Administrative Contractors (MACs) who are responsible for actually managing, processing and paying claims for both Medicare Parts A and B. There are 12 MACs who are multi-state and regionally based. MACs however, do not act as a traditional payer in the sense that they have very limited ability to restrict or manage access to drugs or services, but in particular to drugs. As such, as long as a drug meets the requirements outlined below, it is eligible for reimbursement under Part B (Fig. 3.1).
ADVI Health, 2017
Coding
As discussed previously, CMS controls the assignment of HCPCS codes for physician-administered drugs. Through a combination of legislation (e.g., the Social Security Act (SSA) section 1847a) and regulation, CMS has developed a series of interpretations which guide their coding process. For new brand products, CMS generally considers them to be “single-source” products and therefore assigns a unique J-code and payment rate to those products. The HCPCS process for assigning J-codes is an annual process with CMS assigning codes mid-year with the codes taking effect the following January. Notably, outside of the formal HCPCS process, CMS can assign a “Q-code” which is situated like a J-code, but is typically designed to be a temporary code for a drug or service.
In the CY2016 Medicare Physician Fee Schedule (MPFS) proposed rule, released in July 2015, CMS surprised many stakeholders by establishing a coding and payment policy for biosimilars. At this point, there was only one approved, unlaunched biosimilar in the market, Zarxio® (filgrastim-sndz) by Sandoz. In the proposed rule, CMS outlined that for the purposes of coding and payment, CMS would consider biosimilars utilizing a generic-drug framework, as “multi-source” drugs and therefore, all biosimilars for the same reference product would share a J-code and a blended ASP-based payment rate. At the same time, reference products would retain their own separate J-code and payment rate. In the proposed rule, CMS sought public comment on this proposed policy. CMS received many comments on this policy, the vast majority of which stood in opposition of this policy. Opposition was heard from physician groups, patient advocacy groups, Congress (Biosimilar Development 2017a), commercial payers and manufacturers. In November 2016 in the final CY2016 MPFS, CMS opted to finalize this policy and it took effect January 1, 2016. Interestingly, CMS has actually yet to assign any J-codes for biosimilars, only Q-codes have been assigned.
The launch of Renflexis™ (infliximab-abda) the second biosimilar to reference product Remicade®, put this policy into play in July 2017. Since Inflectra® (infliximab-dyyb) the first biosimilar to Remicade launched in October 2016, there was an established Q-code. Presumably, now that Renflexis™ has launched, all claims for both Remicade® biosimilars will be submitted utilizing Q5102, the Q-code first assigned to Inflectra®.
In conjunction with finalizing its’ policy for blended J-codes, CMS noted that the tracking concerns (described below) of a blended J-code warranted some type of a solution. CMS decided to establish a series of manufacturer-specific modifiers that will be required to be appended to the claim form when a biosimilar claim is submitted (Centers for Medicare and Medicaid Services 2018a) (Table 3.2).
Stakeholder Considerations on the Blended J-Code Policy
While CMS did finalize the policy in November 2015, several key groups of stakeholders continued to express concern over the policy.
Physicians
Physicians who bill Medicare Part B are required to “buy and bill” the products—meaning they purchase the product and bill Medicare upon administering it. This creates some interesting dynamics if the ASP of a product changes between the time they bought it and the time they bill Medicare (described in more detail below). This dynamic was likely to be a concern to physicians and could have resulted in driving them away from the instability of a blended reimbursement in favor of the reference product, which under existing policy is protected from these dynamics.
Patients
The concern for patients, who are typically immune from any issues related to coding of drugs, is that under the policy, CMS is treating all biosimilar products equal. This ignores the potential variability in clinical profiles between biosimilars. The absence of product-specific J-code for each biosimilar could potentially hinder pharmacovigilance efforts designed to support patient safety.
Other Payers
As discussed, the assignment of HCPCS codes is managed by CMS. As such, commercial (including the Exchanges) and Medicaid payers are beholden to CMS coding decisions. A primary concern for payers is that they are unable to effectively manage and/or implement product preferencing across biosimilars, because they all shared a code. This could limit commercial and Medicaid payers from being able to drive biosimilar uptake at the product level, they could only push biosimilars at the class level. This is likely not considered an ideal situation for payers, particularly as they continue to try to bend the cost curve associated with costs. Additionally, physician and patient concerns outlined above are relevant across all payers, not just Medicare.
Manufacturers
Manufacturers, particularly those investing in biosimilars came out very strongly against the CMS coding and payment policy for biosimilars. That is primarily related to the investment required to make biosimilars. A generic drug typically takes 3–5 years to develop at a cost of $1–$5 M. However, a biosimilar takes 7–10 years to develop at a cost upwards of $200 M (FTC 2009). The differences in time and cost reflect the complexity and increased analytical and clinical data requirements for a biosimilar compared to a generic drug. As such, it is concerning that CMS applied the same coding and payment methodology to generics and biosimilar products when they are vastly different.
2018: A New Coding and Payment Policy Will Emerge
In July 2017, in the CY2018 MPFS proposed rule, CMS re-opened its’ controversial coding and payment policy for biosimilars by seeking public comment. CMS received over 200 public comments, the majority of which asked the Agency to overturn the blended coding policy. As outlined above, given that number of stakeholders who opposed this policy, the outpouring of opposition was not surprising. In November 2017, CMS reversed the coding policy and stated (Centers for Medicare and Medicaid Services 2017b):
Thus, in this final rule, we finalizing the policy to separately code and pay for biosimilar products under Medicare Part B … Effective January 1, 2018, newly approved biosimilar biological products with a common reference product will no longer be grouped into the same HCPCS code.
In the final rule, CMS reviewed many of the arguments presented by commenters and concluded that the concerns around the long-term sustainability of the market were the most compelling to drive a policy change (Centers for Medicare and Medicaid Services 2017b).
… We have also considered how the payment policy could affect market entry of new biosimilar manufacturers. If payment amounts limit manufacturers’ willingness to invest in the development of new biosimilars, it could in the long term, decrease the number of biosimilar biological products that are available to prescribe and thus impair price competition. Given that the United States’ biosimilar biological product marketplace is still relatively new, we believe that it is important to maintain a payment policy innovation as well as reasonable pricing for consumers … We believe that this policy change will encourage greater manufacturer participation in the marketplace and the introduction of more biosimilar products, thus creating a stable and robust market, driving competition and decreasing uncertainty about access and payment …
In Q1 2018, CMS released guidance that included new instructions to MACs on appropriate coding for biosimilars and provided new, separate codes for Inflectra(R) (Q5103) and Renflexis(R) (Q5104). Source: https://www.cms.gov/apps/ama/license.asp?file=/Medicare/Medicare-Fee-for-Service-Part-B-Drugs/McrPartBDrugAvgSalesPrice/Downloads/2018-Oct-ASP-Pricing-File.zip
Payment
As outlined above, the payment dynamic in Medicare is such that it can create perverse financial incentives due to the financial realities of the buy and bill landscape. The Medicare Modernization Act (MMA) of 2003 ushered in the ASP payment system into Medicare. The primary reason for changing to ASP was because of concerns around abuse of the average wholesale price (AWP) methodology. The goal of the ASP system was to develop a transparent, public system and take into account other rebates and discounts so the ability for physicians to make money on drugs via buy and bill was limited. Currently, in both the physician office and hospital outpatient department, Medicare pays for physician-administered drugs at ASP +6%. For biosimilars, Congress mandated that they be paid at the same rate, except that the 6% comes from the reference product ASP, this was designed to be a physician incentive to utilize biosimilars (Figs. 3.2 and 3.3).
ASP calculation and timing (ADVI Health 2017)
Quarterly payment for drugs reflects 2 quarter lag (ADVI Health 2017)
The ASP system comes with its’ own challenges for physicians, the most significant of which is the 2 quarter lag that is associated with payment. While manufacturers submit their data quarterly, the published ASP is always based on 2 quarters prior, to allow CMS time to actually manage the data as evidenced above.
It is possible that by the time a drug is administered, the ASP of the product has changed and the physician may be financially “underwater” on the drug, meaning they will get reimbursed less than what they paid for. This dynamic can occur with any drug, but the risk was set to be further multiplied when there were multiple drugs blended into one code. With the revision to the coding policy, biosimilars will be assigned their own payment rate and thus mitigate some of the concerns around being financially underwater.
In summary, biosimilars could be a very promising development to curb costs for Medicare Part B. The changes to the coding and payment policy are anticipated to generate a more sustainable and competitive long-term biosimilar market in the US which will help curb costs.
Medicare Part D
Medicare Part D is the newest benefit within Medicare. The MMA of 2003 which ushered in ASP payment in Part B, also included the development of a prescription drug benefit in Medicare, known as Medicare Part D. Prior to this, there was no coverage for pharmacy benefit drugs in Medicare. Part D is administered by private health plan companies that form their own formularies but CMS national sets certain rules. Part D plans must cover two drugs per USP class/category and cover substantially all drugs in the six protected classes.
CMS has review and oversight of the formularies, but plans can make positive formulary changes (e.g., removing a utilization management tool, decreasing cost-sharing and/or lowering tier placement) any time of year without CMS permission. However, plans are not permitted to make “negative” changes during the benefit year without CMS approval. Additionally, CMS sets forth specific review period, timelines and an appeals process that all Part D plans have to follow.
When Part D was established, it included a provision called the “coverage gap” also referred to as the “donut hole.” The coverage gap is a period of time where patient cost-share is significantly higher than other phases of coverage. The original intent of the coverage gap was (1) to keep the cost of implementing Part D low and (2) to ensure patients have “skin in the game” when it comes to paying for their medicines. Annually, CMS sets the monetary threshold for the coverage gap, referred to as the patients true-out-of-pocket or TrOOP. The figure below illustrates the dollar thresholds for the coverage gap in 2017 (Fig. 3.4).
Overview of Part D coverage gap (ADVI Health 2017)
Low-income subsidy patients do not ever hit the coverage gap, the coverage gap is applicable only to those patients who have not received the LIS subsidy or are dual-eligible (e.g., eligible for Medicare because of age/disability and Medicaid due to low income).
The last important facet of the coverage gap is the ACA-mandated creation of the Coverage Gap Discount Program (CGDP). As a result of the coverage gap thresholds increasing every year and the concern of the financial strain it puts on patients, most of whom are on a fixed income, the ACA included the CGDP provision to help patients through this phase of coverage. The CGDP included a provision that requires the manufacturer of brand products to pay a 50% rebate on their drug while the patient is in the coverage gap. Thus, in 2017, during the coverage gap for a brand product, the manufacturer pays 50%, the patient pays 40% and the plan pays 10%. Additionally, the 50% rebate paid by the manufacturer counts towards the patients TrOOP. By 2020, the coverage gap “closes” meaning it equalizes patient cost-share to a consistent level of 25% throughout the year until the patient hits catastrophic coverage (in 2017 that dollar amount is $4950).
The reason why the coverage gap and the CGDP are so critical to biosimilars lies within the text of the ACA. The text of the CGDP excludes both generic and biosimilar (any products approved under the 351k pathway) products. For generic products, which are typically very low cost, this is a logical exclusion—a manufacturer wouldn’t need to pay a 50% rebate on a very low cost drug. However, it is an entirely different consideration for biosimilars. Even if biosimilars come in at a significant discount, that may still be a discount on a relatively high priced product to begin with, so it is entirely possible a discounted biosimilar could be several thousand dollars. Therefore, the exclusion of biosimilars from the CGDP is very concerning for both patients and Part D plans.
What Does this Mean for Patients? (Biosimilar Development 2017b)
-
The impact of biosimilars being excluded from the CGDP is twofold for patients:
-
They face a higher cost share for a biosimilar
-
They remain in the donut hole longer
-
-
While the patient is in the donut hole, the 50% manufacturer rebate on branded drugs counts toward the patient’s TrOOP costs, thus moving the patient through the donut hole faster and helping to reduce the cost to patients.
-
Since biosimilars are excluded from the CGDP, any discount offered to the plan on the biosimilar would not count toward TrOOP and therefore, the patient has both higher cost share and is in the donut hole longer than if they were on a branded drug.
-
Notably, the coverage gap closes for patients in 2020; patients will pay 25% of the cost of a branded or generic/biosimilar drug once they reach the coverage gap. However, the impact to TrOOP will still result in the patient being in the coverage gap longer if they take a biosimilar.
What Does this Mean for Part D Plans?
-
The impact of biosimilars being excluded from the CGDP is:
-
As evidenced in Fig. 3.1 below, the cost of the biosimilar will be higher to the plan through 2020 and beyond:
-
Plan responsibility for a brand product in the donut hole in 2020: 25%
-
Plan responsibility for a generic product in the donut hole in 2020: 75%
-
-
-
The result of this policy makes it potentially very unlikely for a Part D sponsor to push the use of biosimilars under Medicare Part D
Figure 3.5 illustrates how the exclusion of biosimilars from the CGDP is an immediate concern for patients through 2020 and remains a concern for health plans:
Solutions have been suggested though not implemented. In April 2016, Avalere Health conducted an independent analysis on this topic and outlined two potential solutions (Avalere Health 2018):
-
Allow biosimilars to participate in the CGDP and pay the 50% rebate
-
Allow CMS to create a new biosimilar tier (and necessary program rules) to give Part D plans flexibility on how they manage (e.g., coverage, specify cost share, etc.) biosimilars
Note that either change requires legislative action. While both represent potential solutions, the first is the more likely and timely solution as it can be utilized for approved, but not-yet-marketed, biosimilars under Medicare Part D. As the U.S. biosimilars market is in its infancy, reimbursement policies to appropriately support their use are essential, and CMS is positioned to play a pivotal role in the development of these policies. Addressing the coverage gap in Part D is a critical place to start.
In November 2017, CMS released an off-cycle proposed rule pertaining to CY2019 Part D and Medicare Advantage. In the rule, CMS proposed changes to cost-sharing levels for biosimilar (Centers for Medicare and Medicaid Services 2017c). CMS proposed increased flexibility for plan sponsors to categorize biosimilars as generics for the purposes of cost-sharing:
-
For Low-Income Subsidy (LIS) patients—throughout the plan year
-
For non-LIS beneficiaries—during the catastrophic phase of coverage
CMS finalized this policy in early 2018, these provisions provide Part D plans the flexibility to drive biosimilar utilization.
In February 2018, a provision was included in the Bipartisan Budget Act of 2018 to make biosimilars "applicable drugs" for the purposes of the Coverage Gap Discount Program effective January 1, 2019. This change is significant for biosimilars to be on a level playing field with the reference product.
Medicaid Reimbursement and Biosimilars
With the expansion afforded by the ACA, Medicaid programs have expanded significantly since 2014. As of May 2017, approximately 68.8 M individuals were enrolled in Medicaid (another 5.7 M were enrolled in the Children’s Health Insurance Program [CHIP]), this is an increase of approximately 17 M since the implementation date of the ACA-included expansion (Centers for Medicare and Medicaid Services 2018b). To-date 32 states including Washington DC expanded their programs under the ACA. Expansion allowed states to expand to both a higher income threshold as well as a new population of childless adults.
Medicaid is a jointly-funded program between the federal government and states. The Federal Medical Assistant Percentage (FMAP) determines the share of each state’s Medicaid expenditures that are funded by the federal government. FMAP is determined based on the states average income to the national personal income average. FMAP varies based on state income and reevaluated every 3 years. States have the flexibility to determine where non-federal funding for Medicaid comes from, but generally it comes from state appropriations. As it relates to ACA expansion, states who opted to expand were able to capture 100% of the costs of the new population via FMAP funds. By 2020, the FMAP for this population will decrease to 90%.
As it relates to prescription drugs, all Medicaid programs offer prescription drug benefits despite that not being a required benefit in statute. An important component of prescription drugs in Medicaid is the mandated Medicaid Drug Rebate Program (MDRP). The MDRP requires manufacturers to pay statutorily mandated rebates on all prescription drugs. The ACA increased the mandated rebate for drugs to 23.1% as compared to 13% for generic drugs (Centers for Medicare and Medicaid Services 2017d). Over 600 manufacturers currently participate in the MDRP and participation in the MDRP also extends to two other federal pricing programs: the 340B drug pricing program and the Federal Supply Schedule operated by the Department of Veterans Affairs. The MDRP also requires drug manufacturers to provide the Medicaid program with the lowest price they offer across the marketplace, otherwise known as “Medicaid Best Price.” Prior to this being codified in law, health maintenance organizations (HMOs), hospital systems and group purchasing organizations (GPOs) were able to negotiate deep discounts in the 1990s, often deeper than Medicaid programs. Therefore, Congress established the Best Price mandate in the Omnibus Reconciliation Act of 1990 (OBRA ’90).
In addition to the mandated rebate, brand drugs also face a Consumer Price Index-Urban (CPI-U) adjustment. For products on the market for several years that have taken price increases regularly, can essentially be at a very high rebate level once the 23.1% plus the CPI-U adjustment is taken. Thus, Medicaid programs have a variety of brand drugs they receive at a very high rebate. The other dynamic relevant to prescription drugs in Medicaid, though not mandated in statute, is the inclusion of supplemental rebates. States can negotiate with drug manufacturers to generate additional rebates and further reduce expenditures. Supplemental rebates are reported back to the Federal government on the basis of the FMAP amounts. States can enter into supplemental rebates alone or in conjunction with other states (Department of Health and Human Services 2014).
Medicaid programs establish Preferred Drug Lists (PDLs) which are their version of formularies that spell out products that are covered and utilization management tools applied. Since Medicaid eligibility is based on an individual being low-income, there are very low copayments assigned to drugs—and many Medicaid programs do not even collect these due to the burden on patients. As such, the PDL is the primary way Medicaid programs control access and spending.
The last and relevant component of Medicaid is the influx of Managed Care Organizations (MCOs) infiltrating what was traditionally a state-run program. Traditional MCOs typically have more sophisticated tools and approaches to manage spending, so increasingly MCOs have entered into contractual relationships with state programs to control escalating expenditures. Currently, 39 states controls with MCOs and in 2014, nearly 55 M individuals had some aspect of their care touched by an MCO (Centers for Medicare and Medicaid Services 2018c). With the continued proliferation of MCOs in Medicaid, referred to as Medicaid Managed Care, the ACA included provisions to allow MCOs to keep supplemental rebates they negotiate with drug manufacturers.
As it pertains directly to biosimilar reimbursement, these considerations are critical. In March 2015 and reaffirmed in 2016, CMS notified manufacturers that for the purposes of the MDRP, biosimilars will be considered single-source, brand drugs, and therefore, responsible for the 23.1% mandated rebate (Centers for Medicare and Medicaid Services 2016) as well as any supplemental rebates. This of course is direct opposition to CMS’ treatment of biosimilars within Medicare Part B, where biosimilars are considered “multi-source” and in Part D, where biosimilars are “non-applicable” drugs.
Outside of CMS’ interpretation of biosimilars within Medicaid, is the reality of how the reference products are currently rebated and covered under Medicaid. Since many products that are likely to have a biosimilar competitor have taken price increases and been on the market for several years, it is entirely possible that products will be highly rebated and/or at 100% rebate. Therefore, biosimilar penetration could be very challenging in state Medicaid programs as Medicaid programs may not want to give up that rebate for the reference product, and/or it does not make financial sense for them to do so.
Coverage and payment for physician-administered drugs (or Part B drugs) in Medicaid varies significantly from program to program. But effective in 2006, states were required to collect specific information on physician-administered drugs to collect rebates. While coverage and reimbursement methodology varies across programs, since physician-administered products are required to pay the same rebates as self-administered drugs, the dynamics of products that are at a high level of rebate with biosimilar competition will face the same complexities in getting traction long-term. Currently, many Medicaid programs also utilize the ASP methodology established by Medicaid, though it is up to the individual program to determine the additional percentage they pay above the 6%, if any. As discussed earlier, state Medicaid programs are also beholden to the CMS coding decision for biosimilars, thus there will be limited ability for a state Medicaid program to do any product preferencing since all products are blended into one code currently.
In summary, the dynamics of the MDRP may mean biosimilar utilization in Medicaid programs is low compared to other government programs; quite ironic given that Medicaid is for low-income individuals who could benefit from a lower cost option.
Commercial Reimbursement and Biosimilars
Given the continued rising spend on specialty drugs, commercial payers have long supported the proliferation of a robust biosimilar market in the US. And while the potential cost savings associated with biosimilars is undoubtedly attractive to payers, like most things reimbursement-based, complexities around the clinical and financial considerations loom large.
As discussed in Chap. 5, the purpose of the biosimilar pathway is not to independently prove safety and efficacy, but rather to prove biosimilars are highly-similar to the reference product, with no clinically meaningful differences. Stakeholder lack of familiarity relating to biosimilars and potential concerns will be top of mind for commercial payers as they consider aggressive moves towards biosimilars. Table 3.3 below illustrates the top pharmacy benefit managers (PBMs) moves on biosimilars for 2018 formularies:
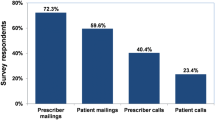
To date, payer activity has been slow; however, there remains a limited number of biosimilars launched, so it is not unexpected. Recent payer research illustrates that commercial payers are relatively open to incorporating biosimilars into their formularies. Recent research indicates payers expect biosimilars to be priced at a 20–30% discount (Covance Inc 2014).
The financial considerations for a commercial payer around biosimilars will vary significantly by the benefit where the product is covered, therapeutic area and existing marketplace considerations. Some areas, like immunology, have many brand options and thus are inherently competitive from a payer perspective in terms of rebates and/or discounts being offered. This is particularly prevalent for pharmacy benefit products. The medical benefit of commercial payers still remains less competitive in terms of rebates/discounts and is more driven by physician choice versus payer influence. Commercial payers will most certainly consider the economics of rebates lost from the innovator compared to rebates gained from a biosimilar manufacturer as they evaluate biosimilar inclusion in formulary decisions.
Physician acceptance of biosimilars is likely to also influence commercial payer considerations around biosimilars. For example, although payers have tools in their arsenal to push utilization of biosimilars, physician acceptance will still be critical. Commercial payers rely on physicians to drive their formulary choices and buy into those choices, as not to create disruption at the provider or patient level. This concept will remain especially critical when it comes to a new market like biosimilars.
Patient acceptance is also critical for commercial payers to consider. While payers can look at a variety of utilization management tools; patient cost-share changes may be the most powerful to drive biosimilar utilization. However, this will depend significantly on the therapeutic area and what the patient responsibility has been for the brand product. Some areas like immunology have had a competitive landscape with many brand products competing for market share. As such, copay cards which insulate patients from payer-mandated coinsurance or higher copayment amounts, have been prevalent. Thus, a payer may have limited means to drive biosimilar utilization due to changing of copay or coinsurance structure of a brand product. Brand companies are unlikely to forgo copay cards in light of biosimilar competition.
In summary, commercial payers will play a critical role in the uptake of biosimilars moving forward in the US. Early activity shows payer interest remains high particularly among the big three PBMs in the US. However, it is not as simple as lower price equals payer utilization, the financial picture is complex and payers do have to consider the level of disruption they are willing to put forth on physicians and patients. Lastly, as discussed earlier, commercial payers are beholden to the CMS coding decision for biosimilars, thus there will be limited ability for a commercial payer program to do any product preferencing since all products are blended into one code currently.
Spotlight on the European Experience
By: Jennifer Cook, Global Market Access lead, Biosimilars, Boehringer Ingelheim GmbH Jennifer.cook@boehringer-ingelheim.com
Relative to Europe, who has had biosimilars since 2006 and over 20 launched; the US market is very young in having biosimilars experience. It begs the question, are there lessons we can learn from the European experience around reimbursement policy?
Biosimilar Experiences in Europe So Far: Lessons Learned
Since 2006, European countries have approved 36 biosimilars, accumulated over 700 million patient days on therapy and realized significant savings (European Medicines Agency 2017). Biosimilars in the US is still in its relative infancy; how they will affect the rising spend of biologics in the US remains to be seen.
While the European and US regulatory environment share many similarities related to biosimilars, including the approach for demonstrating similarity and the extrapolation of indications, the marked differences in how drugs are purchased, priced, and distributed makes it difficult to fully extrapolate Europe’s experience to the US. However, there are valuable experiences from the intended and unintended impact of various pricing and market access (P&MA) policies that have been implemented across Europe to date.
Discounting biosimilars is one way to affect the adoption rates, however evidence shows that that tailor made payer policies that address the specific market characteristics and needs of the payer, provider and pharmaceutical companies are essential to drive uptake and foster a more sustainable market. A recent study by Rémuzat et al. (2017) looking at the key drivers for market penetration in Europe has shown that incentive policies to enhance uptake remain an important driver of biosimilar penetration, while biosimilar price discounts have no impact on share.
An overview of the policies that have been introduced across selection European countries can be seen in Table 3.4.
European Policies: Those Driving and Not Driving a Competitive Biosimilar Market
Germany: Driving
We have seen varying levels of uptake of biosimilars by country and by product across Europe. Let’s take a look at Germany; a country where biosimilar adoption has been relatively strong, Filgrastim, a physician-administered product for mostly acute use, and thus largely a payer-driven therapy selection, the uptake of biosimilars has been greater than 50%, while for somatropin, a chronic treatment where therapy selection is largely driven by patients and providers, uptake has been quite limited. Across Europe, Germany has seen the greatest incentives to drive biosimilar use. The statutory health insurers (Gesetzliche Krankenversicherung) officially called “Sickness funds” (Krankenkassen, KKs) and physician’s associations (Kassenarztliche Vereinigung, KVs) have been pro-active in reaching out to physicians in order to encourage them to prescribe biosimilars and meet their prescribing targets as well as their regional biosimilar quotas, which can be as high as 50% relative to originator biologics to new patients. This has been supported by education campaigns, highlighting the savings potential of biosimilars (IMS Health, 2016a, b). However, the lack of monitoring has meant that up until now, many of the German KV regions have not met their biosimilar quotas, leaving room for improvement.
From a procurement perspective, the Sickness funds (Krankenkassen) in Germany have ‘open house rebate contracts’ with pharmaceuticals. The Sickness funds negotiate rebates to reduce net price in return for agreed market shares with the manufacturer. This challenges the possible price advantage of biosimilars vs originator on the net level. In addition, theFederal Joint Committee (GBA)) along with the National Association of Statutory Health Insurance Funds (GKV-Spitzenverband) has also instituted reference pricing for biosimilars further reducing the price advantage of biosimilars vs originator on the list price level.
UK: Driving
Adoption of biosimilars has been amongst the highest in the United Kingdom (UK). For example Benepali, a biosimilar of Etanercept (launched in March 2016), achieved 52% biosimilar volume market share just after 14 months and the uptake was significantly faster than Infliximab biosimilar (39% biosimilar volume share after 14 months).
Biosimilars in the UK are procured through regional tenders, and adoption has been greater in regions where financial incentives in place e.g. gain share agreements that rewards cost effective prescribing. Any savings which are generated through the implementation of the biosimilars are split between Clinical Commissioning Groups (CCGs) who are responsible for funding and the hospital responsible for prescribing. However, this is not yet a wide spread phenomenon in the UK due to administrative burden and the complexity of splitting the savings generated between CCGs and hopsitals.
In 2015, NICE (National Institute of Health and Care Excellence) imposed guidelines recommending the use of more cost-effective drugs, and as part of their Health Technologies Adoption programme, NICE developed a step by step guide for clinical and non-clinical staff on how to facilitate use of biosimilars to Infliximab (Inflectra® and Remsima®), including practical advice on topics like patient identification, switching, monitoring and project management (NICE 2015).
Over the last few years, with the increase number of biosimilar players coming onto the market, we have seen increasing levels of discounts required on the net price level, reducing the attractiveness of the market for pharmaceutical companies.
France and Belgium: Not Driving
Biosimilar adoption in France and Belgium has been the lowest across Europe. Price is currently the main driver for biosimilar access. Both countries have a national management process i.e. fixed biosimilar price reduction. Furthermore, in the retail setting; France has introduced mandatory list price discounts which are not balanced by P&MA policies to drive the use of more cost effective treatment options impeding the use of biosimilars (Medicines for Europe 2016). In the hospital setting, they have introduced the gainsharing (T2A drugs) to facilitate broader use of biosimilars. However, to date on the prescription side there has been no payer guidance, prescribing incentives or quotas to incentivize physicians to prescribe biosimilars. Physicians typically base their prescription decision on the hospital formulary.
Italy and Spain: Not Driving
Despite the initial cultural resistance, Italy and Spain are now catching up. In Italy, regional and local quotas/usage guidelines are already in place for existing biosimilars (filgrastim, somatropin, epoetin) in Tuscany, Veneto and Campania. However, as in Germany, the quotas are not legally binding, and so far, real-life prescribing is not fully reflecting the regional quotas that have been set.
Biosimilars for somatropin, epoetin, filgrastim, and infliximab are currently purchased in regional or local/hospital tenders in Italy and Spain. However, the single-winner tenders, as well as the mandatory price discounts on the list price, limits the flexibility for pharmaceuticals to negotiate the price (9). This creates an unfavourable procurement environment reducing the commercial attractiveness for manufacturers who are looking to invest longer term.
Norway: Driving Short-Term but Long-Term Remains to Be Seen
Discount levels in Norway is the highest we see in Europe. Earlier this year, Orion won the Norwegian market for infliximab with a 72% price reduction for the biosimilar Remsima®. Other examples can be seen with epoetin and filgrastim that are used for in-hospital treatment (paid by the regional health authority) and by patients at home (paid for by national insurance). Tender prices of biosimilars of these two products are discounted up to 89%, with a high volume of sales to hospitals (Mack 2015). Despite these high levels of discounts, sales of epoetin and filgrastim are still not comparable to sales of biological drugs that do not have biosimilar competition, such as pegfilgrastim and darbepoetin, which dominate the market suggesting there are other factors at play.
Norway has a national healthcare system which is centralized and highly integrated. The Norwegian Drug Procurement Cooperation (LIS) is responsible for procurement and delivery agreements for pharmaceutical manufacturers in cooperation with state-owned hospitals, thereby reducing costs through a national tendering process. The Norwegian authorities pay for the bulk of drugs through national insurance and hospitals (regional health authority budgets).
Infliximab has had a more rapid penetration into the market than other biosimilars available in Norway. Several factors have contributed to this. The national annual tender processes for tumour necrosis factor (TNF) biosimilar drugs (infliximab) has been running at the LIS since 2007, therefore the process is well established. A key factor was that the specialists, clinicians and hospital management all supported the recommendations from a clinical and economic perspective. Furthermore, its low price puts Remsima® at the top of the ranking for all its in-hospital treatment indications. The drug costs for in-hospital Remsima® are much lower than are the drug costs for home treatment with injectable products, which resulted in a larger proportion of treatments being carried out in hospitals where the switching of patients to biosimilars is also widely accepted and common practice. Therefore, is a great example demonstrating factors including healthcare systems specificities in terms of pricing, reimbursement, procurement in addition to payer policies that meet the needs of the physicians and patients are all necessary components to promote uptake.
Interchangeability
The EU regulatory path has no separate development for interchangeables and leaves biosimilar substitution up to the individual member states. As such, each European country adopts biosimilars differently as we have discussed here, most without allowing automatic substitution. The exception is now France, which recently passed a law allowing substitution by pharmacists, but only for treatment-naïve patients. Germany is also expecting the introduction of automatic substitution in the future. Currently, there is convergence across EU countries that biologic medicines should not be substituted at the pharmacy level without the involvement of the clinical decision maker. The lack of interchangeability in many EU countries has been a natural barrier to biosimilar adoption, and as a result, biosimilars haven’t yet eroded the EU market share of several reference biologics as fast as many experts had expected.
In summary, the experiences so far with Biosimilars in Europe illustrate the heterogeneity between biosimilar products, therapy areas, and countries (both across and within). There is not just one formula that will work to achieve the projected savings potential, but learnings can be taken from all areas as evidenced below (Fig. 3.6).
Reimbursement Landscape Moving Forward
The key question behind all of the considerations laid out in this chapter is—in a time of significant change in the US healthcare system, what does this mean for biosimilar utilization long-term?
The US is quickly trying to move away from the fee-for-service (FFS) model to a more value-based approach to delivering and paying for healthcare. This shift is taking many forms across all payers and is primarily driven by concerns around rising costs of care, FFS incentives driving overuse and continued concern that growing expenditures do not reflect quality of care.
The federal government has actually been an early mover in driving the shift. In January 2015, then HHS Secretary Sylvia Burwell announced very ambitious targets for value-based payment:

While the goals were initially suggested to be very ambitious for a government agency; HHS succeeded by hitting these goals, early, in March 2016; 9 months ahead of schedule. A division within CMS, the Center for Medicare and Medicaid Innovation (CMMI) was established via ACA to develop, test and implement APMs to drive savings and improve quality. To-date, CMMI has over 80 programs being tested and many were instrumental in HHS hitting its’ goal to move towards quality and value.
In addition to federal activity, commercial payers are also doing a lot to drive the shift away from FFS. As it pertains to biosimilars, in theory, biosimilars fit very well into the idea of improving value and reducing cost. After all, the value equation in healthcare is fairly straight forward, value = quality divided by cost. The higher the quality the more improved the value. Biosimilars represent the opportunity for sustained quality at a lower cost.
Additionally, as APMs further take shape, biosimilars fit very well into more episodic-based models. Biosimilars aim to provide the same safety and efficacy, at a lower cost, thus they should be a natural fit within evolving payment models. In addition to APMs, the shift away from FFS has also ushered in an influx of value frameworks – or entities evaluating the value of medicines in a more complex and methodological way. The Institute for Clinical Effectiveness and Research (ICER), NCCN, ASCO and Memorial Sloan Kettering Cancer Centers have all created tools to further define the “value” of products. Again, in a biosimilar market where biosimilars come in at a discount to the reference product, the value of biosimilars should be high. Thus, market forces are driving towards reimbursement for high-value products, and it would seem biosimilars fits into this movement quite well.
In final summary, the reimbursement landscape for biosimilars is complex and in some areas requires changes to ensure a long-term robust and sustainable market. However, biosimilars represent an opportunity to help curb drug costs. As such, an appropriate reimbursement framework that encompasses coverage, coding and payment is mission critical for the US to see a sustainable, robust biosimilar market.
References
ADVI Health. July 2017.
Avalere Health. Medicare beneficiaries will pay more for biosimilars than for their biologic reference products in Part D. 2018. http://avalere.com/expertise/life-sciences/insights/medicare-beneficiaries-will-pay-more-for-biosimilars-than-for-their-biologi.
Biosimilar Development. Biosimilars forum applauds senator roberts, reps. barton, eshoo for leadership on medicare policy on biosimilar coding. 2017a. https://www.biosimilardevelopment.com/doc/biosimilars-forum-senator-roberts-reps-barton-eshoo-medicare-biosimilar-coding-0001.
Biosimilar Development. CMS’ coverage gap is a significant challenge for biosimilars. 2017b. https://www.biosimilardevelopment.com/doc/cms-coverage-gap-is-a-significant-challenge-for-biosimilars-0001.
Centers for Medicare and Medicaid Services. Medicaid biosimilars website. 2016. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Prescription-Drugs/Downloads/Rx-Releases/MFR-Releases/mfr-rel-103.pdf.
Centers for Medicare and Medicaid Services. Part B average sales price files. 2017a. https://www.cms.gov/apps/ama/license.asp?file=/Medicare/Medicare-Fee-for-Service-Part-B-Drugs/McrPartBDrugAvgSalesPrice/Downloads/2017-July-ASP-Pricing-File.zip.
Centers for Medicare and Medicaid Services. CY2018 medicare physician fee schedule final rule. Published November 2017b. https://www.gpo.gov/fdsys/pkg/FR-2017-11-15/pdf/2017-23953.pdf.
Centers for Medicare and Medicaid Services. CMS proposes policy changes and updates for medicare advantage and the prescription drug benefit program for contract year 2019 (CMS-4182-P). November 2017c. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2017-Fact-Sheet-items/2017-11-16.html.
Centers for Medicare and Medicaid Services. Medicaid drug rebate program. 2017d. https://www.medicaid.gov/medicaid/prescription-drugs/medicaid-drug-rebate-program/index.html.
Centers for Medicare and Medicaid Services. Part B payment website. 2018a. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Part-B-Drugs/McrPartBDrugAvgSalesPrice/Part-B-Biosimilar-Biological-Product-Payment.html.
Centers for Medicare and Medicaid Services. Medicaid enrollment website. 2018b. https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html.
Centers for Medicare and Medicaid Services. Medicaid managed care website. 2018c. https://www.medicaid.gov/medicaid/managed-care/index.html.
Covance Inc. Biosimilars: the commercial challenge. 2014. https://www.covance.com/content/dam/covance/assetLibrary/whitepapers/Biosimilars-WPCMA001.pdf.
Department of Health and Human Services. States’ collection of offset and supplemental rebates – OIG report. December 2014 https://oig.hhs.gov/oei/reports/oei-03-12-00520.pdf.
European Medicines Agency, Biosimilars in the EU: information guide for healthcare professionals. 2017. http://www.ema.europa.eu/docs/en_GB/document_library/Leaflet/2017/05/WC500226648.pdf.
FTC. Federal trade commission report. 2009. https://www.ftc.gov/sites/default/files/documents/reports/emerging-health-care-issues-follow-biologic-drug-competition-federal-trade-com-mission-report/p083901biologicsreport.pdf.
Health Affairs–Health Policy Briefs. Specialty pharmaceuticals. November 2013. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=103.
IMS Health. Delivering on the potential of biosimilar medicine: the role of functioning competitive markets. Parsippany, NJ: IMS Health; 2016a.
IMS Health. The impact of biosimilar competition. Parsippany, NJ: IMS Health; 2016b.
Janssen Pharmaceuticals. Remicade billing guide. 2016. https://www.janssencarepath.com/sites/www.janssencarepath.com/files/remicade-billing-guide.pdf.
Mack A. Norway, biosimilars in different funding systems. What works? GaBi. 2015;4(2):90–2.
Medicines for Europe. Payers’ P&MA policies supporting a sustainable biosimilar market. Final report. July 2016.
NICE. Introducing biosimilar versions of Infliximab: Inflectra and Remsima. 2015. http://www.biosimilars-nederland.nl/wp-content/uploads/2015/08/NICE-Adoption-Resource-Biosimilar-Infliximab-2015_07_31.pdf.
PwC Health Research Institute. Medical cost trend: behind the numbers. 2016. https://www.pwc.com/us/en/health-industries/behind-the-numbers/assets/pwc-hri-medical-cost-trend-chart-pack-2016.pdf.
Rémuzat C, Dorey J, Cristeau O, Ionescu D, Radière G, Toumi M. Key drivers for market penetration of biosimilars in Europe. J Mark Access Health Policy. 2017;5(1):1272308.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Disclaimer: The views, opinions and statements made in this publication are solely those of the author and may not reflect the views of Boehringer Ingelheim Pharmaceuticals, Inc. or its affiliates.
Rights and permissions
Copyright information
© 2018 American Association of Pharmaceutical Scientists
About this chapter
Cite this chapter
Burich, M. (2018). The Changing US Reimbursement Landscape and Biosimilars. In: Gutka, H., Yang, H., Kakar, S. (eds) Biosimilars. AAPS Advances in the Pharmaceutical Sciences Series, vol 34. Springer, Cham. https://doi.org/10.1007/978-3-319-99680-6_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-99680-6_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-99679-0
Online ISBN: 978-3-319-99680-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)