Abstract
Pharmacokinetic issues have been identified as a major cause for the attrition of new chemical entities in drug discovery. High development costs and time investments are associated with the discovery of such issues during clinical drug development. To overcome this problem, various in vitro and in silico ADME (Absorption, Distribution, Metabolism, Excretion) tools have been developed to predict drug pharmacokinetics using only a minimal amount of experimental data. Selecting the most appropriate option(s) from this broad range of in vitro and in silico ADME tools is challenging for drug discovery scientists as it requires consideration of a number of factors including the stage of the discovery process, any data already generated for a lead molecule or series and an awareness of the limitations and advantages of each ADME tool. ADME parameters, obtained through experimental approaches and/or in silico prediction, are also essential inputs to physiologically based pharmacokinetic models for the prediction of in vivo pharmacokinetics. Available in vitro and in silico ADME tools are presented and assessed in the following book chapter.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- In vitro methods
- In silico methods
- Absorption
- Distribution
- Metabolism
- Excretion
- Physiologically based pharmacokinetic modelling
1 Introduction
A study in 1997 showed that 39% of new chemical entities failed in clinical drug development due to issues related to pharmacokinetics (Kennedy 1997). This finding underlined the need for the development of tools suitable to identify compounds with a poor bioavailability at an early stage in the drug discovery process. In the last decades, a large number of in vitro and in silico tools for ADME prediction has been developed that contributed to the reduction of the drug attrition rate due to poor pharmacokinetic properties to 10% in 2000 (Kola and Landis 2004). Especially, the prediction of cytochrome P450 (CYP)-related metabolism added to this improvement. ADME prediction for drug candidates using in vitro and in silico tools helps in the selection of lead compounds before reaching clinical trials. In turn, unsuccessful drug candidates can be identified at an earlier stage resulting in saving time and costs. The knowledge of advantages and limitations of each ADME prediction tool are key to selecting the appropriate tool and to build confidence in the prediction. Considering drug absorption, solubility and dissolution studies are especially important for poorly soluble drugs, while for other compounds absorption may be limited by intestinal membrane permeability. Drug distribution can have implications on the duration of the drug effect and be associated with a risk of not reaching therapeutic concentrations in vivo, especially for lipophilic drugs. The use of in vitro and in silico tools assessing plasma protein binding, partitioning into red blood cells and distribution into peripheral tissues helps to identify those issues. Drug metabolism by metabolic enzymes influences the clearance profile and is often a source of interindividual pharmacokinetic variability or drug-drug interactions. In vitro and in silico predictions of drug metabolism should consider the enzymatic reaction as well as the relevant enzymatic expression in the respective tissue. Drug exposure can also be limited by drug excretion. Therefore, in vitro and in silico tools are available for the complex processes of biliary and renal excretion. While the consideration of each of the previous ADME processes separately helps to identify issue related to one process, their mutual interaction can negate or improve the drug’s pharmacokinetic profile. Physiologically based pharmacokinetic (PBPK) models take into account all ADME processes together by integration of various experimental results, and in silico predictions of unknown parameters and in vivo performance can be made.
2 Absorption
Drug absorption after oral administration is a very complex process influenced by drug properties, formulation-dependent factors and physiological conditions. Drug absorption includes several underlying processes, e.g. release and/or dissolution of the drug from the pharmaceutical formulation in the gastrointestinal fluids and permeation of the dissolved drug through the gastrointestinal membrane. Therefore, determination of the rate-limiting process governing the absorption of the investigated drug based on its physicochemical properties is essential.
The Biopharmaceutics Classification System (BCS), introduced in 1995 by Amidon et al. (1995), aimed to correlate in vitro drug dissolution with in vivo bioavailability. Drugs are classified based on three dimensionless parameters determining their absorption (dose number, dissolution number and absorption number) and their underlying drug properties (solubility and permeability). Four different BCS classes are defined: BCS class 1 includes compounds with high solubility and high permeability for which gastric emptying (for when drug dissolution is very rapid) or drug dissolution is the rate-limiting step to drug absorption. BCS class 2 drugs have a low solubility and a high permeability presenting solubility or dissolution rate-limited absorption. BCS class 3 contains high solubility and low permeability compounds for which the rate-limiting step to drug absorption is permeability. BCS class 4 includes low solubility and low permeability compounds which are usually challenging for oral drug delivery. Once a compound is classified according to the BCS, formulation development can be guided. For example, if the solubility of a compound is problematic, subsequent efforts in formulation development with, e.g. enabling formulations may be required.
Several ‘rule of thumb’ approaches have been introduced to categorise new chemical entities according to characteristics which increase their likeliness to be adequately absorbed in vivo. The most popular method to identify compounds at risk of poor absorption and permeation was developed based on an analysis of the World Drug Index and is called Lipinski’s ‘rule of five’. The rule implies that drugs with >5 hydrogen bond donors, a molecular weight >500 Da, an octanol-water partition coefficient (log P) >5 and >10 hydrogen bond acceptors have an increased risk for poor absorption (Lipinski et al. 2001). An exception of this rule are drug classes that are substrates for biological transporters. Another analysis by Veber et al. (2002) used oral bioavailability data of over 1000 drugs in rats and identified that drugs with ≤10 rotatable bonds and a polar surface area ≤140 Å2 (or 12 or fewer H-bond donors and acceptors) are likely to have a good oral bioavailability. The bioavailability score is another approach stating that the predominant charge at biological pH determines the properties that are important for a compound’s bioavailability (Martin 2005). The important parameter for anions is the polar surface area, while for neutral, zwitterionic or cationic compounds, the previously described Lipinski’s rule of five is more predictive. Additional strategies aim to identify drug-like molecules that are also expected to meet ADME profiles using simple structural rules or neural network approaches (Muegge et al. 2001).
2.1 In Vitro Methods
2.1.1 Solubility
Drug solubility can be a limiting factor in drug absorption, and its importance is highlighted by the fact that 75% drug development candidates are poorly soluble and belong to BCS class 2 or 4 (Di et al. 2009). In early development, high- throughput methods are used to determine the solubility of a large number of compounds. These methods typically include a concentrated stock solution of the investigated drug in DMSO which is either directly added to a buffer (often pH 6.5 or 7.4) or evaporated, and subsequently a buffer is added to the remaining material to reduce the effect of DMSO on solubility. The solution can be analysed by different methods including light scattering, turbidimetry, LC-UV or LC-MS. The drug concentration at which the first induced precipitate appears in a solution is called kinetic solubility. A ‘semi-equilibrium’ solubility refers to the solution being incubated for approximately 1 day followed by its filtration and the determination of drug concentration (Di et al. 2012a). While the latter method allows some time for equilibration between solid drug and solution, supersaturation is a frequent problem for kinetic solubility measurements. Additionally, the evaporation of DMSO can leave the drug in an energetically higher state (amorphous form) possibly resulting in a higher solubility. Consequently, high-throughput methods present the ‘best case scenario’ of drug solubility (Di et al. 2012a).
Equilibrium (thermodynamic) solubility refers to the concentration of the saturated solution in equilibrium with the thermodynamically stable polymorph (Bergstrom et al. 2014). Measurements of equilibrium solubility are performed with the shake flask method in later phases of drug development when crystalline drug material becomes available. The characterisation of the solid form by, e.g. polarized light microscopy and powder X-ray diffraction provides information about potential solid form changes.
At this stage, apart from simple buffers (pH 1.2, 6.5, 7.4), the solubility is also tested in biorelevant media that closely simulate the gastrointestinal fluids (Di et al. 2012a). Biorelevant media were developed since the solubility of a drug in water or simple buffers is not always reflective of the solubility in the gastrointestinal lumen (Galia et al. 1998). Especially for lipophilic drugs, biliary secretions or dietary lipids can enhance drug solubility. To consider these differences in in vitro experiments, biorelevant media can reflect the osmolality, pH and buffer capacity of gastrointestinal fluids and can include bile components, dietary lipids, lipid digestion products and enzymes. Depending on the investigated drug, not all components and properties of the medium may be necessary to reflect the in vivo solubility, and thus, the level of the biorelevant medium can be chosen accordingly (Fig. 13.1) (Markopoulos et al. 2015).
2.1.2 In Vitro Release and Dissolution Testing
Apart from the solubility of a drug, the dissolution rate can also be limiting for the drug absorption of poorly soluble drugs. Additionally, the release of the drug substance from a drug product can be critical for the drug product performance in vivo. For development purposes, in vitro tests should adequately represent the gastrointestinal physiology to be able to sufficiently reflect drug dissolution, degradation, supersaturation, precipitation and redissolution in vivo and to guide formulation development (Kostewicz et al. 2014b; Wang et al. 2009). Therefore, the experimental design should consider the composition, volume, flow rates and mixing patterns of the gastrointestinal fluids (Dressman et al. 1998; Fotaki and Vertzoni 2010).
Four dissolution apparatus are included in the United States Pharmacopoeia (USP) for oral drug products. In the USP apparatus 1 (basket apparatus), the investigated drug product is placed in a spinning basket in the middle of a cylindrical vessel with hemispherical bottom filled with dissolution medium (US Pharmacopoeia Convention 2005). The USP apparatus 2 (paddle apparatus) uses the same vessel, but a paddle is used as stirring element (US Pharmacopoeia Convention 2005). For both apparatus, methods usually use high volumes of dissolution medium (500–1000 mL) to generate sink conditions. Especially in the fasted state, the high volumes are unlikely to match the in vivo situation. This is particularly an issue if sink conditions are not maintained in vivo resulting in an overestimation of drug dissolution. For drugs with high solubility (BCS class 1 and 3), sink conditions are usually maintained in vivo. For drugs with low solubility, the conditions in those dissolution experiments are likely to mismatch the in vivo situation. At highest risk are BCS class 4 drugs, since the high membrane permeability of BCS class 2 drugs results in constant removal of dissolved drug from the luminal fluids (Kostewicz et al. 2014b). Furthermore, coning effects and variability in hydrodynamics depending on the investigated dosage form (size, shape, density) and its location in the vessel often result in a lack of correlation to physiological conditions (Kostewicz et al. 2014b). In the USP apparatus 3 (reciprocating cylinder), the drug product is placed in a glass tube with a mesh base that reciprocates vertically in a cylindrical, flat-bottomed glass vessel filled with dissolution medium (US Pharmacopoeia Convention 2005). Media changes can be easily performed by moving the glass tube from one vessel to another vessel but limit the usage of the apparatus to non-disintegrating dosage forms. Typical volumes of dissolution medium are 250 mL in each glass vessel. Hydrodynamics can be adjusted by changing the rate of the reciprocating movement and mesh size of the sieve. For these three USP apparatus, the temperature can be controlled with a tempered water bath surrounding the dissolution vessels. In the USP apparatus 4 (flow-through cell), the drug product is placed in a flow-through cell, through which the dissolution medium can be pumped with an adjustable flow rate (usually 4–16 mL/min) and which is immersed in a tempered water bath. The advantages of the flow-through cell are the possibility to change flow rate and media within a single experiment and to maintain sink conditions if the system is used in open mode (continuously fresh dissolution medium from the reservoir) (Fotaki 2011).
Apart from the apparatus described in the USP, various biopharmaceutical tools have been developed to simulate the dissolution process in vitro. Biphasic dissolution tests can be useful for poorly soluble compounds as membrane permeation is simulated with an organic layer constantly removing drug from the aqueous medium to maintain sink conditions. Integrated permeation systems such as the μFlux™ (Pion Inc., Woburn, MA, US) have the advantage of simultaneous measurements of dissolution and permeability. Surface dissolution imaging is used to understand surface effects during dissolution and quantify swelling, erosion and disintegration kinetics . The use of physiologically relevant bicarbonate buffers in dissolution tests was shown to be more discriminative, for e.g. enteric-coated formulations, but is laborious, and results were shown to be less reproducible (Liu et al. 2011; Boni et al. 2007). Transfer models were able to successfully predict drug precipitation of weak bases in vivo by constantly transferring medium from a gastric donor compartment to an intestinal acceptor compartment (Kostewicz et al. 2004). Complex gastrointestinal simulators such as the TNO Gastro-Intestinal Model (TNO, Zeist, Netherlands) simulate the conditions in the lumen of the gastrointestinal tract very closely by mimicking digestive fluids, constant removal of metabolites and control of pH, temperature and luminal transit.
2.1.3 Permeability
For the prediction of the permeability of a compound across the intestinal barrier, several methods can be used ranging from simple filter-immobilised artificial membranes, in vitro cell cultures to in situ perfusion studies (Table 13.1).
In the early stages of drug discovery, methods suitable for high-throughput screening are used such as parallel artificial membrane permeability assay (PAMPA). PAMPA consists of a microporous filter which is infused by a lipid or a lipid mixture dissolved in a nonpolar solvent and which separates two aqueous, pH-buffered solutions in a microplate sandwich (Caldwell and Yan 2014). The concentration gradient between the two compartments is the driving force for the permeability of the investigated compound. This driving force can be maintained, and the experimental time can be reduced with the use of a pH-gradient, the addition of cosolvents/solubilising agents or addition of compounds to simulate protein binding in the donor compartment (Caldwell and Yan 2014).
Other permeability assays use immortalised cell cultures with the ability to form polarised monolayers (with distinct apical and basolateral morphologies) as membranes (Alqahtani et al. 2013). The most commonly used cells are Caco-2 cells, derived from a human colon adenocarcinoma and also available for high-throughput screening. Caco-2 cells are usually cultured for at least 20 days to express high amounts of transporter enzymes, form tight junctions and obtain cell polarity (Alqahtani et al. 2013; Bohets et al. 2001). The expression of endogenous transporter systems such as P-glycoprotein (P-gp) and several drug- metabolising enzymes like aminopeptidase, esterase, sulfatase and some CYP450 isoenzymes is the main advantage of Caco-2 cells, while paracellular permeability is often underpredicted due to ‘tighter’ tight junctions (Alqahtani et al. 2013; Lea 2015). The use of Madin-Darby canine kidney cells (MDCK), derived from the distal tubular part of the dog kidney, has the advantage of reducing the time needed for the formation of a polarised monolayer with well-defined tight junctions. Additionally, the transepithelial electrical resistance (TEER) is lower compared to Caco-2 cells indicating increased ‘leakiness’ (Braun et al. 2000). The non-human origin of these cells has the disadvantage of different enzyme and transporter expression. To overcome this issue, it is possible to transfect the cells with, e.g. P-gp, MRPs (multidrug resistance-associated protein) or BCRP (breast cancer resistance protein). To only investigate passive permeability, special cell lines with low expression of endogenous canine transporters such as MDCKII-low-efflux cells can be used (Di et al. 2011). The apparent permeability observed using cultured cell lines must be normalized according to accessible intestinal surface area, paracellular permeability, pH dependence, resistance of the aqueous boundary layer and transcellular permeability to predict the effective permeability in vivo (Avdeef 2012).
Additionally, permeability can be assessed ex vivo using Ussing chambers. An excised intestinal segment (from rat, mouse, rabbit, dog, monkey or human) is mounted between two diffusion cells usually filled with Krebs-Ringer bicarbonate buffer (Alqahtani et al. 2013). Despite the supply of nutrients and carbogen gas during the experiment, tissue viability can only be maintained for 2–3 h. The method results in good predictions of intestinal drug absorption and provides information about influx/efflux transport and drug metabolism.
A labour-intensive method is the in situ perfusion model. This includes the perfusion of an isolated intestinal segment of the small bowel of rats with a solution containing the investigated drug (Alqahtani et al. 2013). The rat is unconscious during the experiment, and its body temperature is controlled with a heating pad or an overhead lamp (Stappaerts et al. 2015). Drug permeability can then be calculated by the difference between inlet and outlet flow of the investigated drug. To account for differences in drug concentration due to water absorption or secretion, non-absorbable markers (e.g. phenol red) or gravimetric methods can be used (Stappaerts et al. 2015). The method allows distinction between regional permeability differences and considers active transport mechanisms. Additionally, intestinal metabolism can also be investigated, for example, by concomitant administration of inhibitors of metabolising enzymes or by mesenteric blood sampling (Stappaerts et al. 2015). By considering only the difference in drug perfusate concentration, drug absorption may be overestimated for drugs that are accumulated in the gut wall or metabolised by intestinal enzymes. Furthermore, the use of anaesthesia can have a possible impact on drug permeability.
2.1.4 Active Transport
The involvement of active transport mechanisms in the membrane permeation of a drug can mediate or limit its absorption but also be responsible for drug-drug interactions. Bioavailability can be increased by drug transport from the luminal to the basolateral site via influx transporters or decreased by transport in opposite direction via efflux transporters.
The in vitro assessment of active transport mechanisms includes cell-based and subcellular assays. In both cases, cells are incubated with a drug solution followed by the monitoring of changes in drug concentration. In cell-based assays, transport proteins are overexpressed in a transfected cell line such as MDCK cells, HEK (human embryonic kidney) or LLC-PK1 (Lewis lung carcinoma-pig kidney) (Caldwell and Yan 2014). Another approach is to partially or completely silence (knock down) a natively expressed transporter protein in a cell line, for example, P-gp in Caco-2 cells and compare the drug permeability to the unmodified cell line (Caldwell and Yan 2014). Other methods for active transport studies include the use of primary cells such as hepatocytes and membrane vesicles (described in detail below in Sect. 13.5.1).
2.1.5 Gut Wall Metabolism
The intestine with numerous metabolising enzymes is involved in the metabolism of compounds undergoing phase 1 and 2 reactions. Several in vitro methods are available to investigate intestinal drug metabolism. For drugs that are rapidly metabolised, suitable methods include the use of isolated intestinal perfusion, the everted sac method and Ussing chambers (van de Kerkhof et al. 2007). For isolated intestinal perfusions, a segment of the intestine is removed from an animal (e.g. rat) and placed in a bath filled with buffer followed by perfusion with the investigated compound from the luminal or vascular side (van de Kerkhof et al. 2007). The everted sac method includes eversion of intestine (most often from rat) and its cannulation from both sides followed by drug perfusion. Disadvantages of these two methods are their limitation to short-term incubation and the animal origin of the tissue. The Ussing chamber, as described above in Sect. 13.2.1.3, can also be used for investigations of intestinal drug metabolism.
For drugs that are slowly metabolised, more appropriate in vitro tools for gut wall metabolism are biopsies, intestinal precision-cut slices (thickness 250–400 μm) and primary cells (van de Kerkhof et al. 2007). Limitations of these methods are that it is not possible to study the direction of excretion and the very difficult isolation procedures for primary enterocytes (van de Kerkhof et al. 2007).
For mechanistic investigations of relevant metabolic enzymes, interaction studies and enzyme kinetics, in vitro assays include subcellular fractions from enterocytes and cell cultures similarly to the assays for hepatic metabolism as further discussed below in Sect. 13.4.1.
2.2 In Silico Methods
2.2.1 Solubility
In the initial stages of drug development, in silico solubility predictions are used to screen new chemical entities for drug-like characteristics. A large number of in silico tools are available for the prediction of aqueous solubility based on training sets of experimental data and either experimentally determined properties or computational 1D, 2D and 3D molecular descriptors such as hydrophobicity, molecular surface area and electron distribution (Fig. 13.2) (Dokoumetzidis et al. 2007). The lipophilicity (log P, clog P), the size of the molecule and the surface area of the nonpolar atoms have been identified as the most important predictors for aqueous solubility (Dokoumetzidis et al. 2007).
Various types of molecular descriptors used for in silico prediction of ADME parameters. (Modified from Dokoumetzidis et al. 2007)
Aqueous solubility is determined by the sublimation energy and hydration energy of a drug. The extensively used modified Yalkowsky’s general solubility equation (Eq. 13.1) describes the water solubility of a molecule (S0(M)) using the logarithm of the octanol/water partition coefficient (log POct) to reflect the hydration energy and the melting point (m. p.) to reflect the crystal lattice energy (Jain and Yalkowsky 2001).
For highly lipophilic drugs, micellar solubilisation can improve drug solubility, while for drugs with a high melting point, solubility can be improved by modifications of the structure resulting in a reduction of lattice energy (Sugano 2012). To consider ionisation effects, it has been proposed to use the logarithm of the distribution coefficient (log D) at pH 7.4 instead of the log POct for the solubility prediction (Hill and Young 2010).
For weakly acidic and basic drugs, differences in drug solubility along the gastrointestinal tract can be a result of drug ionisation. pH-dependent solubility profiles can be predicted in silico using the Henderson-Hasselbalch equation (Hansen et al. 2006). Additionally, the aqueous solubility may differ from the solubility in gastrointestinal fluids, especially for lipophilic compounds, due to, e.g. luminal surfactants such as bile salts or lecithin. If reliable predictions of drug solubility in gastrointestinal fluids could be obtained using computational models, this could replace laborious biorelevant solubility studies. For several compounds, successful predictions for the increase in solubility as a function of bile salt concentrations could be made using an empirical equation introduced by Mithani et al. 1996 (Eqs. 13.2 and 13.3) (Mithani et al. 1996).
where SR is the solubilisation ratio, CSX is the solubility [μg/mL] in the presence of taurocholate, CSO is the aqueous solubility [μg/mL], MW is the molecular weight and [NaTC] is the concentration of sodium taurocholate. It should be noted that the equation only considers the effect of sodium taurocholate, but gastrointestinal fluids are more complex containing, e.g. lipids and mixed micelles as colloidal aggregates.
For solvation processes, Abraham et al. (1987) described a solvation-related property based on several parameters such as the McGowan’s characteristic volume, hydrogen-bonding acidity and basicity, polarizability and an excess molar refraction descriptor. These Abraham solvation predictors have been successfully used to predict the solubility enhancement in biorelevant media (Fasted State Simulated Intestinal Fluid) compared to a simple buffer (Niederquell and Kuentz 2018). Most prominent were a positive effect of McGowan’s characteristic volume and a negative effect of drug basicity on solubility enhancement.
2.2.2 Drug Release and Dissolution
In most oral dosage forms, the active pharmaceutical ingredient is administered in solid form. For these formulations , the drug needs to be released from the formulation and dissolve in the gastrointestinal fluids prior to its intestinal membrane permeation. If drug dissolution occurs slowly in the gastrointestinal tract, it can be the limiting step for drug absorption. Diffusion theory is widely used to describe particle dissolution assuming drug dissolution is controlled by the diffusion of the solute through a stagnant diffusion layer surrounding solid particles.
In 1897, it was shown by Noyes and Whitney (1897) that the rate of drug dissolution is proportional to the difference between the saturation solubility (Cs) and the present drug concentration at time t. This relationship was further modified to the Nernst-Brunner law:
where C is the concentration, t is the time, D is the diffusion coefficient, S is the surface of the solid particles, V is the volume of the dissolution medium and h is the thickness of the diffusion layer (Brunner 1904; Nernst 1904). This dissolution model is still widely used today (Dokoumetzidis et al. 2007). The diffusion coefficient can be derived from the Stokes-Einstein equation or the Hayduk-Laudie equation for non-electrolytes (Hayduk and Laudie 1974). A further improvement was made by Wang and Flanagan resulting in a generalised diffusion layer model for spherical particles (Eq. 13.5) that considers a time-dependent reduction of the particle radius, a nonlinear concentration gradient in the diffusion layer and changes in the thickness of the effective boundary layer (Wang and Flanagan 1999, 2002).
The particle radius, rt, is time dependent and influences the thickness of the effective boundary layer h. In the case of small particles (r < 30 μm), the particle radius is considered to be equal to h, while for larger particle radii (r > 30 μm), h is set to 30 μm (Peters 2012).
For particles with substantially larger diameters compared to the diffusion layer thickness, the diffusion layer can be assumed as planar resulting in the cube root equation:
with the cube roots of the weight of a spherical particle at time 0, Q01/3, and time t, Q1/3, and the cube root rate constant, k1/3 , as described by Hixson and Crowell (Hixson and Crowell 1931). The cube rate constant can be further described as:
with D as the diffusion coefficient, Cs as the equilibrium solubility, h as the thickness of the diffusion layer and ρ as the density.
For the modelling of in vitro dissolution data, fitting of the data can be obtained using empirical equations. The Weibull equation is the most commonly used equation due to its flexibility to fit almost any dissolution data:
where Wt is the amount dissolved at time t, Wmax is the maximum amount dissolved, t is time, Tlag is the lag time before the onset of dissolution, a is a scale parameter and b is a shape parameter characterising the curve (exponential curve b = 1, sigmoid curve b >1, parabolic curve b <1) (Langenbucher 1972). Other empirical approaches include gamma distribution, power laws, discrete time-step difference equations and stochastic differential equations (Dokoumetzidis et al. 2007). For in vivo predictions of drug dissolution, parameters with physical meaning derived from mechanistic models are usually used in absorption models (Dokoumetzidis et al. 2007).
In certain cases, drug absorption can also be determined by the release of a drug from the formulation. Controlled-release formulations are, for example, developed to reduce dosing frequency, to avoid toxicity for drugs with a narrow therapeutic index or to locally deliver drugs in the gastrointestinal tract. The drug release rate of these formulations is constant over a certain time and is diffusion-controlled, swelling-controlled or chemically-controlled (Siepmann and Peppas 2011). This steady release process allows the direct use of in vitro release profiles for in vivo predictions or even to use empirical equations. For the analysis of drug release data, the Higuchi model is widely used but should only be applied to the first 60% of drug release:
with q(t) as the drug released at time t, q∞ as cumulative amount of drug released at infinite time and the constant k (Higuchi 1961). Assumptions behind this model are that the carrier is of a thin planar geometry and the medium acts as a prefect sink. Adapted models for carriers with different geometries have been proposed in literature (Baker 1987). Other models used for drug release are the Peppas equation, Weibull equation, Baker and Lonsdale equation, Hixson and Crowell equation or Monte Carlo simulation methods (Carbinatto et al. 2014).
2.2.3 Permeability
In silico approaches to predict passive permeability of novel compounds are mostly developed based on data sets of compounds with known in vitro permeability in different cell lines (e.g. Caco-2, MDCK, PAMPA) and are used in drug discovery for the selection of novel compounds for synthesis (Broccatelli et al. 2016). Often these in silico models are based on multivariate statistical analysis (e.g. partial least-squares regression) that correlate in vitro results to 2D or 3D molecular descriptors (Zhang et al. 2006; Broccatelli et al. 2016). Other in silico approaches include mechanistic mathematical models developed for the passive transcellular drug transport which are, for example, based on simple physicochemical properties such as log P and pKa (Zhang et al. 2006).
Such mechanistic models describing passive permeability can be augmented with additional processes such as active influx and efflux transport. This more complex system description can be used to define the properties of the enterocyte as a separate compartment for absorption (Dokoumetzidis et al. 2007). Such models are, for example, implemented in PBPK models that are commercially available such as the software Simcyp® (Certara, Sheffield, UK) or GastroPlus™ (Simulations Plus, US).
2.2.4 Active Transport
Drug-transporter interactions can be modelled in silico either based on a set of compounds with known transporter activity (substrate-based methods) or based on the 3D structure of the transporter (transporter-based methods) (Chang and Swaan 2006). Substrate-based methods use molecular descriptors or chemical properties for pharmacophore or 3D-QSAR) modelling without the need for prior information about the structure of the transporter. Such models exist for a variety of different transporters such as P-glycoprotein, organic cation and anion transporters, bile acid transporters and nucleoside transporters (Chang and Swaan 2006). Transporter-based methods include ab initio modelling and homology modelling. Ab initio modelling generates the 3D structure of the transport protein from its primary sequence, while homology modelling uses structural information of a template protein with mutual sequence similarity (Chang and Swaan 2006).
For the modelling of active carrier-mediated transport, most often the saturable Michaelis-Menten kinetic is used. The input parameters Vmax, the maximum reaction velocity, and km, the substrate concentration with 50% Vmax (Michaelis constant) are determined in vitro. While at low concentrations, the rate of transport increases almost linear, at high concentrations, transporter saturation occurs resulting in a constant maximum transport rate.
2.2.5 Gut Wall Metabolism
For in silico predictions of gut wall metabolism , an allometric scale-up approach is followed if in vitro data is available. For example, the slice weight and organ weight are used for the scaling of experimental data from precision-cut intestinal slices to the in vivo situation. Alternative approaches include scaling of the information of specific enzymes determined for hepatic metabolism to the gut wall metabolism. Therefore, information about the kinetics of the specific enzymatic reaction, enzyme abundance in the in vitro assay used for the determination of the kinetics of the enzymatic reaction and enzyme scaling factors (e.g. derived from immunoquantified enzyme expression levels in the intestine and liver) are needed (Heikkinen et al. 2012). With these approaches, the intrinsic intestinal clearance is determined and can further be used to calculate the fraction of drug escaping gut wall metabolism. Using a similar approach to the well-stirred liver model, the fraction of drug escaping gut wall metabolism (Fg) can be described with the Qgut-model:
where fu, g is the fraction of unbound drug in the enterocytes and CLuint, g is the intrinsic metabolic clearance in the gut (Yang et al. 2007). Qgut can further be described as:
where Qvilli is the villous blood flow and CLperm is the cellular permeability. Purely in silico approaches are used to identify the investigated compound as a substrate for specific enzymatic reactions following ligand-based or structure-based approaches as further described below in Sect. 13.4.2.
2.2.6 Dynamic Transit Models
Dynamic transit models are dependent on a temporal variable and include mixing tank models, the compartmental absorption transit model (CAT) and dispersion models (Yu et al. 1996). With these models, it is not only possible to predict the fraction of dose absorbed but also to predict the rate of drug absorption which can help in the simulations of plasma concentration profiles and predictions of in vivo performance.
The mixing tank model introduced by Dressman and Fleisher (1986) is based on mass balance considerations and suitable for drugs with dissolution-rate limited absorption. The model considers the gastrointestinal tract as a single well-stirred compartment with uniform drug concentration, in which transit and absorption follow first-order kinetics. The drug is administered as bolus, and the transport of solid and dissolved drug occurs at the same rate. Despite several limitations of the model such as no consideration of luminal degradation, gut metabolism or heterogeneity of the gastrointestinal tract, the model could successfully predict the determining factors limiting the absorption of digoxin (dissolution rate) and griseofulvin (solubility).
The compartmental absorption transit model (CAT) considers the gastrointestinal tract as a series of well-stirred compartments with different volumes and flow rates but equal residence time of the drug. For the small intestine, seven compartments resulted in the best fit of available literature data (Yu and Amidon 1999). Further modifications of the CAT model included addition of compartments of unreleased drug and undissolved drug, pH-dependent solubility, precipitation, gastric and colonic compartments, information of effective absorptive surface area and drug transporter processes resulting in the advanced compartmental absorption transit (ACAT™), the basis of the commercial software GastroPlus™ (Simulations Plus, US) (Kuentz 2008).
The current version of the ACAT™ model considers ionisation effects on solubility and permeability, paracellular permeability, nanoparticles effects, food effects, bile salt-enhanced solubility, precipitation and active transport. It can be used for immediate release, delayed release and controlled release formulations. Apart from human gut physiology , physiological gut models are available for a variety of species (dog, rat, mouse, rhesus monkey, cynomolgus monkey, minipig, rabbit and cat). Drug dissolution can be predicted with several dissolution models (e.g. Hintz and Johnson equation, Wang and Flanagan equation, Z-Factor Model) (Hintz and Johnson 1989; Takano et al. 2006). A similar advanced compartmental absorption model is integrated in the Simcyp® software (Certara, Sheffield, UK) under the name Advanced Dissolution, Absorption, Metabolism (ADAM) model. The ADAM model uses the Wang and Flanagan equation (described above in Sect. 13.2.2.2) as default model for drug dissolution (Wang and Flanagan 1999).
The dispersion models consider the gastrointestinal tract as a continuous single tube with constant velocity, dispersion behaviour and concentration profile across the tube diameter and spatially varying properties along the tube (Yu et al. 1996). The convection-dispersion equation is used to describe the drug absorption process:
where C is the concentration, x is the axial distance from the stomach, α is the dispersion coefficient, β is the linear flow velocity in the axial direction and γ is the drug absorption rate constant (Ni et al. 1980). With a modified version of this concept, drug absorption in rats and later in humans was successfully predicted (Willmann et al. 2003; Willmann et al. 2004). The earlier versions of the absorption model of the PBPK software PK-Sim® (Open Systems Pharmacology) were evolved from this model which was later replaced by a 12 compartmental absorption model (Willmann et al. 2012).
3 Distribution
3.1 In Vitro Methods
Plasma protein binding (PPB) is an important parameter for the distribution of a drug in the body. Highly protein-bound drugs are retained in plasma and often less prone to distribute into body tissues resulting usually in a low volume of distribution. In terms of pharmacodynamics, highly protein-bound drugs may not reach therapeutic concentrations as usually only the fraction unbound is available for receptor or enzyme interaction. Plasma contains 7% proteins of which human serum albumin is the most important protein for drug binding followed by α1-acid glycoprotein and lipoproteins (Caldwell and Yan 2014). The preferred method for the determination of plasma protein binding is equilibrium dialysis since the method is less susceptible to non-specific binding. For classical equilibrium dialysis (CED) , a regenerated cellulose membrane (cut-off 12–14 kDa) separates two 1 mL paired Teflon cells filled with buffer and plasma which are tempered at 37 °C and rotated for a predetermined period (4–12 h) (Caldwell and Yan 2014). Typical methods used for drug analysis are scintigraphy or LC-MS/MS analysis. Further development of the method resulted in the rapid equilibrium dialysis (RED) with faster preparation and equilibration times and suitability for higher throughput of samples. Another method to determine PPB is ultracentrifugation where plasma is added to the device followed by centrifugation for 10–20 min at 1000–2000 × g in a fixed angle rotor (Caldwell and Yan 2014). The accuracy of this method is limited by the non-specific binding to the filtration apparatus. Additionally, high-performance affinity chromatography can be used to determine PPB using immobilised albumin or α1-acid glycoprotein as stationary phase and correlate chromatographic retention to the percentage of drug binding to albumin or α1-acid glycoprotein (Lambrinidis et al. 2015). Longer chromatographic retention time indicates higher percentage of protein binding.
Similar to PPB, drug partition into red blood cells (RBC), the major cellular component of blood, can influence drug distribution. For the in vitro determination of RBC partitioning, radiolabelled or unlabelled drug is mixed with whole blood followed by centrifugal separation of RBC and plasma and the determination of drug concentration in both compartments (Hinderling 1984). Measurements at several time points also permit to determine the rate of RBC partitioning.
In vitro tissue distribution can be assessed using tissue homogenates, tissue slices or isolated tissue components. After an incubation period of the tissue with the investigated drug, the tissue-to-medium distribution coefficient can be calculated using the separately measured drug concentration in tissue and medium (Ballard et al. 2003). While tissue homogenates are the most widely used method, the disruption of cellular integrity can result in an overestimation of tissue distribution for drugs mainly restricted to the extracellular space.
3.2 In Silico Methods
Computational models to predict plasma protein binding have been developed using ligand-based approaches with quantitative structure activity relationships and structure-based approaches focusing on the crystal structure of drug-protein complexes. Due to the predominant role of human serum albumin in PPB, most approaches only focus on albumin, and only recently advances for α1-acid glycoprotein have been made. Due to the different binding sites of albumin, global models for a broad range of compounds are challenging, and in the beginning, in silico models focused on similar compounds using the same binding site. Based on training sets of compounds and multivariate statistical analysis, lipophilicity (log P), electronic properties, acidity, shape-modulating factors, polarity terms and fraction ionised (cationic and anionic) were identified as important predictive factors in ligand-based in silico models (Lambrinidis et al. 2015).
Drug distribution in the body has been described by different mechanistic models. The steady-state volume of distribution (Vss) describes the extent of tissue distribution and can be defined as:
where Vt is the fractional volume of a tissue, Pt : p is the plasma/partition coefficient, Ve is the fractional volume of erythrocytes, E : P is the erythrocyte/plasma ratio and VP is the plasma volume (Poulin and Theil 2002). The erythrocyte/plasma ratio can be described as:
where B : P is the blood/plasma ratio which can be determined in vitro (as described above in Sect. 13.3.1) and Ht is the haematocrit (volume percentage of red blood cells in blood) (Poulin and Theil 2002).
Literature data is available for the different body volumes (e.g. lung, brain, heart, liver, bone, kidney, muscle, skin, adipose) in Eq. 13.13 and for the estimation of tissue/plasma partition coefficients, the following in silico models can be used.
An in silico model developed by Poulin and Theil (2002) and modified by Berezhkovskiy (2004) accounts for plasma and tissue being composed of neutral lipids, phospholipids and water and only the unionised fraction of the drug permeating the membrane. This resulted in the following description of the tissue-partition coefficient, Pt : p, for non-adipose tissue:
where Po : w is the n-octanol/buffer partition coefficient of the non-ionized species; V is the fractional tissue volume content of neutral lipids (nl), phospholipids (ph), and water (w) in either tissue (t) or plasma (p); and fu is the fraction unbound. The fraction unbound in tissue, fut, can mechanistically be estimated (Eq. 13.16) from the fraction unbound in plasma according to:
as described by Poulin and Theil (2000).
Further models developed by Rodgers and Rowland differentiated between intra and extracellular space and added an acidic phospholipid fraction in tissues resulting in an improvement of the prediction for strong bases (Rodgers et al. 2005a, b; Rodgers and Rowland 2006, 2007). Additionally to passive permeability of the unionized fraction of the drug, a further modification of the model includes membrane permeability of the ionized fraction and is integrated in the Simcyp® simulator (Certara, Sheffield, UK).
4 Metabolism
Drug metabolism or biotransformation of orally administered drugs occurs mainly in the small intestine (as described above in Sect. 13.2.1.5) and liver. Physicochemical characteristics of drugs such as a high lipophilicity as indicated by a high logD7.4 were shown to be associated with high metabolic clearance (van de Waterbeemd and Gifford 2003). A variety of metabolising enzymes is available to facilitate the excretion of xenobiotics by increasing their aqueous solubility. Enzymatic biotransformation can be divided in Phase 1 and Phase 2 metabolism. Phase 1 reactions are reactions of functionalisation (e.g. oxidation, hydrolysis or reduction) that introduce polar functional groups to molecules resulting in either facilitated excretion or further metabolism (Westhouse and Car 2007). In Phase 2 reactions , large polar molecules (e.g. glucuronate, acetate and sulfate) are conjugated to drug molecules further resulting in an increased aqueous solubility to facilitate excretion (Westhouse and Car 2007).
4.1 In Vitro Methods
Different in vitro assays are available to predict hepatic drug metabolism. Recombinant CYP enzymes expressed in different cell types can be used to identify the specific CYP enzymes involved in the metabolism of the investigated drug. Additionally, incubation of these recombinant CYP enzymes with the investigated compound provides information about the metabolic enzyme activity per mass of protein which can further be scaled up to the in vivo situation.
The homogenisation of liver and subsequent centrifugation at 1000 g and 9000 g separate the pellet with nuclei and mitochondria, respectively, from the supernatant with cytosolic and microsomal enzymes (Richardson et al. 2016). The supernatant is the hepatic S9 pool and can be used as in vitro system for investigating hepatic metabolism. An additional ultracentrifugation step at 100,000 g results in the separation of the cytosol subcellular fraction in the supernatant and the microsomal subcellular fractions in the pellet (Richardson et al. 2016). Human liver microsomes are commonly used in the pharmaceutical industry due to their richness of metabolic cytochrome P450 enzymes, low cost and ease in use (Di et al. 2012b). However, metabolic pathways in the assay can be incomplete since the present enzymes are limited to enzymes contained in endoplasmic reticulum (Phase 1 reactions) (Richardson et al. 2016).
Primary hepatocytes, taken from living tissue (e.g. biopsy material), are grown in vitro and represent more closely the in vivo situation due to the full range of metabolic enzymes (e.g. aldehyde oxidase and monoamine oxidase), cofactors and membrane transporters (Di et al. 2012b). Since it is not possible to culture primary hepatocytes indefinitely, cryopreservation of hepatocytes was introduced. This resulted in constant availability of the in vitro assay in the drug discovery setting by retaining the full activity during storage of the hepatocytes in liquid nitrogen for 1 year. When comparing assays of liver microsomes with hepatocytes, intrinsic clearance of compounds metabolised over non-CYP pathways was faster in hepatocytes (Di et al. 2012b). On the other hand, the intrinsic clearance of drugs with rate-limiting hepatic uptake was faster in microsomes (Di et al. 2012b).
4.2 In Silico Methods
For the prediction of hepatic metabolic clearance in vivo, the previously mentioned in vitro assays (S9 pool, liver microsomes, hepatocytes) can be scaled to the in vivo situation. For example, the intrinsic clearance of the unbound fraction of the drug in a human liver microsome assay is given in μL/min/mg protein and can be scaled up to the in vivo situation based on information about the level of microsomal proteins per gram of liver and liver weight. The hepatic clearance is also dependent on the amount of drug that comes into contact with the hepatic metabolising enzymes that can further depend on, e.g. hepatic blood flow or fraction unbound in blood. For the hepatic clearance, CLh, most often the well-stirred liver model is used:
where Qh is the hepatic blood flow, fub is the fraction unbound in blood and CLint is the intrinsic hepatic clearance (Pang and Rowland 1977). Assumptions behind this model are an instant equilibrium between hepatocytes and adjacent blood and a homogenous drug distribution in the liver. In contrast, the parallel tube model considers that the drug concentration decreases along the direction of the blood flow (Pang and Rowland 1977).
For the prediction of drug metabolism only with in silico methods , ligand-based approaches or structure-based approaches have been used especially for CYP enzymes. Ligand-based approaches, such as QSAR, pharmacophore-based algorithms or shape-focused models, consider the chemical structure and properties of the drugs, while structure-based approaches also model the interaction between the investigated substrate and the metabolic enzyme (Andrade et al. 2014; de Groot 2006).
5 Excretion
The removal of unaltered drug and its metabolites from the body is known as excretion. Apart from the rate of metabolism, drug clearance from blood is influenced by the biliary and urinary excretion rate of unchanged drug. Drug elimination occurs mainly via the highly perfused primary eliminating organs liver and kidney and is dependent on the physicochemical and structural characteristics of the drugs. Lipophilic drugs with a high molecular weight are often associated with biliary excretion (Ghibellini et al. 2006).
Drug excretion into urine via the kidney, known as renal clearance, is a complex process involving passive glomerular filtration, active tubular secretion and passive and active reabsorption (Paine et al. 2010). If the drug is only cleared by filtration, the renal clearance equals the mathematical product of fraction unbound and glomerular filtration rate (fu × GFR). If the renal clearance exceeds this mathematical product, the drug may be a substrate for active tubular secretion by transporters. If the renal clearance is inferior to this mathematical product, it can be assumed that the drug gets reabsorbed. The importance of renal elimination is highlighted by the fact that 32% of the top 200 prescribed drugs in the United States in 2010 were at least partially excreted unchanged in urine (≥25%) (Morrissey et al. 2013).
5.1 In Vitro Methods
Several in vitro methods can be used to study biliary excretion: sandwich-cultured hepatocytes, suspended hepatocytes, vectoral transport using polarised cell lines, single-cell expression systems and membrane vesicles (Ghibellini et al. 2006).
Sandwich-cultured hepatocytes , from rat or human origin, have the advantage that basolateral uptake and canalicular efflux transport can be studied and metabolic functions are retained (Ghibellini et al. 2006). In contrast to the conventionally cultured hepatocytes, the culturing of hepatocytes between two layers of gelled collagen enhances cell viability and allows the formation of functional bile canalicular networks and polarised excretory function (Swift et al. 2010). Suspended hepatocytes are relatively cheap, easy-to-handle and can be used for up to 4 h (Elaut et al. 2006). Their use is limited to the investigation of uptake mechanisms and metabolism since it is not possible to discriminate canalicular excretion from sinusoidal efflux (Swift et al. 2010). Cell lines (e.g. MDCK), transfected with transporter proteins such as multidrug resistance-associated protein 2 (MRP2) and organic anion transporting polypeptide (OATP) 1B1 and/or 1B3 and grown on a permeable membrane, are used to determine the contribution of an individual transport protein, identify driving forces and identify inhibitors (Ghibellini et al. 2006). While the extrapolation to the in vivo situation is difficult as these cell lines are less representative of hepatocytes (different expression levels of transport proteins, no complete set of transport proteins, metabolic enzymes and cofactors), the transfected systems are routinely used in drug development due to their ease in use and good availability (Ghibellini et al. 2006; Swift et al. 2010). Single-cell expression systems such as Xenopus laevis oocytes can transiently express membrane transporters and channels following the injection of their cRNA (Bröer 2010). These expression systems are mainly used to study the mechanism of transport and the effect of genetic diseases (Ghibellini et al. 2006). Inside-out plasma membrane vesicles from cell lines (e.g. insect or mammalian cells) transfected with specific membrane proteins were used to study polymorphisms and substrate specificity of efflux transporters (Ghibellini et al. 2006). For insect cells, the modification of the membrane composition (addition of cholesterol) results in a similar transporter function to mammalian cells (Caldwell and Yan 2014).
In terms of renal excretion, different in vitro experiments can be used for the processes of passive tubular reabsorption and active tubular secretion and reabsorption. For passive tubular permeability , similar in vitro assays as for intestinal permeability are used with cell lines such as LLC-PK1, MDCK and Caco-2 (Scotcher et al. 2016a). The proximal tubule cell line, LLC-PK1, derived from pig (Sus scrofa) kidney, is grown on permeable filter membranes and has been used for transepithelial transport studies investigating the renal disposition of drugs. Apart from the formation of polarised cell monolayers, this cell line has the benefit of expressing endogenous transport proteins (P-gp, MRP2, BCRP) (Kuteykin-Teplyakov et al. 2010; Takada et al. 2005). Recently, the bidirectional epithelial permeation of 20 compounds was studied in this cell line, and good correlations to human renal clearance of drugs were obtained after upscaling of the in vitro parameters (Kunze et al. 2014). For anionic drugs, however, clearance was underpredicted due to restricted secretion in LLC-PK1 cells indicative of limited activity of organic anion transporters (Kunze et al. 2014). To closer mimic the conditions in the kidney, the apical to basolateral pH gradient should be considered in the experimental design, and the experimental results should be scaled by the corresponding tubular surface area (Scotcher et al. 2016b).
For active tubular secretion and reabsorption , similar in vitro techniques are used as for metabolism or biliary excretion. The range of in vitro assays includes membrane vesicles, transfected cells (e.g. organic anion transporter 1-expressing Chinese Hamster Ovary cells (CHO-OAT1), organic anion transporter 3-expressing human embryonic kidney cells 293 (HEK293-OAT3)), immortalised kidney cell lines, primary cultured renal tubule cells and kidney slices (Scotcher et al. 2016a). Human kidney slices can be used to investigate drug uptake at the basolateral membrane but lack information about tubular reabsorption (Watanabe et al. 2011). Their use is restricted due to the limited tissue availability but, if available, complex studies with multiple transporter substrates or inhibitors can be performed with the full set of endogenous transporters (Scotcher et al. 2016a).
5.2 In Silico Methods
Considering biliary excretion, several in silico models have been developed based on QSAR and compound data of in vivo rat biliary excretion. One of these models was developed using principal component regression analysis based on rat biliary excretion data from 56 compounds and 2D molecular descriptors which revealed hydrophobicity (cLogD) as most important factor for the prediction of biliary excretion (Chen et al. 2010). Another model used similar data from 50 compounds and identified a correlation of polar surface area, the presence of a carboxylic acid moiety and free energy of aqueous solvation with biliary excretion (Luo et al. 2010). A model, based on 217 compounds, was developed using a simple regression tree model with the classification and regression trees (CART) algorithm and revealed higher biliary excretion for relatively hydrophilic and large compounds, especially when anionic or cationic (Sharifi and Ghafourian 2014).
A variety of in silico approaches has been used for the prediction of renal excretion. Allometric models were developed for the prediction of renal clearance in men from animal data (Mahmood 1998; Paine et al. 2011; Lave et al. 2009). Appropriate upscaling of the in vitro result to the in vivo situation is necessary, as for in vitro assays (Kunze et al. 2014). In silico models focusing on the likelihood or extent of renal clearance were developed based on QSAR approaches using Volsurf descriptors (2D numerical molecular descriptors calculated from 3D interaction energy grid maps) or physicochemical and structural descriptors (e.g. log D, H-bond donors, ionisation potential) (Doddareddy et al. 2006; Manga et al. 2003; Dave and Morris 2015). The rate of renal clearance was predicted using in silico models developed with different statistical tools such as partial least squares (PLS) and random forests (RF) based on a human renal clearance data set of 349 drugs with active secretion and net reabsorption (Paine et al. 2010).
A mechanistic kidney model has been developed based on various physiological and anatomical parameters (e.g. nephron size and number, number of proximal tubular cells per gram of kidney, flow rates of tubular fluid and urine and pH values in tubular cells/fluid) and is incorporated in the Simcyp® simulator (Certara, Sheffield, UK) (Jamei et al. 2009). In this model, the nephron is divided into eight segments with three compartments (tubular fluid, cell mass and blood space). The processes integrated in the model include passive permeability across basal and apical membranes of each cell compartment, uptake and efflux transport across the basal and apical membranes of each proximal tubular cell compartment, metabolic clearance in proximal tubular cell compartments and bypass of a fraction of the renal blood flow (no passage through glomerulus, the Loop of Henle and subsequent segments) (Neuhoff et al. 2013). The input needed in terms of drug properties is information about drug binding and ionisation, passive permeability and transporter kinetics. The advantage of such a mechanistic model is that interindividual variability (demographics, gender, disease) can be integrated.
6 Physiologically Based Pharmacokinetic Models
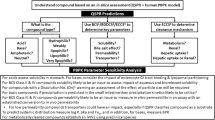
The various previously presented in vitro and in silico ADME tools can be used separately to consider each of the ADME parameters. Linking the information from the different in vitro assays and in silico predictions offers the opportunity to predict in vivo performance, such as plasma concentration profiles and drug concentrations in specific compartments of the body, and to investigate drug-drug interactions. PBPK models were built for this purpose and consider the processes of absorption, distribution, metabolism and excretion of a drug mechanistically (Fig. 13.3).
For drug absorption , the complex compartmental absorption transit models (as described above in Sect. 13.2.2.6) are used in PBPK models together with information about various physiological parameters such as gastrointestinal transit times, luminal fluid volumes, luminal fluid pHs, regional differences in enzyme/transporter density and surface area of the gastrointestinal tract (Jamei et al. 2009). Drug release from different pharmaceutical formulation types such as controlled or modified release systems, enteric-coated granules or tablets and suspensions can also be considered.
Regarding drug distribution, PBPK models consider the whole body using predicted tissue/partition coefficients (as described above in Sect. 13.3.2) and literature data from physiological parameters such as body and organ size, blood flow rates, tissue and blood composition. Tissues include, for example, bone, brain, gut, heart, kidney, liver, lung, pancreas, muscle, skin, spleen and adipose tissue which are usually defined as perfusion-limited tissues. A modification to permeability-limited tissues and integration of active transporter processes using experimental data of transport kinetics are possible. This mechanistic approach allows tracking of the drug concentration in a specific tissue. If such a complex distribution model is not needed, simple compartmental or minimal pharmacokinetic models can be used.
Metabolism and excretion can be integrated at the enzymatic level (metabolizing enzymes and transporters) in the metabolizing and/or eliminating organs which can be considered as perfusion- or permeability-limited tissues (Kostewicz et al. 2014a). For metabolising enzymes or transporters, the input data required includes in vitro information about enzyme kinetics (e.g. Vmax and km) which is scaled to the whole organ with literature information about enzymatic expression in specific organs and organ size. It is also possible to use other in vitro approaches such as hepatocytes with appropriate scaling factors as described above in Sect. 13.4.2.
Apart from physiological data based on the population, additional input data includes drug-dependent parameters, formulation-dependent parameters and information about the design of the virtual trial. For several drug-dependent parameters, it is also possible to use in silico predictions as input information instead of experimental data (e.g. log P, permeability, PPB, RBC partitioning, aqueous and bile micelle-mediated solubility) (Fotaki 2009). As more in vitro, preclinical or clinical data becomes available in the drug discovery process, these data can be used to refine the existing model. PBPK models can also be coupled with pharmacodynamic models to study the relevance of pharmacokinetic changes on therapeutic effects. In recent years, PBPK models were constantly improved by integrating more physiological processes, increasing the mechanistic background of the model and updating physiological information with newly available literature data such as gastrointestinal transit times, demographics and expression of transporters and metabolising enzymes (Rostami-Hodjegan 2012). A main advantage of PBPK models is the integration of population variability in the model to investigate drug product performance in populations that are not usually represented in clinical trials. For example, in the Simcyp® simulator (Certara, Sheffield, UK), default populations include different disease states (obesity, liver cirrhosis, renal impairment, rheumatoid arthritis), ethnicities (Chinese, Japanese, Caucasian), pregnancy and age groups (paediatric, geriatric) (Jamei et al. 2009).
7 Conclusion
Many interrelated processes contribute to determining the pharmacokinetic profile of a drug. A variety of useful in vitro and in silico methods to predict single ADME parameters is available to predict specific processes. The choice of the in vitro and in silico method depends on the drug discovery stage, the drug properties and the available compound data. Current approaches aim to integrate available in silico tools and experimental data from in vitro assays to predict drug plasma profiles using PBPK modelling. With the integration of physiological data from different populations in PBPK models, it is also possible to predict pharmacokinetics in special populations and to estimate interindividual variability. All these tools contribute to the reduction of drug attrition rates in later stages of drug development, to the minimisation of time and costs in drug development and to the reduction of clinical studies. Further advancements are expected when PBPK models are set up in very early stages of drug development and confidence in the model grows by further integrating in vitro, preclinical and clinical data as it becomes available.
References
Abraham MH, Grellier PL, McGill RA (1987) Determination of olive oil–gas and hexadecane–gas partition coefficients, and calculation of the corresponding olive oil–water and hexadecane–water partition coefficients. J Chem Soc Perkin Trans 2:797–803. https://doi.org/10.1039/p29870000797
Alqahtani S, Mohamed LA, Kaddoumi A (2013) Experimental models for predicting drug absorption and metabolism. Expert Opin Drug Metab Toxicol 9:1241–1254. https://doi.org/10.1517/17425255.2013.802772
Amidon GL, Lennernas H, Shah VP et al (1995) A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res 12:413–420
Andrade CH, Silva DC, Braga RC (2014) In silico prediction of drug metabolism by P450. Curr Drug Metab 15:514–525
Avdeef A (2012) Permeability: Caco-2/MDCK. John Wiley & Sons, Inc., Hoboken. https://doi.org/10.1002/9781118286067.ch8
Baker RW (1987) Controlled release of biologically active agents. John Wiley & Sons, New York
Ballard P, Leahy DE, Rowland M (2003) Prediction of in vivo tissue distribution from in vitro data. 2. Correlation between in vitro and in vivo tissue distribution of a homologous series of nine 5-n-alkyl-5-ethyl barbituric acids. Pharm Res 20:864–872. https://doi.org/10.1023/A:1023912318133
Berezhkovskiy LM (2004) Volume of distribution at steady state for a linear pharmacokinetic system with peripheral elimination. J Pharm Sci 93:1628–1640. https://doi.org/10.1002/jps.20073
Bergstrom CA, Holm R, Jorgensen SA et al (2014) Early pharmaceutical profiling to predict oral drug absorption: current status and unmet needs. Eur J Pharm Sci 57:173–199. https://doi.org/10.1016/j.ejps.2013.10.015
Bohets H, Annaert P, Mannens G et al (2001) Strategies for absorption screening in drug discovery and development. Curr Top Med Chem 1:367–383. https://doi.org/10.2174/1568026013394886
Boni JE, Brickl RS, Dressman J (2007) Is bicarbonate buffer suitable as a dissolution medium? J Pharm Pharmacol 59:1375–1382. https://doi.org/10.1211/jpp.59.10.0007
Braun A, Hammerle S, Suda K et al (2000) Cell cultures as tools in biopharmacy. Eur J Pharm Sci 11:S51–S60
Broccatelli F, Salphati L, Plise E et al (2016) Predicting passive permeability of drug-like molecules from chemical structure: where are we? Mol Pharm 13:4199–4208. https://doi.org/10.1021/acs.molpharmaceut.6b00836
Bröer S (2010) Xenopus laevis oocytes. In: Yan Q (ed) Membrane transporters in drug discovery and development: methods and protocols. Humana Press, Totowa, pp 295–310. https://doi.org/10.1007/978-1-60761-700-6_16
Brunner E (1904) Reaktionsgeschwindigkeit in heterogenen Systemen. Z Phys Chem 47U. https://doi.org/10.1515/zpch-1904-4705
Caldwell GW, Yan Z (2014) Optimization in drug discovery: in vitro methods, 2nd edn. Humana Press, Springer, New York
Carbinatto FM, de Castro AD, Evangelista RC et al (2014) Insights into the swelling process and drug release mechanisms from cross-linked pectin/high amylose starch matrices. Asian J Pharm Sci 9:27–34. https://doi.org/10.1016/j.ajps.2013.12.002
Chang C, Swaan PW (2006) Computational approaches to modeling drug transporters. Eur J Pharm Sci 27:411–424. https://doi.org/10.1016/j.ejps.2005.09.013
Chen Y, Cameron K, Guzman-Perez A et al (2010) Structure-pharmacokinetic relationship of in vivo rat biliary excretion. Biopharm Drug Dispos 31:82–90. https://doi.org/10.1002/bdd.692
Dave RA, Morris ME (2015) Quantitative structure-pharmacokinetic relationships for the prediction of renal clearance in humans. Drug Metab Dispos 43:73–81. https://doi.org/10.1124/dmd.114.059857
de Groot MJ (2006) Designing better drugs: predicting cytochrome P450 metabolism. Drug Discov Today 11:601–606. https://doi.org/10.1016/j.drudis.2006.05.001
Di L, Fish PV, Mano T (2012a) Bridging solubility between drug discovery and development. Drug Discov Today 17:486–495. https://doi.org/10.1016/j.drudis.2011.11.007
Di L, Keefer C, Scott DO, Strelevitz TJ et al (2012b) Mechanistic insights from comparing intrinsic clearance values between human liver microsomes and hepatocytes to guide drug design. Eur J Med Chem 57:441–448. https://doi.org/10.1016/j.ejmech.2012.06.043
Di L, Kerns EH, Carter GT (2009) Drug-like property concepts in pharmaceutical design. Curr Pharm Des 15:2184–2194
Di L, Whitney-Pickett C, Umland JP et al (2011) Development of a new permeability assay using low-efflux MDCKII cells. J Pharm Sci 100:4974–4985. https://doi.org/10.1002/jps.22674
Doddareddy MR, Cho YS, Koh HY et al (2006) In silico renal clearance model using classical Volsurf approach. J Chem Inf Model 46:1312–1320. https://doi.org/10.1021/ci0503309
Dokoumetzidis A, Kalantzi L, Fotaki N (2007) Predictive models for oral drug absorption: from in silico methods to integrated dynamical models. Expert Opin Drug Metab Toxicol 3:491–505. https://doi.org/10.1517/17425225.3.4.491
Dressman JB, Amidon GL, Reppas C et al (1998) Dissolution testing as a prognostic tool for oral drug absorption: immediate release dosage forms. Pharm Res 15:11–22. https://doi.org/10.1023/a:1011984216775
Dressman JB, Fleisher D (1986) Mixing-tank model for predicting dissolution rate control or oral absorption. J Pharm Sci 75:109–116
Elaut G, Papeleu P, Vinken M et al (2006) Hepatocytes in suspension. Methods Mol Biol 320:255–263. https://doi.org/10.1385/1-59259-998-2:255
Fotaki N (2009) Pros and cons of methods used for the prediction of oral drug absorption. Expert Rev Clin Pharmacol 2:195–208. https://doi.org/10.1586/17512433.2.2.195
Fotaki N (2011) Flow-through cell apparatus (USP apparatus 4): operation and features. Dissolut Technol 18:46–49. https://doi.org/10.14227/DT180411P46
Fotaki N, Vertzoni M (2010) Biorelevant dissolution methods and their applications in in vitro in vivo correlations for oral formulations. Open Drug Delivery J 4:2–13. https://doi.org/10.2174/1874126601004010002
Galia E, Nicolaides E, Horter D et al (1998) Evaluation of various dissolution media for predicting in vivo performance of class I and II drugs. Pharm Res 15:698–705
Ghibellini G, Leslie EM, Brouwer KL (2006) Methods to evaluate biliary excretion of drugs in humans: an updated review. Mol Pharm 3:198–211. https://doi.org/10.1021/mp060011k
Hansen NT, Kouskoumvekaki I, Jorgensen FS et al (2006) Prediction of pH-dependent aqueous solubility of druglike molecules. J Chem Inf Model 46:2601–2609. https://doi.org/10.1021/ci600292q
Hayduk W, Laudie H (1974) Prediction of diffusion-coefficients for nonelectrolytes in dilute aqueous-solutions. AIChE J 20:611–615. https://doi.org/10.1002/aic.690200329
Heikkinen AT, Baneyx G, Caruso A et al (2012) Application of PBPK modeling to predict human intestinal metabolism of CYP3A substrates - an evaluation and case study using GastroPlus. Eur J Pharm Sci 47:375–386. https://doi.org/10.1016/j.ejps.2012.06.013
Higuchi T (1961) Rate of release of medicaments from ointment bases containing drugs in suspension. J Pharm Sci 50:874–875
Hill AP, Young RJ (2010) Getting physical in drug discovery: a contemporary perspective on solubility and hydrophobicity. Drug Discov Today 15:648–655. https://doi.org/10.1016/j.drudis.2010.05.016
Hinderling PH (1984) Kinetics of partitioning and binding of digoxin and its analogues in the subcompartments of blood. J Pharm Sci 73:1042–1053
Hintz RJ, Johnson KC (1989) The effect of particle size distribution on dissolution rate and oral absorption. Int J Pharm 51:9–17. https://doi.org/10.1016/0378-5173(89)90069-0
Hixson AW, Crowell JH (1931) Dependence of reaction velocity upon surface and agitation. Ind Eng Chem 23:923–931. https://doi.org/10.1021/ie50260a018
Jain N, Yalkowsky SH (2001) Estimation of the aqueous solubility I: application to organic nonelectrolytes. J Pharm Sci 90:234–252. https://doi.org/10.1002/1520-6017(200102)90:2<234::AID-JPS14>3.0.CO;2-V
Jamei M, Marciniak S, Feng K et al (2009) The Simcyp® population-based ADME simulator. Expert Opin Drug Metab Toxicol 5:211–223. https://doi.org/10.1517/17425250802691074
Kennedy T (1997) Managing the drug discovery/development interface. Drug Discov Today 2:436–444. https://doi.org/10.1016/S1359-6446(97)01099-4
Kola I, Landis J (2004) Can the pharmaceutical industry reduce attrition rates? Nat Rev Drug Discov 3:711–715. https://doi.org/10.1038/nrd1470
Kostewicz ES, Aarons L, Bergstrand M et al (2014a) PBPK models for the prediction of in vivo performance of oral dosage forms. Eur J Pharm Sci 57:300–321. https://doi.org/10.1016/j.ejps.2013.09.008
Kostewicz ES, Abrahamsson B, Brewster M et al (2014b) In vitro models for the prediction of in vivo performance of oral dosage forms. Eur J Pharm Sci 57:342–366. https://doi.org/10.1016/j.ejps.2013.08.024
Kostewicz ES, Wunderlich M, Brauns U et al (2004) Predicting the precipitation of poorly soluble weak bases upon entry in the small intestine. J Pharm Pharmacol 56:43–51. https://doi.org/10.1211/0022357022511
Kuentz M (2008) Drug absorption modeling as a tool to define the strategy in clinical formulation development. AAPS J 10:473–479. https://doi.org/10.1208/s12248-008-9054-3
Kunze A, Huwyler J, Poller B et al (2014) In vitro-in vivo extrapolation method to predict human renal clearance of drugs. J Pharm Sci 103:994–1001. https://doi.org/10.1002/jps.23851
Kuteykin-Teplyakov K, Luna-Tortos C, Ambroziak K et al (2010) Differences in the expression of endogenous efflux transporters in MDR1-transfected versus wildtype cell lines affect P-glycoprotein mediated drug transport. Br J Pharmacol 160:1453–1463. https://doi.org/10.1111/j.1476-5381.2010.00801.x
Lambrinidis G, Vallianatou T, Tsantili-Kakoulidou A (2015) In vitro, in silico and integrated strategies for the estimation of plasma protein binding. A review. Adv Drug Deliv Rev 86:27–45. https://doi.org/10.1016/j.addr.2015.03.011
Langenbucher F (1972) Linearization of dissolution rate curves by the Weibull distribution. J Pharm Pharmacol 24:979–981
Lave T, Chapman K, Goldsmith P et al (2009) Human clearance prediction: shifting the paradigm. Expert Opin Drug Metab Toxicol 5:1039–1048. https://doi.org/10.1517/17425250903099649
Lea T (2015) Caco-2 cell line. In: Verhoeckx K, Cotter P, López-Expósito I et al (eds) The impact of food bioactives on health: in vitro and ex vivo models. Springer International Publishing, Cham, pp 103–111. https://doi.org/10.1007/978-3-319-16104-4_10
Lipinski CA, Lombardo F, Dominy BW et al (2001) Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings1PII of original article: S0169-409X(96)00423-1. The article was originally published in advanced drug delivery reviews 23 (1997) 3–25.1. Adv Drug Deliv Rev 46:3–26. https://doi.org/10.1016/S0169-409X(00)00129-0
Liu F, Merchant HA, Kulkarni RP et al (2011) Evolution of a physiological pH 6.8 bicarbonate buffer system: application to the dissolution testing of enteric coated products. Eur J Pharm Biopharm 78:151–157. https://doi.org/10.1016/j.ejpb.2011.01.001
Luo G, Johnson S, Hsueh MM et al (2010) In silico prediction of biliary excretion of drugs in rats based on physicochemical properties. Drug Metab Dispos 38:422–430. https://doi.org/10.1124/dmd.108.026260
Mahmood I (1998) Interspecies scaling of renally secreted drugs. Life Sci 63:2365–2371
Manga N, Duffy JC, Rowe PH et al (2003) A hierarchical QSAR model for urinary excretion of drugs in humans as a predictive tool for biotransformation. QSAR Comb Sci 22:263–273. https://doi.org/10.1002/qsar.200390021
Markopoulos C, Andreas CJ, Vertzoni M et al (2015) In-vitro simulation of luminal conditions for evaluation of performance of oral drug products: choosing the appropriate test media. Eur J Pharm Biopharm 93:173–182. https://doi.org/10.1016/j.ejpb.2015.03.009
Martin YC (2005) A bioavailability score. J Med Chem 48:3164–3170. https://doi.org/10.1021/jm0492002
Mithani SD, Bakatselou V, TenHoor CN et al (1996) Estimation of the increase in solubility of drugs as a function of bile salt concentration. Pharm Res 13:163–167
Morrissey KM, Stocker SL, Wittwer MB et al (2013) Renal transporters in drug development. Annu Rev Pharmacol Toxicol 53:503–529. https://doi.org/10.1146/annurev-pharmtox-011112-140317
Muegge I, Heald SL, Brittelli D (2001) Simple selection criteria for drug-like chemical matter. J Med Chem 44:1841–1846
Nernst W (1904) Theorie der reaktionsgeschwindigkeit in heterogenen systemen. Z Phys Chem 47(1). https://doi.org/10.1515/zpch-1904-4704
Neuhoff S, Gaohua L, Burt H et al (2013) Accounting for transporters in renal clearance: towards a mechanistic kidney model (Mech KiM). In: Sugiyama Y, Steffansen B (eds) Transporters in drug development: discovery, optimization, clinical study and regulation. Springer, New York, pp 155–177. https://doi.org/10.1007/978-1-4614-8229-1_7
Ni PF, Ho NFH, Fox JL et al (1980) Theoretical model studies of intestinal drug absorption V. Non-steady-state fluid flow and absorption. Int J Pharm 5:33–47. https://doi.org/10.1016/0378-5173(80)90048-4
Niederquell A, Kuentz M (2018) Biorelevant drug solubility enhancement modeled by a linear solvation energy relationship. J Pharm Sci 107:503–506. https://doi.org/10.1016/j.xphs.2017.08.017
Noyes AA, Whitney WR (1897) The rate of solution of solid substances in their own solutions. J Am Chem Soc 19:930–934. https://doi.org/10.1021/ja02086a003
Paine SW, Barton P, Bird J et al (2010) A rapid computational filter for predicting the rate of human renal clearance. J Mol Graph Model 29:529–537. https://doi.org/10.1016/j.jmgm.2010.10.003
Paine SW, Menochet K, Denton R et al (2011) Prediction of human renal clearance from preclinical species for a diverse set of drugs that exhibit both active secretion and net reabsorption. Drug Metab Dispos 39:1008–1013. https://doi.org/10.1124/dmd.110.037267
Pang KS, Rowland M (1977) Hepatic clearance of drugs. I. Theoretical considerations of a “well-stirred” model and a “parallel tube” model. Influence of hepatic blood flow, plasma and blood cell binding, and the hepatocellular enzymatic activity on hepatic drug clearance. J Pharmacokinet Biopharm 5:625–653. https://doi.org/10.1007/bf01059688
Peters SA (2012) Physiologically-based pharmacokinetic (PBPK) modeling and simulations. John Wiley & Sons, Inc., Hoboken
Poulin P, Theil FP (2000) A priori prediction of tissue:plasma partition coefficients of drugs to facilitate the use of physiologically-based pharmacokinetic models in drug discovery. J Pharm Sci 89:16–35. https://doi.org/10.1002/(sici)1520-6017(200001)89:1<16::aid-jps3>3.0.co;2-e
Poulin P, Theil FP (2002) Prediction of pharmacokinetics prior to in vivo studies. 1. Mechanism-based prediction of volume of distribution. J Pharm Sci 91:129–156
Richardson SJ, Bai A, Kulkarni AA et al (2016) Efficiency in drug discovery: liver S9 fraction assay as a screen for metabolic stability. Drug Metab Lett 10:83–90. https://doi.org/10.2174/1872312810666160223121836
Rodgers T, Leahy D, Rowland M (2005a) Physiologically based pharmacokinetic modeling 1: predicting the tissue distribution of moderate-to-strong bases. J Pharm Sci 94:1259–1276. https://doi.org/10.1002/jps.20322
Rodgers T, Leahy D, Rowland M (2005b) Tissue distribution of basic drugs: accounting for enantiomeric, compound and regional differences amongst beta-blocking drugs in rat. J Pharm Sci 94:1237–1248. https://doi.org/10.1002/jps.20323
Rodgers T, Rowland M (2006) Physiologically based pharmacokinetic modelling 2: predicting the tissue distribution of acids, very weak bases, neutrals and zwitterions. J Pharm Sci 95:1238–1257. https://doi.org/10.1002/jps.20502
Rodgers T, Rowland M (2007) Mechanistic approaches to volume of distribution predictions: understanding the processes. Pharm Res 24:918–933. https://doi.org/10.1007/s11095-006-9210-3
Rostami-Hodjegan A (2012) Physiologically based pharmacokinetics joined with in vitro-in vivo extrapolation of ADME: a marriage under the arch of systems pharmacology. Clin Pharmacol Ther 92:50–61. https://doi.org/10.1038/clpt.2012.65
Scotcher D, Jones C, Posada M et al (2016a) Key to opening kidney for in vitro–in vivo extrapolation entrance in health and disease: part I: in vitro systems and physiological data. AAPS J 18:1067–1081. https://doi.org/10.1208/s12248-016-9942-x
Scotcher D, Jones C, Rostami-Hodjegan A et al (2016b) Novel minimal physiologically-based model for the prediction of passive tubular reabsorption and renal excretion clearance. Eur J Pharm Sci 94:59–71. https://doi.org/10.1016/j.ejps.2016.03.018
Sharifi M, Ghafourian T (2014) Estimation of biliary excretion of foreign compounds using properties of molecular structure. AAPS J 16:65–78. https://doi.org/10.1208/s12248-013-9541-z
Siepmann J, Peppas NA (2011) Higuchi equation: derivation, applications, use and misuse. Int J Pharm 418:6–12. https://doi.org/10.1016/j.ijpharm.2011.03.051
Stappaerts J, Brouwers J, Annaert P et al (2015) In situ perfusion in rodents to explore intestinal drug absorption: challenges and opportunities. Int J Pharm 478:665–681. https://doi.org/10.1016/j.ijpharm.2014.11.035
Sugano K (2012) Biopharmaceutics modeling and simulations: theory, practice, methods, and applications. John Wiley & Sons, Inc., Hoboken. https://doi.org/10.1002/9781118354339
Swift B, Pfeifer ND, Brouwer KL (2010) Sandwich-cultured hepatocytes: an in vitro model to evaluate hepatobiliary transporter-based drug interactions and hepatotoxicity. Drug Metab Rev 42:446–471. https://doi.org/10.3109/03602530903491881
Takada T, Suzuki H, Sugiyama Y (2005) Characterization of polarized expression of point- or deletion-mutated human BCRP/ABCG2 in LLC-PK1 cells. Pharm Res 22:458–464. https://doi.org/10.1007/s11095-004-1884-9
Takano R, Sugano K, Higashida A et al (2006) Oral absorption of poorly water-soluble drugs: computer simulation of fraction absorbed in humans from a miniscale dissolution test. Pharm Res 23:1144–1156. https://doi.org/10.1007/s11095-006-0162-4
US Pharmacopoeial Convention (2005) USP 29, NF 24: the United States Pharmacopeia, the National Formulary. 711 Dissolution
van de Kerkhof EG, de Graaf IA, Groothuis GM (2007) In vitro methods to study intestinal drug metabolism. Curr Drug Metab 8:658–675
van de Waterbeemd H, Gifford E (2003) ADMET in silico modelling: towards prediction paradise? Nat Rev Drug Discov 2:192–204. https://doi.org/10.1038/nrd1032
Veber DF, Johnson SR, Cheng HY et al (2002) Molecular properties that influence the oral bioavailability of drug candidates. J Med Chem 45:2615–2623
Wang J, Flanagan DR (1999) General solution for diffusion-controlled dissolution of spherical particles. 1. Theory. J Pharm Sci 88:731–738. https://doi.org/10.1021/js980236p
Wang J, Flanagan DR (2002) General solution for diffusion-controlled dissolution of spherical particles. 2. Evaluation of experimental data. J Pharm Sci 91:534–542. https://doi.org/10.1002/jps.10039
Wang QX, Fotaki N, Mao Y (2009) Biorelevant dissolution: methodology and application in drug development. Dissolut Technol 16:6–12. https://doi.org/10.14227/Dt160309p6
Watanabe T, Kusuhara H, Watanabe T et al (2011) Prediction of the overall renal tubular secretion and hepatic clearance of anionic drugs and a renal drug-drug interaction involving organic anion transporter 3 in humans by in vitro uptake experiments. Drug Metab Dispos 39:1031–1038. https://doi.org/10.1124/dmd.110.036129
Westhouse RA, Car BD (2007) Chapter 9 - concepts in pharmacology and toxicology. In: Prendergast GC, Jaffee EM (eds) Cancer immunotherapy. Academic Press, Burlington, pp 149–166. https://doi.org/10.1016/B978-012372551-6/50073-0
Willmann S, Schmitt W, Keldenich J et al (2003) A physiologic model for simulating gastrointestinal flow and drug absorption in rats. Pharm Res 20:1766–1771
Willmann S, Schmitt W, Keldenich J et al (2004) A physiological model for the estimation of the fraction dose absorbed in humans. J Med Chem 47:4022–4031. https://doi.org/10.1021/jm030999b
Willmann S, Thelen K, Lippert J (2012) Integration of dissolution into physiologically-based pharmacokinetic models III: PK-Sim®. J Pharm Pharmacol 64:997–1007. https://doi.org/10.1111/j.2042-7158.2012.01534.x
Yang J, Jamei M, Yeo K et al (2007) Prediction of intestinal first-pass drug metabolism. Curr Drug Metab 8:676–684. https://doi.org/10.2174/138920007782109733
Yu LX, Amidon GL (1999) A compartmental absorption and transit model for estimating oral drug absorption. Int J Pharm 186:119–125. https://doi.org/10.1016/S0378-5173(99)00147-7
Yu LX, Lipka E, Crison JR et al (1996) Transport approaches to the biopharmaceutical design of oral drug delivery systems: prediction of intestinal absorption. Adv Drug Deliv Rev 19:359–376
Zhang X, Shedden K, Rosania GR (2006) A cell-based molecular transport simulator for pharmacokinetic prediction and cheminformatic exploration. Mol Pharm 3:704–716. https://doi.org/10.1021/mp060046k
Acknowledgements
This work has received funding from Horizon 2020 Marie Sklodowska-Curie Innovative Training Networks programme under grant agreement No. 674909 (PEARRL).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Effinger, A., O’Driscoll, C.M., McAllister, M., Fotaki, N. (2018). In Vitro and In Silico ADME Prediction. In: Talevi, A., Quiroga, P. (eds) ADME Processes in Pharmaceutical Sciences. Springer, Cham. https://doi.org/10.1007/978-3-319-99593-9_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-99593-9_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-99592-2
Online ISBN: 978-3-319-99593-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)