Abstract
A hallmark of cancer cells is the deregulated uptake of glucose in an effort to sustain the biosynthetic demands of rapid cellular proliferation. This metabolic process was first described by German physiologist Otto Warburg in the 1920s. In the seminal study, Warburg et al. observed a significant increase in glucose consumption and lactic acid production by cancer cells as compared to normal (non-cancerous) cells, despite aerobic conditions, suggesting an anomalous energy metabolism. Subsequent investigators have corroborated this clinical observation and concluded that cancer cells have the ability to reprogram their energy metabolism such that they rely primarily on glucose catabolism for cellular energy production. In contrast, the energy pathway favored by normal tissue cells under aerobic conditions is the coupling of glycolysis with mitochondrial oxidative phosphorylation, as it yields an approximately 18-fold increase in energy production in comparison to glycolysis alone. However, cancer cells are able to compensate by upregulating glucose transporters (GLUT) on the cell membrane, namely, GLUT1, resulting in an increased uptake of glucose into cells.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- 18F-Fluorodeoxyglucose positron-emission tomography (FDG-PET)
- Computed tomography (CT)
- FDG-PET/CT imaging
- Pancreatic cancer
Introduction
A hallmark of cancer cells is the deregulated uptake of glucose in an effort to sustain the biosynthetic demands of rapid cellular proliferation [1, 2]. This metabolic process was first described by German physiologist Otto Warburg in the 1920s. In the seminal study, Warburg et al. observed a significant increase in glucose consumption and lactic acid production by cancer cells as compared to normal (non-cancerous) cells, despite aerobic conditions, suggesting an anomalous energy metabolism [3]. Subsequent investigators have corroborated this clinical observation and concluded that cancer cells have the ability to reprogram their energy metabolism such that they rely primarily on glucose catabolism for cellular energy production. In contrast, the energy pathway favored by normal tissue cells under aerobic conditions is the coupling of glycolysis with mitochondrial oxidative phosphorylation, as it yields an approximately 18-fold increase in energy production in comparison to glycolysis alone [2]. However, cancer cells are able to compensate by upregulating glucose transporters (GLUT) on the cell membrane, namely, GLUT1, resulting in an increased uptake of glucose into cells [2, 4].
Today, molecular imaging techniques such as integrated 18F-fluorodeoxyglucose positron-emission tomography with computed tomography (FDG-PET/CT) have enabled the visualization and quantification of such cellular processes using molecular probes which mimic endogenous substrates metabolized by cells. FDG is a radioactive glucose analog which is imported into cells via GLUT. However, FDG is not completely metabolized upon entry into cells, in contrast to glucose, and accumulates proportionately to the amount of uptake and metabolic activity within cells [4]. This results in an increased accumulation of FDG within cells, particularly those which have high rates of glycolytic activity as cancers cells.
High levels of FDG uptake have been observed in several solid tumors and associated with poor survival outcomes [5,6,7,8]. This clinical observation has fueled the hypothesis that tumor FDG avidity on FDG-PET/CT may be a surrogate marker for tumor biology. Among patients with pancreatic cancer, tumor characteristics on FDG-PET/CT have been shown to closely correlate with clinical outcomes. For example, pancreatic cancers which have high levels of FDG uptake on pretreatment FDG-PET/CT imaging have been associated with more aggressive histologic tumor grade, early treatment failures, and poor survival outcomes, despite the receipt of multimodality therapy [8,9,10,11,12,13,14]. However, the role of FDG-PET/CT imaging in the management of pancreatic cancer has been somewhat limited and remains poorly defined. This chapter will review the use of FDG-PET/CT imaging as a prognostic tool among patients with pancreatic cancer.
FDG-PET/CT in the Staging of Pancreatic Cancer
At present, FDG-PET/CT is primarily utilized in the context of equivocal extra-pancreatic lesions on staging CT concerning for metastases or in select patients thought to be high risk for harboring occult metastases due to either a large primary tumor, significant elevation of serum carbohydrate antigen 19–9 (CA19–9), or the presence of suspicious lymph nodes on CT imaging. FDG-PET/CT has been shown to improve the detection of occult metastases in patients with pancreatic cancer. In a review including 65 patients with localized pancreatic cancer, clinical staging was performed using CT angiogram and FDG-PET/CT, and the sensitivities for detecting metastases were 57% and 61% using CT angiogram and FDG-PET/CT, respectively. However, when FDG-PET/CT was used in combination with CT angiogram, the sensitivity for detecting metastases increased to 87%. Importantly, the detection of occult metastatic disease with FDG-PET/CT altered the initial plan of care in 7 (11%) of the 65 patients [15]. Similarly, in a review of 71 patients with locally advanced pancreatic cancer who underwent FDG-PET/CT imaging as part of radiation therapy planning, FDG-PET/CT detected occult metastases in 19 (26%) patients which were not identified on CT imaging. In each of these 19 patients, the treatment modality and/or sequencing of therapies were influenced by the diagnosis of metastatic disease [16]. This underscores the importance of accurate staging of disease and the value of multimodality imaging, which may prevent the application of invasive therapies to patients who will derive little oncologic benefit yet endure the associated morbidity.
In the absence of suspected metastatic disease, the routine use of FDG-PET/CT is not recommended [17]. This is largely due to conflicting evidence that FDG-PET/CT imaging improves the accuracy of diagnosis of pancreatic cancer as compared to CT alone. A recent multi-institutional study including 550 patients with suspected pancreatic cancer found FDG-PET/CT to be superior to CT at diagnosing pancreatic cancer. In this study, all patients underwent both multidetector CT and FDG-PET/CT imaging as part of their diagnostic evaluation, and 261 (47%) of the 550 patients were found to have pancreatic cancer. Multidetector CT had a sensitivity and specificity of 88.5% and 70.6%, respectively, at diagnosing pancreatic cancer, whereas FDG-PET/CT had a sensitivity and specificity of 92.7% and 75.8%, respectively [18]. However, prior meta-analyses have demonstrated comparable diagnostic capabilities for CT and FDG-PET/CT [19, 20].
A meta-analysis including 65 studies demonstrated a pooled sensitivity and specificity of 91% and 85%, respectively, for diagnosing pancreatic cancer with conventional CT imaging. In addition, CT was determined to be superior to both magnetic resonance imaging (MRI) and ultrasound (US) at diagnosing pancreatic cancer; FDG-PET/CT was not evaluated in this study [19]. However, in later meta-analysis which included 35 studies, the pooled sensitivity and specificity were 90% and 76%, respectively, for diagnosing pancreatic cancer with FDG-PET/CT imaging. Therefore, the authors of this analysis concluded that FDG-PET/CT may not provide any additional benefit to CT at diagnosing pancreatic cancer. Interestingly, in the discussion of this analysis, the authors proposed the clinical utility of FDG-PET/CT may be disease prognostication, as several studies in the meta-analysis reported a correlation between tumor FDG avidity and survival outcomes [20].
Prognostic Value of Pretreatment FDG-PET/CT Imaging
Value of Pretreatment FDG-PET/CT
There is substantial evidence to suggest that tumor FDG avidity on FDG-PET/CT imaging may be prognostic of patient outcomes. Several parameters to quantify FDG uptake by tumor cells have been evaluated, including maximal standard uptake value (SUV), total lesion glycolysis (TLG), and metabolic tumor volume (MTV); however, SUV may be the most well studied. SUV is a semi-quantitative measure of FDG uptake which is determined by the equation: [region of interest activity (mCi/mL) x patient body weight (g)] / injected FDG dose [21]. The prognostic value of tumor SUV on FDG-PET/CT has been studied in a variety of cancers and shown to correlate with overall survival (OS) outcomes [5,6,7,8].
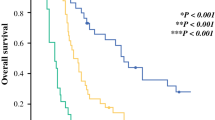
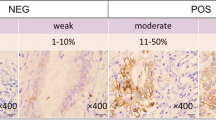
Data is evolving which suggests that pancreatic cancers with high SUVs on FDG-PET/CT may be associated with more aggressive tumor phenotypes and, subsequently, worse survival outcomes. For example, in a review of 102 patients with pancreatic cancer, SUV on pretreatment FDG-PET/CT directly correlated with pathologic tumor grade. The mean SUVs were 4.93, 6.47, and 7.29 for patients with well-, moderately, and poorly differentiated tumors, respectively. Further, the investigators observed an inverse relationship between maximal SUV and OS outcomes (p = 0.002) [9]. In another review including 42 patients with pancreatic cancer who underwent FDG-PET/CT imaging at diagnosis, there was a positive correlation between SUV and histologic grade, though this did not reach statistical significance. However, the investigators did observe a strong correlation between SUV and Ki-67 proliferative index (PI). The mean SUVs were 4.2, 6.0, and 8.6 for patients with low (≤ 5%), moderate (6% to 50%), and high (>50%) Ki-67 PI, respectively (p < 0.001) [11]. These findings suggest that SUV on FDG-PET/CT may be a surrogate marker for the biologic aggressiveness of pancreatic cancers. More compelling evidence to support this hypothesis may be the clinical observation that patients with higher SUVs experience worse survival outcomes as compared to patients with lower SUVs (Figs. 15.1 and 15.2). Table 15.1 summarizes studies which have demonstrated a correlation between tumor SUV on FDG-PET/CT and survival outcomes among patients with pancreatic cancer.
FDG-PET/CT imaging of a 69-year-old female with a pancreatic head mass/neck and serum CA19–9 level of 933 U/mL. Axial fused FDG-PET/CT imaging (a) demonstrating increased FDG uptake throughout the pancreatic head/neck mass with a maximal SUV = 10.6. Axial FDG-PET (b) and noncontrast CT (c) are shown for comparison Endoscopic ultrasound-guided fine needle aspiration confirmed pancreatic cancer. The mass was staged as borderline resectable, and the patient was treated with neoadjuvant therapy prior to surgical resection. The patient developed recurrent disease 7 months from surgery and succumbed to her disease 19 months from initial pancreatic cancer diagnosis
FDG-PET/CT imaging of a 69-year-old male with a pancreatic head mass and significant elevation of serum CA19–9 level to 1775 U/mL. Axial fused FDG-PET/CT imaging (a) demonstrating heterogenous FDG uptake throughout the pancreatic head mass with a maximal SUV = 5.0. Axial FDG-PET (b) and noncontrast CT (c) are shown for comparison. Endoscopic ultrasound-guided fine needle aspiration confirmed pancreatic cancer. The mass was staged as borderline resectable and the patient treated with neoadjuvant therapy prior to surgical resection. The patient developed recurrent disease 28 months from surgery and succumbed to disease 54 months from initial pancreatic cancer diagnosis
In a recent analysis of 105 patients with early-stage pancreatic cancer who underwent FDG-PET/CT imaging prior to resection, the investigators observed a significantly improved OS among patients with a low SUV (<5.1) as compared to those with a high SUV (>5.1). Of the 105 patients, the median OS of the 51 (49%) patients with low SUV was 28 months as compared to 16 months among the 54 (51%) patients with high SUV (p = 0.036) [8]. Similarly, in review of 128 patients with resected pancreatic cancer who underwent preoperative FDG-PET/CT imaging, the investigators used a cutoff of 6.0 to classify tumor SUV as either low (<6.0) or high (≥6.0). Of the 128 patients, the median OS of the 59 (46%) patients with low SUV was 37 months as compared to 18 months among the 69 (54%) patients with high SUV (p < 0.001) [14].
FDG-PET/CT has also been investigated among patients with advanced disease and similarly has demonstrated prognostic value. In a review of 69 patients with unresected, locally advanced pancreatic cancer treated with either chemotherapy, chemoradiation, or radiotherapy alone, the investigators observed a superior OS among patients with low SUV (≤5.5) as compared to those with high SUV (>5.5). In this study, FDG-PET/CT imaging was performed prior to the initiation of all therapies. Of the 69 patients, the median OS of the 34 (50%) patients with low SUV was 16.6 months as compared to 12.6 months among the 35 (50%) patients with high SUV (p = 0.025) [22]. These findings were consistent with a prior analysis which included 55 patients with unresected, locally advanced pancreatic cancer. In this study, patients were treated with chemotherapy and stereotactic body radiotherapy (SBRT). The investigators used the median SUV of 6.2 to classify patients as having either a low SUV (<6.2) or high SUV (≥6.2), and a superior OS was observed among patients with low SUV as compared to those with high SUV (15.3 vs 9.8 months, respectively; p < 0.01) [13].
Other Prognostic FDG-PET/CT Parameters
Volumetric parameters such as TLG and MTV have also been studied and shown to correlate with clinical outcomes among patients with pancreatic cancer [23]. MTV is the total volume of tumor with FDG uptake (usually over a set threshold), and TLG is derived by multiplying the MTV by the mean SUV. In contrast to maximal SUV which only measures FDG uptake in the region of the tumor with the highest level of metabolic activity, MTV and TLG provide a three-dimensional measure of total tumor burden and account for the metabolic heterogeneity among the different cell types comprising the tumor. High MTV and TLG values have been associated with worse survival outcomes among patients with pancreatic cancer. In an analysis of 55 patients with locally advanced pancreatic cancer treated with SBRT, the median MTV was 57.5 for all patients. Of the 55 patients, the median OS of patients with low MTV (<57.5) was 18.0 months as compared to 10.1 months among patients with high MTV (≥57.5; p < 0.01).
Similarly, in a retrospective review of 122 patients with resected pancreatic cancer who underwent FDG-PET/CT imaging prior to surgery, patients were classified as low or high using the MTV and TLG median values of 15.7 and 57.7, respectively, as cutoffs. Of the 122 patients, the median OS of patients with high MTV and high TLG was 9.7 months as compared to 24.2 months among patients with low MTV and low TLG (p < 0.001). In the multivariable hazards analysis, the investigators observed that high MTV (HR: 2.72; p < 0.001), high TLG (HR: 2.79; p < 0.001), and elevated CA19–9 at diagnosis (HR: 2.65; p = 0.006) were independent factors associated with an increased risk of death. These data suggest the metabolic activity of pancreatic cancers on FDG-PET/CT at diagnosis is an important prognostic marker. When used in combination with CA19–9 level, which has been correlated with stage of disease, rates of resection, and survival outcomes, clinicians may be able to provide patients with highly accurate predictions of disease outcomes [24, 25].
FDG-PET/CT as a Predictor of Response to Therapy
Unfortunately, the vast majority of patients with resected pancreatic cancer will succumb to systemic disease recurrence. Among those who undergo up-front surgery followed by adjuvant therapy, the median time to first disease recurrence is approximately 13 months from the time of surgical resection [26, 27]. The timing and patterns of disease recurrence following neoadjuvant therapy and surgery are less clear; this is currently being investigated. Several predictors of disease recurrence have been identified, including positive resection margins, regional lymph node metastases, and perineural invasion – all determined upon pathologic review of surgically resected specimens [28]. At present, there are limited preoperative prognostic markers to stratify patients, with the exception of serum CA19–9 level. As such, identifying patients who are high risk for early treatment failures remains a major challenge in the management of patients with pancreatic cancer. Recent studies evaluating tumor FDG avidity on pretreatment FDG-PET/CT as a predictor of disease recurrence have demonstrated promising results. In a recent review of 46 patients with resected pancreatic cancer, patients with SUV < 6.0 (n = 19, 41%) experienced a median disease-free survival (DFS) of 25 months as compared to 13 months among patients with SUV ≥ 6.0 (n = 27, 59%; p = 0.003). In a multivariable hazards analysis, SUV ≥ 6.0 was associated with a 2.28-fold increased risk of disease recurrence (HR: 2.28; p = 0.024) [29].
FDG-PET/CT has been particularly successful at predicting early disease recurrences after surgery. For example, in a report including 128 patients with resected pancreatic cancer, the investigators observed an increased incidence of early (<6 months) postoperative recurrences among patients with SUV ≥ 6.0 as compared to those with SUV < 6.0 (49% vs 5%; p < 0.001). Of the 128 patients, the 3- and 5-year DFS rates and median DFS were 39.1%, 36.5%, and 23 months, respectively, for patients with SUV < 6.0, as compared to 13.0%, 13.0%, and 6 months among patients with SUV ≥ 6.0 (p < 0.001) [14]. Similarly, in a review of 56 patients treated with a surgery-first approach, 22 (39%) patients experienced disease recurrences within 6 months from surgery. The median SUV on pretreatment FDG-PET/CT among the 22 (39%) patients with early (<6 months) postoperative recurrences was 7.9 as compared to 4.2 among the 34 (61%) patients who did not experience an early recurrence (p = 0.004) [12]. This data suggests that patients with pancreatic cancers which demonstrate high FDG uptake on FDG-PET/CT may be at a higher risk for early disease recurrence due to aggressive tumor biology. This taken in the context of a significantly elevated CA19–9 should warrant careful consideration of the oncologic benefit of invasive therapies such as surgery (Figs. 15.1 and 15.3).
FDG-PET/CT imaging of a 76-year-old male with a pancreatic body mass and serum CA19–9 level of 647 U/mL. Axial fused FDG-PET/CT imaging (a) demonstrating intense FDG uptake throughout the pancreatic body mass with a maximal SUV = 11.9. Axial FDG-PET (b) and noncontrast CT (c) are shown for comparison. Endoscopic ultrasound-guided fine needle aspiration confirmed pancreatic cancer. The mass was staged as resectable. The patient received neoadjuvant therapy prior to surgical resection and adjuvant therapy. The patient developed recurrent disease 8 months from surgery and succumbed to disease 17 months from initial pancreatic cancer diagnosis
Among patients with unresected disease, pretreatment FDG-PET/CT SUV has been shown to be predictive of time to disease progression. In an analysis of 106 patients with unresected, stage II–IV pancreatic cancer who underwent initial staging with FDG-PET/CT, prior to the start of therapy, maximal SUV was shown to correlate with progression-free survival (PFS). Using a SUV cutoff of 4.93, the investigators observed that patients with SUV < 4.93 progressed at median of 385 days as compared to 204 days among patients with SUV > 4.93 [10]. Table 15.2 summarizes studies which have demonstrated a correlation between tumor SUV on FDG-PET/CT and disease progression in patients with pancreatic cancer.
Limitations of FDG-PET/CT
Though published data would suggest a pancreatic mass with a SUV greater than 2.0 to 4.0 on FDG-PET/CT is consistent with pancreatic cancer, differentiating benign inflammatory lesions from pancreatic cancers can be challenging [30, 31]. Similar to pancreatic cancer, inflammatory diseases of the pancreas such as acute/chronic pancreatitis may result in high levels of FDG uptake. A review of 47 patients with pancreatic lesions demonstrated that there is considerable overlap between the SUV ranges of patients with mass-forming pancreatitis (n = 14, 30%) and those with pancreatic cancer (n = 33, 70%). However, at both 1 hour and 2 hours post FDG injection, the SUVs of pancreatic cancers were generally higher than the SUVs of mass-forming pancreatitis (p = 0.001 and p = 0.012, respectively) [32]. In addition, the sensitivity of FDG-PET/CT at diagnosing pancreatic cancer has been shown to be significantly decreased among patients with elevated serum glucose levels, resulting in false negative studies [33]. As such, adequate glycemic control at the time of image acquisition is essential to accurately diagnose pancreatic cancers.
Future Directions
In recent years, integrated FDG-PET/MRI has emerged as an imaging modality for pancreatic cancer. FDG-PET/MRI may offer several potential advantages over FDG-PET/CT, as MRI produces superior imaging of soft tissue pathologies. In addition, the simultaneous acquisition of the FDG-PET and MRI results in optimal fusion of images and minimizes misregistration artifact associated with the sequential acquisition of FDG-PET and CT [34, 35]. Furthermore, FDG-PET/MRI is associated with an approximately 40% to 60% reduction in radiation exposure, which is particularly important among cancer patients who undergo frequent imaging for staging and/or surveillance purposes [34].
FDG-PET/MRI has been shown to be superior to FDG-PET/CT at differentiating pancreatic cancers from benign pancreatic lesions. In a review of 47 patients with pancreatic lesions, the diagnostic accuracy of FDG-PET/MRI at diagnosing pancreatic cancer was 93% and 90.7% for T1-weighted and T2-weighted fusion images, respectively, as compared to 88.4% for FDG-PET/CT [36]. Consistent with these findings, an analysis including 119 patients with pancreatic lesions reported a sensitivity, specificity, and accuracy of 99%, 82.6%, and 96.6%, respectively, at diagnosing pancreatic cancer with FDG-PET/MRI, as compared to 96.9%, 43.5%, and 86.6%, respectively, with FDG-PET/CT [37]. Despite preliminary data demonstrating improved diagnostic capabilities, FDG-PET/MRI has not been readily incorporated into clinical practice. This may be due to its limited availability, higher cost, and the specialized training required by technologists. Additionally, FDG-PET/MRI protocols for assessing pancreatic cancers have not been validated in the current literature.
Conclusion
The clinical utility of FDG-PET/CT in the management of patients with pancreatic cancer is evolving. Current data has demonstrated a strong correlation between tumor FDG avidity and clinical outcomes among patients with pancreatic cancer, suggesting the true value of FDG-PET/CT may be as prognostic tool, rather than diagnostic. Maximal SUV on FDG-PET/CT is an objective measure of tumor metabolic activity which may be a surrogate marker of tumor biology. Early insight into the biologic behavior of pancreatic cancers is extremely valuable information which may improve patient risk stratification and enable the delivery of more personalized and comprehensive treatment.
References
Pavlova NN, Thompson CB. The emerging hallmarks of cancer metabolism. Cell Metab. 2016;23(1):27–47.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Warburg O, Wind F, Negelein E. The metabolism of tumors in the body. J Gen Physiol. 1927;8(6):519–30.
Halbrook CJ, Lyssiotis CA. Employing metabolism to improve the diagnosis and treatment of pancreatic cancer. Cancer Cell. 2017;31(1):5–19.
Swisher SG, Erasmus J, Maish M, Correa AM, Macapinlac H, Ajani JA, Cox JD, Komaki RR, Hong D, Lee HK, Putnam JB Jr, Rice DC, Smythe WR, Thai L, Vaporciyan AA, Walsh GL, Wu TT, Roth JA. 2-Fluoro-2-deoxy-D-glucose positron emission tomography imaging is predictive of pathologic response and survival after preoperative chemoradiation in patients with esophageal carcinoma. Cancer. 2004;101(8):1776–85.
Kim JW, Oh JS, Roh JL, Kim JS, Choi SH, Nam SY, Kim SY. Prognostic significance of standardized uptake value and metabolic tumour volume on (1)(8)F-FDG PET/CT in oropharyngeal squamous cell carcinoma. Eur J Nucl Med Mol Imaging. 2015;42(9):1353–61.
Kim YH, Lee JA, Baek JM, Sung GY, Lee DS, Won JM. The clinical significance of standardized uptake value in breast cancer measured using 18F-fluorodeoxyglucose positron emission tomography/computed tomography. Nucl Med Commun. 2015;36(8):790–4.
Pimiento JM, Davis-Yadley AH, Kim RD, Chen DT, Eikman EA, Berman CG, Malafa MP. Metabolic activity by 18F-FDG-PET/CT is prognostic for stage I and II pancreatic cancer. Clin Nucl Med. 2016;41(3):177–81.
Ahn SJ, Park MS, Lee JD, Kang WJ. Correlation between 18F-fluorodeoxyglucose positron emission tomography and pathologic differentiation in pancreatic cancer. Ann Nucl Med. 2014;28(5):430–5.
Chirindel A, Alluri KC, Chaudhry MA, Wahl RL, Pawlik TM, Herman JM, Subramaniam RM. Prognostic value of FDG PET/CT-derived parameters in pancreatic adenocarcinoma at initial PET/CT staging. AJR Am J Roentgenol. 2015;204(5):1093–9.
Hu SL, Yang ZY, Zhou ZR, Yu XJ, Ping B, Zhang YJ. Role of SUV(max) obtained by 18F-FDG PET/CT in patients with a solitary pancreatic lesion: predicting malignant potential and proliferation. Nucl Med Commun. 2013;34(6):533–9.
Okamoto K, Koyama I, Miyazawa M, Toshimitsu Y, Aikawa M, Okada K, Imabayashi E, Matsuda H. Preoperative 18[F]-fluorodeoxyglucose positron emission tomography/computed tomography predicts early recurrence after pancreatic cancer resection. Int J Clin Oncol. 2011;16(1):39–44.
Schellenberg D, Quon A, Minn AY, Graves EE, Kunz P, Ford JM, Fisher GA, Goodman KA, Koong AC, Chang DT. 18Fluorodeoxyglucose PET is prognostic of progression-free and overall survival in locally advanced pancreas cancer treated with stereotactic radiotherapy. Int J Radiat Oncol Biol Phys. 2010;77(5):1420–5.
Yamamoto T, Sugiura T, Mizuno T, Okamura Y, Aramaki T, Endo M, Uesaka K. Preoperative FDG-PET predicts early recurrence and a poor prognosis after resection of pancreatic adenocarcinoma. Ann Surg Oncol. 2015;22(2):677–84.
Farma JM, Santillan AA, Melis M, Walters J, Belinc D, Chen DT, Eikman EA, Malafa M. PET/CT fusion scan enhances CT staging in patients with pancreatic neoplasms. Ann Surg Oncol. 2008;15(9):2465–71.
Topkan E, Parlak C, Yapar AF. FDG-PET/CT-based restaging may alter initial management decisions and clinical outcomes in patients with locally advanced pancreatic carcinoma planned to undergo chemoradiotherapy. Cancer Imaging. 2013;13(3):423–8.
Network NCC. Pancreatic Adenocarcinoma 2017. Available from: http://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf.
Ghaneh P, Hanson R, Titman A, Lancaster G, Plumpton C, Lloyd-Williams H, Yeo ST, Edwards RT, Johnson C, Abu Hilal M, Higginson AP, Armstrong T, Smith A, Scarsbrook A, McKay C, Carter R, Sutcliffe RP, Bramhall S, Kocher HM, Cunningham D, Pereira SP, Davidson B, Chang D, Khan S, Zealley I, Sarker D, Al Sarireh B, Charnley R, Lobo D, Nicolson M, Halloran C, Raraty M, Sutton R, Vinjamuri S, Evans J, Campbell F, Deeks J, Sanghera B, Wong WL, Neoptolemos JP. PET-PANC: multicentre prospective diagnostic accuracy and health economic analysis study of the impact of combined modality 18fluorine-2-fluoro-2-deoxy-d-glucose positron emission tomography with computed tomography scanning in the diagnosis and management of pancreatic cancer. Health Technol Assess. 2018;22(7):1–114.
Bipat S, Phoa SS, van Delden OM, Bossuyt PM, Gouma DJ, Lameris JS, Stoker J. Ultrasonography, computed tomography and magnetic resonance imaging for diagnosis and determining resectability of pancreatic adenocarcinoma: a meta-analysis. J Comput Assist Tomogr. 2005;29(4):438–45.
Rijkers AP, Valkema R, Duivenvoorden HJ, van Eijck CH. Usefulness of F-18-fluorodeoxyglucose positron emission tomography to confirm suspected pancreatic cancer: a meta-analysis. Eur J Surg Oncol. 2014;40(7):794–804.
Lin E, Alavi A. Pancreatic Cancer. PET and PET/CT: A Clinical Guide. 2nd ed. New York: Thieme; 2005. p. 190–5.
Wang SL, Cao S, Sun YN, Wu R, Chi F, Tang MY, Jin XY, Chen XD. Standardized uptake value on positron emission tomography/computed tomography predicts prognosis in patients with locally advanced pancreatic cancer. Abdom Imaging. 2015;40(8):3117–21.
Xu HX, Chen T, Wang WQ, Wu CT, Liu C, Long J, Xu J, Zhang YJ, Chen RH, Liu L, Yu XJ. Metabolic tumour burden assessed by (1)(8)F-FDG PET/CT associated with serum CA19-9 predicts pancreatic cancer outcome after resection. Eur J Nucl Med Mol Imaging. 2014;41(6):1093–102.
Aldakkak M, Christians KK, Krepline AN, George B, Ritch PS, Erickson BA, Johnston FM, Evans DB, Tsai S. Pre-treatment carbohydrate antigen 19-9 does not predict the response to neoadjuvant therapy in patients with localized pancreatic cancer. HPB (Oxford). 2015;17(10):942–52.
Katz MH, Varadhachary GR, Fleming JB, Wolff RA, Lee JE, Pisters PW, Vauthey JN, Abdalla EK, Sun CC, Wang H, Crane CH, Lee JH, Tamm EP, Abbruzzese JL, Evans DB. Serum CA 19-9 as a marker of resectability and survival in patients with potentially resectable pancreatic cancer treated with neoadjuvant chemoradiation. Ann Surg Oncol. 2010;17(7):1794–801.
Oettle H, Neuhaus P, Hochhaus A, Hartmann JT, Gellert K, Ridwelski K, Niedergethmann M, Zulke C, Fahlke J, Arning MB, Sinn M, Hinke A, Riess H. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310(14):1473–81.
Neoptolemos JP, Palmer DH, Ghaneh P, Psarelli EE, Valle JW, Halloran CM, Faluyi O, O'Reilly DA, Cunningham D, Wadsley J, Darby S, Meyer T, Gillmore R, Anthoney A, Lind P, Glimelius B, Falk S, Izbicki JR, Middleton GW, Cummins S, Ross PJ, Wasan H, McDonald A, Crosby T, Ma YT, Patel K, Sherriff D, Soomal R, Borg D, Sothi S, Hammel P, Hackert T, Jackson R, Buchler MW, European Study Group for Pancreatic C. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet. 2017;389(10073):1011–24.
Groot VP, Rezaee N, Wu W, Cameron JL, Fishman EK, Hruban RH, Weiss MJ, Zheng L, Wolfgang CL, He J. Patterns, timing, and predictors of recurrence following pancreatectomy for Pancreatic ductal adenocarcinoma. Ann Surg. 2018;267(5):936.
Pergolini I, Crippa S, Salgarello M, Belfiori G, Partelli S, Ruffo G, Pucci A, Zamboni G, Falconi M. SUVmax after (18)fluoro-deoxyglucose positron emission tomography/computed tomography: a tool to define treatment strategies in pancreatic cancer. Dig Liver Dis. 2018;50(1):84–90.
Imdahl A, Nitzsche E, Krautmann F, Hogerle S, Boos S, Einert A, Sontheimer J, Farthmann EH. Evaluation of positron emission tomography with 2-[18F]fluoro-2-deoxy-D-glucose for the differentiation of chronic pancreatitis and pancreatic cancer. Br J Surg. 1999;86(2):194–9.
Delbeke D, Rose DM, Chapman WC, Pinson CW, Wright JK, Beauchamp RD, Shyr Y, Leach SD. Optimal interpretation of FDG PET in the diagnosis, staging and management of pancreatic carcinoma. J Nucl Med. 1999;40(11):1784–91.
Kato K, Nihashi T, Ikeda M, Abe S, Iwano S, Itoh S, Shimamoto K, Naganawa S. Limited efficacy of (18)F-FDG PET/CT for differentiation between metastasis-free pancreatic cancer and mass-forming pancreatitis. Clin Nucl Med. 2013;38(6):417–21.
Diederichs CG, Staib L, Glatting G, Beger HG, Reske SN. FDG PET: elevated plasma glucose reduces both uptake and detection rate of pancreatic malignancies. J Nucl Med. 1998;39(6):1030–3.
Matthews R, Choi M. Clinical utility of positron emission tomography magnetic resonance imaging (PET-MRI) in gastrointestinal cancers. Diagnostics (Basel). 2016;6(3).
Yeh R, Dercle L, Garg I, Wang ZJ, Hough DM, Goenka AH. The role of 18F-FDG PET/CT and PET/MRI in pancreatic ductal adenocarcinoma. Abdom Radiol (NY). 2017.
Tatsumi M, Isohashi K, Onishi H, Hori M, Kim T, Higuchi I, Inoue A, Shimosegawa E, Takeda Y, Hatazawa J. 18F-FDG PET/MRI fusion in characterizing pancreatic tumors: comparison to PET/CT. Int J Clin Oncol. 2011;16(4):408–15.
Nagamachi S, Nishii R, Wakamatsu H, Mizutani Y, Kiyohara S, Fujita S, Futami S, Sakae T, Furukoji E, Tamura S, Arita H, Chijiiwa K, Kawai K. The usefulness of (18)F-FDG PET/MRI fusion image in diagnosing pancreatic tumor: comparison with (18)F-FDG PET/CT. Ann Nucl Med. 2013;27(6):554–63.
Lee JW, Kang CM, Choi HJ, Lee WJ, Song SY, Lee JH, Lee JD. Prognostic value of metabolic tumor volume and total lesion glycolysis on preoperative (1)(8)F-FDG PET/CT in patients with pancreatic cancer. J Nucl Med. 2014;55(6):898–904.
Hwang JP, Lim I, Chang KJ, Kim BI, Choi CW, Lim SM. Prognostic value of SUVmax measured by Fluorine-18 Fluorodeoxyglucose positron emission tomography with computed tomography in patients with pancreatic cancer. Nucl Med Mol Imaging. 2012;46(3):207–14.
Sperti C, Pasquali C, Chierichetti F, Ferronato A, Decet G, Pedrazzoli S. 18-Fluorodeoxyglucose positron emission tomography in predicting survival of patients with pancreatic carcinoma. J Gastrointest Surg. 2003;7(8):953–9; discussion 959-960.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Barnes, C.A., Holt, M., Tsai, S. (2019). Role of 18F-Fluorodeoxyglucose Positron-Emission Tomography (FDG-PET) in the Management of Pancreatic Cancer. In: Tsai, S., Ritch, P., Erickson, B., Evans, D. (eds) Management of Localized Pancreatic Cancer . Springer, Cham. https://doi.org/10.1007/978-3-319-98944-0_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-98944-0_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98943-3
Online ISBN: 978-3-319-98944-0
eBook Packages: MedicineMedicine (R0)