Abstract
Diaphragmatic injury remains an elusive diagnosis for many clinicians as these injuries are often asymptomatic or masked by more severe concomitant injuries at time of presentation. A management algorithm focusing on expedient diagnosis and treatment of these injuries is essential to minimize the long-term morbidity and potential mortality associated with untreated diaphragmatic injuries. The most crucial diagnostic tool in diaphragmatic injury diagnosis is a high degree of suspicion. This can be supplemented with adjunctive imaging though management is primarily operative. Clinical presentation of diaphragmatic injury can be stratified based upon chronicity of injury. In the acute setting, most diaphragmatic injuries are often found during intervention for concomitant injury. These injuries are primarily via an abdominal approach. Chronic injuries typically present with symptoms of obstruction or respiratory compromise and are conversely repaired through a thoracic approach. Variations on repair technique depend on additional findings at time of intervention.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Traumatic diaphragmatic injury
- Diaphragmatic injury
- Acute diaphragmatic injury
- Chronic diaphragmatic injury
- Thoracoabdominal trauma
- Penetrating trauma
- Management of diaphragmatic injury
- Trauma management
- Algorithm
- Diaphragm
Algorithmic Approach
-
A.
Diagnosis of diaphragmatic injury in the acute setting presents a unique challenge to many clinicians as these injuries are often asymptomatic or masked by other concomitant injuries. As such, the most important tool in the initial assessment of the patient with diaphragmatic injury is a high index of suspicion [1]. Primary and secondary surveys should be completed as outlined by advanced trauma life support (ATLS) protocol [2]. After establishing that the patient is hemodynamically stable, additional history should include questions regarding the mechanism of injury, severity of impact, and trajectory of any missile-related injuries [3].
-
B.
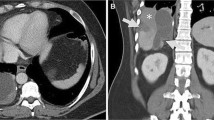
Once hemodynamic stability has been established, adjuncts to history and physical may include the focused abdominal sonography for trauma (FAST) exam (may detect large ruptures associated with blunt force), plain chest radiographs (intra-abdominal contents may be seen in the left hemithorax), or helical computed tomography (CT) scan of the chest, abdomen, and pelvis with 3D reconstructions [3]. It is important to note that these imaging studies are intended more to rule in a diaphragmatic injury rather than to rule one out.
-
C.
If clinical suspicion of a diaphragmatic injury persists after imaging studies, operative intervention to establish a diagnosis is mandated [4]. Operative approach for management of diaphragmatic injury is stratified based upon chronicity of injury, the presence of concomitant injuries, and the hemodynamic stability of the patient [3].
-
D.
For acute injuries in which there is no other indication for laparotomy , a minimally invasive technique may be employed with preference given to thoracoscopy over laparoscopy due to an increased risk of precipitating ipsilateral tension pneumothorax during establishment of pneumoperitoneum [3]. For acute diaphragmatic injuries associated with concomitant injury, operative approach is via laparotomy with trans-diaphragmatic exploration of the ipsilateral thoracic cavity to rule out further hemorrhage or injury [1].
-
E.
In the event that a damage control laparotomy in a hemodynamically unstable patient reveals a diaphragmatic injury, it is considered acceptable to temporarily pack any defect found with laparotomy pads and return for definitive repair once the patient is stabilized [3].
-
F.
For chronic injuries, many favor thoracotomy due to tendency of dense pleural adhesions to form in this setting requiring extensive lysis.
-
G.
Intraoperative technique in all settings is dependent upon size of defect and degree of contamination from associated injury or perforation of a strangulated viscus [5].
-
H.
Because of the natural progression of diaphragmatic defects toward herniation, strangulation, and obstruction or perforation of intra-abdominal viscera, all defects should be repaired regardless of size [3]. All non-viable tissue should be debrided. Primary repairs should be conducted using non-absorbable suture due to an increased risk of recurrence when absorbable sutures are utilized [1].
-
I.
Defects less than 8 cm in size can be repaired primarily. Defects larger than this size favor prosthetic synthetic mesh repair or transposition and re-implantation of the diaphragm cephalad by 1–2 interspaces [1].
-
J.
In the event of gross spillage of intestinal contents, a washout of the thoracic cavity should be done using saline irrigation containing antibiotics [3]. The use of synthetic mesh should be avoided in these cases in favor of autologous tissue (latissimus dorsi, rectus abdominis, or external oblique muscle flaps) or biologic mesh (that is replaced with synthetic mesh at a later date) [1].
-
K.
Postoperatively, the clinician should be mindful of complications such as breakdown of repair, iatrogenic injuries to the phrenic nerve leading to hemiparesis of the diaphragm, atelectasis, empyema, pneumonia, and morbidity related to concomitant injuries [3].

Algorithm 160.1

Algorithm 160.2
References
Mattox K, Moore E, Feliciano D. Trauma. 7th ed. New York: McGraw-Hill Medical; 2013. p. 901–17.
American College of Surgeons. Advanced trauma life support. 9th ed. Chicago: American College of Surgeons; 2013.
Cameron J, Cameron A. Cameron current surgical therapy. 11th ed. Philadelphia: Saunders; 2014. p. 2692–9.
Brunicardi F, Anderson D, Billiar T, Dunn D, Hunter J, Matthews J, Pollock R. Schwartz’s principles of surgery. 9th ed. New York: McGraw-Hill; 2010. p. 324.
Townsend C, Beauchamp R, Evers B, Mattox K. Sabiston textbook of surgery: the biological basis of modern surgical practice. 19th ed. Philadelphia: Saunders; 2012. p. 454–5.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Onursal, E., Vinces, F. (2019). Management Algorithm for Acute and Chronic Diaphragmatic Injuries. In: Docimo Jr., S., Pauli, E. (eds) Clinical Algorithms in General Surgery . Springer, Cham. https://doi.org/10.1007/978-3-319-98497-1_160
Download citation
DOI: https://doi.org/10.1007/978-3-319-98497-1_160
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98496-4
Online ISBN: 978-3-319-98497-1
eBook Packages: MedicineMedicine (R0)